Abstract
Purpose
To report two cases of severe acute corneal hydrops that were resolved by intracameral gas injection alone.
Observations
Case 1 is a 27-year-old woman with bilateral severe keratoconus who developed sequential acute corneal hydrops in the right eye followed by the left eye that were each successfully treated using intracameral 20% sulfur hexafluoride gas injection. Case 2 is a 62-year-old man that developed a large fluid cleft beneath a pre-existing LASIK flap, which resolved with intracameral 20% sulfur hexafluoride gas injection without the need for corneal transplantation.
Conclusions and importance
In acute corneal hydrops, intracameral gas injection to tamponade Descemet's membrane tears with decompression of stromal fluid can be an effective intervention to delay or avoid keratoplasty in individuals whose corneal hydrops does not improve with conventional medical management.
Keywords: Acute corneal hydrops, Intracameral gas injection, Sulfur hexafluoride, LASIK, Keratoconus, Descemet's membrane
1. Introduction
Acute corneal hydrops is characterized by sudden ingress of aqueous fluid into the corneal stroma secondary to a tear in Descemet's membrane. It is a known sequela of conditions that result in bowing and thinning of the cornea, ranging from keratoconus to laser in situ keratomileusis (LASIK)-associated ectasia.1,8 Typically, it is managed medically with hypertonic saline, topical steroids, and aqueous suppressants. For ensuing visually significant scars or persistent edema, deep anterior lamellar keratoplasty or penetrating keratoplasty may be performed.2 Other surgical treatments for unrelenting edema have been reported, such as endothelial keratoplasty and intracameral gas injection as ways to tamponade the posterior corneal fistula.2 In this series, we present three eyes of two patients with severe acute hydrops that resolved with intracameral gas injection. In Case 1, penetrating keratoplasty was ultimately needed in both eyes due to visually significant corneal scars. In Case 2, a large fluid cleft within the LASIK flap interface was completely resolved with sustained visual improvement, allowing the patient to avoid a corneal transplant.
2. Findings
2.1. Case 1
A 27-year-old woman with bilateral severe keratoconus presented with a one-month history of worsening vision, pain, and photophobia in her right eye. Slit lamp exam of the right eye revealed severe acute corneal hydrops with a large stromal fluid cleft (Fig. 1a). Best uncorrected vision was light perception in the right eye and counting fingers at 3 feet in the left eye. Topical 5% sodium chloride solution, homatropine, prednisolone, timolol, and brimonidine were initiated, but two weeks later, clinical worsening was observed with progression of the hydrops and development of a giant stromal fluid cleft and a large tear in Descemet's membrane. The patient was taken to the operating room and, under monitored anesthesia care (MAC), underwent needle decompression of the stromal fluid cleft and intracameral injection of a 20% sulfur hexafluoride (SF6) gas bubble occupying 50% of the anterior chamber. The pupil was dilated to avoid pupillary block, and the patient reclined in a supine position overnight and alternated between 2 h on and 2 h off of supine positioning on post-operative day (POD) 1–2.
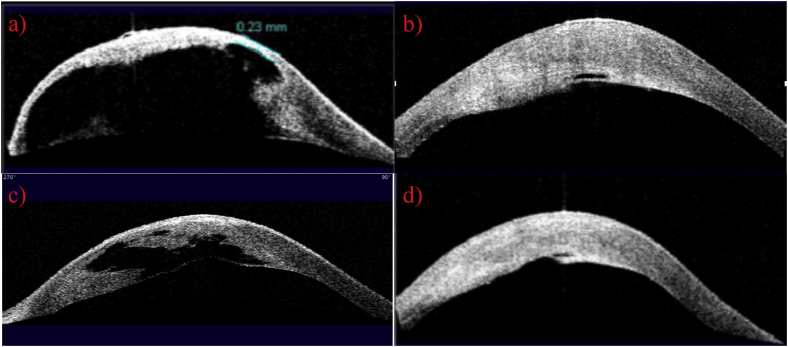
Fig. 1.
Case 1 – (a) Right Eye, Pre-operative Image. Anterior segment (AS)-OCT examination demonstrates severe acute corneal hydrops with a large stromal cleft in the right eye. (b) Right Eye, Post-Operative Month One. AS-OCT examination demonstrates significant reduction in the fluid cleft in the right eye. (c) Left Eye, Pre-operative Image. AS-OCT examination demonstrates severe acute corneal hydrops with a large stromal cleft in the left eye. (d) Left Eye, Post-Operative Week 2. AS-OCT examination reveals significant reduction in the fluid cleft in the left eye.
At her post-operative month one visit, the fluid cleft in the right eye had significantly improved (Fig. 1b). Unfortunately, at the same visit, acute hydrops was observed in the contralateral eye (Fig. 1c). Topical homatropine, 5% sodium chloride, alcaftadine, timolol, and dorzolamide were initiated but no improvement was observed after one month, so the patient underwent the same procedure in that eye: needle decompression of the stromal fluid cleft and intracameral injection of a 20% SF6 gas bubble occupying 50% of the anterior chamber. Two weeks later, the corneal hydrops had substantially improved (Fig. 1d). Eventually, due to visually significant scarring, penetrating keratoplasty (PKP) was performed on both eyes. Her best uncorrected vision was 20/20 OU two years following PKP.
2.2. Case 2
A 62-year-old man presented to the emergency room with three days of worsening vision accompanied by a gritty sensation in the left eye. His prior history included bilateral LASIK followed by severe bilateral post-LASIK ectasia, which he managed with scleral contact lenses. Exam revealed acute left corneal hydrops secondary to a tear in Descemet's membrane with a large fluid cleft at the interface between the LASIK flap and the underlying stromal bed (Fig. 2). Uncorrected visual acuity (UCVA) was 20/100 pinhole (PH) 20/25 in the right eye and 20/100 PH 20/30 in the left eye. Intraocular pressure measured peripheral to the LASIK flap was 10 and 12 mm Hg in the right and left eye, respectively. He was started on 5% sodium chloride ophthalmic solution four times daily (QID), 5% sodium chloride ointment at bedtime, and prednisolone acetate 1% every four hours, which was tapered to QID after four days. His situation worsened, however, and five weeks after the onset of the acute corneal hydrops, best corrected vision decreased to count fingers (CF) at one foot in the left eye. The patient's exam revealed severe microcystic corneal edema affecting 75% of the cornea, including centrally. Prednisolone was changed to difluprednate QID without improvement.
Fig. 2.
Case 2. (a) Slit lamp examination demonstrated severe en face corneal clouding and (b) the presence of a fluid cleft at the LASIK flap interface. (c) AS-OCT revealed the presence of a large fluid cleft secondary to a tear in Descemet's membrane and resulting fistula in the posterior stromal bed in the left eye.
One month later, the patient was taken to the operating room for surgery under topical/MAC anesthesia. A small surgical iridectomy was performed inferiorly using MST forceps (MicroSurgical Technology, Redmond, WA) and MST scissors. An intracameral injection of 20% SF6 gas was then placed to generate a bubble that occupied 90% of the anterior chamber, and a venting incision was then made through the LASIK flap inferonasally to decompress the fluid cleft. The patient was asked to remain in supine position overnight following the operation. On POD1, the fluid cleft was reduced by 85% on anterior segment OCT and clinical evaluation, with a small cleft persisting inferiorly. The patient was placed on prednisolone 1% QID and moxifloxacin QID and was asked to alternate 1h on and 1h off of supine positioning through POD2. By post-operative week one (POW1), his best corrected visual acuity (BCVA) in the left eye improved to 20/40 + 2 with a scleral lens, which was his pre-hydrops visual acuity.
At POW3, the patient reported significant improvement in his vision and no pain. Slit lamp exam revealed a clear cornea with a minimally discernable cleft of fluid in the LASIK flap interface inferiorly and no fluid centrally (Fig. 3). However, a Seidel test was positive at the venting incision, and he was placed on timolol 0.5% twice daily and a bandage contact lens (BCL). At post-operative month (POM) 1, the Seidel test remained slightly positive, and a 10-0 nylon suture was placed through the leaking incision in the minor procedure room. When the patient was seen one week later in the clinic, his cornea was Seidel negative, and his BCVA was 20/50 by pinhole. By POW6, his cornea was compact with no remaining interface fluid, and he had stopped all topical medications. By POM2.5, the patient's vision had stabilized to a BCVA by pinhole of 20/30. At his POM4.5 return visit, his BCVA in his left eye with scleral lens in place was 20/20. Given his improvement and excellent BCVA, the decision was made to continue observation without further surgical intervention. The ASC-OCT images of the patient's cornea at his postoperative visits are shown in Fig. 3(b-f). The appearance of the patient's cornea at POM6 is shown in Fig. 4. The patient has been stable and has not required corneal transplantation in either eye, which as of this publication is 19 months since the intracameral gas procedure.
Fig. 3.
Case 2 – Pre-operative (a) and successive post-operative AS-OCT images illustrating resolution of acute corneal hydrops. Images were taken 2 weeks (b), 4 weeks (c), 3 months (d), 5 months (e), and 7 months (f) post-operatively. The pre-operative image in (a) shows the presence of a stromal fistula within the stromal bed adjacent to the LASIK-flap interface.
Fig. 4.
Case 2 – POM6 image of patient's cornea after intracameral 20% SF6 showing resolution of corneal edema and interfacial fluid. 10-0 nylon suture was placed to close the venting incision and was later removed. BCVA with scleral lens eventually improved to 20/20.
3. Discussion
Acute corneal hydrops, a known sequela of keratoconus and post-LASIK ectasia, results in stromal edema accompanied by sudden onset of impaired vision, light sensitivity, and pain.1,3 In treating acute corneal hydrops, conservative management typically aims to provide symptomatic relief and promote spontaneous resolution of hydrops via aqueous suppressants, steroids, and hyperosmotic agents.2 Pain and photophobia can be managed with a BCL, cycloplegic agents, dark glasses, and topical steroids or non-steroidal anti-inflammatory drugs (NSAIDS).1,2 Administration of broad-spectrum antibiotics should be considered to prevent secondary infections, particularly when the epithelium is compromised and/or if a BCL is used.2
When hydrops persists despite conservative measures, intracameral air or gas injection into the anterior chamber can be an effective first-line intervention.2,4 This procedure may effectively tamponade small to medium-sized Descemet's breaks and in turn promote more rapid wound healing of corneal endothelial cells.2,4 Options for intracameral injection include air or 20% SF6, with the latter offering a longer duration of action that generally reduces the need for repeat injections.5,6
In the setting of larger breaks, intracameral gas injection runs the risk of the bubble traversing into the fluid cleft and failing to form a secure tamponade.2 In these cases, a lamellar transplant procedure such as Descemet's stripping automated endothelial keratoplasty (DSAEK) may seal off the tear and in turn promote resolution of the hydrops.7 If hydrops persists despite these measures, PKP may be indicated, particularly when there is a large intrastromal cleft and/or corneal neovascularization.2
In this case series, Case 1 represents the first report of sequential bilateral acute hydrops that was successively and successfully treated using 20% SF6 gas injection in a single patient. While back-to-back acute hydrops in the same patient is rare, it was not surprising in this patient given her underlying history of keratoconus in both eyes. Although this patient ultimately required PKPs in both eyes due to visually significant scarring, this would not have been a good option initially due to acute inflammation and the large area of hydrops involvement that would have necessitated a large decentered graft extending to the limbus. By promoting apposition of the anterior and posterior stroma through resolution of the hydrops, initial interventions with intracameral gas injection and anterior needle decompression prepared the patient's corneas to ultimately undergo PKPs.
In contrast, Case 2 represents the first reported instance of using 20% SF6 gas injection to treat acute corneal hydrops in a patient with post-LASIK ectasia who had developed a large cleft of interface fluid. The LASIK flap provided an interface in which fluid could collect as it moved anteriorly from the tear in Descemet's membrane and through the fistula that had formed in the posterior stroma (Fig. 3a). What made this patient's case unique was the size and extent of the interface fluid cleft, which turned the LASIK flap into a very large, tense fluid bulla. This put the cornea at risk of rupture through either flap edge dehiscence or a direct tear through the flap.
Observation alone was not considered a good option since the fistula did not spontaneously resolve. PKP would have definitively and simultaneously addressed the patient's underlying problems (the fluid cleft, the posterior fistula, and the ectatic cornea), but it was also the most invasive option and was complicated by the presence of the large cleft and extensive edema, which could have made suturing more challenging. DSAEK to cover the fistula posteriorly was also discussed as an option but would likely still have required a PKP in the future and thus would expend two donor grafts within relatively short succession. The most conservative surgical approach was intracameral gas tamponade alone without a graft. It was not clear pre-operatively whether a gas bubble alone would be sufficient to tamponade a fistula of this size and provide lasting resolution of the fluid cleft. While the venting incision successfully evacuated all the interface fluid at the time of surgery, a slow leak was noted at POW1, implying that the fistula was not completely closed and that fluid was still building up in the stroma. The leak was initially managed with aqueous suppression and a BCL. We posit that a secondary effect of conservatively managing the Seidel leak initially was that it gave the flap and posterior stroma time to gradually adhere together in parallel with complete closure of the fistula. If a suture had been placed earlier or even intraoperatively, the fluid cleft may have re-formed to its pre-operative size, since it was evident that fluid was still tracking into the cleft in the early post-operative period. After the incision was sutured at POM1, the cornea remained stable with no recurrence of the fluid cleft and only mild paracentral scarring overlying the site of the stromal fistula. His BCVA continued to improve and, by POM4.5, was 20/20 with scleral lens in place. The patient has since avoided the need for further intervention or surgery.
4. Conclusions
While medical management of acute hydrops may lead to full symptom resolution in some patients, surgical intervention may be required in refractory cases. 20% SF6 gas injection to tamponade Descemet's tears along with stromal fluid cleft decompression should be considered as an initial intervention before keratoplasty in individuals whose corneal hydrops does not improve despite treatment with aqueous suppression and steroids. Although visual improvement may ultimately require corneal transplantation, as was true for the first case presented herein, intracameral gas injection with fluid decompression alone may be sufficient to restore satisfactory visual acuity, as demonstrated in the second case.
Patient consent
Written informed consent was obtained from patients for publication of these case reports and any accompanying images.
Acknowledgements
Funding: Departmental core grants from Research to Prevent Blindness (RPB) and the National Eye Institute (P30-EY026877) as well as career development awards for author D.M. from RPB and the National Eye Institute (K08EY028176). Author D.M. also acknowledges funding from the E. Matilda Ziegler Foundation for the Blind.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: JJS, HL, CL, DM.
References
- 1.Tuft S.J., Gregory W.M., Buckley R.J. Acute corneal hydrops in keratoconus. Ophthalmology. 1994;101(10):1738–1744. doi: 10.1016/s0161-6420(94)31110-9. [DOI] [PubMed] [Google Scholar]
- 2.Sharma N., Maharana P.K., Jhanji V., Vajpayee R.B. Management of acute corneal hydrops in ectatic corneal disorders. Curr Opin Ophthalmol. 2012;23(4):317–323. doi: 10.1097/ICU.0b013e328354a2a8. [DOI] [PubMed] [Google Scholar]
- 3.Maharana P.K., Sharma N., Vajpayee R.B. Acute corneal hydrops in keratoconus. Indian J Ophthalmol. 2013;61(8):461–464. doi: 10.4103/0301-4738.116062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miyata K., Tsuji H., Tanabe T., Mimura Y., Amano S., Oshika T. Intracameral air injection for acute hydrops in keratoconus. Am. J. Opthalmol. 2002;133:750–752. doi: 10.1016/s0002-9394(02)01437-x. [DOI] [PubMed] [Google Scholar]
- 5.Basu S., Vaddavalli P.K., Ramappa M., Shah S., Murthy S.I., Sangwan V.S. Intracameral perfluoropropane gas in the treatment of acute corneal hydrops. Ophthalmology. 2011;118(5):934–939. doi: 10.1016/j.ophtha.2010.09.030. [DOI] [PubMed] [Google Scholar]
- 6.Panda A., Aggarwal A., Madhavi P. Management of acute corneal hydrops secondary to keratoconus with intracameral injection of sulfur hexafluoride (SF6) Cornea. 2007;26(9):1067–1069. doi: 10.1097/ICO.0b013e31805444ba. [DOI] [PubMed] [Google Scholar]
- 7.Dapena I., Ham L., Melles G.R. Endothelial keratoplasty: DSEK/DSAEK or DMEK - the thinner the better? Curr Opin Ophthalmol. 2009;20(4):299–307. doi: 10.1097/ICU.0b013e32832b8d18. [DOI] [PubMed] [Google Scholar]
- 8.Cooke M.D., Koenig S.B. Spontaneous resolution of acute corneal hydrops in a patient with post-LASIK ectasia. Cornea. 2015 Jul;34(7):835–837. doi: 10.1097/ICO.0000000000000450. [DOI] [PubMed] [Google Scholar]