Abstract
Tubulinopathies are a heterogeneous group of complex cortical malformations that are associated with mutations in tubulin genes. TUBB3 gene mutation is associated with a broader spectrum of central nervous system malformations and constitutes about 10% of all tubulinopathies. The diagnosis may not be immediately apparent on imaging, though the differential diagnosis may be narrowed based on imaging findings and allow for more directed genetic testing. We report a 22-year-old gravida-1 nulliparous female whose routine second trimester fetal ultrasound revealed ventriculomegaly and possible agenesis of the corpus callosum. Fetal magnetic resonance imaging showed severe lateral and third ventriculomegaly and a dysplastic, z-shaped brainstem without any evidence of ocular abnormalities. Genetic testing revealed a pathogenic mutation in TUBB3.
Keywords: Brain malformation, Brainstem kinking, Cerebellar hypoplasia, Fetal ventriculomegaly, Tubulinopathy, TUBB3 mutation
Introduction
Tubulinopathies are a heterogeneous group of complex cortical malformations that are associated with mutations in tubulin genes, that is, TUBA1A, TUBA8, TUBB3, TUBB5, and TUBG1 [1]. A significant portion of the result from de novo mutations. Dysmorphic basal ganglia, lissencephaly, micro-lissencephaly, pachygyria, polymicrogyria, simplified gyral cortical dysplasia, cerebellar hypoplasia, or aplasia and agenesis of the corpus callosum are some of the described malformations associated with tubulin gene mutations. They have a broad spectrum of clinical presentation, severity, and outcome. Clinically, patients present with symptoms ranging from seizures, ocular abnormalities, intellectual dysfunction, motor deficits or even death [2]. Most of the mutations associated with tubulinopathies are inherited as an autosomal dominant pattern; however, few exceptions like TUBA8 have a recessive pattern [1]. Imaging findings can help to narrow the differential diagnosis and allow for more directed genetic testing.
Case report
A 22-year-old gravida-1 nulliparous female with unremarkable maternal past medical history presented for fetal magnetic resonance imaging (MRI) to evaluate ventriculomegaly and possible agenesis of the corpus callosum identified on a routine second trimester anatomy ultrasound. Fetal MRI was obtained at 21 weeks and 5 days gestation on a 3T Phillips Achieva MRI scanner. The MRI demonstrated a single intrauterine female fetus with severe lateral and third ventriculomegaly and a dysplastic, z-shaped brainstem (Figs. 1 and 2). The atria of the lateral ventricles measured up to 15 mm bilaterally. The cerebral aqueduct was not well-visualized, and the fourth ventricle was normal in caliber. The cerebellar vermis was hypoplastic, measuring 5 mm in the craniocaudal dimension. The cisterna magna and the transverse cerebellar diameter were normal in size for gestational age (Fig. 3). There was subjectively decreased volume of supratentorial brain parenchyma noted, though no definite supratentorial cortical malformations were identified. The biparietal diameter was normal for gestational age, measuring 53 mm. No additional fetal anomalies were identified.
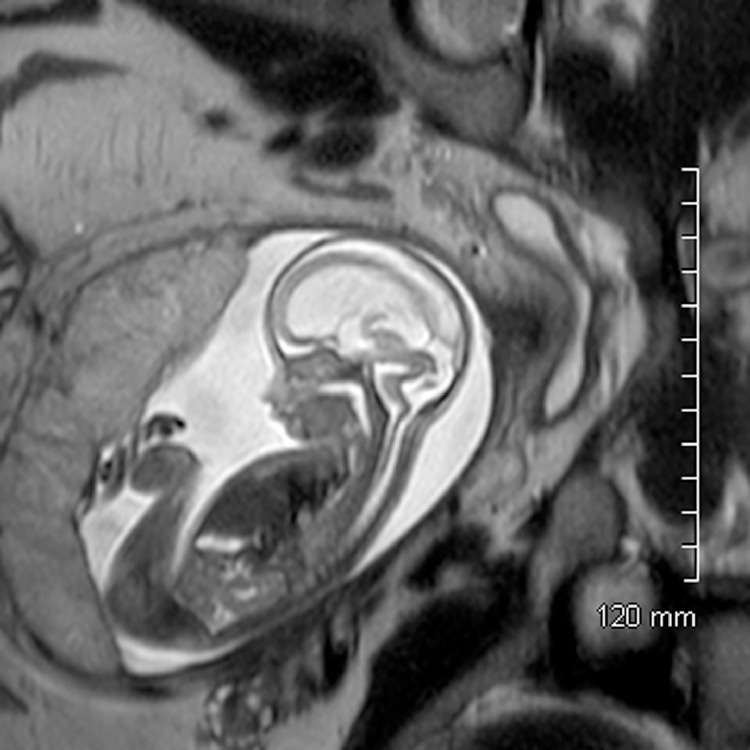
Fig. 1.
Sagittal T2SS image of the fetus demonstrating the kinked or Z-shaped brainstem with severe lateral and third ventriculomegaly and hypoplastic cerebellar vermis.
Fig. 2.
Axial T2SS image through the fetal brain with severe lateral ventriculomegaly.
Fig. 3.
Axial T2SS image through the fetal brain demonstrating normal cerebellar diameter for gestational age.
Following the fetal MRI the parents were able to meet with clinicians specializing in Palliative Care, Genetics, and Neurosurgery. These clinical teams also followed the child after birth. A detailed family history obtained by a genetic counselor revealed no history of birth defects or known genetic disorders.
The child was born at 36 weeks, 4 days, with decelerations during attempted induction of labor which required emergent cesarean section. The infant was apneic at birth with no spontaneous movement or respirations. Apgar scores were 2 at 1 minute and 5 and 5 minutes. Therapeutic hypothermia was initiated. A head ultrasound after birth revealed severe ventriculomegaly and severe brain parenchymal volume loss (Fig. 4). Following discussion with the clinical team, the parents elected to withdraw care and the patient passed away on day 2 of life when ventilator support was withdrawn. Genetic sequencing revealed a de novo pathogenic mutation in TUBB3.
Fig. 4.
Head ultrasound at 1-day old demonstrating massive lateral ventriculomegaly. There is severely thinned brain parenchyma.
Discussion
TUBB3 gene mutations make up about 10% of all tubulinopathies and can have a broad spectrum of central nervous system malformations. A significant portion of tubulinopathies result from de novo mutations [2]. TUBB3 mutation is an exception, wherein most of the reported cases had a familial origin [3,4] Fetal ventriculomegaly is seen in approximately 0.9% of all pregnancies, but fetal brainstem kinking is rarely seen on fetal MRI. The combination of fetal ventriculomegaly and brainstem kinking occurs in certain conditions such as alpha-dystroglycanopathies, tubulinopathies, and X-linked hydrocephalus as described by Amir et al. L1CAM gene mutation is associated with X-linked hydrocephalus and was unlikely in this case given that the fetus was female. Ocular anomalies are often present in alpha-dystroglycanopathies, though the absence at an early gestational age does not necessarily exclude the diagnosis [7]. Few cases have been reported showing ocular anomalies on postnatal imaging in a genetically confirmed alpha-dystroglycanopathy whose fetal MRI showed kinking of the brain stem and ventriculomegaly [5].
Tischfield et al reported cases of variable TUBB3 gene mutations in which most have ocular motility disorder, CFEOM3. Some of these cases had associated intellectual and behavioral impairments, facial paralysis, and later-onset axonal sensorimotor polyneuropathy. MRI of these patients showed dysgenesis of the corpus callosum, anterior commissure and internal capsule, generalized loss of white matter, and basal ganglia dysmorphisms in a majority of cases; however, none of these had cortical dysplasia [6]. Another study by Poirier et al reported 9 cases with TUBB3 mutations with dysplastic basal ganglia, brainstem hypoplasia, agenesis of the corpus callosum, and cerebellar hypoplasia on imaging studies but none of them had ocular defects [7]. In our case, there were no ocular abnormalities, dysplastic basal ganglia, or significant cortical dysplasia noted, though the early timing of the fetal MRI (21 weeks and 5 days) limits evaluation of for these findings. Ultimately, a kinked brain stem on imaging is a sign of severe neurologic malformation and further imaging studies as well as consideration of genetic evaluation may be warranted.
Conclusion
A broad clinical spectrum is commonly seen in tubulinopathies with associated wide range of non-specific prenatal imaging findings. Findings of ventriculomegaly and a kinked brainstem on fetal MRI can narrow the differential diagnosis, allowing for more detailed prenatal counseling and genetic testing. This case demonstrated that findings of ventriculomegaly and a kinked brainstem on fetal MRI can be seen as early as 21 weeks and 5 days gestation in a case which ultimately was proven to be a TUBB3 mutation.
Footnotes
Written informed consent was obtained for this case report.
References
- 1.Bahi-Buisson N, Cavallin M. Tubulinopathies overview. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews((R)). Seattle (WA): University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved; 1993. NBK350554 [bookaccession]. [PubMed]
- 2.Bahi-Buisson N, Poirier K, Fourniol F, Saillour Y, Valence S, Lebrun N. The wide spectrum of tubulinopathies: what are the key features for the diagnosis. Brain. 2014;137(Pt 6):1676–1700. doi: 10.1093/brain/awu082. [DOI] [PubMed] [Google Scholar]
- 3.Gronborg S, Kjaergaard S, Hove H, Larsen VA, Kirchhoff M. Monozygotic twins with a de novo 0.32 mb 16q24.3 deletion, including TUBB3 presenting with developmental delay and mild facial dysmorphism but without overt brain malformation. Am J Med Genet A. 2015;167A(11):2731–2736. doi: 10.1002/ajmg.a.37227. [DOI] [PubMed] [Google Scholar]
- 4.Blumkin L, Leibovitz Z, Krajden-Haratz K, Arad A, Yosovich K, Gindes L. Autosomal dominant TUBB3-related syndrome: fetal, radiologic, clinical and morphological features. Eur J Paediatr Neurol. 2020 doi: 10.1016/j.ejpn.2020.03.001. doi: S1090-3798(20)30044-1 [pii] [DOI] [PubMed] [Google Scholar]
- 5.Amir T, Poretti A, Boltshauser E, Huisman TA. Differential diagnosis of ventriculomegaly and brainstem kinking on fetal MRI. Brain Dev. 2016;38(1):103–108. doi: 10.1016/j.braindev.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Tischfield M, Baris H, Wu C, Rudolph G, Maldergem L, He W. Human TUBB3 mutations perturb microtubule dynamics, kinesin interactions, and axon guidance. Cell. 2010;140(1):74–87. doi: 10.1016/j.cell.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poirier K, Saillour Y, Bahi-Buisson N, Jaglin X, Fallet-Bianco C, Nabbout R. Mutations in the neuronal β-tubulin subunit TUBB3 result in malformation of cortical development and neuronal migration defects. Hum Mol Genet. 2010;19(22):4462–4473. doi: 10.1093/hmg/ddq377. [DOI] [PMC free article] [PubMed] [Google Scholar]