Abstract
Background: Anatomical knowledge about the suprascapular notch is very important in understanding the risk of suprascapular nerve entrapment syndrome. Suprascapular nerve injuries have become commonly recognized as a cause of shoulder pain and dysfunction. This study aimed to describe the morphometrical influence of the suprascapular notch on the course of the suprascapular nerve.
Method: A total of 138 dry human scapulae of both sides of the unknown sex were used. Four measurements were defined and collected for every suprascapular notch: maximum depth (MD), superior transverse diameter (STD), middle transverse diameter (MTD), and total circumferential diameter (TCD).
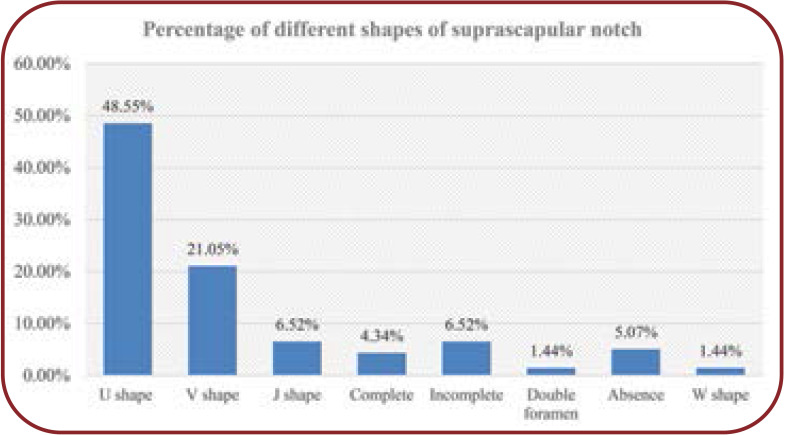
Result: In the present study we found different shapes of suprascapular notches. Out of 138 scapulae, 67 (48.55%) had U-shaped notch, 29 (21.01%) V-shaped notch and 14 (10.14%) J-shaped notch. Nine (6.52%) scapulae had incomplete notch. Two (1.44%) scapulae had large double foramen. Six (4.34%) scapulae had complete suprascapular notch. In seven (5.07%) scapulae, the notch was absent. Interestingly, in two (1.44%) scapulae, we found a W-shaped notch. This observation was unique and not reported anywhere in the literature before.
Conclusion: Anatomical knowledge about the morphology of the suprascapular notch is of extreme importance for clinicians, radiologists, neurosurgeons, and orthopedic surgeons in making a proper diagnosis and for planning the surgical procedures of the shoulder region.
Keywords:suprascapular notch, superior traverse diameter, middle traverse diameter, total circumferential diameter.
INTRODUCTION
The suprascapular notch (SSN) is a small depression on the superior border of the scapula and it forms a tunnel with the superior transverse scapular ligament (STSL). The suprascapular nerve and vein run under the superior transverse ligament. The suprascapular artery runs above the ligament (1, 2). The suprascapular nerve provides motor innervation to the supraspinous and infraspinous muscles and sensory innervation to the rotator cuff muscles and ligaments of the acromioclavicular and shoulder joints. The suprascapular notch is the most common site where the suprascapular nerve is compressed, thus causing nerve injury and entrapment (3). In 1959, Koppel and Thompson (4) first described the suprascapular nerve entrapment syndrome. Traumatic injuries such as scapular, clavicular, and proximal humeral fracture and dislocation of the acromioclavicular or shoulder joint may cause compression of the nerve at the notch (5, 6). Compression of the suprascapular nerve is commonly observed at the suprascapular or spinoglenoid notch, and it causes an entrapment syndrome – an acquired neuropathy. This syndrome is characterized by vague pain on the posterolateral aspect of the shoulder joint with atrophy of the supraspinatus and infraspinatus muscles (7).
This study aims to determine anatomical variations of the suprascapular notch for a better understanding of the possible predisposing factors for suprascapular neuropathy.
MATERIALS AND METHODS
The present study was carried out on 138 dried adult scapulae of unknown sex that were obtained from the Bone bank, Department of Anatomy, BLDE (Deemed to be University) Shri B. M. Patil Medical College and Research Centre Vijayapur, Karnataka, India.
The scapulae that had physical deformities or of unknown age or race were excluded from the study.
All scapulae were grossly examined for the presence or absence of the suprascapular notch. The superior transverse diameter (STD), middle transverse diameter (MTD), maximum depth (MD), and circumference of the notch were measured by using the Vernier caliper. The resulting data were recorded and tabulated. Scapulae of various notch shapes were photographed and documented.
Suprascapular notch morphometry
Superior transverse diameter is the horizontal distance between the superior corners of the suprascapular notch at the superior border of the scapula.
Mid transverse diameter is the horizontal distance between the opposite walls of the suprascapular notch and is perpendicular on distance of maximum depth at its midpoint.
Maximum depth is the distance between the superior corner and the deepest point of the suprascapular notch.
Total circumferential diameter (TCD) of the notch – Thread is placed along the medial end, deepest point and lateral end and length and is measured on a scale.
Morphology
In the present study we categorized 138 dry scapulae according to Natsis (8) classification system and recorded the length of all scapulae with the help of digital Vernier calipers.
Statistical analysis
Calculation was performed using a statistical analysis program, IBM® SPSS® Statistics version 26.
RESULTS
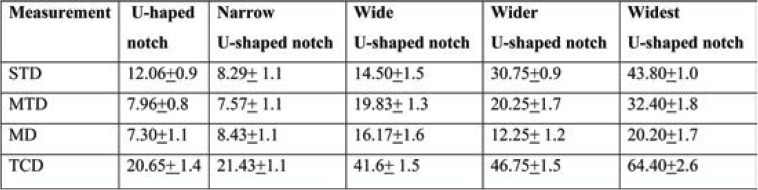
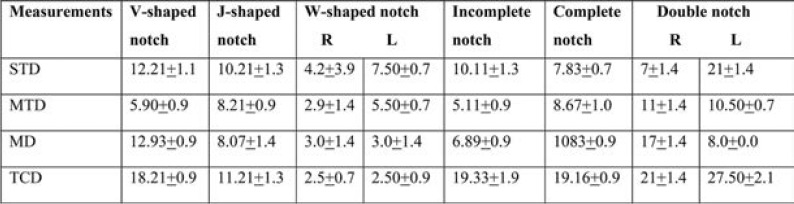
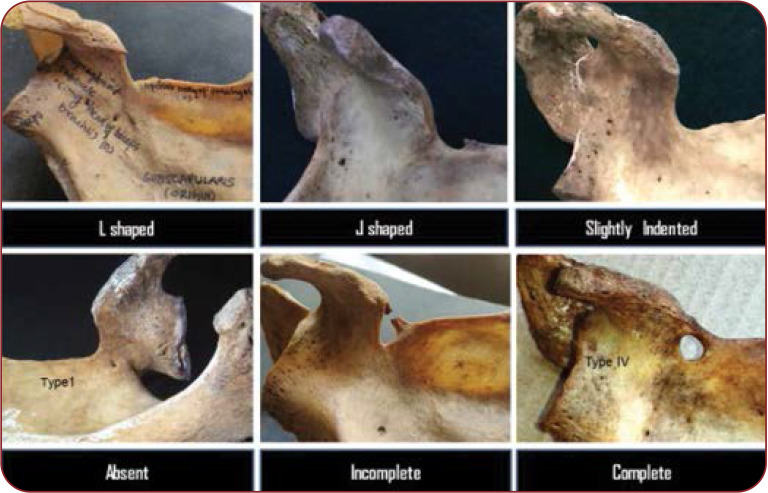
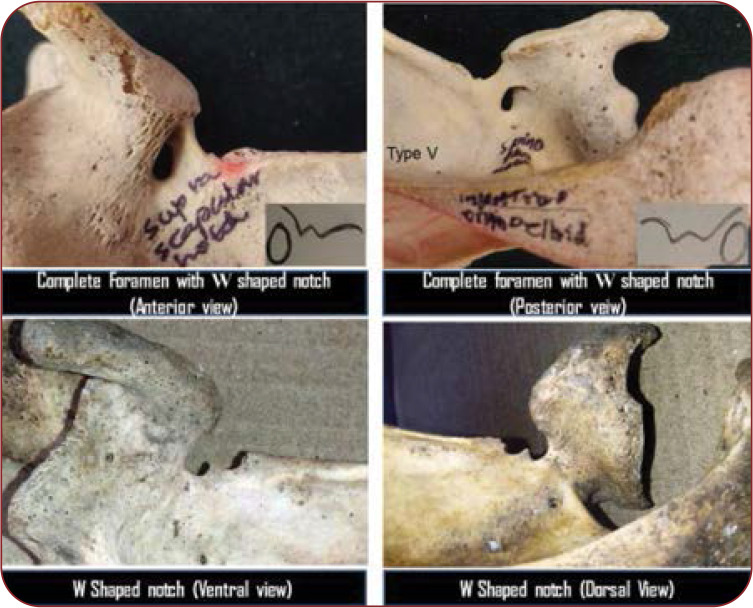
In the present study we examined different types of U-shaped notches at the superior margin of the scapula by using all four parameters (Table 1, Figures 1 and 3). We analysed seven different shapes of the suprascapular notch (Table 2, Figure 2). Of the 138 scapulae, 67 (48.55%) were U-shaped, 29 (21.01%) V-shaped, 14 (10.14%) J-shaped, nine (6.52%) had an incomplete suprascapular notch (Figure 4), two (1.44%) had a double foramen (Figure 6), and two (1.44%) had L-shaped suprascapular notch. The complete ossification of the suprascapular notch was observed in six scapulae (4.34%). Complete absence of the notch was found in seven (5.07%) scapulae. Interestingly, unique W-shaped notches were found in two (1.44%) scapulae (Figure 5).
DISCUSSION
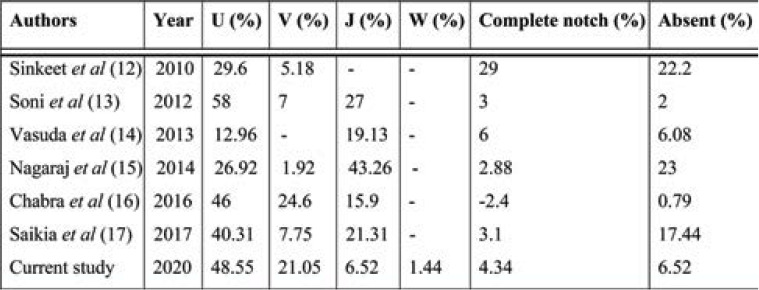
Anatomical knowledge of the shape and size of the suprascapular notch (SSN) is one of the most important risk factors in suprascapular nerve entrapment. The suprascapular foramen is formed between the suprascapular notch and the transverse scapular ligament, which bridges the borders of the notch. The suprascapular nerve, an important branch of the brachial plexus, passes below the suprascapular ligament. The suprascapular vessels generally pass over the transverse scapular ligament (9). The anatomy of different shapes of the suprascapular notch and ossification of suprascapular ligament have been reported by various authors in different populations based on different parameters such as the vertical length of the notch, transverse diameter of the notch, and shape of the notch (10, 11) (Table 3).
Morphometry of the suprascapular notch in our study was comparative with other published reports (Table 3). U-shape was the most commonly seen shape of the suprascapular notch [67 (48.55%) of the 138 dry scapulae], which is in good accordance with previously reported findings (13, 17).
In the present study, we encountered a different type of U-shaped suprascapular notches at the superior border of the scapulae (Figure 3). Measurements revealed that the narrow U-shaped notch had a smaller diameter compared to other types of U-shaped notches, which could be a predisposing factor for suprascapular nerve entrapment.
Of all examined dry scapulae, J-shaped suprascapular notch was found by us in 6.52%, similarly to Saikia et al.’s report (17), and V-shaped notch in 21.05%, similarly to the findings of Chabra et al. (16). V-shaped notches have lesser width than other shapes of the scapular notch, which is the most common causative factor for the suprascapular entrapment syndrome (12) (Figure 3).
A rare, unique W-shaped notch was observed in 1.44% of dry scapulae (Figure 5), which has never been reported in the literature so far. W-shaped notch is proposed as a possible cause of the suprascapular nerve entrapment syndrome due to changed morphology and reduced morphometry. The occurrence of W-shaped notch may be due to developmental abnormality scapula or abnormal attachment or division of the suprascapular ligament or change in the course of suprascapular blood vessels. The presence of an inconspicuous additional notch (W) may cause entrapment of the suprascapular nerve, compressing the suprascapular blood vessels. In their study of 211 cadaveric adult scapulae, Rengachary et al. (18) classified six basic types of a suprascapular notch: type 1=absence of notch; type 2=V-shaped notch; type 3=U-shaped notch; type 4=small V-shaped notch; type 5=U-shaped notch with partial ossification of the suprascapular ligament; and type 6=complete ossification of the suprascapular ligament. But W-shaped notch is not mentioned anywhere in the literature.
We observed another variation of the ossified suprascapular ligament that resulted in two large foramina below the ossified ligament (Figure 6). The shape of the two large foramina was horizontal tetrahedral and vertical oval, respectively. The presence of double large suprascapular foramina is a rare variation of the development and it was proposed as a possible cause of the suprascapular entrapment neuropathy. Formation of large foramen may be due to narrowing or blockage in the main vessels of the limb or abnormal attachment of the suprascapular ligament. Polguj et al. (19) proposed four hypotheses for the formation of the double foramen. The first one was highlighted to be the cause for double foramen. This type of variation may be involved in compression of both nerves and vessels.
We observed the complete absence of the notch at the superior border of the scapula in 5.07% and ossification of the suprascapular ligament in 4.34% of cases (Figure 4), similarly to the report of Vasudha et al. (14) that suggested the absence of the suprascapular notch as a possible risk factor for the suprascapular entrapment syndrome (14).
During the fifth week of intraembryonic life, mesenchymal cells originating from the lateral plate mesoderm migrate along the central axis of the limb bud and their condensation results in the formation of mesenchymal bone. Chondrification occurs in the sixth week of intrauterine life. Ossification of hyaline cartilage models leads to the formation of the suprascapular bony bridge by endochondral ossification, which finally converts the notch into the foramen (20). The anomalous course of the suprascapular nerve and vessels constitutes suprascapular nerve entrapment (3). Other predisposing factors for the suprascapular nerve entrapment are rotator cuff tear, medial retracted supraspinatus muscle with thickened supraspinatus fascia, the hypertrophied subscapularis muscle, double suprascapular foramen, and anomalous position of the suprascapular artery (21, 22). Knowledge about suprascapular ossification is important during operations of post-traumatic peripheral neuropathies and reconstructive nerve grafting following brachial plexus injuries and coracoids process grafting and shoulder arthroplasty procedures (23).
Suprascapular nerve entrapment neuropathy
Anatomical variation in the suprascapular notch and its morphology is important in understanding the suprascapular notch entrapment syndrome. The suprascapular nerve is a mixed nerve branched out from the c5 and c6 roots of the brachial plexus at Erb’s point. Suprascapular nerve travels deep to the suprascapular foramen and spinoglenoid notch, then it divides into motor and sensory branches. Motor branch supply supra and infraspinatus muscle and sensory branch supply subacromial bursa acromioclavicular and glenohumeral joint (24).
Some of the most frequent causes of suprascapular nerve entrapment neuropathy are ganglion cyst and soft tissue tumors. Many published reports highlighted that variations in the morphology of the superior transverse scapular ligament-like ossification, calcification, bifurcation, trifurcation and hypertrophy, and shape of the suprascapular notch are the causative factors for suprascapular neuropathy. The complete absence of the notch and ossification of the suprascapular ligament are the most common variants of the scapula and critical factors for suprascapular entrapment neuropathy (25). It has been hypothesized that suprascapular nerve entrapment was more likely to be associated with a narrow V-shaped notch (26).
Atrophy of the supra- and infraspinatus muscles results in weakness and pain during physical examination. Electromyography, nerve conduction velocity study and magnetic resonance imaging (MRI) are preferred gold standard diagnostic tools for the anatomical demonstration of suprascapular nerve entrapment (27).
CONCLUSION
Anatomical knowledge about the suprascapular notch and ossification of the suprascapular ligament is important to understand the suprascapular nerve entrapment syndrome. A narrow notch shape together with a thick and ossified suprascapular ligament at the superior border of the scapula has been associated with nerve entrapment. An ossified suprascapular ligament and change in the morphology of the notch are of extreme importance for clinicians, radiologists, neurosurgeons and orthopedic surgeons in making a proper diagnosis and for planning the surgical procedures of the shoulder region.
Conflict of interests: none declared
Financial support: none declared.
Acknowledgement: We duly acknowledge with thanks for the cooperation rendered by the Parashuram Katake bone bank in charge Department of Anatomy, Shri B. M. Patil Medical College Research Center, BLDE (Deemed to be University), Vijayapura, Karnataka, India.
TABLE 1.
Measurements of different types of U-shaped suprascapular notch at the superior border of the scapula
TABLE 2.
Measurements of other different shapes of the suprascapular notch at the superior border of the scapula
FIGURE 1.
Diameters of the suprascapular notch used to determine its type. S1: maximal vertical diameter of the notch; S2: transverse diameter of the notch; L1: imaginary line joining the superior corners of the notch. TCD: total circumferential diameter
FIGURE 2.
Percentage of different shapes of suprascapular notch
FIGURE 3.
Different types of U-shaped suprascapular notches at the superior border of the scapula (Types III and II Natsis classification)
FIGURE 4.
Different types of suprascapular notches at the superior border of the scapula (Types I and IV Natsis classification)
FIGURE 5.
W-shaped suprascapular notches at the superior border of the scapula (Type V Natsis classification)
FIGURE 6.
Ossified suprascapular ligament with double foramen at the superior border of the scapula
TABLE 3.
Different shapes of suprascapular notch in different populations studied by various authors
Contributor Information
Ishwar B. BAGOJI, Department of Anatomy, SRI B.M. Patil Medical College, BLDE (deemed to be University), Vijayapur, Karnataka, India
Gavishiddappa A. HADIMANI, Department of Anatomy, SRI B.M. Patil Medical College, BLDE (deemed to be University), Vijayapur, Karnataka, India
R. S. BULGOUD, Department of Anatomy, SRI B.M. Patil Medical College, BLDE (deemed to be University), Vijayapur, Karnataka, India
Vikas DESAI, Department of Dentistry, SHRI B.M. Patil Medical College, Hospital and Research Centre, Vijayapura, Karnataka, India.
KG PRAKASH, Department of Anatomy, Azeezia Institute of Medical Sciences and Research, Meeyyannoor, Kollam, Kerala, India.
Ambadasu BHARATHA, Faculty of Medical Sciences, University of The West Indies, Cave Hill Campus, Barbados, West Indies.
References
- 1.Standring S. Pectoral girdle and upper limb. In: Gray’s Anatomy: The Anatomical Basis of Clinical Practices. 2008. pp. 793–821.
- 2.Thompson W, Kopell H. Peripheral entrapment neuropathies of the upper extremity. N Engl J Med. 1959;25:1261–1265. doi: 10.1056/NEJM195906182602503. [DOI] [PubMed] [Google Scholar]
- 3.Zehetgruber H, Noske H, Lang T, Wurnig C. Suprascapular nerve entrapment. A meta-analysis. Surg Gynecol Obstet. 2002;26:339–343. doi: 10.1007/s00264-002-0392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kopell HP, Thompson WAL. Pain and the frozen shoulder. Surg Gynecol Obstet. 1959;109:92–96. [PubMed] [Google Scholar]
- 5.Bhatia DN, de Beer JF, van Rooeyn KS, du Toit DF. Arthroscopic suprascapular nerve decompression at the suprascapular notch. Arthroscopy. 2006;22:1009–1013. doi: 10.1016/j.arthro.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 6.Shishido H, Kikuchi S. Injury of the suprascapular nerve in shoulder surgery: An anatomic study. J Shoulder Elbow Surg. 2001;10:372–376. doi: 10.1067/mse.2001.115988. [DOI] [PubMed] [Google Scholar]
- 7.Piatt BE, Hawkins RJ, Fritz RC, et al. Clinical evaluation and treatment of spinoglenoid notch ganglion cysts. J Shoulder Elbow Surg. 2002;11:600–604. doi: 10.1067/mse.2002.127094. [DOI] [PubMed] [Google Scholar]
- 8.Natsis K, Totlis T, Tsikaras P, et al. Proposal for classification of the suprascapular notch: A study on 423 dried scapulas. Clin Anat. 2007;20:135–139. doi: 10.1002/ca.20318. [DOI] [PubMed] [Google Scholar]
- 9.Ishwar B Bagoji, Shankarappa D Desai, Gavishiddappa A, et al. Anomalous Sub Scapulo- Suprascapular Arterial Trunk – A Case Report. IOSR Journal of Dental and Medical Sciences. 2012;1:5–6. [Google Scholar]
- 10.Iqbal K, Iqbal R, Khan SG. Anatomical variations in shape of suprascapular notch of scapula. J Morphol Sci. 2010;27:1–2. [Google Scholar]
- 11.Wang HJ, Chen C, Wu LP, et al. Variable Morphology of the Suprascapular Notch: An investigation and Quantitative Measurements in Chinese Population. Clin Anat. 2011;24:47–55. doi: 10.1002/ca.21061. [DOI] [PubMed] [Google Scholar]
- 12.Sinkeet SR, Awori KO, Odula PO, et al. The Suprascapular notch: its Morphology and distance from the glenoid cavity in a Kenyan population. Folia Morphol. 2010;69:241–245. [PubMed] [Google Scholar]
- 13.Soni G, Malik VS, Shukla L, et al. Morphometric analysis of the suprascapular notch. The Internet Journal of Biological Anthropology. 2012;1:20–27. [Google Scholar]
- 14.Vasudha TK, Shetty A, Gowd S, Rajasekhar SSSN. Morphological study on suprascapular notch and superior transverse scapular ligaments in human scapulae. Int J Med Res Health Sci. 2013;4:793–798. [Google Scholar]
- 15.Nagaraj S, Krishnaiah MK, Praveen Kumar M, Sherke AR. Study of morphological variations of suprascapular notch. IOSR Journal of Dental and Medical Sciences. 2014;6:121–123. [Google Scholar]
- 16.Chhabra N, Prakash S, Ahuja MS. Morphometry and morphology of suprascapular notch: Its importance in suprascapular nerve entrapment. Int J Anat Res. 2016;4:2536–2541. [Google Scholar]
- 17.Saikia R, Baishya RJ, Deka B. Variations in the Shape of the Suprascapular Notch in Dry Human Scapula: An Anatomical Study. International Journal of Scientific Study. 2017;1:187–190. [Google Scholar]
- 18.Rengachary SS, Neff JP, Singer PA, Brackett CF. Suprascapular nerve entrapment neuropathy: A clinical, anatomical and comparative study. Part 1: Clinical study. Neurosurg. 1979;4:441–446. doi: 10.1227/00006123-197910000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Polguj MJ, Drzejewski K, Majos A, Topol M. Variations of bifid superior transverse scapular ligament as a possible factor of suprascapular entrapment: an anatomical study. International Orthopaedics. 2012;36:2095–2100. doi: 10.1007/s00264-012-1618-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh Vishram. Textbook of Clinical Embryology. London: Elsevier Health Sciences APAC, 2014. Internet resource.
- 21.Bagoji IB, Hadimani GA, Bannur BM, Patil BG, Bharatha A. Unique branching pattern of the axillary artery: a case report. J Clin Diagn Res. 2013;12:2939–2940. doi: 10.7860/JCDR/2013/5883.3795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hadimani GA, Desai SD, Bagoji IB, Patil BS. Fenestration of Axillary Vein by a Variant Axillary Artery. Kathmandu Univ Med J. 2013;2:162–164. doi: 10.3126/kumj.v11i2.12494. [DOI] [PubMed] [Google Scholar]
- 23.Duparc F, Coquerel D, Ozeel J, et al. Anatomical basis of the suprascapular nerve entrapment, and clinical relevance of the supraspinatus fascia. Surg Radiol Anat. 2010;32:277–284. doi: 10.1007/s00276-010-0631-7. [DOI] [PubMed] [Google Scholar]
- 24.Bagoji IB, Doshi MA, Hadimani GA, et al. Bilateral absence of musculocutaneous nerve and its clinical and surgical implications. Journal of Chemical and Pharmaceutical Research. 2015;4:1479–1481. [Google Scholar]
- 25.Boykin RE, Friedman DJ, Higgins LD, Warner JJ. Suprascapular neuropathy. J Bone Joint Surg Am. 2010;13:2348–2364. doi: 10.2106/JBJS.I.01743. [DOI] [PubMed] [Google Scholar]
- 26.Moen TC, Babatunde OM, Hsu SH, et al. Suprascapular neuropathy: what does the literature show. J Shoulder Elbow Surg. 2012;6:835–846. doi: 10.1016/j.jse.2011.11.033. [DOI] [PubMed] [Google Scholar]
- 27.Hadley MN, Sonntag VK, Pittman HW. Suprascapular nerve entrapment: a summary of seven cases. J Neurosurg. 1986;6:843–848. doi: 10.3171/jns.1986.64.6.0843. [DOI] [PubMed] [Google Scholar]