Abstract
In March 2020, several international organizations started making recommendations regarding the need for prompt coronavirus-based diagnosis in order to prevent its spread among the world's population. The most widely used test for confirmation of COVID-19 is real-time PCR (RT-PCR). This technique uses plastic supplies in its procedures, which are 100% disposable to avoid cross-contamination and biological risks. The scientific community has become increasingly worried because of the environmental impacts associated with the current COVID-19 pandemic, such as medical plastic residues. We classified and estimated the amount of plastic residues generated as a consequence of COVID-19 diagnostic tests and analyzed the relationships of the plastics generated with number of confirmed cases, population size, and gross domestic product in each country. We evidenced that the RT-PCR generates 37.27 g of plastic residues per sample. All patients COVID-19 tested with RT-PCR have generated 15,439.59 tons of plastic residue worldwide, until August 2020. The plastic residues generated by the COVID-19 tests have no relation with size population or gross domestic product of the countries. There is also no relationship between the plastic residues generated by the COVID-19 tests and the confirmed cases. About 97% of the plastic residues from diagnostic tests for coronavirus are incinerated due to their hazardous nature to humans, but toxic chemicals are released into the environment during the process. In the short term, there is a need to reduce plastic waste and improve controls of gas emissions from incineration plants in countries where there is a deficit. In the long term, biodegradable biomedical manufacturing that are free of releasing toxic chemicals when they are incinerated, must be considered.
Keywords: COVID-19, SARS-CoV-2, Plastic, Environment impacts, Human health, Air pollution
Graphical abstract
1. Introduction
SARS-CoV-2 is the virus that causes coronavirus disease by COVID-19, which has been transmitted and spread in a short period of time since its first report in China, becoming a global pandemic (Jin et al., 2020). In March of 2020, the World Health Organization and the Global Emergency Committee called for early and fast detection in order to prevent the spread of the virus (Sohrabi et al., 2020).
Whether a person is infected with SARS-CoV-2 or not is an issue that a medical procedure can reveal by the genome (or parts of the genome) of these viruses, through the antigen (virus coat), or through the antibodies produced by the immune system to deal with the infection (Beeching et al., 2020). Although gene detection is the most complex technique, it is an accurate test because the genes of the virus are totally identified. Therefore, this procedure is currently used to confirm positive and negative SARS-CoV-2 cases. For genetic identification, a swab is needed to get a sample from the nose, mouth and/or lungs, which is placed into a plastic tube containing chemicals preservatives. Afterwards, the sample is extracted and analyzed by means of a Polymerase Chain Reaction (PCR). This technique uses various supplies, most of which are single-use plastics (Tang et al., 2020). In contrast, virus detection by antibodies can detect active infections, but more importantly, it can tell whether a person has been infected in the past, since antibodies can be conserved for a long time after infection. The commercial rapid diagnostic test for SARS-CoV-2 provides qualitative detection of IgG and/or IgM from human serum, whole blood or plasma in approximately 10–15 min; these kits are also mostly made of plastics. The SARS Coronavirus Envelope Protein technique, which is immune reactive with serum from SARS-infected individuals, is the least used due to the fact that antigens can be produced by other viruses, and thus give too many false positive results (Scohy et al., 2020).
The use of plastic is widespread globally, and medical supplies are not an exception (McKeen, 2014). Plastics have become persistent pollutants across-the-board, generating serious effects on the environment and menacing wildlife (Vegter et al., 2014; Wilcox et al., 2015; Worm et al., 2017). These microplastics are also being consumed by humans which could result in adverse side effects (Campanale et al., 2020; Cox et al., 2019; Prata et al., 2020a). Countless international initiatives have been enforced to raise awareness of the effects of plastics, and encourage the use of alternative biodegradable materials (Hermabessiere et al., 2017; Lambert and Wagner, 2017; Li et al., 2016; Rujnić-Sokele and Pilipović, 2017). The majority of health facilities use incineration as a way to inactivate pathogens (such as the virus that causes COVID-19) in biohazardous residues (Ghodrat et al., 2017). Among these wastes are plastics, which when burned release persistent chemical pollutants, such as dioxin and polycyclic aromatic hydrocarbon (PAH) (Li et al., 2019; Wisniewski et al., 2020). These chemical contaminants are highly harmful to humans and environmental health (Andersen et al., 2018; Hylland, 2006; Lv et al., 2020; Mandal, 2005; Mocarelli et al., 1996).
Researchers are concerned about the possible environmental impacts (positive or negative) that could result as a consequence of the ongoing global pandemic. Medical plastic residues undoubtedly possess a potential for negative impacts (Espejo et al., 2020; Klemeš et al., 2020; Prata et al., 2020b; Saadat et al., 2020; Zambrano-Monserrate et al., 2020). Quantifying the global impact of medical plastic residues during this pandemic is difficult but necessary. We recognize the need for diagnostic testing SARS-CoV-2 to identify virus hotspots in urban and rural areas, as well as the implementation of public health measures that could decrease the virus spreading. Single-use plastics and COVID-19 are currently unavoidable. It is necessary however, to assess the environmental impacts of this pandemic and reduce the use of plastic in medical supplies. Many of which are incalculable (such a Personal Protective Equipment, PPE), as there is no source to quantify them. The plastics generated by the COVID-19 tests can be estimated because the number of tests performed is known and the RT-PCR technique is the standard worldwide. The aim of this approach is to estimate the types and the mass of plastic residues from COVID-19 diagnostic tests, as well as discover where these medical plastic residues commonly end up.
Although this article focuses on plastic waste and possible impacts generated by the confirmatory COVID-19 test, we do recognize the important role of this test in detecting COVID-19. This pandemic is a human tragedy, which has already taken the lives of many people. Nevertheless, an analysis of the waste generated in this pandemic can be useful to determine possible negative impacts on health and the environment. Moreover, the information presented here is useful in order to evaluate the short- and long-term alternatives that can mitigate potential negative impacts in the future.
2. Materials and methods
Using standard protocols for RNA extraction and SARS-CoV-2 detection by Geneaid Biotech and Thermo Fisher Scientific, all plastic inputs normally used in COVID-19 diagnostic tests (ranging from sample collection to result) were identified in detail. For this purpose, coronavirus disease tests using real-time PCR (RT-PCR) for COVID-19 were considered because this medical technique is widely used throughout the world. During the next step, the plastic supplies used on each diagnostic test were identified, weighed separately using an EJ-610 balance, with a detection limit of 0.01 g. The weights were analyzed in triplicate after which an average was obtained. The results were expressed in grams. With this information, the plastic residues generated by each RT-PCR diagnostic test was estimated. The available cumulative COVID-19 test data and tests performed per confirmed case of COVID-19 were obtained through the official websites of each country or global databases (Afghanistan, Albania, Algeria, Argentina, Armenia, Australia, Austria, Azerbaijan, Bahrain, Bangladesh, Barbados, Belarus, Belgium, Bhutan, Bolivia, Bosnia and Herzegovina, Brazil, Bulgaria, Burkina Faso, Cameroon, Canada, Chile, China, Colombia, Costa Rica, Croatia, Cuba, Cyprus, Czechia, Denmark, DR Congo, Ecuador, Egypt, El Salvador, Estonia, Ethiopia, Finland, France, Germany, Ghana, Greece, Grenada, Guinea, Hungary, Iceland, India, Indonesia, Iran, Iraq, Ireland, Israel, Italy, Ivory Coast, Jamaica, Japan, Kazakhstan, Kenya, Kosovo, Kyrgyzstan, Latvia, Lebanon, Libya, Lithuania, Luxembourg, Madagascar, Malawi, Malaysia, Maldives, Malta, Mauritius, Mexico, Moldova, Montenegro, Morocco, Mozambique, Myanmar, Nepal, Netherlands, New Zealand, Nigeria, North Korea, Norway, Oman, Pakistan, Palestine, Panama, Paraguay, Peru, Philippines, Poland, Portugal, Qatar, Romania, Russia, Rwanda, Saint Lucia, Saudi Arabia, Senegal, Serbia, Singapore, Slovakia, Slovenia, South Africa, South Korea, Spain, Sri Lanka, Sudan, Sweden, Switzerland, Taiwan, Tanzania, Thailand, Trinidad and Tobago, Tunisia, Turkey, Uganda, Ukraine, United Arab Emirates, United Kingdom, United States, Uruguay, Uzbekistan, Venezuela, Vietnam, Zimbabwe; see Table S1) on August 13, 2020. Data on population and gross domestic product (GDP) were obtained from the “Our World in Data” (Roser et al., 2020). The total weight of plastic residues generated by RT-PCR tests was estimated according to the cumulative COVID-19 tests worldwide, by continent and country levels (total number of tests carried out until August 2020). The plastic residues generated from confirmatory testing for COVID-19 were compared with population and GDP of each country. Furthermore, we identified the mass of medical plastic waste incinerated at global, continent, and country level, as well as the mass of those residues that ended up in landfills. Finally, we indicated environmental and health impacts of the chemical emissions that are produced when medical plastic waste is incinerated.
3. Results
3.1. Identification and classification of plastic residues from a single RT-PCR tests for coronavirus disease
Worldwide single Real-time Polymerase Chain Reaction (RT-PCR) test, using disposable plastics in several of its steps were identified (Table 1 ). The plastics used are listed below, the procedure for collected samples is made by using a 10 cm plastic swab (2.89 g), which is inserted into a 5 ml falcon plastic tube (3.31 g). Once in the laboratory, the sample is transferred into 15 ml falcon plastic tube (6.93 g) using a micropipette with a 1000 μl plastic tip (0.70 g), and then the RNA extraction is performed. An automatic RNA extraction was considered, as it generates less plastic residues and is currently used for this purpose. The samples are transferred into commercial plastic vessels (114.5 g per eight samples) using single-use Pasteur plastic pipettes (1.25 g). At this stage, reagents are added to Eppendorf plastic tubes (0.98 g per twenty-four samples) by means of a micropipette using a 200 μl plastic tip (0.25 g per twenty-four samples). Automatic sample homogenization is performed using 1000 μl plastic tips (0.70 g). The RNA extraction equipment uses three buffers that come with 1 l disposable plastic bottle (88.7 g per bottle); each buffer container holds 400 samples. Following the extraction, the sample is placed into Eppendorf plastic tubes (0.98 g) using a 200 μl tipped plastic micropipette (0.25 g). The plastic estimation for PCR reaction was based on TaqMan™ 2019-nCoV Assay Kit v1 (Applied Biosystems). A master-mix is performed in a 1.5 ml screw-capped microcentrifuge plastic tube (0.98 g), in which the Master Mix (4×), the 2019-nCoV assay (20×), the RNAse P assay (20×) 1.25 and the RT-PCR grade water all well mixed. Each master-mix in a 1.5 ml screw-capped microcentrifuge plastic tube is just for 40 samples. The master mix has several formats, but the biggest is a 10 ml bottle that allows 16,000 reactions. A plastic cryovial (2.22 g) containing the other reagents for just 50 reactions of 25uL each. Aerosol plastic barrier tips are used per each transfer of samples (2.49 g per tip). Finally, to read the samples, these are placed into a 96-well PCR plastic plate (23.6 g) and covered with MicroAmp™ Optical Adhesive Film (7 g); it must be considered that each plate includes positive and negative controls, thus 40 tests are made per plate. Therefore, each RT-PCR diagnostic test for COVID-19 uses 37.27 g of disposable plastics.
Table 1.
Identification and classification of the plastic residues derived from a single RT-PCR tests for coronavirus disease.
| Step | Supply | Usage description | Plastic grams per unit | Quantity for a single RT-PCR sample | Plastic grams for a single RT-PCR sample | Plastic type | Final disposal |
|---|---|---|---|---|---|---|---|
| Collected samples | 10 cm plastic swab | Sample extraction | 2.89 | 1 | 2.89 | Polyester | Incineration |
| 5 ml falcon tube | Sample transport | 3.31 | 1 | 3.31 | Polypropylene | Incineration | |
| RNA extraction | 15 ml falcon tube | Laboratory sample transfer | 6.93 | 1 | 6.93 | Polypropylene | Incineration |
| 1000 μl plastic tip | Sample transfer into the falcon tube | 0.7 | 1 | 0.7 | Polypropylene | Incineration | |
| Commercial plastic vessels | Vessels for automatic RNA extraction | 114.5 | 1 for 8 samples | 14.3125 | polyethylene | Incineration | |
| Pasteur plastic pipettes | Sample transfer into the plastic vessels | 1.25 | 1 | 1.25 | polyethylene | Incineration | |
| Eppendorf plastic tubes | Reagents | 0.98 | 1 for 24 samples | 0.040833333 | Polypropylene | Landfill | |
| 200 μl plastic tip | Reagent transfer | 0.25 | 1 for 24 samples | 0.010416667 | Polypropylene | Landfill | |
| 1000 μl plastic tips | Sample homogenization | 0.7 | 1 | 0.7 | Polypropylene | Incineration | |
| Buffers plastic bottle | Buffers container | 88.7 | 3 for 24 samples | 0.66525 | Tereftalato de polietileno | Landfill | |
| 200 μl tipped plastic | Transfer to eppendof tubes | 0.25 | 1 | 0.25 | Polypropylene | Incineration | |
| Eppendorf plastic tubes | Final container for transfer to PCR amplification | 0.98 | 1 | 0.98 | Polypropylene | Incineration | |
| PCR amplification | 2019-nCoV (ORF1ab) (Tube 1) FAM™ dye 75 μL 20× | Reagent for master-mix | 2.22 | 1 for 50 samples | 0.0444 | Polypropylene | Landfill |
| 2019-nCoV (S Protein) (Tube 2) FAM™ dye 75 μL 20× | Reagent for master-mix | 2.22 | 1 for 50 samples | 0.0444 | Polypropylene | Landfill | |
| 2019-nCoV (N Protein) (Tube 3) FAM™ dye 75 μL 20× | Reagent for master-mix | 2.22 | 1 for 50 samples | 0.0444 | Polypropylene | Landfill | |
| RNase P Assay (Tube 4) | Reagent for master-mix | 2.22 | 1 for 1000 samples | 0.00222 | Polypropylene | Landfill | |
| Eppendorf plastic tubes | Master-mix container | 0.98 | 1 for 40 samples | 0.0245 | Polypropylene | Landfill | |
| Aerosol plastic barrier tips | Transfer of master mix reagents | 2.49 | 5 for 40 samples | 0.31125 | Polypropylene | Landfill | |
| Aerosol plastic barrier tips | Transfer of samples to 96-well PCR plastic plate | 2.49 | 1 | 2.49 | Polypropylene | Incineration | |
| MicroAmp™ Optical Adhesive Film | Reading by PCR | 7 | 1 for 40 samples | 0.175 | Polyester | Incineration | |
| 96-well PCR plastic plate | Reading by PCR | 23.6 | 1 for 40 samples | 0.59 | Polypropylene | Incineration | |
| Optical plastic cap | Reading by PCR | 5 | 12 for 40 samples | 1.5 | Polypropylene | Incineration | |
| TaqPath™ 1-Step RT-qPCR Master Mix, CG | Reading by PCR | 10.96 | 1 for 1600 samples | 0.00685 | Polypropylene | Landfill |
3.2. Plastic residues at global, continent and country levels produced with diagnostic tests for COVID-19
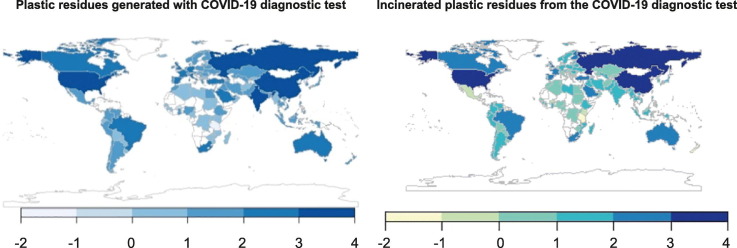
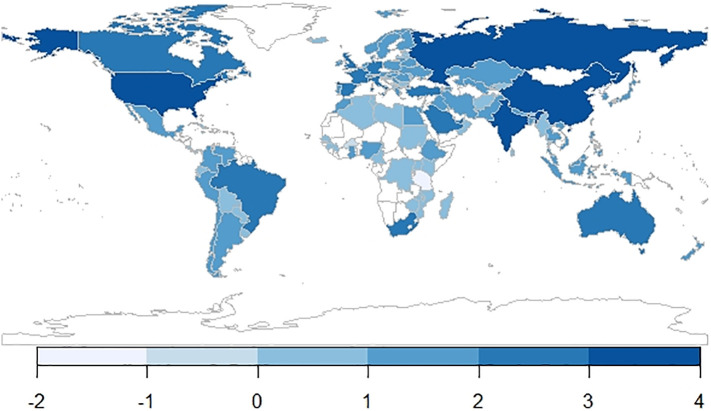
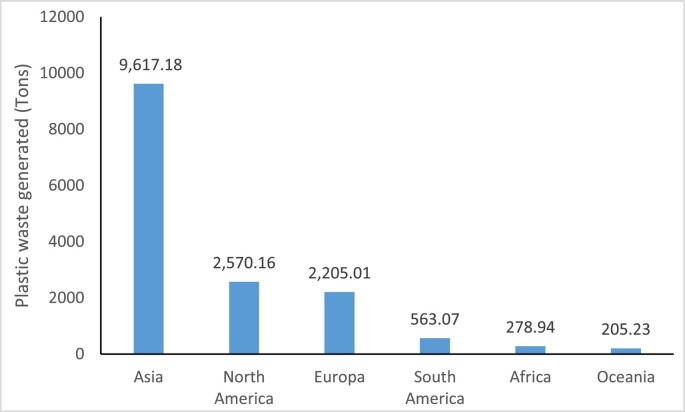
The mass of global plastic residues from RT-PCR tests for COVID-19 are indicated in Fig. 1 . The cumulative tests for coronavirus disease (COVID-19) at the global level are shown in Table S1. According to the information available, we estimated that a mass of 15,439.59 tons of plastic residues have been generated worldwide as a consequence of using the RT-PCR diagnostic tests until August 2020. By continent (Fig. 3), the plastic waste generated by RT-PCR diagnostic test are the following in decreasing order; Asia (62.29%), North America (16.65%), Europe (14.28%), South America (3.65%), Africa (1.81%) and Oceania (1.33%). The ten countries with the most plastic residues are: China (38.62%), United States (15.38%), Russia (7.40%), India (6.48%), United Kingdom (3.33%), Germany (1.93%), Italy (1.67%), Spain (1.61%), United Arab Emirates (1.38%) and Turkey (1.27%). Of all the countries recorded in Fig. 1, these 10 countries represent 79.07% of all plastic residues generated with RT-PCR tests for coronavirus.
Fig. 1.
World map of plastic residues (Log-tonnes) derived from RT-PCR tests for COVID-19 (our design with data from Table S2).
Fig. 3.
Plastic residues (tonnes) derived from RT-PCR tests for coronavirus disease by continent (our design with data from Table S2).
Unlike other plastic residues (e.g., domestic garbage), medical plastic residues derived from COVID-19 tests have no correlation to population size nor to a country's gross domestic product. There is also no relationship between the plastic residues from COVID-19 tests and confirmed cases for coronavirus. This lack of correlation is because most COVID-19 tests carried out depend more on political decisions of health authorities of each country.
Of all the plastics used in confirmatory testing for COVID-19, 89.99% (33.54 g) correspond to polypropylene, 8.22% (3.06 g) to polyester, and 1.78% (0.66 g) to polyethylene.
3.3. Fate and impacts on the health due to plastic residues from confirmatory testing for COVID-19
Currently, management of the final disposal of plastic waste generated by the RT-PCR test for COVID-19 worldwide depends principally on whether it is biohazardous waste, biological samples possibly exposed to COVD-19, or non-biohazardous waste which correspond mainly to plastic residues that have been in contact with reagents and not directly with biological samples. Biohazardous plastic residues are commonly incinerated, representing about 97% of the total plastic residues. These plastic residues correspond to 91.50% (33.01 g) of polypropylene, 8.49% (3.06 g) to polyester, and 0.01% to polyethylene. In contrasts, 3.20% of the total plastic residues are classified as non-biohazardous plastic residues, which commonly end up in landfill; these residues correspond to 55.69% (0.66 g) of polyethylene, 44.30% (0.05 g) of polypropylene, and 0.01% of polyester.
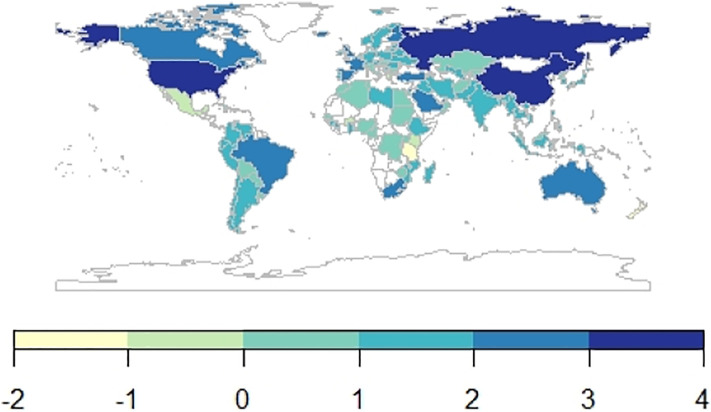
According to data indicated in Table 1 (incineration or landfill) and data from Table S1 (sum of the tests performed in each country), we calculated that at the global level more than 14,900 tons of COVID-19 test plastic residues have been incinerated, whereas only 494 tons of the plastic waste have ended up in landfills. Most countries have more than 10 tons of plastic waste that is incinerated (see Fig. 2 and Table S2). It was estimated that the 99.2% of the global COVID-19 test plastic residues incinerated are composed of polypropylene. The estimated percentage was calculated taking data from Tables 1 and S1.
Fig. 2.
World map of incantation plastic residues (Log-tonnes) derived from RT-PCR tests for COVID-19 (our design with data from Table S2).
Non-biohazardous plastic residues usually go to landfills, but once there they might be exposed to wild animals, such as birds that could eat plastic fragments. With adequate control systems, these plastics should not cause negative impacts on the environment and health, even beyond the years it takes to degrade them. Non-biohazardous plastic residues usually go to landfills, but once there they might be exposed to wild species, such as birds, which could eat plastic fragments.
Bio-hazardous plastics can produce extremely toxic chemical pollutants when burned (Mandal, 2005). In the 1980s, the incineration of plastic waste itself generated gases that were dangerous to human health, especially when different types of hospital waste were burned (Allen et al., 1986). Incineration process techniques to control emissions of toxic gases into the atmosphere from the burning of plastics and other waste have been modernized (Tait et al., 2020). These advanced technologies for gas control generated by incineration processes are currently used in developed countries such as USA and in the European Union, thus the emissions of toxic chemical compounds are significantly reduced. On the other hand, less developed countries are still using old incineration technologies and thus emitting toxic chemicals to the air (Tait et al., 2020). In any case, any incineration of plastic chemicals when burned emits some chemicals to a lesser or greater extent (Tait et al., 2020; Walker and Cooper, 1992).
Toxic gas emissions generated by the incineration process for plastic residues with COVID-19 tests are likely to be lower than those generated by other emissions sources. It is difficult to measure the gas emissions generated by the incineration process for COVID-19 plastic residues, since their burning is usually done along with other associated wastes. Furthermore, these emissions can vary among gas control techniques implemented in various geographical location around the world. During this pandemic, it is troublesome to assess burned COVID-19 waste emissions while numerous locations are still in lockdown, and with increased restrictions to areas that are likely to have higher volumes of contagious waste.
However, many of these chemicals emitted such as dioxins, PAHs and other persistent organic compounds are chemicals that have no biological threshold. Their mere presence can cause biological alterations and their emissions should not be underestimated (Newman, 2009). Furthermore, in the atmosphere this fraction of pollutants generated by the incineration of COVID-19 tests (which can be the lowest when modern gas emission controls are used) is mixed with other air pollutants from different sources, increasing the levels of atmospheric contaminants and producing a synergistic effect that may result in severe biological effects. These chemicals emitted by the incineration of plastics can enter living organisms leading to serious environmental and health effects (Li et al., 2019). Health effects may include disruption of normal hormone signaling pathways, reproductive and developmental defects, immunotoxicity, liver damage, wasting syndrome, and cancer (Kogevinas, 2001; Mandal, 2005; Yoshida et al., 2000). Furthermore, pollutants such as dioxins last a long time because of their chemical stability and their ability to be absorbed by fat tissue (WHO, 2010).
Air pollution has been described as an influential factor in the increase of cases of COVID-19. Particulate matter (PM2.5 and PM10) obstructs the respiratory tract, and the chemicals that make up these particles (such as dioxins and PAHs) have a role in promoting viral diseases by sharing the same mechanisms of action in the immune system. These can affect COVID-19 as well as other viral respiratory diseases (Espejo et al., 2020). The burning of biohazardous materials derived from COVID-19 tests can influence the susceptibility of diseases.
4. Discussion
The lockdown in many cities caused the collapse of the oil price thus lowering the costs of oil products such as plastics. As a result, they are cheaper to manufacture than to recycle (Adyel, 2020). Plastic waste has increased during the pandemic, especially when one looks at hospital and household residues (Espejo et al., 2020). The increase in plastic waste has attracted considerable concern from scientists and policy makers (Klemeš et al., 2020; Silva et al., 2020). Scientific articles that highlight the problem of environmental impact that could be generated by the increased use of plastics in various sectors in the pandemic (Espejo et al., 2020; Silva et al., 2020).
In the first days of the coronavirus pandemic in Wuhan (China), more than 200 tons of medical residues from hospitals were reported daily, i.e. four times the usual amount (Saadat et al., 2020). On March 21st 2020, China's national medical waste treatment daily capacity increased from 48,092.8 tons to 6066.8 tons. In Wuhan, it varied from 50 tons before the pandemic to 265.6 tons (Chen and Guo, 2020). The average value of medical waste in Dhaka, Bangladesh added up to 206 tons per day during the pandemic (Rahman et al., 2020). Medical waste found in Indonesia (Jakarta) reached about 12,740 tons, approximately 60 days after people in the area were first infected with SARS-CoV-2 (Sangkham, 2020). The North Delhi Municipal Corporation (NDMC) also observed an additional 11.4 tons of hazardous waste generated by households (Abhimanyu, 2020). The Apollo Hospital in Ahmedabad reported a fatality rate that increased 1.5 times compared to the normal daily rate. (Yahoo, 2020). The Catalan Agency for Waste Management of Spain reported 350% increase of medical waste, implying an increase of 925 tons per month over the usual records (ACR, 2020). During the eight-week lockdown in Singapore, packaged takeaway plastics added an additional 1400 tons of plastic waste (Bengali, 2020).
Although the aim of this study was to evaluate the plastics generated by the COVID-19 confirmatory test (Prata et al., 2020b), one should bear in mind that PPE have also increased, although in the latter is more complicated to evaluate their contribution to the increase in plastic waste, since many of these products, such as masks, are made from a mixture of vegetable and synthetic fibers (Fadare and Okoffo, 2020). It is estimated that over 129 billion masks and 65 billion gloves have been used worldwide each month (Prata et al., 2020b). 116 million single-use masks were marketed on a single day in February in China, about 12 times the usual amount (Bermingham and Tan, 2020). Incorrect disposal of only 1% of the masks exceeds 10 million items, weighing 30,000 to 40,000 kg (Adyel, 2020). In the United States is reported that the PPEs has multiplied growth (Justine, 2020) and medical waste has grown by up to 370% and the demand for packaging plastics by up to 40% (Silva et al., 2021).
It is difficult to estimate the medical plastic residues generated by other diagnostic techniques (e.g., antigen or antibody), since there is no official data on the number of tests performed, whether positive or negative. In addition, there are many other medical supplies linked to COVID-19 diagnostic centers that also use disposable plastics, such as gloves, biosafety gowns, sleeves, masks, shoe covers, biohazard bag caps, among others. Hospital plastic residues from medical examinations and treatments could increases the mass of plastic residues. The current amount of medical plastic residue and its impact is still difficult to estimate, but we project that it will be worrisome if the coronavirus pandemic persists for months or even years. Although PPE are usually made of plastic and weigh more than the test itself, their use is not standardized and depends on socio-cultural variables of each country, which makes it difficult to estimate the plastic waste generated globally. Disposable plastics generated with COVID-19 tests are easily estimated because the numbers of tests performed periodically by each country must be reported, and also the technique of the confirmatory test by RT-PCR is largely standardized.
In the present study it was estimated that until August 2020 around 15,000 tons of plastic waste have been generated worldwide by COVID-19 test (total number of tests carried out up to August 2020). It is difficult to make a projection of how much plastic waste will be generated by RT-PCR diagnostic tests carried out at the end of the pandemic, because these do not follow a known pattern and depend largely on the political decisions of the Ministries of Health of each country. Countries have different relationships between test performed and the confirmed case of COVID-19 (see Table S1). While some countries continue to increase the number of tests performed daily despite a decreasing number of confirmed cases, other countries have acted otherwise (Roser et al., 2020). The plastic residues generated by the COVID-19 confirmatory tests correspond to only a part of the hospital plastic residues generated in a pandemic. In many countries the management of medical waste is regulated, however its management is not exempt from negative environmental impacts.
The generation of plastic residues is nonetheless inevitable because most diagnostic tests are essential for an early detection of SARS-CoV-2, and to prevent spreading the virus. Real-time PCR and RDT tests are routinely used for detecting a large number of other human and veterinary diseases. It is time to recognize that these diagnostic tests must be environmentally friendly, and there are some short- and long-term actions that should be implemented to reduce the negative impacts of plastic residues from COVID-19 tests.
To reduce the negative impacts generated by non-biohazard plastic waste in the short-term, some practical measures can be taken to reduce the amount of packaging containing reagents to be used in PCR assays, before they end up in a landfill. Considering the huge number of samples analyzed, this may be effectively done by acquiring all reagents in larger containers. In addition, nucleotide extraction and PCR reading (both procedures that are time consuming and labor intensive) may be automatized, which can help to reduce plastic waste.
Regarding bio-hazardous plastic waste, the incineration process remains the most cost-effective technique to kill pathogens. Thus, reducing the negative impacts generated by combustion necessarily must include better gas emission control capable of capturing 99.9% of chemical pollutants. High efficiency incineration used in cement plants, for instance, is capable of significantly reducing dioxin emissions (Richards and Agranovski, 2017), constituting a good option for reducing toxic emissions generated by burning plastics. Nevertheless, it is necessary to consider that this option may require long-distance transport of bio-hazardous materials in most countries, as cement plants are located on suburban areas of the cities, increasing the potential risk of spreading pathogens. Those countries that have waste-to-energy incinerators dedicated to plastics should prioritize this type of incineration for hospital plastic residues.
Long-term actions to reduce the environmental impacts of medical waste used with COVID-19 testing, must include the manufacture of biodegradable medical inputs free major compounds in smoke from burning plastics. Therefore, their decomposition would be faster in the case of inputs ended up in landfills, where they would not emit persistent toxic chemicals if they are incinerated. Bioplastics are the most promising possible alternative materials to solve plastic contamination (Shen et al., 2020). One such bioplastic initiative suggests the use of polylactic acid (PLA), starch, and protein for making biodegradable polymers (Scheer, 2007). A U.S. Patent indicates the possibility of using high-quality biodegradable resins that have the ability to be sterilized just before medical supplies are manufactured (Kulshrestha et al., 2012). Bioplastics still have some difficulties because some bacteria only have the ability to degrade specific polymers and not all types of bioplastics, since degradation depends largely on the morphology and physical characteristics of the polymers. Furthermore, in many cases this biological degradation must be supported by UV degradation or hydrolysis processes. Therefore, composting centers must be built and their use disseminated throughout the world (Luyt and Malik, 2019).
The manufacture of plastic-alterative medical products is more complicated than the substitution of plastic in other economic sectors. Alternative materials used with diagnostic tests for virus infection should be easily sterilized (resistant to high temperatures), not interfere with the analysis, and must be incinerated without environmental risk. They should also be produced at low cost, as they are needed in massive quantities and are vital in medicine. Possible alternatives in financing for these biomaterials with social and health impacts should be explored. Reductions in taxes on these products and even partial or total subsidies should be considered to more efficiently combat the pandemic and the adverse environmental effects. Incentives in R&D for the specific development of low or no toxicity compounds that support the diagnosis and fight against the current and possible future pandemics must go hand in hand.
It is important to analyze the negative environmental impacts of this pandemic caused by medical plastic residues. Furthermore, it is relevant to highlight the urgency of manufacturing sustainable diagnostic tests and PPEs, thus making medicine environmentally friendly. Poor control measures during the incineration process in less developed countries, of these plastic residues can emit toxic pollutants into the atmosphere, which in addition to other pollutant sources can be harmful to human health and the environment. The synergistic mixture of these pollutants can exacerbate disease patterns. Consequently, it is crucial in the short-term to promote better measures to control gas emissions during the incineration process, particularly in countries with poor control measures. On behalf of a sustainable medicine, it is required to drive toward the manufacture of medical tests (and other supplies) able to produce residues that can be incinerated without entailing a risk to human health.
5. Conclusion
The new coronavirus COVID-19 that was officially identified in December 2019, has increased the use of diagnostic tests during the pandemic, which contain medical inputs that are mostly made of plastic. Confirmatory testing for COVID-19 have generated more than 15,000 tons of residues. Most of plastics are made from polypropylene, a type of plastic that is frequently used in different medical applications. Considering that medical plastic residues are classified as biohazardous materials, their fate is mainly done through incineration. There is a risk associated to plastic residues incineration under poor control measures, considering that low-income countries are still using old incineration technologies and thus emitting toxic chemicals to the air, resulting harmful to human health and the environment. The sum of these pollutants can exacerbate disease patterns. In the short-term, it is crucial to enforce better measures to reduce gas emissions during the incineration process, especially in those countries where methods of handling, treatment, and disposal of waste are poor. In the interest of a sustainable medicine, it is necessary to promote medical test manufacturing capable of producing residues that can be incinerated without entailing a risk to human health.
CRediT authorship contribution statement
José E. Celis: Writing – original draft. Winfred Espejo: Conceptualization, Investigation, Resources, Writing – original draft. Esteban Paredes-Osses: Investigation, Resources. Sonia A. Contreras: Investigation, Resources. Gustavo Chiang: Writing – review & editing. Paulina Bahamonde: Investigation, Resources, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
W. Espejo is supported by the FONDECYT Postdoctorado 3200302 of the Agencia Nacional de Investigación y Desarrollo de Chile (ANID). P. Bahamonde also thanks the projects FONDECYT Initiation 11180914 and is supported by Núcleo Milenio INVASAL funded by Chile's Government Program. The authors thank Fabiola Moenne for her helpful support. Thank you also to Kayleigh Karinen for reviewing the English grammar and syntax of this paper.
Editor: Damia Barcelo
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2020.144167.
Appendix A. Supplementary data
Supplementary tables
References
- Abhimanyu C. Fighting from the bottom, India's sanitation workers are also frontline workers battling Covid. 2020. https://indianexpress.com/article/india/india-sanitation-workers-waste-pickers-coronavirus-pandemic-6414446/ Retrieved November 21, 2020.
- Adyel T.M. Accumulation of plastic waste during COVID-19. Science. 2020;369(6509):1314–1315. doi: 10.1126/science.abd9925. [DOI] [PubMed] [Google Scholar]
- Allen R., Brenniman G., Darling C. Air pollution emissions from the incineration of hospital waste. Journal of the Air Pollution Control Association. 1986;36(7):829–831. [Google Scholar]
- Andersen M.H.G., Saber A.T., Clausen P.A. Association between polycyclic aromatic hydrocarbon exposure and peripheral blood mononuclear cell DNA damage in human volunteers during fire extinction exercises. Mutagenesis. 2018;33(1):105–115. doi: 10.1093/mutage/gex021. [DOI] [PubMed] [Google Scholar]
- Association of Cities and Regions ACR (2020). Municipal waste management and COVID-19. Retrieved November 21, 2020 from https://www.acrplus.org/en/municipal-waste-management-covid-19#spain
- Beeching N.J., Fletcher T.E., Beadsworth M.B. British Medical Journal Publishing Group; 2020. Covid-19: Testing Times. [DOI] [PubMed] [Google Scholar]
- Bengali S. 2020. The COVID-19 Pandemic Is Unleashing a Tidal Wave of Plastic Waste. The Los Angeles Times. [Google Scholar]
- Bermingham F., Tan S. Vol. 12. South China Morning Post; 2020. Coronavirus: China’s Mask-making Juggernaut Cranks Into Gear, Sparking Fears of Over-reliance on World’s Workshop. [Google Scholar]
- Campanale C., Massarelli C., Savino I., Locaputo V., Uricchio V.F. A detailed review study on potential effects of microplastics and additives of concern on human health. Int. J. Environ. Res. Public Health. 2020;17(4):1212. doi: 10.3390/ijerph17041212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Guo C. Handbook of emergency disposal and management of medical waste in China. Royal Collins Publishing Company. 2020;2020 [Google Scholar]
- Cox K.D., Covernton G.A., Davies H.L., Dower J.F., Juanes F., Dudas S.E. Human consumption of microplastics. Environmental Science & Technology. 2019;53(12):7068–7074. doi: 10.1021/acs.est.9b01517. [DOI] [PubMed] [Google Scholar]
- Espejo W, Celis JE, Chiang G, Bahamonde P (2020) Environment and Covid-19: pollutants, impacts, dissemination, management and recommendations for facing future epidemic threats. Science of the Total Environment:141314. [DOI] [PMC free article] [PubMed]
- Fadare O.O., Okoffo E.D. Covid-19 face masks: a potential source of microplastic fibers in the environment. Sci. Total Environ. 2020;737:140279. doi: 10.1016/j.scitotenv.2020.140279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghodrat M., Rashidi M., Samali B. Energy Technology 2017. Springer; 2017. Life cycle assessments of incineration treatment for sharp medical waste; pp. 131–143. [Google Scholar]
- Hermabessiere L., Dehaut A., Paul-Pont I. Occurrence and effects of plastic additives on marine environments and organisms: a review. Chemosphere. 2017;182:781–793. doi: 10.1016/j.chemosphere.2017.05.096. [DOI] [PubMed] [Google Scholar]
- Hylland K. Polycyclic aromatic hydrocarbon (PAH) ecotoxicology in marine ecosystems. J. Toxic. Environ. Health A. 2006;69(1–2):109–123. doi: 10.1080/15287390500259327. [DOI] [PubMed] [Google Scholar]
- Jin Y., Yang H., Ji W. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12(4):372. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justine C. (2020). The COVID-19 pandemic is generating tons of medical waste. Retrieved November 21, 2020 from https://www.theverge.com/2020/3/26/21194647/the-covid-19-pandemic-is-generating-tons-of-medical-waste.
- Klemeš J.J., Van Fan Y., Tan R.R., Jiang P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sust. Energ. Rev. 2020;127:109883. doi: 10.1016/j.rser.2020.109883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogevinas M. Human health effects of dioxins: cancer, reproductive and endocrine system effects. Apmis. 2001;109(S103):S223–S232. doi: 10.1093/humupd/7.3.331. [DOI] [PubMed] [Google Scholar]
- Kulshrestha A.S., Calistri-Yeh M., Amora L.P.L., Giddes R. 2012. Recycled Resin Compositions and Disposable Medical Devices Made Therefrom. (Google Patents) [Google Scholar]
- Lambert S., Wagner M. Environmental performance of bio-based and biodegradable plastics: the road ahead. Chem. Soc. Rev. 2017;46(22):6855–6871. doi: 10.1039/c7cs00149e. [DOI] [PubMed] [Google Scholar]
- Li W.C., Tse H., Fok L. Plastic waste in the marine environment: a review of sources, occurrence and effects. Sci. Total Environ. 2016;566:333–349. doi: 10.1016/j.scitotenv.2016.05.084. [DOI] [PubMed] [Google Scholar]
- Li H.-Y., Gao P.-P., Ni H.-G. Emission characteristics of parent and halogenated PAHs in simulated municipal solid waste incineration. Sci. Total Environ. 2019;665:11–17. doi: 10.1016/j.scitotenv.2019.02.002. [DOI] [PubMed] [Google Scholar]
- Luyt A.S., Malik S.S. Plastics to Energy. Elsevier; 2019. Can biodegradable plastics solve plastic solid waste accumulation? pp. 403–423. [Google Scholar]
- Lv M., Luan X., Liao C. Human impacts on polycyclic aromatic hydrocarbon distribution in Chinese intertidal zones. Nature Sustainability. 2020:1–7. [Google Scholar]
- Mandal P.K. Dioxin: a review of its environmental effects and its aryl hydrocarbon receptor biology. J. Comp. Physiol. B. 2005;175(4):221–230. doi: 10.1007/s00360-005-0483-3. [DOI] [PubMed] [Google Scholar]
- McKeen LW (2014) Plastics used in medical devices. Handbook of Polymer Applications in Medicine and Medical Devices. Elsevier, p 21-53.
- Mocarelli P., Brambilla P., Gerthoux P.M., Patterson D.G., Jr., Needham L.L. Change in sex ratio with exposure to dioxin. Lancet. 1996;348(9024):409. doi: 10.1016/s0140-6736(05)65030-1. [DOI] [PubMed] [Google Scholar]
- Newman M.C. CRC Press; 2009. Fundamentals of Ecotoxicology. [Google Scholar]
- Prata J.C., da Costa J.P., Lopes I., Duarte A.C., Rocha-Santos T. Environmental exposure to microplastics: an overview on possible human health effects. Sci. Total Environ. 2020;702:134455. doi: 10.1016/j.scitotenv.2019.134455. [DOI] [PubMed] [Google Scholar]
- Prata J.C., Patrício Silva A.L., Walker T.R., Duarte A.C., Rocha Santos T. COVID-19 pandemic repercussions on the use and management of plastics. Environmental Science & Technology. 2020 doi: 10.1021/acs.est.0c02178. [DOI] [PubMed] [Google Scholar]
- Rahman M.M., Bodrud-Doza M., Griffiths M.D., Mamun M.A. 2020. Biomedical waste amid COVID-19: perspectives from Bangladesh. The Lancet Global Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards G., Agranovski I.E. Dioxin-like pcb emissions from cement kilns during the use of alternative fuels. J. Hazard. Mater. 2017;323:698–709. doi: 10.1016/j.jhazmat.2016.10.040. [DOI] [PubMed] [Google Scholar]
- Roser M., Ritchie H., Ortiz-Ospina E., Hasell J. Published online at OurWorldInData. org; 2020. Coronavirus Pandemic (COVID-19) [Google Scholar]
- Rujnić-Sokele M., Pilipović A. Challenges and opportunities of biodegradable plastics: a mini review. Waste Manag. Res. 2017;35(2):132–140. doi: 10.1177/0734242X16683272. [DOI] [PubMed] [Google Scholar]
- Saadat S, Rawtani D, Hussain CM (2020) Environmental perspective of COVID-19. Science of the Total Environment:138870. [DOI] [PMC free article] [PubMed]
- Sangkham S (2020) Face mask and medical waste disposal during the novel COVID-19 pandemic in Asia. Case Studies in Chemical and Environmental Engineering:100052. [DOI] [PMC free article] [PubMed]
- Scheer F. 2007. Bio Based Biodegradable Polymer Compositions and Use of Same. (Google Patents) [Google Scholar]
- Scohy A, Anantharajah A, Bodéus M, Kabamba-Mukadi B, Verroken A, Rodriguez-Villalobos H (2020) Low performance of rapid antigen detection test as frontline testing for COVID-19 diagnosis. Journal of Clinical Virology:104455. [DOI] [PMC free article] [PubMed]
- Shen M, Song B, Zeng G, et al. (2020) Are biodegradable plastics a promising solution to solve the global plastic pollution? Environmental Pollution:114469. [DOI] [PubMed]
- Silva A.L.P., Prata J.C., Walker T.R. Rethinking and optimising plastic waste management under COVID-19 pandemic: policy solutions based on redesign and reduction of single-use plastics and personal protective equipment. Sci. Total Environ. 2020;742:140565. doi: 10.1016/j.scitotenv.2020.140565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva A.L., Prata J.C., Walker T.R., Duarte A.C., Ouyang W., Barcelò D., Rocha-Santos T. Increased plastic pollution due to COVID-19 pandemic: challenges and recommendations. Chem. Eng. J. 2021;405:126683. doi: 10.1016/j.cej.2020.126683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O’Neill N. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tait P.W., Brew J., Che A. The health impacts of waste incineration: a systematic review. Aust. N. Z. J. Public Health. 2020;44(1):40–48. doi: 10.1111/1753-6405.12939. [DOI] [PubMed] [Google Scholar]
- Tang Y.-W., Schmitz J.E., Persing D.H., Stratton C.W. Laboratory diagnosis of COVID-19: current issues and challenges. J. Clin. Microbiol. 2020;58(6) doi: 10.1128/JCM.00512-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vegter A.C., Barletta M., Beck C. Global research priorities to mitigate plastic pollution impacts on marine wildlife. Endanger. Species Res. 2014;25(3):225–247. [Google Scholar]
- Walker B.L., Cooper C.D. Air pollution emission factors for medical waste incinerators. J. Air Waste Manage. Assoc. 1992;42(6):784–791. [Google Scholar]
- WHO (2010) Exposure to dioxins and dioxin-like substances: a major public health concern. Preventing Disease Through Healthy Environments:6.
- Wilcox C., Van Sebille E., Hardesty B.D. Threat of plastic pollution to seabirds is global, pervasive, and increasing. Proc. Natl. Acad. Sci. 2015;112(38):11899–11904. doi: 10.1073/pnas.1502108112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisniewski A., Zimmerman M., Crews T., Jr., Haulbrook A., Fitzgerald D.C., Sistino J.J. Reducing the impact of perfusion medical waste on the environment. J Extra Corpor Technol. 2020;52(2):135–141. doi: 10.1182/ject-1900023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worm B., Lotze H.K., Jubinville I., Wilcox C., Jambeck J. Plastic as a persistent marine pollutant. Annu. Rev. Environ. Resour. 2017;42 [Google Scholar]
- Yahoo (2020). As coronavirus cases surge, Ahmedabad hospitals shell Out Rs 45/kg for disposal of Covid-19 Bio-waste. Retrieved November 21, 2020 from https://in.news.yahoo.com/coronavirus-cases-surge-ahmedabad-hospitals-061800880.html.
- Yoshida K., Ikeda S., Nakanishi J. Assessment of human health risk of dioxins in Japan. Chemosphere. 2000;40(2):177–185. doi: 10.1016/s0045-6535(99)00253-2. [DOI] [PubMed] [Google Scholar]
- Zambrano-Monserrate MA, Ruano MA, Sanchez-Alcalde L (2020) Indirect effects of COVID-19 on the environment. Science of the Total Environment:138813. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables