Abstract
Background
We evaluated a community‐engaged stroke preparedness intervention that aimed to increase early hospital arrival and emergency medical services (EMS) utilization among patients with stroke in the South Side of Chicago, Illinois.
Methods and Results
We compared change in early hospital arrival (<3 hours from symptom onset) and EMS utilization before and after our intervention among patients with confirmed ischemic stroke at an intervention hospital on the South Side of Chicago with concurrent data from 6 hospitals in nonintervention communities on the North Side of Chicago and 17 hospitals in St Louis, Missouri. We assessed EMS utilization for suspected stroke secondarily, using geospatial information systems analysis of Chicago ambulance transports before and after our intervention. Among 21 497 patients with confirmed ischemic stroke across all sites, early arrival rates at the intervention hospital increased by 0.5% per month (95% CI, −0.2% to 1.2%) after intervention compared with the preintervention period but were not different from North Side Chicago hospitals (difference of −0.3% per month [95% CI, −0.12% to 0.06%]) or St Louis hospitals (difference of 0.7% per month [95% CI, −0.1% to 1.4%]). EMS utilization at the intervention hospital decreased by 0.8% per month (95% CI, −1.7% to 0.2%) but was not different from North Side Chicago hospitals (difference of 0.004% per month [95% CI, −1.1% to 1.1%]) or St Louis hospitals (difference of −0.7% per month [95% CI, −1.7% to 0.3%]). EMS utilization for suspected stroke increased in the areas surrounding the intervention hospital (odds ratio [OR], 1.4; 95% CI, 1.2–1.6) and in the South Side (OR, 1.2; 95% CI, 1.1–1.3), but not in the North Side (OR, 1.0; 95% CI, 0.9–1.1).
Conclusions
Following a community stroke preparedness intervention, early hospital arrival and EMS utilization for confirmed ischemic stroke did not increase. However, ambulance transports for suspected stroke increased in the intervention community compared with other regions.
Registration
URL: https://www.clinicaltrials.gov; Unique identifier: NCT02301299.
Keywords: acute stroke, education campaigns, emergency medical services
Subject Categories: Ischemic Stroke, Health Services, Behavioral/Psychosocial Treatment
Nonstandard Abbreviations and Acronyms
- CEERIAS
Community Engagement for Early Recognition and Immediate Action in Stroke
- EMS
emergency medical services
- FAST
face, arm, speech, time
- GWTG
Get With The Guidelines
Clinical Perspective
What Is New?
Following a community‐engaged stroke preparedness intervention in the South Side of Chicago, there was no increase in early hospital arrival or emergency medical services utilization for patients with confirmed ischemic stroke.
However, emergency medical services utilization for suspected stroke increased in a graded manner with the greatest effect size in areas of the greatest intervention penetration.
What Are the Clinical Implications?
Our approach and findings should inform future study designs of community‐engaged stroke preparedness interventions.
Early hospital arrival increases the likelihood of receiving proven acute stroke treatments. 1 , 2 However, delayed arrival of a patient to the hospital remains the primary reason for low rates of tissue plasminogen activator treatment. 3 An important predictor of early hospital arrival is the use of emergency medical services (EMS). 4 In the United States, less than two‐thirds of patients with stroke are transported by EMS. 5
Increasing early arrival and EMS utilization in the community remain important goals of stroke education efforts. These efforts have focused largely on improving public knowledge, using slogans such as FAST (face, arm, speech, time). 6 , 7 , 8 , 9 , 10 However, mass media public education campaigns have not resulted in meaningful changes in early arrival or EMS utilization after stroke. 11 , 12 , 13 Perceptions, attitudes, cultural and social norms, and self‐efficacy, in addition to knowledge, may determine behavioral intent and precede behaviors or actions. As a result, community‐engaged and community‐participatory approaches 14 have been recommended to address these decisional factors.
We applied a community‐engaged approach to develop a novel face‐to‐face stroke preparedness intervention in the South Side of Chicago, where stroke incidence and mortality rates were high and EMS utilization was low. We hypothesized that a community‐engaged and ‐delivered stroke preparedness intervention would increase early arrival and EMS utilization after stroke symptom onset.
METHODS
Study Overview
The CEERIAS (Community Engagement for Early Recognition and Immediate Action in Stroke) study was funded by the Patient‐Centered Outcomes Research Institute (ClinicalTrials.gov identifier NCT02301299). The ethics boards at all participating hospitals granted approval. The study principal investigators had full access to all data and take responsibility for its integrity and for the data analysis. The data that support the findings of this study are available from the corresponding author on reasonable request.
Study Setting and Population
The city of Chicago has a population of 2.7 million and an area of 247 square miles. A single municipal fire‐based EMS agency, the Chicago Fire Department, responds to all 9‐1‐1 calls. EMS system protocols require paramedics to screen patients with suspected stroke using the Cincinnati Prehospital Stroke Scale and to transport to the closest stroke center hospital. The South Side of Chicago has a population of nearly 800 000 residents and is predominantly (>93%) Black. During the study period, there were 16 stroke centers in Chicago but only 2 primary stroke centers and 1 comprehensive stroke center in the South Side.
We targeted an urban underserved setting surrounding the 2 primary stroke centers on the South Side of Chicago for the intervention, based on baseline data on stroke incidence and EMS use, field observations, and community town halls facilitated by the research team. We selected concurrent comparison hospitals in the North Side of Chicago (n=6) and St Louis, Missouri (n=17), to provide contemporaneous reference data to data from the intervention hospitals and to account for potential unintended diffusion of the intervention. We selected St Louis because it is another Midwestern city with a diverse urban population and outside the Chicago media market. We are unaware of any local, regional, and national stroke awareness campaigns that were active in the North Side of Chicago or St Louis during the study period.
Changes to Study Protocol
We excluded data from one of the South Side intervention hospitals based on data‐quality assessments in 2015 that suggested data sampling and incomplete and inaccurate reporting of EMS mode of arrival into the Get With The Guidelines–Stroke (GWTG‐Stroke; Quintiles Real World and Late Phase Research) database. A replacement hospital was not available because these 2 hospitals are the only primary stroke centers in the South Side of Chicago. Because suspected patients with stroke who activate EMS are transported to primary stroke centers per regional policy, non–stroke center hospitals would not have been appropriate replacement hospitals.
Stroke Preparedness Intervention
We integrated 2 pilot stroke awareness programs using focus groups and key informant interviews, as previously published, 15 to create a community‐engaged stroke preparedness intervention. A central concept of the intervention was the “Pact to Act FAST,” a pledge that community members signed attesting that they would call 9‐1‐1 if they witnessed someone having a stroke. The other key standardized components of the intervention were as follows: (1) a rigorous training program for stroke promoters recruited from the community that included didactic material, a hospital tour, workshops, and role‐playing sessions; (2) the use of educational materials (eg, cards, magnets) provided by the CEERIAS team; (3) the use of strategies and activities gleaned from the training sessions to overcome specific barriers encountered (eg, mistrust in hospitals); (4) the use of the CEERIAS website to log activities and pacts online and to discuss successes and failures with other stroke promoters; and (5) regular contact between the study team and stroke promoters for 6 months following training. We performed no specific additional education for paramedics or hospital staff beyond the routine annual training they receive regarding prehospital stroke care.
Training and Implementation
We implemented the intervention in December 2015 and monitored its reach, penetration, and adoption until November 2016. First, we identified and recruited laypeople and community members from the South Side to serve as stroke education promoters (heretofore referrred to as "stroke promoters") and to undergo training. Each 4‐hour structured training session included lectures, didactic material on stroke statistics relevant to South Side communities, hospital‐based tours of the “stroke patient journey,” case examples, multimedia aids, role‐playing activities, and storytelling of shared experiences and feelings to enhance the learning process. We then tasked each trained stroke promoter with disseminating the educational materials to his or her constituents (eg, parishioners, school‐aged children, and customers) and presenting the program at least twice a month for 6 months following the training. We required stroke promoters to obtain pacts in person, with zip‐code verification of the individual making the pledge, and provided training and tools for tracking the pacts and event activities on the study website. We evaluated other aspects of the intervention using the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE‐AIM) framework. 16 See Data S1 and Figures S1 through S3 for further details of intervention development and implementation.
Primary Outcomes
The 2 primary outcomes were (1) monthly early hospital arrival rate and (2) monthly EMS utilization rate among confirmed ischemic patients with stroke. We defined early hospital arrival as a confirmed ischemic stroke patient arriving at a hospital within 3 hours of symptom onset (or last known well if symptom onset time was unknown), and EMS utilization as a confirmed ischemic stroke patient arriving at the hospital emergency department by Chicago Fire Department ambulance rather than by private transport, taxi, or other form of transportation.
Secondary Outcome
The secondary outcome was the frequency of ambulance transports for paramedic‐suspected strokes. We defined a suspected stroke as any EMS patient encounter with paramedic documentation in the prehospital electronic patient care record of “suspected stroke” or “rule‐out stroke” or transport to a primary stroke center bypassing non–stroke centers.
Data Collection and Variables
We collected hospital data using the GWTG‐Stroke registry, including demographic, clinical, and hospital outcome data. 3 All stroke center hospitals in Chicago and St Louis used this registry for data collection. With a waiver of informed consent under the common rule for data collected for quality improvement, we accessed and downloaded anonymized GWTG‐Stroke records from all participating hospitals between January 1, 2013, and December 31, 2017, for review and analysis.
We included records with ischemic stroke type and arrival mode by EMS, private transport, taxi, other means of transportation, or walk‐in. Records with elective or direct admission, unknown or interhospital transfer arrival mode, and stroke occurrence after admission were excluded. Hemorrhagic stroke was not included in the analyses because (1) the primary stroke center hospitals in the intervention community did not routinely collect data on this subset of patients with stroke; (2) these patients are often transferred emergently from a primary stroke center to comprehensive stroke centers; and (3) unlike ischemic stroke, no proven, specific, time‐dependent intervention exists for hemorrhagic stroke. Extracted data included demographics (age, sex, race, and ethnicity), mode of hospital arrival, and times of symptom onset and hospital arrival. Race and ethnicity were categorized into 4 groups for analysis: non‐Hispanic White, non‐Hispanic Black, Hispanic, and Other, which included Asian, American Indian/Alaska Native, Native Hawaiian/Pacific Islander, UTD (unable to determine), and other mixed races.
We created an early arrival variable by subtracting the symptom onset time from the hospital arrival time. When symptom onset time was unknown or missing, we used the last known well time as symptom onset time, consistent with the convention in stroke care and research. When both symptom onset time and last known well time were unknown or missing, we treated that admission as a late arrival (>3 hours from onset).
For the secondary outcome, we obtained deidentified EMS records from the Chicago Fire Department’s electronic medical‐record system (SafetyPAD; ESO Solutions). EMS records included the paramedics’ clinical impression, the destination hospital and reason, and the location of patient contact.
Statistical Analysis
We conducted all primary outcome analyses using SAS 9.4 (SAS Institute). First, we performed frequency analysis for the number of admissions by years and months and descriptive analysis of patient’s characteristics, such as age, sex, and race and ethnicity. We conducted a seasonally adjusted interrupted time series analysis for the intervention hospital to examine the effects of the intervention on early arrival and EMS utilization rates. 17 We specified an impact model before the analysis, based on our hypothesis that the change in the outcome (eg, rate of early arrival or EMS use) would be both a gradual change in the slope over time with an abrupt change in the level after the intervention. In addition, we assumed that there would be a change in the slope before intervention and that there would be autocorrelation between consecutive observations. The early arrival and EMS utilization variables were aggregated by month (total of 60 months) to create monthly early arrival rates and monthly EMS utilization rates for time series analysis. We excluded the outcome data during the 4‐month period from December 2015 to March 2016 from time series analysis because this was the implementation period over which more than half of pacts were obtained. These resulted in 35 preintervention‐month points and 21 postintervention months.
To correct for autocorrelation, we used a backstep approach that initially fitted a high‐order model with 12 autoregressive lags and then sequentially eliminated autoregressive parameters until all remaining autoregressive parameters had significant t tests. The regression models of the interrupted time series data included the following 4 terms: intercept (ie, monthly EMS utilization rate at the first month [January 2013]), time point in months (0–60 months), level change after intervention (ie, change in a monthly EMS utilization rate immediately after the intervention month), and slope change after intervention (ie, change in a monthly EMS utilization rate over time after the intervention). A maximum likelihood method was used to estimate parameters.
Because interrupted time‐series analysis may not completely account for background temporal trends unrelated to the intervention, we sought to compare the primary outcomes at the South Side Chicago intervention hospitals with those from concurrent nonintervention hospitals in the North Side of Chicago and St Louis. A series of 3 interrupted time series analyses were conducted for 3 different samples: (1) the intervention hospital alone, (2) the intervention hospital and 6 North Side Chicago nonintervention hospitals, and (3) the intervention hospital and 17 St Louis nonintervention hospitals.
We did not match hospitals by demographics or other features or adjust for differences between the groups. Instead, we conducted subgroup analyses by age group (<66 versus ≥66 years), sex (male versus female), and race/ethnicity (Black versus non‐Black) to examine whether the results differed by the subgroups. Because we conducted 10 statistical tests in prespecified subgroup analyses (2 outcomes by 5 subgroups [age <66 years, age ≥66 years, men, women, and Black patients]), we conservatively considered P<0.005 to be significant in subgroup analyses using the Bonferroni method.
Because we aggregated individual patient data on a monthly basis and the model regressed monthly early arrival rates and monthly EMS arrival rates on time in months, the sample unit of the regression model was a time point (month), not patients. Therefore, the sample size was the number of months and not the number of patients per month or the number of hospitals in the analysis. For power calculation, we assumed that the postintervention period would be at least one‐third of the total months of data available from the hospitals, which we achieved with 35 months of preintervention data (January 2013–November 2015) and 21 months of postintervention data (April 2016–December 2017). The effect size was defined as the sum of the expected slope change and the expected level change over the standard deviation in monthly early hospital arrival rates or monthly EMS use rates. Assuming an autocorrelation level of 0.3, an effect size of 0.5 (which would translate to a 4% level change and a 1% change/month with a 10% SD in early arrival or EMS use) would be detectable at 90% power at a significance level of 0.05. Such an effect size would mean an absolute increase in either primary outcome by >10% over 1 year of postintervention observation, which would be considered meaningful. 18
For the secondary outcome, we used ArcGIS and ArcGIS Pro (ESRI) for geographic information system analysis. We geolocated ambulance transport locations using addresses provided in the records for a period before the CEERIAS intervention and compared these with an equal period after the intervention. HotSpot Analysis was used to analyze all ambulance transports, regardless of incident type or paramedic impression, applying a false discovery rate correction to account for multiple comparisons. Using Getis‐Ord Gi* analysis, we identified hot spots for paramedic‐suspected stroke transports. Statistical hot and cold spots were defined as areas where there is <1% likelihood that case clusters occur by chance alone. We used χ2 tests to compare the proportion of EMS utilization for suspected stroke versus overall EMS utilization in the pre‐ and postintervention periods in specific geographic locations in Chicago: (1) a 3.5‐mile radius around the intervention hospitals, (2) the South Side (defined as south of Interstate 290), and (3) the North Side (defined as north of Interstate 290). A standardized 3.5‐mile radius was chosen to include the historic catchment areas for the hospitals and visual inspection of the maps.
RESULTS
We identified 297 potential stroke promoters; 55 (18.5%) declined to participate or did not return multiple attempts of phone contact. In total, we conducted 21 training sessions for 242 community promoters (81 Black men, 133 Black women, 4 Hispanic men, 5 Hispanic women, 3 non‐Hispanic White men, and 16 non‐Hispanic White women) between October 2015 and May 2016. Of these stroke promoters, 87 (40.0%) were self‐employed, 63 (26.0%) were from faith‐based organizations, 28 (11.6%) were from healthcare organizations, 24 (9.9%) were from schools, and 40 (16.5%) were from other community advocacy groups and local businesses. Stroke promoters distributed >110 000 educational materials including FAST cards and magnets and participated in at least 167 large‐scale community events. A total of 39 795 Pact to Act FAST pledges were registered between December 2015 and November 2016; of those, 80.3% were registered at South Side zip‐codes (Figure 1). The intervention’s penetration in the excluded intervention hospital’s geographic service area was lower than the penetration for the included intervention hospital (an estimated 4.3% penetration of 140 855 households versus 19.4% penetration of 58 427 households using 2010 census data).
Figure 1. Pacts received by Chicago zip‐code.
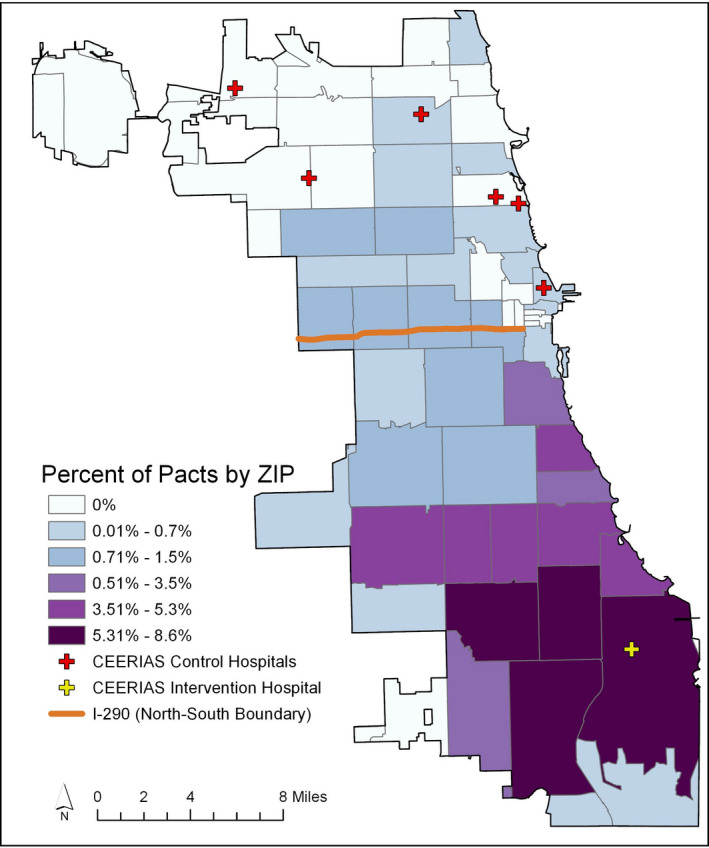
CEERIAS indicates Community Engagement for Early Recognition and Immediate Action in Stroke.
Primary Outcomes
We analyzed 21 497 patients with confirmed ischemic stroke across all sites (Table 1). Compared with the nonintervention hospitals, patients at the intervention hospital were more likely to be women, Black, and slightly younger. Monthly stroke admissions and patient characteristics were stable between pre‐ and postintervention periods, except that the proportions of Black and White patients at North Side hospitals declined from the pre‐ to postintervention period.
Table 1.
Patient Characteristics at the Intervention, North Side, and St Louis Hospitals, n (%)
| Intervention Hospital (n=1) | North Side Hospitals (n=6) | St Louis Hospitals (n=17) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Pre | Post | Total | Pre | Post | Total | Pre | Post | |
| Total | 1322 (100) | 865 (100) | 457 (100) | 3566 (100) | 1894 (100) | 1672 (100) | 16 609 (100) | 8401 (100) | 8208 (100) |
| Aged <66 y | 550 (41.6) | 355 (41.0) | 195 (42.7) | 1415 (39.8) | 742 (39.3) | 673 (40.3) | 5627 (36.7) | 3174 (37.8) | 2453 (35.5) |
| Male | 571 (43.2) | 364 (42.1) | 207 (45.3) | 1868 (52.4) | 997 (52.6) | 871 (52.1) | 7934 (47.8) | 3993 (47.5) | 3941 (48.0) |
| Hispanic | 87 (6.6) | 49 (5.7) | 38 (8.3) | 474 (13.3) | 229 (12.1) | 245 (14.7) | 76 (0.5) | 31 (0.4) | 45 (0.5) |
| Black | 1176 (89.0) | 777 (89.8) | 399 (87.3) | 689 (19.3) | 407 (21.5) | 282 (16.9) | 4420 (26.6) | 2266 (27.0) | 2154 (26.2) |
| White | 43 (3.3) | 28 (3.2) | 15 (3.3) | 1673 (46.9) | 966 (51.0) | 707 (42.3) | 11 767 (70.8) | 5915 (70.4) | 5852 (71.3) |
| Other (including Asian, American Indian/Alaska Native, Native Hawaiian/Pacific Islander, UTD, and other mixed races | 16 (1.2) | 11 (1.3) | 5 (1.1) | 729 (20.4) | 292 (15.4) | 437 (26.2) | 346 (2.1) | 189 (2.2) | 157 (1.9) |
UTD indicates unable to determine.
For early arrival rates and EMS utilization rates for confirmed ischemic stroke (Table 2), we observed no level or slope change in early arrival at the intervention hospital. Slope change did not differ between the intervention hospital and the North Side hospitals or St Louis hospitals for either primary outcome. Subgroup analyses by age group (<66 versus ≥66 years), sex (male versus female), and race and ethnicity (Black versus non‐Black) showed that the slope for early arrival increased after the intervention for patients who were <66 years old (increase of 0.8% per month [95% CI, 0.06%–1.6%]; P=0.036), among men (increase of 1.2% per month [95% CI, 0.1%–2.3%]; P=0.026), and among Black patients (increase of 0.9% per month [95% CI, 0.05%–1.7%]; P=0.037). However, none reached statistical significance using the Bonferroni correction method.
Table 2.
Interrupted Time Series Regression Model for the Primary Outcomes at the Intervention South Side Chicago Hospital and Comparison to North Side Chicago Hospitals and St Louis Hospitals
| Intervention Hospital | Comparison With North Side Chicago Hospitals | Comparison With St Louis Hospitals | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Early arrival (<3 h from symptom onset) | ||||||
| Intercept | 0.287 | 0.227, 0.348 | −0.152 | −0.231, −0.072 | 0.032 | −0.030, 0.094 |
| Time | −0.002 | −0.005, 0.001 | 0.005 | −0.001, 0.009 | −0.003 | −0.006, 0.0001 |
| Level change | −0.001 | −0.106, 0.103 | −0.043 | −0.181, 0.094 | 0.035 | −0.072, 0.142 |
| Slope change | 0.005 | −0.002, 0.012 | −0.003 | −0.012, 0.006 | 0.007 | −0.001, 0.014 |
| EMS arrival | ||||||
| Intercept | 0.587 | 0.513, 0.661 | 0.028 | −0.055, 0.111 | 0.013 | −0.062, 0.088 |
| Time | −0.001 | −0.004, 0.004 | 0.003 | −0.001, 0.007 | −0.0002 | −0.004, 0.004 |
| Level change | 0.056 | −0.100, 0.211 | −0.092 | −0.267, 0.083 | 0.043 | −0.116, 0.202 |
| Slope change | −0.008 | −0.017, 0.002 | <0.001 | −0.011, 0.011 | −0.007 | −0.017, 0.003 |
A level change is an abrupt change right after intervention implementation. A slope change is the change per month over time after intervention implementation. EMS indicates emergency medical services.
Secondary Outcome
We successfully geolocated 418 796 (98%) EMS transports in a 20‐month period before the CEERIAS intervention (April 2014–November 2015) and 430 426 (97%) in a 20‐month period after the CEERIAS intervention (April 2016–November 2017). The distributions of overall EMS utilization were unchanged citywide and in the areas adjacent to the intervention hospitals (Figure 2A). However, the frequency of ambulance transports for suspected strokes changed from a cold spot to a hot spot relative to other Chicago areas in 3 geographic areas near the intervention hospitals (Figure 2B). EMS utilization for suspected stroke increased (Table 3) in the areas surrounding the intervention hospital (odds ratio [OR], 1.4; 95% CI, 1.2–1.6) and in the South Side (OR, 1.2; 95% CI, 1.1–1.3) but not in the North Side (OR, 1.0; 95% CI, 0.9–1.1).
Figure 2. Geographic information system analysis of effect of intervention on secondary outcomes in Chicago before and after intervention; statistical hot and cold spots are defined as areas where there is <1% likelihood that case clusters occur by chance alone.
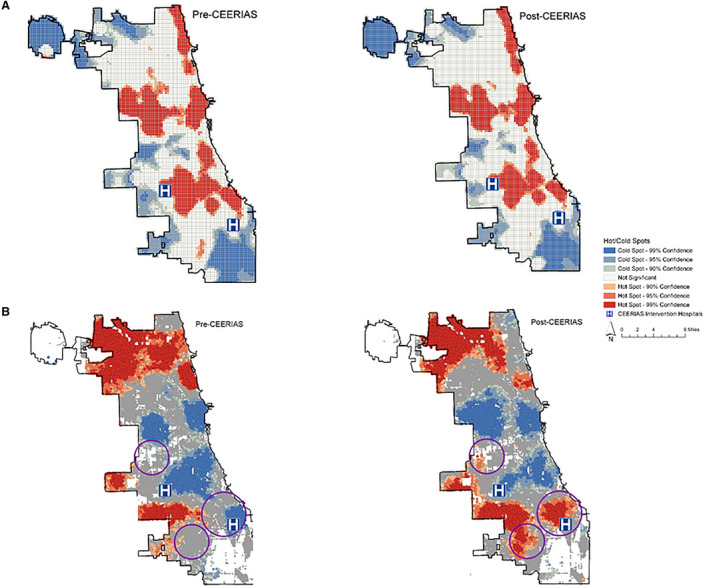
A, Overall EMS utilization; B, EMS utilization for suspected stroke (purple circles indicate geocoded regions where cold spots became hot spots after the intervention). CEERIAS indicates Community Engagement for Early Recognition and Immediate Action in Stroke.
Table 3.
EMS Utilization for Suspected Stroke in Specific Regions of Chicago Before and After Intervention
| Preintervention, Suspected Stroke/Total EMS Calls, n (%) | Postintervention, Suspected Stroke/Total EMS Calls, n (%) | OR (95% CI) | P Value | |
|---|---|---|---|---|
| Area centered around included intervention hospital (3.5‐mile circular radius) |
440/48 150 (0.91) |
603/47 714 (1.26) |
1.4 (1.2–1.6) | <0.001 |
| Area centered around excluded intervention hospital (3.5‐mile circular radius) |
684/69 949 (0.98) |
846/69 547 (1.22) |
1.2 (1.1–1.4) | <0.001 |
| South Side (south of interstate 290) | 2342/260 388 (0.90) | 2897/267 479 (1.08) | 1.2 (1.1–1.3) | <0.001 |
| North Side (north of interstate 290) |
1904/158 408 (1.20) |
1978/162 947 (1.21) | 1.0 (0.9–1.1) | 0.757 |
EMS indicates emergency medical services; and OR, odds ratio.
DISCUSSION
Implementation of a community‐based stroke preparedness intervention in the South Side of Chicago did not increase early arrival or EMS utilization for confirmed ischemic stroke at the hospital level. However, EMS utilization for suspected strokes increased in the areas of greatest intervention penetration and in the South Side overall, suggesting a potential intervention effect. These conflicting findings may be due to an overrepresentation of false‐positive strokes (eg, EMS‐suspected stroke but final hospital diagnosis was not stroke), transient ischemic attacks, or hemorrhagic strokes that were not included in the primary outcome measures.
A recent systematic review of stroke preparedness interventions found that 10 of 13 studies decreased prehospital delay, but only 1 study was a prospective cluster randomized clinical trial. 13 This trial showed a reduction in prehospital delay in Berlin, Germany, among women but not men. 19 Although some observational studies have noted an effect of stroke preparedness interventions on arrival time or tissue plasminogen activator utilization for stroke, 6 , 20 , 21 these have included both public and professional (eg, physicians, nurses, and paramedics) education, limiting causal inference. Others have introduced community‐engaged approaches including youth‐based programs such as the hip‐hop stroke program in Harlem, New York, although they have not yet evaluated the effects on behavioral outcomes (eg, calling 9‐1‐1). 22 , 23 , 24 , 25 , 26
Our study may be informative for future stroke preparedness interventions. First, using a community‐engaged approach enabled us to develop potential solutions to address culturally bound barriers and perceptions and to deliver messaging using trained nonmedical stroke promoters from the intervention community. Unlike most prior interventions, CEERIAS focused on key decisional factors (eg, perceptions about stroke severity, mistrust, or the costs and benefits of calling 9‐1‐1) in addition to knowledge of stroke symptoms. Second, we applied behavioral change theories to develop solutions that were the most acceptable in the community in the forms of a “social contract” approach (pacts) and a culturally representative stroke promoter training program as part of the community‐partnered intervention. Third, we used geographic information system analysis of EMS utilization for suspected strokes, a potential primary outcome in future stroke preparedness intervention trials because it captures the intended behavior at the community level without the limitations imposed by data collection and analysis of confirmed strokes at the hospital level.
Our study had several limitations. Although we achieved nearly 20% penetration of our intervention in targeted neighborhoods, successful interventions may require even higher community penetration than we achieved to observe significant behavioral changes. 27 Although our results are likely generalizable to other urban settings with high proportions of Black residents or people at a socioeconomic disadvantage, 28 , 29 comparison and translation to other populations, including Hispanic communities, is uncertain. Cities without established community networks may also find reproducing our intervention challenging. As with other community‐engaged stroke preparedness programs, the significant effort required to conduct training sessions and face‐to‐face workshops and to monitor events may limit sustainability and broad dissemination. 24 , 30 , 31 Detailed assessment of every promoter activity, especially informal and small‐group sessions, was not feasible and, therefore, not done; this limited our ability to completely verify the fidelity of the intervention’s adoption. Furthermore, although the complex and nonstandardized nature of our intervention had the advantage of being pragmatic in its approach, it may limit generalizability, replication, and application elsewhere.
Because we did not match hospitals, imbalances in baseline characteristics between comparison groups may have also affected our results. A cluster randomized trial would be an ideal design to account for hospital‐ and region‐level imbalances and confounding but was beyond the scope of this project. The loss of the planned second intervention hospital could have increased the random sampling variability and thus reduced statistical power. However, because our unit of analysis was months, not patients, and because we had sufficient data from the other intervention hospital, excluding one of 2 planned intervention hospitals had a minimal impact on power. Nevertheless, patients in the service area of the included intervention hospital may have been transported to or arrived at the excluded hospital, biasing our results toward the null. It is also possible that the excluded hospital found no effect or an opposite effect on early arrival from the included hospital. We also did not collect hospital data beyond 1 year after intervention; therefore, long‐term effects of our intervention cannot be assessed. Last, although we trained stroke promoters on addressing the cost of EMS care, which is also disproportionately levied on minority communities, patients may have been disincentivized to call 9‐1‐1 for suspected stroke because of financial concerns.
In summary, we did not observe a significant effect of a community‐engaged stroke preparedness intervention on early arrival or EMS use for confirmed ischemic stroke in the South Side of Chicago. In secondary geographic information system analyses of EMS data, the observed increase in EMS use for suspected stroke in areas with the greatest message penetration with no discernable (unintended) effect on EMS use for other medical conditions suggests a possible intervention benefit. Our approach and findings should inform future study designs of community‐engaged stroke preparedness interventions.
Sources of Funding
This work was supported by the Patient‐Centered Outcomes Research Institute (AD‐1310‐07237).
Disclosures
The authors all received support from PCORI during the conduct of the study.
Supporting information
Data S1
Figures S1–S3
Acknowledgments
This research was supported by many community partners and organizations that all played essential roles throughout the duration of the project. Our research team would like to express our gratitude to all Community Advisory Board members for their committed involvement, guidance, and expertise throughout each phase of CEERIAS (Community Engagement for Early Recognition and Immediate Action in Stroke). We particularly acknowledge the efforts of our collaborator, Peggy Jones, who first developed the concept of the Pact to Act FAST. We also acknowledge the following community organizations and partners: American Heart Association/American Stroke Association Midwest Affiliate, A Safe Haven, the Chicago Fire Department, the Coalition of Limited English Speaking Elderly, the Chicago Hispanic Health Coalition, Walk With a Doc, Illinois Heart Rescue, and the Chicago and St Louis Regional Stroke Committee leadership and hospital members. We appreciate the number of volunteers who dedicated their time to our project. We also thank the staff and leadership at the intervention hospitals in the South Side of Chicago for allowing us to partner with them and improve the lives in their surrounding communities. Carlos Corado, a coordinator at Northwestern University, was invaluable in leading the Spanish‐speaking focus groups. Finally, we thank the participants in our focus groups, our promoters, and all other participants for their honesty and willingness to contribute meaningfully to this project.
(J Am Heart Assoc. 2020;9:e016344 DOI: 10.1161/JAHA.120.016344.)
Supplementary Materials for this article are available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.120.016344
For Sources of Funding and Disclosures, see page 9.
The results of this work were presented in abstract form at the International Stroke Conference, February 6 to 8, 2019, in Honolulu, Hawaii.
References
- 1. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;e46–e110. [DOI] [PubMed] [Google Scholar]
- 2. Prabhakaran S, Ruff I, Bernstein RA. Acute stroke intervention: a systematic review. JAMA. 2015;1451–1462. [DOI] [PubMed] [Google Scholar]
- 3. Schwamm LH, Ali SF, Reeves MJ, Smith EE, Saver JL, Messe S, Bhatt DL, Grau‐Sepulveda MV, Peterson ED, Fonarow GC. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With the Guidelines‐Stroke hospitals. Circ Cardiovasc Qual Outcomes. 2013;543–549. [DOI] [PubMed] [Google Scholar]
- 4. Schroeder EB, Rosamond WD, Morris DL, Evenson KR, Hinn AR. Determinants of use of emergency medical services in a population with stroke symptoms: the Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke. 2000;2591–2596. [DOI] [PubMed] [Google Scholar]
- 5. Ekundayo OJ, Saver JL, Fonarow GC, Schwamm LH, Xian Y, Zhao X, Hernandez AF, Peterson ED, Cheng EM. Patterns of emergency medical services use and its association with timely stroke treatment: findings from Get With the Guidelines‐Stroke. Circ Cardiovasc Qual Outcomes. 2013;262–269. [DOI] [PubMed] [Google Scholar]
- 6. Alberts MJ, Perry A, Dawson DV, Bertels C. Effects of public and professional education on reducing the delay in presentation and referral of stroke patients. Stroke. 1992;352–356. [DOI] [PubMed] [Google Scholar]
- 7. Becker K, Fruin M, Gooding T, Tirschwell D, Love P, Mankowski T. Community‐based education improves stroke knowledge. Cerebrovasc Dis. 2001;34–43. [DOI] [PubMed] [Google Scholar]
- 8. Marx JJ, Nedelmann M, Haertle B, Dieterich M, Eicke BM. An educational multimedia campaign has differential effects on public stroke knowledge and care‐seeking behavior. J Neurol. 2008;378–384. [DOI] [PubMed] [Google Scholar]
- 9. Mikulik R, Goldemund D, Reif M, Brichta J, Neumann J, Jarkovsky J, Kryza J. Calling 911 in response to stroke: no change following a four‐year educational campaign. Cerebrovasc Dis. 2011;342–348. [DOI] [PubMed] [Google Scholar]
- 10. Wall HK, Beagan BM, O'Neill J, Foell KM, Boddie‐Willis CL. Addressing stroke signs and symptoms through public education: the Stroke Heroes Act FAST campaign. Prev Chronic Dis. 2008;A49. [PMC free article] [PubMed] [Google Scholar]
- 11. Flynn D, Ford GA, Rodgers H, Price C, Steen N, Thomson RG. A time series evaluation of the FAST National Stroke Awareness Campaign in England. PLoS One. 2014;e104289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hodgson C, Lindsay P, Rubini F. Can mass media influence emergency department visits for stroke? Stroke. 2007;2115–2122. [DOI] [PubMed] [Google Scholar]
- 13. Mellon L, Doyle F, Rohde D, Williams D, Hickey A. Stroke warning campaigns: delivering better patient outcomes? A systematic review. Patient Relat Outcome Meas. 2015;61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Salimi Y, Shahandeh K, Malekafzali H, Loori N, Kheiltash A, Jamshidi E, Frouzan AS, Majdzadeh R. Is community‐based participatory research (CBPR) useful? A systematic review on papers in a decade. Int J Prev Med. 2012;386–393. [PMC free article] [PubMed] [Google Scholar]
- 15. Eisenstein AR, Song S, Mason M, Kandula NR, Richards C, Aggarwal NT, Prabhakaran SK. A community‐partnered approach to inform a culturally relevant health promotion intervention for stroke. Health Educ Behav. 2018;697–705. [DOI] [PubMed] [Google Scholar]
- 16. Gaglio B, Shoup JA, Glasgow RE. The RE‐AIM framework: a systematic review of use over time. Am J Public Health. 2013;e38–e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lahr MM, van der Zee DJ, Vroomen PC, Luijckx GJ, Buskens E. Thrombolysis in acute ischemic stroke: a simulation study to improve pre‐ and in‐hospital delays in community hospitals. PLoS One. 2013;e79049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Muller‐Nordhorn J, Wegscheider K, Nolte CH, Jungehulsing GJ, Rossnagel K, Reich A, Roll S, Villringer A, Willich SN. Population‐based intervention to reduce prehospital delays in patients with cerebrovascular events. Arch Intern Med. 2009;1484–1490. [DOI] [PubMed] [Google Scholar]
- 20. Wein TH, Staub L, Felberg R, Hickenbottom SL, Chan W, Grotta JC, Demchuk AM, Groff J, Bartholomew LK, Morgenstern LB. Activation of emergency medical services for acute stroke in a nonurban population: the T.L.L. Temple Foundation Stroke Project. Stroke. 2000;1925–1928. [DOI] [PubMed] [Google Scholar]
- 21. Morgenstern LB, Staub L, Chan W, Wein TH, Bartholomew LK, King M, Felberg RA, Burgin WS, Groff J, Hickenbottom SL, et al. Improving delivery of acute stroke therapy: the TLL Temple Foundation Stroke Project. Stroke. 2002;160–166. [DOI] [PubMed] [Google Scholar]
- 22. Morgenstern LB, Gonzales NR, Maddox KE, Brown DL, Karim AP, Espinosa N, Moye LA, Pary JK, Grotta JC, Lisabeth LD, et al. A randomized, controlled trial to teach middle school children to recognize stroke and call 911: the kids identifying and defeating stroke project. Stroke. 2007;2972–2978. [DOI] [PubMed] [Google Scholar]
- 23. Skolarus LE, Zimmerman MA, Murphy J, Brown DL, Kerber KA, Bailey S, Fowlkes S, Morgenstern LB. Community‐based participatory research: a new approach to engaging community members to rapidly call 911 for stroke. Stroke. 2011;1862–1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Skolarus LE, Zimmerman MA, Bailey S, Dome M, Murphy JB, Kobrossi C, Dombrowski SU, Burke JF, Morgenstern LB. Stroke ready intervention: community engagement to decrease prehospital delay. J Am Heart Assoc. 2016;e003331 DOI: 10.1161/JAHA.116.003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Williams O, DeSorbo A, Noble J, Gerin W. Child‐mediated stroke communication: findings from hip hop stroke. Stroke. 2012;163–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Williams O, Leighton‐Herrmann E, DeSorbo A, Hecht M, Hedmann M, Huq S, Gerin W, Chinchilli V, Ogedegbe G, Noble J. Hip hop stroke: study protocol for a randomized controlled trial to address stroke literacy. J Clin Trials. 2015;242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Merzel C, D'Afflitti J. Reconsidering community‐based health promotion: promise, performance, and potential. Am J Public Health. 2003;557–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Skolarus LE, Murphy JB, Zimmerman MA, Bailey S, Fowlkes S, Brown DL, Lisabeth LD, Greenberg E, Morgenstern LB. Individual and community determinants of calling 911 for stroke among African Americans in an urban community. Circ Cardiovasc Qual Outcomes. 2013;278–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Willey JZ, Williams O, Boden‐Albala B. Stroke literacy in Central Harlem: a high‐risk stroke population. Neurology. 2009;1950–1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kilkenny MF, Purvis T, Werner M, Reyneke M, Czerenkowski J, Cadilhac DA. Improving stroke knowledge through a ‘volunteer‐led’community education program in Australia. Prev Med. 2016;1–5. [DOI] [PubMed] [Google Scholar]
- 31. Yang L, Zhao Q, Zhu X, Shen X, Zhu Y, Yang L, Gao W, Li M. Effect of a comprehensive health education program on pre‐hospital delay intentions in high‐risk stroke population and caregivers. Qual Life Res. 2017;2153–2160. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Figures S1–S3


