Abstract
Background
Octogenarians (≥80 years old) are high‐risk patients for acute aortic dissection (AAD) surgery. However, no population‐based study has investigated the late outcomes of AAD surgery in octogenarians. This study aimed to investigate the late outcomes of AAD surgery in octogenarians.
Methods and Results
A total of 3998 patients who received AAD surgery from 2005 to 2013 were identified from the Taiwan National Health Insurance Research Database. In‐hospital complications and late outcomes including all‐cause mortality, major adverse cardiac and cerebrovascular event, respiratory failure, and redo aortic surgery were evaluated. The risks of late outcomes between octogenarians and nonoctogenarians were compared using the multivariable Cox proportional hazard model or Fine and Gray competing model. The numbers of the octogenarians who underwent type A and B AAD surgeries were 206 (6%; 206/3423) and 79 (13.7%; 79/575), respectively. Compared with the nonoctogenarians, the type A octogenarians had higher risks of in‐hospital mortality and several in‐hospital complications, whereas the type B octogenarians did not. Furthermore, compared with the nonoctogenarians, the type A octogenarians had a higher risk of all‐cause mortality (61.7% vs 32.5%; hazard ratio [HR], 2.35; 95% CI, 1.95–2.84) and a higher cumulative incidence of major adverse cardiac and cerebrovascular event and respiratory failure, and the type B octogenarians demonstrated a higher risk of all‐cause mortality (44.3% vs 30.4%; HR, 1.74; 95% CI, 1.18–2.55). The octogenarians receiving AAD surgeries had higher mortality rates than the normal octogenarian population.
Conclusions
Octogenarians receiving AAD surgeries exhibit worse late outcomes than nonoctogenarian counterparts.
Keywords: acute aortic dissection, age, aortic dissection, aortic dissection surgery, octogenarian
Subject Categories: Aging, Epidemiology, Cardiovascular Surgery, Aortic Dissection
Nonstandard Abbreviations and Acronyms
- AAD
acute aortic dissection
- LHID
Longitudinal Health Insurance Database
- MACCE
major adverse cardiac and cerebrovascular event
- NHI
National Health Insurance
- NHIRD
National Health Insurance Research Database
Clinical Perspective
What Is New?
The number of octogenarians receiving acute aortic dissection (AAD) surgery is increasing.
Compared with nonoctogenarians, octogenarians who received type A AAD surgery had higher risks of in‐hospital mortality and a higher cumulative incidence of all‐cause mortality, major adverse cardiac and cerebrovascular event, and respiratory failure, whereas octogenarians who received type B AAD surgery only showed a higher cumulative incidence of all‐cause mortality.
What Are the Clinical Implications?
Old age is not a contraindication for AAD surgery, but the patient and family members should be well informed about the high risks involved in the surgery.
Acute aortic dissection (AAD) is an emergency condition with high rates of mortality and morbidity. 1 , 2 According to the International Registry of Acute Aortic Dissection (IRAD), the surgical mortality rate of type A aortic dissection has significantly decreased from 25% to 18% during 1995 through 2013. In type B aortic dissection, the mortality rate of open surgical repair has decreased from 30% to 21%, with increasing trends in endovascular treatment. 3 Age is associated with the mortality rate in patients with AAD, 4 , 5 , 6 , 7 especially in octogenarians. 8 , 9 , 10 , 11 Thus, with population aging, AAD in octogenarians is becoming a concern. The number of octogenarians with AAD is expected to rise in future, and these patients with limited life spans and relatively high surgical risks need to receive appropriate treatments. Consequently, additional studies on AAD in octogenarians are needed.
Recent studies 11 , 12 , 13 , 14 , 15 , 16 , 17 have shown that octogenarians with AAD should receive type A AAD surgery, with satisfactory outcomes; however, these studies have small sample sizes. Other studies 18 , 19 have shown the epidemiology and late outcomes of type B AAD surgery, but they have not focused on the octogenarian population. Therefore, a nationwide cohort study evaluating the late outcomes of AAD surgery in octogenarians is warranted.
Aortic surgeries are reimbursed by the National Health Insurance (NHI) program, which covers more than 99% of the population of Taiwan. In this nationwide cohort study, using the Taiwan National Health Insurance Research Database (NHIRD), we investigated the late outcomes of both type A and type B AAD surgery in octogenarians in Taiwan.
METHODS
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Population and Validation
By using NHIRD, 20 , 21 , 22 patients who were admitted to the hospital with the diagnostic code of aortic dissection (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] code 441.0) and who received NHI reimbursement codes (69024, 69035, 69036, and 69037) for surgical treatment of aortic dissection from 2005 to 2013 were identified. Those who had a previous diagnosis of aortic dissection or received redo aortic dissection surgery were excluded. Subsequently, patients newly diagnosed with aortic dissection were classified into type A or type B groups using Taiwan NHI reimbursement codes and surgical material codes of vascular graft of aorta and endovascular prosthesis. The admission date of AAD surgery was assigned as the index date.
Additionally, an octogenarian group who were not diagnosed with aortic dissection and did not undergo AAD surgery was identified from the Longitudinal Health Insurance Database 2000 (LHID 2000), which is a subset of the NHIRD and contains the claims data of 1 million individuals randomly sampled from the year 2000 Registry of Beneficiaries. Each octogenarian in the type A or type B AAD groups was frequency‐matched with 10 nondissection octogenarian controls based on birth date (±180 days) and sex. The index date of each octogenarian control was assigned as the date of surgery of their corresponding matched octogenarian patient. The octogenarian control cohort was created separately for type A and type B AAD groups.
Internal validation was performed to verify the accuracy of the inclusion criteria of our AAD population of this study. The validation was conducted through a chart review of consecutive patients diagnosed with aortic dissection at Linkou Chang Gung Memorial Hospital from 2011 to 2013. The anonymous data of patients in the NHIRD were linked with the hospital records based on sex, birth date, and admission and discharge dates. In our validation, the positive predictive values of the ICD-9-CM code 441.0 (which represents aortic dissection) and surgical reimbursement codes were 97.06% (297/306) and 94.41% (152/161), respectively. The positive predictive values of type A and type B AAD were 88.98% (105/118) and 92% (46/50), respectively (data not shown). The study was exempted from ethical review because all data in the NHIRD were anonymized (104‐7990B), and the internal validation was approved by the institutional review board of Chang Gung Memorial Hospital (201601407B0).
Comorbidities and Outcomes
Comorbidities were detected using diagnostic codes in inpatient records before the index date, which could be tracked to the year 1997. In‐hospital complications during the index admission were identified using ICD‐9‐CM diagnostic or Taiwan NHI reimbursement codes. Late outcomes were all‐cause mortality, major adverse cardiac and cerebrovascular event (MACCE), respiratory failure, and redo aortic surgery. Mortality was defined as withdrawal from the NHI program. 23 MACCE was defined as admission with a principal diagnosis of acute myocardial infarction, heart failure, or stroke, with validated diagnostic codes. 24 , 25 , 26 Respiratory failure was verified based on the possession of a catastrophic illness certificate, and redo aortic surgery was detected using Taiwan NHI reimbursement codes. Details of ICD-9-CM codes are provided in Table S1.
Information regarding follow‐ups was extracted from the Registry for Beneficiaries, which is a subset of the NHIRD. All patients were followed up from index admission to December 31, 2013, or the date of death, whichever occurred first.
Statistical Analysis
Baseline characteristics between groups were compared using the chi‐square test for categorical variables or the independent sample t test for continuous variables. In‐hospital outcomes in the octogenarians and nonoctogenarians were compared using multivariate logistic regression for categorical variables or multivariate linear regression for continuous variables. The risk factors for in‐hospital death were identified by introducing the variables with P<0.2 into the multivariate logistic regression analysis with backward selection. The risk of all‐cause mortality (including in‐hospital death) between the octogenarians and nonoctogenarians was compared using multivariable Cox proportional hazard regression. The cumulative incidence of other time‐to‐event outcomes (MACCE, respiratory failure, and redo aortic surgery) between the groups was compared using the multivariable Fine and Gray model, in which all‐cause mortality was considered as a competing risk. All regression analyses were adjusted for sex, hospital volume of AAD surgery, surgery year, and other details pertaining to the surgical procedure.
A two‐sided P value lower than 0.05 was considered statistically significant, and no adjustment for multiple testing (multiplicity) was made in this study to avoid a low statistical power. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC), including the procedure of “phreg” for survival analyses and the macro “% cif” for generating cumulative incidence.
RESULTS
Epidemiology of AAD Surgery
A total of 3998 patients, including 206 and 79 octogenarians receiving type A and B AAD surgery, respectively, were included in this study (Figure 1A). From 2005 to 2013, the numbers of AAD surgeries had increased (P<0.001), with an increase in the proportion of octogenarians (P=0.008) who underwent the procedure; however, no significant decrease was observed in the in‐hospital mortality rate in the octogenarians (P=0.839; Figure 1B).
Figure 1. Inclusion of the study patients (A) and the epidemiology of AAD surgery (B).
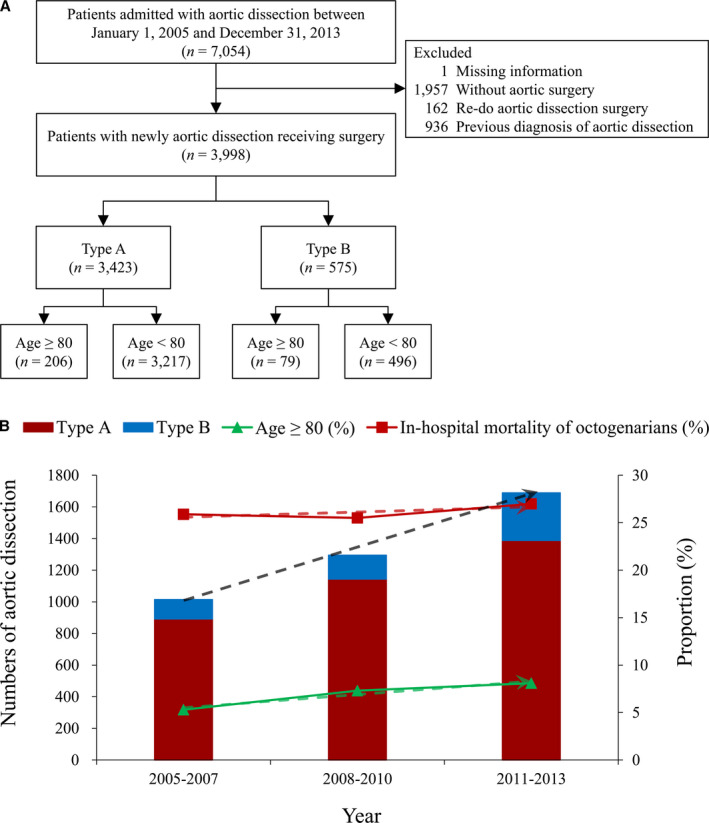
The dashed line represents the fitted (predicted) trend based on the observed data. AAD indicates acute aortic dissection.
Population Characteristics
The clinical and surgical characteristics of the study population are listed in Table 1. The type A octogenarians had a higher prevalence of comorbidities and higher Charlson comorbidity index scores. The type B octogenarians had a higher prevalence of chronic obstructive pulmonary disease and were more likely to receive aortic stent surgery at a high‐volume center.
Table 1.
Clinical and Surgical Characteristics of the Study Population
| Variables | Type A | Type B | ||||||
|---|---|---|---|---|---|---|---|---|
|
Total (n=3423) |
Age ≥80 y (n=206) |
Age <80 y (n=3217) |
P Value |
Total (n=575) |
Age ≥80 y (n=79) |
Age <80 y (n=496) |
P Value | |
| Characteristic | ||||||||
| Age, y | 59.1±13.6 | 83.7±2.7 | 57.5±12.5 | 62.4±15.6 | 84.5±3.7 | 58.9±13.7 | ||
| Male | 2351 (68.7) | 89 (43.2) | 2262 (70.3) | <0.001 | 470 (81.7) | 61 (77.2) | 409 (82.5) | 0.262 |
| Comorbidity | ||||||||
| Marfan syndrome | 84 (2.5) | 0 (0.0) | 84 (2.6) | 0.019 | 7 (1.2) | 0 (0.0) | 7 (1.4) | 0.288 |
| Hypertension | 2355 (68.8) | 141 (68.4) | 2214 (68.8) | 0.910 | 426 (74.1) | 63 (79.7) | 363 (73.2) | 0.216 |
| Diabetes mellitus | 364 (10.6) | 39 (18.9) | 325 (10.1) | <0.001 | 74 (12.9) | 8 (10.1) | 66 (13.3) | 0.433 |
| Heart failure | 162 (4.7) | 33 (16.0) | 129 (4.0) | <0.001 | 33 (5.7) | 4 (5.1) | 29 (5.8) | 0.781 |
| Old myocardial infarction | 71 (2.1) | 2 (1.0) | 69 (2.1) | 0.252 | 27 (4.7) | 6 (7.6) | 21 (4.2) | 0.190 |
| Peripheral arterial disease | 123 (3.6) | 7 (3.4) | 116 (3.6) | 0.877 | 45 (7.8) | 9 (11.4) | 36 (7.3) | 0.204 |
| Atrial fibrillation | 204 (6.0) | 31 (15.0) | 173 (5.4) | <0.001 | 13 (2.3) | 3 (3.8) | 10 (2.0) | 0.323 |
| Old stroke | 270 (7.9) | 30 (14.6) | 240 (7.5) | <0.001 | 70 (12.2) | 8 (10.1) | 62 (12.5) | 0.549 |
| Chronic kidney disease | 179 (5.2) | 13 (6.3) | 166 (5.2) | 0.472 | 49 (8.5) | 7 (8.9) | 42 (8.5) | 0.907 |
| Liver cirrhosis | 38 (1.1) | 3 (1.5) | 35 (1.1) | 0.625 | 11 (1.9) | 2 (2.5) | 9 (1.8) | 0.666 |
| Coagulopathy | 74 (2.2) | 6 (2.9) | 68 (2.1) | 0.445 | 13 (2.3) | 1 (1.3) | 12 (2.4) | 0.522 |
| COPD | 133 (3.9) | 21 (10.2) | 112 (3.5) | <0.001 | 41 (7.1) | 10 (12.7) | 31 (6.3) | 0.040 |
| Previous cardiac surgery | 52 (1.5) | 4 (1.9) | 48 (1.5) | 0.609 | 18 (3.1) | 1 (1.3) | 17 (3.4) | 0.306 |
| CCI score | 2.1±1.5 | 2.7±1.8 | 2.0±1.5 | <0.001 | 2.3±1.8 | 2.6±1.8 | 2.3±1.8 | 0.139 |
| Hospital volume of aortic dissection surgery | 0.571 | 0.006 | ||||||
| First quartile (1–94) | 845 (24.7) | 51 (24.8) | 794 (24.7) | 120 (20.9) | 15 (19.0) | 105 (21.2) | ||
| Second quartile (109–206) | 893 (26.1) | 52 (25.2) | 841 (26.1) | 104 (18.1) | 12 (15.2) | 92 (18.5) | ||
| Third quartile (207–334) | 904 (26.4) | 62 (30.1) | 842 (26.2) | 125 (21.7) | 8 (10.1) | 117 (23.6) | ||
| Fourth quartile (336–665) | 781 (22.8) | 41 (19.9) | 740 (23.0) | 226 (39.3) | 44 (55.7) | 182 (36.7) | ||
| Surgery year | 0.151 | 0.366 | ||||||
| 2005–2007 | 892 (26.1) | 42 (20.4) | 850 (26.4) | 122 (21.2) | 12 (15.2) | 110 (22.2) | ||
| 2008–2010 | 1143 (33.4) | 72 (35.0) | 1071 (33.3) | 152 (26.4) | 22 (27.8) | 130 (26.2) | ||
| 2011–2013 | 1388 (40.5) | 92 (44.7) | 1296 (40.3) | 301 (52.3) | 45 (57.0) | 256 (51.6) | ||
| Type A dissection surgical detail | ||||||||
| Extension of aortic surgery | ||||||||
| Partial or total aortic arch replacement | 1012 (29.6) | 67 (32.5) | 945 (29.4) | 0.337 | … | … | … | … |
| Aortic root replacement (Bentall operation) | 360 (10.5) | 13 (6.3) | 347 (10.8) | 0.042 | … | … | … | … |
| Elephant trunk | 86 (2.5) | 1 (0.5) | 85 (2.6) | 0.055 | … | … | … | … |
| Ascending aorta replacement only | 2044 (59.7) | 130 (63.1) | 1914 (59.5) | 0.306 | … | … | … | … |
| Additional surgery | ||||||||
| CABG | 335 (9.8) | 20 (9.7) | 315 (9.8) | 0.969 | … | … | … | … |
| Valve replacement | 308 (9.0) | 23 (11.2) | 285 (8.9) | 0.262 | … | … | … | … |
| Type B surgery type | <0.001 | |||||||
| Open repair | … | … | … | … | 234 (40.7) | 16 (20.3) | 218 (44.0) | |
| Aortic stent | … | … | … | … | 341 (59.3) | 63 (79.7) | 278 (56.0) | |
| Follow‐up, y | 2.7±2.6 | 1.6±2.1 | 2.8±2.6 | <0.001 | 2.3±2.3 | 2.0±1.9 | 2.4±2.4 | 0.146 |
CABG indicates coronary artery bypass graft; CCI, Charlson comorbidity index; and COPD, chronic obstructive pulmonary disease.
In‐Hospital Complications
Several covariates, including sex, hospital volume of AAD surgery, surgery year, and other surgical details, were adjusted for in comparisons of in‐hospital complications. The type A octogenarians had higher rates of in‐hospital mortality (odds ratio [OR], 2.20; 95% CI, 1.61–3.01) and complications. In addition, the duration of stay in the intensive care unit (regression coefficient [B], 2.75; 95% CI, 0.99–4.51) and the hospital (B, 3.93; 95% CI, 0.57–7.29) was longer in this group than in the nonoctogenarian counterparts (Table 2). By contrast, no significant difference was observed in in‐hospital outcomes between the octogenarians receiving type B AAD surgery and the nonoctogenarian counterparts (Table 2). It is noted that the nonsignificant group differences in type B surgery may be due to the small sample size.
Table 2.
Operation‐Related Complications and Outcomes of Type A and Type B Aortic Dissection Surgery in the Octogenarians and Nonoctogenarians
| Variables | Type A | Type B | ||||
|---|---|---|---|---|---|---|
|
Age ≥80 y (n=206) |
Age <80 y (n=3217) |
OR/B for Age ≥80 y (95% CI)* |
Age ≥80 y (n=79) |
Age <80 y (n=496) |
OR/B for Age ≥80 y (95% CI)* |
|
| Categorical parameter | ||||||
| Cardiogenic shock and need MCS | 22 (10.7) | 254 (7.9) | 1.53 (0.95 to 2.47) | 1 (1.3) | 22 (4.4) | 0.36 (0.05 to 2.82) |
| Respiratory failure | 60 (29.1) | 553 (17.2) | 1.92 (1.39 to 2.65)† | 7 (8.9) | 68 (13.7) | 0.64 (0.27 to 1.47) |
| New onset stroke | 16 (7.8) | 376 (11.7) | 0.63 (0.37 to 1.07) | 4 (5.1) | 29 (5.8) | 1.06 (0.35 to 3.22) |
| New onset ischemic stroke | 15 (7.3) | 355 (11.0) | 0.63 (0.36 to 1.08) | 4 (5.1) | 27 (5.4) | 1.22 (0.40 to 3.74) |
| New onset hemorrhagic stroke | 1 (0.5) | 33 (1.0) | 0.47 (0.06 to 3.52) | 0 (0.0) | 5 (1.0) | NA |
| Reexploration for bleeding | 14 (6.8) | 248 (7.7) | 0.89 (0.51 to 1.57) | 1 (1.3) | 18 (3.6) | 0.40 (0.05 to 3.24) |
| De novo dialysis | 40 (19.4) | 484 (15.0) | 1.54 (1.07 to 2.22)† | 5 (6.3) | 62 (12.5) | 0.66 (0.25 to 1.75) |
| Sepsis | 20 (9.7) | 184 (5.7) | 1.82 (1.11 to 2.98)† | 0 (0.0) | 32 (6.5) | NA |
| Deep wound infection | 11 (5.3) | 119 (3.7) | 1.58 (0.83 to 3.03) | 0 (0.0) | 16 (3.2) | NA |
| In hospital mortality | 70 (34.0) | 649 (20.2) | 2.20 (1.61 to 3.01)† | 5 (6.3) | 78 (15.7) | 0.56 (0.21 to 1.47) |
| Continuous parameter | ||||||
| ICU duration, d | 12.9±14.9 | 10.1±12.2 | 2.75 (0.99 to 4.51)† | 6.6±12.3 | 8.9±12.5 | −0.85 (−3.81 to 2.10) |
| In hospital stay | 27.9±27.7 | 23.8±23.4 | 3.93 (0.57 to 7.29)† | 22.6±23.4 | 26.2±27.9 | −1.81 (−8.32 to 4.69) |
| In hospital cost (NTD×104) | 64.0±37.2 | 61.6±41.5 | 4.15 (−1.32 to 9.62) | 62.7±47.5 | 69.2±43.2 | −4.73 (−14.62 to 5.15) |
B indicates regression coefficient; ICU, intensive care unit; MCS, mechanical circulatory support system; NA, not applicable; NTD, New Taiwan dollar; and OR, odds ratio.
Adjusted with sex, hospital volume of type A aortic dissection surgery, surgery year, and surgery details.
P<0.05.
Risk Factor Analysis of In‐Hospital Mortality
The risk factors for in‐hospital mortality for the type A octogenarians were history of heart failure (OR, 2.36; 95% CI, 1.10–5.07) and aortic root replacement (OR, 3.27; 95% CI, 1.01–10.58), and in the type B octogenarians, aortic stent surgery was a protective factor (OR, 0.05; 95% CI, 0.01–0.47; Figure 2). The in‐hospital mortality rates of octogenarians with type A AAD who had zero, one, and two risk factors were 28.8, 52.5, and 66.7%, respectively. The in‐hospital mortality rates of octogenarians with type B AAD who underwent aortic stent surgery and who did not undergo aortic stent surgery were 1.6% (1/63) and 25% (4/16), respectively.
Figure 2. Risk factor analysis of in‐hospital death in the octogenarians.
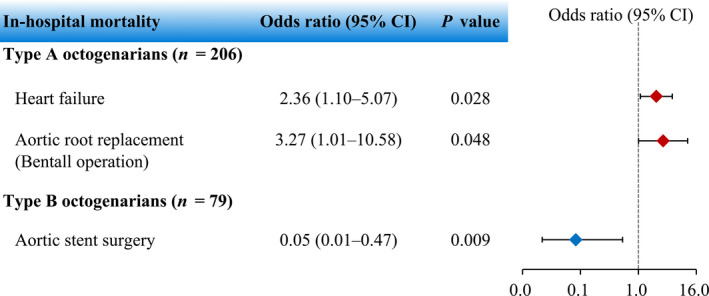
CI indicates confidence interval.
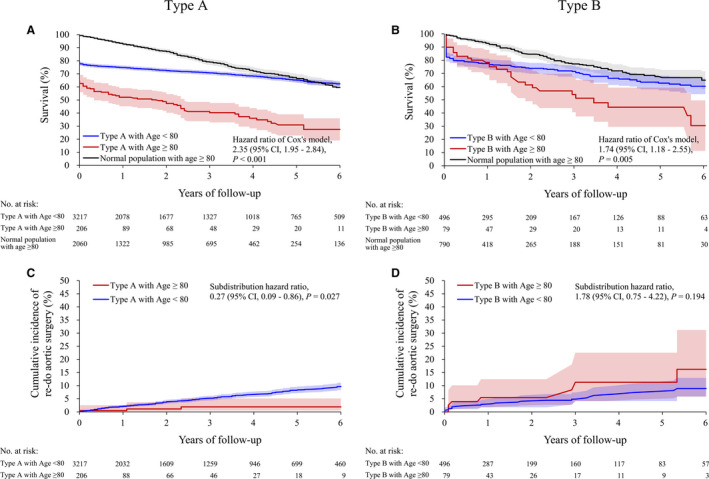
Late Outcomes During Follow‐Up
The median follow‐up of the entire analyzed cohort was 1.97 (25th–75th percentile, 0.15–4.59) years. During long‐term follow‐up, the type A octogenarians had a higher risk of all‐cause mortality (61.7% vs 32.5%; hazard ratio [HR], 2.35; 95% CI, 1.95–2.84; Figure 3A), a higher cumulative incidence of MACCE (11.2% vs 6.8%; subdistribution HR, 1.76; 95% CI, 1.13–2.74; Figure S1) and respiratory failure (18.9% vs 7.1%; subdistribution HR, 2.93; 95% CI, 2.05–4.18; Figure S2), and a lower rate of redo aortic surgery (1.5% vs 6.5%; subdistribution HR, 0.27; 95% CI, 0.09–0.86; Figure S3). The type B octogenarians had a higher risk of all‐cause mortality (44.3% vs 30.4%; HR, 1.74; 95% CI, 1.18–2.55; Figure 3B). However, no significant differences were observed in the cumulative incidence of MACCE, respiratory failure (Figures S3 and S4), and redo aortic surgery between the two groups (Figure 3D). It is noted that the nonsignificant group differences in type B surgery may be due to the small sample size. Both type A and B groups had higher mortality rates than the normal octogenarian population (Figures 3A and 3B). The cumulative mortality rate was 26.2% at 1 year and 32% at 5 year for the type A octogenarians, and the rate was 21.7% at 1 year and 30.4% at 5 year for the type B octogenarians.
Figure 3. Cumulative Kaplan–Meier survival of all‐cause mortality in patients who received type A surgery (A) and type B surgery (B) and cumulative incidence of redo aortic surgery in patients who received type A surgery (C) and type B surgery (D).
DISCUSSION
In this study, we reported the epidemiology and late outcomes of AAD surgery in octogenarians. Pape et al 3 showed improvements in surgical mortality in patients receiving type A and B AAD surgery, and Jones et al 19 reported decreasing mortalities in patients who underwent open surgery or endovascular treatments for type B AAD. Nonetheless, improvements in surgical techniques and perioperative care were not reflected in total in‐hospital mortality in the octogenarians in the current nationwide study.
Type A Aortic Dissection
Several studies 4 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 have shown acceptable in‐hospital mortality rates and late outcomes of surgery in octogenarians with type A AAD; however, these studies have small sample sizes. Piccardo et al 11 reported an in‐hospital mortality rate of 44.3% and 5‐year overall survival of 32% in type A octogenarians (n=79) in Europe, and they recommended surgery only for uncomplicated cases. In a study in Japan, 17 the in‐hospital mortality and 5‐year overall survival rates in type A octogenarians (n=112) were 6.3 and 57.1%, respectively, with no differences in surgical mortality or complications between the octogenarian and nonoctogenarian groups. In the present nationwide study with a large sample size (n=206 octogenarians), the in‐hospital mortality and 5‐year cumulative mortality rates were 34% and 68%, respectively. In contrast to the nonoctogenarian group, octogenarians presented with higher in‐hospital mortality and a higher cumulative incidence of morbidity during long‐term follow‐up. However, the rate of redo aortic surgery was lower in octogenarians than in nonoctogenarians, and aortic root replacement was found to be a risk factor for in‐hospital mortality. These findings are consistent with those of previous studies, which indicate that conservative surgical strategies should be considered for patients with limited life spans and low reintervention rates. 15 , 16 , 17 This study showed that the in‐hospital mortality rates of octogenarians with type A AAD who had zero, one, and two risk factors were 28.8, 52.5, and 66.7%, respectively. Thus, octogenarians with type A AAD who have risk factors may have a similar in‐hospital mortality rate irrespective of whether they undergo surgical or medical treatment 3 , 12 ; further studies on this high‐risk group are required. The quality of life after surgery must also be considered in these patients, 12 , 14 because type A AAD is associated with high mortality and morbidity. Old age is not a contraindication for type A AAD surgery, but the patient and family members should be well informed about the high risks involved in the surgery. Thus, based on the clinical condition of the individual, the most appropriate treatment must be selected.
Type B Aortic Dissection
Recent studies 3 , 19 have reported the increasing use of the endovascular approach for the treatment of type B aortic dissection, and this approach resulted in excellent in‐hospital mortality compared with traditional open surgical repair. Old age is a risk factor for in‐hospital mortality for type B AAD surgery. 6 , 7 In this study, we demonstrated the increasing trend of aortic stent surgery. Unlike octogenarians with type A AAD, those with type B AAD who underwent surgery were few and more likely to undergo aortic stent surgery at a high‐volume center; additionally, their comorbidities were almost the same as those of nonoctogenarians, which may have influenced our results. The mortality rate in the octogenarians who received aortic stent surgery was also excellent when compared with those who underwent open surgery. Therefore, rather than traditional open surgical repair, aortic stent surgery should be strongly considered for octogenarians with type B AAD. However, according to recent research, treatment for type B AAD should be based on the clinical condition of the patient (complicated or uncomplicated) and whether medical or endovascular treatment should be used in uncomplicated cases is still under debate. 1 In this study, we did not have clinical data to differentiate between aortic dissection patients with complicated and uncomplicated conditions, and the data of patients receiving medical treatment were not available. Thus, whether medical or endovascular treatment should be selected in the octogenarians in this study was not discussed.
Study Strengths
This study has several advantages. First, this is a population‐based cohort study with a large sample size and a nearly complete long‐term follow‐up. Second, AAD surgeries are reimbursed by the Taiwan NHI program, thus eliminating selection bias due to economic reasons. Third, we could differentiate the types of AAD by using the Taiwan NHI reimbursement and surgical material codes, and the accuracy of the types of AAD was validated in this study.
Study Limitations
Nevetheless, there are a few limitations of this study. First, the diagnosis of AAD and classification into type A and B were based on ICD-9-CM, Taiwan NHI reimbursement, and surgical material codes; thus, the possibility of coding errors cannot be eliminated. However, we performed internal validation to verify the accuracy of the inclusion criteria of our AAD population. Second, detailed clinical data are unavailable in the Taiwan NHIRD. Therefore, such information, which may influence the outcomes, was not included in this study. However, experts in the NHI program regularly review medical records to ensure that every procedure, including laboratory and radiologic examinations, medication, and surgery, is compatible with the indications and treatment guidelines for reimbursement. Therefore, this bias may have limited impact on our conclusion. Third, we could not identify the type of dissection in patients who did not undergo surgery by using the Taiwan NHIRD. Therefore, we added a nonsurgical group of patients who had either type A or type B AAD as a reference for comparison with our study population (Table S2). Finally, the evidence level of our study was limited by the retrospective nature of the analysis and its inherent limitations.
CONCLUSIONS
In conclusion, octogenarians receiving AAD surgeries exhibit worse late outcomes than nonoctogenarian counterparts. With population aging globally, it is important to improve the outcomes of AAD in the elderly population.
Sources of Funding
This work was supported by a grant from Chang Gung Memorial Hospital, Taiwan CMRPG3J0661 (S.W.C.) and by the Ministry of Science and Technology grant MOST 107‐2314‐B‐182A‐152 (S.W.C.).
Disclosures
None.
Supporting information
Tables S1–S2
Figures S1–S4
Acknowledgments
This study was based on data from the NHIRD provided by the NHI administration, Ministry of Health and Welfare of Taiwan, and managed by the National Health Research Institutes of Taiwan. However, the interpretation and conclusions contained in this paper only represent the authors. The authors thank for the statistical assistance and acknowledge the support of the Maintenance Project of the Center for Big Data Analytics and Statistics (Grant CLRPG3D0045) at Chang Gung Memorial Hospital for statistical consultation and data analysis. The authors also thank Alfred Hsing‐Fen Lin and Zoe Ya‐Jhu Syu for their assistance with the statistical analysis.
(J Am Heart Assoc. 2020;9:e017147 DOI: 10.1161/JAHA.120.017147.)
Supplementary Materials for this article are available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.120.017147
For Sources of Funding and Disclosures, see page 8.
References
- 1. Mussa FF, Horton JD, Moridzadeh R, Nicholson J, Trimarchi S, Eagle KA. Acute aortic dissection and intramural hematoma: a systematic review. JAMA. 2016;316:754–763. [DOI] [PubMed] [Google Scholar]
- 2. Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, Evangelista A, Fattori R, Suzuki T, Oh JK, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283:897–903. [DOI] [PubMed] [Google Scholar]
- 3. Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S, Evangelista A, Myrmel T, Larsen M, Harris KM, Greason K, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17‐year trends from the International Registry of Acute Aortic Dissection. J Am Coll Cardiol. 2015;66:350–358. [DOI] [PubMed] [Google Scholar]
- 4. Trimarchi S, Eagle KA, Nienaber CA, Rampoldi V, Jonker FH, de Vincentiis C, Frigiola A, Menicanti L, Tsai T, Froehlich J, et al. Role of age in acute type A aortic dissection outcome: report from the International Registry of Acute Aortic Dissection (IRAD). J Thorac Cardiovasc Surg. 2010;140:784–789. [DOI] [PubMed] [Google Scholar]
- 5. Rylski B, Hoffmann I, Beyersdorf F, Suedkamp M, Siepe M, Nitsch B, Blettner M, Borger MA, Weigang E. Acute aortic dissection type A: age‐related management and outcomes reported in the German Registry for Acute Aortic Dissection Type A (GERAADA) of over 2000 patients. Ann Surg. 2014;259:598–604. [DOI] [PubMed] [Google Scholar]
- 6. Trimarchi S, Nienaber CA, Rampoldi V, Myrmel T, Suzuki T, Bossone E, Tolva V, Deeb MG, Upchurch GR Jr, Cooper JV, et al. Role and results of surgery in acute type B aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation. 2006;114:I357–364. [DOI] [PubMed] [Google Scholar]
- 7. Tolenaar JL, Froehlich W, Jonker FH, Upchurch GR Jr, Rampoldi V, Tsai TT, Bossone E, Evangelista A, O’Gara P, Pape L, et al. Predicting in‐hospital mortality in acute type B aortic dissection: evidence from International Registry of Acute Aortic Dissection. Circulation. 2014;130:S45–S50. [DOI] [PubMed] [Google Scholar]
- 8. Biancari F, Vasques F, Benenati V, Juvonen T. Contemporary results after surgical repair of type A aortic dissection in patients aged 80 years and older: a systematic review and meta‐analysis. Eur J Cardiothorac Surg. 2011;40:1058–1063. [DOI] [PubMed] [Google Scholar]
- 9. Bruno VD, Chivasso P, Guida G, Vohra HA. Surgical repair of Stanford type A aortic dissection in elderly patients: a contemporary systematic review and meta‐analysis. Ann Cardiothorac Surg. 2016;5:257–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Piccardo A, Regesta T, Pansini S, Concistrè G, Dell’Aquila A, Scarano F, Martinelli L, Passerone G. Should octogenarians be denied access to surgery for acute type A aortic dissection? J Cardiovasc Surg. 2009;50:205–212. [PubMed] [Google Scholar]
- 11. Piccardo A, Le Guyader A, Regesta T, Gariboldi V, Zannis K, Tapia M, Collart F, Kirsch M, Caus T, Cornu E, et al. Octogenarians with uncomplicated acute type a aortic dissection benefit from emergency operation. Ann Thorac Surg. 2013;96:851–856. [DOI] [PubMed] [Google Scholar]
- 12. Hata M, Sezai A, Niino T, Yoda M, Unosawa S, Furukawa N, Osaka S, Murakami T, Minami K. Should emergency surgical intervention be performed for an octogenarian with type A acute aortic dissection? J Thorac Cardiovasc Surg. 2008;135:1042–1046. [DOI] [PubMed] [Google Scholar]
- 13. Hata M, Sezai A, Yoshitake I, Wakui S, Minami K, Shiono M. Midterm outcomes of rapid, minimally invasive resection of acute type A aortic dissection in octogenarians. Ann Thorac Surg. 2010;89:1860–1864. [DOI] [PubMed] [Google Scholar]
- 14. Tang GH, Malekan R, Yu CJ, Kai M, Lansman SL, Spielvogel D. Surgery for acute type A aortic dissection in octogenarians is justified. J Thorac Cardiovasc Surg. 2013;145:S186–S190. [DOI] [PubMed] [Google Scholar]
- 15. El‐Sayed Ahmad A, Papadopoulos N, Detho F, Srndic E, Risteski P, Moritz A, Zierer A. Surgical repair for acute type A aortic dissection in octogenarians. Ann Thorac Surg. 2015;99:547–551. [DOI] [PubMed] [Google Scholar]
- 16. Kondoh H, Satoh H, Daimon T, Tauchi Y, Yamamoto J, Abe K, Matsuda H. Outcomes of limited proximal aortic replacement for type A aortic dissection in octogenarians. J Thorac Cardiovasc Surg. 2016;152:439–446. [DOI] [PubMed] [Google Scholar]
- 17. Kawahito K, Kimura N, Yamaguchi A, Aizawa K, Misawa Y, Adachi H. Early and late surgical outcomes of acute type A aortic dissection in octogenarians. Ann Thorac Surg. 2018;105:137–143. [DOI] [PubMed] [Google Scholar]
- 18. Tsai TT, Fattori R, Trimarchi S, Isselbacher E, Myrmel T, Evangelista A, Hutchison S, Sechtem U, Cooper JV, Smith DE, et al. Long‐term survival in patients presenting with type B acute aortic dissection: insights from the International Registry of Acute Aortic Dissection. Circulation. 2006;114:2226–2231. [DOI] [PubMed] [Google Scholar]
- 19. Jones DW, Goodney PP, Nolan BW, Brooke BS, Fillinger MF, Powell RJ, Stone DH. National trends in utilization, mortality, and survival after repair of type B aortic dissection in the Medicare population. J Vasc Surg. 2014;60:11–19.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chen SW, Chang CH, Lin YS, Wu VC, Chen DY, Tsai FC, Hung MJ, Chu PH, Lin PJ, Chen TH. Effect of dialysis dependence and duration on post‐coronary artery bypass grafting outcomes in patients with chronic kidney disease: a nationwide cohort study in Asia. Int J Cardiol. 2016;223:65–71. [DOI] [PubMed] [Google Scholar]
- 21. Chou AH, Chen CC, Lin YS, Lin MS, Wu VC, Ting PC, Chen SW. A population‐based analysis of endovascular aortic stent graft therapy in patients with liver cirrhosis. J Vasc Surg. 2018;69:1395–1404. [DOI] [PubMed] [Google Scholar]
- 22. Chen CC, Chen TH, Tu PH, Wu VC, Yang CH, Wang AY, Lee ST, Tsai FC, Chen SW. Long‐term outcomes for patients with stroke after coronary and valve surgery. Ann Thorac Surg. 2018;106:85–91. [DOI] [PubMed] [Google Scholar]
- 23. Cheng CL, Chien HC, Lee CH, Lin SJ, Yang YH. Validity of in‐hospital mortality data among patients with acute myocardial infarction or stroke in National Health Insurance Research Database in Taiwan. Int J Cardiol. 2015;201:96–101. [DOI] [PubMed] [Google Scholar]
- 24. Cheng CL, Lee CH, Chen PS, Li YH, Lin SJ, Yang YH. Validation of acute myocardial infarction cases in the National Health Insurance Research Database in Taiwan. J Epidemiol. 2014;24:500–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf. 2011;20:236–242. [DOI] [PubMed] [Google Scholar]
- 26. Hsieh CY, Chen CH, Li CY, Lai ML. Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J Formos Med Assoc. 2015;114:254–259. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S2
Figures S1–S4


