Abstract
In general merchant ships do not have medical facilities on board. When seafarer got sickness or accident, either ship captain or officers who are in charge will assist them, but these people do not have enough medical knowledge. To overcome this, we developed a Seafarer Health Expert System (SHES) that can facilitate telemedical services in an emergency. A comprehensive analysis of seafarers’ medical issues that were conducted from medical records of patients assisted on board ships by the International Radio Medical Center (C.I.R.M.), Italy. Data mining techniques are involved to manage epidemiological data analysis in a two-phase setup. In the first phase, the common pathologies that occurred onboard were analyzed, later a detailed questionnaire for each medical problem was developed to provide precise symptomatic information to the onshore doctor. In this paper, we mainly highlighted the SHES framework, design flow, and functionality. Besides, nine designing policies and three actors with separate working panels were clearly described. The proposed system is easy and simple to operate for anyone of no computer experience and create medical requests for the fast delivery of symptomatic information to an onshore doctor.
Keywords: Seafarer’s health, C.I.R.M, design frameworks, web servers, firewall
Introduction
About two million seafarers are working in 50,000 merchant ships and carrying 90% of global merchandise. Seafaring is a kind of occupational group that is more vulnerable to safety and personal health issues.1 These people are largely connected with severe health risks mainly caused because of isolation, climatic changes, and heavy workload. Accidents onboard are also common during material shipping.1,2 Despite ecological factors, disturbance and ship vibrations are also effects working quality and rest progression.3 Other medical problems such as musculoskeletal strain, clamor, and exhaustion make them high work pressure.4 Ship sailing involved continuous working hours, and spend long periods away from the coastal life.5
Seafarers have come across a proper medical check-up before they entering into a vessel, but because of anomalies in marine life, there is always a constant risk of getting sick or to experience injuries. In this case, the lack of health professionals onboard makes the situation even worse. By staying away from home initiate sadness and isolation in seafarers.6 Seafarers need a better companion at work and recommend developing habits of having a conversation with colleagues, maintain a healthy diet, and always engaged in positive activities like sports, listen to music, also reading could relieve them excessive stress.7
The studies related to seafarer’s health had concluded all sailing works could not be substantial. The better information on associated risk factors from well-conducted studies could explore the seafarer's medical problems.8–10 Also, it is beyond the expectation to diagnose disease with limited symptomatic information, and shipping staff usually approach ship pharmacy for simple medical problems. In case of emergency, the ship’s captain can seek medical advice from a Telemedical Maritime Assistance Service (TMAS) centers.11 But there is a constant risk for transferring true medical evidence just only through telephone or electronic mails. In such cases, proper use of modern telecommunications and remote medical care technologies could help in favor of seafarer’s health issues.
Shipping is an individual working environment of primary features like age, lifestyle, body mass index (BMI), and physical activities.12 When compared to onshore residents, seafarers had more rights for medical care and health safety.13 But, the possibility of having better onboard medical assistance in case of serious pathologies has been becoming a challenge for ages.14 The unavailability of medical doctors, limited medical supplies for ship pharmacy represent relevant obstacles in providing reasonable quality medical care to seafarers.15,16 Recent technical advancements if properly used could offer the chances for the development of seafarer’s medical systems. In this frame we have developed a seafarer's health expert system (SHES) to help seafarers to generate quality telemedicine services.17 It can bring a significant advantage in the case of onboard diseases or injuries and allows remote doctors in better pathology assessment.
There is a constant advantage for expert systems and the internet of things (IoT) in particular. Expert systems help solve complex problems with human knowledge, and these systems can represent the human intelligence or commands of machine language.18 On the other hand, a person who is in charge of the healthcare onboard had limited medical knowledge and provide nominal medical support.19 Sometimes, symptomatic information of pathology could hinder by lack of medical expertise to ship captain or medical officers. In such a condition, the TMAS doctor cannot identify the exact medical condition of the seafarer. By digital healthcare equipment like SHES, an onshore doctor can access patient data without a problem. This paper explains the idea behind SHES development, working functionality, and architecture principles in the provision of medical help to seafarers from a remote area.
SHES guidelines and principles
Patient records
Seafarer's medical records were extracted from the clinical database of the International Radio Medical Center (C.I.R.M).20 C.I.R.M. is the Italian TMAS and represents the maritime assistance center with the largest experience worldwide in providing medical assistance to sailing seafarers. The clinical data of ship workers were securely stored with limited access for authorized people. C.I.R.M. is maintaining these records for 20 years with good maintenance and encryption. The clinical data of ship workers were securely stored with limited access for authorized people. C.I.R.M is maintaining these records for 20 years with good maintenance and encryption.
SHES principles and policies
A review of medical records was properly executed to categorize diagnostic characteristics, and problem statements. Each record has been investigated in the two-step methods. At first, simulation of common seafarers' medical problems was done by adopting text mining techniques. Text mining is a type of Natural Language Processing (NLP) technique that performs the linguistic analysis.21 Long sentences in patient records are breaks down into understandable words for structural medical description and were evaluated by the tokenization method.21 We identified 52 medical issues including 35 diseases and 17 accidents type (Table 1). Secondly, depending on individual pathology, a specific questionnaire item has developed for each disease. Identification of individual pathology integrated with symptomatic data further studied. Table 2 presents nine SHES principles accompanied by its guidelines and outcomes.
Table 1.
Onboard medical issues.
| Type | Category |
|---|---|
| Diseases | 1.Fever, 2.Dizziness (Seasickness), 3.Fainting, 4.Anxiety (Panic crisis), 5.Aggressiveness (Hallucinations), 6.Tachycardia, 7.Cough, 8.Breathing difficulties, 9.Nausea (Vomit), 10.Constipation, 11.Diarrhea, 12.Black colored feces, 13.Diarrhea, 14.Red blood in the feces, 15.Hematuria (blood in the urine) or Dysuria (urinating difficulties), 16.Lesions (abnormal secretions of the genitals), 17.Skin lesion (cutis), 18.Swelling (tumefaction), 19.Eyes pain or reddening (not caused by a traumatism or an accident), 20.Sight problems, 21.Pregnancy in women, 22.Breathlessness in a child, 23.Cough in a child, 24. Vomit in a child, 25.Diarrhea in a child, 26.Headache, 27.Earache, 28.Toothache and lesions of the mouth, 29.Sore throat/hoarse voice, 30.Neck pain or swelling, 31.Pain in the arm, 32.Chest pain, 33.Lumbar pain, 34.Abdominal pain, 35.Leg pain |
| Accidents | 1. General accidents, 2. Traumatism (Head/face/nose), 3.Traumatism of the eye, 4. Neck traumatism, chest traumatism, 5. Traumatism in the hip (lumbar region), 6. Traumatism of the shoulder (upper limb), 7. Traumatism of the wrist or hand,8. Traumatism of the lower limb,9. Toxic gas (Vapors/Fumes), 10. Unsafe food/drinks, 11. Medicines or drug overdose, 12. Burns caused by fire(heat/radiation), 13. Electrocution injury caused by electricity, 14. Sunstroke (Heat gust), 15. Prolonged exposure to the cold, 16. Drowning, 17. Scuba diving accident |
Table 2.
System designing principles along with guidelines.
| Functionality | Principle | Guidelines | Outcomes |
|---|---|---|---|
| Services | 1. Service-oriented system | The designed system should be compiled with the requirements of seafarers’ health | SHES should be ready to display all the symptoms associated with the primary diseases |
| 2. User benefits | Seafarers could easily access the system | The system should be compatible with user requirements | |
| 3. Integration | The system could easily integrate with user requirements | All web or desktop applications will compile with a secure application programmable interface (API). In general, API documentation provides usage and implementation characteristics | |
| Database | 4. Collection | All the data that register in the CIRM database were adequately collected and analyzed | The data analysis needs to be done in system implementation |
| 5. Integration | Data integration is the crucial step to transfer the data into meaningful or understandable information | Data integration improves decision making, improve customer expertise and streamline the operations | |
| 6. Access | Easy access in data enables seafarers to make better decisions | It will help make better and quick decisions in SHES | |
| 7. Security | All the medical records stored in SHES protected by European GDPR | SHES could manage security risk, and provide excellent data governance | |
| Application | 8. Usability | The system should be used to every seafarer despite educational background and computational knowledge | The SHES must implement an interface that allows usability function |
| 9. Flexibility | The SHES must be flexible to store any health records | The SHES could be a ready update to itself if any changes are required in future |
CIRM: Center of International Radio Medicine; GDPR: general data protection regulation
SHES designing and functionality
Designing flow
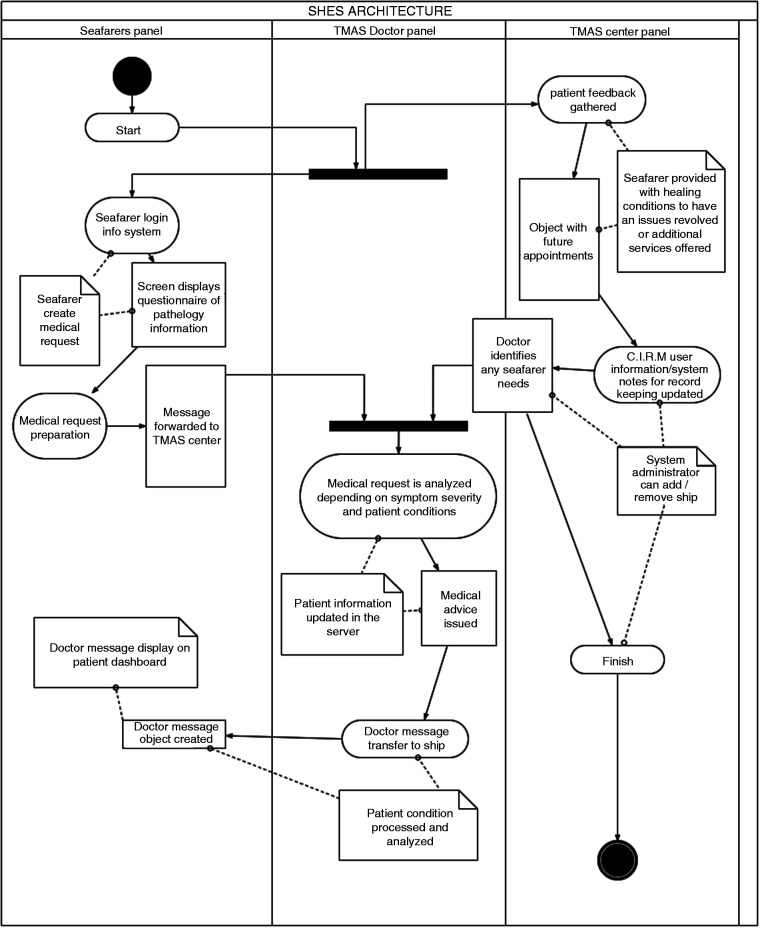
Design flow provides ideas behind system design in a documented manner.22 Figure 1 illustrates the SHES design flow with three individual panels and its functionalities. In the seafarers’ panel, the onboard healthcare staff operates SHES with predefined credentials for generating new medical requests. After adding seafarer’s details like gender, age, nationality, blood pressure, pulse rate, BMI, etc. In the follow-up screen, it asks to select a medical problem from the list defined in Table 1. Thereafter the system presents a new screen with a symptomatic questionnaire of a selected category. The collective response of each questionnaire is directly transmitted to a doctor panel called ‘medical flag’.
Figure 1.
SHES design flow.
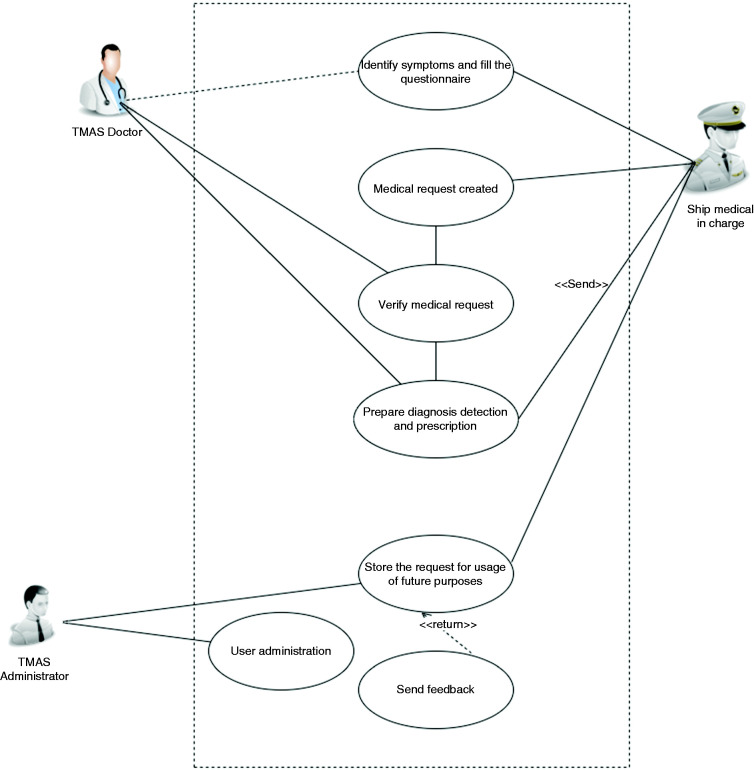
TMAS doctor panel assesses the medical flag. Subsequent analysis of seafarers' requests and specialists delivers responses including diagnostic and drug information, treatment measures, and immediate precautions that have to follow onboard. The Administrative (TMAS center) panel is update medical flag status and keeps active in the system until the seafarer completely recovers. The use diagram of three SHES actors including duties is presented in Figure 2.
Figure 2.
SHES use-case diagram.
Technical design
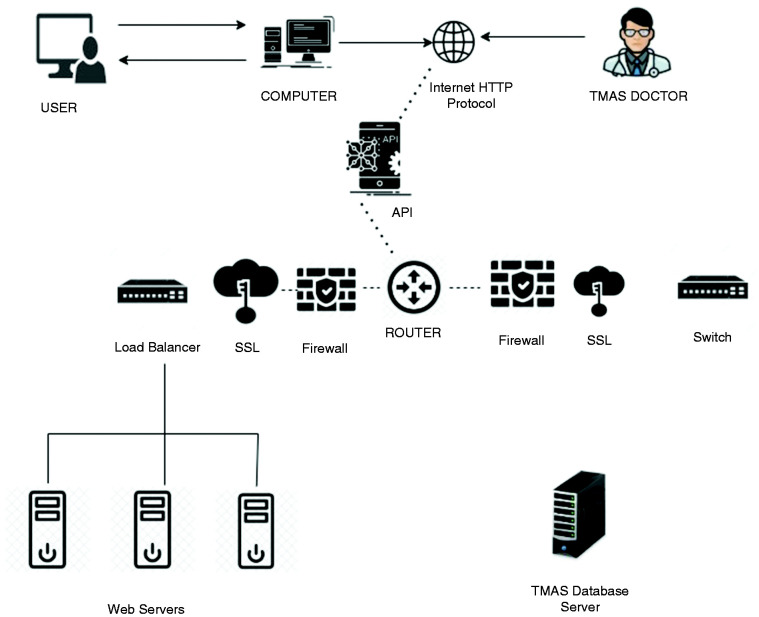
The SHES is a centralized application that all users can utilize the system through a centralized server. Technical design defines the adaptation of application principles and characteristics (Table 2) to an organized solution that meets user standards. Front end-user interface (UI) elements enable seafarers to create a medical flag. This flag carries and stores symptomatic information to the webserver and the SHES desktop screen collects and transfers to the TMAS doctor. A load balancer is introduced among these WEB servers in the distribution of workloads and enhance the system performance (Figure 3). Two main servers (i.e., WEB and TMAS) are included to manage the patient requests, and application programmable interface (API) directs the server access, collects and delivers responses.23 The SHES accessing via the internet with a secure sockets layer (SSL) implementation, and firewall for data protection between systems are introduced. Two network firewalls were imposed to have system security from unauthorized access and private network usage. Authentication for each user can be provided by the system administrator.
Figure 3.
SHES technical architecture model.
Discussion
When a seafarer gets sick, communication between doctor and patient can be done either by phone or email. Sometimes, it is hard to evaluate the actual patient situation with limited clinical information. Therefore, the demand for telemedical services is encouraged by the possibility of creating a new medical expert system.24 In this paper, we proposed a design of SHES that can create a better improvement of seafarers' health, and this system is designed for the goal of providing long term health services. The SHES is a software application for easy management of telemedical services to crew members with limited medical knowledge. As mentioned, onboard staff possess limited medical knowledge and the medical capabilities of these people are modest. Therefore, the SHES application can explore the possibility of providing onboard medical care.
The SHES architecture was designed after careful understanding of C.I.R.M medical records of seafarers and developed with individual strategies, principles, and guidelines. All clinical records were properly analyzed and onboard medical problems are labeled into two distinct categories such as diseases and accidents. Every medical problem is predefined by a specific set of questions that aims to deliver symptomatic information to the TMAS doctor. Nine separate principles are defined on service, database, and application functionalities. The SHES design flow consists of three panels namely ship, doctor, and TMAS center panels. The technical architecture is developed with web and TMAS servers. Web servers are incorporated to process the medical flags and TMAS servers are incorporated to securely store the medical requests. We also added two network firewalls to protect SHES from unauthorized access and private networks.
Conclusions
Since the beginning of the 21st century, developments in IoT technologies encourage the development of new medical systems. This paper presents the introduction of SHES development that aims to deliver medical services for seafarers onboard. We employed contemporary IoT methods for SHES designing and it could be a primary application in maritime health. The idea behind current development can open new possibilities for future inventions of remote healthcare centers.
Acknowledgments
We would like to acknowledge the support provided by ITF trust (Grant No. 1276/2018).
Footnotes
Contributorship: GB: Study development and manuscript preparation, FA: Critically reviewed and approved the study.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The ethical committee at Center Of International Radio Medicine (C.I.R.M.) has approved the study.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Executive board of the International Transport Workers’ Federation (ITF) supports this project and partly getting support from the International Radio Medical Center (C.I.R.M).
Guarantor: F AMENTA.
Peer Review: This manuscript was reviewed by reviewers who have chosen to remain anonymous.
ORCID iD: Gopi Battineni https://orcid.org/0000-0003-0603-2356
References
- 1.Bhattacharya Y. Measuring safety culture on ships using safety climate: a study among Indian officers. Int J e-Navigation Marit Econ 2015; 3. doi:10.1016/j.enavi.2015.12.006
- 2.Hystad SW, Eid J. Sleep and fatigue among seafarers: the role of environmental stressors, duration at sea and psychological Capital. Saf health work 2016; 7: 363–371. doi:10.1016/j.shaw.2016.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim JH, Jang SN. Seafarers’ quality of life: organizational culture, self-efficacy, and perceived fatigue. Int J Environ Res Public Health 2018; 15: 2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sau A and Bhakta I. Screening of anxiety and depression among the seafarers using machine learning technology. Informatics in Medicine Unlocked 2019; 16: 100149. doi:10.1016/j.imu.2018.12.004
- 5.Carotenuto A, Molino I, Fasanaro AM, et al. Psychological stress in seafarers: a review. Int Marit Health 2012; 63: 188–194. [PubMed] [Google Scholar]
- 6.Lefkowitz RY, Slade MD and Redlich CA. Rates and occupational characteristics of international seafarers with mental illness. Occupational Medicine 2019; 69: 279–282. 10.1093/occmed/kqz069 [DOI] [PubMed]
- 7.Iversen RT. The mental health of seafarers. Int Marit Health 2012; 63: 78–89. [PubMed]
- 8.Tu M, Jepsen JR. Hypertension among Danish seafarers. Int Marit Health 2016; 67: 196–204. doi: 10.5603/IMH.2016.0037 [DOI] [PubMed]
- 9.Grappasonni I, Petrelli F, Amenta F. Deaths on board ships assisted by the centro internazionale radio medico in the last 25 years. Travel Med Infect Dis 2012; 10: 186–191. doi:10.1016/j.tmaid.2012.06.006 [DOI] [PubMed] [Google Scholar]
- 10.Jepsen JR, Zhao Z, van Leeuwen WM. Seafarer fatigue: a review of risk factors, consequences for seafarers’ health and safety and options for mitigation. Int Marit Health 2015; 66: 106–117. doi:10.5603/IMH.2015.0024 [DOI] [PubMed] [Google Scholar]
- 11.Westlund K, Attvall S, Nilsson R, et al. Telemedical Maritime assistance service (TMAS) to Swedish merchant and passengers ships 1997-2012. Int Marit Health 2016; 67: 24–30. doi:10.5603/IMH.2016.0006 [DOI] [PubMed] [Google Scholar]
- 12.Battineni G, Di Canio M, Chintalapudi N, et al. G. Development of physical training smartphone application to maintain fitness levels in seafarers. Int Marit Health 2019; 70: 180–186. doi:10.5603/IMH.2019.0028 [DOI] [PubMed] [Google Scholar]
- 13.Nittari G, Pallotta G, Battineni Get al. Comparative analysis of the medicinal compounds of the ship's “medicine chests” in European Union maritime countries. Need for improvement and harmonization. Int Marit Health 2019; 70: 143--150. doi:10.5603/IMH.2019.0023 [DOI] [PubMed] [Google Scholar]
- 14.Ricci G, Pirillo I, Rinuncini C, et al. Medical assistance at the sea: legal and medico-legal problems. Int Marit Health 2014; 65: 205–209. doi:10.5603/IMH.2014.0039 [DOI] [PubMed] [Google Scholar]
- 15.Nittari G, Arcese A, Battineni Get al. Design and evolution of the Seafarer's Health Passport for supporting (tele)-medical assistance to seafarers. Int Marit Health 2019; 70: 151--157. doi:10.5603/IMH.2019.0024 [DOI] [PubMed] [Google Scholar]
- 16.Amenta F, Dauri A, Rizzo N. Telemedicine and medical care to ships without a doctor on board. J Telemed Telecare 1998; 4: 44–45. [DOI] [PubMed] [Google Scholar]
- 17.Nittari G, Khuman R, Baldoni S, et al. Telemedicine practice: review of the current ethical and legal challenges. Telemed e-Health. Epub ahead of print 12 February 2020. doi:10.1089/tmj.2019.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biles JA. Building expert systems. In: Proceedings of the IEEE, vol. 73, no. 2, February 1985, pp. 383–383. doi: 10.1109/PROC.1985.13159 [Google Scholar]
- 19.Li GQ. Research on seafarer physical and psychological evaluation model and physical activity intervention measures. Inf Technol J 2013; 12: 7821–7826. doi:10.3923/itj.2013.7821.7826 [Google Scholar]
- 20.Mahdi SS, Amenta F. Eighty years of CIRM. A journey of commitment and dedication in providing Maritime medical assistance. Int Marit Health 2016; 67: 187–195. doi:10.5603/IMH.2016.0036 [DOI] [PubMed] [Google Scholar]
- 21.Collobert R, Weston J, Bottou L, et al. Natural language processing (almost) from scratch. J Mach Learn Res 2011; 12: 2493–2537. [Google Scholar]
- 22.Sahm H, Sauppe M, Markert E, et al. Optimized ASIC/FPGA design flow for energy efficient network nodes. Bell Labs Tech J 2013; 18: 195–209, doi: 10.1002/bltj.21634
- 23.Ofoeda J, et al. Application Programming Interface (API) Research: A Review of the Past to Inform the Future. Int J Enterp Inf Syst 2019; 15: 76–95.
- 24.Tedesco LMR, Ferrara P, Stromillo L, et al. Seafarers’ perceptions of job demand: a cross-sectional study. Arch Environ Occup Heal 2018; 73: 278–283. doi:10.1080/19338244.2017.1342590 [DOI] [PubMed] [Google Scholar]