Transcatheter aortic valve replacement (TAVR) is an established alternative to surgical aortic valve replacement (SAVR) for patients with severe aortic stenosis [1,2]. While TAVR usage has increased greatly, the clinical impact and outcomes of surgical TAVR valve explantation and SAVR (TAVR-explant) are not well understood [3]. Despite the feasibility of a repeat TAVR procedure, there has been an increasing need for TAVR-explant as the number of TAVR implants has increased. There are reports of TAVR valves causing neoendothelialization between the device and contacting native tissue (Figure 1A and 1B), making device explantation a more morbid procedure than originally thought [3]. The difficulty of SAVR after TAVR may be another consideration for the initial choice of TAVR versus SAVR in younger patients. This study was undertaken to review registry TAVR-explant data in order to better understand the challenges and outcomes of surgical TAVR-explant procedures.
Figure 1.
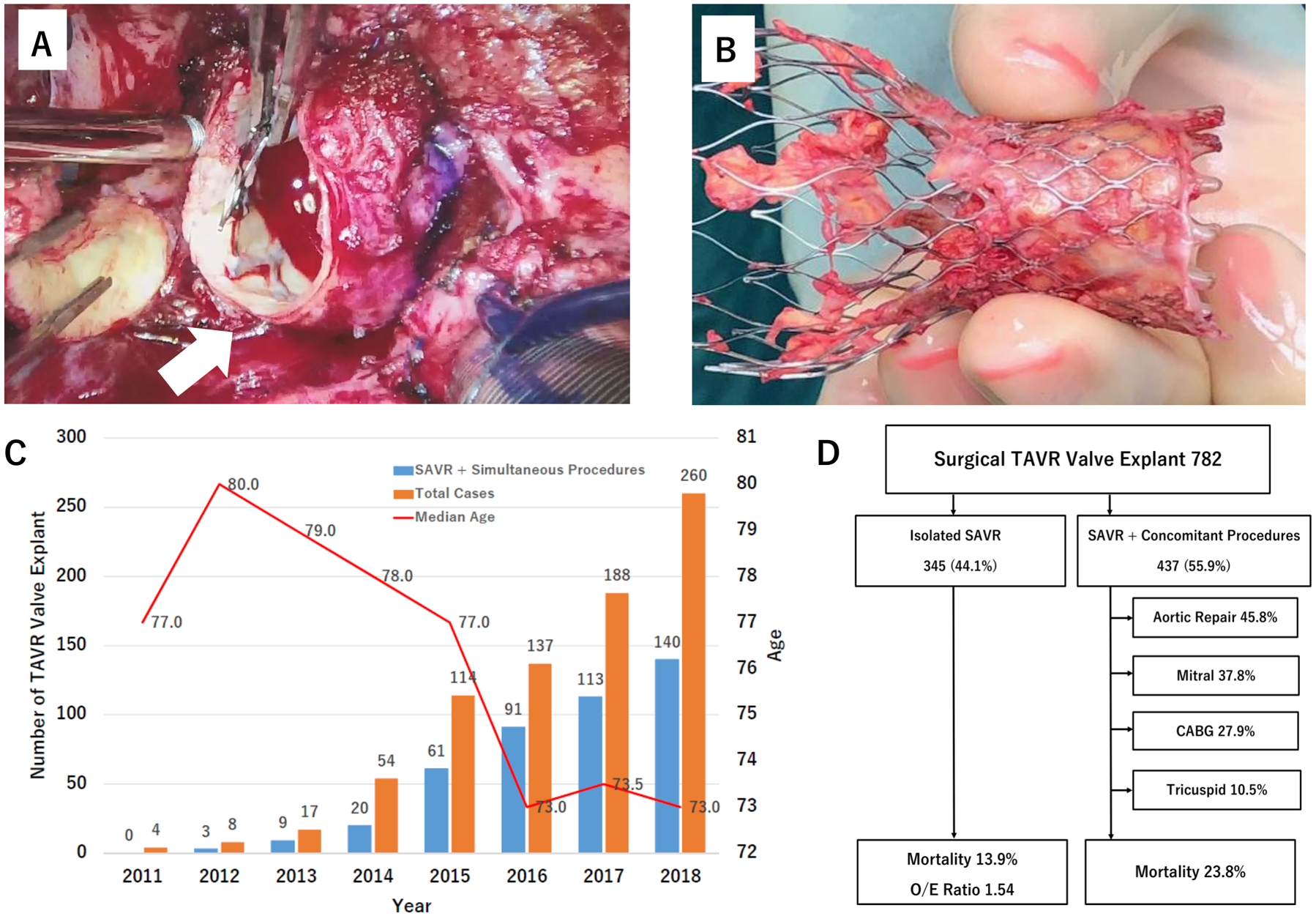
Summary of the present investigation. (A) Trend of surgical transcatheter aortic prosthesis explant total case number (orange bar), case number with simultaneous procedures (blue bar) and patient median age (red line) by year. (B) Overview of the study cohort, the frequency of simultaneous other procedures and clinical outcomes. (C) Intraoperative photograph representing distinct technical challenges of surgical transcatheter bioprosthesis explant. Neoendothelialization formed between the sinotubular junction and self-expandable device (arrow). (D) Explanted self-expandable transcatheter bioprosthesis with denuded aortic intima remnants attached to the stent cage.
This study was approved by the Society of Thoracic Surgeons (STS) and the University of Michigan institutional review board. The data were provided by STS National Database Participant User File Research program. The data are available from the corresponding author upon reasonable request. TAVR-explant was defined as a non-same-day surgical TAVR valve explant with SAVR performed in post-TAVR patients. Between 2011 and 2018, 782 patients with TAVR-explant were identified. The STS predicted risk of mortality (STS-PROM) score was available in patients with isolated SAVR. Where available, the observed-to-expected 30-day mortality ratio (O/E ratio) is reported.
These TAVR-explant procedures were performed by 483 surgeons (median 1.0 case per surgeon [interquartile range (IQR) 1.0–2.0]) from 313 centers (median 1.0 case per center [IQR 1.0–3.0]) across the nation. Figure 1C shows the annual number of patients with TAVR-explant with/without simultaneous cardiac procedures. The case number increased over time from 4 in 2011 to 260 in 2018. The annual number of patients requiring simultaneous other procedures also increased each year. The median age was 74.0 (IQR 67.0–81.0) which trended down over the study period from 80.0 (IQR 70.8–87.0) to 73.0 (IQR 66.3–80.0). Thirty-nine percent were female and 55.1% demonstrated NYHA class III-IV symptoms. Additionally, more than 60% had previous cardiac surgeries. The leading indication for TAVR-explant was failed repair/positioning/sizing issue (27%) followed by aortic insufficiency/paravalvular leak (21.5%), stenosis (20.2%), endocarditis (17.7%) and structural valve degeneration (6.5%).
Among those with simultaneous procedures (n=437; 55.9%), aortic repair was the most frequent procedure (n=200; 45.8%), which comprises aortic root (76.0%) and/or ascending aortic replacement (48.5%). Mitral procedure was the second most common (n=165; 37.8%) followed by coronary artery bypass grafting (CABG) (n=122; 27.9%), tricuspid procedure (n=46; 10.5%) (Figure 1D) and ventricular septal defect (VSD) repair (n=20; 4.6%). A quarter of the patients received two or more additional procedures. The overall 30-day mortality was 19.4%. The 30-day mortality in patients with isolated SAVR versus SAVR with simultaneous procedure was 14.8 and 23.8% (p=0.002), respectively. Of the 283 patients with isolated SAVR with available STS-PROM, the mortality was 13.1% and the O/E ratio was 1.54. Additionally, patients with simultaneous procedures demonstrated a higher hospital readmission (18.3 vs. 11.1%; p=0.011), more frequent prolonged mechanical ventilation (43.3 vs. 29.9%; p< 0.001), postoperative sepsis (6.6 vs. 2.6; p=0.009) and blood transfusions. Among patients with simultaneous procedures, the mortality in those with aortic repair was the worst (28.5%). Aortic repair was performed across all indications despite being non-aortic indications. Stenosis and structural valve degeneration were the two leading indications which had more than 50% of the aortic repair rates. Furthermore, a subgroup analysis among the 395 patients with documented explanted TAVR valve type, comprised 80.5% balloon expandable and 19.5% self-expandable devices, showed a comparable mortality (20.8% vs, 19.8%; p=0.85). Patients with a self-expandable device underwent more frequent ascending aortic replacement than those with a balloon-expandable device (18.2 vs. 8.2%; p=0.009), whereas the aortic root replacement rate was similar (22.1 vs. 18.9%; p=0.52). Ascending aortic repair alone was rare (2.8%) in the balloon-expandable group.
This study represents the largest series describing TAVR-explant using a national database to provide insight into the incidence and clinical implications of TAVR-explants. The primary findings include the frequent combined cardiac procedure rate and high mortality along with the high O/E ratios for TAVR explants. A major limitation is the lack of the actual number of TAVR implants, or denominator, for these reported TAVR-explant procedures. Based on the STS/American College of Cardiology (ACC) Transcatheter Valve Therapy (TVT) data, the incidence of TAVR-explant is estimated approximately 0.4% (782/200,000 TAVR procedures between 2011 and 2018 [4,5]). Other limitations include the absence of clarity regarding interval after TAVR and, precise indications for the TAVR-explant. As the role of TAVR continues to expand in the treatment of lower risk patients, an increase in TAVR-explant procedures are expected in the next decade. Optimal management of patients requiring TAVR-explant may require treatment in high volume aortic surgery centers.
Acknowledgements
The data for this research were provided by The Society of Thoracic Surgeons’ National Database Participant User File Research Program. Data analysis was performed at the investigators’ institution. We would like to thank Dr. Robert Habib, Director of the STS Research Center, and Ms. Kristin Mathis, senior coordinator of STS Research Center, for their great support for the data acquisition and organization for the present investigation.
Glossary
- TAVR
transcatheter aortic valve replacement
- SAVR
surgical aortic valve replacement
- O/E
observed-to-expected
Footnotes
Disclosures:
Dr. Fukuhara serves as a consultant and research investigator for Terumo Aortic. Dr. Deeb serves on an advisory board and as a proctor for Medtronic; as a consultant and research investigator for Edwards Lifesciences; as a consultant and proctor for Terumo; and as a research investigator for Gore Medical with all fees paid to his institution. Dr. Brescia is supported by the National Research Service Award postdoctoral fellowship (No. 5T32HL076123).
References
- 1.Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, Kapadia SR, Malaisrie SC, Cohen DJ, Pibarot P, Leipsic J, Hahn RT, Blanke P, et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med. 2019;380:1695–1705. [DOI] [PubMed] [Google Scholar]
- 2.Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D, Bajwa T, Heiser JC, Merhi W, Kleiman NS, Askew J, Sorajja P, Rovin J, et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med. 2019;380:1706–1715. [DOI] [PubMed] [Google Scholar]
- 3.Fukuhara S, Brescia AA, Shiomi S, Rosati CM, Yang B, Kim KM, Deeb GM. Surgical explantation of transcatheter aortic bioprostheses: Results and clinical implications. J Thorac Cardiovasc Surg. 2020. January 12;S0022-5223(20)30061-1. doi: 10.1016/j.jtcvs.2019.11.139. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huded CP, Tuzcu EM, Krishnaswamy A, Mick SL, Kleiman NS, Svensson LG, Carroll J, Thourani VH, Kirtane AJ, Manandhar P, et al. Association Between Transcatheter Aortic Valve Replacement and Early Postprocedural Stroke. JAMA. 2019;321:2306–2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bavaria JE. TAVR Update: New Insights and Perspectives from the US National STS/ACC TVT Registry. Society of Thoracic Surgeons. https://www.sts.org/sites/default/files/102419%201645.%20Bavaria.%20TVT.pdf (Accessed March 23, 2020)


