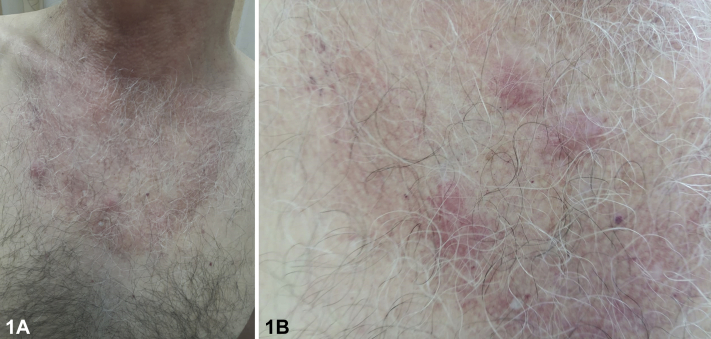
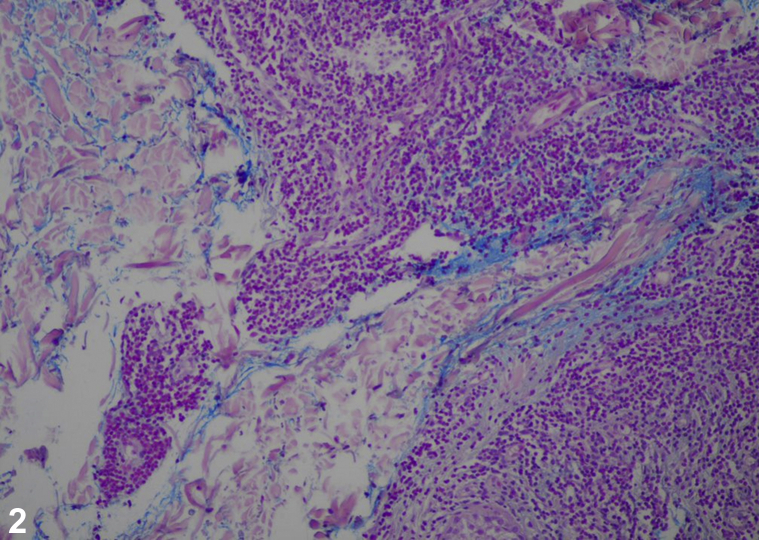
A 40-year-old man with no significant medical history presented with a 10-year relapsing and remitting rash. The lesions were pruritic, painless, pink papules and plaques on his chest in a netlike configuration (Fig 1, A and B), which were exacerbated by sunlight exposure, without a family history of similar cutaneous lesions. Physical examination was unremarkable and ancillary testing included complete blood count; basic metabolic panel; viral serology for HIV, hepatitis B virus, and hepatitis C virus; and chest X-ray, all of which were within normal limits. Autoantibody tests for antinuclear antibodies, antibodies to double-stranded DNA, and autoantibodies against Ro/SSA, La/SSB, and Smith antigen were negative. The application of high-potency topical corticosteroids resulted in minimal therapeutic response. A biopsy was performed for histopathologic analysis (Fig 2, mucin stain).
Fig 1.
Fig 2.
Question 1: Considering the clinical, laboratory, and histopathologic images, what is the most likely diagnosis?
-
A.
Discoid lupus erythematous
-
B.
Polymorphous light eruption (PMLE)
-
C.
Reticular erythematous mucinosis (REM)
-
D.
Seborrheic dermatitis
-
E.
Lupus erythematosus (LE)
Answer:
-
A.
Discoid lupus erythematous—Incorrect. Clinically, discoid lupus erythematous consists of erythematous plaques with an adherent scale, evolving into atrophy, scarring, and pigmentary changes. Mucin deposits might appear in the dermis. Histopathologically, the involvement of the epidermis and deposits of IgG and C3 at the dermoepidermal junction are noted.
-
B.
PMLE—Incorrect. Although a photo-aggravated dermatitis, PMLE is more diverse morphologically and resolves once the exposure to sunlight has ceased, unlike the present case. Histopathologically, a perivascular lymphocytic infiltrate and papillary dermal edema are the hallmarks of the disease without any mucin deposition in the papillary dermis.
-
C.
REM—Correct. REM is a rare chronic disorder of dermal mucin accumulation,1 exacerbated by sun exposure. It predominantly affects the chest and upper portion of the back in a reticulated pattern of lesions. Histologically, a perivascular lymphohistiocytic infiltrate is noted and mucin is vastly present in the papillary dermis.
-
D.
Seborrheic dermatitis—Incorrect. Fine scales are present on the sebaceous areas of the face and anterior aspect of the chest. No involvement of seborrheic areas such as the scalp, eyebrows, eyelids, and nasolabial creases was noted in this case.
-
E.
LE—Incorrect. Cutaneous lupus is characterized by erythematous papules, nodules, and plaques, often involving V of the neck and the upper portion of the back. Serologic tests for LE were negative. Histopathologically, epidermal changes or fibrinoid necrosis at the dermoepidermal junction with liquefactive degeneration and atrophy of epidermis were not found. The tumidus subtype variant of lupus has affinity for the neck and face and presents with erythematous plaques. However, lupus tumidus lesions are strongly photosensitive, do not display reticulate midline lesions, and could potentially have additional lupus features. Lupus tumidus cannot be differentiated from REM based solely on pathology, with its mucin deposits in the papillary dermis.2
Question 2: Which of the following statements is characteristic for REM?
-
A.
Reports of possible association with internal malignancy and thyroid disease
-
B.
Association with PMLE
-
C.
Systemic steroids are the treatment of choice
-
D.
No age or gender predominance
-
E.
Epidermal atrophy
Answer:
-
A.
Reports of possible association with internal malignancy and thyroid disease—Correct. In general, REM is not related to systemic diseases but the reports of a potential association have been documented.3 In particular, concomitant autoimmune disease, thyroid disease (Hashimoto disease and hyperthyroidism), and malignancies of the lung, breast, and colon have been reported.
-
B.
Association with PMLE—Incorrect. Associations of PMLE and REM have not been reported. However, REM might be associated with LE.4
-
C.
Systemic steroids are the treatment of choice—Incorrect. Antimalarial agents are considered the first-line therapy for REM and have been associated with the improvement of skin lesions within 4-8 weeks.5
-
D.
No age or gender predominance—Incorrect. There is a female predominance of REM, which favors women in the third and fourth decades of life.
-
E.
Epidermal atrophy—Incorrect. The epidermis is normal. In our patient's biopsy, there were 2 cardinal histologic features: interstitial deposits of small amounts of mucin in the papillary dermis and a mononuclear infiltrate situated predominantly around blood vessels and hair follicles that consisted of T-cell infiltrate.
Question 3: Which of the following special stains will be used to identify mucin deposition in the skin?
-
A.
Masson trichrome
-
B.
Prussian blue
-
C.
Gomori trichrome
-
D.
Alcian blue
-
E.
Grocott methenamine silver stain
Answer:
-
A.
Masson trichrome—Incorrect. This stain characterizes muscle and soft tissue components, staining the collagen fibers in blue. It distinguishes leiomyomas from dermatofibromas and neural tumors. Perivascular fibrosis, scar formation, and sclerotic lesions are also diagnosed with this special stain.
-
B.
Prussian blue—Incorrect. It is used for the identification of iron as a source of pigment. Ferric ions react to form a deep blue color. This helps to distinguish melanin from hemosiderin.
-
C.
Gomori trichrome—Incorrect. It is intended to identify an increase in collagen fibers in the muscle tissue and can be used to test for certain forms of mitochondrial myopathy.
-
D.
Alcian blue—Correct. Mucin, a mixture of acid mucopolysaccharides (glycosaminoglycans), is a component of the dermal extracellular matrix and is normally produced by fibroblasts. The presence of either a blue-staining material between separated collagen bundles or void spaces within the dermis suggests mucin deposition. The stain molecules carry a positive charge and are attracted to the negative acid mucins. Adjustments for pH of the Alcian blue solution allow the demonstration of different types of acid mucins: nonsulfated acid mucopolysaccharides stain with Alcian blue at pH 2.5 but not at pH 0.5. Other mucin special stains used in common practice are colloidal iron and toluidine blue. Dermal mucin is periodic acid–Schiff negative.
-
E.
Grocott methenamine silver stain—Incorrect. It is used widely to screen for fungal organisms by identifying carbohydrates in fungal microorganisms. The cell walls of these organisms are outlined by brown to black stain. In addition, it is useful for staining Pneumocystis jiroveci.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
IRB approval status: Not applicable.
References
- 1.Thareja S., Paghdal K., Lien M.H., Fenske N.A. Reticular erythematous mucinosis-a review. Int J Dermatol. 2012;51(8):903–909. doi: 10.1111/j.1365-4632.2011.05292.x. [DOI] [PubMed] [Google Scholar]
- 2.Patsinakidis N., Kautz O., Gibbs B.F., Raap U. Lupus erythematosus tumidus: clinical perspectives. Clin Cosmet Investig Dermatol. 2019;12:707–719. doi: 10.2147/CCID.S166723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rongioletti F., Merlo V., Riva S. Reticular erythematous mucinosis: a review of patients' characteristics, associated conditions, therapy and outcome in 25 cases. Br J Dermatol. 2013;169(6):1207–1211. doi: 10.1111/bjd.12577. [DOI] [PubMed] [Google Scholar]
- 4.Sidwell R.U., Francis N., Bunker C.B. Hormonal influence on reticular erythematous mucinosis. Br J Dermatol. 2001;144(3):633–634. doi: 10.1046/j.1365-2133.2001.04105.x. [DOI] [PubMed] [Google Scholar]
- 5.Woollons A., Darley C.R. Erythematous rash on the chest. Arch Dermatol. 2002;138(9):1245–1250. doi: 10.1001/archderm.138.9.1245-c. [DOI] [PubMed] [Google Scholar]