Introduction
Granuloma annulare (GA) is a chronic, inflammatory granulomatous disease of unknown etiology that can be therapeutically challenging. Based on preclinical studies and success of the tumor necrosis factor alpha (TNF-α) inhibitor class, GA has been thought to be primarily a helper T cell type 1 (Th1) immune-mediated disease.1 Yet, there are patients who do not respond to TNF-α inhibitors, and paradoxical cases of GA have also been reported, suggesting that an alternate pathway may be implicated in certain individuals.2 Min et al recently showed that in lesional GA skin, a wide array of inflammatory markers is expressed.3 While Th1 cytokine levels were expectedly increased, the helper T cell type 2 (Th2) axis was surprisingly overly expressed as well. Dupilumab is a monoclonal antibody that binds to the alpha subunit of interleukin 4 (IL-4) receptor. Through blockade of IL-4Rα, dupilumab modulates signaling of IL-4 and IL-13, both of which are key cytokines in the Th2 pathway. Herein, we report a patient with generalized GA that was refractory to adalimumab treatment who showed dramatic improvement with dupilumab.
Case report
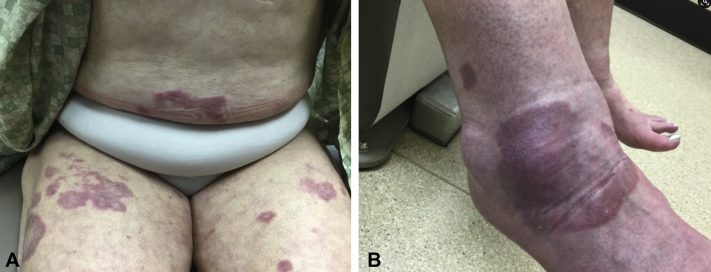
A 74-year-old woman with a past medical history of hypertension, hyperlipidemia, and depression presented with a 2-year history of dark-red annular dermal plaques with clearly distinguishable thickening involving the arms, chest, abdomen, and legs (Fig 1). Histopathology was consistent with GA. Previous treatment with ultrapotent topical steroids, oral antibiotics (rifampin, ofloxacin, and minocycline), hydroxychloroquine, methotrexate, niacinamide, allopurinol, and adalimumab had failed. Based on the results of a preclinical study showing that Th2 signaling may play a role in GA, the patient agreed to off-label treatment with dupilumab.3
Fig 1.
GA on the trunk, thighs (A) and right ankle (B) prior to initiating dupilumab. GA, Granuloma annulare.
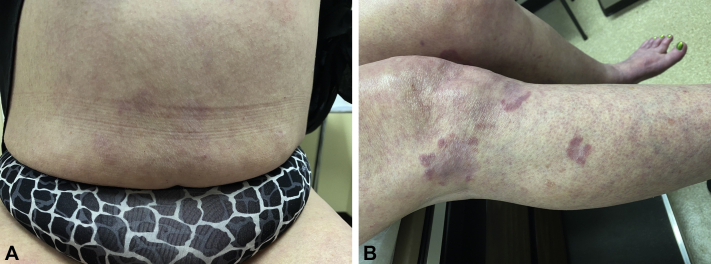
A standard biologic screening was done, which included complete blood count, comprehensive metabolic panel, quantiferon gold, hepatitis B panel, and hepatitis C antibody. A loading dose of 600 mg of dupilumab was administered subcutaneously at week 0 and then decreased to 300 mg every 2 weeks thereafter. At her 4-week follow up, the patient had complete clearance of the plaques on her abdomen, distal shins, and dorsal aspect of the feet (Fig 2). She still had some residual annular dermal plaques on her arms and thighs, but the erythema and induration had significantly improved. At her 12-week follow up, the patient remained clear except for the proximal aspect of her arms and thighs. The patient overall was very satisfied with her improvement and stated that her skin had no-to-minimal impact on her quality of life.
Fig 2.
Complete clearance of GA plaques on abdomen after 4 weeks of dupilumab (A). Residual GA plaques on lower extremities with significant improvement of erythema and induration after 4 weeks of dupilumab (B). GA, Granuloma annulare.
Discussion
Despite our evolving understanding of the pathogenesis of GA, effective treatment has proved to be elusive. Multiple reports of successful treatment with TNF-α inhibitors suggest GA to be, in part, a Th1-mediated process.1,4,5 Paradoxically, there have also been reports of GA induced by infliximab, adalimumab, and etanercept.2 Min et al recently provided evidence that GA may also be driven by other immune pathways, including Th2 and Janus kinase signaling.3
Macrophage polarization has been recognized as an important mediator in GA pathogenesis, with classically activated macrophages contributing to the early development of GA and alternatively activated macrophages contributing to the late development of GA. Classically activated macrophages are characterized by the expression of high levels of proinflammatory cytokines and promotion of a Th1 response. Alternatively activated macrophages are stimulated by Th2 cytokines, such as IL-4, IL-10, and IL-13, and are involved in extracellular matrix remodeling, which is a key feature of GA.6 One can speculate that the response to Th1 or Th2 inhibition will depend on the stage of granuloma formation. Given that our patient had a long history of GA and failed treatment with a TNF-α inhibitor, it would stand to reason that her disease was being driven primarily by Th2 signaling, which would explain her dramatic response to dupilumab. The patient did not have any associated comorbid asthma, atopic dermatitis, or chronic rhinosinusitis, which would have correlated with a positive response to dupilumab.
To our knowledge, this is the first reported case of generalized GA being successfully treated with dupilumab. Further studies need to be done to corroborate our preliminary findings. It would be of interest to know whether inhibition of the Th2 pathway would lead to the same high level of efficacy as seen with TNF-α inhibitors or whether it should be reserved for those in whom more traditional treatment that targets Th1 signaling has failed.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
IRB approval status: Not applicable.
References
- 1.Min M.S., Lebwohl M. Treatment of recalcitrant granuloma annulare (GA) with adalimumab: a single-center, observational study. J Am Acad Dermatol. 2016;74(1):127–133. doi: 10.1016/j.jaad.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 2.Voulgari P.V., Markatseli T.E., Exarchou S.A., Zioga A., Drosos A.A. Granuloma annulare induced by anti-tumour necrosis factor therapy. Ann Rheum Dis. 2008;67(4):567–570. doi: 10.1136/ard.2007.075663. [DOI] [PubMed] [Google Scholar]
- 3.Min M.S., Wu J., He H. Granuloma annulare skin profile shows activation of T-helper cell type 1, T-helper cell type 2, and Janus kinase pathways. J Am Acad Dermatol. 2020;83(1):63–70. doi: 10.1016/j.jaad.2019.12.028. [DOI] [PubMed] [Google Scholar]
- 4.Chen A., Truong A.K., Worswick S. The role of biologics in the treatment of chronic granuloma annulare. Int J Dermatol. 2019;58(5):622–626. doi: 10.1111/ijd.14350. [DOI] [PubMed] [Google Scholar]
- 5.Lukács J., Schliemann S., Elsner P. Treatment of generalized granuloma annulare — a systematic review. J Eur Acad Dermatol Venereol. 2015;29(8):1467–1480. doi: 10.1111/jdv.12976. [DOI] [PubMed] [Google Scholar]
- 6.Asai J. What is new in the histogenesis of granulomatous skin diseases? J Dermatol. 2017;44(3):297–303. doi: 10.1111/1346-8138.13662. [DOI] [PubMed] [Google Scholar]