Background:
In response to the novel coronavirus disease (COVID-19) pandemic, Australia introduced public health and physical distancing restrictions in late March 2020. We investigated the impact of these restrictions on HIV preexposure prophylaxis (PrEP) use among Australian gay and bisexual men (GBM).
Methods:
Participants in an ongoing online cohort study previously reported PrEP use from 2014 to 2019. In April 2020, 847 HIV-negative and untested participants completed questionnaires assessing changes in PrEP use as a result of COVID-19 public health measures. Binary logistic multiple regression was used to estimate adjusted odds ratios (aOR) and 95% confidence intervals (95% CI) to compare changes in PrEP use behaviors.
Results:
Among 847 men, mean age was 44.1 years (SD: 12.7). PrEP use rose from 4.9% in 2015 to 47.2% in 2020. Among those, 41.8% (n = 167) discontinued PrEP use during COVID-19 restrictions. Discontinuing PrEP during COVID-19 restrictions was independently associated with being less likely to have recently tested for HIV (aOR: 0.17; 95% CI: 0.09 to 0.34; P < 0.001) and less likely to report sex with casual partners (aOR: 0.28; 95% CI: 0.14 to 0.54; P < 0.001).
Conclusions:
By April 2020, following the introduction of COVID-19 restrictions, GBM dramatically reduced PrEP use, coinciding with a reduction in sexual activity. Longer-term impacts of COVID-19 restrictions on sexual behaviors among GBM need to be monitored because they may foreshadow fluctuations in prevention coverage and risk of HIV infection. Our findings indicate a potential need for clear, targeted information about resumption of PrEP and on-demand optimal dosing regimens in response to ongoing changes in restrictions.
Key Words: cohort, COVID-19, gay and bisexual men, HIV preexposure prophylaxis, PrEP cessation, PrEP discontinuation
INTRODUCTION
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), which causes the 2019 novel coronavirus disease (COVID-19), was first identified in December 2019.1 Similar to other coronaviruses, COVID-19 is transmissible through close proximity or physical contact with an infected person.2,3 Without effective treatments or vaccines, countries across the globe have implemented preventive measures, to prevent transmission and reduce the burden on health care settings.4 From early March through April 2020, all Australian jurisdictions responded to COVID-19 with a range of public health restrictions.5 These include increased hygiene measures; travel restrictions, border closures and quarantining of people returning from overseas; and physical distancing. Physical distancing measures apply to both individuals and the community, through restrictions on mass gatherings, closure of schools, workplaces, and public spaces and recommendations for keeping at least 1.5 m (5 ft) distance from other people.4
Although restrictions vary between jurisdictions, during “lockdown” periods, people are only permitted to leave their homes for food or essential shopping, to provide care or seek medical treatment, to exercise, or to work or study if not possible from home. They were also required to restrict sexual encounters to established intimate partners.5 Specific messaging for different subpopulations, including gay and bisexual men (GBM), was also developed by community organizations, recommending GBM avoid casual sex.6,7 As restrictions eased in some parts of the country, messaging around sexual activity has expanded to provide guidance to GBM about how to reduce exposure to the risk COVID-19 during sex.8
In Australia, HIV preexposure prophylaxis (PrEP) is subsidized under the Pharmaceutical Benefits Scheme, ensuring that individuals at risk of HIV have affordable access.9 Between 2013 and 2020, PrEP use among HIV-negative GBM increased from 0.9% to 39% in Australia's most populous states.10,11 By June 2019, 26,520 people had been prescribed PrEP in Australia.12 The rapid uptake of PrEP corresponds with the widespread availability of PrEP through state-funded implementation trials.13 Between 2014 and 2019, there was a 23% decline in new HIV infections in Australia, with the most substantial decline observed among GBM.13,14 This decrease corresponded with sustained high rates of HIV testing, sustained high levels of treatment among people diagnosed with HIV, and rapid uptake of PrEP among HIV-negative GBM since 2016.
Recent international data indicate that COVID-19 restrictions have disrupted sexual practices among GBM.15–21 GBM have substantially reduced their sexual contacts with partners other than primary relationship partners.21 For some men, stopping sex with nonprimary partners may obviate the need for PrEP.15,22 Conversely, some GBM may prefer to continue their PrEP use as discontinuation may undermine the habit of pill-taking, the reassurance of being protected from HIV, or inhibit their motivation to reinitiate. Some men also seem to believe that PrEP may offer some protection against COVID-19.16 They may also be unsure about how long COVID-19 restrictions will remain in place and prefer to be prepared for when restrictions are lifted. Given that the impact of the COVID-19 pandemic on PrEP use remains unclear, understanding how COVID-19 public health and physical distancing restrictions affect PrEP use among GBM is critical to ongoing HIV prevention programs.
This article investigates the early impact of COVID-19 restrictions on PrEP use among Australian GBM and assesses implications for ongoing HIV prevention responses.
METHODS
Study Design and Procedures
The Following Lives Undergoing Change (Flux) Study is a national, online, open, prospective, observational study of GBM in Australia, which launched in 2014. A detailed description of the study has been published previously.23 Men were eligible if they were at least 16 years of age, identified as gay or bisexual or had sex with a man in the previous 12 months, and lived in Australia. No compensation was offered for participation.
Study promotion occurred via online advertising through social media, including popular gay dating sites and apps, and Facebook. At enrollment, online informed consent was obtained from all participants. Once enrolled, participants completed online surveys at 6-monthly intervals based on the date of baseline data entry. On April 4, 2020, all participants were invited to complete an optional special survey with questions about the impact of COVID-19; this survey forms the basis of the present analyses. Online informed consent was obtained from all participants who participated in this special survey to link their responses to their responses in previous survey rounds. Ethical approval was granted for this COVID-19–specific survey by the Human Research Ethics Committee of the UNSW Sydney.
Measures
Baseline and 6-monthly follow-up questionnaires were completed online using computer-assisted self-interviewing software.23 Sociodemographic and behavioral items included state of residence, education, employment status, sexual identity, and self-reported HIV status and HIV testing history.
Since 2015, HIV-negative and unknown status men indicated whether they had used PrEP in the previous 6 months and whether they were still using PrEP at the time of their survey. They were also asked if they used PrEP daily, sporadically, or used the on-demand method, which involves taking 2 pills at least 2 hours before sex and 1 pill each day for the 2 days following sex.24,25 Three categories of male sex partners were included: “boyfriends” or “husbands” (a regular committed partner with whom they maintained a romantic relationship), “fuckbuddies” (nonromantic regular partners), and casual partners.26
COVID-19–related items were developed to measure the impact on PrEP use, changes in sexual behavior, and reasons ascribed by participants for these changes. Whereas in previous interviews participants reported on their PrEP use during the previous 6 months, on this occasion, those questions were adapted to focus on PrEP use in the 6 months before the introduction of COVID-19 restrictions in March 2020 (hereafter referred to as “before COVID-19 restrictions”). Participants were then asked about PrEP use following implementation of COVID-19 restrictions (hereafter referred to as “during COVID-19 restrictions”). These comprised the 2 reporting periods described.
Analysis
Data were analyzed using SPSS version 26 software. Only HIV-negative and unknown status participants were included in the analyses. Descriptive statistics were used to characterize men according to their reported changes in PrEP use. Categorical variables were analyzed using the Pearson χ2 test. Continuous variables were analyzed using 1-way analysis of variance. Assumptions of normality were satisfactory as determined by the central limit theory. We used type I error of 5% for these analyses.
In univariate logistic analyses, we assessed age, HIV testing histories, access to PrEP, number of months using PrEP, number of sexual partners, and sexual partner type. We used a type I error rate of 5% for these analyses. All factors with a P value of <0.10 were included in binary logistic simultaneous multiple regression analysis to compare GBM who continued to use PrEP during COVID-19 restrictions with participants who stopped using PrEP, controlling for confounding factors. Results are presented as adjusted odds ratios (aOR) and 95% confidence intervals (CI). Associations with a P value of <0.05 were retained in the final model.
RESULTS
Sample Characteristics
In 2019, 1164 non–HIV-positive men participated in the Flux Study. These men were invited to complete the one-off COVID-19 survey. Among those, 847 completing the COVID-19 questionnaire in full. Using data from 2019, compared with those who responded, those who did not participate were younger (mean: 33.0 vs. 39.4; P < 0.001) but otherwise similar. No differences were observed when comparing number of sexual partners (mean: 13.0 vs. 11.3; P = 0.421) or PrEP use (51.1% vs. 44.1%; P = 0.158). Between 4 and 29 April 2020, 847 HIV-negative and untested participants completed the survey about the impact of COVID-19. Almost all (n = 801; 94.6%) expressed some general, self-defined concern about COVID-19, with 32.5% stating their concern about COVID-19 began before March 1, 2020, and 60.9% becoming concerned by April 1, 2020. Almost half (n = 400, 47.2%) reported PrEP use before COVID-19 restrictions. Subsequent analyses were restricted to these 400 men.
Mean age was 44.1 years (SD: 12.7). Most (n = 342; 85.5%) had been tested for HIV in the previous 3 months. One in 5 (n = 85; 21.3%) had lost their job or had their working hours reduced, and 37.8% (n = 151) were working from home because of COVID-19.
Trends in PrEP Use, HIV Testing, and Sexual Behavior, 2015–2020
Among the 400 men who reported PrEP use before COVID-19, 58.3% continued to use PrEP during COVID-19 restrictions, and 41.8% discontinued use once restrictions were put in place.
Looking back at responses from 2015 onward among the 400 HIV-negative and unknown status men who had reported previous PrEP use, PrEP use at the time of the survey rose from negligible levels in 2015 (4.9%) to 48.2% at the beginning of 2020 and then fell to just 28.8% during COVID-19 restrictions (Fig. 1). After they first reported their PrEP use, 40 men (10.0%) subsequently discontinued PrEP at some time between 2015 and 2019 but had recommenced using it in early 2020 or before 2020. Among the 41.8% men who discontinued PrEP during COVID-19 restrictions, 19 men (11.4%) had previously discontinued its use. Among men who used PrEP in 2019, 92.5% reported they were using it daily.
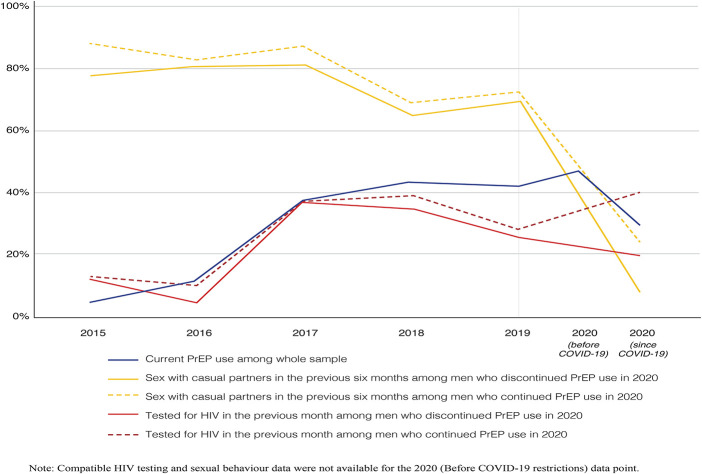
FIGURE 1.
Trends in sex with casual partners recent HIV testing among men who continued and discontinued PrEP use during COVID-19 physical distancing restrictions, 2015 – 2020 (N = 400).
Among the 233 men who continued using PrEP during COVID-19 restrictions, the majority reported sex with casual partners in the 6 months before survey between 2015 (88.2%) and 2019 (72.7%), but this fell to 23.6% during COVID-19 restrictions. Prevalence of HIV testing in the month before survey rose from 13.3% in 2015 to 36.9% in 2017 and remained stable since then, including during the early months of the COVID-19 pandemic (40.3%).
Among the 167 men who discontinued using PrEP during COVID-19 restrictions, on average, the majority reported sex with casual partners in the 6 months before survey completion between 2015 (78.3%) and 2019 (69.8%), but this fell to 7.8% during COVID-19 restrictions. Prevalence of HIV testing rose from 13.3% in 2015 to 36.9% in 2017 and then fell back to 25.7% in 2019, and further declined to 19.8% during COVID-19 restrictions.
Characteristics Associated With Continuation and Discontinuation of PrEP Use
Continuing or discontinuing PrEP was unrelated to sexual identity, education level, state/territory of residence, changes in employment during COVID-19 restrictions, and time since becoming concerned about COVID-19 (Table 1). Men who discontinued PrEP during COVID-19 restrictions were younger than those who continued using PrEP (mean: 42.44 vs. 45.24; P = 0.031) (Table 1). They were also less likely to have recently tested for both HIV and other sexually transmitted infections (STIs) than those who continued using PrEP.
TABLE 1.
Characteristics of the Sample Stratified According to Changes in PrEP Use During COVID-19 Physical Distancing Restrictions Among People With a History of PrEP (N = 400)
| N (%) | Continued to Use PrEP During Physical Distancing Restrictions, n = 233 (58.3) | Stopped Using PrEP After Introduction of Physical Distancing Restrictions, n = 167 (41.8) | P |
| Age, yr | 45.24 (12.88) | 42.44 (12.41) | 0.031 |
| Median: 42 | |||
| Mean: 44.0709 | |||
| SD: 12.74701 | |||
| 16–25 | 10 (4.3) | 6 (3.6) | |
| 26–35 | 52 (22.3) | 54 (32.3) | |
| 36–45 | 64 (27.5) | 45 (26.9) | |
| 46–55 | 51 (21.9) | 34 (20.4) | |
| 56+ | 56 (24.0) | 28 (16.8) | |
| Country of birth | 0.513 | ||
| Australia | 177 (76.0) | 127 (76.0) | |
| Oceania | 6 (2.6) | 10 (6.0) | |
| Asia | 19 (8.2) | 12 (7.2) | |
| North America | 5 (2.1) | 1 (0.6) | |
| South central American countries | 4 (1.7) | 2 (1.2) | |
| Europe | 20 (8.6) | 13 (7.8) | |
| Middle East | 1 (0.4) | 0 (0.0) | |
| Africa | 1 (0.4) | 2 (1.2) | |
| Employment | 0.430 | ||
| No change | 88 (37.8) | 61 (36.5) | |
| Laid off permanently/temporarily or reduced hours | 54 (23.2) | 31 (18.6) | |
| Working from home | 81 (34.8) | 70 (41.9) | |
| Redeployed/new job | 8 (3.4) | 5 (3.0) | |
| Did not answer | 2 (0.9) | 0 (0.0) | |
| Sexuality | 0.305 | ||
| Gay/homosexual | 216 (92.7) | 148 (88.6) | |
| Bisexual | 9 (3.9) | 12 (7.2) | |
| Other | 8 (3.4) | 7 (4.2) | |
| Education | 0.103 | ||
| Less than year 12 high school | 5 (2.1) | 6 (3.6) | |
| Completed high school (year 12) | 35 (15.0) | 13 (7.8) | |
| Trade certificate | 38 (16.3) | 18 (10.8) | |
| Undergraduate degree | 80 (34.3) | 63 (37.7) | |
| Postgraduate degree | 72 (30.9) | 64 (38.3) | |
| Did not answer | 3 (1.3) | 3 (1.8) | |
| HIV status | 0.495 | ||
| HIV negative | 230 (98.7) | 166 (99.4) | |
| Unknown HIV status | 3 (1.3) | 1 (0.6) | |
| HIV testing | <0.001 | ||
| In the previous month | 94 (40.3) | 33 (19.8) | |
| 1–3 mo | 120 (51.5) | 95 (56.9) | |
| More than 3 months ago | 19 (8.2) | 39 (23.4) | |
| STI testing | <0.001 | ||
| In the previous month | 99 (42.5) | 36 (21.6) | |
| 1–3 mo ago | 115 (49.4) | 94 (56.3) | |
| More than 3 mo ago | 19 (8.2) | 37 (22.2) | |
| No. of days since becoming personally concerned about COVID-19 | 36.88 (21.68) | 35.97 (21.54) | 0.680 |
| Difficulty in accessing PrEP following physical distancing restrictions | 0.043 | ||
| Less difficult following physical distancing restrictions | 4 (1.7) | 9 (5.4) | |
| About the same following physical distancing restrictions | 189 (81.1) | 139 (83.2) | |
| More difficult following physical distancing restrictions | 40 (17.2) | 19 (11.4) | |
| No. of months using PrEP (mean SD) | 27.55 (14.21) | 24.61 (15.43) | 0.050 |
| Prior experience recommencing PrEP | 0.437 | ||
| No prior experience reported | 212 (91.0) | 148 (88.6) | |
| Prior experience reported | 21 (9.0) | 19 (11.4) |
PrEP Access During Physical Distancing Restrictions
Among men who discontinued PrEP, most (83.2%) indicated that they believed their access to PrEP remained the same as before physical distancing restrictions, but 11.4% reported that they had found it more difficult to access PrEP during physical distancing restrictions (Table 1). Among men who continued to use PrEP during COVID-19 restrictions, most (81.3%) indicated that their access to PrEP had remained the same.
Sexual Behavior During COVID-19 Restrictions
Almost all men (98.0%; n = 392) reported at least one sex partner in the 6 months before COVID-19 restrictions, with 92.5% (n = 370) reporting more than 1 sex partner at that time (Table 2). No differences in the number of their reported sex partners before COVID-19 were observed between men who continued PrEP use during COVID-19 restrictions and those who discontinued (P = 0.339). However, during COVID-19 restrictions, men who continued to use PrEP were more likely to report more than 1 sex partner compared with those who discontinued PrEP (26.2% vs. 9.0%; P < 0.001).
TABLE 2.
Sexual Behaviors Stratified According to Changes in PrEP Use During COVID-19 Physical Distancing Restrictions Among People With a History of PrEP Use (N = 400)
| n % | Continued to Use PrEP During Physical Distancing Restrictions, n = 233 (58.3) | Stopped Using PrEP After Introduction of Physical Distancing Restrictions, n = 167 (41.8) | P |
| No. of sex partners before physical distancing restrictions | 0.339 | ||
| 0 sex partner before physical distancing restrictions | 3 (1.3) | 5 (3.0) | |
| 1 sex partner before physical distancing restrictions | 11 (4.7) | 11 (6.6) | |
| More than 1 sex partner before physical distancing restrictions | 219 (94.0) | 151 (90.4) | |
| No. of sex partners following physical distancing restrictions | <0.001 | ||
| 0 sex partner following physical distancing restrictions | 99 (42.5) | 111 (66.5) | |
| 1 sex partner following physical distancing restrictions | 73 (31.3) | 41 (24.6) | |
| More than 1 sex partner following physical distancing restrictions | 61 (26.2) | 15 (9.0) | |
| Casual partners following COVID-19 physical distancing restrictions | <0.001 | ||
| No recent casual partners | 178 (76.4) | 154 (92.2) | |
| Recent casual partners | 55 (23.6) | 13 (7.8) | |
| Fuckbuddies following COVID-19 physical distancing restrictions | <0.001 | ||
| No recent fuckbuddies | 165 (70.8) | 152 (91.0) | |
| Recent fuckbuddies | 68 (29.2) | 15 (9.0) | |
| Nonrelationship sexual partners | <0.001 | ||
| No sex with both fuckbuddies and casual partners during physical distancing restrictions | 143 (61.4) | 146 (87.4) | |
| Sex with fuckbuddy or casual partners during physical distancing restrictions | 90 (38.6) | 21 (12.6) |
Men who discontinued PrEP were more likely than those who continued PrEP to have stopped having sex with fuckbuddies (91.0% vs. 76.4%; P < 0.001) and with casual partners (92.2% vs. 76.4%; P < 0.001) during COVID-19 restrictions. Overall, men who discontinued PrEP use were less likely to report nonrelationship sex partners than were those who continued PrEP use during COVID-19 restrictions (87.4% vs. 61.4%; P < 0.001). Men who continued to engage in sex with nonrelationship partners during COVID-19 restrictions were more likely to be protected by PrEP during sex with fuckbuddies (29.2% vs. 9.0%) and casual partners (23.6% vs. 7.8%) compared with those who discontinued PrEP. Sex with a boyfriend or husband was not associated with changes in PrEP use during COVID-19 restrictions (27.9% vs. 21.0%; P = 0.114).
One in 6 men who discontinued PrEP use during COVID-19 restrictions (N = 21) continued to have sexual encounters with nonromantic partners. Of these 21 men, 20 (95.2%) described themselves as having “less sex” during COVID-19 restrictions, and 1 participant reported no change. Of these 21 men, 17 (81.0%) stated that their access to PrEP had not changed during COVID-19 restrictions. Among the 21 men who continued to engage in nonrelationship sex and discontinued PrEP during COVID-19 restrictions, 12 (57.1%) reported having sex with more than 1 man.
Reasons for Discontinuing PrEP During COVID-19 Restrictions
Participants were asked to indicate whether PrEP discontinuation was related to COVID-19 (Table 3). Among the 167 men who discontinued PrEP, most (86.2%; n = 144) indicated that their reason for discontinuation was “I'm not having sex.” Men who reported sex with more than 1 partner during COVID-19 restrictions were the least likely to report this reason for discontinuing PrEP (6.3%). Other reasons included avoiding doctors' clinics (8.4%) or being unable to get a doctor's appointment (5.4%).
TABLE 3.
Reasons for Discontinuing PrEP During COVID-19 Restrictions Stratified According to Number of Sex Partners (n = 167)
| n (%) | No Sex Partners (n = 207) | 1 Sex Partner (n = 113) | 2 or More than Sex Partners (n = 74) | P |
| I'm not having sex | 104 (72.2) | 31 (21.5) | 9 (6.3) | <0.001 |
| Unable to get a doctor's appointment | 6 (66.7) | 3 (33.3) | 0 (0.0) | 0.562 |
| I'm avoiding doctor's clinics | 8 (57.1) | 6 (42.9) | 0 (0.0) | 0.161 |
| It's hard to buy PrEP | 2 (33.3) | 3 (50.0) | 1 (16.7) | 0.214 |
Covariates of PrEP Discontinuation During COVID-19 Restrictions
In multivariable analysis, PrEP discontinuation was not associated with age, STI testing, access to PrEP, length of time using PrEP, number of male sex partners, and having sex with fuckbuddies or nonrelationship sex (Table 4). Compared with men who continued to use PrEP during COVID-19 restrictions, those who discontinued PrEP use were less likely to have recently tested for HIV (aOR: 0.17; 95% CI: 0.09 to 0.34; P < 0.001) and less likely to report sex with casual male partners (aOR: 0.28; 95% CI: 0.14 to 0.54; P < 0.001).
TABLE 4.
Factors Associated With Discontinuation of PrEP During COVID-19 Physical Distancing Restrictions Among People With a History of PrEP Use (N = 400)
| Univariate Analysis | Multivariate Analysis | |||||||
| OR | 95% CI | P | aOR | 95% CI | P | |||
| Upper | Lower | Upper | Lower | |||||
| Age, yr | 0.983 | 0.967 | 0.998 | 0.031 | ||||
| HIV testing | ||||||||
| More than 3 mo | 1 | 1 | ||||||
| 1–3 mo | 0.386 | 0.209 | 0.710 | 0.002 | 0.392 | 0.210 | 0.732 | 0.003 |
| Previous month | 0.171 | 0.087 | 0.336 | <0.001 | 0.174 | 0.087 | 0.347 | <0.001 |
| STI testing | ||||||||
| More than 3 mo | 1 | |||||||
| 1–3 mo | 0.420 | 0.227 | 0.778 | 0.006 | ||||
| Previous month | 0.187 | 0.095 | 0.366 | <0.001 | ||||
| Access to PrEP | ||||||||
| About the same | 1 | |||||||
| Less difficult | 3.059 | 0.923 | 10.137 | 0.067 | ||||
| More difficult | 0.646 | 0.359 | 1.163 | 0.145 | ||||
| No. of months using PrEP | 0.986 | 0.971 | 1.000 | 0.056 | ||||
| No. of sex partners since COVID-19 | ||||||||
| No sex partners | 1 | |||||||
| 1 sex partner | 0.501 | 0.313 | 0.800 | 0.004 | ||||
| More than 1 sex partners | 0.219 | 0.117 | 0.410 | <0.001 | ||||
| Casual partners | ||||||||
| No sex with casual partners | 1 | 1 | ||||||
| Any sex with casual partners during COVID-19 | 0.273 | 0.144 | 0.519 | <0.001 | 0.277 | 0.143 | 0.537 | <0.001 |
| Fuckbuddies | ||||||||
| No sex with fuckbuddies | 1 | |||||||
| Any sex with fuckbuddies during COVID-19 | 0.239 | 0.131 | 0.437 | <0.001 | ||||
| Any nonrelationship sex | ||||||||
| No nonrelationship sex | 1 | |||||||
| Any nonrelationship sex during COVID-19 | 0.229 | 0.135 | 0.387 | <0.001 | ||||
DISCUSSION
Our data indicate a significant reduction in PrEP use by GBM following the introduction of COVID-19 restrictions in Australia. This substantial decline in PrEP use also corresponds with a substantial reduction in sexual contacts among men in this sample.21 For most men, reductions in PrEP use accompanied reductions in the number of sexual partners and nonrelationship sex. Although sexual contacts among men who continued to use PrEP declined, less substantially than among men who discontinued its use, overall sexual contact among GBM declined since the COVID-19 restrictions. This suggests that, in relation to sexual contacts, GBM have largely adhered to public health and physical distancing restrictions implemented by Australian governments guidelines to combat the spread of COVID-19.7 Most men (82.0%) reported no difference in access to PrEP during COVID-19 restrictions, suggesting that discontinuation had little to do with access and that, to date, there has been no disruption in the provision of services supporting access to PrEP in Australia.
Before COVID-19, HIV infections in Australia were decreasing,14 associated with the rapid uptake of PrEP among HIV-negative and unknown status GBM.27 Following the substantial reduction in nonrelationship sex during COVID-19 restrictions, further and potentially substantial reductions in HIV transmission may occur over time while physical distancing and other pandemic-related restrictions are in place. Fluctuations in HIV epidemiological trends can also be expected following changes in frequency of sexual contacts, depending on the extent to which these changes are accompanied by the use of risk reduction strategies, including the use of PrEP. The observed reduction in PrEP use is likely to be a temporary response to current COVID-19 restrictions. Changes in sexual behaviors have and will likely continue to reflect changes in COVID-19 restrictions. Longer-term impacts on sexual behavior and the use of PrEP among HIV-negative and unknown status GBM need to be monitored to ensure timely and appropriate responses are implemented.
Among men who discontinued PrEP during COVID-19 restrictions, recent HIV testing had also dropped since 2019 and was substantially lower than among men who continued using PrEP. As PrEP prescriptions in Australia are tied to regular HIV and STI screening, among men who continued PrEP, HIV testing would still be required for new PrEP prescriptions. For some of the men who discontinued PrEP and who had been less recently tested for HIV and other STIs, their supply of pills probably declined sooner. Some of these men may have chosen to discontinue PrEP use, or to conserve their pills, rather than to return to their doctor for a new prescription. This may have been because of the concerns about visiting clinics during COVID-19 restrictions, and it may have been because they had mostly stopped engaging in sex with nonrelationship partners.
Both before and, especially, after their initiation of PrEP use, men in this cohort who had been using PrEP had mostly discontinued consistent condom use with nonrelationship partners.28 It is therefore important that they are able to recommence PrEP use in a timely fashion because they adjust their sexual activity in response to changes in physical distancing restrictions. Depending on the course of the pandemic, public health measures may ease and then be reimposed. The continued use, the recommencement, any subsequent discontinuation, and changes in mode of use will need to be carefully monitored, particularly given the previous preponderance of daily use.
Between 2015 and 2019, 11.4% of the men who had discontinued PrEP during COVID-19 restrictions reported also discontinuing use on a previous occasion before 2020, suggesting relatively low experience reinitiating PrEP. So, the majority of men lack prior experience with stopping and recommencing PrEP. GBM who discontinued PrEP during COVID-19 restrictions may be unprepared to recommence PrEP use as and when they return to nonrelationship sex or develop new patterns of sexual behavior because of changes in COVID-19 restrictions. Potential issues include the length of time required from initiation to protective coverage, potential side effects after restarting, and the need for HIV testing before reinitiation of PrEP, if they have run out of PrEP. There is a need to consider what is required for appropriate recommencement of PrEP use.
Although on-demand dosing is a potential useful strategy for GBM who discontinued PrEP during COVID-19 restrictions but nonetheless either remained sexually active or have recommenced sporadic sexual activity outside committed relationships, large-scale public campaigns about on-demand use have not been implemented in Australia. Most HIV-negative GBM appear to have inaccurate knowledge of how to use PrEP on-demand.29 The easing of restrictions may be an appropriate opportunity to introduce on-demand messaging, especially for GBM who gradually or intermittently increase their sexual contacts and for whom daily use may be unwarranted at that time. Daily preference for PrEP may be because of insufficient knowledge about on-demand use.30
The small number of men who discontinued PrEP use during COVID-19 restrictions but continued to have sexual encounters with nonromantic partners may nonetheless have been trying to adhere to physical distancing restrictions, given that they also described themselves as having reduced their sexual contacts. Further research to understand the reasons for their decisions about PrEP and sexual behavior during COVID-19 restrictions is required. To avoid short-term increases in HIV infections as physical distancing fluctuate in response to the pandemic, information about appropriate methods and requirements for reinitiation of PrEP, both on-demand and continuous dosing should be available to men who discontinued PrEP during COVID-19 restrictions.
Limitations
This study used an online convenience sample and findings may not be representative of all gay, bisexual, or other men who have sex with men in Australia. Nonetheless, the demographics, characteristics, and the prevalence of sexual behavior reported in this sample is similar to other Australian community-based samples recruited online or in person.31
Although adherence to daily PrEP was not assessed in 2020, most men using PrEP in this sample in 2019 reported using it on a daily basis. This is consistent with findings from other samples of Australian GBM, where clinical and community level adherence to daily use is greater than 90.0%.30,32 PrEP was listed for public subsidy in 2018 in Australia and may have affected the rate of uptake of PrEP use in this sample. However, the uptake of PrEP use in this sample mirrors other Australian samples of GBM.31
Our data are also subject to recall and social desirability bias.33 Men may have been unwilling to report all sexual behaviors during the COVID-19 pandemic. However, our participants were recruited before the COVID-19 pandemic, and the automated online methodology may reduce social desirability bias in reporting illegal or stigmatized behaviors.34 Although the recall periods for sexual behaviors before and after the implementation of physical distancing restrictions differed, we were able to compare the periods to behaviors reported in previous years.
CONCLUSIONS
GBM in Australia substantially reduced their PrEP use shortly after the introduction of COVID-19 restrictions, and this was associated with a large reduction in sexual activity. However, as restrictions fluctuate in response to changing levels of COVID-19 risk in Australia, trends in HIV and other STIs are also likely to fluctuate.
There is a need for a strong HIV and STI health policy and health promotion and policy responses to support GBM to navigate how they recommence PrEP use as their sexual behaviors adjust to the lifting and reimposing of restrictions over the course of the COVID-19 pandemic. One potential component of this response may include increasing awareness of how to successfully restart PrEP among GBM who have discontinued PrEP during COVID-19 restrictions.
ACKNOWLEDGMENTS
The study investigators thank all participants for their continued contribution to the Flux Study.
Footnotes
Supported by the New South Wales Ministry of Health, via the Prevention Research Support Program and NSW Research Program for HIV, STIs and Viral Hepatitis, the Kirby Institute UNSW Sydney, and Australian Research Council Discovery Project.
The authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Mil Med Res. 2020;7:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Considerations in Adjusting Public Health and Social Measures in the Context of COVID-19: Interim Guidance: World Health Organization; 2020. [Google Scholar]
- 5.Commonwealth of Australia as represented by the Department of Health. COVID-19 National Incident Room Surveillance Team. COVID-19, Australia: Epidemiology Report 14 (Reporting Week Ending 23:59 AEST 3 May 2020): Communicable diseases intelligence; 2020:44. [DOI] [PubMed] [Google Scholar]
- 6.ACON Health. COVID-19 Update: Visiting Other People at Home, Physical Distancing & Casual Sex. 2020. Available at: https://www.acon.org.au/about-acon/latest-news/#acon-covid-19-update-visiting-other-people-at-home-casual-sex-and-physical-distancing. Accessed May 15, 2020. [Google Scholar]
- 7.Thorne Harbour Health. Sex, Intimacy and Coronavirus; 2020. Available at: https://thorneharbour.org/news-events/news/info-sheet-sex-intimacy-and-coronavirus/. Accessed May 19, 2020. [Google Scholar]
- 8.ACON Health. COVID-19: Casual Sex and Sex on Premises Venues; 2020. Available at: https://www.acon.org.au/what-we-are-here-for/covid19/. Accessed August 1, 2020. [Google Scholar]
- 9.Pharmaceutical Benefits Advisory Committee. December 2017 PBAC Meeting-Positive Recommendations. Canberra, Australia: PBA; 2018. [Google Scholar]
- 10.Chan C, Broady T, Bavinton B, et al. Gay Community Periodic Survey: Sydney 2020. Sydney, Australia. [Google Scholar]
- 11.Broady T Chan C Bavinton B, et al. Gay Community Periodic Survey: Melbourne 2020. Sydney, Australia. [Google Scholar]
- 12.Kirby Institute. Monitoring HIV Pre-exposure Prophylaxis Uptake in Australia. Sydney, Australia: UNSW Sydney: Kirby Institute; 2019. [Google Scholar]
- 13.Grulich AE, Guy R, Amin J, et al. Population-level effectiveness of rapid, targeted, high-coverage roll-out of HIV pre-exposure prophylaxis in men who have sex with men: the EPIC-NSW prospective cohort study. Lancet HIV. 2018;5:e629–e37. [DOI] [PubMed] [Google Scholar]
- 14.Torjesen I. HIV Diagnoses Fall by a Quarter after PrEP Roll-Out in Australia: British Medical Journal Publishing Group; 2018. 363:k4382. [Google Scholar]
- 15.Brawley S, Dinger J, Nguyen C, et al. Impact of COVID-19 related shelter-in-place orders on PrEP access, usage and HIV risk behaviors in the United States [OADLB0101]. Presented at: 23rd International AIDS Conference; Virtal Conference 2020; San Francisco, CA.
- 16.de Sousa AFL, Oliveira LB, Schneider G, et al. Casual sex among MSM during the period of social isolation in the COVID-19 pandemic: nationwide study in Brazil and Portugal. medRxiv. 2020. Available at: https://www.medrxiv.org/content/10.1101/2020.06.07.20113142v2. [Google Scholar]
- 17.Fernandes DE, Ferreira PRA, Kirsztajn GM. Pre-Exposure Prophylaxis during COVID-19 Pandemic: Can PrEP Prevent Flu-like Symptoms? (Under Review); 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McKay T, Henne J, Gonzales G, et al. The COVID-19 pandemic and sexual behavior among gay and bisexual men in the United States. Available at SSRN: https://ssrn.com/abstract=3614113 or 10.2139/ssrn.3614113. Accessed May 29, 2020. [DOI]
- 19.Pebody R. A Quarter of Gay Men Report Casual Sex during UK Lockdown. 2020. Available at: https://www.aidsmap.com/news/jun-2020/quarter-gay-men-report-casual-sex-during-uk-lockdown. Accessed June 11, 2020. [Google Scholar]
- 20.Sanchez TH, Zlotorzynska M, Rai M, et al. Characterizing the Impact of COVID-19 on Men Who Have Sex with Men across the United States in April; 2020. AIDS Behavior; 2020;29:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hammoud MA, Maher L, Holt M, et al. Physical distancing due to COVID-19 disrupts sexual behaviours among gay and bisexual men in Australia: implications for trends in HIV and other sexually transmissible infections. JAIDS J Acquired Immune Deficiency Syndromes. 2020;85:309–315. [DOI] [PubMed] [Google Scholar]
- 22.Chow EP, Hocking JS, Ong JJ, et al. Changing the use of HIV pre-exposure prophylaxis among men who have sex with men during the COVID-19 pandemic in Melbourne, Australia. Open Forum Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hammoud MA, Jin F, Degenhardt L, et al. Following Lives Undergoing Change (Flux) study: implementation and baseline prevalence of drug use in an online cohort study of gay and bisexual men in Australia. Int J Drug Pol. 2017;41:41–50. [DOI] [PubMed] [Google Scholar]
- 24.Molina J-M, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237–2246. [DOI] [PubMed] [Google Scholar]
- 25.Molina J-M, Charreau I, Spire B, et al. Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. Lancet HIV. 2017;4:e402–e10. [DOI] [PubMed] [Google Scholar]
- 26.Bavinton BR, Duncan D, Grierson J, et al. The meaning of “regular partner” in HIV research among gay and bisexual men: implications of an Australian cross-sectional survey. AIDS Behav. 2016;20:1777–1784. [DOI] [PubMed] [Google Scholar]
- 27.amfAR, AVAC, & Friends of the Global Fight. Translating Progress into Success to End the AIDS Epidemic; 2019. AVAC. Available at: https://www.avac.org/sites/default/files/resource-files/EndEpidemic_nov2019.pdf. Accessed June 9, 2020. [Google Scholar]
- 28.Prestage G, Maher L, Grulich A, et al. Brief report: changes in behavior after PrEP initiation among Australian gay and bisexual men. J Acquir Immune Defic Syndr. 2019;81:52–56. [DOI] [PubMed] [Google Scholar]
- 29.Bavinton BR, Chan C, Vaccher S, et al. Knowledge of event-driven pre-exposure prophylaxis (ED-PrEP) among PrEP-experienced gay and bisexual men in Australia [PEC0636]. Presented at: 23rd International AIDS Conference; Virtal Conference 2020; San Francisco.
- 30.Fraser D, Chan C, Vaccher S, et al. Report on the PrEP in NSW Transition Study, 2018-2020. Sydney, Australia: Kirby Institute, UNSW Sydney; 2020. [Google Scholar]
- 31.Holt M, Lea T, Mao L, et al. Community-level changes in condom use and uptake of HIV pre-exposure prophylaxis by gay and bisexual men in Melbourne and Sydney, Australia: results of repeated behavioural surveillance in 2013–17. Lancet HIV. 2018;5:e448–e56. [DOI] [PubMed] [Google Scholar]
- 32.Vaccher SJ, Marzinke MA, Templeton DJ, et al. Predictors of daily adherence to hiv pre-exposure prophylaxis in gay/bisexual men in the prelude demonstration project. AIDS Behav. 2019;23:1287–1296. [DOI] [PubMed] [Google Scholar]
- 33.Engel RJ, Schutt RK. The Practice of Research in Social Work. London, United Kingdom: Sage Publications; 2016. [Google Scholar]
- 34.Islam MM, Topp L, Conigrave KM, et al. The reliability of sensitive information provided by injecting drug users in a clinical setting: clinician-administered versus audio computer-assisted self-interviewing (ACASI). AIDS Care 2012;24:1496–1503. [DOI] [PubMed] [Google Scholar]