Abstract
Objective
To determine the content priorities and design preferences for a longitudinal care plan (LCP) among caregivers and healthcare providers who care for children with medical complexity (CMC) in acute care settings.
Materials and Methods
We conducted iterative one-on-one design sessions with CMC caregivers (ie, parents/legal guardians) and providers from 5 groups: complex care, primary care, subspecialists, emergency care, and care coordinators. Audio-recorded sessions included content categorization activities, drawing exercises, and scenario-based testing of an electronic LCP prototype. We applied inductive content analysis of session materials to elicit content priorities and design preferences between sessions. Analysis informed iterative prototype revisions.
Results
We conducted 30 design sessions (10 with caregivers, 20 with providers). Caregivers expressed high within-group variability in their content priorities compared to provider groups. Emergency providers had the most unique content priorities among clinicians. We identified 6 key design preferences: a familiar yet customizable layout, a problem-based organization schema, linked content between sections, a table layout for most sections, a balance between unstructured and structured data fields, and use of family-centered terminology.
Discussion
Findings from this study will inform enhancements of electronic health record-embedded LCPs and the development of new LCP tools and applications. The design preferences we identified provide a framework for optimizing integration of family and provider content priorities while maintaining a user-tailored experience.
Conclusion
Health information platforms that incorporate these design preferences into electronic LCPs will help meet the information needs of caregivers and providers caring for CMC in acute care settings.
Keywords: chronic disease, health information exchange, hospital medicine, patient care planning, patient portals, pediatrics, transitional care, user-computer interface, care coordination
INTRODUCTION
Care coordination is critically important for patients with multiple chronic conditions who face an increasingly fragmented healthcare system in the United States.1 Children with medical complexity (CMC) are a prototypical example of these patients, receiving care from an average of 13 different healthcare providers across multiple care settings.2,3 Helping families relay information between multiple care team members (eg, family caregivers, primary care provider, specialists, care coordinators, social workers, school staff, etc) should be a healthcare system priority to support CMC and their families.4–6 A longitudinal care plan (LCP) can be a valuable tool for providing such support within a patient-centered medical home.8,9 An LCP is a holistic, dynamic, and integrated plan that documents important disease prevention and treatment plans of care.8 An LCP should also be patient-centered, incorporating the patient’s values, preferences, and goals of care.8,9 As components of multifaceted interventions, LCPs have been associated with improved care experiences and patient-reported outcomes in pediatric and adult populations.10
However, studies report barriers to creating comprehensive, multidisciplinary, and integrated LCPs.11–13 Existing care plans are often discipline- or setting-specific (eg, seizure care plan or emergency care plan).14–16Paper-based LCPs are lengthy, making it difficult for particular care team members to find the information they need in a timely manner.11 Existing LCPs focus heavily on the information needs of providers compared to families, and designing an LCP that balances these perspectives has remained challenging.11,17 Furthermore, tools to build LCPs within the electronic health record (EHR) have been underutilized or untested, leaving us with few examples of how to optimally design EHR-integrated LCPs.17
Electronic platforms, either web-based or EHR-based, provide us with more flexibility to create user-centered LCPs compared to paper-based LCPs that have a “one-size-fits-all” format. An electronic platform allows users to easily navigate between sections of the LCP using hyperlinks rather than scanning through a lengthy document. Yet, we still understand little of how to optimally design electronic LCPs for CMC.11,17–20
OBJECTIVE
The study objective was to understand the content priorities and design preferences (ie, what content and how to display it) for electronic LCPs to enhance their usability and usefulness among caregivers and healthcare providers who care for CMC in acute care settings (primary care clinics, specialty care clinics, or hospitals).
MATERIALS AND METHODS
Study design and population
To meet our objective, we followed user-centered design principles21 and conducted iterative cycles of design sessions, prototype development, and prototype testing with individuals from 6 care team member groups who care for CMC in acute care settings: family caregivers (ie, parents or legal guardians, henceforth referred to as caregivers), complex care providers, primary care providers, emergency care providers, subspecialty care providers, and care coordinators. All study procedures were approved by the Seattle Children’s Hospital Institutional Review Board.
We enrolled English-speaking caregivers of CMC (0 to 18 years of age) who received care at a tertiary children’s hospital between August 2017 and March 2019. CMC were followed by the institution’s complex care service and met the Pediatric Medical Complexity Algorithm complex chronic conditions designation.22 We used a qualitative strategy, purposive sampling, to maximize participant diversity and perspectives by recruiting eligible participants based on the following characteristics: child age, types of medical conditions, child and parent race/ethnicity, and geographic county. Trained research staff used a standardized recruitment protocol to approach eligible caregivers either in-person (during a child’s hospital admission) or by telephone.
We identified providers who care for CMC within the study institution or from clinical sites within the institution’s 5-state catchment area through professional acquaintances of current and former hospital providers (eg, residency program graduates). We used purposive sampling to maximize diversity of provider participants based on age, practice years, practice location, and familiarity with the study institution’s EHR. Trained research staff recruited providers using a standardized electronic mail recruitment script.
We recruited and enrolled caregivers and providers until we achieved thematic saturation, meaning few new ideas or themes emerged from our analysis as we continued conducting design sessions within each care team member group and across groups.23
Design sessions
We conducted design sessions in the child’s hospital room, a private hospital meeting room, a provider’s office, or by telephone for geographically distant participants. One to 2 research team members conducted each design session which lasted approximately 1 hour and included a combination of card sorting, drawing exercises, and scenario-based prototype testing activities.
In the card sorting activity, we asked participants to sort through 30–40 cards with key pieces of LCP content elicited from a prior study.11 We then asked them to arrange these cards on a table to represent content they would prioritize on their LCP “homepage” versus content they would prefer to access via hyperlinks from their homepage. We took photos of their final card arrangements. In the drawing exercise, we invited participants to draw examples of their ideal homepage layout and specific LCP sections on paper templates of a mobile or desktop screen. We encouraged them to think of features that they find useful in existing applications such as tiles, show/hide windows, navigation bars, and hyperlinks. In the prototype testing activity, we asked participants to walk through a scenario pertinent to their role in caring for CMC using the evolving prototype that we were concurrently developing. The LCP prototype contained mock patient data. For example, we presented participants in the emergency care provider group with a scenario of a CMC presenting to the emergency department without their parent. Not all participants completed all 3 activities, as the focus of design sessions shifted from identifying content priorities to prototype testing. More than one-third of participants completed each activity and all participants completed 2 or more activities.
All design sessions were audio-recorded in their entirety. Recordings were not transcribed because it was easier for research team members to review card sorting photos, participant drawings, and the prototype while listening to audio-recordings versus reading through a written transcript during our analysis. While this approach was more time-intensive, we were able to catch subtle nuances in the conversation that would not be captured in written transcripts. Participants received a $25 gift card after completing the design session.
Data analysis
Between each design session, at least 2 research team members reviewed each session’s audio-recording, photos, and drawings. Each member independently noted content priorities, formatting preferences, and prototype usability issues using conventional content analysis techniques.23 Research team members met after every design session to discuss findings and rereviewed audio-recordings if necessary, focusing on priorities, preferences, and prototype usability issues that were common within each care team member group and across groups. Each session informed the content of subsequent design sessions, and we revised the prototype between sessions based on our iterative content analysis. We initially created paper prototypes based on participant drawings and then moved to a digital, interactive prototype as we continued through design sessions.
RESULTS
We conducted 30 design sessions: 10 with caregivers and 20 with providers to achieve thematic saturation within each care team member group and across groups. Of the 13 eligible caregivers that we approached, 10 (77%) participated in the study (Table 1). Of the 27 eligible providers that we approached 20 (74%) participated in the study (4 in each provider group; Table 1).
Table 1.
Characteristics of caregiver and provider participants
| No. (%) | ||
|---|---|---|
| Caregivers | N = 10 | |
| Age, years | ||
| <35 | 2 (20) | |
| 36–45 | 3 (30) | |
| >45 | 5 (50) | |
| Ethnicity | ||
| Hispanic or Latinx | 3 (30) | |
| Not Hispanic or Latinx | 7 (70) | |
| Race | ||
| White | 9 (90) | |
| Not White | 1 (10) | |
| Level of education | ||
| At most high school graduate or GED | 2 (20) | |
| Some college/university without a 4-year degree | 3 (30) | |
| 4-year university degree or more | 5 (50) | |
| Primary residence | ||
| Within same county as study institution | 4 (40) | |
| Within state (but not same county as study institution)a | 5 (50) | |
| Out-of-state | 1 (10) | |
| Number of caregivers in the home | ||
| 1 | 1 (10) | |
| 2 | 4 (40) | |
| >3 | 5 (50) | |
| Number of years child has had a care plan | ||
| No care plan (not applicable) | 4 (40) | |
| <1 year | 1 (10) | |
| 1–5 years | 3 (30) | |
| >5 years | 2 (20) | |
| Frequency caregiver refers to care plan | ||
| No care plan (not applicable) | 4 (40) | |
| Never | 1 (17) | |
| 1–2 times in past 6 months | 4 (66) | |
| Daily | 1 (17) | |
| Providers | N = 20 | |
| Age, years | ||
| <35 | 8 (40) | |
| 36–45 | 6 (30) | |
| >45 | 6 (30) | |
| Type of Provider | ||
| Complex care provider | 4 (20) | |
| Primary care provider | 4 (20) | |
| Emergency department provider | 4 (20) | |
| Subspecialty provider | 4 (20) | |
| Care coordinator/Case manager | 4 (20) | |
| Number of years in practice | ||
| 0–5 | 8 (40) | |
| 6–10 | 4 (20) | |
| 11–20 | 5 (25) | |
| >20 | 3 (15) | |
| Primary practice location | ||
| Based at study institution | 13 (65) | |
| In-state (not based at study institution) | 5 (25) | |
| Out-of-state | 2 (10) | |
| Provider has created or reviewed a patient care plan | 15 (75) | |
| Provider comfort level caring for CMCb | 94 [76 100] | |
| Provider comfort level using EHRb | 96 [80 100] | |
| Technology Comfort Level | N = 30 | |
| Participant comfort level with navigating websites on a computerb | ||
| Caregivers | 94 [75 100] | |
| Providers | 97 [75 100] | |
| Participant comfort level with using smartphone appsb | ||
| Caregivers | 95 [74 100] | |
| Providers | 93 [61 100] | |
| Participant comfort level storing PHI on a mobile deviceb | ||
| Caregivers | 83 [50 100] | |
| Providers | 82 [28 100] | |
Abbreviations: CMC, children with medical complexity; EHR, electronic health record; GED, general equivalency; diploma; PHI, personal health information.
Participants were from 5 different counties within the state.
Mean comfort level and range on a scale from 1–100 with higher ranking indicating higher comfort level.
We divided findings into 2 categories based on our objectives: content priorities and design preferences. Below, we present similarities and differences in content priorities within and across care team member groups with all content priorities presented in Table 2. We also present 6 key design preferences and how we incorporated preferences in revisions of the LCP prototype. Illustrative quotes for each category are presented in Tables 3 and 4.
Table 2.
Combined content priorities of caregivers and providers by longitudinal care plan section
Profile header
|
Medication list
|
Diet and nutrition
|
Content is linked from other care plan sections.
Content within this section will link to the baseline management plan for each active issue listed here.
Table 3.
Illustrative quotes from caregivers and providers regarding content priorities
| Themes | Illustrative Quotes |
|---|---|
| Caregivers prioritized having a baseline photo and sections to highlight unique care preferences, developmental status, and child’s baseline for providers to see |
“A baseline photo would be good. Then there’s a ‘I know when he's getting sick because he gets purple under his eyes’. Also, if I wasn’t there I would want somebody to know that you can’t put his meds through his J tube too fast.” (Caregiver #3) “90% of the time we are next to his bed when he is inpatient, but sometimes we go to eat and he wakes up, sometimes they don't know how to calm him down. Those things are important for [the nurses] to know.” (Caregiver #9) “[Referencing the ‘About Me’ section] Some of these things are more general, like, she has 2 pets. If you had another section for the specific medical things I want them to know about her, because I don’t think all the doctors will read [the ‘About Me’ section]. They will probably go more to the sections about her major issues.” (Caregiver #8) |
| Caregiver content priorities for their homepage differed based on individualized information needs and gaps |
“Emergency care plan is my biggest thing. Because they are not you guys. They tend to not know him because they are not a specialty pediatric hospital. I want to be able to pull it out of my purse and say this is his plan for seizures, imaging… Instead of them saying ‘I talked to pulmonary and they want X, Y, Z.’” (Caregiver #3) “Things happen so frequently, things get muddled after a while. A timeline of events would be very useful. That’s a recurrent theme for illness, nutrition, diet changes, weight changes, medication changes…being able to correlate those dates to changes in his health.” (Caregiver #4) “If on the calendar you had a tab with information of every provider that was needed on that date. That would be easier, because otherwise I carry my calendar and another folder that has all the cards of contact information.” (Caregiver #2) |
| Emergency providers prioritized resuscitation and stabilization plans with baseline status on a 1-page summary |
“If they have a difficult airway to intubate, that's really key to know. That's probably the first thing.” (Emergency Provider, Provider #12) “For lines, tubes, and shunts. Do they have a Hickman? With how many ports? I don’t care where you put it on the page, but I want to know if they have a [ventriculoperitoneal] shunt, trach, all that stuff.” (Emergency Provider, Provider #8) “Baseline status is helpful. This kid doesn’t spike fevers or they were always hypotensive. So every time they come in I'm not going to jump on them for their heart rate of 40. If the family is not there, this is something I need to know and is often hard to discriminate.” (Emergency Provider, Provider #10) “I could get to more detailed information if I needed to. But I could always look under the [problem] to look at the details, because I care about that information. If all that information is so easily accessible here I don’t have to go through all their neurosurgery notes.” (Emergency Provider, Provider #8) |
| Non-emergency clinicians prioritized a focus on pertinent history, baseline management plans, and sick plans for each active issue |
“I like being able to click these boxes on the [navigation bar] and this gives me all the active issues that are going on. I'm probably there for the hydrocephalus, but it clues me in to what things we'll be talking about today. I like to be more holistic, rather than going in and only talking about what I want to talk about.” (Neurosurgery Provider, Provider #13) “Just to push a little bit on this. This is the well and sick plan, but it doesn’t include the kid’s meds. I would argue that the meds in that system should pop up as well, and even maybe the contacts. There’s no reasons you couldn’t have it populate in here.” (Complex Care Provider, Provider #2) “I need a task list for sure. For me that's healthcare maintenance. Do I need to repeat a thyroid study? If they have a bone marrow transplant, what’s the protocol if they have low immunoglobulins? You know, the primary care stuff that I don’t actually remember the details of.” (Primary Care Provider, Provider #9) |
| Subspecialists also prioritized labs and imaging studies | “Having customizable reports and studies on home page like a recent ultrasound with a link to the image and report. A scroll box for pertinent labs that's customizable. I don't want to see all components of their blood count, but I want to know their recent kidney function and electrolytes. (Urologist, Provider #15) |
| Care coordinators prioritized care team member list | “The care team contact information tab is the best tab for me, because I do a lot of emailing and phone calls to do care coordination for the patient.” (Care Coordinator, Provider #20) |
Table 4.
Illustrative quotes from caregivers and providers regarding design preferences
| Themes | Illustrative quotes |
|---|---|
| Familiar yet customizable layout |
“I really like the buttons, because you can fit more on a home screen and have easier access. You know how your phone is set up, with all the app icons, having the different icons would give you easier access to a whole bunch of information. People are used to that.” (Caregiver #6) “You have the same pallet of widgets to choose from. Widgets can have a predetermined set of possible sizes depending on the priority you want to give them. The widget idea gives you a lot of flexibility. The backend information never changes, just the presentation of the information.” (Caregiver #4) “This [navigation bar design] feels like the format is better for the inpatient setting, but [this icon design] would have more versatility outside of the hospital setting. For me, the [navigation bar design] would be better as an inpatient provider.” (Complex Care Provider, Provider #2) |
| Problem-based content organization is more inclusive | “I think problems are a little more elegant, but our hand-off culture is systems-based. In an ideal world we'd just be problem oriented. It's nice to get away from systems. For instance, a diagnosis like storming, is it neurology? Is it cardiology? You make these arbitrary distinctions and what happens is now you're forcing the user to click on something…try again…go back…it's an efficiency issue.” (Complex Care Provider, Provider #3) |
| Redundancies built into the platform |
“[On the ‘Active Issues’ page], I would want to see the problem, their current therapies. It would be helpful to have some sort of timeline or some sort of brief medical history related to that problem.” (Cardiologist, Provider #16) “[Under each system], I would have their summary of current state, labs, lines/tubes/shunts, sick plan, well plan. And I would have a hyperlink to the front page—care team. So you’re not putting it in 3 different times, 3 different ways, but you know who to contact.” (Care Coordinator, Provider #18) “I don’t think the baseline vitals should only be under the emergency care plan. I’m not sure if you can add it as a separate tab as well. It would be valuable for emergency room settings, but to other subspecialty providers.” (Pulmonologist, Provider #14) |
| Table layout for most sections with search, sort, and filter functionality | “Appointments would be part of care team as well as insurance. It would be like a grid. It would be care team, contact, appointment.” (Care Coordinator, Provider #18) |
| Balance of structured versus unstructured data fields |
“Free texting can be a little more descriptive, but a little less standardized. ICD-10 codes are the opposite. There are benefits to both. I’m used to ICD-10 codes in the electronic health record. But I also value the more descriptive terms that we don’t get from standard coding.” (Pulmonologist, Provider #14) “I would have an ‘other’ at the bottom because in real-time. If a new thing is presenting, I would love to be able to add that in to say there’s this new issue. Let me just free text something in and then the person who is in charge can decide if it’s important enough to categorize later.” (Emergency Provider, Provider #8) |
| Clear and family-centered terminology | “With “emergency information” I was expecting to see patient and family emergency contact information and not resuscitation and stabilization information. Coming up with a different term would be better.” (Pulmonologist, Provider #14) |
ICD: International Classification of Diseases.
Content priorities
Caregivers
Universally, caregivers prioritized displaying a photo of their child at baseline on the LCP homepage. The majority prioritized sections for families to document their child’s unique care preferences (eg, “tips for interacting with the child” and baseline developmental status, signs, and symptoms). Beyond these areas, caregivers prioritized different content depending on their perceptions of the purpose of the LCP. For example, 1 caregiver noted that the emergency care plan would be a central focus of their homepage because they live in a rural town where local emergency providers are unfamiliar with caring for CMC. In contrast, another caregiver emphasized the need for an event tracker to log their child’s symptoms so they could correlate changes in symptoms with changes in the child’s management plan to prevent future hospitalizations. Within each section, caregivers expressed similar information needs as noted in Table 2. Thus, caregivers prioritized different LCP sections rather than specific content within each section.
Providers
Provider content priorities differed primarily at the group level, especially in the case of emergency providers and care coordinators; however, content priorities were mostly consistent within each provider group. One provider summarized this need for user-tailored content as:
“I'm sure each specialty could think about things unique to their patients that they would want to know and would shape how they thought about a patient.”—Cardiologist (Provider #16)
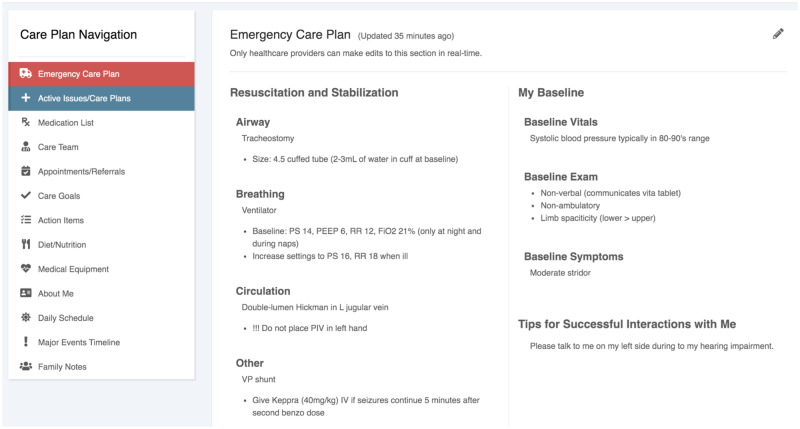
Among clinician groups, emergency providers expressed the most unique content priorities. They prioritized a homepage that would succinctly summarize resuscitation and stabilization information with a focus on the child’s “lines, tubes, and shunts” (Figure 1). They also noted this single page view should include the child’s baseline vitals and exam to guide appropriate management decisions (eg, “blood pressure typically runs low, avoid extra fluids”), as well as a short section providing tips for interacting with the child to provide more family-centered care. They recommended additional details about the child’s active issues should be available via a hyperlink from the homepage.
Figure 1.
Emergency care plan succinctly summarizes resuscitation and stabilization information with a focus on the child's medical equipment. The page also includes the child's baseline vitals and exam findings, as well as a brief section on child/parent preferences for care. A deeper dive into each of the child's active issues is accessible via a tab in the left-sided navigation bar (in blue).
The remaining clinician groups were generally aligned with prioritizing a list of the child’s active issues on the homepage with hyperlinks to obtain additional details such as clinical notes, a medication list, and care team member information. Our institution’s paper-based care plans included a “sick plan,” which provided the child’s unique illness management plan for each problem. Provider participants liked the concept of this sick plan and recommended it should include the child’s common presenting symptoms and the individualized plan for that presentation (eg, “if [child’s name] presents with vomiting, then obtain a shunt series”). They noted sick plans should include escalation plans for different settings (eg, home, school, outpatient, and inpatient settings). We noted a few differences in content priorities between clinician groups: primary care providers highlighted the need for an action items list to track health maintenance activities, whereas subspecialists mentioned lab and imaging information should be included in the medical history section.
Care coordinators universally emphasized the care team contact list as the most important section for their LCP homepage, with an appointment list, an action item list, and clinical notes as secondary priorities. Within the contact list, communication information such as e-mail addresses or back-end telephone lines would be particularly useful. However, they acknowledged that some providers may be concerned that caregivers would use this information as their primary communication mode with providers if it was visible to caregivers. This situation highlighted the need for custom visibility of certain data elements based on care team member role given the LCP would be accessible to caregivers and providers.
Design preferences
Familiar yet customizable layout
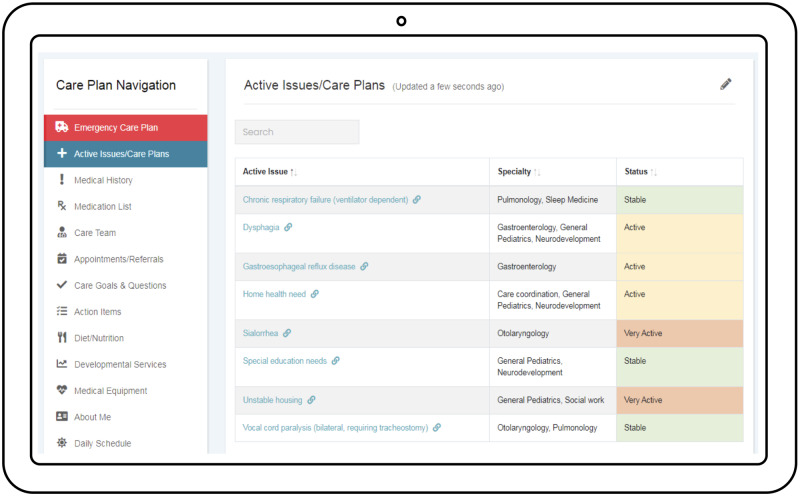
Based on caregiver drawings from a prior study,11 we initially presented caregivers with paper prototypes using 3 design layouts for the LCP homepage: (1) an icon design with clickable icons representing each section; (2) a snapshot design, with a visible preview of preset sections such as the medication list and calendar with other sections accessible via a menu; and (3) a timeline design, in which information from each section was searchable by tags on a chronological timeline. We included both mobile and desktop design layouts given our prior work which found that caregivers preferred different device options depending on when they accessed the LCP.11 Caregivers felt the icon design was most intuitive and familiar, similar to the design of mobile devices. They also liked having the flexibility to move icons so we revised the homepage design to facilitate this level of customization based on their content priorities as opposed to having a fixed set of icons (Figure 2). We included a scroll bar of LCP section icons with an optional free-form family notes section. Caregivers could drag and drop icons into placeholder sections to set their homepage and move or replace these icons over time as their needs changed.
Figure 2.
Customized icon homepage design, where caregivers can choose from a core set of care plan sections to customize their home page based on their content priorities.
Providers noted that the LCP should have a similar design to the EHR with a header on the top and a left-sided navigation bar. Caregivers also preferred this layout when accessing the LCP on a desktop device. However, participants preferred to rearrange the order of tabs in the navigation bar based on their content priorities. Providers also suggested that the platform should apply filters based on their role at the time of login to efficiently direct them to their role-specific homepage and list of active issues.
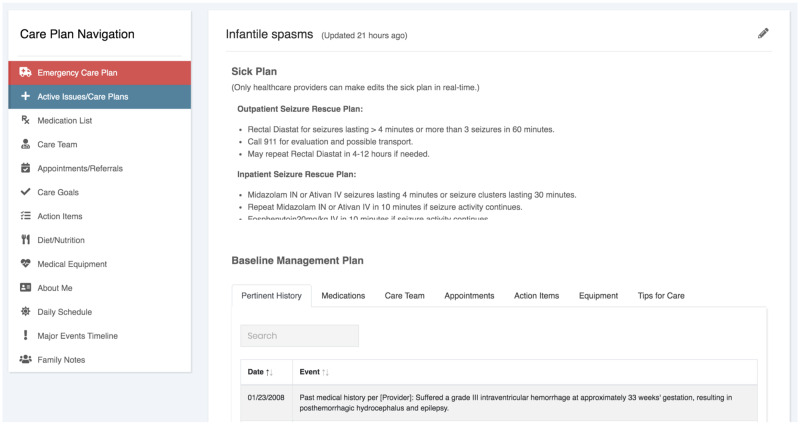
Problem-based content organization is more inclusive
Our initial LCP homepage design for providers consisted of system-based folders organized by specialty with a table of pertinent problems within each folder (Supplementary MaterialFigure 1). Each problem contained 2 columns for each active issue within that system (ie, specialty): a “well plan” column, which included medical history and baseline management plan information and a sick plan column as previously mentioned (Supplementary MaterialFigure 2). In general, emergency care providers and sub-specialty care providers preferred this system-based organization, whereas primary care providers preferred a problem-based format. Complex care providers and care coordinators had mixed perspectives. After testing both schemas, we identified that content organization by the child’s active issues (ie, problem-based) was more family-centered and more streamlined (ie, fewer information layers, Figure 3). Additionally, caregivers and providers noted that a problem-based format would facilitate the inclusion of “nonmedical” issues that could be included within an LCP, such as special education needs, home health needs, or housing needs, which may not be associated with a clinical specialty. To integrate both perspectives, we included the ability to link each active issue to individual or multiple body systems with filtering functionality so providers could quickly find the issues that were pertinent to their role (Figure 3).
Figure 3.
Active issues list. Each active issue (i.e. problem) can be associated with multiple “specialties” (i.e. systems) to accommodate the preferences of users who prefer a problem-based format versus a systems-based format. A search box allows users to filter active issues by specialty. Status presents a quick visual overview of high priority issues and can be edited by anyone on the care team.
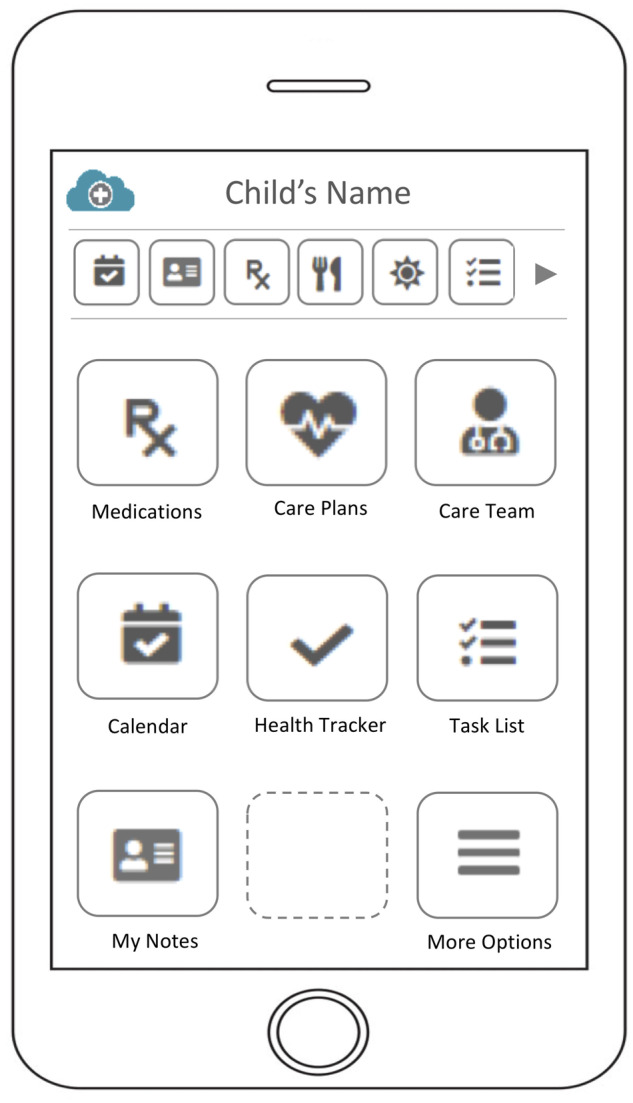
Redundancies built into the platform
The initial LCP layout included discrete sections (eg, “system-based” care plans, medication list, contact list, appointment list) accessible via a navigation bar. As design sessions progressed, it became evident that participants wanted to link information between different LCP sections. For example, most of the information contained in the “well plan” (eg, baseline management plan) could be found in other LCP sections, such as care team members, appointments, and medical equipment. Providers suggested that redundancies should be built into the system so that content would appear within its own section and within each active issues page. This would help to avoid conflicting information between sections and maintain a cohesive LCP. For example, 1 provider stated:
“Having redundancy in the system is important, so you have multiple ways of getting to the same information because everyone has a different thought process.” Pulmonologist, (Provider #14)
This feedback led to an important prototype revision, in which we created an active issues page with linked content from other sections (Figure 4). Thus, a single “active issues” page would present a holistic view of the past medical history, baseline management plan, and sick plan pertinent to that issue. Users could still obtain a comprehensive list of information within each section using the navigation bar (Figure 4). Caregivers and providers noted that these types of redundancies would help ensure information such as “tips for interacting with my child” could appear in both family sections and “medical information” sections, decreasing the likelihood this information would be ignored or overlooked by providers.
Figure 4.
Active issues page with sick plan. For each active issue, the baseline management plan information is linked from other care plan sections, which are accessible via a left-sided navigation bar.
Table layout for most sections with search, sort, and filter functionality
We initially presented participants with the most simplistic design—a table format—to organize section content. Participants agreed that for most sections this design was clear, with familiar search, sorting, and filtering functionality to quickly retrieve needed information. Some suggested a calendar view and a medication schedule may be more helpful for caregivers than an appointment or medication list. Therefore, the ability to toggle between different views (eg, list versus calendar) would provide a more user-centered experience for some sections. Finally, in reference to the sick plan, participants suggested that a cascade of tabs presenting a stepwise progression from “home/school escalation plan” to “inpatient management plan” would be helpful.
Balance of structured versus unstructured data fields
As design sessions progressed, participants desired similar categories of information within a particular section (eg, medication information should include name, concentration, dosage, prescriber, etc). However, not all the information that caregivers or providers found to be important fit neatly within these categories. Therefore, we opted to add an optional “notes” category to all sections of the care plan.
Caregivers also highlighted similar issues with “family information” sections. Caregivers noted that the “About Me” template in the initial prototype, which included discrete fields for siblings, pets, and child’s likes/dislikes, may not be relevant to all families. Therefore, some suggested leaving this template as an open-ended text box with hints of what information caregivers could include. For unstructured text fields, we added these “hint boxes” throughout the prototype and character counts for specific sections. This could help reduce the cognitive burden for caregivers and providers when adding or editing content, while maintaining brevity and uniformity.
Clear and family-centered terminology
Given a single LCP would be used by families and providers, participants recommended paying careful attention to terminology throughout the LCP. For example, a “problem list” is a provider-centric term referring to a list of the child’s diagnoses; however, the term “active issues” was thought to be easily understandable to all care team members including caregivers. In the initial prototype, 1 of the navigation tabs said, “emergency info”, which linked to resuscitation and stabilization information. Many participants assumed this meant emergency contact information, so this tab was changed to “emergency care plan.” Caregivers also suggested including hover boxes to clarify medical terminology, such as “Pulmonologist: Breathing Provider” or including layman’s terms for diagnoses.
DISCUSSION
This study provided an in-depth exploration of the content priorities of caregivers and providers who care for CMC and identified 6 key LCP design preferences that would support their information needs. Design preferences included the ability of individual caregivers to customize their homepage based on their current content priorities and having customized homepage layouts for different provider groups, particularly in the case of emergency care providers and care coordinators. Design preferences also included a problem-based organizational framework with individual active issue pages displaying a sick plan, pertinent history, and baseline management information that were linked from individual LCP sections. Additional design preferences highlighted the need for flexibility in how content within each section is structured and displayed to balance the needs of families and different provider groups.
As interest in LCPs continues to grow,8,24 these findings will be informative for EHR vendors and technology companies to develop LCPs that are consistent with the needs, priorities, and constraints of caregivers and providers who care for pediatric patients, particularly those with complex chronic conditions. Commercially available EHRs, patient portals, and external web-based applications do not currently support their needs.25–30 Our study provides specific guidance to enhance the usability and usefulness of these applications for both families and providers. For example, the primary function of the EHR-embedded problem list is to provide a snapshot of the patient’s active issues, yet they continue to remain underutilized.29,31,32 Although a snapshot of active issues is important, we describe a template for how to leverage the problem list so that it can serve as a central gateway for key information about the child’s pertinent medical history, baseline management plan, and contingency plan for each problem in a single view. Our design recommendation would potentially save providers time by replacing the practice of searching through multiple documents or tabs to find the information they need for an upcoming clinical encounter. In patient portals, using active issues to link information between LCP sections could help caregivers better understand the relationship between their child’s medications, appointments, and care team members and each active issue. These user-centered design recommendations serve as a foundation for building health information systems that incorporate relationships between discrete data fields to present an easy to retrieve and meaningful story, which can be used to guide more efficient, effective, and patient-centered health encounters.
This study also provides valuable design ideas to create a shared representation of the child’s health history, care goals, and care plans by balancing family and provider perspectives within a single LCP. For example, by integrating a “tips for interacting with the child” section within the emergency care plan, by displaying “family goals of care and questions” within each active issue page, or by presenting the “sick plan” as a cascade of care plans from the home to the hospital, the LCP transforms into more of an integrated, shared representation of care plans and goals from the entire team, including families.8,11 Thus, templates integrating these combined content priorities should be a core feature of vendor-supplied EHRs versus add-on features. This study also addresses gaps in the design of patient portals, which currently pull in structured data from provider-centric EHRs without much consideration of the content priorities of patients and families, let alone CMC.11,33,34 Our findings demonstrate how “codesigning” with families can yield valuable insights to enhance the usability and usefulness of patient-facing applications.35,36 One question this study raises is whether LCPs should be the central focus of patient portals versus a standalone feature. Thus, instead of considering the LCP and patient portal as two separate tools, we encourage EHR vendors and technology developers to incorporate these design preferences into a cohesive patient-facing application that meets the shared information needs and content priorities of caregivers and providers.
Limitations and future work
We note some limitations of this study. First, the study was conducted with English-speaking families only; therefore, this study should be replicated with non-English speaking families who will likely require different or additional design considerations. Second, this study focused on providers who care for CMC in acute care settings. Although we included care coordinators and case managers to incorporate the perspective of nursing professionals, further research is needed to understand the content priorities and design preferences of diverse groups of nursing professionals who care for CMC in emergency, inpatient, and ambulatory care settings. Furthermore, many CMC receive care from multidisciplinary and inter-professional team members in the home, school, and community such as home nurses, school nurses, therapists, and social workers. While the design preferences we identified in this study are likely applicable to these groups, it is essential that we conduct additional design work to understand how to add or modify these design preferences to incorporate their content priorities and perspectives, as well as the perspectives of patients themselves.
We recognize further study is required to test these design preferences in real-world settings. Optimizing how caregivers and providers will access and collaboratively manage LCP content within their current workflows also necessitates further study. Additionally, studies are needed to measure the cognitive burden of linking new content to active issues, to assess the impact of an electronic LCP for improving information retrieval efficiency, and most importantly, to measure the effectiveness of this tool on family experiences and health outcomes.
CONCLUSION
This study provides an extensive assessment of the content priorities of a diverse group of team members who care for CMC and identifies 6 key design preferences for an electronic LCP. These design recommendations will address existing gaps in EHR and patient portal functionality, such as providing customized layouts, using active issues pages to link content between LCP sections, and integrating both caregiver and provider content priorities within single page views to provide a shared representation of the patient’s history, management plan, and care goals. Health information systems that incorporate these design preferences into LCPs have the potential to promote efficiency, enhance communication, facilitate coordinated care, and improve health outcomes for these patients.
FUNDING
This study was supported by a Patient-Centered Outcomes Research (PCOR) Mentored Clinical Investigator Award from the Agency of Healthcare Research and Quality under award number K08HS024299 (PI: Arti D. Desai).
AUTHOR CONTRIBUTIONS
AD conceptualized and designed the study, collected data, participated in data analysis, and drafted the initial manuscript. GW and JW collected data and participated in data analysis. DK and VS participated in data analysis. WP and SA participated in the design of the study. All authors reviewed, revised, and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We would like to acknowledge the University of Washington Mary Gates Scholars Program and the University of Washington Undergraduate Research Program for providing undergraduate student support to pursue research opportunities. Icon images were obtained from Font Awesome (fontawesome.com). We would also like to thank Drs. Rita Mangione-Smith and Maria Britto for their mentorship during the course of this study and the Seattle Children's Hospital Digital Health Team and Dr. Brett Leggett for his clinical informatics expertise.
CONFLICT OF INTEREST STATEMENT
None declared.
Abbreviations
- CMC
Children with medical complexity
- EHR
Electronic health records
- LCP
Longitudinal Care Plan
REFERENCES
- 1. Bodenheimer T. Coordinating care-a perilous journey through the health care system. N Engl J Med 2008; 358 (10): 1064–71. [DOI] [PubMed] [Google Scholar]
- 2. Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A.. Patterns and costs of health care use of children with medical complexity. Pediatrics 2012; 130 (6): e1463–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Horsky J, Morgan SJ, Ramelson HZ.. Coordination of care for complex pediatric patients: perspectives from providers and parents. AMIA Annu Symp Proc 2014; 2014 (681) [PMC free article] [PubMed] [Google Scholar]
- 4. Antonelli RC, McAllister JW, Popp J, Fund C. Making care coordination a critical component of the pediatric health system: a multidisciplinary framework. The Commonwealth Fund. https://www.lpfch.org/sites/default/files/care_coordination_a_multidisciplinary_framework.pdf. Accessed April 6, 2020
- 5. Allshouse C, Comeau M, Rodgers R, Wells N.. Families of children with medical complexity: a view from the front lines. Pediatrics 2018; 141 (Supplement 3): S195–201. [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics Council on Children with Disabilities. Care coordination in the medical home: integrating health and related systems of care for children with special health care needs. Pediatrics 2005; 116 (5): 1238–44. [DOI] [PubMed] [Google Scholar]
- 7. Turchi RM, Antonelli RC, Norwood KW, et al. Patient- and family-centered care coordination: a framework for integrating care for children and youth across multiple systems. Pediatrics 2014; 133 (5): e1451–60. [DOI] [PubMed] [Google Scholar]
- 8. Dykes PC, Samal L, Donahue M, et al. A patient-centered longitudinal care plan: vision versus reality. J Am Med Inform Assoc 2014; 21 (6): 1082–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McAllister JW. Achieving a Shared Plan of Care with Children and Youth with Special Health Care Needs. Lucile Packard Foundation for Children’s Health. https://www.lpfch.org/publication/achieving-shared-plan-care-children-and-youth-special-health-care-needs. Accessed April 6, 2020
- 10. Lion KC, Mangione-Smith R, Britto MT.. Individualized plans of care to improve outcomes among children and adults with chronic illness: a systematic review. Care Manag J 2014; 15 (1): 11–25. [DOI] [PubMed] [Google Scholar]
- 11. Desai AD, Jacob-Files EA, Wignall J, et al. Caregiver and Healthcare Provider Perspectives on Cloud-Based Shared Care Plans for Children with Medical Complexity. Hosp Pediatr 2018; 8 (7): 394–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Adams S, Cohen E, Mahant S, Friedman JN, Macculloch R, Nicholas DB.. Exploring the usefulness of comprehensive care plans for children with medical complexity (CMC): a qualitative study. BMC Pediatr 2013; 13 (1): 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Berry JG, Goldmann DA, Mandl KD, et al. Health information management and perceptions of the quality of care for children with tracheotomy: a qualitative study. BMC Heal Serv Res 2011; 11: 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pyles LA. Testing the Consensus-Based Emergency Information Form. Pediatrics 2016; 138 (2): e20161715. [DOI] [PubMed] [Google Scholar]
- 15. Jacobsen PB, DeRosa AP, Henderson TO, et al. Systematic review of the impact of cancer survivorship care plans on health outcomes and health care delivery. J Clin Oncol 2018; 36 (20): 2088–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Albert DVF, Moreland JJ, Salvator A, et al. Seizure action plans for pediatric patients with epilepsy: a randomized controlled trial. J Child Neurol 2019; 34 (11): 666–73. [DOI] [PubMed] [Google Scholar]
- 17. Ming DY, Jackson GL, Sperling J, et al. Mobile complex care plans to enhance parental engagement for children with medical complexity. Clin Pediatr (Phila) 2019; 58 (1): 34–41. [DOI] [PubMed] [Google Scholar]
- 18. Ranade-Kharkar P, Norlin C, Fiol D.. G. Formative evaluation of care nexus: a tool for the visualization and management of care teams of complex pediatric patients. AMIA Annu Symp Proc 2017; 2017: 1458–67. [PMC free article] [PubMed] [Google Scholar]
- 19. Amir C, Grosz BJ, Gajos KZ, Swenson SM, Sanders LM, Amir O. From Care Plans to Care Coordination: Opportunities for Computer Support of Teamwork in Complex Healthcare. In: proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems; April 18, 2015; Seoul Republic of Korea.
- 20. Amir O, Grosz BJ, Gajos KZ, Swenson SM, Sanders LM. AI support of teamwork for coordinated care of children with complex conditions. In: proceedings of the 2014 AAAI Fall Symposium Series; September 24, 2014; Arlington, VA.
- 21. Kinzie MB, Cohn WF, Julian MF, Knaus WA.. A user-centered model for web site design needs assessment, user interface design, and rapid prototyping. J Am Med Informatics Assoc 2002; 9 (4): 320–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Simon TD, Cawthon ML, Popalisky J, Mangione-Smith R, Of C.. Excellence on quality of care measures for children with complex needs (COE4CCN). Development and validation of the pediatric medical complexity algorithm (PMCA) Version 2.0. Hosp Pediatr 2017; 7 (7): 373–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hsieh HF, Shannon SE.. Three approaches to qualitative content analysis. Qual Health Res 2005; 15 (9): 1277–88. [DOI] [PubMed] [Google Scholar]
- 24. Bates WD. Health information technology and care coordination: the next big opportunity for informatics? Yearb Med Inform 2015; 24 (01): 11–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Horsky J, Morgan SJ, Ramelson HZ.. Coordination of care for complex pediatric patients: perspectives from providers and parents. AMIA Annu Symp Proc 2014; 2014: 681–90. [PMC free article] [PubMed] [Google Scholar]
- 26. Peters KA, Green TF, Schumacher RM. Improving the user interface and adoption of online personal health records. In: proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2009; 53 (11): 704–8; Los Angeles, CA: SAGE Publications.
- 27. Flanagan ME, Saleem JJ, Millitello LG, Russ AL, Doebbeling BN.. Paper- and computer-based workarounds to electronic health record use at three benchmark institutions. J Am Med Informatics Assoc 2013; 20 (e1): e59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Koopman RJ, Steege LM, Moore JL, et al. Physician information needs and electronic health records (EHRs): time to reengineer the clinic note. J Am Board Fam Med 2015; 28 (3): 316–23. 1; [DOI] [PubMed] [Google Scholar]
- 29. Borbolla D, Taft T, Taber P, et al. Understanding primary care providers’ information gathering strategies in the care of children and youth with special health care needs. AMIA Annu Symp Proc 2018; 2018 (272). [PMC free article] [PubMed] [Google Scholar]
- 30. Zhao JY, Buer Song EA, Schwartz D, Panesar M, Jackson GP, Elkin PL.. Barriers, facilitators, and solutions to optimal patient portal and personal health record use: a systematic review of the literature. AMIA Annu Symp Proc 2017; 2017: 1913. [PMC free article] [PubMed] [Google Scholar]
- 31. Wright A, Feblowitz J, Maloney FL, Henkin S, Bates DW.. Use of an electronic problem list by primary care providers and specialists. J Gen Intern Med 2012; 27 (8): 968–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li RC, Garg T, Cun T, et al. Impact of problem-based charting on the utilization and accuracy of the electronic problem list. J Am Med Inform Assoc 2018; 25 (5): 548–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Adams S, Nicholas D, Mahant S, et al. Care maps for children with medical complexity. Dev Med Child Neurol 2017; 59 (12): 1299–306. [DOI] [PubMed] [Google Scholar]
- 34. Ranade-Kharkar P, Weir C, Norlin C, et al. Information needs of physicians, care coordinators, and families to support care coordination of children and youth with special health care needs (CYSHCN). J Am Med Inform Assoc 2017; 24 (5): 933–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rigby M, Georgiou A, Hyppönen H, et al. Patient portals as a means of information and communication technology support to patient-centric care coordination–the missing evidence and the challenges of evaluation. Yearb Med Inform 2015; 24 (01): 148–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Irizarry T, Dabbs AD, Curran CR.. Patient portals and patient engagement: a state of the science review. J Med Internet Res 2015; 17 (6): e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.