Abstract
Background:
Quadriceps weakness is a predictor of long-term knee function and strength recovery can vary from months to years after anterior cruciate ligament reconstruction (ACLR). However, few studies evaluate quadriceps strength and self-reported function within the first several weeks after ACLR.
Hypothesis/Purpose:
To examine changes over time in quadriceps strength symmetry, quadriceps peak torque, and self-reported knee function prior to and at six, 12, and 24 weeks post-ACLR. The hypotheses were 1) quadriceps strength symmetry, bilateral quadriceps peak torque, and patient-reported function would improve over time from pre-ACLR to 24 weeks post-ACLR and 2) significant improvements in patient-reported function, but not strength symmetry, would occur between time points.
Study Design:
Prospective, cohort study
Methods:
Thirty participants completed four testing sessions: pre-surgery and six, 12, and 24 weeks post-ACLR. Isometric quadriceps strength testing was performed at six weeks and isokinetic quadriceps strength was measured at all other testing points. Quadriceps index was calculated to evaluate between limb quadriceps strength symmetry. The Knee injury and Osteoarthritis Outcome Score (KOOS) and International Knee Documentation Committee Subjective Knee Evaluation Form (IKDC) were administered at each time point. A repeated-measures analysis of variance evaluated changes over time, with post-hoc comparisons to determine at which time-point significant changes occurred.
Results:
Quadriceps strength symmetry, involved limb quadriceps peak torque and all patient-reported outcome scores increased over time (p<0.02). Post-hoc tests showed that neither self-reported outcomes, nor quadriceps index improved between pre-surgery and six-weeks post-ACLR. From six to 12 weeks post-ACLR, scores on IKDC and KOOS Pain, Symptoms, Quality of Life, and Sport subscales improved (p≤0.003). From 12 to 24 weeks post-ACLR, quadriceps strength symmetry, involved limb quadriceps peak torque, KOOS-Symptoms, Quality of Life, and Sport subscales and the IKDC improved (p≤0.01). Uninvolved limb quadriceps peak torque did not change across any time point (p≥0.18).
Conclusion:
Patient-reported knee function increased between six and 24 weeks post-ACLR, while increases in involved limb quadriceps strength and quadriceps strength symmetry were not noted until 12-24 weeks post-ACLR.
Level of Evidence:
2b, individual cohort study
Keywords: Anterior Cruciate Ligament Reconstruction, Quadriceps Strength Symmetry, Self-Reported Outcomes, Movement System
INTRODUCTION
Tens of thousands of athletes every year suffer an anterior cruciate ligament (ACL) injury resulting in devastating functional outcomes.1 ACL reconstruction (ACLR) is the primary management strategy to restore knee joint stability and facilitate return to sports. Gait abnormalities, changes in neuromuscular activation patterns, loss of knee motion, and quadriceps muscle weakness are characteristic impairments after acute ACL injury.2-9 Even after ACLR and extensive, criterion-based rehabilitation, these impairments persist and can significantly inhibit high-level knee function.10-13
The acute loss of quadriceps strength is omnipresent following acute ACL rupture14,15 and is negatively associated with pre-operative10,11,16 and post-operative knee function.7,11,13,17,18 Quadriceps strength symmetry less than 85% are associated with reduced dynamic knee stability,10,13 reduced knee joint excursions and external knee flexion moments during gait,19-21 and poorer self-reported knee function.7,11,13 However, athletes who sustain unilateral ACLR demonstrate similar impairments on the contralateral limb, including decreased quadriceps strength22 and activation,23 lower knee extension moments during gait,24 and decreased performance on unilateral functional tasks.25-29 Therefore, additional attention to changes in individual limb strength changes may provide clarity in recovery of quadriceps strength symmetry.
Quadriceps weakness is a predictor of worse long-term knee function30,31 and strength recovery can vary from months to years after ACLR.10,17,18,32-34 Few studies evaluate quadriceps strength and self-reported function within the first several weeks after ACLR.35-37 The majority of current longitudinal data examine changes in strength and function after ACLR beginning three to six months post-operatively,10,11,16,19,38-41 and indicate that 27-52% of patients do not recover symmetrical quadriceps strength by six months post-operatively, with 12-21% not able to achieve strength symmetry milestones even 12 months after ACLR.16,42 Athletes who do not meet strength symmetry milestones may present with impaired knee biomechanics,19 dynamic knee function,13 and importantly, may be at risk for a second injury.43 Multiple studies have demonstrated that pre-operative quadriceps strength predicts post-operative outcomes7,30 and therefore, it is possible to consider that early quadriceps strength metrics post-ACLR may also affect long term post-operative outcomes. Due to the significant negative prognostic implications, further investigation of the recovery of quadriceps strength and knee-related function in the early post-operative phases of rehabilitation may help to identify individuals who are not meeting rehabilitation milestones and help prevent delayed quadriceps strength recovery. Additionally, patient perception of function does not always reflect knee function;44,45 therefore, early evaluation of these metrics may provide insight to patient's perception of knee function and help clinicians provide appropriate education during the early phase of recovery. The purpose of this study was to examine changes over time in quadriceps strength symmetry and knee-related function pre-operatively and at six, 12, and 24 weeks post-ACLR. The hypotheses were 1) quadriceps strength symmetry, bilateral quadriceps peak torque, and patient-reported function would improve over time from pre-ACLR to 24 weeks post-ACLR and 2) significant improvements in patient-reported function, but not strength symmetry, would occur between time points.
METHODS
Participants: Individuals with acute primary, unilateral ACL ruptures between the ages of 14-50 years were recruited from a larger randomized controlled trial for this prospective cohort study. The Ohio State University Human Subjects Review Board approved this study protocol and all eligible participants and/or guardians provided written informed consent. For the larger randomized controlled trial, ACL rupture was confirmed through positive Lachman, anterior drawer, or pivot shift tests and magnetic resonance imaging findings and participants were scheduled for ACLR. For this study, individuals were eligible if they participated in IKDC Level I/II cutting, pivoting, jumping, and lateral movement sports for at least 50 hours per year prior to their injury,46,47 and had no previous lower extremity or lumbar spine injury history. Individuals were excluded if they presented with the following concomitant injuries: contralateral ACL rupture, chondral defects requiring surgical treatment, or concurrent grade III ligamentous injuries.
Surgery and Post-Operative Rehabilitation: ACLR was performed by one of three sports medicine fellowship-trained surgeons in an ambulatory setting. Arthroscopic anatomic single bundle ACLR was performed using a hamstring autograft. Femoral fixation was achieved using a cortical button and tibial fixation was performed with an interference screw. Tourniquets were not used during the procedure. No post-operative bracing was used. Subjects initiated formal rehabilitation within one week of surgery. Rehabilitation was standardized using ACLR criterion-based rehabilitation guidelines based on the Multicenter Orthopedic Outcomes Network (MOON) recommendations.48-50 The rehabilitation guidelines in the acute phase of recovery focuses on reducing pain and effusion, restoring knee extension range of motion, initiating quadriceps activation and strength, and normalizing gait. Effusion management, quadriceps strengthening and restoration of full, symmetrical active knee range of motion continues through the sub-acute phase, while late phase rehabilitation focuses on power generation through quadriceps, hamstrings and gluteus musculature as well as incorporating unilateral dynamic stability tasks. Athletes were individually progressed through rehabilitation based on achievement of specific clinical criteria.
Quadriceps Strength Testing Procedures: The testing sessions were conducted at The Ohio State University Sports Medicine Research Institute and four testers were trained on the assessment protocols. Quadriceps strength was quantified with isometric and isokinetic dynamometry (Biodex System III, Biodex Medical Systems, Shirley, NY) with procedures shown to provide reliable and valid measures of quadriceps strength after ACL injury and ACLR.32,51,52 For this study, concentric isokinetic testing of the quadriceps (60 °/second) was used pre-ACLR and at 12 and 24 weeks post-ACLR to record peak torque (ft/lbs). In order to prevent excessive strain on the ACL graft at the 6-week post-ACLR testing session, isometric testing of the quadriceps with the knee flexed to 90 ° was used to measure peak volitional torque. Participant positioning was the same for both isokinetic and isometric testing procedures. Participants were seated on the dynamometer with the hips at 90 ° of flexion and pelvis secured with chest and waist straps, femoral straps secured the distal femur, and a tibial strap secured two finger-widths superior to the medial malleoli.
At six weeks post-ACLR, isometric quadriceps strength testing was performed with the knee fixed at 90 ° of flexion. Two practice test repetitions were performed prior to five test repetitions. Participants were verbally encouraged to “kick, kick, kick,” during each isometric contraction for five seconds with 20 seconds of rest between repetitions. Two test sets were performed, first on the uninvolved limb followed by the involved limb. The highest peak torque values from each limb were normalized to body weight and used to calculate quadriceps index (QI) [(involved limb peak torque/uninvolved limb peak torque) x 100%].
Isokinetic testing was performed at pre-ACLR and at 12 and 24 weeks post-ACLR. Participants were instructed to actively extend and flex the knee with maximal effort between 10 ° of knee extension to 100 ° of knee flexion “as hard and as fast” as they could. Two practice repetitions were conducted followed by two test sets consisting of five repetitions of knee flexion and extension at 60 °/second. Each test set was followed by 90 seconds of rest. This procedure was performed first on the uninvolved limb and then the involved limb. Testers provided strong verbal encouragement to the subject during each test to “kick, kick, kick,” during quadriceps activation to elicit maximal effort during extension repetitions. Quadriceps peak torque values were recorded for both test sets. For each test limb, the highest peak torque values of the two sets for knee extension was used in data analysis to represent the subject's best effort. The highest peak torque values from each limb were normalized to body weight and were used to calculate QI.
Self-Reported Outcome Measures: To measure knee-related function, two patient-reported outcome measures were administered at each testing session. The Knee injury and Osteoarthritis and Outcome Score (KOOS) evaluated knee-related function in the areas of symptoms and stiffness (Symptoms), pain (Pain), activities of daily living (ADL), sport and recreation (Sport), and quality of life (QOL) with each subset scored independently (0-100). The KOOS is a validated outcome measure for use with athletes after ACLR to document change in perceived function with higher scores representing higher functional status53 and was used to assess the different aspects of function after ALCR. The International Knee Documentation Committee Subjective Knee Evaluation Form (IKDC) evaluated knee-related function with higher scores indicating higher function (0-100). The IKDC is a validated and reliable functional outcome tool for athletes after ACLR as well as healthy individuals.54,55 The IKDC was administered in addition to the KOOS to capture values for overall knee-related function and for comparative analysis with currently published ACLR research.
STATISTICAL ANALYSIS
Mean and standard deviations were calculated for quadriceps peak torque for each limb, QI and all patient-reported outcomes at each time point (pre-operative, 6 weeks, 12 weeks, and 24 weeks post-ACLR). Repeated measures analysis of variance (ANOVA) determined whether mean values of quadriceps peak torque (pre-ACLR, 12 and 24 weeks post-ACLR only), QI, KOOS subscales and IKDC score changed over time. If appropriate, post-hoc testing was performed with paired t-tests to determine the time point at which significant changes in quadriceps peak torque, QI, KOOS, and IKDC occurred. Statistical significance was defined as a p-value less than 0.05, with adjustments made for multiple comparisons using a Bonferroni correction. Effect sizes (ES) were also calculated at each time point (small d=0.2; medium: d=0.5; large: d=0.8).56 All available data were used in the analysis of change over time, including early time point data from subjects lost to later follow-up.
Required sample size was estimated a priori using G-power 3.1 (http://www.psycho.uni-duesseldorf.de/abteilungen/aap/gpower3/) and previous work36 reporting early changes in patient-reported function post-ACLR. Using an alpha level of 0.05 and desired power of 0.90, 16 subjects were needed to demonstrate significant change over time in patient-reported function.
RESULTS
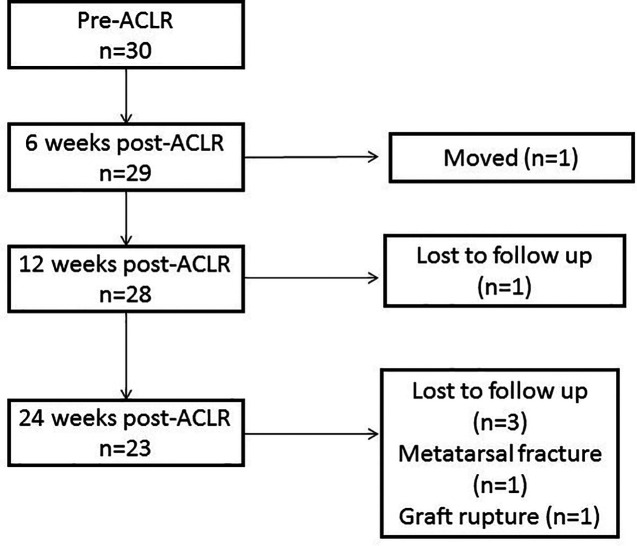
Thirty individuals (Table 1) participated. Over the course of the study, seven participants missed at least one testing session and 23 participants (76.7%) completed all testing time-points (Figure 1).
Table 1.
Subject Demographics.
| Subjects | N=30 |
|---|---|
| Sex | 20 males 10 females |
| Age (year) | 22.2 ± 9.1 |
| Height (meters) | 1.7 ± 0.1 |
| Weight (kilograms) | 77.8 ± 15.7 |
| Body Mass Index (kilograms/meter²) | 26.3 ± 4.9 |
| Time from Injury to ACLR (months) | 2.2 ± 3.4 |
| Time from Pre-ACLR testing to ACLR (days) | 2.5 ± 1.9 |
ACLR = Anterior cruciate ligament reconstruction
Figure 1.
Participation flow chart.
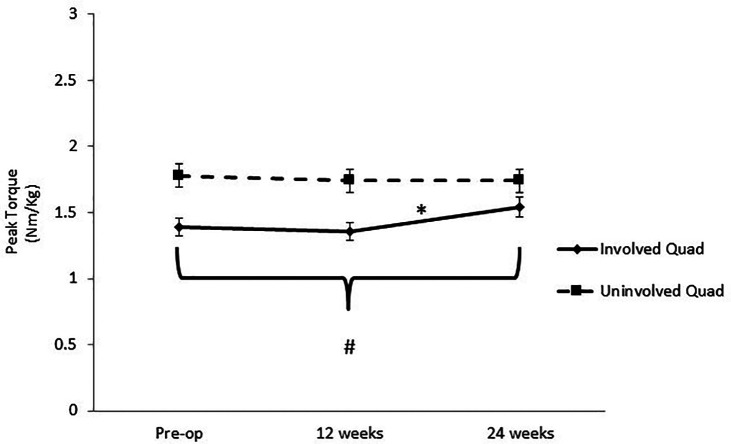
Quadriceps Peak Torque (Table 2, Figure 2): Six-week data were not included in this analysis given the different testing modes (isokinetic versus isometric) and impact on peak torque. From pre-ACLR to 24 weeks post-ACLR, involved quadriceps peak torque improved (p = 0.019). There was no change in involved quadriceps peak torque from pre-ACLR to 12 weeks post-ACLR (1.39-1.36 Nm/Kg, p = 0.59). Involved limb quadriceps peak torque significantly increased from pre-ACLR to 24 weeks post-ACLR (1.39 to 1.54 Nm/Kg; p=0.03; ES=0.30) and from 12 to 24 weeks post-ACLR (1.36-1.54 Nm/Kg; p=0.01; ES=0.35). There was no significant change in uninvolved limb quadriceps peak torque over time (p = 0.57).
Table 2.
Strength and patient-reported function from pre-ACLR to 24 weeks post-ACLR.
| Pre-ACLR (n=30) | Six weeks post-ACLR (n=29) | 12 weeks post-ACLR (n=28) | 24 weeks post-ACLR (n=23) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | % of participants at 90 | Mean ± SD | % of participants at 90 | Mean ± SD | % of participants at 90 | Mean ± SD | % of participants at 90 | |
| Involved QF PT (Nm/kg) | 1.390 ± 0.48 | 1.36 ± 0.60 | 1.36 ± 0.52 | 1.54 ± 0.52 β | ||||
| Uninvolved QF PT (Nm/kg) | 1.78 ± 0.43 | 1.96 ± 0.54 | 1.74 ± 0.47 | 1.74 ± 0.45 | ||||
| QI (%) | 78 ± 21 | 23 | 71 ± 27 | 10 | 74 ± 19 | 18 | 84 ± 19β | 44 |
| KOOS Pain | 74.7 ± 11.1 | 7 | 79.1 ± 13.7 | 14 | 89.0 ± 11* | 50 | 93.0 ± 16.8 | 74 |
| KOOS Symptoms | 67.5 ± 18.9 | 3 | 68.7 ± 15.5 | 4 | 81.3 ± 13.7* | 15 | 89.1 ± 8.9 | 48 |
| KOOS ADL | 87.0 ± 9.4 | 53 | 92.3 ± 8.7 | 71 | 96.8 ± 6.0 | 96 | 98.9 ± 2.3 | 100 |
| KOOS Sport | 50.6 ± 19.4 | 3 | 49.3 ± 18.2 | 4 | 73.2 ± 17.8* | 32 | 83.0 ± 20.5 β | 61 |
| KOOS QOL | 44.3 ± 18.4 | 0 | 46.9 ± 21.9 | 0 | 58.3 ± 20.2 * | 4 | 67.9 ± 22.3 β | 22 |
| IKDC | 55.4 ± 13.4 | 0 | 60.1 ± 11.6 | 0 | 73.6 ± 11.9* | 11 | 85.3 ± 12.3 β | 52 |
ACLR = anterior cruciate ligament reconstruction; SD = standard deviation; QF = quadriceps femoris muscles; PT = peak torque; QI = Quadriceps Index; KOOS = Knee injury and Osteoarthritis Outcomes Score; ADL = activities of daily living; QOL = quality of life; IKDC = International Knee Documentation Committee Subjective Knee Form.
Significant changes between 6 to 12 weeks. βSignificant change between 12-24 weeks
Figure 2.
Changes in Quadriceps Peak Torque Over Time. Changes in quadriceps peak torque (Newton Meters/Kilogram) for involved and uninvolved limb from pre-ACLR to 24 weeks post-ACLR. *Significant changes in quadriceps peak torque between adjacent time points (p≤0.05)
# Significant change in involved quadriceps peak torque from pre-ACLR to 24 weeks post-ACLR (p≤0.05).
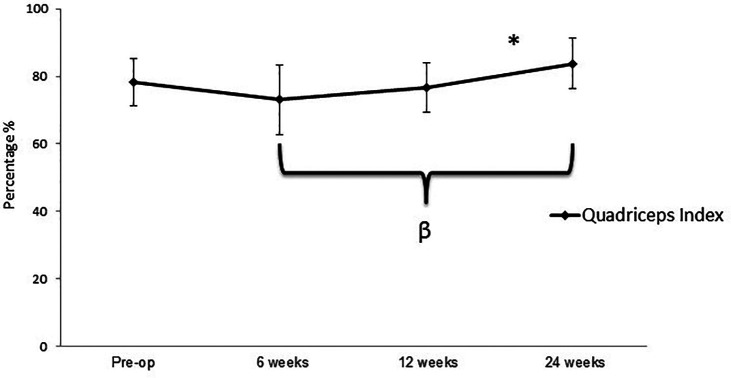
Quadriceps Strength Symmetry (Table 2, Figure 3): Across all study visits, QI improved over time (p<0.0001) and at final follow-up was an average of 84 ± 19%. Post-hoc analysis showed that QI did not improve from pre-ACLR (78 ± 21%) to six weeks post-ACLR (71 ± 27%; p = 0.17) or from six to 12 weeks post-ACLR (74 ± 19%; p = 0.65). At six- and 12-weeks post-ACLR, 10% and 18% of participants, respectively, met 90% QI indicating nearly symmetrical quadriceps strength symmetry. A significant increase in QI was observed from 12 weeks to 24 weeks post-ACLR (p = 0.005; ES = 0.53), with 44% of participants demonstrating 90% QI at 24 weeks post-ACLR. Mean QI at 24 weeks post-ACLR was not different from the mean pre-operative QI (p=0.057).
Figure 3.
Changes in Quadriceps Index over time. Changes in QI Over Time. Changes in Quadriceps Index (QI) from pre-ACLR to 24 weeks post-ACLR. β Significant change from six weeks post-ACLR to 24 weeks post-ACLR. (p ≤ 0.005), *Significant changes in QI denoted from 12 to 24 weeks post-ACLR (p ≤ 0.005).
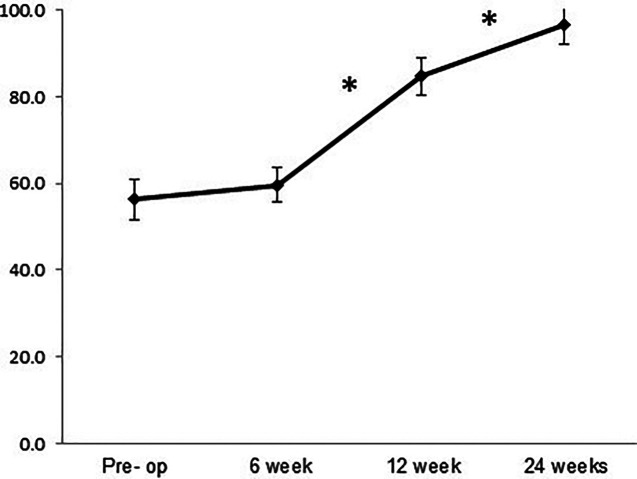
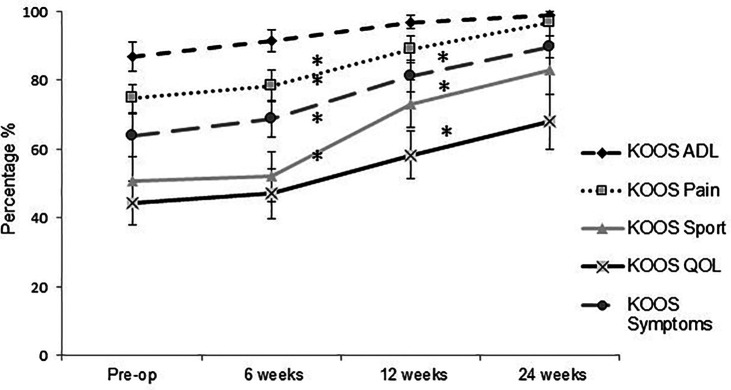
Self-Reported Outcomes (Table 2, Figures 4 and 5): The KOOS subscales and IKDC score improved over time (p≤0.0001). Post-hoc analysis showed that IKDC score and KOOS subscales did not change between the pre-operative and 6-week post-ACLR time points (p ≥ 0.6). Significant improvements were observed from six to 12 weeks post-ACLR in IKDC scores (p≤0.0001; ES = 1.2) and KOOS-Pain (p=0.003; ES=0.80), Symptoms (p=0.0002; ES=0.86), QOL (p=0.003; ES = 0.54) and Sport subscales (p=0.0001; ES = 1.7). From the 12 to 24-week time points, scores improved on the IKDC (p≤0.0001; ES=0.97), KOOS-Symptoms (p=0.0001; ES=0.68), QOL (p=0.001; ES=0.45), and Sport (p=0.001; ES=0.97). IKDC scores and all KOOS subscales improved from pre-ACLR to 12-weeks post-ACLR (p≤0.001), from six to 24-weeks post-ACLR (p≤0.001) and from pre-ALCR to 24 weeks post-ACLR (p≤0.001).
Figure 4.
Changes in the International Knee Documentation Committee subjective knee form from pre-ACLR to 24 weeks post-ACLR. *Significant changes denoted between six and 12 weeks and 12 and 24 weeks post-ACLR (p ≤ 0.001).
Figure 5.
Changes in the Knee injury and Osteoarthritis Outcomes Score over time. Changes in Knee Injury and Osteoarthritis Outcomes Score (KOOS)-Activities of Daily Living (ADL), Pain, Sport, Quality of Life (QOL) and symptoms subscales from pre-ACLR to 24 weeks post-ACLR; *Significant changes in KOOS- Pain subscales from six to 12 weeks (p = 0.003); *Significant changes in KOOS-Symptoms, Sport and QOL subscales (p ≤ 0.002)
DISCUSSION
The purpose of this study was to evaluate the changes in quadriceps strength symmetry, bilateral quadriceps peak torque, and knee-related function prior to ACLR and at six, 12, and 24 weeks post-ACLR. The hypothesis was that quadriceps peak torque, quadriceps symmetry, and self-reported knee function would improve over time and significant improvement in patient-reported knee function, but not strength symmetry, would be observed at each time point. Consistent with the study hypothesis, all variables improved over time. Significant improvements in patient-reported knee function occurred from six to 12 weeks and 12 to 24 weeks post-ACLR while improvements in quadriceps symmetry did not occur until the 12-24-week time point.
The loss of quadriceps strength is pervasive after ACL injury.14,15 The vast majority of literature begins to evaluate strength at 24 weeks post-ACLR10,16,38,57,58 while little is known about quadriceps recovery in the early post-operative phase. Only two other studies35,37 have evaluated changes in strength in the first three months after ACLR. In this cohort, there were no significant improvements in QI from pre-ACLR to six weeks post-ACLR or six to 12 weeks post ACLR. Similarly, quadriceps peak torque did not improve from pre-ACLR to 12 weeks post-ACLR. Harput et al.37 observed significant improvements in involved quadriceps strength at four, eight and 12 weeks post-ACLR with significant improvements in QI between four and eight weeks but not between eight and 12 weeks post-ACLR. Similarly, Chmielewski et al.35 observed QI improvements between one and six weeks post-ACLR but not between six and 12 weeks post-ACLR. Varied restoration of quadriceps strength after ACLR makes it difficult to predict timelines for full recovery.10,17,18,33,34 The lack of progressive improvement is interesting considering rehabilitation efforts focus on improving quadriceps strength during this time frame. This may indicate that rehabilitation efforts during this phase of recovery are insufficient or it may represent the slower natural recovery of the quadriceps muscle following ACLR. These findings are remarkable considering recent studies indicate that joint loading and joint mechanics are altered with QI scores less than 80% and 85% respectively.19 The mean QI at 12 weeks post-ACLR for our cohort was 74%. Therefore, initiation of high impact activities, which typically occurs during this time frame,59,60 may not be appropriate for some athletes in our cohort. This highlights the importance of objectively measuring quadriceps strength during early rehabilitation to better direct rehabilitation.
Limb symmetry indexes are routinely used to determine when sufficient quadriceps strength has been restored in the involved limb. However, deficits in the uninvolved limb after ACLR have been documented in the literature.22,24,26,27,29,61 In this cohort, uninvolved limb quadriceps strength did not change over time which is not consistent with other literature. Harput et al.37 found significant improvement in uninvolved limb quadriceps strength between four, eight, and 12 weeks post-ACLR. Thomee et al.62 evaluated involved and uninvolved quadriceps power at pre-ACLR, six, 12 and 24 months post-ACLR and demonstrated asymmetrical quadriceps power recovery between limbs over time. In this cohort, improvements in involved limb quadriceps strength mimicked improvements in QI and uninvolved limb peak torque did not significantly change over time. However, the inability to compare strength measures at six weeks to adjacent time points due to change in strength testing mode, may explain why uninvolved limb strength changes were not observed. The varied results in the literature continue to make clinical decision making difficult for rehabilitation specialists. However, a recent study by Wellsdandt et al63 utilized pre-ACLR strength values of the uninvolved limb at all strength testing time points to calculate QI which better predicted second ACL injury. Results of this study demonstrated that this method of comparison may eliminate the variability in uninvolved limb strength recovery and improve the clinician's ability to determine if sufficient involved limb strength has been restored. If pre-ACLR data is not available, utilizing age, sex, and gender-matched normative values should be considered as well.
Studies examining the changes in knee-related function early in the post-ACLR rehabilitation process are limited. Contrary to the study hypothesis, participants did not demonstrated improvements in patient-reported function from pre-ACLR to six weeks post-ACLR which may be due to the additional joint trauma that is incurred with surgery.64 However, this cohort six and 12 week data are consistent with work by Chmielewski et al.65 who reported significant improvements in the Global Rating score (GRS) between six and 12 weeks post-ACLR and Christensen et al.36 who reported significant improvements in IKDC scores at four and eight weeks post-ACLR. Consensus on what is considered a successful outcome after ACLR is lacking. Patient-reported knee function scores between 85 and 90 have been recommended in the literature.66 In this cohort, KOOS- Pain, Symptoms, ADL subscales and IKDC scores met the recommended threshold, which is consistent with other six-month post-ACLR literature.16,44,58 Hartigan et al.16 reported scores on the Knee Outcome Survey Activities of Daily Living (KOS-ADL) and Global Rating Scale of Perceived Knee Function (GRS) greater than 90 and Logerstedt et al.58 reported scores of 97, 93 and 87 on the KOS-ADL, GRS, and IKDC respectively. In this cohort, KOOS-Sport and QOL subscales (83 and 68 respectively) did not meet the recommended threshold. This is consistent with work by Ingelsrud et al.,44 who found that subjects who perceived their symptoms as “acceptable” at six months had KOOS Sport and QOL subscales of 69 and 72, respectively. This may indicate that what an athlete feels is acceptable may not be consistent with what medical practitioners deem as acceptable which reinforces the need to use multiple metrics to determine progression of activity and return to sport.
Variation in quadriceps recovery and patient-reported knee function scores demonstrate that not all aspects of the athletes’ function recover at the same rate after ACLR. This cohort further illustrates this as the percentage of athletes that reach recovery milestones varies between each outcome measure. Less than 50% of this cohort achieved QI of 90% at six months post-ACLR while the percentage of athletes scoring >90 on the KOOS Sport and IKDC were 61% and 52% respectively. The only outcome measure in which 100% of the cohort achieved 90% was the KOOS-ADL.
Understanding the progression of strength and self-reported knee function in the first six months after ACLR is imperative to directing post-operative rehabilitation and patient expectations. Additionally, these data support other studies67,68 reporting that current rehabilitation efforts to restore symmetry may be inadequate and that modifications to rehabilitation guidelines may be necessary in order to maximize quadriceps strength recovery. Objective and serial strength testing early in the rehabilitation process may be beneficial to quickly identify athletes who are not meeting strength milestones and establish a more rigorous set of guidelines to augment the timing of quadriceps recovery. This would direct rehabilitation specialist to modify treatment in order to prevent prolonged muscle weakness and delayed recovery of long-term function. More focused quadriceps strengthening including neuromuscular electrical stimulation and isolated progressive resistive quadriceps exercises may continue to be necessary during this timeframe. Furthermore, the significant improvement in patient-reported knee function from six to 12 and 12 to 24 weeks post-ACLR and the delayed improvements in strength symmetry, reinforce the concept that even though an athlete may perceive a high level of function, it does not mean that they demonstrate resolution of impairments or other deficits. Specific patient education should be provided to prevent inappropriate knee joint stress and to establish appropriate patient expectations.
There are several limitations to this study. In order to capture and compare quadriceps strength changes at six weeks post-ACLR, isometric testing was utilized to protect the graft. There are limitations in comparing isokinetic and isometric testing; therefore, individual limb strength comparisons were not included in this analysis, but felt quadriceps strength symmetry metrics were valuable to the study. Quadriceps strength continues to improve beyond six months after ACLR10 but this analysis did not assess QI or self-reported knee function beyond this time point; therefore this analysis does not provide a complete illustration of quadriceps and functional recovery as it relates to return to sport success or long-term knee function. Finally, there was loss of participants during the follow-up period, particularly at the final 24-week follow-up. This attrition has some potential to bias the results at this time point, but the relatively consistent findings with prior time points make this unlikely.
CONCLUSIONS
This study focused on evaluating quadriceps strength and functional recovery early in the rehabilitation process. Based on these results, there are no changes in quadriceps peak torque and quadriceps symmetry from pre-ACLR to 12 weeks post-ACLR. However, patient-reported knee function improves as early as six weeks post-ACLR. Specifically, significant improvements were observed in KOOS-Pain, Symptoms, Sport, QOL subscales and IKDC scores. Continued examination of the association between quadriceps strength and patient-reported knee function in this early post-operative time-frame may provide valuable insight to long-term recovery variability. Specifically, additional research to determine if early quadriceps strength metrics predict post-operative outcomes at six and 12 months post-ACLR is warranted.
REFERENCES
- 1.Biau DJ Tournoux C Katsahian S, et al. ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res. 2007;458:180-187. [DOI] [PubMed] [Google Scholar]
- 2.Daniel DM Fithian DC. Indications for ACL surgery. Arthroscopy. 1994;10(4):434-441. [DOI] [PubMed] [Google Scholar]
- 3.Hartigan E Axe MJ Snyder-Mackler L. Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. J Orthop Res. 2009;27(6):724-729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berchuck M Andriacchi TP Bach BR, et al. Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am. 1990;72(6):871-877. [PubMed] [Google Scholar]
- 5.Rudolph KS Eastlack ME Axe MJ, et al. 1998 Basmajian Student Award Paper: Movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8(6):349-362. [DOI] [PubMed] [Google Scholar]
- 6.Rudolph KS Axe MJ Buchanan TS, et al. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):62-71. [DOI] [PubMed] [Google Scholar]
- 7.Eitzen I. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43(5):371-376. [DOI] [PubMed] [Google Scholar]
- 8.Williams GN Buchanan TS Barrance PJ, et al. Quadriceps weakness, atrophy, and activation failure in predicted noncopers after anterior cruciate ligament injury. Am J Sports Med. 2005;33(3):402-407. [DOI] [PubMed] [Google Scholar]
- 9.McHugh MP Tyler TF Gleim GW, et al. Preoperative indicators of motion loss and weakness following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1998;27(6):407-411. [DOI] [PubMed] [Google Scholar]
- 10.de Jong SN van Caspel DR van Haeff MJ, et al. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23(1):21-28, 28 e21-23. [DOI] [PubMed] [Google Scholar]
- 11.Logerstedt D Grindem H Lynch A, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: The Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40(10):2348-2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roewer BD Di Stasi SL Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech. 2011;44(10):1948-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmitt LC Paterno MV Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hart JM Pietrosimone B Hertel J, et al. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45(1):87-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lynch AD Logerstedt DS Axe MJ, et al. Quadriceps activation failure after anterior cruciate ligament rupture is not mediated by knee joint effusion. J Orthop Sports Phys Ther. 2012;42(6):502-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hartigan EH Axe MJ Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bush-Joseph CA Hurwitz DE Patel RR, et al. Dynamic function after anterior cruciate ligament reconstruction with autologous patellar tendon. Am J Sports Med. 2001;29(1):36-41. [DOI] [PubMed] [Google Scholar]
- 18.Mattacola CG Perrin DH Gansneder BM, et al. Strength, Functional Outcome, and Postural Stability After Anterior Cruciate Ligament Reconstruction. J Athl Train. 2002;37(3):262-268. [PMC free article] [PubMed] [Google Scholar]
- 19.Lewek M Rudolph K Axe M, et al. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech. 2002;17(1):56-63. [DOI] [PubMed] [Google Scholar]
- 20.Patel RR Hurwitz DE Bush-Joseph CA, et al. Comparison of clinical and dynamic knee function in patients with anterior cruciate ligament deficiency. Am J Sports Med. 2003;31(1):68-74. [DOI] [PubMed] [Google Scholar]
- 21.Snyder-Mackler L Ladin Z Schepsis AA et al. Electrical stimulation of the thigh muscles after reconstruction of the anterior cruciate ligament. Effects of electrically elicited contraction of the quadriceps femoris and hamstring muscles on gait and on strength of the thigh muscles. J Bone Joint Surg Am. 1991;73(7):1025-1036. [PubMed] [Google Scholar]
- 22.Hiemstra LA Webber S MacDonald PB, et al. Contralateral limb strength deficits after anterior cruciate ligament reconstruction using a hamstring tendon graft. Clin Biomech. 2007;22(5):543-550. [DOI] [PubMed] [Google Scholar]
- 23.Urbach D Nebelung W Becker R, et al. Effects of reconstruction of the anterior cruciate ligament on voluntary activation of quadriceps femoris a prospective twitch interpolation study. J Bone Joint Surg Br. 2001;83(8):1104-1110. [DOI] [PubMed] [Google Scholar]
- 24.Dl Stasi S Hartigan EH Snyder-Mackler L. Sex-Specific Gait Adaptations Prior to and up to 6 Months After Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther. 2015;45(3):207-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamazaki J Muneta T Ju YJ, et al. Differences in kinematics of single leg squatting between anterior cruciate ligament-injured patients and healthy controls. Knee Surgery, Sports Traumatol Arthrosc. 2010;18(1):56-63. [DOI] [PubMed] [Google Scholar]
- 26.Clagg S Paterno MV, Hewett TE, et al. Performance on the modified star excursion balance test at the time of return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015:1-25. [DOI] [PubMed] [Google Scholar]
- 27.Paterno MV Schmitt LC Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zult T Gokeler A van Raay JJ, et al. An anterior cruciate ligament injury does not affect the neuromuscular function of the non-injured leg except for dynamic balance and voluntary quadriceps activation. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):172-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goerger BM Marshall SW Beutler AI, et al. Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: the JUMP-ACL study. Br J Sports Med. 2015;49(3):188-195. [DOI] [PubMed] [Google Scholar]
- 30.Logerstedt D Lynch A Axe MJ, et al. Pre-operative quadriceps strength predicts IKDC2000 scores 6months after anterior cruciate ligament reconstruction. Knee. 2013;20(3):208-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McHugh MP Tyler TF Browne MG, et al. Electromyographic predictors of residual quadriceps muscle weakness after anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30(3):334-339. [DOI] [PubMed] [Google Scholar]
- 32.Jarvela T Kannus P Latvala K, et al. Simple measurements in assessing muscle performance after an ACL reconstruction. Int J Sports Med. 2002;23(3):196-201. [DOI] [PubMed] [Google Scholar]
- 33.Kobayashi A Higuchi H Terauchi M, et al. Muscle performance after anterior cruciate ligament reconstruction. Int Orthop. 2004;28(1):48-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Risberg MA Holm I. The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: A randomized controlled clinical trial with 2 years of follow-up. Am J Sports Med. 2009;37(10):1958-1966. [DOI] [PubMed] [Google Scholar]
- 35.Chmielewski TL Wilk KE Snyder-Mackler L. Changes in weight-bearing following injury or surgical reconstruction of the ACL: relationship to quadriceps strength and function. Gait Posture. 2002;16(1):87-95. [DOI] [PubMed] [Google Scholar]
- 36.Christensen JC Goldfine LR Barker T, et al. What can the first 2 months tell us about outcomes after anterior cruciate ligament reconstruction? J Athl Train. 2015;50(5):508-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harput G Kilinc HE Ozer H, et al. Quadriceps and hamstring strength recovery during early neuromuscular rehabilitation after ACL hamstring-tendon autograft reconstruction. J Sport Rehabil. 2015;24(4):398-404. [DOI] [PubMed] [Google Scholar]
- 38.Keays SL Bullock-Saxton J Keays AC. Strength and function before and after anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2000(373):174-183. [DOI] [PubMed] [Google Scholar]
- 39.Keays SL Bullock-Saxton J Keays AC, et al. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. Knee. 2001;8(3):229-234. [DOI] [PubMed] [Google Scholar]
- 40.Keays SL Bullock-Saxton JE Newcombe P, et al. The relationship between knee strength and functional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21(2):231-237. [DOI] [PubMed] [Google Scholar]
- 41.Lee JC Kim JY Park GD. Effect of 12 weeks of accelerated rehabilitation exercise on muscle function of patients with ACL reconstruction of the knee joint. J Phys Ther Sci. 2013;25(12):1595-1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Logerstedt D Lynch A Axe M, et al. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatol Arthrosc. 2013;21(4):859-868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grindem H Snyder-Mackler L Moksnes H, et al. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ingelsrud LH Granan LP Terwee CB, et al. Proportion of patients reporting acceptable symptoms or treatment failure and their associated KOOS values at 6 to 24 months after anterior cruciate ligament reconstruction: A study from the Norwegian knee ligament registry. Am J Sports Med. 2015;43(8):1902-1907. [DOI] [PubMed] [Google Scholar]
- 45.Ardern CL Taylor NF Feller JA, et al. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41(7):1549-1558. [DOI] [PubMed] [Google Scholar]
- 46.Daniel DM Stone ML Dobson BE, et al. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22(5):632-644. [DOI] [PubMed] [Google Scholar]
- 47.Hefti F Muller W Jakob RP, et al. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226-234. [DOI] [PubMed] [Google Scholar]
- 48.Kruse LM Gray B Wright RW. Rehabilitation after anterior cruciate ligament reconstruction: A systematic review. J Bone Joint Surg. 2012;94(19):1737-1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wright RW Preston E Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part II: open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. J Knee Surg. 2008;21(3):225-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wright RW Preston E Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part I: continuous passive motion, early weight bearing, postoperative bracing, and home-based rehabilitation. J Knee Surg. 2008;21(3):217-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilk KE Romaniello WT Soscia SM, et al. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20(2):60-73. [DOI] [PubMed] [Google Scholar]
- 52.Brosky JA Jr. Nitz AJ Malone TR, et al. Intrarater reliability of selected clinical outcome measures following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29(1):39-48. [DOI] [PubMed] [Google Scholar]
- 53.Roos EM Roos HP Lohmander LS, et al. Knee injury and osteoarthritis outcome score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88-96. [DOI] [PubMed] [Google Scholar]
- 54.Irrgang JJ Anderson AF Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600-613. [DOI] [PubMed] [Google Scholar]
- 55.Irrgang JJ Anderson AF Boland AL, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34(10):1567-1573. [DOI] [PubMed] [Google Scholar]
- 56.Cohen J. A power primer. Psychol Bull. 1992;112(1):155-159. [DOI] [PubMed] [Google Scholar]
- 57.Di Stasi SL Logerstedt D Gardinier ES, et al. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310-1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Logerstedt D Lynch A Axe MJ, et al. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2013;21(4):859-868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cascio BM Culp L Cosgarea AJ. Return to play after anterior cruciate ligament reconstruction. Clin Sports Med. 2004;23(3):395-408, ix. [DOI] [PubMed] [Google Scholar]
- 60.Marx RG Jones EC Angel M, et al. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19(7):762-770. [DOI] [PubMed] [Google Scholar]
- 61.Yamazaki J Muneta T Ju YJ, et al. Differences in kinematics of single leg squatting between anterior cruciate ligament-injured patients and healthy controls. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):56-63. [DOI] [PubMed] [Google Scholar]
- 62.Thomeé R Kaplan Y Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798-1805. [DOI] [PubMed] [Google Scholar]
- 63.Wellsandt E Failla MJ Snyder-Mackler L. Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2017;47(5):334-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Palmieri-Smith RM Thomas AC Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27(3):405-424. [DOI] [PubMed] [Google Scholar]
- 65.Chmielewski TL. Asymmetrical lower extremity loading after ACL reconstruction: more than meets the eye. J Orthop Sports Phys Ther. 2011;41(6):374-376. [DOI] [PubMed] [Google Scholar]
- 66.Lynch AD Logerstedt DS Grindem H, et al. Consensus criteria for defining ‘successful outcome’ after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2015;49(5):335-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hartigan EH Axe MJ Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Logerstedt D Di Stasi S Grindem H, et al. Self-reported knee function can identify athletes who fail return-to-activity criteria up to 1 year after anterior cruciate ligament reconstruction: A Delaware-Oslo ACL cohort study. J Orthop Sports Phys Ther. 2014;44(12):914-923. [DOI] [PMC free article] [PubMed] [Google Scholar]