Abstract
Background:
The gluteus medius (GMed) and gluteus minimus (GMin) muscle segments demonstrate different responses to pathology and ageing, hence it is important in rehabilitation that prescribed therapeutic exercises can effectively target the individual segments with adequate exercise intensity for strengthening.
Purpose:
The purpose of this systematic review was to evaluate whether common therapeutic exercises generate at least high ( > 40% maximum voluntary isometric contraction (MVIC)) electromyographic (EMG) activity in the GMed (anterior, middle and posterior) and GMin (anterior and posterior) segments.
Methods:
Seven databases (MEDLINE, EMBASE, CINAHL, AusSPORT, PEDro, SPORTdiscus and Cochrane Library) were searched from inception to May 2018 for terms relating to gluteal muscle, exercise, and EMG. The search yielded 6918 records with 56 suitable for inclusion. Quality assessment, data extraction and data analysis were then undertaken with exercise data pooled into a meta-analysis where two or more studies were available for an exercise and muscle segment.
Results:
For the GMed, different variations of the hip hitch/ pelvic drop exercise generated at least high activity in all segments. The dip test, and isometric standing hip abduction are other options to target the anterior GMed segment, while isometric standing hip abduction can be used for the posterior GMed segment. For the middle GMed segment, the single leg bridge; side-lying hip abduction with hip internal rotation; lateral step-up; standing hip abduction on stance or swing leg with added resistance; and resisted side-step were the best options for generating at least high activity. Standing isometric hip abduction and different variations of the hip hitch/ pelvic drop exercise generated at least high activity in all GMin segments, while side-lying hip abduction, the dip test, single leg bridge and single leg squat can also be used for targeting the posterior GMin segment.
Conclusion:
The findings from this review provide the clinician with confidence in exercise prescription for targeting individual GMed and GMin segments for potential strengthening following injury or ageing.
Level of Evidence:
Level 1.
What is known about the subject:
Previous reviews on GMed exercises have been based on single electrode, surface EMG measures at middle GMed segment. It is not known whether these exercises effectively target the other segments of GMed or the GMin at a sufficient intensity for strengthening.
What this study adds to existing knowledge:
This review provides the clinician with confidence in exercise prescription of common therapeutic exercises to effectively target individual GMed and GMin segments for potential strengthening.
Keywords: EMG, gluteal muscle, hip, exercise therapy, movement system
INTRODUCTION
Gluteal muscle dysfunction is associated with pain and symptoms at the ankle,1-3 knee,4-6 hip,7-9 and lower back.10,11 There is also evidence that severity of symptoms on clinical presentation is associated with atrophied or weak muscles.12,13 It is therefore important to understand the most effective methods of activating the gluteal muscles with therapeutic exercise for the purpose of strengthening these muscles in clinical populations.14-16
The effectiveness of hip strengthening programs for improving symptoms and quality of life in clinical conditions is variable. While there are clear benefits of hip strengthening exercises for conditions of the knee,17 results for conditions such as hip osteoarthritis are less convincing with only mild benefits in the short term.18 Two reasons that may account for variable effects are; (1) the exercises used in typical rehabilitation programs may not activate the muscles with sufficient intensity to elicit strength and/or hypertrophic adaptations, or (2) the exercises typically prescribed may not target individual segments of gluteus medius (GMed) and gluteus minimus (GMin) and/or with sufficient intensity. These muscles consist of distinct individual segments (anterior, middle and posterior for GMed; and anterior and posterior for GMin) with separate innervations, different muscle fiber orientations, and diverse functional roles.19-21 In addition to generalized muscle atrophy of GMin and GMed in clinical presentations such as hip osteoarthritis,22 gluteal tendinopathy,23 and following total hip replacement,24,25 there is evidence of specific segmental atrophy and dysfunction.24-26 Understanding the role of exercises for targeting individual muscle segments of GMin and GMed may enable better tailoring of exercise interventions to people with varied underlying presentations, or those for specific conditions.
There are a number of reviews27-31 that have reported GMed activity levels for various therapeutic exercises but have mostly contained studies that utilize a single surface electrode positioned over the middle GMed segment to record electromyographic (EMG) activity. No previous reviews have considered exercises to target the individual segments of the GMed, and none have examined therapeutic exercises for the GMin. An updated systematic review will inform clinicians of the effectiveness of exercises targeting individual GMed and GMin segments.
The purpose of this systematic review was to evaluate whether common therapeutic exercises generate at least high ( > 40% maximum voluntary isometric contraction (MVIC)) electromyographic (EMG) activity in the GMed (anterior, middle and posterior) and GMin (anterior and posterior) segments.
METHODS
Search strategy
This review was conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) statement guidelines32 A systematic literature search was conducted of MEDLINE, CINAHL, EMBASE, AUSPORT, SPORTDiscus, PEDRO and the Cochrane Library from inception to first week May 2018. These databases were searched using free-text words, keywords mapped to medical subject headings (MeSH), and filters were applied for human subjects where possible. Boolean operators were used to combine the key words with truncated search terms: (glut* OR buttock* OR hip rotat* OR hip abduct*) AND (strength* OR contract* OR electromyo* OR EMG OR electrode* OR activ* OR intensit* OR peak amplitude* OR funct*)
Further relevant studies were searched through reference scanning of included full-text studies.
From the initial search yield, articles were imported into Endnote version X8, duplicate papers were removed, and the abstracts and titles of the remaining papers were screened by two reviewers (DM and TP) independently through application of the inclusion and exclusion criteria. Full-text was obtained for the remaining studies to determine eligibility for inclusion into the review through consultation and consensus between the reviewers (DM and TP).
Inclusion and Exclusion Criteria
Inclusion and exclusion criteria were determined prior to administering the search strategy. Since most studies in this area of research are either cross-sectional or single-group pre- and post-test design, all study designs were eligible for inclusion except clinical commentary or opinion articles, and unpublished material such as theses, abstracts, and conference proceedings.
Studies comprising of only healthy participants were included in this review. A study with pathological participants was only included if there was a group of healthy controls with separate data presented.
Normalized muscle activity measured using surface or intramuscular EMG was selected as the outcome measure of interest since it has been long established and universally advocated as the method of choice in measuring and comparing muscle activity between different exercises and individuals.33-36 To be included, studies had to normalize EMG to a MVIC since this has been found to be the most reliable method for comparing exercises for the GMed in healthy participants37 and is clinically interpretable. This also allows a more meaningful comparison between studies and a logical synthesis of findings.
Due to the vast breadth of studies that have evaluated exercises for the GMed, only studies that evaluated the GMed and / or the GMin, and contained at least one commonly evaluated therapeutic exercise (including squats, lunges, steps, hip hitches, standing hip abduction, supine bridges, side lie hip abduction and side lie hip clam) and the different variations of these exercises were accepted into this review. Exercises using custom-made devices or commercial gym equipment were excluded from this review as were plyometric exercise activities such as hopping, running or jumping.
Quality assessment
Methodological quality of included studies in this review were assessed independently by two reviewers (DM and TP) using a standardized quality assessment tool recommended by the Non-Randomized Studies Group of the Cochrane Collaboration and previously adapted for EMG study reviews.38,39 With the scope of the tool covering external validity, performance bias and detection bias, these items are then displayed in its raw form individually for the reader to evaluate the study quality for each item rather than be determined by an overall summary score.
Data extraction
Data were extracted by one reviewer (DM) and verified by a second (TP) using a standardized form40 that was modified for this review. The main study characteristics extracted included; participant characteristics; electrode placement; normalisation method; exercise characteristics; and study results. Where studies had healthy and pathological participants performing therapeutic exercises, data were extracted for the healthy participants. Data relating to muscle activity for each exercise was summarized as mean % MVIC with 95% confidence interval (CI). Data reported as medians and inter-quartile range (IQR) were converted to means and standard deviations (SD) using methods described by Wan, et al.41 The meta (v 4.9-5) R statistical software package was used to convert the SD to a 95% CI. Calculations were performed in the log scale and backtransformed to raw units (% MVIC) for ease of interpretation. Electromyographical technical data for collection, processing and analysis were also extracted from all the included studies since collection, normalisation and processing methods can influence muscle activity profiles.42
Data analysis
Data were grouped according to muscle segment and exercise and summarised qualitatively according to level of activity. Where two or more studies were available for a specific muscle segment and exercise, data were pooled quantitatively in a meta-analysis using the meta package in R. A random effects model was used for data pooling, and statistical heterogeneity was described using the I2 statistic (0-100%) where 25%, 50% or 75% was considered low, moderate or high level of heterogeneity respectively.43
For simplicity in analyzing the exercises for activation levels across the studies, exercise results were characterized into very-high (>60% MVIC), high (41-60% MVIC), moderate (21-40% MVIC) or low (0-20% MVIC) levels of activation as has been utilized in previous reviews.28,31,44
RESULTS
Study selection
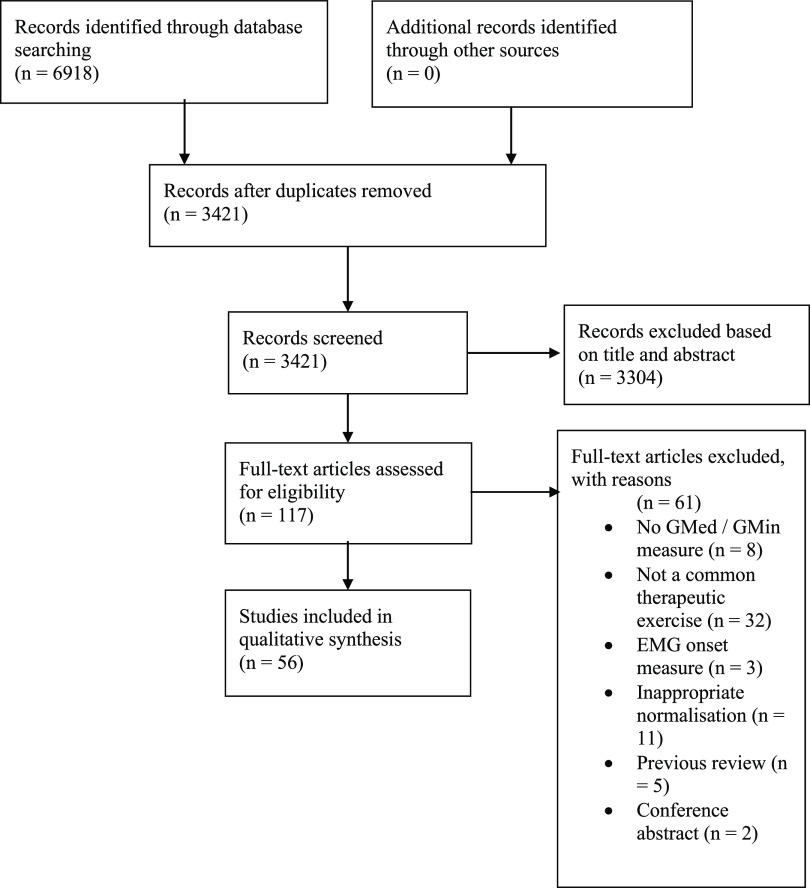
The flow of studies through the review is illustrated in Figure 1. Fifty-six studies satisfied the eligibility criteria and were included in this review.
Figure 1.
PRISMA diagram of study selection through the review.
Methodological quality
The risk of bias across studies is summarized in Table 1. All but four studies provided adequate demographic data for the study population and only one study had a blinded data analyst for raw EMG data45 (Table 1). Eighteen studies provided insufficient information on appropriate electrode positioning and 14 studies did not randomize the exercise protocol in order to minimize the potential for bias as a result of learning effects and fatigue (Table 1).
Table 1.
Methodological quality of the included studies using a risk of bias assessment
| Study | External validity | Internal validity | ||||
|---|---|---|---|---|---|---|
| Detection | Selection bias / control of confounding | |||||
| Representative | Blinded assessors | Appropriate electrode positioning | Randomisation of exercises | Appropriate normalisation procedure | Appropriate statistical tests used to assess EMG activity | |
| Ayotte et al. (2007) | ✔ | × | × | ✓ | ✓ | ✓ |
| Barton et al. (2013) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Berry et al. (2015) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Bolgla et al. (2014) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Bolgla et al. (2016) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Bolgla & Uhl (2005) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Boren et al. (2011) | × | × | ✓ | ✓ | ✓ | × |
| Boudreau et al. (2009) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Bouillon et al. (2012) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Cambridge et al. (2012) | ✓ | × | × | ✓ | ✓ | ✓ |
| Chan et al. (2017) | ✓ | × | × | ✓ | ✓ | ✓ |
| Cynn et al. (2006) | ✓ | × | ✓ | × | ✓ | ✓ |
| Distefano et al. (2009) | ✓ | × | × | ✓ | ✓ | ✓ |
| Dwyer et al. (2010) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Dwyer et al. (2016) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Ekstrom et al. (2007) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Felecio et al. (2011) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Ganderton et al. (2017) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Harput et al. (2016) | ✓ | × | ✓ | × | ✓ | ✓ |
| Hatfield et al. (2016) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Heo et al. (2013) | ✓ | × | × | × | × | ✓ |
| Hertel et al. (2005) | ✓ | × | × | ✓ | ✓ | ✓ |
| Ju & Yoo (2017) | ✓ | × | × | × | ✓ | ✓ |
| Ju & Yoo (2016) | ✓ | × | ✓ | × | ✓ | ✓ |
| Kang et al. (2014) | ✓ | × | ✓ | × | ✓ | × |
| Kim et al. (2015) | ✓ | × | × | × | ✓ | ✓ |
| Krause et al. (2018) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Krause et al. (2009) | ✓ | × | × | ✓ | ✓ | ✓ |
| Lee et al. (2013) | ✓ | × | × | ✓ | ✓ | ✓ |
| Lee et al. (2014) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Lehecka et al. (2017) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Lin et al. (2016) | ✓ | × | × | × | ✓ | ✓ |
| Lubahn et al. (2011) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| MacAskill et al. (2014) | ✓ | × | × | ✓ | ✓ | ✓ |
| Mauntel et al. (2013) | ✓ | × | × | ✓ | ✓ | ✓ |
| McBeth et al. (2013) | ✓ | × | ✓ | × | ✓ | ✓ |
| Monteiro et al. (2017) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Moore et al. (2018) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Morimoto et al. (2018) | × | × | × | × | ✓ | ✓ |
| Noh et al. (2012) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Oliver & Stone (2016) | × | × | ✓ | × | ✓ | ✓ |
| Oliver et al. (2010) | × | × | ✓ | ✓ | ✓ | ✓ |
| O’Sullivan et al. (2012) | ✓ | × | ✓ | × | ✓ | ✓ |
| O’Sullivan et al. (2010) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Petrofsky et al. (2005) | ✓ | × | × | × | ✓ | ✓ |
| Philippon et al. (2011) | ✓ | × | × | ✓ | ✓ | ✓ |
| Selkowitz et al. (2013) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Sidorkewicz et al. (2014) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Sinsurin et al. (2015) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Souza & Powers (2009) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Webster & Gribble (2013) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Willcox & Burden (2013) | ✓ | × | × | ✓ | ✓ | ✓ |
| Youdas et al. (2014) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Youdas et al. (2015) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Youdas et al. (2013) | ✓ | × | ✓ | × | ✓ | ✓ |
| Zeller et al. (2003) | ✓ | × | ✓ | ✓ | ✓ | ✓ |
Note:✓ indicates the quality measure was addressed adequately, × indicates the quality measure was not addressed adequately or not reported clearly in the study
Representative: ✓ if the study describes demographic details (age, gender, height, weight).
Blinded assessors: ✓ if data assessed or processed by a blinded assessor.
Appropriate electrode positioning: ✓ if surface electrodes were described being placed according to SENIAM guidelines or anatomy atlas.
Appropriate normalisation procedure:✓ if procedure described tested position and contraction type.
Study characteristics
The 56 included studies for this review are summarized in Tables 2 and 3. There were 55 studies included for GMed and two studies46,47 for GMin with one study46 evaluating both GMed and GMin. All the studies were cross-sectional with six including a comparison group.5,48-52 These comparison groups included a specific lower limb pathology (including patellofemoral pain, chronic ankle instability, hip osteoarthritis and anterior cruciate ligament reconstruction) or various orthotic conditions. Sample sizes of the included studies ranged from six to 44 participants. Most studies contained a mixture of men and women aged 20-30 years with 13 studies5,46,52-62 comprising a single gender population, and one study46 recruiting healthy elderly participants.
Table 2.
Summary of included gluteus medius studies.
| Study and type | Participant characteristics | EMG electrode type and placement | Normalisation method | Exercise characteristics | Results (% MVIC (SD)) |
|---|---|---|---|---|---|
| Ayotte et al. (2007) (Cross-sectional) | 23 (16 M) physically active Department of Defence. 31.2 (5.8) years; 173.1 (10.1) cm; 77 (13.9) kg. | Surface (33% iliac crest to greater trochanter) dominant limb. | MVIC 3 trials x 3 secs in side-lie 00 abd., neutral flex. / ext. 1 min rest between trials. | Exercises – 5 randomised: wall squat; mini squat; forward step-up; lateral step-up; retro step-up. Repetitions – 3 of 1.5 secs concentric and 1.5 secs eccentric to a metronome (40 bpm). Practice reps before. Rest – 5 mins between MVIC testing and exs. | wall squat 52 (22); forward step-up 44 (17); lateral step-up 38 (18); retro step-up 37 (18); mini squat 36 (17). |
| Barton et al. (2013) (Cross-sectional) | 19 (11 M) healthy university. 28.4 (2.7) years; 172.4 (5.8) cm; 67.8 (10.4) kg. | Surface105 on dominant limb. | MVIC 3 trials x 5 sec in side-lie 100 abd, neutral hip flex. - ext. 1 min rest between reps. | Exercises – 4 randomised: wall squat; wall squat against gym ball; SL squat with contralateral leg wall support; SL squat with contralateral leg against gym ball wall support. Repetitions – 3 trials, 2 secs eccentric, 5 secs isometric, 2 secs concentric. 1 practice trial before. Rest - 30 secs between trials. | SL squat with ball 46 (15); SL squat 42 (12); squat with ball 10 (7); squat 9 (5). |
| Berry et al. (2015) (Cross-sectional) | 24 (12 M) healthy college. 22.9 (2.9) years; 171.1 (10.5) cm; 68.6 (12.9) kg | Surface106 post. portion bilaterally. | MVIC 1 trial x 3 secs in side-lie abd. 1 practice rep before. | Exercises – 2 randomised: side-step upright posture with elastic resistance; side-step squat posture with elastic resistance. Repetitions – 8 for each ex. for each direction. | squat posture stance limb 35.7 (13.8); squat posture moving limb 23.3 (11.2); upright posture stance limb 22.9 (9.5); upright posture moving limb 18.7 (8.0). |
| Bolgla et al. (2016) (Cross-sectional) | 34 (18 M) healthy active university. 24.3 (3.4) years (M), 24 (1.5) years (F); 1.8 (0.1) m (M), 1.65 (0.1) m (F); 81.2 (9.7) kg (M), 59.9 (8.8) kg (F). | Surface (33% iliac crest to greater trochanter) on dominant limb. | MVIC 2 trials x 5 sec in side-lie abd. 1 practice trial before. 30 secs rest between trials. | Exercises – 4 randomised: SL wall squat; SL mini squat; lateral step down; forward step down. Repetitions – 15 to a metronome (40 bpm), 1 beat down, 1 beat up, 1 beat rest. Practice reps before. Rest – 3 mins between exs. |
SL wall squat 26.5 (12); SL mini squat 23.2 (12.2); front step down 22.8 (12.2); lateral step down 21.4 (10.7). |
| Bolgla et al. (2014) (Cross-sectional) | 34 (18M) healthy active university. 24.3 (3.4) years (M), 24 (1.5) years (F); 1.8 (0.1) m (M), 1.65 (0.1) m (F); 81.2 (9.7) kg (M), 59.9 (8.8) kg (F). | Surface on dominant limb. | MVIC 2 trials x 5 sec in side-lie abd | Exercises – 4 randomised: SL wall squat; SL mini squat; lateral step down; forward step down. Repetitions – 15 to a metronome (40 bpm). Rest – 3 mins between exs. | SL wall squat 21.6 (8.6) (M), 32 (13.1) (F); SL mini squat 20.3 (11.2) (M), 26.6 (12.8) (F); front step down 19 (9.2) (M), 27.2 (13.9) (F); lateral step down 18.5 (10.2) (M), 24.6 (10.6) (F). |
| Bolgla and Uhl (2005) (Cross-sectional) | 16 (8 M) healthy university. 27 (5) years; 1.7 (0.2) m; 76 (15) kg. | Surface (33% iliac crest to greater trochanter) on (R) limb. | MVIC 3 trials x 3-5 secs in side-lie 250 abd. 1 min rest between trials. | Exercises – 6 randomised: side-lie hip abd; stand hip abd NWB; stand hip abd hip flex 300 NWB; pelvic drop; stand hip abd; stand hip abd with hip flex 300. NWB exs had cuff weight 3% body weight on (R) leg. Repetitions – 15 to a metronome (60 bpm) of 1 beat up, 1 beat down and 1 beat rest. 8-10 practice reps 10 mins before testing. Rest - 3 mins between exs. |
pelvic drop 57 (32); stand abd with hip flex 300 46 (34); stand abd 42 (27); side-lie abd 42 (23); stand abd NWB 33 (23); stand abd with hip F 300 NWB 28 (21). |
| Boren et al. (2011) (Cross-sectional) (Exercise data partially extracted) | 26 healthy university and surrounds. | Surface (positioned per standard EMG protocol) on dominant limb. | MVIC 3 trials x 5 secs in side-lie abd. 1 min rest between trials. | Exercises – 22 randomised including: SL squat; clam hip flex.450; side-lie abd; lateral step-up; skater squat; pelvic drop; SL bridge stable; forward step-up; SL bridge unstable. Repetitions – 8 to a metronome (60 bpm) of 1 beat up and 1 beat down including 3 practice reps. Rest – 2 mins between exs. |
SL squat 82.26; side-lie abd 62.91; lateral step-up 59.87; skater squat 59.84; pelvic drop 58.43; SL bridge s Table 54.99; forward step-up 54.62; SL bridge unsTable 47.29; clam hip flex. 450 47.23. |
| Boudreau et al. (2009) (Cross-sectional) | 44 (22 M) healthy. 23.3 (5.1) years; 174.5 (9.1) cm; 74.6 (16.5) kg | Surface (33% iliac crest to greater trochanter ant to the GMax) bilaterally. | MVIC 3 trials x 3 secs in stand hip abd. 30 sec rest between trials. | Exercises – 3 randomised: SL squat; lunge; step-up and over. Repetitions – 3 trials for each ex. 2 practice trials before. Rest – 30 secs between trials and 2 mins between exs. |
DOM: SL squat 30.1 (9.1); lunge 17.7 (8.8); step-up and over 15.2 (6.9). Non-DOM: lunge 19.0 (11.7); step-up and over 16.8 (10.4); SL squat 12.0 (7.5). |
| Bouillon et al. (2012) (Cross-sectional) | 40 (20 M) healthy active university and surrounds. 23.2 (1.9) years (M), 22.4 (1.8) years (F); 1.8 (.09) m (M), 1.6 (.07) m (F); 87.8 (20) kg (M), 42.5 (7) kg (F). | Surface (3cm inf. to iliac crest) on dominant limb. | MVIC 3 trials x 5 sec in side-lie abd., neutral rotation, slight hip ext. 3 secs rest between trials and 5 mins between MVIC and exs. | Exercises - 3 randomised: step down; forward lunge; side lunge. Repetitions – 1 trial of 10 to metronome (80 bpm) with 4 beats per repetition 10 practice reps before. Rest – 30 secs between sets |
step down (M & F) 14 (3); side lunge (M) 13 (3), (F) 13 (2); lunge (M & F) 12 (2). |
| Cambridge et al. (2012) (Cross-sectional) (Exercise data partially extracted) | 9 healthy males university. 22.6 (2.2) years; 181.9 (9.2) cm; 85.8 (15.4) kg. | Surface bilaterally | MVIC 1 trial side-lie abd. | Exercises – 2 randomised: sumo walks with elastic resistance band at 3 different positions for each ex. Repetitions – 3 trials for each ex. Practice reps before. |
Sumo walk with feet band ∼ 35 (12); sumo walk with ankle band ∼ 29 (8); sumo walk with knee band ∼ 24 (8.5). |
| Chan et al. (2017) (Cross-sectional) | 20 (10 M) healthy university. 21.10 (1.70) years, 166.75 (7.90) cm; 58.10 (9.20). | Surface (33% iliac crest to greater trochanter) | MVIC side-lie abd, neutral rotation and slight ext. | Exercises – 2 randomised: clam hip flex 450; side-lie abd with normal core activation and enhanced core activation. Repetitions – 3 trials to metronome (60 bpm). 3 secs up, 3 secs hold, 3 secs down. Practice reps before. Rest – 3 sec between trials and 1 min between exs. |
Enhanced core: side-lie abd 31.38 (12.02); clam hip flex 450 18.39 (10.66). Normal core: side-lie abd 28.89 (7.92); clam hip flex 450 15.63 (10.53). |
| Cynn et al. (2006) (Cross-sectional) | 18 (9 M) healthy university. 23.5 (3.5) years; 59.3 (5.1) kg; 167.7 (4.3) years. | Surface (33% iliac crest to greater trochanter) on dominant limb. | MVIC 3 trials side-lie abd. | Exercises - 2: side-lie abd; side-lie abd with pressure biofeedback unit. Repetitions – 5 sec hold. Practice reps before. |
Side-lie abd 25.03 (10.25); side-lie abd with pressure biofeedback unit 46.06 (21.20). |
| Distefano et al. (2009) (Cross-sectional) (Exercise data partially extracted) | 21 (9 M) healthy recreationally active. 22 (3) years; 171 (11) cm; 70.4 (15.3) kg. | Surface (33% greater trochanter to iliac crest) on dominant limb. | MVIC 3 trials x 5 secs in side-lie 250 abd. 1 practice trial before. | Exercises – 9 randomised including clam hip flex 300; clam hip flex 600; side-lie hip abd; SL squat; forward lunge; sideways lunge; transverse lunge; lateral band walk. Repetitions – 8 to metronome (60 bpm) with 2 beats up and 2 beats down. Practice reps before. Rest – 2 mins between exs. 5 mins between exs and MVIC. |
Side-lie hip abd 81 (42); SL squat 64 (24); lateral band walk 61 (34); transverse lunge 48 (21); forward lunge 42 (21); clam hip flex 300 40 (38); sideways lunge 39 (19); clam hip flex 600 38 (29). |
| Dwyer et al. (2013) (Cross-sectional) (Exercise data extracted for healthy controls) | 17 healthy local controls. 50.8 (1.4) years; 173.1 (2.5) cm; 77.3 (3.8) kg. | Surface (33% iliac crest to greater trochanter) bilaterally. | MVIC 3 trials x 3 secs in stand hip abd on stance leg. Practice trials before. 30 sec rest between trials. | Exercises – 2 randomised: step-up; step-down Repetitions – 3 trials for each limb to a metronome (55bpm) Rest – 30 secs between trials and 2 mins between exs. |
DOM step up 29.4 (2.4); non-DOM step up 28.9 (2.5); non-DOM step down 22.1 (4.5); DOM step down 19.9 (1.7). |
| Dwyer et al. (2010) (Cross-sectional) | 42 (21 M) healthy asymptomatic. 23 (5.8) years (F), 23 (4.0) years (M); 167.6 (5.1) cm (F), 181.4 (7.4) cm (M); 63.7 (5.9) kg (F), 85.6 (16.5) kg (M). | Surface107 bilaterally. | MVIC 3 trials x 3 secs in stand abd. 30 sec rest between trials. | Exercises – 3 randomised: SL squat; lunge; step-up-and-over. Repetitions – 3 trials for each ex. Practice reps before. Rest – 30 secs between trials and 2 mins between exs. |
Concentric and eccentric phases DOM; SL squat 31.2 (10.9), 25.3 (11.5) (M), 29.5 (7.5), 26.6 (6.8) (F); step-up-and–over 15.5 (7.9), 14.4 (9.6) (M), 16.5 (5.7), 14.5 (4.6) (F); lunge 11.6 (8.3), 15.5 (9) (M), 11.4 (4.8), 17.8 (8.8) (F). Concentric and eccentric phases non-DOM; SL squat 11.6 (6.1), 10.6 (5.8) (M), 12.5 (9.3), 12.6 (9) (F); lunge 17.2 (7.3), 14.8 (4.7) (M), 24.6 (18.1), 20.8 (15.9) (F); step-up-and-over 14.8 (3.8), 13.3 (4.6) (M), 20.7 (14.6), 18.7 (14.3) (F). |
| Ekstrom et al. (2007) (Cross-sectional) (Exercise data partially extracted) | 30 (19 M) healthy university. 27 (8) years; 176 (8) cm; 74 (11) kg. | Surface (ant-sup. to GMax and inf. to the iliac crest) applied unilaterally. | MVIC 3 trials x 5 secs in side-lie neutral hip rot, slight ext, end AROM abd. 30 sec rest between trials. | Exercises – 8 randomised including: side-lie hip abd; bridge; SL bridge with opposite knee ext; lateral step-up; stand lunge. Repetitions – 3 for trunk stabilisation exercises held for 5 secs; lateral step-up and lunge held 5 secs at max knee. flex; Practice reps before. Rest – 30 secs between trials; 1 min between exs. |
SL bridge 47 (24); lateral step-up 43 (18); side-lie abd 39 (17); lunge 29 (12); bridge 28 (17). |
| Felicio et al. (2011) (Cross-sectional) | 15 healthy sedentary females with misalignment of lower limb. 22.26 (2.22) years; 161.7 (7.33) cm; 56.56 (4.68) kg. | Surface108 bilaterally. | MVIC 3 trials x 6 secs in side-lie 200 abd, 100 ext. | Exercises – 3 randomised with 25% additional body weight: ball wall squat; ball wall squat with add; ball wall squat with abd. Repetitions – 3 trials for each ex. held for 6 secs. Rest – 2 mins between trials. | DOM: squat with add 59 (22); squat with abd 47 (20); squat 33 (27). Non-DOM: squat with add 59 (27); squat with abd 52 (24); squat 26 (13). |
| Ganderton et al. (2017) (Cross-sectional) (Exercise data partially extracted) | 10 healthy post-menopausal women. 60.2 (2.7) years; 164.7 (4.3) cm; 70.0 (10.2) kg. | Fine-wire into 3 GMed segments (anterior, middle & posterior) via standardised landmarks on dominant leg. | MVICs 3 trials x 5 secs in side-lie hip abd, side lie clam, seated hip ER / IR to determine max for each segment. 3 min rest between trials. | Exercises – 7 exercises randomised including: hip hitch; hip hitch with toe tap; hip hitch with hip swing; isometric hip abduction; dip test; clam hip flex 450. Repetitions – 2 sets of 6 reps to metronome 2 secs concentric and 2 secs eccentric for dynamic exs. 3 reps of 15 secs hold for isometric exs. Rest – 1 min between isometric reps and dynamic sets; 2 mins between each ex. | Anterior GMed: hip hitch swing 82.18 (54.71); hip hitch 68.74 (40.98); hip hitch toe tap 75.60 (47.82); dip test 44.75 (29.11); stand isometric hip abd 55.65 (49.65); clam 3.06 (2.81). Middle GMed: dip test 71.06 (64.53); hip hitch swing 66.26 (38.37); hip hitch 65.90 (47.54); hip hitch toe tap 57.91 (43.51);; stand isometric hip abd 29.81 (18.81); clam 13.26 (16.34). Posterior GMed: hip hitch 73.80 (53.89); hip hitch swing 72.15 (43.32); hip hitch toe tap 45.55 (13.10); stand isometric hip abd 40.52 (44.30); dip test 28.35 (14.29); clam 22.79 (17.03). |
| Harput et al. (2016) (Cross-sectional) (Exercise data partially extracted for healthy controls) | 15 (8 M) healthy controls 26.3 (6.6) years; 171.6 (10.8) cm; 75.1 (9.2) kg. | Surface (50% iliac crest to greater trochanter) on dominant leg. | MVIC 3 trials x 5 secs in stand hip abd on stance leg. 1 practice trial before. 30 secs between trials. | Exercises - 3 exercises including step down. Repetitions – 3 reps in 2 directions for SEBT (4 practice reps); 5 for step down to metronome (75bpm) (1 practice rep). |
Step down ascending 28.2 (10.4), descending. 27.5 (11.4). |
| Hatfield et al. (2016) (Cross-sectional) | 20 (10 M) healthy university. 26.6 ± 5.1 years; 1.73 ± 0.08 m; 66.1 ± 9.2 kg. | Surface105 randomly allocated to a side. | MVIC 2 trials x 3 secs in prone hip abd. Practice trials before. | Exercises – 4 randomised: SL squat; step down; half step down; step up. Repetitions – 5 reps to metronome (1Hz) 4 sec count. Practice reps before. |
Step down 27.42 (7.37); (2) half step down 21.23 (6.2); SL squat 23.71 (5.98); step up 16.87 (4.34). |
| Heo et al. (2013) (Exercise data partially extracted) | 15 healthy females. 23.53 (3.15) years; 162.06 (4.78) cm; 52.60 (4.84) kg. | Surface for 3 GMed segments: anterior (50% ASIS to greater trochanter); middle (50% iliac crest to greater trochanter); and posterior. (33% posterior ilium to greater trochanter) | MVIC hip abd. | Exercises – 4 including SL wall squat with abd; SL wall squat with add; SL squat with abd; SL squat with add. Repetitions – 3 reps for 5 sec holds for each ex. Rest - 30 secs between reps and 1 min between exs. |
Anterior GMed: SL squat with add 42.11 (20.63); SL wall squat with abd 28.72 (14.7); SL squat with abd 19.36 (13.32); SL wall squat with add 15.66 (10.50). Middle GMed: SL wall squat with abd 32.95 (10.86); SL squat with add 31.32 (17.38); SL squat with abd 26.84 (13.20); SL wall squat with add 20.69 (9.56). Posterior GMed: SL wall squat with abd 43.81 (19.42); SL squat with abd 32.99 (10.84); SL wall squat with add 27.97 (19.78); SL squat with add 22.43 (10.10). |
| Hertel et al. (2005) (Cross-sectional) (Exercise data extracted for no orthotic condition) | 30 (15 M) healthy recreationally active equally divided into 3 groups depending on foot-type (pes planus, pes cavus, pes rectus). 21.1 (1.6) years; 170.2 (6.1) cm; 69.1 (13.9) kg. | Surface (50% iliac crest to greater trochanter) on leg contralateral to dominant throwing arm. | MVIC 3 trials in SL stance in a custom-made device. 90 secs rest between trials. | Exercises – 2 randomised: SL squat; lateral step-down. Repetitions – 3 trials for each ex. Metronome (60 bpm) 2 secs down, 2 secs up for lateral step down. Rest – 5 mins between each orthotic condition. |
SL squat ∼ 77 (5); lateral step down ∼ 74 (6). |
| Ju & Yoo (2017) (Cross-sectional) (Exercise data partially extracted) | 15 healthy males. 29.1 (2.9) years; 173.4 (7.1) cm; 71.7 (8.5) kg. | Surface anterior segment (50% ASIS to greater trochanter). | MVIC in side-lie abd. | Exercises – 4 including pelvic drop. Repetitions – 5 secs contraction. | Pelvic drop 25.40. |
| Ju & Yoo (2016) (Cross-sectional) (Exercise data partially extracted) | 15 healthy males. 29.13 (2.85) years, 173.4 (7.08) cm, 71.73 (8.52) kg. | Surface for 3 GMed segments: anterior (50% ASIS to greater trochanter); middle (50% iliac crest to greater trochanter); posterior (33% distance posterior ilium to greater trochanter). | MVIC in side-lie abd, prone hip ER, and prone hip IR to determine max. for each segment. 30 secs rest between trials. | Exercises – 4 including pelvic drop. Repetitions – 3 trials for each ex. 2 secs up, 2 secs down. Rest – 30 secs between trials and 1 min between exs. | Anterior GMed: pelvic drop 25.40 (7.77). Middle GMed: pelvic drop 23.43 (8.65). Posterior GMed: pelvic drop 21.63 (9.06). |
| Kang et al. (2014) | 17 healthy males. 23.06 (1.47) years; 172.88 (5.65) cm; 68.29 (4.69) kg. | Surface109 on dominant limb. | MVIC 2 trials x 5 secs in side-lie abd. 1 min rest between trials. | Exercises – 2: squat; squat with resisted shoulder flex. Repetitions – 3 trials to metronome (3 secs down and 3 secs up). | Eccentric phase: squat with resisted shoulder flex 12.09 (6.29); squat 8.82 (3.91). Concentric phase: squat with resisted shoulder flex 11.58 (5.96); squat 8.44 (3.59). |
| Kim et al. (2015) (Cross-sectional) (Exercise data partially extracted) | 10 healthy males 31 (4.2) years; 176.8 (8.3) cm; 76.7 (8.1) kg. | Surface (33% iliac crest to greater trochanter) bilaterally. | MVIC 3 trials in side-lie 50 abd. | Exercise – 2 including side-lie abd. Repetitions – 3 trials, 5 secs hold. Rest – 30 secs between trials. |
Side-lie abd. 24.30 (5.45). |
| Krause et al. (2018) (Cross-sectional) (Exercise data partially extracted) | 30 (15 M) healthy. 23.9 (1.7) years, BMI 24.21 (2.88). | Surface (33% iliac crest to greater trochanter) on dominant limb. | MVIC 1 trial x 5 secs in side-lie abd 50. 1 submaximal practice trial before. | Exercise – 2 including lunge. Repetitions – 3 to a metronome, 3 secs down, 1-2 secs hold, 3 secs up. Practice trials before. |
Lunge 15.3 (11.4) |
| Krause et al. (2009) (Cross-sectional) (Exercise data partially extracted) | 20 (6 M) healthy recreationally active. 23.6 (1.7) years (F), 26.3 (2.5) years (M); 169.3 (9.5) cm (F), 172.2 (12.9) cm (M); 65 (9.2) kg (F), 85 (10.1) kg (M). | Surface (50% greater trochanter to iliac crest) on dominant limb. | MVIC 3 trials in side-lie abd 300, slight hip ext. Adequate rest between trials. | Exercises – 5 randomised including SL squat; SL squat on Airex cushion. Repetitions – 3 trials for each ex. Stance exs held for 10 secs and squats for 3 reps. Practice reps before. Rest – adequate rest between each set of exs. |
SL squat on Airex 58.5 (35.32); SL squat 47.79 (22.61). |
| Lee et al. (2013) (Cross-sectional) | 20 healthy with normal ITB length and BMI < 25. 22.3 (1.9) years, 168.7 (7.2) cm; 65.5 (12.4) kg. | Surface (33% iliac crest to greater trochanter) on dominant limb. | MVIC 2 trials x 5 secs in side-lie abd 50% AROM, slight ext and ER. 30 secs rest between trials. | Exercises – 3 randomised: side-lie abd.; side-lie abd. + IR; side-lie abd + ER. Repetitions – 3 trials x 5 sec hold. Rest – 3 mins between exs. |
Side-lie abd. + IR 45.3 (20.5); side-lie abd + ER 35.3 (12.5); side-lie abd 34.2 (11.8). |
| Lee et al. (2014) (Cross-sectional) | 19 (8 M) healthy with weak GMed and BMI < 25. 21 (1.73) years; 166 (.07) cm; 59.79 (9.61) kg. | Surface (33% iliac crest to greater trochanter) on dominant limb. | MVIC 2 trials x 5 secs in side-lie abd 50% AROM, slight ext and ER. 3 mins rest between trials. | Exercises – 3 randomised: side-lie abd; side-lie abd + IR; side-lie abd + ER. Repetitions – 3 trials x 5 sec hold. Rest – 3 mins between exs. |
Side-lie abd + IR ∼ 61.34 (4); side-lie abd + ER ∼ 48.96 (7); side-lie abd ∼ 45.22 (6). |
| Lehecka et al. (2017) (Cross-sectional) | 28 (12 M) healthy. 23.43 (2.28) years; 1.73 (0.11) m; 72.57 (13.93) kg. | Surface (inf. to lat. aspect of iliac crest on a line to greater trochanter) on dominant limb. | MVIC 3 trials x 7 secs in side-lie abd end range, slight ext. 30 secs rest between trials. | Exercises – 5 randomised: SL bridge with knee flex 900; SL bridge with knee flex. 1350; SL bridge with knee flex 900 opposite leg bent; SL bridge with knee flex 900 ankle DF, opposite leg bent; SL bridge with knee flex 1350 ankle DF, opposite leg bent. Repetitions – 8 to metronome (60 bpm) for each including 2 practice reps before. |
SL bridge with knee flex 900 57.81 (20.72); SL bridge knee flex 1350 57.23 (27.82); SL bridge knee flex 900, opposite leg bent 55.05 (20.71); SL bridge knee flex 900 ankle DF, opposite leg bent 54.27 (20.01); SL bridge knee flex 1350 ankle DF, opposite leg bent 41.63 (18.19). |
| Lin et al. (2016) (Cross-sectional) (Exercise data partially extracted) | 12 (6 M) healthy. 26.1 (4.7) years; 168.8 (2.7) cm; 63.6 (9.6) kg. | Surface (33% greater trochanter to iliac crest) on dominant limb. | MVIC 2 trials x 5 secs in side-lie hip abd. 30 secs rest between trials. | Exercises – 3: clam hip flex 600; SL squat; lunge. Repetitions – 5 for each ex. to a metronome (1 rep per 2 secs). |
Clam 19.1 (8.8); SL squat 18.4 (7.9); lunge 8.2 (3.8). |
| Lubahn et al. (2011) (Cross-sectional) | 18 healthy females; 22.3 (2.3) years; 166.82 (9.2) cm; 61.1 (7.1) kg. | Surface107 on dominant limb. | MVIC 3 trials x 5 secs in side-lie abd. with neutral hip. | Exercises – 4 randomised: squat; squat with lateral resistance band; step-up; SL squat. Repetitions – 5 for each ex. to a metronome (40 bpm) with 1 beat for start of rep. then beat 2 at midpoint then beat 3 for end of rep. Several practice reps before. Rest - 10-15 secs between reps. 45-60 secs rest between each ex. |
SL squat 65.6 (23.8); step-up 48.2 (20.4); squat with lateral resistance band 23.7 (16.3); squat 20.8 (14.7). |
| MacAskill et al. (2014) (Cross-sectional) (Exercise data partially extracted) | 34 (14 M) healthy. 21.2 (1.8) years (M), 21.7 (1.6) years (F); 177.8 (15.3) cm (M), 163.2 (6.7) cm (F); 77.1 (8.9) kg (M), 58.1 (6.2) kg (F). | Surface (2-3 cm distal to midpoint iliac crest) on dominant limb. | MVIC 3 trials x 5 secs in side-lie abd 50% AROM. 1 sec rest between trials. | Exercises – 4 randomised including forward step-up; lateral step-up; 10 RM side-lie abd with cuff weight. Repetitions – 3 trials of 5 reps, 2 secs for each rep Rest – 3 mins between sets |
10 RM side-lie abd ∼ 100 (23); lateral step-up ∼ 63 (21); forward step-up ∼ 62 (19). |
| Mauntel et al. (2013) (Cross-sectional) | 40 (20 M) healthy active divided equally into 2 groups – control and medial knee displacement (MKD). 20.2 (1.5) years, 20.2 (1.8) years (MKD); 173.1 (10.1) cm, 173.8 (8.8) cm (MKD); 71 (14.6) kg, 71.8 (14.7) kg (MKD). | Surface on dominant limb. | MVIC 3 trials x 5 secs in side-lie abd. 1 min rest between trials. | Exercise – 1: SL squat Repetitions – 5 trials to a metronome (60 bpm). 2 beats down, 2 beats up. Rest – 1 min between trials. |
Control group: SL squat 37.1 (17.3). MKD group: SL squat 32.9 (17.2). |
| McBeth et al. (2012) (Cross-sectional) | 20 (9 M) healthy community runners ( > 40 km / week). 25.45 ± 5.8 years (M), 26.1 ± 5.2 years (F); 1.75 ± 0.08 m (M), 1.68 ± 0.03 m (F); 69.3 ± 7.1 kg (M), 61.3 ± 6.6 kg (F). | Surface (33% iliac crest to greater trochanter) on dominant limb. | MVIC 3 trials x 5 secs in side-lie abd 350, slight ext. and ER. 10 sec rest between trials. | Exercises – 3: side-lie abd; side-lie abd + ER; clam hip flex 450. All performed with 5% body weight cuff weight. Repetitions – 7 set to a metronome (60 bpm) of 1 beat up, 1 beat down, and 4 beat rest. 4 practice sets of 5 reps before. Rest - 1 min between exs. 2 mins between MVIC testing and exs. |
side lie abd 79.1 (29.9); side-lie abd + ER 53.03 (28.4); clam hip flex 450 32.6 (16.9). |
| Monteiro et al. (2017) (Cross-sectional) | 17 (6 M) healthy sedentary, BMI (19-25 kg/m2). 25.6 (1.4) years; 168.29 (8.64) cm; 70 (9.98) kg. | Surface (50% iliac crest to greater trochanter) on dominant limb. | MVIC 3 trials x 3 secs in side-lie abd 300. 1 min rest between trials. | Exercises – 3 randomised: pelvic drop; pelvic drop + hip IR; pelvic drop + hip ER. Repetitions – 2 trials of 4 to metronome (60 bpm). 60 practice reps for each ex before. |
pelvic drop + IR 42.43 (15.45); pelvic drop 42.11 (18.39); pelvic drop + ER 32.77 (14.01). |
| Morimoto et al. (2018) (Cross-sectional) (Exercise data partially extracted) | 11 healthy. 22 (2) years; 174 (7.5) cm; 71,7 (13.5) kg. | Surface on dominant limb. | MVIC in side-lie abd. | Exercises – 7 including side-lie abd; side-lie abd + hip ER; side-lie abd + hip IR. | Side-lie abd + ER 40.5 (16.9); side-lie abd 38 (14.2); side-lie abd + IR 36.3 (16.7). |
| Noh et al. (2012) (Cross-sectional) | 15 (10 M) healthy. 25.07 (3.59) years; 172.07 (5.03) cm; 65.93 (6.31) kg. | Surface (33% iliac crest to greater trochanter) on dominant limb. | MVIC 2 trials x 5 secs in side-lie abd. | Exercises – 3 randomised: lateral step up; lateral step up + hip IR; lateral step up + hip ER. Repetitions – 3 trials for 2 secs up to a metronome. Rest – 1 min between trials and 5 mins between exs. |
lateral step-up + IR 41.27 (13.16); lateral step-up 38.81 (13.01); lateral step-up + ER 30.17 (9.81). |
| Oliver et al. (2010) (Cross-sectional) (Exercise data partially extracted) | 30 healthy active college students. 23.4 (1.4) years; 171.3 (10.3) cm; 73.3 (16.2) kg. | Surface110 bilaterally. | MVIC 2 trials x 5 secs in side-lie abd. | Exercises – 4 randomised including bridge and SL bridge. Repetitions – 3 for each ex. Held for 10 secs. Practice reps before. |
(L) side: (R) SL bridge ∼ 35 (17); bridge ∼ 17 (11); (L) SL bridge ∼ 10 (13). (R) side: (L) SL bridge ∼ 33 (16); bridge ∼ 17 (9); (R) SL bridge ∼ 14 (14). |
| Oliver & Stone (2016) (Cross-sectional) (Exercise data partially extracted) | 28 healthy active college students. 22 (2) years; 168 (8) cm; 66 (10) kg. | Surface107 on dominant limb. | MVIC 3 trials x 5 secs in side-lie abd. | Exercises – 2 including SL step down. | SL step down 187 (80). |
| O’Sullivan et al. (2013) (Cross-sectional) (Exercise data partially extracted for control group) | 12 healthy active women. 21 (1) years; 164.6 (7.9) cm; 62.6 (9.9) kg. | Surface for 3 GMed segments: anterior (50% ASIS to greater trochanter); middle (50% greater trochanter to iliac crest); posterior (33% posterior ilium to greater trochanter) on dominant limb. | MVIC 3 trials x 5 secs in side-lie abd including 2 practice trials. 30 sec rest between trials | Exercises – 4 non-randomised including pelvic drop; step up and over; SL squat. Repetitions – 3 for each ex. Step up and over held for 5 secs. Pelvic drop and SL squat 2 secs down, 2 secs up to a metronome (60 bpm). 3 practice trials before. Rest – 30 secs between trials and 2 min rest between exs. |
Anterior GMed: SL squat 89.6 (24.6); step up and over 88.4 (19.6); pelvic drop 79.9 (24.8). Middle GMed: SL squat 91.7 (36.9); pelvic drop 87.6 (32.6); step up and over 85.4 (29.6). Posterior GMed: pelvic drop 87.9 (23.9); SL squat 86.7 (16); step up and over 81.2 (28.8). |
| O’Sullivan et al. (2010) (Cross-sectional) (Exercise data partially extracted) | 15 (7 M) healthy university. 22 (4) years; 170 (12) cm; 68 (12) kg. | Surface for 3 GMed segments: anterior (50% ASIS to greater trochanter); middle (50% greater trochanter to iliac crest); posterior (33% posterior ilium to greater trochanter) on (R) limb. | MVIC 3 trials x 5 secs in stand hip 300 abd, neutral flex / ext / ER / IR; prone hip ER; and prone hip IR to determine max for each segment. 30 sec rest between trials. | Exercises – 3 randomized including SL wall squat; pelvic drop. Repetitions – 3 for each ex. with wall squat held for 5 secs. Pelvic drop 2 secs down and 2 secs up. 3 practice reps for each ex. before. Rest – 30 secs between reps and 1 min between exs. |
Anterior GMed: pelvic drop 21.12 (6.80); SL wall squat 13.30 (7.50). Middle GMed: pelvic drop 28.45 (8.49); SL wall squat 24.60 (8.89). Posterior GMed: pelvic drop 38.17 (16.76); SL wall squat 34.82 (19.86). |
| Petrofsky et al. (2005) (Cross-sectional) (Exercise data partially extracted) | 6 (4 M) healthy. 25.3 (1.5) years; 169.9 (6.7) cm; 69.8 (9.6) kg. | Surface (over muscle belly and 2 cm distal) on (R) limb. | MVIC 3 trials x 3 secs in side-lie hip abd 1 min rest between trials. | Exercises – 6 including 450 squat; 900 squat. | 900 squat 28.4 (6.7); 450 squat 22.1 (9.3). |
| Philippon et al. (2011) (Cross-sectional) (Exercise data partially extracted) | 10 (5 M) healthy. 28.7 (2.0) years; 1.72 (0.04) m; 67 (4.3) kg | Fine-wire (2.5 cm distal to midpoint of iliac crest under US guidance). | MVIC 3 trials x 3 secs in stand hip abd, slight hip ER. 3-5 sec rest between trials. | Exercises – 13 randomised including bridge; clam hip – knee flex 450; clam hip neutral, knee flex 900; side-lie abd with hip IR; side-lie abd with hip ER; side-lie abd with hip ext; SL bridge. Repetitions – 2 trials of 5 for each ex. to a metronome. |
Concentric phase: SL bridge 35.1 (33.8); side-lie abd. + IR 33.3 (27.2); side-lie abd + ext 31.4 (22.5); side-lie abd + ER 23.3 (17.7); clam flex 450 16.7 (13.6); bridge 10.8 (8.9). |
| Selkowitz et al. (2013) (Cross-sectional) (Exercise data partially extracted) | 20 (10 M) healthy university. 27.9 (6.2) years. | Fine-wire (2.5 cm distal to midpoint of iliac crest) on dominant limb. | MVIC 1 trial X 5 secs in side-lie abd 300, neutral flex. | Exercises – 11 randomised including side-lie abd; bridge; elastic resistance clam hip flex 450; hip hike; lunge; elastic resistance side-step; squat; step up; SL bridge. Repetitions – 5 for each ex to a metronome (40bpm). Side-step 3 trials x 2 strides in each direction to metronome (80 bpm). Rest – 2 mins between exs. |
Side-lie abd 43.5 (14.7); hip hike 37.7 (15.1); SL bridge 30.9 (20.7); side-step 30.2 (15.7); step-up 29.5 (14.9); clam flex 450 26.7 (18); lunge 19.3 (12.9); bridge 15 (10.5); squat 9.7 (7.3). |
| Sidorkewicz et al. (2014) (Cross-sectional) | 13 healthy males. 24.8 (4.2) years; 179.7 (5.4) cm; 75.9 (9.8) kg. | Surface105 on (R) limb. | MVIC 3 trials in side-lie abd. 2 mins rest between trials. | Exercises – 6 randomised: side lie abd; side lie abd + hip IR; side lie abd + hip ER; clam hip flex 300; clam hip flex 450; clam hip flex 600. Repetitions – 3 trials for each ex. Practice reps before. | side lie abd + IR 48.67 (20.21); side lie abd 36.70 (14.55); side lie abd + ER 36.50 (16.46); clam hip flex 600 36.49 (33.06); clam hip flex 450 35.55 (34.25); clam hip flex 300 26.80 (24.08). |
| Sinsurin et al. (2015) (Cross-sectional) (Exercise data partially extracted) | 9 healthy sedentary males. (18-25 years); BMI (18.5-23 kg/m2); dominant (R) limb. | Surface (50% iliac crest to greater trochanter) bilaterally. | MVIC 3 trials x 3 secs in side-lie abd, neutral hip. 3 submaximal practice trials before. 90 secs rest between trials. | Exercises – 7 randomised including (L) stance, (R) hip abd Repetitions – 3 trials Rest – 30 secs between trials. 2 mins between exs. | (L) stance limb: hip abd 43.71 (15.05); (R) swing limb: hip abd 63.59 (41.16); |
| Souza & Powers (2009) (Cross-sectional) Exercise data partially extracted for controls) | 20 healthy females. 26 (5) years; 1.7 (0.6) m; 62.9 (6.6) kg. | Surface (2.5cm inferior to iliac crest) on 13 matched (R) and 7 matched (L) limbs. | MVIC 1 trial x 5 secs in side-lie abd 200, 50 ext. | Exercise – 3 including step down Repetitions – 3 trials, 2 secs down, 2 secs up to a metronome. |
Step down ∼ 17 (5). |
| Webster & Gribble (2012) (Cross-sectional) (Exercise data partially extracted for controls) | 9 healthy active controls. 22.9 (4.6) years; 164.5 (6.5) cm; 65.4 (10) kg. | Surface (2.5 cm below iliac crest) on matched assigned limb. | MVIC 3 trials x 10 secs in side-lie abd. 1 min rest between trials. 2 mins rest before exs. | Exercises – 2 randomised: rotational lunge; SL squat with rotational reach. Repetitions – 10 to metronome (72 bpm) – 2 beats out, 2 beats back. Rest – 2 mins between exs. |
rotational lunge ∼ 68 (32); rotational squat ∼ 66 (55). |
| Willcox & Burden (2013) (Cross-sectional) | 17 (10 M) healthy active. 25 (5) years (M), 23 (4) years (F); 182 (8) cm (M), 165 (4) cm (F); 77 (13) kg (M), 60 (11) kg (F). | Surface (33% greater trochanter to iliac crest) on dominant limb. | MVIC 5 secs in side-lie abd. | Exercises – 6 randomised: clam hip flex 00; clam hip flex 300; clam hip flex 600. Exs were then repeated with pelvis reclined 350. Repetitions – 10 for each ex. holding for 6 secs. Rest – 3 mins between exs. |
Pelvis neutral: clam hip flex 600 ∼ 22.5 (4.5); clam hip flex 300 ∼ 21 (5); clam hip flex 00 ∼ 17 (4). Pelvis reclined: clam hip flex 600 ∼ 17.5 (4.5); clam hip flex 300 ∼ 13 (3.5); clam hip flex 00 ∼ 12.5 (3). |
| Youdas et al. (2012) (Cross-sectional) | 21 (10 M) healthy active university. 25 (3.1) years (M), 24.5 (1.4) years (F); 1.8 (0.1) m (M), 1.7 (0.1) m (F); 82.2 (7.9) kg (M), 69.1 (4.9) kg (F). | Surface109 bilaterally. | MVIC 1 trial x 5 secs in side-lie abd 300. | Exercises – 3 randomised: lateral step against elastic resist, hips neutral; lateral step against elastic resist, hips ER; lateral step against elastic resist, hips IR. Repetitions- 3 for each ex. to metronome (40bpm). Several practice trials before. Rest – 30 – 45 secs between exs. |
Stance limb: lateral step hips IR 57.8 (24.3); lateral step hips neutral 49.9 (21.9); lateral step hips ER 47.6 (21.5). Moving limb: lateral step hips IR 43.8 (27); lateral step hips neutral 32.8 (21.9); lateral step hips ER 27.3 (18.1). |
| Youdas et al. (2014) (Cross-sectional) (Exercise data partially extracted) | 26 (13 M) healthy active. 25.3 (3.1) years (M), 23.7 (1.3) years (F). | Surface109 bilaterally. | MVIC 1 trial x 2-3 secs in side-lie abd 300. Practice reps before. | Exercises – 4 randomised including reverse cross over pull against elastic resist. Repetitions – 3 reps to metronome (40 bpm). Practice reps before. Rest – 2-3 mins between exs. |
Stance limb: reverse cross over pull 50.0 (25.1). Moving limb: reverse cross over pull 52.9 (17.6). |
| Youdas et al. (2015) (Cross-sectional) (Exercise data partially extracted) | 26 (13 M) healthy active. 23.4 (1.3) years (M), 23.5 (1.2) years (F); 1.8 (0.1) m (M), 1.7 (0.1) m (F); 79.7 (10.6) kg (M), 63.7 (7.4) kg (F). | Surface109 on (R) limb. | MVIC 5 sec in side-lie abd 200. | Exercises – 6 randomised including DL bridge; DL bridge unstable; SL bridge; SL bridge unstable. Repetitions – 3 reps to metronome (40 bpm). Rest – 1 min between exs. |
SL bridge unsTable 42 (10.2); SL bridge 40 (11.6); DL bridge 21.4 (7.4); DL bridge unsTable 19.9 (10) |
| Zeller et al. (2003) (Cross-sectional) | 18 (9 M) healthy college athletes. 20.33 (1) years (M), 20 (1.5) years (F); 72.44 (2.01) in (M), 67.44 (2.4) in (F); 173.89 (8.94) lbs (M), 141.89 (12.33) lbs (F). | Surface107 on dominant limb. | MVIC 2 trials x 3 secs in side-lie abd. | Exercises – 1: SL squat Repetitions – 5 with 5 sec duration. Practice reps before. |
SL squat 77.3 (64.3) (M), 41 (29.5) (F). |
Key: abd – abduction; add – adduction; ant – anterior; ASIS – anterior superior iliac spine; BMI – body mass index; bpm – beats per minute; cm – centimeters; DL – double leg; DOM – dominant limb; ER – external rotation; exs – exercises; ext – extension; F – females; flex – flexion; GMed – gluteus medius; in – inches; inf – inferior; IR – internal rotation; kg – kilograms; kg/m2 – kilograms per metres squared; lat – lateral; lbs – pounds; M – males; max – maximum; m – metres; mins – minutes; MVIC – maximum voluntary isometric contraction; non-DOM – non dominant limb; NWB – non-weight-bearing; PBU – pressure biofeedback unit; post – posterior; reps – repetitions; resist – resistance; secs – seconds; SL – single leg; sup – superior; WB – weight-bearing
Table 3.
Summary of included gluteus minimus studies.
| Study and type | Participant characteristics | EMG electrode type and placement | Normalisation method | Exercise characteristics | Results (% MVIC (SD)) |
|---|---|---|---|---|---|
| Ganderton et al. (2017) (Cross-sectional) | 10 healthy post-menopausal women. 60.2 (2.7) years; 164.7 (4.3) cm; 70.0 (10.2) kg | Fine-wire into 2 segments (anterior & posterior) of GMin via standardised landmarks on dominant limb. | MVICs 3 trials x 5 secs in side-lie abd, side-lie clam, seated hip ER, seated hip IR to find max for each segment. 3 min rest between trials. | Exercises – 7 randomised including hip hitch; hip hitch with toe tap; hip hitch with hip swing; isometric hip abduction; dip test; clam hip flex 450. Repetitions – 2 sets of 6 reps to metronome 2 secs concentric and 2 secs eccentric for dynamic exs. 3 reps of 15 secs hold for isometric exs. Rest – 1 min between isometric reps and dynamic sets; 2 mins between each ex. |
Anterior GMin: hip hitch 68.77 (21.74); hip hitch swing 59.70 (17.26); isometric stand hip abd 54.79 (33.49); hip hitch toe tap 48.30 (16.07); dip test 21.33 (12.30); clam 7.31 (8.94). Posterior GMin: hip hitch swing 78.64 (20.93); hip hitch 83.71 (40.17); hip hitch toe tap 66.73 (25.99); dip test 64.41 (35.54); isometric hip abd 48.62 (30.58); clam 19.59 (20.38). |
| Moore et al. (2018) (Cross-sectional) | 10 (6 M) healthy active university. 23.8 (1.6) years; 177.5 (10) cm; 79.9 (18.5) kg. | Fine-wire into 2 segments (anterior & posterior) of GMin via standardised landmarks on dominant limb. | MVICs 3 trials x 5 secs in side-lie abd, side-lie abd + IR, side-lie clam, side-lie hip flex, side-lie hip IR, prone hip ext to find max for each segment. 3 mins rest between trials. | Exercises – 6 randomised including SL squat; SL bridge; side lie hip abd; clam hip flex 450. Repetitions – 3 trials of 6 for each ex to a metronome (ranging from 40 – 90 bpm depending on ex). Practice reps before. Rest- 1 – 2 mins between exs and trials. 3 mins between exs and MVIC. |
Anterior GMin: side-lie abd 37.62 (14.07); SL squat 25.42 (9.49); SL bridge 13.62 (11.36); clam 2.98 (2.91). Posterior GMin: SL bridge 46.04 (27.83); side-lie abd 43.49 (15.96); SL squat 45.76 (29.99); clam 8.00 (6.44). |
Key: abd – abduction; add – adduction; ant – anterior; bpm – beats per minute; cm – centimeters; DL – double leg; DOM – dominant limb; ER – external rotation; ext – extension; flex – flexion; GMed – gluteus medius; GMin - gluteus minimus; inf – inferior; IR – internal rotation; kg – kilograms; lat – lateral; MVIC – maximum voluntary isometric contraction; mins – minutes; non-DOM – non dominant limb; NWB – non-weight-bearing; post – posterior; reps – repetitions; secs – seconds; SL – single leg; sup – superior; WB – weight-bearing.
A single surface electrode positioned at the middle segment of GMed on the dominant limb was used in most GMed studies with six different electrode positions described (Table 2). Five studies46,52,55,62,63 recorded EMG measurements for the anterior, middle and posterior segments of GMed with only one study46 using fine wire electrodes. Two studies46,47 recorded the anterior and posterior segments of GMin using fine wire electrodes.
Normalization of the EMG signal was typically performed with side-lying hip abduction MVIC for GMed (Table 2). Standing hip abduction48,63-67 was used in other studies, while one study48 used an isometric single leg wall squat in a custom-made apparatus to determine MVIC. Two studies46,63 for GMed and two studies46,47 for GMin determined each segments’ maximum value from performing MVICs for different hip actions.
Therapeutic exercise characteristics were diverse across the included studies (Tables 2 and 3). All included studies attempted to standardize exercise performance and control EMG signal variability between participants by employing strategies such as allowing practice repetitions before testing; controlling exercise ROM; and using a metronome to control contraction speed (Tables 2 and 3). For most studies, the potential impact of fatigue was minimized by randomizing the exercise order; having rest periods between exercises and trials; and restricting numbers of trials (Tables 2 and 3).
Only two studies49,65 reported on all technical parameters for collection, processing and analysis of the EMG signal (Table 4).
Table 4.
Electromyographic technical aspects of included studies
| Study | EMG unit type | Electrode size and skin preparation | Inter-electrode distance (mm) | Input impedance (Ω) | Common mode rejection ratio (dB) | Amplifier gain | Data filtering (Hz) | Sampling frequency (Hz) | Rectification (full or half wave) | Data processing (ms) |
|---|---|---|---|---|---|---|---|---|---|---|
| Ayotte et al. (2007) | Nicolet Viking IV | NS; skin debrided and cleansed | 30 | NS | >110 @ 50-60 Hz | NS | Band pass 30 –10000 | 20000 | Full | Integrated over 1.5sec |
| Barton et al. (2013) | Noraxon Telomyo 2400 G2 | SENIAM, 2011 | 20 | NS | NS | NS | Band pass 10 – 500 RMS smoothing 100 epoch |
1500 | Full | Mean amplitude |
| Berry et al. (2015) | Bagnoli Delsys | 10x1mm; skin scrubbed | 10 | 1015 | 100 | NS | Band pass 20 - 390 4th order Butterworth RMS smoothing 100ms | 1000 | Full | Average RMS |
| Bolgla et al. (2016) | 8 channel Run Technologies | 5 mm diameter; skin shaved and cleaned | 20 | 1M | 90 | 2000 | Band pass 20 - 500 | 2000 | Full | Average RMS for each repetition |
| Bolgla et al. (2014) | 8 channel Run Technologies | 5 mm diameter; skin shaved and cleaned | 20 | 1M | 90 | 2000 | Band pass 20 - 500 | 2000 | Full | Average RMS for each repetition |
| Bolgla and Uhl (2005) | 16 channel Run Technologies | 5 mm diameter; skin prepared in standard manner | 20 | NS | 90 | 2000 | Band pass 20-500 RMS smoothing 15ms |
1000 | Full | Average RMS for each repetition |
| Boren et al. (2011) | Schiller America | NS; skin cleansed | NS | NS | NS | NS | RMS smoothing 50ms | NS | Full | Average amplitude: surround peak activity (100 ms of time) |
| Boudreau et al (2009) | 16 channel Run Technologies | 5 mm diameter; skin debrided and cleansed | 20 | NS | 90 | 2000 | Band pass 20-500 RMS smoothing 20ms |
1339 | Full | Average amplitude |
| Bouillon et al (2012) | 8 channel Noraxon myosystem 900 12 bit A-D converter | NS; skin shaved, abraded and cleaned | 20 | 10M | 115 | 1000 | Band pass 10-500 RMS 300 |
1000 | Full | Average activity per repetition |
| Cambridge et al. (2012) | 16 channel AMT 8 Bortec A-D converter | NS | NS | 1M | 115 @ 60 Hz | NS | Band pass 30-500 Low-pass smoothing: Butterworth 2.5Hz Sampled at 60Hz (synchronisation with kinematic data) |
2160 | Full | Peak amplitude |
| Chan et al. (2017) | Myomuscle Noraxon | Skin shaved, abraded and cleaned | 10 | NS | 80 | NS | Band pass 10-500 Butterworth 4th order RMS smoothing 500ms | 1024 | Full | Average amplitude for each repetition |
| Cynn et al. (2006) | Bagnoli | Skin cleansed | 20 | NS | NS | NS | Band pass 20-450 Backstop filter (60Hz) | NS | Full | Average amplitude (RMS) |
| Distefano et al. (2009) | Bagnoli 8 Delsys | NS; skin cleansed | 10 | NS | >80 @ 60 Hz | 10000 | Band pass 20-350 RMS smoothing (20ms) |
1000 | Full | Average amplitude of each repetition |
| Dwyer et al. (2013) | 16 channel Run Technologies | 5 mm diameter; skin prepared | 20 | 1M | 90 | 2000 | Band pass 20-500 RMS smoothing (30ms) |
1000 | Full | Average amplitude |
| Dwyer et al. (2010) | 16 channel Run Technologies | 5 mm diameter; skin debrided and cleansed | 20 | 1M | 90 | 2000 | Band pass 20-500 RMS smoothing (20ms) |
1339 | Full | Average amplitude for each phase (concentric and eccentric) |
| Ekstrom et al. (2007) | 8 channel Noraxon myosystem 1200 | NS; skin debrided and cleansed | 20 | 10M | >100 @ 60 Hz | 1000 | Band pass 10-500 Butterworth (1st order high-pass, 4th order low-pass) RMS smoothed (20ms) |
1000 | Full | Average activity of 1 secs surrounding peak amplitude |
| Felicio et al. (2011) | Myosystem BR 1P84 | 23x21x5 mm; skin prepared | 10 | 10G | 130 | 20 | Band pass 20-500 | 2000 | Full | Average activity (RMS) across the whole repetition |
| Ganderton et al. (2017) | Delsys Trigno EMG | Stainless steel,teflon-coated 20 cm and 25 cm lengths | NS | >80 @ 60 Hz | 1000 | Band pass 20-900 Butterworth high-pass, 4th order, 50Hz Butterworth low-pass smoothed, 4th order, 6Hz | 2000 | Full | Average activity for each repetition | |
| Harput et al. (2016) | Telemyo DTS Noraxon | 10 mm width; skin shaved, abraded and cleaned | 20 | 10m | 80 | NS | Band pass 10-500 RMS smoothed (25ms) |
1000 | Full | Average activity in each phase (concentric, eccentric) |
| Hatfield et al. (2016) | Delsys Trigno | NS | NS | NS | 80 | NS | Band pass 20-450 Low pass filtered, Butterworth, 4th order, 25 Hz |
2000 | Full | Integrated activity over entire task |
| Heo et al. (2013) | Biopac MP150WSW | 3 mm diameter; skin shaved and cleaned | NS | NS | NS | NS | Band pass 20 – 500 | 1000 | Full | Average activity (RMS) |
| Hertel et al. (2005) | Biopac MP 100 | 10 mm contact area; skin debrided and cleansed | 20 | 2M | 11 | 1000 | 10-500 RMS smoothing (500ms moving window) | 1000 | Full | Peak RMS activity within trials |
| Ju & Yoo (2017) | Biopac MP 150 | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Ju & Yoo (2016) | EL503 Biopac | 3mm diameter | NS | NS | NS | NS | Band pass 20 -500 RMS of 250 samples |
1000 | Full | Average (RMS) of the middle 3 seconds of a 5 secs trial |
| Kang et al. (2014) | Delsys surface EMG | NS | NS | NS | NS | NS | Band pass 20-450 | 2000 | NS | Average activity of each phase (descend and ascend components) |
| Kim et al. (2015) | Telemyo 2400 T2 | NS; skin shaved and scrubbed | 20 | NS | NS | 500 | Band pass 30 – 500 RMS smoothed (100ms window) |
1500 | Full | Average (RMS) for each trial |
| Krause et al. (2018) | 16 bit NI-DAQ PCI-6 220 A-D card Bagnoli 16 amplifier | 10 mm; skin scrubbed | 10 | >1015 @ 100 Hz | 92 @ 60 Hz | 100 - 10000 | Band pass 20 – 450 (Butterworth, 4th order) RMS smoothing (200ms) | 1000 | Full | Average activity of 1 secs surrounding peak activity of the ascending phase |
| Krause et al. (2008) | GCS67 Therapeutics unlimited | NS; skin cleansed | 22 | >15M @ 100 Hz | 87 @ 60 Hz | 35 | RMS smoothed (55ms) | 1000 | Full | Peak activity over three squats |
| Lee et al. (2013) | Telemyo DTS | NS; skin shaved and cleansed | NS | NS | NS | NS | Band pass 20 -450 RMS smoothed (50ms) |
1000 | Full | Average activity of middle 3 secs of the isometric phase |
| Lee et al. (2014) | Telemyo DTS | NS; skin shaved and cleaned | 20 | NS | 92 @ 60 Hz | Band pass 20 – 450 RMS smoothed (50ms) |
1000 | Full | Average activity of middle 3 secs of the isometric phase | |
| Lehecka et al. (2017) | Noraxon telemyo 2400T GT | NS; skin shaved, abraded | NS | NS | NS | NS | Band pass 15 - 500 High-pass filtered (Butterworth, 4th order, 15Hz) Low-pass filtered (Butterworth, 4th order, 500Hz) Moving average smoothed (50ms) | 3000 | Full | NS |
| Lin et al. (2016) | Bagnoli Delsys | 10x1 mm; skin shaved and cleaned | 10 | NS | NS | NS | Band pass 20 – 450 Low-pass filtered (12Hz) |
1000 | Full | Average activity from 5 repetitions |
| Lubahn et al. (2011) | Bagnoli 8 Delsys | NS; skin debrided and cleansed | NS | NS | NS | 1000 | Band pass 20 -450 High-pass filtered (Butterworth, 4th order, 30Hz) Low-pass filtered (Butterworth, 4th order, 6Hz) | 960 | NS | Integrated activity over the duration of the exercise |
| MacAskill et al. (2014) | 16 channel Motion Lab | 15 mm diameter; skin shaved and scrubbed | 20 | 1M | 90 | 50 | Band pass 20 – 450 RMS smoothing (50ms) |
4000 | Full | Integrated EMG activity across a repetition. |
| Mauntel et al. (2013) | Delsys Bagnoli | Skin shaved, abraded and cleaned | NS | NS | NS | NS | Band pass 10 -350 Low-pass (Butterworth, 4th order, 14.5 Hz) Notch filtered 59,5-60.5 Hz RMS smoothed (25ms) |
1000 | Full | Average activity from the descent phase |
| McBeth et al. (2012) | 16 channel Run Technologies | NS; skin debrided and cleansed | 26 | NS | NS | 1000 | Band pass 10 -499 (Butterworth filter) RMS smoothed (20ms) |
1000 | Full | Average activity from 3 trials |
| Monteiro et al. (2017) | 8 channel EMG system Brazil 16 bit resolution | 10 mm diameter; skin shaved, abraded and cleaned. | 20 | NS | NS | NS | Band pass 10 - 500 | NS | Full | Average (RMS) of the concentric phase |
| Morimoto et al. (2018) | Biolog DL 5000 | NS | NS | NS | NS | NS | Band pass 20 – 500 | 1000 | Full | Average (RMS) |
| Noh et al. (2012) | Delsys Trigno | NS; skin rubbed and cleaned | NS | NS | NS | NS | Band pass 20 – 450 | 1000 | Full | Average (RMS) of three trials |
| Oliver et al. (2010) | Noraxon myopic 1400L 8 channel | NS; skin cleansed and debrided | 25 | NS | NS | NS | Band pass 20-350 RMS smoothed (100ms) Notch filtered: 59.5Hz – 60.5Hz |
1000 | Full | Average EMG activity |
| Oliver & Stone (2016) | Delsys Bagnoli 8 channel | NS; skin shaved, abraded and cleaned | 10 | NS | NS | NS | RMS smoothed (100ms) | 1000 | Full | Average EMG activity |
| O’Sullivan et al. (2013) | Motionlab system MA-300 multichannel | 144 mm2; skin cleansed, abraded and shaved | 18 | NS | NS | 2000 | RMS smoothed (150ms) | 1000 | Full | Average (RMS) per trial |
| O’Sullivan et al. (2010) | Motionlab system MA-300 multichannel | 144 mm2; skin cleansed and debrided | 18 | NS | >100 @ 60 Hz | 2000 | Band-pass 5-500 RMS smoothed (150ms) |
1250 | Full | Average (RMS) per trial |
| Petrofsky et al. (2005) | 12 bit A-D card | NS | 20 | NS | NS | 5000 | RMS | 2000 | Full | Average over a 1 second period |
| Philippon et al. (2011) | Delsys Bagnoli | .07 mm fine-wire | NS | >10M | >84 | NS | RMS (50ms) Low pass 10 Hz |
1200 | Full | Average and peak amplitude |
| Selkowitz et al. (2013) | Motionlab system MA-300 multichannel 16 channel | 50 µm fine wire | NS | > 1M | >110 @ 65 Hz | 1.2 k | Band pass 35 -750 (Butterworth) RMS smoothing (75ms) |
1560 | Full | Average activity for each repetition |
| Sidorkewicz et al. (2014) | AMT 8 Bortec 16 Bit converter | NS; skin shaved, rubbed and cleaned | 30 | 10G | 115 @ 60 Hz | NS | Band pass 10 – 500 Low-pass (Butterworth 2nd order, 3 Hz) |
2160 | Full | Peak amplitude |
| Sinsurin et al. (2015) | Noraxon Myosystem | NS; skin shaved, abraded and cleaned | 20 | 10k | NS | NS | Bandpass 20 – 450 (Butterworth) | 1500 | Full | Average activity |
| Souza & Powers (2009) | Motion Control | Skin shaved, abraded and cleaned. | NS | NS | NS | 2000 | Band pass 35-500 Notch filter: 60Hz Moving average smoothing (75ms) |
1560 | Full | Average activity |
| Webster & Gribble (2013) | Noraxon 2000 telemyer system. | 38x28 mm; skin shaved, abraded and cleaned | NS | 100m | >100 | NS | RMS smoothing (50ms) Butterworth 3rd order filter | 1000 | Full | Average activity over 0.4 secs surrounding maximum excursion |
| Willcox & Burden (2013) | Delsys | 10x1 mm; skin shaved and cleaned | 10 | 100M | > 80 | NS | Band pass 20 – 500 RMS smoothing (150ms window, 62ms overlap) |
1080 | Full | Average activity per repetition |
| Youdas et al. (2012) | Delsys Bagnoli | 41x20x5 mm; skin shaved and cleaned. | 10 | 1015 | 92 @ 60 Hz | 100-10000 | Band pass 20 – 450 RMS smoothing (125ms) | 1000 | Full | Peak activity |
| Youdas et al (2014) | Delsys Bagnoli 16 bit A-D card | 41x20x5 mm; skin abraded and cleaned | 10 | 1015 | 92 @ 60 Hz | 100-10000 | Band pass 20 – 450 (Butterworth 4th order) | 1000 | Full | Average activity of 500ms interval surrounding peak |
| Youdas et al. (2015) | Delsys Bagnoli 16 bit A-D card | 41x20x5 mm; skin abraded and cleaned | 10 | 1015 | 92 @ 60 Hz | 100-10000 | Band pass 20 – 450 RMS smoothing (125ms) |
1000 | Full | Average activity of 400ms interval surrounding peak |
| Zeller et al. (2003) | NS | Skin shaved and cleansed. | NS | NS | NS | NS | Low pass filtered (Butterworth, 4th order 15Hz) | 960 | Full | Average activity |
Key: A-D – analogue-digital conversion; cm – centimeters; EMG – electromyography; Hz – hertz; mm – millimeters; ms – milliseconds; NS – not stated; RMS – root mean square; secs – seconds; µs – microseconds.
Non-weight bearing exercises
Side-lying hip abduction
Gluteus medius
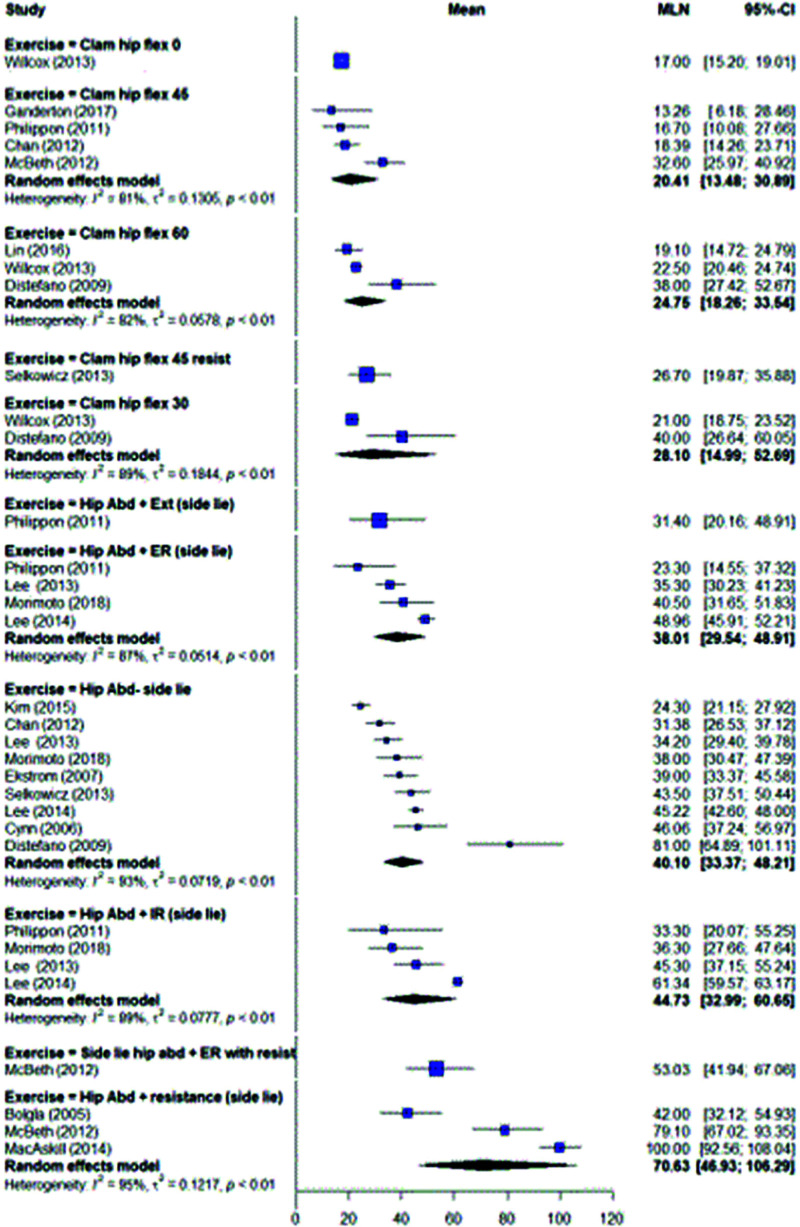
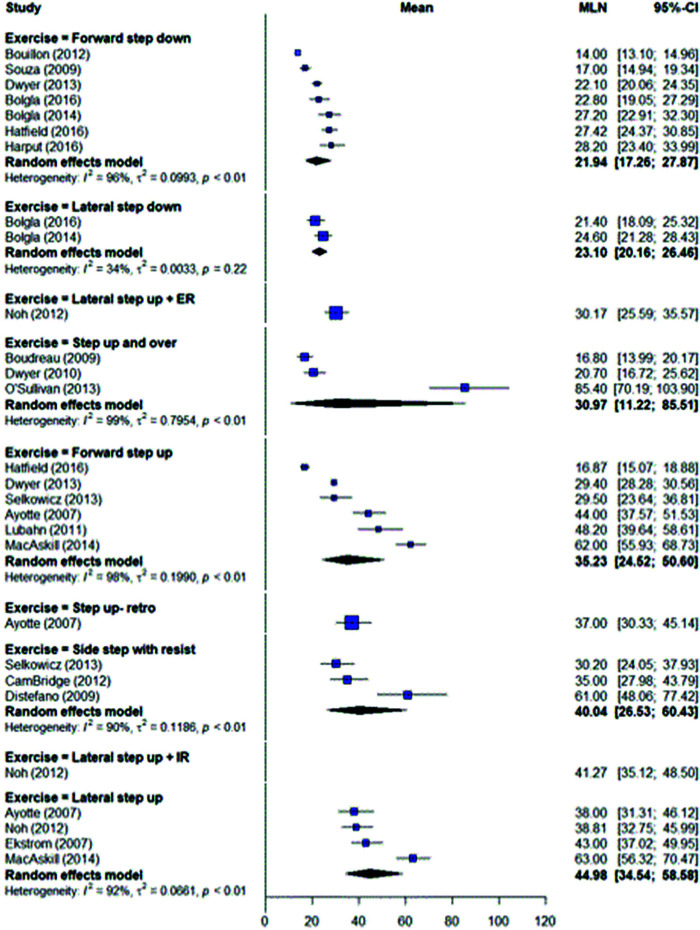
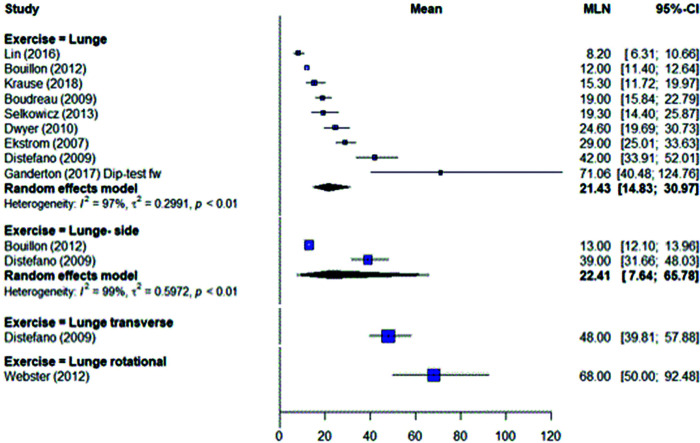
Side-lying hip abduction was the most commonly investigated exercise in the non-weight bearing position for GMed.56,58,66,68-79 Moderate mean activity levels (40.10 (95% CI (33.37, 48.21)) % MVIC) were generated for middle GMed when the results were pooled for 8 studies (Figure 2) (Table 5). The addition of external resistance further increased activity levels to very high, although there was a high degree of heterogeneity (I2 = 95%).
Figure 2.
Gluteus medius middle – side-lie clam and hip abduction exercises.
Table 5.
Segmental mean gluteus medius activity levels (% MVIC) for exercises.
| Exercise category | Exercise | Muscle segment (middle unless indicated) | Low (0‐20% MVIC) | Moderate (21‐10% MVIC) | High (41‐60% MVIC) | Very High (>60% MVIC) |
|---|---|---|---|---|---|---|
| Side‐lie | Hip abduction | 3971; 3475; 37511; 29‐3173; | 42R72; 4576; 4478 | 63“; 870; 79R®; 100R77 | ||
| 3879; 25‐4674; 2456 | ||||||
| Hip abduction + ER | 3575; 3758; 2366 | 53R69; 4179; 4976 | ||||
| Hip abduction + IR | 3679; 3366 | 4575 4958 | 6276 | |||
| Hip abduction + Ext | 3166 | |||||
| Clam hip flex 30 ° | 13‐1780; 1766 | 4070; 2758 | ||||
| Clam hip flex 30 ° | 13‐2130 | |||||
| Clam hip flex 45 ° | Anterior | 346 | ||||
| Middle | 1346; 16‐1873; 1766 | 3369;27R78;3658 | 4758; | |||
| Posterior | 2366 | |||||
| Clam hip flex 60 ° | 1981 | 3658; 3870; 18‐2358 | 90” | |||
| Squat | Single leg squat | Anterior | ||||
| Middle | 1881 | 3683; 3064; 30‐3165; 2384; | 59U67; 4867; 41‐7787 | 8268; 6470; 7741; 6657; 9252 | ||
| 2485; 20‐2788; 33‐3786 | ||||||
| Posterior | 8752 | |||||
| Single leg squat + Abd | Anterior | 1962 | 42‐46111 | |||
| Middle | 2762 | |||||
| Posterior | 3362 | |||||
| Single leg squat + Add | Anterior | 4262 | ||||
| Middle | 3162 | |||||
| Posterior | 2262 | |||||
| Single leg wall squat | Anterior | 1363 | ||||
| Middle | 2563; 2784; 22‐3288 | 5283 | ||||
| Posterior | 3563 | |||||
| Single leg wall squat + Abd | Anterior | 2962 | ||||
| Middle | 3362 | |||||
| Posterior | 4462 | |||||
| Single leg wall squat + Add | Anterior | 1662 | ||||
| Middle | 2162 | |||||
| Posterior | 2862 | |||||
| Single leg skater squat | 6068 | |||||
| Single leg squat + rotation | ||||||
| Squat | 1078; 9‐12R61 | 26‐3354; 2157; 22‐2889 | 6650 | |||
| Wall squat | 9‐10111 | |||||
| Squat + Abd | 24” | 47‐5254 | ||||
| Squat + Add | 5954 | |||||
| Step | Lateral step‐up | 3883; 3994 | 6058; | 6377 | ||
| Lateral step‐up + IR | 3094 | 4194 | ||||
| Lateral step‐up + ER | ||||||
| Lateral step‐down | 2184; 19‐2588 | 7448 | ||||
| Lateral step | Anterior | |||||
| Middle | 24‐35RS53; 30RS78; 33‐ | |||||
| 50RS93 | ||||||
| Posterior | 19‐23RU91; 23‐36RS91 | |||||
| Lateral step + IR | 44‐58RS91 | |||||
| Lateral step + ER | 27‐48RS93 | |||||
| Forward step‐up | 1785 | 2949; 3078 | 4483; 5568; 4857; 45MR57 | 6277 | ||
| Forward step‐down | 1492; 175 | 2384; 20‐2249; 2851;21‐ | ||||
| 2785; 19‐2788 | ||||||
| Forward step‐up and over | Anterior | 15‐1764; 15‐2165 | 8852 | |||
| Middle | 8552 | |||||
| Posterior | 8152 | |||||
| Retro step‐up | 3783 | 45RE46 | ||||
| Lunge | Forward lunge | Anterior | ||||
| Middle | 18-9164; 12-2565;1292 | 2971 | 4270 | 71RE46 | ||
| 1978; 1595; 881 | ||||||
| Posterior | 28RE46 | |||||
| Transverse lunge | 4870 | 6869 | ||||
| Sideways lunge | 1392 | 3970 | 6946; 8052 | |||
| Standing | Hip hitch/ pelvic drop | Anterior | 2163; 2555; 2560 | |||
| Middle | 2863; 2355; 3878 | 5772; 5868; 4296 | 6646; 8852 | |||
| Posterior | 3863; 2255 | 7446; 8852 | ||||
| Hip hitch/ pelvic drop + IR | ||||||
| 4296 | Hip hitch/ pelvic drop + ER | 3396 | 8246 | |||
| Hip hitch/ pelvic drop + leg | Anterior | |||||
| swing | Middle | 6646 | ||||
| Posterior | 7246 | |||||
| Hip hitch/ pelvic drop + toe tap | Anterior | 7646 | ||||
| Middle | 5846 | |||||
| Posterior | 4646 | |||||
| Hip abduction | Anterior | 5646 I | ||||
| Middle | 30I46 | 4246R72; 4459; 50R82 | ||||
| Posterior | 41146 | |||||
| Hip abduction (moving limp) | 28‐3372 | 53R82 | 6459 | |||
| Supine | Single leg bridge | 33‐3597; 3178; 3597 | 40-4299; 5568";47lU68;4771; | |||
| 42‐5898 | ||||||
| Double leg bridge | 1797; 1578; 1166 | 20‐2199; 2871; |
Key: Abd ‐ abduction; Add ‐ adduction; ER ‐ hip external rotation; Ext extension; Flex ‐ flexion; IR ‐ hip internal rotation; I ‐ isometric exercise; MR ‐ added medial resistance; R added externa] resistance; RE rear foot elevated; RS ‐ resisted squat posture; RU ‐ resisted upright posture; U ‐ unstable surface.
High mean GMed middle activity levels were generated by hip abduction with internal rotation (44.73 [32.99, 60.65] % MVIC), while moderate activity levels were elicited for hip abduction with external rotation (38.01 [29.54, 48.91] % MVIC)66,75,76,79 (Figure 2).
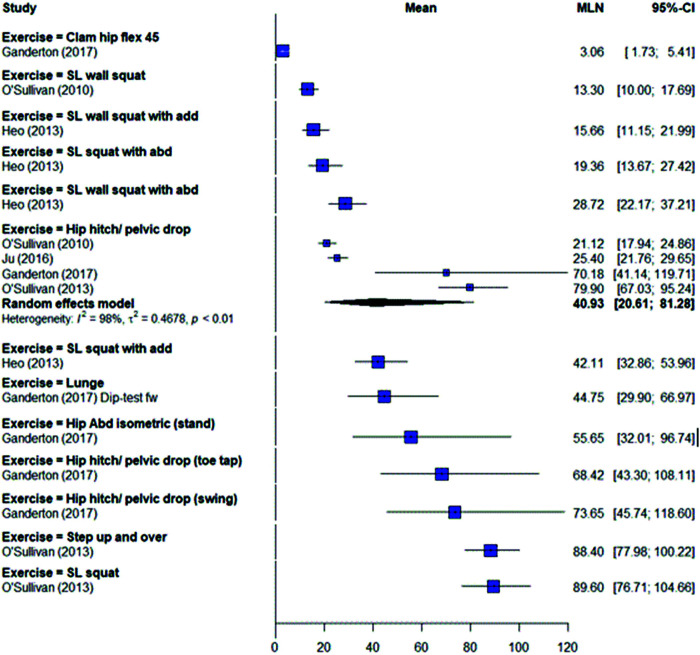
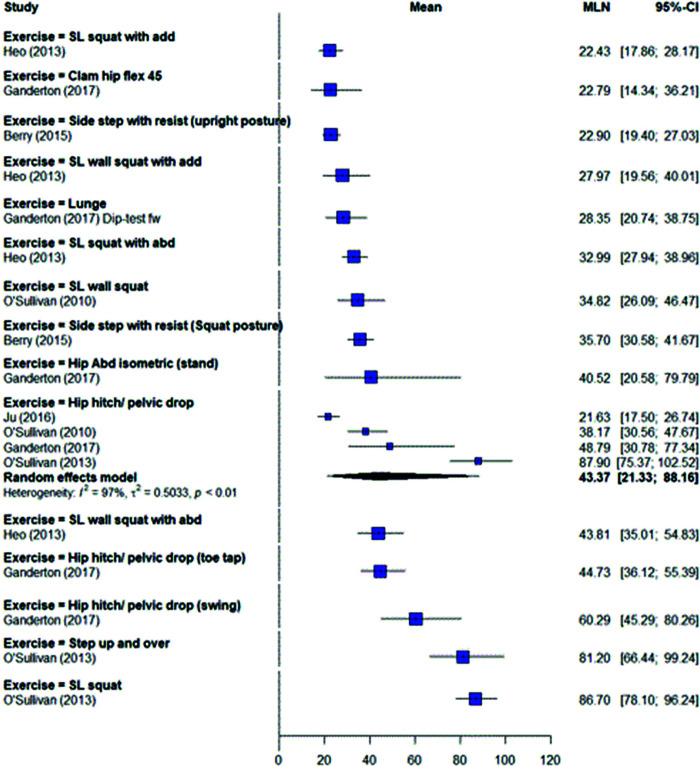
Gluteus minimus
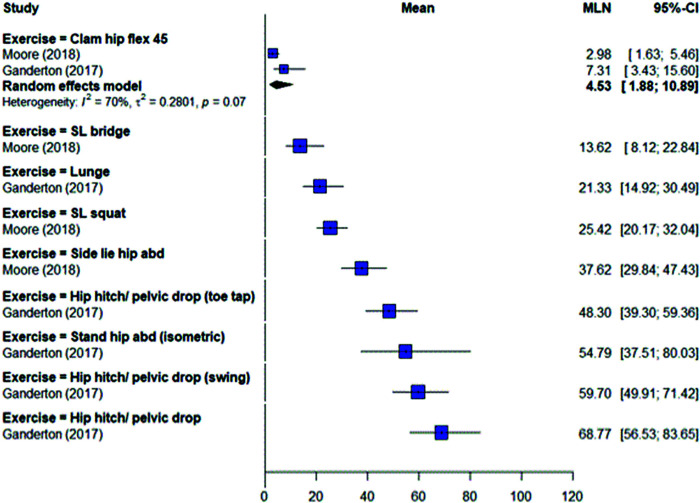
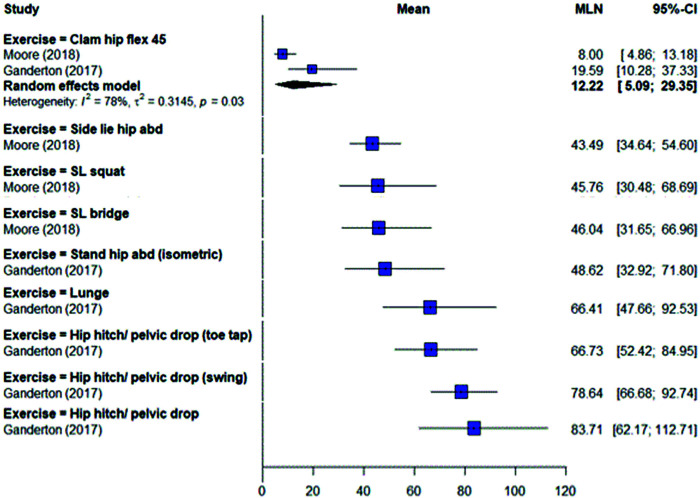
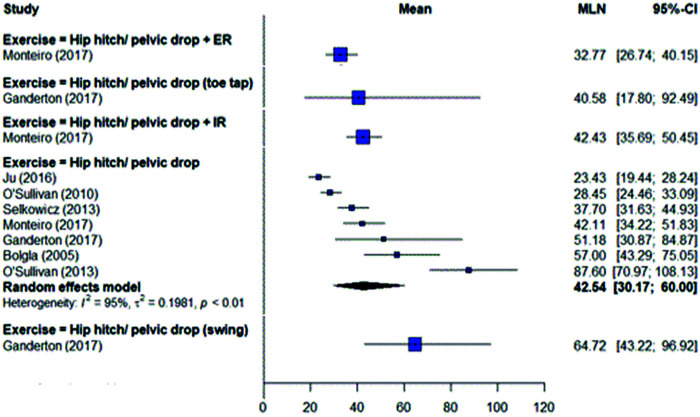
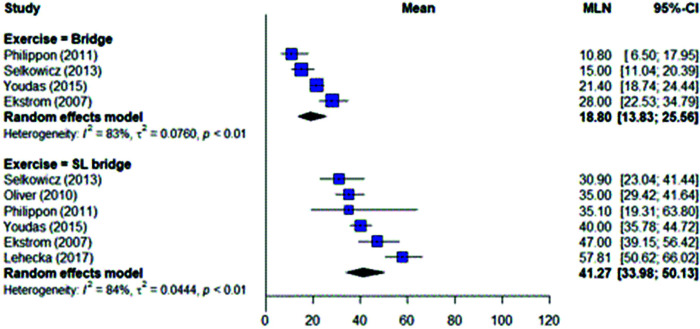
One study47 evaluated GMin activity for side-lying abduction and found moderate activity (38% MVIC) for the anterior segment and high activity (44% MVIC) for the posterior segment (Figures 3 and 4) (Table 6).
Figure 3.
Gluteus minimus anterior exercises.
Figure 4.
Gluteus minimus posterior exercises.
Table 6.
Segmental mean gluteus minimus activity levels (% MVIC) for exercises.
| Exercise category | Exercise | Muscle segment | Low (0‐20% MVIC) | Moderate (21 ‐40% MVIC) | High (41‐60% MVIC) | Very High (>60% MVIC) |
|---|---|---|---|---|---|---|
| Side‐lie | Hip abduction | Anterior | 3847 | |||
| Posterior | 4347 | |||||
| Clam hip flex 45 ° | Anterior | 746; 347 | ||||
| Posterior | 2046; 847 | |||||
| Squat | Single leg squat | Anterior | 2547 | |||
| Posterior | 4647 | |||||
| Lunge | Forward lunge | Anterior | 21RE46 | |||
| Posterior | 66RE46 | |||||
| Standing | Hip hitch/pelvic drop | Anterior | 6946 | |||
| Posterior | 8446 | |||||
| Hip hitch/pelvic drop + leg | Anterior | 6046 | ||||
| swing | Posterior | 7946 | ||||
| Hip hitch/pelvic drop + toe | Anterior | 4846 | ||||
| tap | Posterior | 6746 | ||||
| Hip abduction | Anterior | 55146 | ||||
| Posterior | 49I46 | |||||
| Supine | Single leg bridge | Anterior | 1447 | |||
| Posterior | 4647 |
Key: I ‐ isometric exercise; RE rear‐foot elevated
Side-lying hip clam
Gluteus medius
The side-lying hip clam was evaluated in 10 studies46,58,66,68-70,73,78,80,81 with varying positions of hip flexion. Low to moderate activity levels (17-28% MVIC) were reported across the studies for middle GMed (Figure 3) (Table 5). There were wide variations between studies for exercise technique; angle of hip and knee flexion; repetitions; and use of external loading. One study46 recorded segmental GMed activity levels using fine wire EMG and found low activity levels for the anterior (3% MVIC) and middle segments (13% MVIC), and moderate activity (23% MVIC) for the posterior segment. Altering the angle of hip flexion or trunk position had minimal effect on mean GMed activity levels generated for this exercise80 (Figure 3).
Gluteus minimus
Two studies46,47 evaluated segmental activity levels for GMin. When pooled together, low activity was recorded for anterior (4.53 (95% CI (1.88, 10.89))% MVIC) and posterior (12.22 (5.09, 29.35)% MVIC) segments (Figures 3 and 4) (Table 6).
Standing hip abduction (open chain)
Gluteus medius
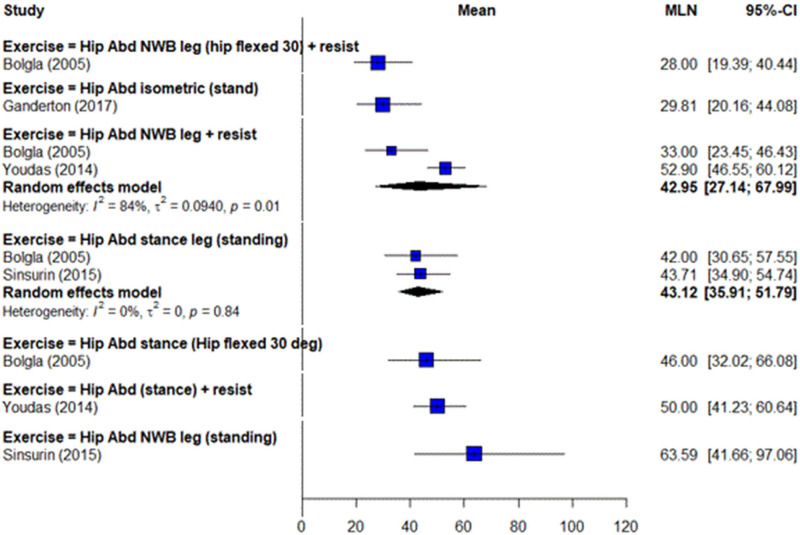
Standing hip abduction on the swing leg was evaluated in three studies59,72,82 (Table 5). Two studies had added external resistance and could be pooled together generating high middle GMed activity levels (42.95 [95% CI 27.14, 67.99] % MVIC) (Figure 7). There was however a high degree of heterogeneity (I2 = 84%). The one study59 without added resistance recorded very high activity levels (64% MVIC).
Figure 7.
Gluteus medius middle - standing hip abduction.
Weight-bearing exercises Squat exercises
Gluteus medius
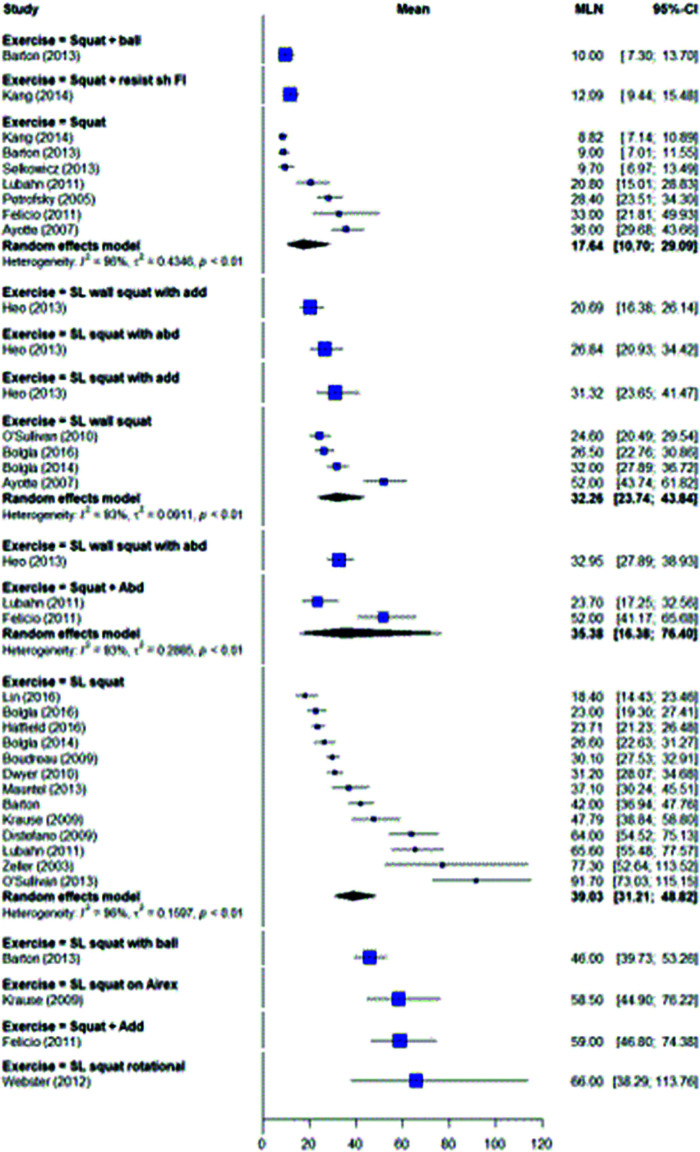
Single leg squats were evaluated in 15 studies48,52,57,64,65,67,68,70,81,83-88 using predominantly single surface electrode measures at middle GMed (Table 5). Moderate activity (39.03 [95% CI 31.21, 48.82] % MVIC) was reported when 13 studies were pooled together (Figure 8). Large variations did however exist between the studies including squat depth, exercise technique and number of repetitions. One study52 recorded activity in all three GMed segments using surface electrodes and found very high activity in all three segments (90% MVIC anterior, 92% MVIC middle, and 87% MVIC posterior). Another study62 measured GMed segmental activity for the single leg squat with isometric hip abduction and with isometric hip adduction. They found moderate activity for both exercises for the middle (27-31% MVIC) and posterior (22-33% MVIC) segments but high anterior segmental activity (42% MVIC) for isometric adduction, and low anterior segmental activity (19% MVIC) for isometric abduction.
Figure 8.
Gluteus medius middle - squat exercises.
Single leg wall squats were evaluated in four studies.63,83,84,88 When pooled together for the middle GMed segment were found to generate moderate activity (32.26 [23.74, 43.84] % MVIC) (Figure 8) (Table 5). Two studies62,63 recorded segmental GMed activity using surface electrodes but one of the studies62 had the single leg wall squat performed using either isometric hip abduction or isometric hip adduction. Low to moderate activity (13-29% MVIC) was reported in the anterior segment and moderate to high activity (28-44% MVIC) in the posterior segment (Figures 5 and 6).
Figure 5.
Gluteus medius anterior exercises.
Figure 6.
Gluteus medius posterior exercises .
Squats with or without medial or lateral resistance, or wall support were evaluated in six studies54,57,61,78,89,90 using single surface electrodes placed on middle GMed (Table 5). When pooled together, squats generated low activity levels (17.64 [10.70, 29.09] % MVIC) and squats with resisted abduction moderate activity levels (35.38 [16.38, 76.40]% MVIC) for the middle GMed segment (Figure 8).
Gluteus minimus
Moderate (25% MVIC anterior) to high (46% MVIC posterior) activity was generated for both segments of GMin during the single leg squat in one study47 (Figures 3 and 4) (Table 6).
Step exercises
Gluteus medius
Step exercises were evaluated in 21 studies5,48,49,51-53,57,64,65,68,71,77,78,83-85,88,91-94 for predominantly single electrode surface measures of middle GMed (Table 5). For studies that could be pooled together, high mean activity levels (44.98 (95% CI (34.54, 58.58))% MVIC) were generated for the lateral step-up and moderate mean activity levels (35.23 (24.52, 50.60)% MVIC) were elicited for the forward step-up (Figure 9). Adding resistance to a side-step exercise also generated high mean activity levels (40.04 [26.53.29, 60.43] % MVIC) for middle GMed (Figure 9). There were wide methodological variations across the studies including exercise technique; step height; step distance; concentric and eccentric phase measures; stepping or supporting leg measures; and addition of external resistance. One study52 measured segmental surface GMed activity and found very high activity (88% MVIC anterior, 85% MVIC middle, and 81% MVIC posterior) for all three segments for the forward step up and over exercise.
Figure 9.
Gluteus medius middle - step exercises.
Lunge exercises
Gluteus medius
The lunge was evaluated in GMed across 10 studies46,50,64,65,70,71,78,81,92,95 (Table 5). For middle GMed, pooled results suggest moderate activity is recorded during the forward (21.43 [95% CI 14.83, 30.97] % MVIC) and side lunge (22.41 [7.64, 65.78] % MVIC) (Figure 10). One study46 measured segmental GMed activity with a rear-foot elevated lunge (dip test) and found high anterior (45% MVIC), very high middle (71% MVIC) and moderate posterior (28% MVIC) GMed segmental activity. There was some variation between the studies on lunge technique, active range of movement and movement plane.
Figure 10.
Gluteus medius middle - lunge exercises.
Gluteus minimus
One study46 found the dip test generated moderate activity (21% MVIC) for the anterior GMin segment and very high activity (66% MVIC) for the posterior GMin segment (Figures 3 and 4) (Table 6).
Hip hitch/pelvic drop
Gluteus medius
The hip hitch/pelvic drop exercise were evaluated in eight studies46,52,55,63,67,68,70,72,78,89,96 (Table 5). For studies that could be pooled together, the hip hitch/pelvic drop generated high GMed anterior activity (40.93 [95% CI 20.61, 81.28] % MVIC), GMed middle (42.64 [30.17, 60.00] % MVIC) and GMed posterior (43.37 [21.33, 88.16] % MVIC) activity (Figures 5, 6 and 11). Three different variations of the hip hitch/pelvic drop exercise were evaluated in one study46 and found very high activity (68-74% MVIC) for the anterior GMed, and high to very high activity for the middle (41-65% MVIC) and posterior (45-60% MVIC) GMed segments.
Figure 11.
Gluteus medius middle - hip hitch/pelvic drop exercises.
Gluteus minimus
Gluteus minimus activity was evaluated in one study46 for three different variations of the hip hitch/pelvic drop exercise and found to generate high to very high activity (48-69% MVIC) for the anterior segment and very high activity (66-84% MVIC) for the posterior segment (Figures 3 and 4) (Table 6).
Standing hip abduction
Gluteus medius
Standing hip abduction was measured on the stance leg in four studies46,59,72,82 (Table 5). For two studies that could be pooled together high activity levels (43.12 [95% CI 35.91, 51.79] % MVIC) were recorded for the middle GMed segment (Figure 7). Moderate to high activity (56% MVIC anterior, 30% MVIC middle and 41% MVIC posterior) was found in one study46 that evaluated GMed segmental activity levels for isometric standing hip abduction.
Gluteus minimus
Gluteus minimus segmental activity levels were also recorded for isometric standing hip abduction, and high activity (55% MVIC anterior and 49% MVIC posterior) were found for both segments46 (Figures 3 and 4) (Table 6).
Supine bridge
Gluteus medius
The single-leg bridge was investigated in seven single electrode GMed middle studies66,68,71,78,97-99 (Table 5). For six studies that could be pooled together, high activity levels (41.27 [95% CI 33.98, 50.13] % MVIC were produced (Figure 12). The double leg bridge was evaluated in five studies66,71,78,97,99 for middle GMed and when pooled together generated low activity levels (18.80 [13.83, 25.66] % MVIC) (Figure 12).
Figure 12.
Gluteus medius middle - bridge exercises.
Gluteus minimus
The single leg bridge was measured in one study47 and generated low activity (14% MVIC) in the anterior GMin segment and high activity (46% MVIC) for the posterior GMin segment (Figures 3 and 4) (Table 6).
DISCUSSION
The aim of this systematic review was to determine whether commonly evaluated rehabilitation exercises generate at least high activity levels in GMed and GMin segments. The results indicate that different variations of the hip hitch/pelvic drop exercise are the best options to generate at least high activity in all segments of GMed. To target the anterior GMed segment, additional options could include isometric standing hip abduction and the dip test. For the middle GMed segment at least high activity was generated by the single leg bridge; side-lying hip abduction with hip internal rotation; lateral step-up; resisted side-step; and standing hip abduction on stance or swing leg with added resistance. Another exercise option for the posterior GMed segment is isometric standing hip abduction.
For the GMin different variations of the hip hitch/pelvic drop exercise and isometric standing hip abduction were the best options to generate at least high activity in both segments. Additional exercises to target the posterior GMin segment included the dip test; single leg bridge; single leg squat; and side-lying hip abduction.
Single leg weight-bearing exercises appeared to generate at least moderate activity in all three segments of GMed. This is despite the wide methodological variations between studies for similar exercises and the relatively small number of studies that evaluated the separate GMed segments for different exercises. This highlights the functional role of GMed as a multi-planar hip and pelvic stabilizer in weight-bearing activities. Based on the large physiological cross-sectional area and favorable coronal plane moment arm,100 GMed is well suited to maintaining pelvic and hip joint equilibrium during single-limb loading tasks.
The clam exercise appeared least favorable in terms of recruiting GMed muscle activity. With a relatively short anti-gravity lever arm to overcome, the clam recorded low activity in the anterior and middle segments, and moderate activity in the posterior segment. This perhaps reflects the biomechanical properties of GMed muscle segments, with the anterior segment having an internal rotation moment arm in the transverse plane, the middle segment a negligible rotation moment arm, and the posterior segment an external rotation moment arm.100 The clam may potentially be useful in early rehabilitation for motor control and recruitment but unlikely to elicit sufficient activity for strengthening.101 This is particularly the case for the anterior and middle segments.
Recruitment of posterior GMin with a wide variety of exercises appears more feasible than anterior GMin. There are a broader range of exercises available for strengthening the posterior GMin with single leg weight-bearing exercises, and side-lying hip abduction potential options. In comparison, the anterior GMin functioning as an anterior hip capsule stabilizer, and prime hip abductor,102 appears to be more difficult to target for strengthening compared to the posterior segment. For example, the single leg squat exercise is broadly useful for recruiting all segments of GMed as well as posterior GMin but may have less utility for anterior GMin (moderate level of activity). This might reflect the tendency of studies to include exercises with an external rotation bias. Since anterior GMin is highly active with internal rotation,19 and has a favorable moment arm for internal rotation,100 further research examining internal rotation-based exercises for anterior GMin highlight further options for recruiting this muscle segment. The clam exercise may not have great utility for GMin muscle strengthening. Both studies in this review showed similar results for the two GMin segments during the clam exercise with low activity generated.46,47
In the clinic, individual assessment is important to ensure that the most appropriate exercise strategy is prescribed to meet the client's functional requirements. Post-surgery or in the acute phases of an injury, some clients may be unable to perform weight-bearing exercises early in the rehabilitation process. Prescribing a suitable non-weight-bearing exercise such as side-lying hip abduction may overcome this barrier while still delivering a strengthening stimulus for the muscle segment being targeted. Exercises that did not generate high levels of activity101 for a specific segment may still be beneficial in a progressive rehabilitation program as hypertrophy may not be the goal in the initial stages particularly if the client is deconditioned or in pain. Further to this, since most included studies contained healthy young participants performing rehabilitation exercises, the results from these studies may not be relevant to the elderly client or for the well-conditioned athlete. In both cases it is likely that the recommended exercises will need modifications to meet the individuals’ functional goals. For example, the elderly client may need decreased loading strategies and less demanding forms of an exercise. In contrast, for the well-conditioned athlete to stimulate hypertrophy, an exercise may need added loading through weights or elastic resistance to meet that goal.101
Strength and limitations
From a summary of the results the authors were able to determine whether commonly evaluated therapeutic exercises specifically target the individual GMed and GMin segments effectively in generating at least high activity levels (>40% MVIC) considered essential for potential strengthening.101 Through application of a stringent methodological process, an objective evaluation of current evidence to date was provided.
A limitation of this systematic review was that not all commonly evaluated therapeutic exercises included in this review have been evaluated for the different segments of GMed and GMin making it difficult to make recommendations for some exercises.
The recording of GMed muscle activity with surface electrodes has some drawbacks. Five included studies46,52,55,62,63 investigated therapeutic exercises for the three individual GMed segments, with one study46 using fine-wire electrodes positioned as per previously validated guidelines103 to measure segmental activity levels. The use of surface electrodes to record activity in the posterior and anterior segments of GMed must be questioned due to the anatomical coverage by the tensor fascia lata and gluteus maximus muscles.103 In fact, even recording GMed activity from the exposed portion of the muscle is subject to crosstalk from the gluteus maximus.20 During exercises involving large ranges of movement, there may also be artefact associated with movement of the muscle relative to the recording electrodes.104
Other limitations of this review may be due to excluding studies that did not contain commonly evaluated therapeutic exercises or utilizing gym and/or custom-made equipment; and eliminating data for dynamic activities like jogging, hopping and walking. The original search strategy may have missed studies due to publication bias and not contacting experts for unpublished papers. Papers not published in peer-reviewed journals such as conference abstracts and theses were also excluded possibly missing potential data. This review only evaluated EMG activation levels and not muscle onset timing patterns or the balance of synergists and antagonists for a therapeutic exercise as may be considered in the clinical setting. Data for pathological populations were not considered in this review which makes it difficult to generalize to such populations.
CONCLUSION
The purpose of this review was to analyze studies that have evaluated segmental activity levels for the GMed and GMin with commonly evaluated therapeutic exercises to improve clinician knowledge of appropriate exercise prescription for targeted strengthening. With at least high activity levels necessary for potential strength gains this review found that despite wide methodological variations between studies, different variations of the hip hitch/pelvic drop exercise elicits activity in all GMed segments sufficiently in healthy individuals. The dip test and isometric standing hip abduction can also be used to strengthen the anterior GMed segment, while isometric standing hip abduction can be used for the posterior GMed segment. For the middle GMed segment the single leg bridge; side-lying hip abduction with hip internal rotation; lateral step-up; standing hip abduction on stance or swing leg with added resistance; and resisted side-step were the best options for strengthening. Isometric standing hip abduction and different variations of the hip hitch/pelvic drop exercise can be prescribed for strengthening both GMin segments while side-lying hip abduction, the dip test, single leg bridge and single leg squat can also be used for targeting the posterior GMin segment.
REFERENCES
- 1.Azevedo LB Lambert MI Vaughan CL, et al. Biomechanical variables associated with achilles tendinopathy in runners. Br J Sports Med. 2009;43(4):288-292. [DOI] [PubMed] [Google Scholar]
- 2.Beckman SM Buchanan TS. Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Arch Phys Med Rehabil. 1995;76(12):1138-1143. [DOI] [PubMed] [Google Scholar]
- 3.Franettovich M Chapman AR Blanch P, et al. Altered neuromuscular control in individuals with exercise-related leg pain. Med Sci Sports Exerc. 2010;42(3):546-555. [DOI] [PubMed] [Google Scholar]
- 4.Hewett TE Myer GD Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492-501. [DOI] [PubMed] [Google Scholar]
- 5.Souza RB Powers CM. Differences in hip kinematics #muscle |strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12-19. [DOI] [PubMed] [Google Scholar]
- 6.Fredericson M Wolf C. Iliotibial band syndrome in runners: innovations in treatment. Sports Med. 2005;35(5):451-459. [DOI] [PubMed] [Google Scholar]
- 7.Casartelli NC Maffiuletti NA Item-Glatthorn JF, et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage. 2011;19(7):816-821. [DOI] [PubMed] [Google Scholar]
- 8.Morrissey D Graham J Screen H, et al. Coronal plane hip muscle activation in football code athletes with chronic adductor groin strain injury during standing hip flexion. Manual Ther. 2012;17(2):145-149. [DOI] [PubMed] [Google Scholar]
- 9.Amaro A Amado F Duarte JA, et al. Gluteus medius muscle atrophy is related to contralateral and ipsilateral hip joint osteoarthritis. Int J Sports Med. 2007;28(12):1035-1039. [DOI] [PubMed] [Google Scholar]
- 10.Bewyer KJ Bewyer DC Messenger D, et al. Pilot data: association between gluteus medius weakness and low back pain during pregnancy. Iowa Orthop J. 2009;29:97-99. [PMC free article] [PubMed] [Google Scholar]
- 11.Nelson-Wong E Gregory DE Winter DA, et al. Gluteus medius muscle activation patterns as a predictor of low back pain during standing. Clin Biomech (Bristol, Avon). 2008;23(5):545-553. [DOI] [PubMed] [Google Scholar]
- 12.Zacharias A Green RA Semciw AI, et al. Atrophy of hip abductor muscles is related to clinical severity in a hip osteoarthritis population. Clin Anat. 2018;31(4):507-513. [DOI] [PubMed] [Google Scholar]
- 13.Lawrenson PR Crossley KM Vicenzino BT, et al. Muscle size and composition in people with articular hip pathology: a systematic review with meta-analysis. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2019;27(2):181-195. [DOI] [PubMed] [Google Scholar]
- 14.Boling MC Bolgla LA Mattacola CG, et al. Outcomes of a weight-bearing rehabilitation program for patients diagnosed with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2006;87(11):1428-1435. [DOI] [PubMed] [Google Scholar]
- 15.Gilchrist J Mandelbaum BR Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476-1483. [DOI] [PubMed] [Google Scholar]
- 16.Sled EA Khoja L Deluzio KJ, et al. Effect of a home program of hip abductor exercises on knee joint loading #strength, |function, and pain in people with knee osteoarthritis: a clinical trial. Phys Ther. 2010;90(6):895-904. [DOI] [PubMed] [Google Scholar]
- 17.Hislop AC Collins NJ Tucker K et al. Does adding hip exercises to quadriceps exercises result in superior outcomes in pain, function and quality of life for people with knee osteoarthritisϿ. A systematic review and meta-analysis. Br J Sports Med. 2020;54(5):263-271. [DOI] [PubMed] [Google Scholar]
- 18.Fransen M McConnell S Hernandez-Molina G, et al. Exercise for osteoarthritis of the hip. The Cochrane Database of Systematic Reviews. 2014(4):CD007912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Semciw AI Green RA Murley GS, et al. Gluteus minimus: an intramuscular EMG investigation of anterior and posterior segments during gait. Gait Posture. 2014;39(2):822-826. [DOI] [PubMed] [Google Scholar]
- 20.Semciw AI Neate R Pizzari T. A comparison of surface and fine wire EMG recordings of gluteus medius during selected maximum isometric voluntary contractions of the hip. J Electromyogr Kinesiol. 2014;24(6):835-840. [DOI] [PubMed] [Google Scholar]
- 21.Semciw AI Pizzari T Murley GS, et al. Gluteus medius: an intramuscular EMG investigation of anterior, middle and posterior segments during gait. Journal of electromyography and kinesiology : official journal of the International Society of Electrophysiological Kinesiology. 2013;23(4):858-864. [DOI] [PubMed] [Google Scholar]
- 22.Zacharias A Pizzari T English DJ, et al. Hip abductor muscle volume in hip osteoarthritis and matched controls. Osteoarthritis Cartilage. 2016;24(10):1727-1735. [DOI] [PubMed] [Google Scholar]
- 23.Woodley SJ Nicholson HD Livingstone V, et al. Lateral hip pain: findings from magnetic resonance imaging and clinical examination. J Orthop Sports Phys Ther. 2008;38(6):313-328. [DOI] [PubMed] [Google Scholar]
- 24.Bremer AK Kalberer F Pfirrmann CW, et al. Soft-tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the transgluteal approaches. Journal of Bone and Joint Surgery 2011;93(7):886-889. [DOI] [PubMed] [Google Scholar]
- 25.Pfirrmann CW Notzli HP Dora C, et al. Abductor tendons and muscles assessed at MR imaging after total hip arthroplasty in asymptomatic and symptomatic patients. Radiology. 2005;235(3):969-976. [DOI] [PubMed] [Google Scholar]
- 26.Muller M Tohtz S Winkler T, et al. MRI findings of gluteus minimus muscle damage in primary total hip arthroplasty and the influence on clinical outcome. Arch Orthop Trauma Surg. 2010;130(7): 927-935. [DOI] [PubMed] [Google Scholar]
- 27.French HP Dunleavy M Cusack T. Activation levels of gluteus medius during therapeutic exercise as measured with electromyography: a structured review. Physical Therapy Reviews. 2013;15(2):92-105. [Google Scholar]
- 28.Ebert JR Edwards PK Fick DP, et al. A systematic review of rehabilitation exercises to progressively load the gluteus medius. J Sport Rehabil. 2017;26(5):418-436. [DOI] [PubMed] [Google Scholar]
- 29.Hamstra-Wright KL Huxel Bliven K. Effective exercises for targeting the gluteus medius. J Sport Rehabil. 2012;21(3):296-300. [DOI] [PubMed] [Google Scholar]
- 30.Macadam P Cronin J Contreras B. An examination of the gluteal muscle activity associated with dynamic hip abduction and hip external rotation exercise: a systematic review. Int J Sports Phys Ther. 2015;10(5):573-591. [PMC free article] [PubMed] [Google Scholar]
- 31.Reiman MP Bolgla LA Loudon JK. A literature review of studies evaluating gluteus maximus and gluteus medius activation during rehabilitation exercises. Physiotherapy Theory and Practice. 2011. [DOI] [PubMed] [Google Scholar]
- 32.Moher D Liberati A Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burden A. How should we normalize electromyograms obtained from healthy participants? What we have learned from over 25 years of research. J Electromyogr Kinesiol. 2010;20(6):1023-1035. [DOI] [PubMed] [Google Scholar]
- 34.De Luca CJ. The use of surface electromyography in biomechanics. J Appl Biomech. 1997;13:135-163. [Google Scholar]
- 35.Soderberg GL Cook TM. Electromyography in biomechanics. Phys Ther. 1984;64(12):1813-1820. [DOI] [PubMed] [Google Scholar]
- 36.Soderberg GL Knutson LM. A guide for use and interpretation of kinesiologic electromyographic data. Phys Ther. 2000;80(5):485-498. [PubMed] [Google Scholar]
- 37.Bolgla LA Uhl TL. Reliability of electromyographic normalization methods for evaluating the hip musculature. J Electromyogr Kinesiol. 2007;17(1):102-111. [DOI] [PubMed] [Google Scholar]
- 38.Semciw AI Neate R Pizzari T. Running related gluteus medius function in health and injury: A systematic review with meta-analysis. J Electromyogr Kinesiol. 2016;30:98-110. [DOI] [PubMed] [Google Scholar]
- 39.Ganderton CP, T. A systematic literature review of the resistance exercises that promote maximal muscle actvity of the rotator cuff in normal shoulders. Shoulder & Elbow. 2013;5:120-135. [Google Scholar]
- 40.York Uo. CRD Report 4 2nd Edition. Published 2001. Accessed May 3, 2012 from http://www.york.ac.uk/inst/crd/crdreport4app3.pdf.
- 41.Wan X Wang W Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kleissen RF. Effects of electromyographic processing methods on computer-averaged surface electromyographic profiles for the gluteus medius muscle. Phys Ther. 1990;70(11):716-722. [DOI] [PubMed] [Google Scholar]
- 43.Higgins JP Thompson SG Deeks JJ, et al. Measuring inconsistency in meta-analyses. Br Med J. 2003;327(7414):557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Escamilla RF Yamashiro K Paulos L, et al. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports Med. 2009;39(8):663-685. [DOI] [PubMed] [Google Scholar]
- 45.Poolman RW Struijs PA Krips R, et al. Reporting of outcomes in orthopaedic randomized trials: does blinding of outcome assessors matter? J Bone Joint Surg. 2007;89(3):550-558. [DOI] [PubMed] [Google Scholar]
- 46.Ganderton C Pizzari T Cook J, et al. Gluteus minimus and gluteus medius muscle activity during common rehabilitation exercises in healthy postmenopausal women. Journal of Orthopaedic and Sports Physical Therapy. 2017;47(12):914-922. [DOI] [PubMed] [Google Scholar]
- 47.Moore D Semciw AI McClelland J, et al. Rehabilitation exercises for the gluteus minimus muscle segments: an electromyography study. J Sport Rehabil. 2019;28(6):544-551. [DOI] [PubMed] [Google Scholar]
- 48.Hertel J Sloss BR Earl JE. Effect of foot orthotics on quadriceps and gluteus medius electromyographic activity during selected exercises. Archives of Physical Medicine and Rehabilitation. 2005;86(1):26-30. [DOI] [PubMed] [Google Scholar]
- 49.Dwyer MK Stafford K Mattacola CG, et al. Comparison of gluteus medius muscle activity during functional tasks in individuals with and without osteoarthritis of the hip joint. Clin Biomech. 2013;28(7):757-761. [DOI] [PubMed] [Google Scholar]
- 50.Webster K Gribble P. A comparison of electromyography of gluteus medius and maximus in subjects with and without chronic ankle instability during two functional exercises. Physical Therapy in Sport. 2013;14(1):17-22. [DOI] [PubMed] [Google Scholar]
- 51.Harput G Howard JS Mattacola C. Comparison of muscle activation levels between healthy individuals and persons who have undergone anterior cruciate ligament reconstruction during different phases of weight-bearing exercises. Journal of Orthopaedic and Sports Physical Therapy. 2016;46(11):984-992. [DOI] [PubMed] [Google Scholar]
- 52.O’Sullivan K Herbert E Sainsbury D, et al. No difference in gluteus medius activation in women with mild patellofemoral pain. J Sport Rehabil. 2012;21(2):110-118. [DOI] [PubMed] [Google Scholar]
- 53.Cambridge ED Sidorkewicz N Ikeda DM, et al. Progressive hip rehabilitation: the effects of resistance band placement on gluteal activation during two common exercises. Clin Biomech. 2012;27(7):719-724. [DOI] [PubMed] [Google Scholar]
- 54.Felício LR Dias LA Silva APMC et al. Muscular activity of patella and hip stabilizers of healthy subjects during squat exercises. / Ativação muscular dos estabilizadores da patela e do quadril durante exercícios de agachamento em indivíduos saudáveis. Braz J Phys Ther. 2011;15(3):206-211. [PubMed] [Google Scholar]
- 55.Ju SK Yoo WG. Electromyographic analysis of gluteus medius subdivisions during hip abductor strengthening exercises. Isokinetics and Exercise Science. 2016;24(2):91-98. [Google Scholar]
- 56.Kim EH Lim TH Park SH, et al. Effect of hip abduction exercise with manual pelvic fixation on recruitment of deep trunk muscles. Am J Phys Med Rehabil. 2015;94(3):201-210. [DOI] [PubMed] [Google Scholar]
- 57.Lubahn AJ Kernozek TW Tyson TL, et al. Hip muscle activation and knee frontal plane motion during weight bearing therapeutic exercises. Int J Sports Phys Ther. 2011;6(2):92-103. [PMC free article] [PubMed] [Google Scholar]
- 58.Sidorkewicz N Cambridge ED McGill SM. Examining the effects of altering hip orientation on gluteus medius and tensor fascae latae interplay during common non-weight-bearing hip rehabilitation exercises. Clin Biomech. 2014;29(9):971-976. [DOI] [PubMed] [Google Scholar]
- 59.Sinsurin K Pluemjai S Srisangboriboon S, et al. Gluteus medius muscle activities during standing hip abduction exercises in the transverse plane at different angles. J Med Assoc Thai. 2015;98 Suppl 5:S42-47. [PubMed] [Google Scholar]
- 60.Ju SK Yoo WG. Comparison of anterior gluteus medius fiber activation during general exercises and PNF exercises. Journal of Physical Therapy Science. 2017;29(3):476-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kang MH Jang JH Kim TH, et al. Effects of Sshoulder flexion loaded by an elastic tubing band on EMG activity of the gluteal muscles during squat exercises. Journal of Physical Therapy Science. 2014;26(11):1787-1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Heo H-J An D-H Yoo W-G, et al. EMG analysis of gluteus medius subdivisions during modified unilateral biofeedback exercises for the lower limbs. Journal of Physical Therapy Science. 2013;25(1):85-88. [Google Scholar]
- 63.O’Sullivan K Smith SM Sainsbury D. Electromygraphic analysis of the three subdivisions of gluteus medius during weight-bearing exercises. SMARTT: Sports Medicine, Arthroscopy #Rehabilitation, |Therapy & Technology. 2010;2:17-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Boudreau SN Dwyer MK Mattacola CG, et al. Hip-muscle activation during the lunge #single-leg |squat, and step-up-and-over exercises. J Sport Rehabil. 2009;18(1):91-103. [DOI] [PubMed] [Google Scholar]
- 65.Dwyer MK Boudreau SN Mattacola CG, et al. Comparison of lower extremity kinematics and hip muscle activation during rehabilitation tasks between sexes. Journal of Athletic Training. 2010;45(2):181-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Philippon MJ Decker MJ Giphart JE, et al. Rehabilitation exercise progression for the gluteus medius muscle with consideration for iliopsoas tendinitis: an in vivo electromyography study. Am J Sports Med. 2011;39(8):1777-1785. [DOI] [PubMed] [Google Scholar]
- 67.Krause DA Jacobs RS Pilger KE, et al. Electromyographic analysis of the gluteus medius in five weight-bearing exercises. Journal of Strength and Conditioning Research. 2009;23(9):2689-2694. [DOI] [PubMed] [Google Scholar]
- 68.Boren K Conrey C Le Coguic J, et al. Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Int J Sports Phys Ther. 2011;6(3):206-223. [PMC free article] [PubMed] [Google Scholar]
- 69.McBeth JM Earl-Boehm JE Cobb SC, et al. Hip muscle activity during 3 side-lying hip-strengthening exercises in distance runners. Journal of Athletic Training. 2012;47(1):15-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Distefano LJ Blackburn JT Marshall SW, et al. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther. 2009;39(7):532-540. [DOI] [PubMed] [Google Scholar]
- 71.Ekstrom RA Donatelli RA Carp KC. Electromyographic analysis of core trunk, hip, and thigh muscles during 9 rehabilitation exercises. J Orthop Sports Phys Ther. 2007;37(12):754-762. [DOI] [PubMed] [Google Scholar]
- 72.Bolgla LA Uhl TL. Electromyographic analysis of hip rehabilitation exercises in a group of healthy subjects. Journal of Orthopaedic and Sports Physical Therapy. 2005;35(8):487-494. [DOI] [PubMed] [Google Scholar]
- 73.Chan MK Chow KW Lai AY, et al. The effects of therapeutic hip exercise with abdominal core activation on recruitment of the hip muscles. BMC Musculoskelet Disord. 2017;18(1):313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cynn H Oh J Kwon O, et al. Effects of lumbar stabilization using a pressure biofeedback unit on muscle activity and lateral pelvic tilt during hip abduction in sidelying. Arch Phys Med Rehabil. 2006;87(11):1454-1458. [DOI] [PubMed] [Google Scholar]
- 75.Lee JH Cynn HS Choi SA, et al. Effects of different hip rotations on gluteus medius and tensor fasciae latae muscle activity during isometric side-lying hip abduction. J Sport Rehabil. 2013;22(4):301-307. [DOI] [PubMed] [Google Scholar]
- 76.Lee JH Cynn HS Kwon OY, et al. Different hip rotations influence hip abductor muscles activity during isometric side-lying hip abduction in subjects with gluteus medius weakness. Journal of Electromyography and Kinesiology. 2014;24(2):318-324. [DOI] [PubMed] [Google Scholar]
- 77.MacAskill MJ Durant TJ Wallace DA. Gluteal muscle activity during weightbearing and non-weightbearing exercise. Int J Sports Phys Ther. 2014;9(7):907-914. [PMC free article] [PubMed] [Google Scholar]
- 78.Selkowitz DM Beneck GJ Powers CM. Which exercises target the gluteal muscles while minimizing activation of the tensor fascia lataϿ. Electromyographic assessment using fine-wire electrodes. J Orthop Sports Phys Ther. 2013;43(2):54-64. [DOI] [PubMed] [Google Scholar]
- 79.Morimoto Y Oshikawa T Imai A, et al. Piriformis electromyography activity during prone and side-lying hip joint movement. Journal of Physical Therapy Science. 2018;30(1):154-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Willcox EL Burden AM. The influence of varying hip angle and pelvis position on muscle recruitment patterns of the hip abductor muscles during the clam exercise. Journal of Orthopaedic and Sports Physical Therapy. 2013;43(5):325-331. [DOI] [PubMed] [Google Scholar]
- 81.Lin CY Tsai LC Press J, et al. Lower-limb muscle-activation patterns during off-axis elliptical compared with conventional gluteal-muscle-strengthening exercises. J Sport Rehabil. 2016;25(2):164-172. [DOI] [PubMed] [Google Scholar]
- 82.Youdas JW Adams KE Bertucci JE, et al. Muscle activation levels of the gluteus maximus and medius during standing hip-joint strengthening exercises using elastic-tubing resistance. J Sport Rehabil. 2014;23(1):1-11. [DOI] [PubMed] [Google Scholar]
- 83.Ayotte NW Stetts DM Keenan G, et al. Electromyographical analysis of selected lower extremity muscles during 5 unilateral weight-bearing exercises. J Orthop Sports Phys Ther. 2007;37(2):48-55. [DOI] [PubMed] [Google Scholar]
- 84.Bolgla LA Cruz MF Roberts LH, et al. Relative electromyographic activity in trunk, hip, and knee muscles during unilateral weight bearing exercises: Implications for rehabilitation. Physiotherapy Theory and Practice. 2016;32(2):130-138. [DOI] [PubMed] [Google Scholar]
- 85.Hatfield GL Charlton JM Cochrane CK, et al. The biomechanical demands on the hip during progressive stepping tasks. Journal of Strength and Conditioning Research. 2017;31(12):3444-3453. [DOI] [PubMed] [Google Scholar]
- 86.Mauntel TC Begalle RL Cram TR, et al. The effects of lower extremity muscle activation and passive range of motion on single leg squat performance. Journal of Strength and Conditioning Research. 2013;27(7):1813-1823. [DOI] [PubMed] [Google Scholar]
- 87.Zeller BL McCrory JL Kibler WB, et al. Differences in kinematics and electromyographic activity between men and women during the single-legged squat. Am J Sports Med. 2003;31(3):449-456. [DOI] [PubMed] [Google Scholar]
- 88.Bolgla LA Cook N Hogarth K, et al. Trunk and hip electromyographic activity during single leg squat exercises do sex differences exist? Int J Sports Phys Ther. 2014;9(6):756-764. [PMC free article] [PubMed] [Google Scholar]
- 89.Petrofsky JS Morris A Bonacci J, et al. Muscle use during exercise: a comparison of conventional weight equipment to pilates with and without a resistive exercise device. Journal of Applied Research. 2005;5(1):160-173. [Google Scholar]
- 90.Barton C Kennedy A Twycross-Lewis R, et al. Gluteal muscle activation during the isometric phase of squatting exercises with and without a Swiss ball. Physical Therapy in Sport. 2014;15(1):39-46. [DOI] [PubMed] [Google Scholar]
- 91.Berry JW Lee TS Foley HD, et al. Resisted Side Stepping: The Effect of Posture on Hip Abductor Muscle Activation. Journal of Orthopaedic and Sports Physical Therapy. 2015;45(9):675-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bouillon LE Wilhelm J Eisel P, et al. Electromyographic assessment of muscle activity between genders during unilateral weight-bearing tasks using adjusted distances. Int J Sports Phys Ther. 2012;7(6):595-605. [PMC free article] [PubMed] [Google Scholar]
- 93.Youdas JW Foley BM Kruger BL, et al. Electromyographic analysis of trunk and hip muscles during resisted lateral band walking. Physiotherapy Theory and Practice. 2013;29(2):113-123. [DOI] [PubMed] [Google Scholar]
- 94.Noh K Kang M An S, et al. Effect of hip joint position on hip abductor muscle activity during lateral step-up exercises. Journal of Physical Therapy Science. 2012;24(11):1145-1148. [Google Scholar]
- 95.Krause DA Elliott JJ Fraboni DF, et al. Electromyography of the hip and thigh muscles during two variations of the lunge exercise: a cross-sectional study. Int J Sports Phys Ther. 2018;13(2):137-142. [PMC free article] [PubMed] [Google Scholar]
- 96.Monteiro RL Facchini JH de Freitas DG, et al. Hip rotations’ influence of electromyographic activity of gluteus medius muscle during pelvic-drop exercise. J Sport Rehabil. 2017;26(1):65-71. [DOI] [PubMed] [Google Scholar]
- 97.Oliver GD Stone AJ Plummer H. Electromyographic examination of selected muscle activation during isometric core exercises. Clinical Journal of Sports Medicine. 2010;20(6):452-457. [DOI] [PubMed] [Google Scholar]
- 98.Lehecka BJ Edwards M Haverkamp R, et al. Building a better gluteal bridge: electromyographic analysis of hip muscle activity during modified single-leg bridges. Int J Sports Phys Ther. 2017;12(4):543-549. [PMC free article] [PubMed] [Google Scholar]
- 99.Youdas JW Hartman JP Murphy BA, et al. Magnitudes of muscle activation of spine stabilizers, gluteals, and hamstrings during supine bridge to neutral position. Physiotherapy Theory and Practice. 2015;31(6):418-427. [DOI] [PubMed] [Google Scholar]
- 100.Dostal WF Soderberg GL Andrews JG. Actions of hip muscles. Phys Ther. 1986;66(3):351-361. [DOI] [PubMed] [Google Scholar]
- 101.Andersen LL Magnusson SP Nielsen M et al. Neuromuscular activation in conventional therapeutic exercises and heavy resistance exercises: implications for rehabilitation. Phys Ther. 2006;86(5):683-697. [PubMed] [Google Scholar]
- 102.Flack NA Nicholson HD Woodley SJ. The anatomy of the hip abductor muscles. Clin Anat. 2014;27(2):241-253. [DOI] [PubMed] [Google Scholar]
- 103.Semciw AI Green RA Pizzari T et al. Verification of a standardized method for inserting intramuscular EMG electrodes into uniquely oriented segments of gluteus minimus and gluteus medius. Clin Anat. 2013;26(2):244-252. [DOI] [PubMed] [Google Scholar]
- 104.Rainoldi A Melchiorri G Caruso I. A method for positioning electrodes during surface EMG recordings in lower limb muscles. Journal of neuroscience methods. 2004;134(1):37-43. [DOI] [PubMed] [Google Scholar]
- 105.SENIAM. Recommendations for sensor locations in hip and upper leg muscles. http://www.seniam.org/. Published 2011. Accessed.
- 106.Konrad P. The ABC of EMG: A Practical Introduction to Kinesiological Electromyography. Scottsdale AZ: Noraxon USA Inc.; 2005. [Google Scholar]
- 107.Cram JR Kasman GS Holtz J. Introduction to Surface Electromyography. Gaithersburg, Maryland: Aspen Publishers, Inc.; 1998. [Google Scholar]
- 108.Hermens HJ Freriks B Disselhorst-Klug C et al. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10(5):361-374. [DOI] [PubMed] [Google Scholar]
- 109.Criswell E CJR. Cram's Introduction to Surface Electromyography 2nd ed. Sudbury, MA: Jones & Bartlett; 2011. [Google Scholar]
- 110.Basmajian JV De Luca CJ. Muscle |Alive #Their Functions Revealed by Electromyography 5th ed. Baltimore, MD: Williams and Wilkins; 1985. [Google Scholar]
- 111.Barton CJ Kennedy A Twycross-Lewis R et al. Gluteal muscle activation during the isometric phase of squatting exercises with and without a Swiss ball. Physical Therapy in Sport. 2014;15(1): 39-46. [DOI] [PubMed] [Google Scholar]