Abstract
Background:
Standardized testing of hip muscle strength and fatigue in the sagittal plane is important for assessing, treating and preventing a number of trunk and lower extremity pathologies. Furthermore, individuals displaying asymmetries of muscle strength between limbs are more likely to sustain an injury.
Purpose:
To evaluate the test-retest reliability of isometric strength and isokinetic fatigue measurements of the hip flexor and hip extensor muscles, and to examine whether there is a significant limb dominance effect on strength, fatigue and flexor-extensor ratios.
Study design:
Cross-sectional study.
Methods:
To evaluate reliability, 30 healthy individuals (33.2 + /- 13.1 years) were included. On a separate occasion, 24 healthy individuals (29.0 + /- 10.3 years) participated to assess between-limb differences. Reliability was established using intraclass correlation coefficients (ICCs), standard error of measurements (SEM) and minimal detectable change (MDC). Isometric strength (best peak torque of three maximal contractions; Nm/kg), isokinetic fatigue (total work of 20 consecutive maximal concentric flexor-extensor contractions at 120 °/s; Joule/kg), and flexor-extensor ratios, were recorded using a Biodex dynamometer.
Results:
Reliability was good-to-excellent (ICCs>0.83) and measurement errors were acceptable (SEM<13.6% and MDC%<37.8%). No significant between-limb differences in strength, fatigue and flexor-extensor ratios were detected.
Conclusions:
Isometric strength and isokinetic fatigue of the hip flexor and hip extensor muscles can be reliably assessed in healthy individuals using the Biodex dynamometer. Limb dominance did not significantly affect strength, fatigue or flexor-extensor ratios.
Level of Evidence:
2b
Keywords: Fatigue, hip joint, limb dominance, muscle strength, reproducibility
INTRODUCTION
Reduced hip flexor (HF) and hip extensor (HE) muscle strength, as well as fatigue, have been identified as important components in a number of trunk and lower extremity pathologies. Weakness of the HE muscles has been found in patients with low back pain, patellofemoral pain and Achilles tendinopathy.1-7 Decreased HF strength has been shown in patients with symptomatic femoroacetabular impingement and anterior cruciate ligament reconstruction.8,9 Furthermore, strength deficits in both HF and HE were reported in patients with hip osteoarthritis (OA).10,11 Reduced HF and HE strength, as well as endurance, were found in patients who had undergone knee surgery.12 Thus, to evaluate the changes in strength and fatigability of the HF and HE muscles following resistance training, reliable measurement techniques are needed.
Isokinetic dynamometry is widely used in both clinical and research settings. The usefulness of an isokinetic dynamometer, however, depends upon the reproducibility of the measurements taken. In the literature, most studies using isokinetic dynamometry have focused on the knee flexors and extensors, and less attention has been directed to the hip joint.13,14 In a systematic review, isokinetic concentric and eccentric HF and HE strength measurements, using a wide range of angular velocities, showed moderate to excellent reliability.15 However, only a few studies have examined the test-retest reliability of isometric HF and HE strength measurements using an isokinetic dynamometer. Isometric testing has the advantage of producing less stress on the musculoskeletal system and can be used to monitor rehabilitation when pathologies are present. In a study to assess muscle strength in patients with hip OA and healthy controls, Arokoski et al. reported moderate to high ICC values of isometric HF and HE strength measurements and moderate to good measurement errors (CV% ranged between 7.5% and 14.1%).16 Steinhilber et al. reported similar measurement errors when testing isometric HF and HE strength in hip OA patients and healthy controls.17 Meyer et al. investigated the test-retest reliability of hip strength measurements in healthy individuals.18 They used an innovative test setup with a leg brace worn on the tested leg to optimize pelvis and trunk stability. Reliability measures of isometric HF and HE strength measurements were excellent, but systematic bias was found for isometric HF strength measurements. Divergent results between studies emphasize the need for standardized assessment protocols of isometric HF and HE strength measurements.
Muscle fatigue is a complex phenomenon resulting from a combination of impairments throughout the neuromuscular system. It can be defined as “exercise-induced decrease in the ability to produce force”.19 Neuromuscular fatigue can be evaluated using a variety of test protocols and assessment methods, for example stimulation of the nerve or muscle to whole-body exercises. Measurements of muscle fatigue using an isokinetic dynamometer refer to the capacity of a muscle to produce force over a series of consecutive isokinetic contractions.13,20 The variables most commonly used to examine isokinetic fatigue include total work as well as losses of peak torque and work.21-23 In the lower limb, isokinetic fatigue testing has focused on the knee flexors and extensors as well as the ankle plantarflexors and dorsiflexors.21,23-27 However, only one study has examined the reliability of HF or HE fatigue measurements using an isokinetic dynamometer.28 In that study, reliability of HF fatigue measurements, evaluated as total work of 20 continuous eccentric/concentric contractions at an angular velocity of 150 º/s, was found to be poor (ICC<0.10). The authors speculate that the poor reliability may be due to difficulty with maintaining a consistent effort at the chosen angular velocity.
The use of unilateral measures (compared between sides) enables clinicians and sport coaches to assess whether a side-to-side strength asymmetry exists. It has been suggested that a 15% or greater disparity between limbs is considered a substantial asymmetry in athletes and could increase the risk of injury.29 Also, lower extremity strength deficit of less than 10% on the affected side compared with the uninjured side is considered a reference value before returning to sport after an injury.30 Studies evaluating the effects of limb dominance on HF and HE strength, using an isokinetic dynamometer, have reported contradictory results. No significant side-to-side difference was shown in healthy adults and ice hockey players.31-34 However, a significant limb dominance effect on HF strength was detected in baseball pitchers, indicating a sport-related asymmetry.35 Furthermore, isometric HE strength was 15.8% higher on the right side than on the left side in a healthy control group of men aged 47-64 years.16
In addition, imbalance in the agonist/antagonist muscular strength ratio may increase the likelihood of injury.36 Values of hip flexor-extensor strength ratios reported in previous studies showed that HF produce 55% to 76% of the torque values generated by HE.20,34,37,38 Numerous factors are presumed to influence the ratio, for example age, sex, limb dominance, physical activity level and velocity of movement.36
The aims of this study were to evaluate the test-retest reliability of isometric strength and isokinetic fatigue measurements of the HF and HE muscles and to examine whether there is a significant limb dominance effect on strength, fatigue and flexor-extensor ratios.
METHODS
Participants
To examine the test-retest reliability, a total of 30 participants (15 men and 15 women) volunteered to participate in the study (test-retest group, TRG), Table 1. On a separate occasion, 24 participants (12 men and 12 women) were recruited to assess between-limb differences of HF and HE strength and fatigue (between-limb group, BLG), Table 1.
Table 1.
Characteristics of participants in the test-retest reliability group (TRG) n=30 and the between-limb difference group (BLG) n=24. Means ± standard deviation (range) and median (range).
| Test-retest reliability group (n=30) | Between-limb difference group (n=24) | p-value | |
|---|---|---|---|
| Age (years) | 33.2 ± 13.1 (15-53) | 29.0 ± 10.3 (18-54) | 0.213 |
| Height (cm) | 176.0 ± 8.3 (155-193) | 174.8 ± 9.1 (156-190) | 0.793 |
| Weight (kg) | 71.7 ± 12.4 (53-101) | 70.9 ± 11.2 (50-90) | 0.603 |
| Saltin-Grimby Physical Activity Level Scale (level 1-6) | 4.0 (2-6) | 4.5 (2-6) | 0.847 |
All participants in TRG and BLG were in good health and participated regularly in recreational sports. A baseline questionnaire, the modified six-graded Saltin-Grimby Physical Activity Level Scale, was completed to ascertain the physical activity habits of the participants.39 Activity levels of each groups are shown in Table 1. Exclusion criteria for participation were neuromuscular dysfunction in the back or lower extremities within the past year. Limb dominance was determined by asking the participants “If you would shoot a ball on a target, which leg would you use to shoot the ball?”.40 All participants preferred the right leg.
Written informed consent was obtained from each individual. Additionally, participants under the age of 18 had informed consent from their legal guardians before participation. The study was approved by the Advisory Committee for Research Ethics in Health Education, Lund University and the principles of the Declaration of Helsinki were followed.
Sample size calculations
To assess the test-retest reliability, a total of 30 participants were included.41,42 The sample size used to examine differences between the dominant and the non-dominant limb was based on the assumption that side differences were < 10 %. Based on α = 0.05 and β = 0.80, a minimum sample size of 23 participants was required. Considering a potential loss of participants, 24 participants were recruited.
Test equipment
All tests were performed using the Biodex® Multi-Joint System 4 isokinetic dynamometer (Biodex Medical Systems Inc. Shirley, New York, USA). Before testing each participant, the dynamometer was calibrated according to the manual. The standard Biodex equipment with the provided Velcro straps was used.
Setup positioning
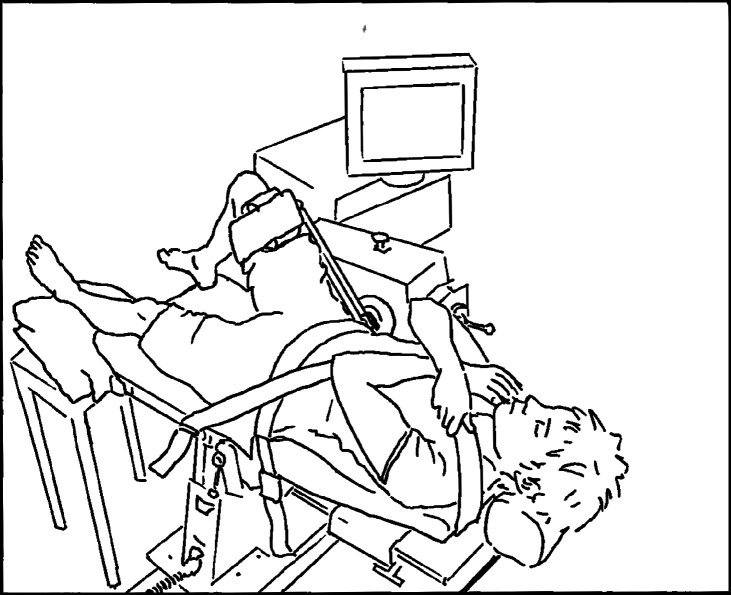
Participants were instructed to lie in supine position (Figure 1). The rotational axis of the dynamometer was aligned with the greater trochanter of the femur, and the dynamometer pad was fixed at the lower end of the thigh about 4 cm proximal to the lateral femoral condyle.
Figure 1.
Position of a participant during testing of hip flexors and hip extensors.
The non-tested limb was placed on a stool. The body was stabilized on the bench with a strap over the pelvis and two straps diagonally from the shoulder to the opposite hip. Participants were instructed to cross their arms over the chest. Prior to the tests, each participant's limb was weighed by the isokinetic dynamometer to allow correction for gravity.
For the isometric strength testing, the angles of the hip and knee joints were set at 60 ° hip flexion and 90 ° knee flexion. The end-range setting for the fatigue tests was standardized for all participants from 15 ° to 110 ° of hip flexion.
Test protocol
Throughout the study, all tests were administered by the same two raters to ensure a high level of standardization of the test procedures. Each participant in TRG underwent two identical test sessions scheduled approximately at the same time of the day, with seven days apart. Only the dominant limb was assessed. To assess differences between the dominant and non-dominant side, the limbs of the participants in BLG were tested in a random order.
Test procedures followed the same routine in TRG and BLG. Isometric strength tests were always performed prior to the isokinetic/fatigue tests. A five-minute warm-up period on a cycle ergometer (100 W for women and 150 W for men) was performed before testing. Thereafter, the participants performed two sub-maximal isometric HF contractions. After a two-minute rest, three maximal isometric HF contractions were executed. Participants were instructed to hold the contraction for five seconds, each contraction separated by a rest period of 12 seconds. Following a one-minute rest, the isometric HE strength was assessed in the same manner as HF. The participants were given visual feedback by observing the force curve displayed on the Biodex computer screen, but no verbal encouragement. After the isometric tests were conducted, participants rested for five minutes before proceeding to the isokinetic fatigue test of the same limb.
To familiarize participants with the isokinetic fatigue testing they were asked to perform three submaximal concentric flexion-extension contractions at 120 °/s. After a two-minute rest, they executed 20 consecutive maximal concentric flexor-extensor contractions at 120 °/s. Participants were instructed to pull and to push “as hard and as fast as possible”, and to complete the full range of motion.43 Strong verbal encouragement was given during the last five contractions. No visual feedback was given, and participants were not informed as to how many repetitions to perform prior to the test. For participants in BLG, a rest period of eight minutes was allowed before the opposite limb was tested.
Statistical analyses
Data are shown as mean ± standard deviation. Normality of the data was tested with the Shapiro-Wilk test, and the Levene's test was used to assess homogeneity of variance between groups. All dependent variables were normally distributed, and the use of parametric statistics was considered appropriate (paired and unpaired Student's t tests). A one-way within-subject multivariate analysis of variance, MANOVA, was used to examine the effect of limb dominance; an independent variable with two levels (dominant and non-dominant) was tested on four dependent variables (HF strength, HE strength, HF fatigue and HE fatigue). Mann-Whitney U test was used to examine differences in physical activity level of the participants in TRG and BLG.
The relative consistency between measurements was examined by the ICC2,1.44 A two-way analysis of variance (ANOVA) random effect model, absolute agreement, was used and the 95% confidence interval (95% CI) for ICC2,1 was obtained from the ANOVA tables. In general, reliability coefficients are suggested to exceed 0.80, but the values could be higher or lower depending on the precision needed for clinical evaluation.45 For the interpretation of reliability, various ICC cut-off points have been proposed such as: excellent (1.00-0.90), good (0.89 -0.75), moderate (0.74-0.50) and poor (<0.50).45
Absolute reliability describes the within-subject variability for repeated measures and quantifies the measurement error in the same unit as the original measurement. The standard error of measurements (SEM) represents the limit for the smallest change that indicates a real change for a group of individuals. SEM was defined as the square root of the within subjects mean square error term from the ANOVA.44,46 The SEM% was defined as: SEM% = (SEM/mean) x 100, where mean is the mean for all the observations from test sessions 1 and 2. This value represents the change in relative terms. The minimal detectable change (MDC) was also calculated, representing the minimum amount of change outside of the measurement error that reflects a real improvement, or a deterioration, for a single individual.44,46 The MDC for the 95% CI was calculated as: MDC = 1.96 x SEM x √ 2 . The value 1.96 is the z score associated with the 95% CI and √ 2 is used to account for the variance of two test sessions. The MDC was also expressed as a percentage value, MDC%, which is independent of the units of measurement (in analogy with SEM%). The MDC% was defined by: MDC% = (MDC/mean) x 100, where mean is the mean for all observations from test sessions 1 and 2. Systematic error between test sessions was assessed by evaluating the F ratios from the repeated-measures ANOVA.
The difference between isometric HF and HE strength in the dominant limb vs non-dominant limb was calculated as: (dominant limb - nondominant limb)/non-dominant limb, and expressed as a percentage. The same procedure was used for isokinetic HF and HE fatigue.
Peak torque (PT) was used to evaluate maximal isometric strength. The highest PT value of three maximal contractions was used for calculations. Isometric strength measures were normalized to bodyweight and reported as Newton-meters per kg (Nm/kg). Total work was used to evaluate fatigue for the entire set, and normalized fatigue measures were expressed as Joules per kg (J/kg).21,24
All statistical measures were performed using IBM SPSS Statistics version 25.0 (IBM Corporation, Armonk, New York, USA). Probability values < 0.05 were considered statistically significant.
RESULTS
Table 1 shows the characteristics of the participants in TRG (n=30) and BLG (n=24). There were no significant differences in age, height, weight or physical activity level between the two groups.
In Table 2, the test-retest reliability study results are reported. There was no systematic error between test session 1 and 2 (p > 0.05). The ICC values for all measurements were good to excellent, and ranged between 0.83 and 0.96. The 95% CIs for ICC were acceptable for all measurements, but wider for isokinetic HE fatigue measurements (0.67-0.92). SEM ranged from 0.08 to 0.37 Nm/kg for the isometric strength measurements, and 1.76 to 7.22 J/kg for the isokinetic fatigue measurements. SEM% were lower for HF strength and fatigue (4.5 % and 6.2 %) than HE strength and fatigue (11.0 % and 13.6%). The MDC% values ranged from 12.5 to 30.5% for HF and HE strength, and 17.1 to 37.8% for HF and HE fatigue.
Table 2.
Normalized isometric strength (Nm/kg) and normalized isokinetic fatigue (J/kg) of the hip flexors and hip extensors at two test sessions (n=30).
| Hip motion | Test 1 (Mean ± SD) | Test 2 (Mean ± SD) | p value | ICC (95% CI) | SEM | SEM % | MDC | MDC % |
|---|---|---|---|---|---|---|---|---|
| Hip flexor strength (Nm/kg) | 1.68 ± 0.40 | 1.67 ± 0.40 | 0.642 | 0.96 (0.92-0.98) | 0.08 | 4.5 | 0.21 | 12.5 |
| Hip extensor strength (Nm/kg) | 3.28 ± 1.18 | 3.35 ± 1.14 | 0.481 | 0.90 (0.81-0.95) | 0.37 | 11.0 | 1.01 | 30.5 |
| Hip flexor fatigue (J/kg) | 28.29 ± 7.16 | 28.67 ± 7.73 | 0.405 | 0.95 (0.89-0.97) | 1.76 | 6.2 | 4.88 | 17.1 |
| Hip extensor fatigue (J/kg) | 51.54 ± 17.51 | 54.74 ± 18.47 | 0.059 | 0.83 (0.67-0.92) | 7.22 | 13.6 | 20.0 | 37.8 |
Nm = Newton meter, J=Joule, kg = kilogram, ICC2.1 = intraclass correlation coefficient; CI = confidence interval; SEM = standard error of measurement; SEM%=relative standard error of measurement; MDC = minimum detectable change at a 95% CI; MDC % = relative minimum detectable change at a 95% CI.
In Table 3, isometric strength and isokinetic fatigue of HF and HE muscles in the dominant and non-dominant limbs are presented. No significant between-limb difference was found between limbs in HF strength (5.3%), as well as HF fatigue (5.4%). Also, there was no significant difference between limbs in HE strength (13.4%) and HE fatigue (12.3%). Flexor-extensor strength ratios were not significantly different between limbs; 56% ± 11% and 55% ± 14% for the dominant and non-dominant limb, respectively. No significant between-limb differences were found in flexor-extensor fatigue ratios; 56% ± 12% (dominant limb) and 54% ± 9% (non-dominant limb).
Table 3.
Normalized isometric strength (Nm/kg) and normalized isokinetic fatigue (J/kg) of the hip flexors and hip extensors in the dominant and non-dominant limb, and the corresponding bilateral differences, (n=24). Values are expressed as mean ± standard deviation (range).
| Dominant limb | Non-dominant limb | Bilateral difference Δ % | F ratio | P value | |
|---|---|---|---|---|---|
| Hip flexor strength, Nm/kg | 1.69 ± 0.34 (1.23 – 2.44) | 1.67 ± 0.32 (1.21 – 2.44) | 5.3 ± 4.8 (-12.6 – 16.7) | 0.038 | P = 0.847 |
| Hip extensor strength, Nm/kg | 3.09 ± 0.78 (1.65 – 4.65) | 3.22 ± 0.89 (1.47 – 4.97) | 13.4 ± 13.8 (-27.4 – 68.2) | 0.284 | P = 0.596 |
| Hip flexor fatigue, J/kg | 28.95 ± 5.61 (20.3 – 40.0) | 28.33 ± 5.72 (17.93 – 39.77) | 5.4 ± 5.9 (-8.9 – 25.4) | 0.145 | P = 0.705 |
| Hip extensor fatigue, J/kg | 54.51 ± 15.93 (27.69 – 82.2) | 53.85 ± 14.63 (23.41 – 81.07) | 12.3 ± 14.1 (-35.1 – 62.4) | 0.022 | P = 0.882 |
DISCUSSION
The results of the study show that isometric strength and isokinetic fatigue measurements of the HF and HE muscles could be reliably assessed in healthy individuals. No differences between limbs for isometric strength, isokinetic fatigue or flexor-extensor ratios were found. This supports the use of isokinetic dynamometers when assessing the hip which makes it possible to detect changes that indicate real improvements.
Isokinetic dynamometry is a useful tool to assess muscle performance. However, the overall results can be influenced by the accuracy of the dynamometer, the test procedures, the reproducibility of the measurement parameters, and subject-related factors.13 In the current study, the ICC value of isometric HF strength measurement was 0.96, indicating an excellent reliability according to Portney.45 Moderate to high ICC values (>0.71) have also been reported in other reliability studies of isometric HF strength measurements, using an isokinetic dynamometer and the supine subject positioning.16,18 In addition, the 95% CI for ICC in the present study was acceptable, and no systematic bias between test sessions was found. However, Meyer et al. reported that measurements of isometric HF strength tended to be larger at the second test occasion than those from the first.18 When systematic bias between test sessions occur, it may be due to a significant learning effect. Therefore, great care should be taken to let participants familiarize themselves before the real trials.46 Although the ICC value in this study indicated excellent reliability, it is well known that several statistical methods and indices are required to fully evaluate reliability. High ICC values do not necessarily imply that a test is suitable for clinical use. Moreover, the ICC is highly influenced by the heterogeneity (or spread) of the sample and can display high values that may be biased.44,46 Measurement errors in absolute and relative terms are often more useful for clinicians. In the current study, the measurement error for isometric HF strength was low (SEM%=4.5%). This value is smaller than SEM% values reported for healthy individuals by Arokoski et al. (CV%=14.1%), Steinhilber et al. (SEM% ∼ 7% from recalculated SEM values) and Meyer et al. (SEM%=6.0%).16-18 The contradictive findings may be due to differences of the hip joint angle used during testing. In this study, 60 ° hip flexion was chosen as an appropriate hip angle, whereas lower hip angles were selected in other studies: 0 ° hip flexion, 20 ° hip flexion and 45 ° hip flexion.16-18 Differences in test procedures, as well as using different isokinetic devices, may also have contributed to the varying results of the measurement errors. The present study, and the study by Meyer et al. used the Biodex equipment, while Lido® and Isomed 2000 was used in the two other studies.16-18 Thus, the finding in this study indicates that isometric HF strength measurement, using the Biodex dynamometer and a standardized test protocol, is considered highly reliable and can be used to detect real changes in isometric HF strength on a group level.
The ICC value of isometric HE strength measurement in the present study demonstrated excellent reliability (ICC=0.90), which corresponds to values found in other studies.16,18 In addition, the 95% CI for ICC was narrow and no systematic change in the mean between test sessions was found. These results indicate that isometric HE strength can be reliably measured and used to identify improvements following an intervention for a group of individuals. However, higher SEM% values for isometric HE measurements than for HF (11.0% and 4.5%, respectively) were detected. This phenomenon is well known, and has been reported in several studies using the supine position during testing, especially when testing HE in the isokinetic mode.15-18,32 During measurements of HE strength, the direction of the limb downwards can result in a lift of the pelvis and potentially change the axis of rotation which can cause errors. Thus, to achieve reliable results of HE strength testing it is important to firmly stabilize the entire dorsum against the bench of the dynamometer.
To detect a real change in isometric HF and HE strength for an individual, the MDC% values were calculated. The results showed that the size of the relative change (MDC%) should exceed 12.5 % and 30.5 % for HF and HE, respectively, to indicate a real change. In the study by Meyer et al., MDC% values were slightly higher, as well as and lower, for HF and HE:16.8% and 23.0%, respectively.18 Muscle strength improves as a result of resistance training and strength gains of approximately 20% to 40% after a short period of resistance training is not unusual for untrained, and moderately trained, individuals.47 Thus, this study shows that MDC% values are sufficiently small to detect true changes in isometric HF and HE strength for a single individual.
The ICC values of the isokinetic HF and HE fatigue testing in this study were good to excellent (ICC>0.83), and measurement errors were acceptable (SEM% < 13.6 and MDC% < 37.8). No systematic bias between test and retest was detected. This lack of systematic change indicates no learning effect and suggests that a single-session test can be used to identify clinically relevant changes in muscle fatigue. Thus, the findings in the present study imply that HF and HE fatigability can be reliably assessed, both for groups and a single individual. However, 95% CIs for isokinetic HE fatigue measurements were wider than for HF and measurement errors were larger. Moreover, reliability measures of isokinetic fatigue measurements were lower compared with isometric strength measurements. A possible explanation is that isokinetic measurements of HF, and especially HE, are more difficult to perform than isometric contractions, since stabilizing the pelvis and trunk is more difficult under dynamic conditions. Therefore, the test position in this study was standardized and the pelvis and upper trunk were firmly secured using the Velcro straps provided by Biodex. Additional equipment or leg braces were avoided because the intention was to create a simple test protocol. Also, recommendations by Zapparoli and Riberto were used to increase reliability of the isokinetic measurements, (i.e. supine position, the dynamometer axis aligned with the greater trochanter, and the lever arm in the most distal region of the thigh).15 In a previous study, Emery et al. reported that fatigue measurements of HF torque measurements were not reliable (ICC<0.10).28 Their poor reliability may have been due to the complexity of the selected eccentric/concentric continuous HF repetitions, which were unfamiliar to the participants and difficult to perform. They used a narrow range-of-motion (ROM) during testing from 0 ° to 70 of hip flexion. Furthermore, many participants were not able to maintain a consistent effort at the selected angular velocity (150 ° /s). In this study, a lower angular velocity (120 ° /s) and a wider range (15 ° to 110 ° of hip flexion) were used. This ROM may be a better representative of frequently used movements in daily living and during sport activities. Testing through a ROM which excludes the end points can also be more applicable in the clinic, for example to persons with hip OA.
In the present study, differences in isometric HF and HE strength between the dominant (right) and non-dominant (left) sides were small: 5.3% and 13.4% respectively. According to the SEM% values presented in this study, the between-limb differences should exceed 4.5% and 11%, respectively, to represent a real difference in isometric strength between limbs. Although the differences between sides exceeded the measurement errors, no significant difference between the dominant and non-dominant side was found. Also, the side-to side strength difference was less than 15%. Limb strength imbalance of 15% or more has been associated with higher injury rates. 29 However, studies evaluating side differences in isokinetic HF and HE fatigue measurements are limited. Emery et al. used total work as the outcome criterion, and reported a side difference of 8.0 % between limbs (3292 Nm on the right side and 3049 Nm on the left side) for HF fatigue.28 There was no report whether the difference between limbs was significant. In the present study, the difference between the dominant and non-dominant limb for isokinetic HF and HE fatigue was 5.4% and 12.3%, respectively, and not significant. Thus, as the reliability of isokinetic fatigue measurements of HF and HE was high, and the between-limb differences small and non-significant, it is shown that the contralateral limb can be used as a reference in the fatigue assessment.
In the current study, hip flexor-extensor isometric strength ratio was 56% in the dominant limb and 55% in the non-dominant limb. These results are slightly lower than those reported by Calmels et al. who found that the flexor-extensor torque ratios in healthy individuals ranged between 58% to 61% in the eccentric mode, and 68% to 75% in the concentric mode.38 Alexander examined top-level sprinters and reported hip flexor-extensor strength ratios of 66% to 75% in the eccentric mode and 61% to 76% in the concentric mode.37 In professional and amateur ice hockey players, hip flexor-extensor ratios ranged between 55% to 71% in the concentric mode.34 The varying results may be due to differences in types of contractions and differences in the sporting levels of the populations. Similar to previous studies, this study found no significant difference in flexor-extensor strength ratio between limbs.34,37,38 Also no significant difference in flexor-extensor fatigue ratio between limbs (56% in the dominant limb and 54% in the non-dominant limb) was found. In conclusion, the hip flexor-extensor strength and fatigue ratios are considered useful reference points to detect hip muscle imbalances in the contralateral side.
The present study included an adequate sample size to determine reliability and detect side-to-side strength and fatigue differences. However, only healthy individuals were included which limits the generalizability to individuals with trunk or lower extremity pathologies.
CONCLUSION
Isometric strength and isokinetic fatigue of the HF and HE muscles can be reliably assessed in healthy individuals using the Biodex dynamometer. Test-retest agreements were good to excellent and measurement errors were acceptable. The SEM% and MDC% values were sufficiently sensitive to detect a real change in muscle strength and fatigue over time, or after an intervention, both for a group of individuals or a single individual. No between-limb differences in isometric strength, isokinetic fatigue or flexor-extensor ratios were found which support the use of the non-injured limb as a reference.
REFERENCES
- 1.de Sousa CS de Jesus FLA Machado MB, et al. Lower limb muscle strength in patients with low back pain: a systematic review and meta-analysis. J Musculoskelet Neuronal Interact. 2019;19:69-78. [PMC free article] [PubMed] [Google Scholar]
- 2.Nadler SF Malanga GA DePrince M, et al. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000;10:89-97. [DOI] [PubMed] [Google Scholar]
- 3.Nourbakhsh MR Arab AM. Relationship between mechanical factors and incidence of low back pain. J Orthop Sports Phys Ther. 2002;32:447-460. [DOI] [PubMed] [Google Scholar]
- 4.Souza RB Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39:12-19. [DOI] [PubMed] [Google Scholar]
- 5.Van Cant J Pineux C Pitance L Feipel V. Hip muscle strength and endurance in females with patellofemoral pain: a systematic review with meta-analysis. Int J Sports Phys Ther. 2014;9:564-582. [PMC free article] [PubMed] [Google Scholar]
- 6.Prince MR van der Wurff P. Females with patellofemoral pain syndrome have weak hip muscles: a systematic review. Aust J Physiother. 2009;55:9-15. [DOI] [PubMed] [Google Scholar]
- 7.Habets B Smits HW Backx FJG, et al. Hip muscle strength is decreased in middle-aged recreational male athletes with midportion Achilles tendinopathy: A cross-sectional study. Phys Ther Sport. 2017;25:55-61. [DOI] [PubMed] [Google Scholar]
- 8.Casartelli NC Maffiuletti NA Item-Glatthorn JF, et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthr Cartil. 2011;19:816-821. [DOI] [PubMed] [Google Scholar]
- 9.Mouzopoulos G Siebold R Tzurbakis M. Hip flexion strength remains decreased in anterior cruciate ligament reconstructed patients at one-year follow up compared to healthy controls. Int Orthop. 2015;39:1427-1432. [DOI] [PubMed] [Google Scholar]
- 10.Loureiro A Constantinou M Diamond LE, et al. Individuals with mild-to-moderate hip osteoarthritis have lower limb muscle strength and volume deficits. BMC Musculoskelet Disord. 2018;19:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friesenbichler B Casartelli NC Wellauer V, et al. Explosive and maximal strength before and 6 months after total hip arthroplasty. J Orthop Res. 2018;36:425-431. [DOI] [PubMed] [Google Scholar]
- 12.Jaramillo J Worrell TW Ingersoll CD. Hip isometric strength following knee surgery. J Orthop Sport Phys Ther. 1994;20:160-165. [DOI] [PubMed] [Google Scholar]
- 13.Dvir Z. Isokinetics Muscle Testing, Interpretation and Clinical Applications. 2nd ed. London, England: Churchill Livingstone; 2004. [Google Scholar]
- 14.Caruso JF Brown LE Tufano JJ. The reproducibility of isokinetic dynamometry data. Isokinet Exerc Sci. 2012;20:239-253. [Google Scholar]
- 15.Zapparoli FY Riberto M. Isokinetic evaluation of the hip flexor and extensor muscles. A Systematic Review. J Sport Rehabil. 2017;26:556-566. [DOI] [PubMed] [Google Scholar]
- 16.Arokoski MH Arokoski JP Haara M, et al. Hip muscle strength and muscle cross sectional area in men with and without hip osteoarthritis. J Rheumatol. 2002;29: 2185-2195. [PubMed] [Google Scholar]
- 17.Steinhilber B Haupt G Boeer J, et al. Reproducibility of concentric isokinetic and isometric strength measurements at the hip in patients with hip osteoarthritis: A preliminary study. Isokinet Exerc Sci. 2011;19:39-46. [Google Scholar]
- 18.Meyer C Corten K Wesseling M, et al. Test-retest reliability of innovated strength tests for hip muscles. PLoS ONE. 2013;8(11):e81149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wan JJ Qin Z Wang PY, et al. Muscle fatigue: general understanding and treatment. Exp Mol Med. 2017;49(10):e384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perrin DH. Isokinetic exercise and assessment. Champaign: Human kinetics; 1993. [Google Scholar]
- 21.Kannus P Cook L Alosa D. Absolute and relative endurance parameters in isokinetic tests of muscular performance. J Sport Rehabil. 1992;1:2-12. [Google Scholar]
- 22.Pincivero DM Lephart SM Karunakara RA. Reliability and precision of isokinetic strength and muscular endurance for the quadriceps and hamstrings. Int J Sports Med. 1997;18:113-117. [DOI] [PubMed] [Google Scholar]
- 23.Bosquet L Maquet D Forthomme B, et al. Effect of the lengthening of the protocol on the reliability of muscle fatigue indicators. Int J Sports Med. 2010;31:82-88. [DOI] [PubMed] [Google Scholar]
- 24.Saenz A Avellanet M Hijos E, et al. Knee isokinetic test-retest: a multicenter knee isokinetic test-retest study of a fatigue protocol. Eur J Phys Rehabil Med. 2010; 46:81-88. [PubMed] [Google Scholar]
- 25.Frykholm E Géphine S Saey D, et al. Inter-day test–retest reliability and feasibility of isokinetic, isometric, and isotonic measurements to assess quadriceps endurance in people with chronic obstructive pulmonary disease: A multicenter study. Chron Respir Dis Volume. 2018;16:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mattes K Eldin AHW Schaffert N Manzer S. Local concentric muscle fatigue of the ankle dorsiflexors and plantar flexors: A reproducibility study. Isokinet Exerc Sci. 2015;23:87-92. [Google Scholar]
- 27.Porter MM Holmbäck AM Lexell J. Reliability of concentric ankle dorsiflexion fatigue testing. Can J Appl Physiol. 2002;27:116-127. [DOI] [PubMed] [Google Scholar]
- 28.Emery CA Maitland ME Meeuwisse WH. Test-retest reliability of isokinetic hip adductor and flexor muscle strength. Clin J Sport Med. 1999;9:79-85. [DOI] [PubMed] [Google Scholar]
- 29.Knapik JJ Bauman CL Jones BH, et al. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19:76-81. [DOI] [PubMed] [Google Scholar]
- 30.Orchard J Best TM Verrall GM. Return to play following muscle strains. Clin J Sport Med. 2005;15:436-441. [DOI] [PubMed] [Google Scholar]
- 31.Abdelmohsen AM. Leg Dominance Effect on Isokinetic Muscle Strength of Hip Joint. J Chiropr Med. 2019;18:27-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Julia M Dupeyron A Laffont I, et al. Reproducibility of isokinetic peak torque assessments of the hip flexor and extensor muscles. Ann Phys Rehabil Med. 2010; 53:293-305. [DOI] [PubMed] [Google Scholar]
- 33.Dugailly B Brassinne E Pirotte E, et al. Isokinetic assessment of hip muscle concentric strength in normal subjects: A reproducibility study. Isokinet Exerc Sci. 2005;13:129-137. [Google Scholar]
- 34.Smith DJ Wenger HA Steadward RD Sexsmith JR. Isokinetic torque outputs of professional and elite amateur ice hockey players. J Orthop Sports Phys Ther. 1981; 3:42-47. [DOI] [PubMed] [Google Scholar]
- 35.Tippett SR. Lower Extremity Strength and Active Range of Motion in College Baseball Pitchers: A Comparison between Stance Leg and Kick Leg. J Orthop Sports Phys Ther. 1986;8:10-14. [DOI] [PubMed] [Google Scholar]
- 36.Calmels PM Minaire P. A review of the role of the agonist/antagonist muscle pairs ratio in rehabilitation. Disabil Rehabil. 1995;17:265-276. [DOI] [PubMed] [Google Scholar]
- 37.Alexander MJ. Peak torque values for antagonist muscle groups and concentric and eccentric contraction types for elite sprinters. Arch Phys Med Rehabil. 1990;71:334-339. [PubMed] [Google Scholar]
- 38.Calmels PM Nellen M van der Borne I, et al. Concentric and eccentric isokinetic assessment of flexor-extensor torque ratios at the hip, knee, and ankle in a sample population of healthy subjects. Arch Phys Med Rehabil. 1997;78:1224-1230. [DOI] [PubMed] [Google Scholar]
- 39.Grimby G. Physical activity and muscle training in the elderly. Acta Med Scand Suppl. 1986;711:233-237. [DOI] [PubMed] [Google Scholar]
- 40.van Melick N Meddeler BM Hoogeboom TJ, et al. How to determine leg dominance: The agreement between self-reported and observed performance in healthy adults. PLoS ONE. 2017;12(12):e0189876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fleiss J. The design and analysis of clinical experiments. New York: John Wiley & Sons; 1986. [Google Scholar]
- 42.Baumgartner T. A. Norm-referenced measurement: Reliability. In: M. J. Safrit T. M. Wood (Eds.) Measurement concepts in physical education and exercise science. Champaign (IL): Human Kinetics; 1989:63. [Google Scholar]
- 43.Rendos NK Harriell K Qazi S, et al. Variations in verbal encouragement modify isokinetic performance. J Strength Cond Res. 2019;33:708-716. [DOI] [PubMed] [Google Scholar]
- 44.Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19:231-240. [DOI] [PubMed] [Google Scholar]
- 45.Portney LG. Foundations of Clinical Research: Applications to Evidence-Based Practice. 4th edition. F.A. Davis Company: Philadelphia; 2020. [Google Scholar]
- 46.Lexell JE Downham DY. How to assess the reliability of measurements in rehabilitation. Am J Phys Med Rehabil. 2005;84:719-723. [DOI] [PubMed] [Google Scholar]
- 47.Kraemer WJ Ratamess NA French DN. Resistance training for health and performance. Curr Sports Med Rep. 2002;1:165-171. [DOI] [PubMed] [Google Scholar]