Abstract
Background:
A recently published Dutch practice guideline emphasizes criterion-based rehabilitation after anterior cruciate ligament reconstruction (ACLR) instead of time-based. As a consequence of this criterion-based rehabilitation, return to play is only suggested when athletes meet specific return to play (RTP) criteria.
Purpose:
The goal of this prospective observational study was to analyze if physical therapists adhere to ACLR practice guideline RTP criteria for testing and return to sport decisions, and to explore whether there is a difference in adherence between physical therapists specialized in sports versus those who are not.
Methods:
When the treating physical therapist cleared an athlete for RTP after ACLR, the primary researcher performed RTP measurements according to the ACLR practice guideline to investigate if all nine quantitative and qualitative RTP criteria were met.
Results:
Of the 158 athletes (54 females and 104 males, mean age 24 ± 6 years, 12 ± 3 months after surgery), 69 (44%) had performed the RTP measurements with their primary physical therapist. Of the athletes tested by their primary physical therapist 23% met all RTP criteria compared to 10% of the athletes who were not tested at all by their primary physical therapist (p = 0.026). Of the athletes rehabilitating with a sports physical therapist, 52% had been tested by their primary physical therapist compared to 34% of the athletes rehabilitating with a non-sports physical therapist (p = 0.024).
Conclusion:
Only 44% of the athletes were tested according to the guideline RTP criteria and only 23% of them were given an RTP advice consistent with the ACLR guideline. Although sports physical therapists adhered to the guideline more often than non-sports physical therapists, the adherence is still alarmingly low. More attention for the implementation of ACLR guidelines and RTP criteria is needed.
Level of evidence:
Therapy, level 2b.
Keywords: anterior cruciate ligament reconstruction, guideline, return to play, sports physical therapist
INTRODUCTION
For most pivoting athletes return to pre-injury sport level after anterior cruciate ligament reconstruction (ACLR) is the desired rehabilitation endpoint.1 A recently published Dutch practice guideline emphasized criterion-based rehabilitation after ACLR instead of time-based. As a consequence of this criterion-based rehabilitation, return to play is only allowed when meeting specific criteria.2,3
Even though several experts recommend to use criterion based RTP decisions, many athletes after ACLR are cleared for return to pivoting sports without meeting these criteria. In Sweden, only 20% of adults and 28% of adolescents who already returned to play met quantitative RTP criteria 12 months after ACLR, while in the USA only 14% of adolescent athletes met quantitative RTP criteria when cleared for RTP.4,5 Those quantitative RTP criteria are the same as described in the Dutch ACLR practice guideline. Besides using RTP measurements for movement quantity (strength tests and single-leg hop tests), the Dutch ACLR practice guideline also highlights using movement quality measurements (single-leg hop-and-hold and double-leg countermovement jump) as RTP criteria to decrease second ACL injury risk.6-9
The ACLR practice guideline was commissioned by the Royal Dutch Society for Physical Therapy (KNGF) and should therefore be used by every Dutch physical therapist, regardless of their experience with pivoting athletes recovering from ACLR.3 However, it remains to be seen whether the guideline have been properly implemented in day-to-day practice so that every Dutch physical therapist is able to work according to the guideline.
Therefore, the first aim of this study was to analyze if physical therapists adhere to ACLR practice guideline RTP criteria for testing and return to sport decisions. The hypothesis is that almost all Dutch physical therapists are able to use RTP measurements and know when to clear an athlete for RTP, since the practice guideline was implemented by the KNGF in 2014, making it publicly available to all Dutch physical therapists. The second aim was to explore whether there is a difference in adherence between physical therapists specialized in sports versus those who are not. The hypothesis is that sports physical therapists more often use RTP measurements, because, in the Netherlands, they have had additional education about pivoting athletes and RTP.
METHODS
Design and Participants
In this prospective observational cohort study, pivoting athletes with an ACL rupture (pre-injury Tegner Activity Scale (TAS) ≥ 6)10, aged 16-50 years, and scheduled for an ACLR between October 2014 and December 2016 were asked to participate. Athletes were excluded if they had undergone revision ACLR surgery, had a contralateral ACL injury or contralateral ACLR in the past. All included participants signed an informed consent form. ACLR surgery was performed by five experienced high-volume orthopaedic surgeons at Clinic ViaSana (Mill, the Netherlands) using an ipsilateral semitendinosus quadruple autograft and TLS® femoral and tibial fixation with all-inside technique (FH Orthopedics, Heimsbrunn, France).
Athletes were allowed to choose their own physical therapist. They notified their choice of physical therapist to the primary researcher (NM), who consecutively contacted the physical therapist by phone or email to provide the nine RTP criteria that needed to be performed at the end of rehabilitation before the athlete was cleared for return to play (Table 1, Appendix A). The physical therapist was informed that in the Netherlands an online version of the guideline, including the nine RTP criteria, is freely accessible. In addition, the athlete provided a paper copy of the guideline to their own (primary) physical therapist.
Table 1.
Return to play criteria according to the anterior cruciate ligament reconstruction practice guideline.2,3
| Tests on quantity of movement | Return to Play permitted when |
|---|---|
| Isometric knee extensor strength | LSI > 90% |
| Isometric knee flexor strength | LSI > 90% |
| Eccentric knee flexor strength | LSI > 90% |
| Isometric hip abduction strength | LSI > 90% |
| Vertical jump | LSI > 90% |
| Mop for distance | LSI > 90% |
| Side hop | LSI > 90% |
| Tests on quality of movement | Return to Play permitted when |
| Single-leg hop-and-hold | Score 'yes' |
| Counter Movement Jump (LESS score) | Score ≤ 5 |
LSI = Limb Symmetry Index, LESS = Landing Error Scoring System
Physical therapists were not additionally educated on how to perform RTP tests. Athletes who did not return to pivoting sports at the end of rehabilitation were also required to meet all RTP criteria, because their knee needed to be able to react to high-demand activities of daily life, including landing from jumps or unexpected movements.
At the end of the rehabilitation period, as judged by the primary physical therapist, the primary researcher was notified that the athlete had been judged ready for return to play, but actual results of RTP measurements were not corresponded to the primary researcher. Then, within one to four weeks, the primary researcher independently performed the RTP measurements as described in the ACLR practice guideline (Table 1) and thus re-evaluated the physical therapist's judgement on whether or not the athlete was able to return to play.2,3 Additionally, the athlete was asked if he/she was familiar with the RTP measurements, to check whether the primary physical therapist had performed RTP measurements at the end of the treatment when he or she decided that return to play was safe. When a patient was not familiar with RTP measurements, this was considered as the primary physical therapist not adhering to the guideline. This study was part of a larger prospective study approved by the Medical Ethics Committee of the Radboudumc Nijmegen, the Netherlands (registration number 2013/368).
PARTICIPATING PHYSICAL THERAPISTS
Physical therapists who participated in this study were asked to report their level of expertise. The specialization level of expertise of the physical therapist as recorded in the Dutch national registry was noted. Distinction was made between registration as a sports physical therapist or not (in this study referred to as non-sports physical therapist). In the Netherlands, instruction regarding return to play or criterion-based rehabilitation are not a common part of bachelor level physical therapy education. To become a registered sports physical therapist in the Netherlands one must follow additional three- to four-year education at the Master level regarding aspects of sport specific training and return to play.
Table 2 lists the similarities and differences between sports physical therapists and non-sports physical therapists.11,12 In this study it was therefore expected that sports physical therapists would perform RTP measurements more often than non-sports physical therapist.
Table 2.
Similarities and differences (in italics) between a physical therapist with and without specialization in sports in the Netherlands.11,12
| Physical therapist | Sports physical therapist | |
|---|---|---|
| Degree | Bachelor's degree | Master's degree |
| Knowledge | Knowledge on movement problems in general | Advanced knowledge considering musculoskeletal problems and sport specific demands |
| Care | Regular and singular care | Multiple and complex care with specialized and advanced knowledge considering sport specific demands |
| Competencies | ||
| Physical therapy activities | Uses methodical approach to provide effective and curative assistance to clients with movement problems, making decisions according to the evidence-based practice principles | Uses methodical approach to provide effective and curative assistance to clients with movement problems with a specific focus regarding sport, making decisions according to the evidence-based practice principles |
| Communication | Both verbally and non-verbally in a clear, transparent, effective and efficient way to reach a high level of patient satisfaction | Both verbally and non-verbal ly in a clear, transparent, effective and efficient way to reach a high level of patient satisfaction within the sport specific context |
| Collaboration | With relevant professionals and in collaborative networks | With relevant professionals, in collaborative sports networks or as a member of a sport team |
| Knowledge sharing and scientific research | Works according to the principles of EBP and developing clinical expertise | Works according to the principles of EBP and developing clinical expertise in a sport specific context, in dose collaboration with scientists |
| Acting in the interest of society | Practices the profession of PT in a socially responsible way | Practices the profession of PT in a socially responsible way, promoting an active and healthy life style |
| Organization | Acts as a manager for his/her own professional activities | Acts as a manager for his/her own professional activities and as a leader within an organization |
| Professional conduct | Takes responsibility for actions and carefully balances personal and professional roles | Takes responsibility for actions and carefully balances personal and professional roles |
A single physical therapist may have rehabilitated more than one pivoting athlete participating in this study.
MEASUREMENT PROCEDURES
To address the first aim, which focused on adherence to the guideline, an athlete was labeled as tested by their primary physical therapist as ‘yes’ or ‘no’ and having met the RTP criteria ‘yes’ or ‘no’ (both dichotomous variables). For the second aim, exploring the difference in practice guideline adherence between sports physical therapists and non-sports physical therapists, the athlete was labeled as having had rehabilitation with a sports physical therapist ‘yes’ or ‘no’ (dichotomous variable).
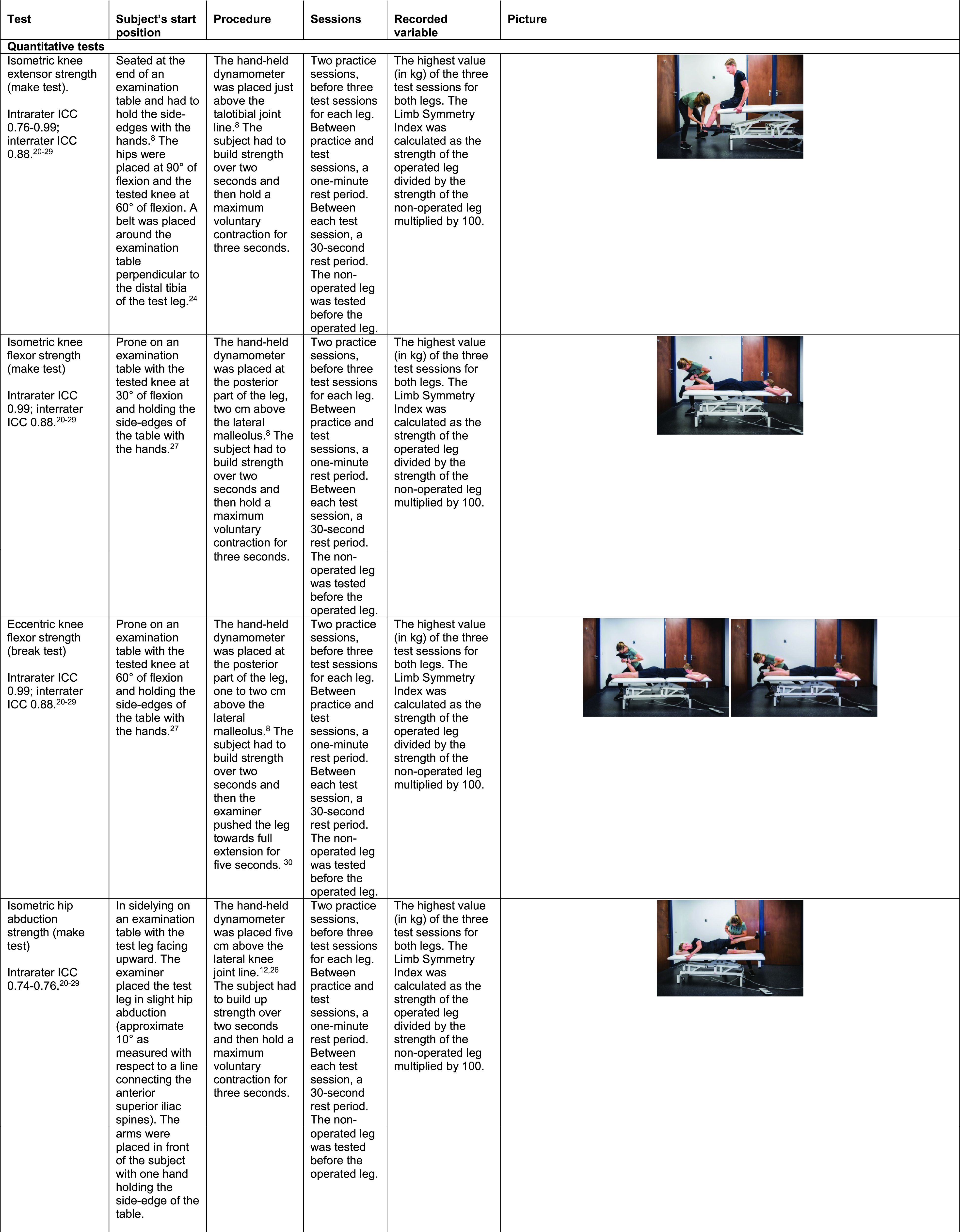
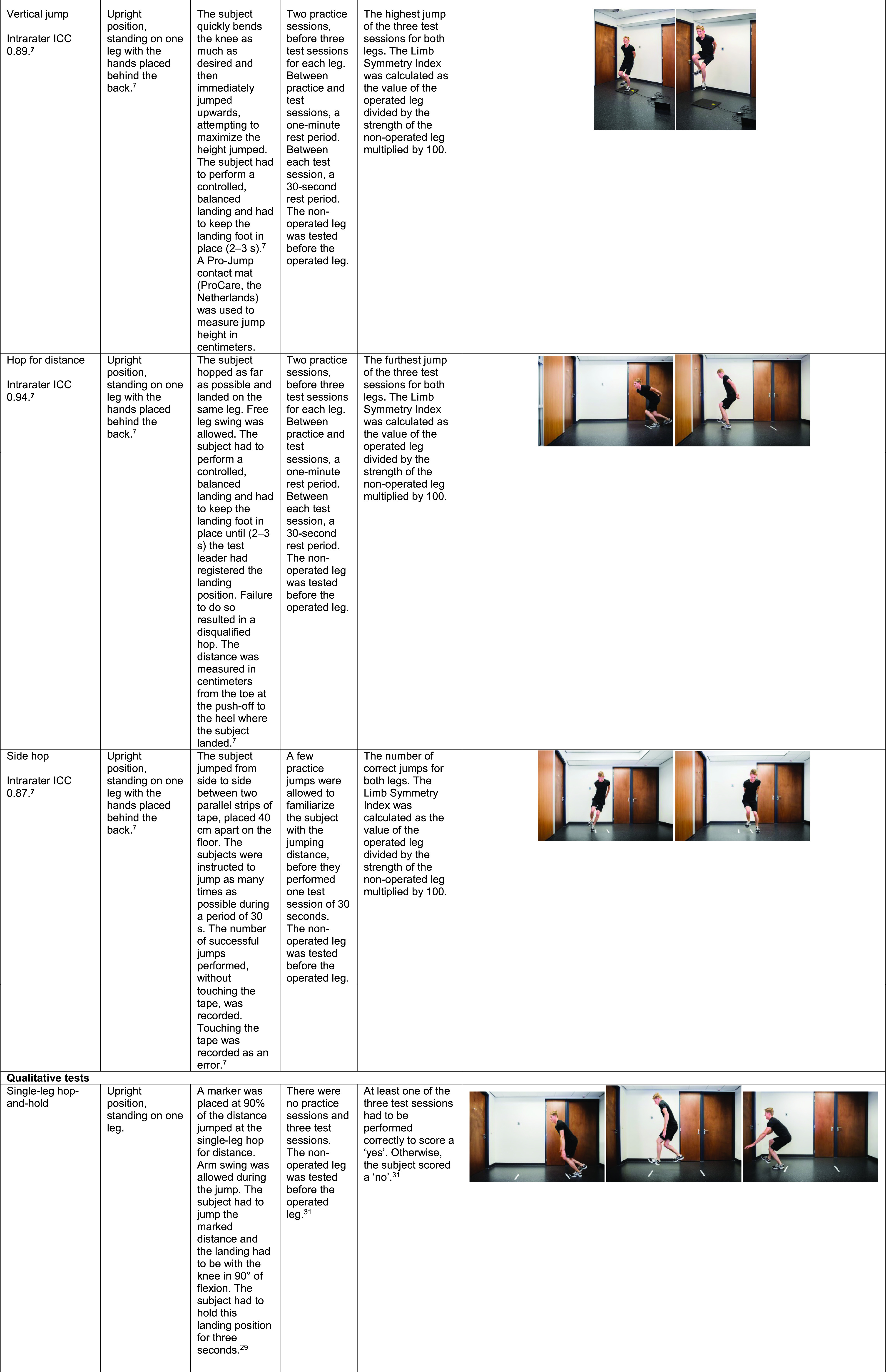
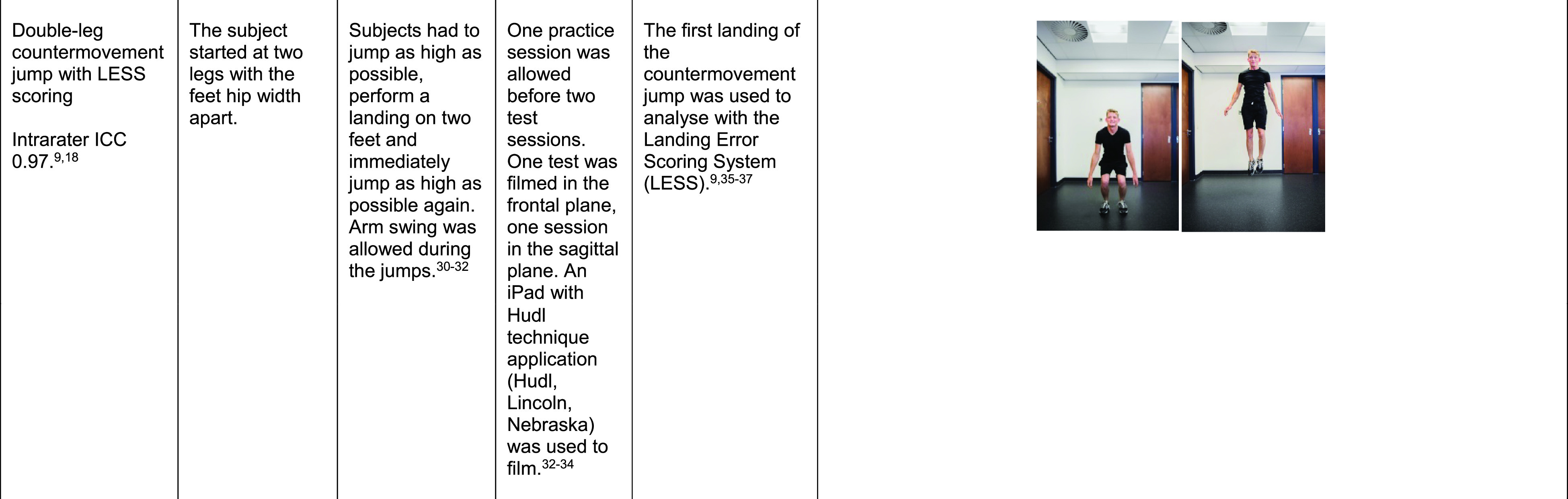
ACLR practice guideline criteria consist of seven movement quantity tests and two movement quality tests.2,3,6-9 All quantitative and qualitative RTP criteria can be found in Table 1 and are described in detail in Appendix A. Isokinetic dynamometry is the gold standard for strength measurements, but only accessible for a small group of Dutch physical therapists due to issues with portability and cost-effectiveness. Therefore, to make sure all Dutch physical therapists were able to perform these tests in daily practice, strength tests for knee and hip muscles were executed with a MicroFET2® hand-held dynamometer (ProCare, the Netherlands).
Meeting the RTP criteria was recorded as ‘yes’ or ‘no’ (dichotomous variable). To score a ‘yes’ all nine quantitative and qualitative RTP criteria had to be met.
All RTP measurements after discharge from the primary physical therapist were performed by the primary researcher (NM) at Clinic ViaSana. The primary researcher is a sports physical therapist with ten years of experience, specialized in ACL rehabilitation, who teaches how to perform RTP measurements to Dutch physical therapists and physical therapy students, and the first author of the Dutch ACLR practice guideline.
STATISTICAL METHODS
Data analysis was performed with IBM SPSS Statistics 21.0 (IBM, Armonk, NY).
To address the first aim, which focussed on adherence to the practice guideline, athlete characteristics were analyzed using descriptive statistics and an independent samples T-test was performed to analyze differences between athletes tested by their primary physical therapist and those not tested. For all RTP measurements means and standard deviations, as well as the number and percentages of athletes meeting the RTP criteria were calculated with descriptive statistics. There were no missing values. Crosstabs with a chi-square test were used for the percentage of athletes meeting the RTP criteria, comparing athletes that were already tested with those not yet tested by their primary physical therapist.
To address the second aim, exploring the difference in practice guideline adherence between sports physical therapists and non-sports physical therapists, an independent samples T-test was performed to analyze differences in baseline characteristics between athletes treated by a sports physical therapist and a non-sports physical therapist. Additionally, crosstabs with a chi-square test were used to compare the number of athletes already tested between sports physical therapists and non-sports physical therapists.
RESULTS
One-hundred-and-fifty-eight pivoting athletes were included (54 females, 104 males; mean age 24 ± 6 years) all of whom completed RTP testing at Clinic ViaSana, at a mean of 12 ± 3 months after ACLR. Characteristics of the pivoting athletes are listed in Table 3. There were no differences in baseline characteristics between athletes tested by their primary physical therapist and those not tested (Table 3). The TAS post-rehabilitation decreased compared to the preoperative TAS (8.6 ± 0.8 respectively 7.8 ± 1.7; p<0.001).
Table 3.
Characteristics of the participating pivoting athletes and comparison between athletes already tested or not tested by their primary physical therapist.
| All athletes | Athletes tested by their primary physical therapist | Athletes not tested by their primary physical therapist | p-value** | |
|---|---|---|---|---|
| N | 158 | 69 | 89 | |
| Sex, N (%) Male | 104(66) | 45 (65) | 59 (66) | 0.888 |
| Female | 54(34) | 24 (35) | 30 (34) | |
| Age in years (mean ± SD*) | 24 ± 6 | 24 ± 6 | 24 ± 7 | 0.486 |
| Weight in kg (mean ± SD) | 73 ± 11 | 73 ± 11 | 74 ± 10 | 0.899 |
| Height in cm (mean ± SD)' | 177 ± 13 | 178 ± 9 | 176 ± 15 | 0.368 |
| Rehabilitation duration in months (mean ± SD) | 12 ± 3 | 12 ± 4 | 12 ± 3 | 0.357 |
| Tegner Activity Scale (TAS) (mean ± SD) | ||||
| Preoperative | 8.6 ± 0.8 | 8.6 ± 0.8 | 8.5 ± 0.8 | 0.844 |
| Post-rehabilitation | 7.8 ± 1.7 | 7.8 ± 1.7 | 7.8 ± 1.6 | 0.955 |
* Age, weight and height were measured preoperatively
** p-value for comparison between athletes tested by their own physical therapist and those not tested by their own physical therapist
Of the 158 participating athletes, 25 (16%) met all nine RTP criteria when the primary researcher (NM) performed the tests. The 158 athletes rehabilitated with 108 different physical therapists, of whom 49 were registered sports physical therapists.
INFLUENCE OF GUIDELINE ADHERENCE
Of the 158 participating athletes that were tested by the primary researcher, 69 (44%) had already been tested by their own physical therapist. Of these 69 athletes, 16 (23%) met all RTP criteria when measured at Clinic ViaSana, compared to nine (10%) of those not tested by their own physical therapist (p = 0.026) (Table 4).
Table 4.
Results on the return to play (RTP) measurements for all athletes (N = 158) and comparison of results between athletes tested by their primary physical therapist (N = 69) and those not tested by their primary physical therapist (N = 89).
| RTP measurement | LSI (all athletes), mean (± SD) | Athletes passing the RTP criterion (all athletes), N (%) | Athletes passing the RTP criterion (athletes tested), N (%) | Athletes passing the RTP criterion (athletes not tested), N (%) | p-value* |
|---|---|---|---|---|---|
| Isometric knee extensor | 100 (±11) | 133(84) | 61(81) | 72 (88) | 0.200 |
| strength | |||||
| Isometric knee flexor | 94 ( ± 12) | 101 (64) | 50 (73) | 51 (57) | 0.049 |
| strength | |||||
| Eccentric knee flexor | 95 ( ± 14) | 98 (62) | 46 (67) | 52 (58) | 0.290 |
| strength | |||||
| Isometric hip abduction strength | 102 ( ± 11) | 136(86) | 60 (87) | 76 (85) | 0.778 |
| Vertical jump | 93 ( ± 12) | 101 (64) | 48 (70) | 53 (60) | 0.194 |
| Hop for distance | 98 ( ± 7) | 139 (88) | 61 (88) | 78 (88) | 0.883 |
| Side hop | 94 ( ± 16) | 107 (68) | 47 (68) | 60 (67) | 0.926 |
| All quantitative measurements | 30 (19) | 17(25) | 13(15) | 0.111 | |
| Single-leg hop-and-hold | |||||
| Operated leg | _ | 136 (86) | 61 (88) | 75 (84) | 0.456 |
| Non-operated leg | - | 138 (87) | 61 (88) | 77(87) | 0.723 |
| CMJ with LESS | |||||
| Operated leg | 4.8 ( ± 2.6) | 101 (64) | 52 (75) | 49 (55) | 0.024 |
| Non-operated leg | 4.8 ( ± 2.6) | 103 (65) | 55 (80) | 48 (54) | 0.003 |
| Both qualitative measurements | |||||
| Only the operated leg | - | 89 (56) | 47 (68) | 42 (47) | 0.009 |
| - | 91 (58) | 50 (73) | 41 (46) | 0.001 | |
| Only the non-operated leg | |||||
| Both legs together | - | 81 (51) | 46 (67) | 35 (39) | 0.001 |
| All 9 measurements | - | 25 (16) | 16 (23) | 9(10) | 0.026 |
| together |
RTP = return to play, LSI = Limb Symmetry Index, CMJ = counter movement jump, LESS = Landing Error Scoring System *p-value for comparison between athletes tested by their own physical therapist and those not tested by their own physical therapist
Thirty athletes (19%) met the RTP criteria for all seven quantitative measurements and 81 athletes (51%) met the RTP criteria for both qualitative measurements (Table 5). Except for isometric knee flexor strength (p = 0.049), there were no differences between athletes that were already tested by their primary physical therapist and those that were not tested by their primary physical therapist in terms of quantitative RTP measurements. However, athletes that were already tested by their primary physical therapist more often met both qualitative RTP criteria (67% versus 39%; p = 0.001) (Table 4).
Table 5.
Countermovement Jump with Landing Error Scoring System (LESS) analysis and number of athletes having the error condition per LESS item.9
| LESS item (filmed in sagittal/frontal plane) | Error descriptor | Error descriptor seen on operated leg, N (%) | Error condition seen on non-operated leg, N (%) |
|---|---|---|---|
| Knee flexion angle at initial contact (sagittal) | Knee flexion < 30 ° | 80(51) | |
| Hip flexion angle at initial contact (sagittal) | Thigh is in line with the trunk | 10(6) | |
| Trunk flexion angle at initial contact (sagittal) | Trunk is vertical on the hip | 47 (30) | |
| Ankle plantarflexion angle at initial contact (sagittal) | Foot lands heel to toe or flat | 6(4) | |
| Knee valgus angle at initial contact (frontal) | Line straight down from centre of the patella is medial to the midfoot | 53 (34) | 58 (37) |
| Lateral trunk flexion angle at initial contact (frontal) | Midline of the trunk is to the left or right side of the body | 82 (52) | |
| Stance width - wide (frontal) | Line straight down from the tip of the shoulder is inside the foot | 19(12) | 16(10) |
| Stance width - narrow (frontal) | Line straight down from the tip of the shoulder is outside the foot | 36 (23) | 36 (23) |
| Foot position - toe in (frontal) | Internal rotation of foot >30 ° | 0(0) | 0(0) |
| Foot position - toe out (frontal) | External rotation of foot >30 ° | 0(0) | 1(1) |
| Symmetric initial foot contact (frontal) | One foot lands before the other | 69 (44) | |
| Knee flexion displacement (sagittal) | Knee flexion displacement < 45 ° | 32 (20) | |
| Hip flexion at max knee flexion (sagittal) | Thigh does not flex more on the trunk during landing | 12(8) | |
| Trunk flexion at max knee flexion (sagittal) | The trunk does not flex more during landing | 23 (15) | |
| Knee valgus displacement (frontal) | Line straight down from center of the patella is medial to the great toe during max knee valgus | 88 (56) | 81 (51) |
The most common LESS errors were a knee flexion angle under 30 ° at initial contact, the presence of lateral trunk flexion at initial contact, a non-symmetrical initial foot contact, and the presence of knee valgus during landing (Table 5).
INFLUENCE OF PHYSICAL THERAPIST
There were no differences in baseline characteristics between athletes that rehabilitated with a sports physical therapist or non-sports physical therapist (Table 6). Eighty-seven athletes rehabilitated with a sports physical therapist and 45 of them (52%) had performed RTP measurements with their primary sports physical therapist. Seventy-one athletes rehabilitated with a non-sports physical therapist and 24 of them (34%) had performed the RTP measurements with their primary non-sports physical therapist (p = 0.024) (Table 7).
Table 6.
Comparison of athlete characteristics between athletes rehabilitating with a sports physical therapist or non-sports physical therapist.
| Athletes rehabilitating with a sports physical therapist | Athletes rehabilitating with a non-sports physical therapist | p-value** | |
|---|---|---|---|
| N | 87 | 71 | |
| Sex, N (%) | |||
| Male | 57 (67) | 47 (66) | 0.929 |
| Female | 30 (33) | 24(34) | |
| Age in years, mean ± SD* | 24 ± 6 | 24 ± 7 | 0.601 |
| Weight in kg, mean ± SD* | 72 ± 10 | 75 ± 12 | 0.161 |
| Height in cm, mean ± SD* | 177 ± 15 | 177 ± 9 | 0.887 |
| Rehabilitation duration in months, mean ± SD | 12 ± 3 | 12 ± 4 | 0.963 |
| Tegner Activity Scale (TAS), mean ± SD | |||
| Preoperative | 8.6 ± 0.8 | 8.6 ± 0.8 | 0.985 |
| Post-rehabiliation | 7.8 ± 1.7 | 7.9 ± 1.6 | 0.712 |
* Age, weight and height were measured preoperatively
** p-value for comparison between athletes rehabilitating with a sports physical therapist and those rehabilitating with a non-sports physical therapist
Table 7.
Crosstabs of number of athletes who had return to play (RTP) measurements taken by their treating physical therapist, compared between sports physical therapists and non-sports physical therapists.
| Athletes rehabilitating with a sports physical therapist (N = 87) | Athletes rehabilitating with a non-sports physical therapist (N = 71) | p-value | |
|---|---|---|---|
| RTP measurements by their treating physical therapist?, N (%) | |||
| Yes | 45 (52) | 24 (34) | 0.024 |
| No | 42 (48) | 47 (66) |
DISCUSSION
The result regarding whether Dutch physical therapists adhere to the provided ACLR practice guideline is disappointing; only 44% of the pivoting athletes were tested by their primary physical therapist. The result concerning whether therapists were advising regarding return to sport using the RTP measurements is even more alarming; only 16 (23%) of the 69 athletes who were tested by their primary physical therapist received an advice consistent with the ACLR guideline, based on the RTP measurements conducted by the primary researcher. An important finding was that athletes who rehabilitated with a sports physical therapist were more commonly tested regarding the ACLR guideline than athletes who rehabilitated with a non-sports physical therapist, 52% versus 34% respectively. This shows that sports physical therapists have a better adherence to the ACLR practice guideline than non-sports physical therapists. However, the percentage of sports physical therapists adhering to the guideline still remains low.
Even after the publication and implementation of the Dutch ACLR practice guideline by the KNGF in 2014, Dutch physical therapists still struggle with using RTP measurements and deciding when to clear their pivoting athletes for RTP, since only 44% of the athletes had performed RTP measurements with their primary physical therapist. This might be caused by lack of equipment or limited knowledge about tests or guideline content.
These findings are consistent with previous studies on guideline adherence in other diagnoses in physical therapy both in Belgium and the United States.13,14 The authors of these studies also found better adherence to published guidelines in physical therapists with a specialization compared to those without with regard to treatment for knee osteoarthritis and low back pain.13,14
It is quite strange that RTP criteria are underutilized, since two previously published studies found that pivoting athletes that passed quantitative RTP criteria including strength and hop tests had a strongly reduced risk of sustaining a second ACL injury in the first two years after ACLR.15,16 Concerning movement quality previous authors have found that altered hip and knee biomechanics when landing from a jump are predictors of a second ACL injury after ACLR rehabilitation and RTP.17,18 The use of qualitative RTP criteria might be not as common as the use of quantitative criteria, but they are also important in the RTP decision.
Considering this, the athletes who do not pass the RTP criteria (84% in this study) but still return to their preinjury sport, might have a higher chance of a second ACL injury in the near future.
Overall, the results of this study suggest that the Dutch ACLR practice guideline was not implemented properly. Incorporating ACLR rehabilitation and RTP measurements into bachelor level physical therapy education is strongly suggested, thereby potentially changing the underutilization of rehabilitation guidelines and RTP testing.19,20
LIMITATIONS OF THE STUDY
It could be suggested that pivoting athletes who recently had performed RTP tests with their primary physical therapist were better prepared for the RTP testing performed at Clinic ViaSana, introducing bias regarding how they performed on those tests via a learning effect. However, many athletes who were tested by the primary researcher did not meet the RTP criteria. Besides, only 23% of the athletes who were already tested by their primary physical therapist had received RTP advice consistent with the ACLR practice guideline. This could indicate that RTP measurements are not the main factor in the RTP decision.
Also, athletes who had already been tested, often reported that their physical therapist did not test eccentric hamstring strength or the side hop test; two criteria that were often not met in this study. This could stress the importance of measuring eccentric hamstring strength and the side hop test, both considered important tests for determining a safe return to play after ACLR.
Because 24 (15%) athletes decided to cease pivoting sports after their ACLR rehabilitation, this could have created bias. However, their primary treating physical therapist was told that these athletes should also meet the RTP criteria as stated in the practice guideline. Three of the athletes who ceased performing pivoting sports (13%) met all the RTP criteria when tested at Clinic ViaSana, indicating they scored at a similar level compared to the all other athletes in this study.
CONCLUSION
Fifty-six percent of pivoting athletes were cleared for RTP by their physical therapist without using criterion-based decisions as advised in the Dutch ACLR practice guideline. Sports physical therapists more often adhered to the practice guideline than non-sports physical therapists (52% versus 34%), but with only half of them adhering, this percentage remains far too low.
Only 16% of pivoting athletes actually met all RTP criteria, but athletes who were already tested by their own physical therapist more commonly met all RTP criteria (23% versus 10%), indicating those not tested might have a higher chance for a second ACL injury. Interestingly, 77% of the athletes tested by their primary physical therapist were given RTP advice, which was inconsistent with the ACLR practice guideline. Based on these results, more attention needs to be paid to implementing the ACLR practice guideline and ACLR rehabilitation and RTP measurements need to be incorporated into general physical therapy education.
Appendix: Return to play (RTP) measurements
REFERENCES
- 1.Ardern CL Taylor NF Feller JA, et al. Fifty-five percent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543-1552. [DOI] [PubMed] [Google Scholar]
- 2.van Melick N van Cingel REH Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50:1506-1515. [DOI] [PubMed] [Google Scholar]
- 3.van Melick N Hullegie W Brooijmans F, et al. KNGF Evidence Statement revalidatie na voorste-kruisbandreconstructie. Amersfoort: De Gans; 2014. [Google Scholar]
- 4.Beischer S Senorski EH Thomeé C, et al. Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:1966-1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toole AR Ithurburn MP Rauh MJ, et al. Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: How many actually meet recommended return-to-sport criterion cutoffs? J Orthop Sports Phys Ther. 2017;47:825-833. [DOI] [PubMed] [Google Scholar]
- 6.Engelen-van Melick N van Cingel RE Tijssen MP, et al. Assessment of functional performance after anterior cruciate ligament reconstruction: a systematic review of measurement procedures. Knee Surg Sports Traumatol Arthrosc. 2013;21:869-879. [DOI] [PubMed] [Google Scholar]
- 7.Gustavsson A Neeter C Thomeé P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:778-788. [DOI] [PubMed] [Google Scholar]
- 8.Muff G Dufour S Meyer A et al. Comparative assessment of knee extensor and flexor muscle strength measured using a hand-held vs. isokinetic dynamometer. J Phys Ther Sci. 2016;28:2445-2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Padua DA Marshall SW Boling MC, et al. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: the JUMP-ACL study. Am J Sports Med. 2009;37:1996-2002. [DOI] [PubMed] [Google Scholar]
- 10.Eshuis R Tegner Y Wolterbeek N, et al. Dutch translation and cross-cultural adaptation of the Lysholm Score and Tegner Activity Scale for patients with anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2016;46:976-983. [DOI] [PubMed] [Google Scholar]
- 11.Rehorst J Tak I Glashouwer P, et al. Beroepscompetentieprofiel sportfysiotherapeut. Amersfoort: NVFS; 2016. [Google Scholar]
- 12.de Vries C Hagenaars L Kiers H, et al. The physical therapist – a professional profile. Amersfoort: KNGF; 2014. [Google Scholar]
- 13.Ladeira CE Cheng MS da Silva RA. Clinical specialization and adherence to evidence-based practice guidelines for low back pain management: a survey of US physical therapists. J Orthop Sport Phys Ther. 2017;47:347-358. [DOI] [PubMed] [Google Scholar]
- 14.Spitaels D Hermens R Van Assche D et al. Are physiotherapists adhering to quality indicators for the management of knee osteoarthritisϿ. An observational study. Musculoskelet Sci Pract. 2017:27:112-123. [DOI] [PubMed] [Google Scholar]
- 15.Grindem H Snyder-Mackler L Moksnes H, et al. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50:804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kyritsis P Bahr R Landreau P, et al. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50:946-951. [DOI] [PubMed] [Google Scholar]
- 17.Paterno MV Schmitt LC Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith HC Johnson RJ Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med. 2012;40:521-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grindem H Arundale AJ Ardern CL. Alarming underutilisation of rehabilitation in athletes with anterior cruciate ligament reconstruction: Four ways to change the game. Br J Sports Med. 2018;52:1162-3. [DOI] [PubMed] [Google Scholar]
- 20.Dingenen B Gokeler A. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: A critical step back to move forward. Sports Med. 2017;47:1487-1500. [DOI] [PubMed] [Google Scholar]
- 21.Toonstra J Mattacola CG. Test-retest reliability and validity of isometric knee-flexion and -extension measurement using 3 methods of assessing muscle strength. J Sport Rehabil. 2013;Technical Notes(7).pii2012-0017. [DOI] [PubMed] [Google Scholar]
- 22.Bittencourt NF Santos TR Gonçalves GG, et al. Reference values of hip abductor torque among youth athletes: Influence of age, sex and sports. Phys Ther Sport. 2016;21:1-6. [DOI] [PubMed] [Google Scholar]
- 23.Jackson SM Cheng MS Smith AR Jr, et al. Intrarater reliability of hand held dynamometry in measuring lower extremity isometric strength using a portable stabilization device. Musculoskelet Sci Pract. 2017;27:137-141. [DOI] [PubMed] [Google Scholar]
- 24.Katoh M. Reliability of isometric knee extension muscle strength measurements made by a hand-held dynamometer and a belt: a comparison of two types of device. J Phys Ther Sci. 2015;27:851-854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim WK Kim DK Seo KM, et al. Reliability and validity of isometric knee extensor strength test with hand-held dynamometer depending on its fixation: A pilot study. Ann Rehabil Med. 2014;38:84-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim SG Lee YS. The intra- and inter-rater reliabilities of lower extremity muscle strength assessment of healthy adults using a hand held dynamometer. J Phys Ther Sci. 2015;27:1799-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thorborg K Bandholm T Hölmich P. Hip- and knee-strength assessments using a hand-held dynamometer with external belt-fixation are inter-tester reliable. Knee Surg Sports Traumatol Arhtrosc. 2013;21:550-555. [DOI] [PubMed] [Google Scholar]
- 28.Thorborg K Petersen J Magnusson SP, et al. Clinical assessment of hip strength using a hand-held dynamometer is reliable. Scand J Med Sci Sports. 2010;20:493-501. [DOI] [PubMed] [Google Scholar]
- 29.Whiteley R Jacobsen P Prior S, et al. Correlation of isokinetic and novel hand-held dynamometry measures of knee flexion and extension strength testing. J Sci Med Sport. 2012;15:444-450. [DOI] [PubMed] [Google Scholar]
- 30.Stratford PW Balsor BE. A comparison of make and break tests using a hand-held dynamometer and the Kin-Com. J Orthop Sports Phys Ther. 1994;19:28-32. [DOI] [PubMed] [Google Scholar]
- 31.Myer GD Ford KR Hewett TE. Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J Athl Train. 2004;39:352-364. [PMC free article] [PubMed] [Google Scholar]
- 32.Munro A Herrington L Carolan M. Reliability of 2-dimensional video assessment of frontal-plane dynamic knee valgus during common athletic screening tasks. J Sport Rehabil. 2012;21:7-11. [DOI] [PubMed] [Google Scholar]
- 33.Myer GD Ford KR Khoury J, et al. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med. 2010;38:2025-2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noyes FR Barber-Westin SD Fleckenstein C, et al. The drop-jump screening test: difference in lower limb control by gender and effect of neuromuscular training in female athletes. Am J Sports Med. 2005;33:197-207. [DOI] [PubMed] [Google Scholar]
- 35.Padua DA Bling MC DiStefano LJ, et al. Reliability of the Landing Error Scoring System-Real Time, a clinical assessment tool of jump-landing biomechanics. J Sport Rehabil. 2011;20:145-156. [DOI] [PubMed] [Google Scholar]
- 36.Gokeler A Eppinga P Dijkstra PU et al. Effect of fatigue on landing performance assessed with the Landing Error Scoring System (LESS) in patients after ACL reconstruction. A pilot study. Int J Sports Phys Ther. 2014;9:302-311. [PMC free article] [PubMed] [Google Scholar]
- 37.Padua DA DiStefano LJ Beutler AI, et al. The Landing Error Scoring System as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. J Athl Train. 2015;50:589-595. [DOI] [PMC free article] [PubMed] [Google Scholar]


