Abstract
Background:
Athletic pubalgia is a prevalent injury in athletes who kick, pivot, and cut, however it is poorly described in the literature. Many athletes with this diagnosis fail conservative management secondary to continued pain with activity and require surgical intervention for return to sport.
Purpose:
The purpose of this case report is to describe an intervention strategy focusing on gait retraining and hip and lumbopelvic stability for a female runner diagnosed with athletic pubalgia and a labral tear of the hip.
Case Description:
This case report involved a 45-year-old female runner who was seen for 14 visits, from examination to return to sport, with a follow up at 12 months post discharge. Interventions included hip, pelvic, and lumbar stability exercises, and gait retraining. Outcomes measurements included: pain on the numeric pain rating scale, the Lower Extremity Functional Scale (LEFS), gait mechanics, strength, and participation in sport.
Outcomes:
At discharge the subject demonstrated improved strength of all muscle groups and changes in lower extremity running biomechanics. Changes in running mechanics included increased cadence, decreased pelvic drop, diminished over striding, and improved knee control with less valgus movement during the stance phase of gait. The subject reported no pain with running or recreational activities at discharge and follow up at 12 months post discharge.
Discussion/Conclusion:
Most of the literature on conservative rehabilitation for athletic pubalgia focuses on athletes whose sports require pivoting and kicking. The literature provides little information on gait analysis and retraining for runners with a diagnosis of athletic pubalgia and/or hip labrum tears. The program used in this case report including gait retraining and hip, pelvic, and lumbar stability training allowed for full return to running in a 45-year-old female with a diagnosis of hip labrum tear and athletic pubalgia. Further research is needed to discern best conservative treatment for runners with athletic pubalgia and/or hip labral tears.
Level of evidence:
4
Keywords: athletic pubalgia, gait retraining, hip labrum tear, movement system, stability training
INTRODUCTION
Athletic pubalgia (AP) is a broad diagnostic term used to describe groin pain experienced by athletes.1 There is inconsistency regarding what specific anatomic structures are involved in this diagnosis and therefore there is no consistent terminology to accurately define the condition. Other diagnostic labels for the condition include ‘sports hernia’, ‘chronic groin pain’, ‘core muscle injury’, and ‘athletic groin pain’. The potential occurrence of more than one pathology contributing to the patient's complaint can further complicate the process of diagnosis.1
Many gaps exist in the literature surrounding athletic pubalgia, leading to unanswered clinical questions. The incidence rate is hard to determine based on unclear diagnostic criteria.2 Athletic pubalgia is more common in men than women according to the literature.3 Athletic pubalgia is historically thought to be most common in sports such as ice hockey, soccer, rugby, Australian rules football, martial arts, basketball, baseball and football2 due to sport demands that include change in direction, twisting, and kicking.4 However, evidence of runners with this diagnosis is emerging.5,6 The mechanism of injury is poorly understood and many theories have been proposed.3 One of the most popular theories of athletic pubalgia development in runners has been attributed to sheering at the pelvis due to a weakness in the lower abdominal muscles as compared to the hip adductors. The result is a disruption in the attachment of the rectus abdominus to the pubic bone.3
The difficulty in diagnosis and the use of widely variant terminology appears to have resulted in the publication of little consistent evidence as to the best rehabilitation strategy for athletic pubalgia.1 Much of the research focuses on surgical interventions or a population of athletes that participate in team sports that require cutting, pivoting, and kicking.1,3,5,7 King et al8 recently reported on conservative rehabilitation with a focus on lumbopelvic control, but her subjects participated in multidirectional sports and were not recreational athletes. Thorborg et al9 reviewed the literature for conservative care in athletes with groin pain and did not find evidence for rehabilitation of groin pain with more than one underlying pathology. Ellsworth et al4 describes the importance of hip and lumbopelvic strength, coordination, and stability but this was based on treatment for an ice hockey athlete. Return to play time varies in the literature, ranging from six weeks to six months for conservative care and 4-24 weeks post-operatively.3,4,7,8,10 Evidence is lacking regarding the use of conservative care in athletes whose primary sport is running and have more than one diagnosis.
Therefore, the purpose of this case report is to describe an intervention strategy focusing on gait retraining and hip and lumbopelvic stability for a female runner diagnosed with athletic pubalgia and a labral tear of the hip.
Case Description: Subject History and Systems Review
The subject was a Caucasian, 45-year-old, female who presented to outpatient physical therapy with pain in the right pubic area and right hip that started five months prior. She reported the pain started during a run, lasted the duration of the run, and then returned on all subsequent runs. She denied an acute injury leading to the pain. Her past medical history was unremarkable except for a left ACL reconstruction three years previously, for which she completed the recommended course of physical therapy and returned to her prior level of function. She participated in running 25-30 miles per week for the two years between her return to prior level of function and the recent hip/groin injury.
At the time of the physical therapy examination, she was limited to running two miles per week due to pain of 5/10 in the hip and lower abdominal area, during running. Prior to her arrival at physical therapy, the subject met with her orthopedist. She had an MRI of her right (R) hip and R pelvis, leading to a diagnosis of athletic pubalgia and a labral tear from the orthopedist. At that time surgery was suggested by the physician, which the subject declined. She had a steroid injection to her right hip three weeks before starting physical therapy. During the five months leading up to physical therapy, the subject tried self-treatment by avoiding running and performing open chain hip strengthening exercises, targeting the glutes. Even with self-management she was still unable to find relief from her symptoms. The subject did, however, report improvement in her pain level after the injection. The subject stated her primary goal was to return to running without pain or other limitations. The subject of this case report was informed that the case would be submitted for publication and she agreed to the use of her data for this purpose.
Clinical Impression #1
The subjective history aligned with the symptoms of athletic pubalgia: unilateral pain with activity,1 insidious onset,1 deep groin/abdominal area pain,11 pain present for several months.1,11 However, runners and females are not commonly described in the athletic pubalgia literature.9,11 The subjective history did not reveal any red flags and therefore the subject was deemed appropriate for physical therapy.1
To complete the objective examination, the plan was to clear the lumbar spine as the source of the pain and observe functional movements in order to note any biomechanical deviations. Range of motion, manual muscle testing (MMT), and palpation would be performed in an attempt to reproduce the subject's pain in order to confirm the hypothesis of athletic pubalgia.
EXAMINATION
Observation revealed a right lateral weight shift during squatting which may have been influenced by the left ACL reconstruction three years prior. Single leg stance with eyes closed resulted in a pelvic drop, bilaterally. Bilateral single leg squats were observed as this is a component of running. During single leg squatting, the subject lacked knee control causing dynamic valgus movement bilaterally, but greater on the right knee than the left. Kibler and colleagues12 have suggested the use of single leg squat as an indicator of core strength.
Running gait was observed because this was the one activity that caused pain for the subject. The subject ran on a treadmill, at her preferred speed of 6.0 miles per hour, at a 0% incline. She was in her preferred running shoe, a neutral, cushioned shoe without orthotics. She was recorded in the frontal and sagittal planes with the Hudl Technique application (Agile Sports Technology, Inc., Lincoln, NE) that allowed the video to be slowed for assessment. The recording started after the subject ran for five minutes. While running, the subject demonstrated over striding, defined by the foot being anterior to the center of mass and knee in full extension, in the sagittal plane, during initial contact.13 In addition, increased hip adduction and dynamic knee valgus at midstance were noted. All of these gait characteristics were observed bilaterally. No foot or ankle abnormalities were observed. Her cadence was 160 steps per minute at initial examination. The 2D video gait examination, performed in the frontal and sagittal planes, has previously been described as being reliable.14
Additional examination findings are listed in Table 1. Both MMT and palpation were used in an attempt to reproduce the subject's pain.1,9 No pain was reproduced during MMT however, the subject reported pain with eccentric control of the rectus femoris and iliopsoas during leg lowering, from mid-range to the table, of a straight leg raise motion. The patient did not have pain with palpation of the pubic ramus.4 The lumbar exam did not reproduce the subject's pain, however hypomobility was found during palpation. Both the Thomas Test and Ober's Test were positive.15 The Lower Extremity Functional Scale (LEFS) was used because it has been found to be reliable and valid for outpatient physical therapy for individuals with lower extremity dysfunction.17 The subject scored 73/80 on the initial LEFS.
TABLE 1.
Objective measures at examination and discharge.
| Initial examination | Discharge | ||
|---|---|---|---|
| Hip MMT15 | Hip flexion Hip extension Hip abduction Hip adduction Hip internal rotation Hip external rotation |
R 5/5 L 5/5 R 4+/5 L 4+/5 R 4/5 L 4+/5 R 4+/5 L 4+/5 R 4/5 L 4+/5 R 4/5 L 4+/5 |
5/5 B 5/5 B 5/5 B 5/5 B 4+/5 B 4+/5 B |
| Lumbar AROM16 |
Flexion Extension |
Dysfunctional, no pain Functional, no pain |
Functional, no pain Functional, no pain |
| Palpation | Lumbar PAIVMs Pubic tubercles Hip adductors |
Pain free Pain free “Increased tension and tone” |
|
| Hip ROM15 | Thomas test Ober's test Internal and external rotation |
R positive for iliopsoas Positive B WNL B |
|
| Running gait13 | Cadence Over striding Knee flexion at initial contact |
160 Yes Decreased |
170 No WNL |
| LEFS | 73/80 | 80/80 |
Abbreviations: manual muscle test (MMT), right (R), left (L), bilateral (B), active range of motion (AROM), passive accessory intervertebral movements (PAIVMs), range of motion (ROM), within normal limits (WNL)
Clinical Impression #2
During the examination, the authors cleared the lumbar spine as the source of the R pubic and hip pain with movement testing and palpation.1,18 Running was the only examination technique that reproduced the subject's pain. Based on the poor motor control during single leg stance, squats, single leg squats, and gait, along with pain during running, the authors hypothesized that the subject's hip and pelvis were incurring additional stress during running that could be contributing to the pain. The subject did have a medical diagnosis of athletic pubalgia and hip labral tear on MRI and her subjective history was consistent with athletic pubalgia, but her objective findings were not as clear. She did have pain with exertion (running) and pain with eccentric hip flexion but, she lacked tenderness over the pubic ramus.4
Prior to attending physical therapy, the subject tried complete rest from the activity that caused pain (running) as well as general hip muscle strengthening in the open chain. Despite consistent open chain strength training, the subject demonstrated motor control deficits in the hip and lumbopelvic region on examination. In both single leg squat and running, the subject demonstrated an increase in closed chain hip adduction. For these reasons, the authors determined the interventions should include closed chain strength and stability training. Gait retraining was determined to be necessary to decrease over striding and dynamic knee valgus.
With the addition of gait retraining and hip and lumbopelvic stability exercises, the authors expected to see improved biomechanics, decreased pain with running, and an improvement in the LEFS to 80/80 within six weeks. The improvements were expected in six weeks, based on time needed to make both neural and hypertrophy adaptations in muscle.19,20,21
INTERVENTION
A licensed physical therapist, with board-certification in orthopedics or sports physical therapy demonstrated, supervised, and/or performed all interventions. The physical therapists provided verbal and visual cues during the exercises with a goal of the subject being able to control the pelvis in the frontal and sagittal planes while maintaining a neutral spine. An outline of the one-on-one treatment sessions can be seen in Table 2. Exercise prescription was based on how challenging the exercises were to the subject, her ability to complete the exercises correctly, and with an overall goal of improved motor control and strength.
TABLE 2.
Outline of treatment sessions.
| Weeks | Interventions | Dosage |
|---|---|---|
| Week 1-2 | Single leg squat Single leg deadlift Posterior lunge with knee drive Standing hip abduction/ adduction Standing hip flexion/extension Supine core activation CPA: lumbar spine Trigger point release: hip adductors, psoas on right |
x10, B x10, B x10, B x20, B x20, B Grade III-oscillating until increase an in motion was palpated |
| Week 3 | Single leg squat Curtsy squat Single leg dead lift Modified side plank with hip abduction |
15x2, B x10, B 10lbs, 15x2, B Green resistance band, 2x10, B |
| Week 4 | Curtsy squat Posterior lunge with glider Lateral lunge with glider Supine dead bug with kick out Single leg bridge Side step Tall kneeling Palloff press Gait retraining |
x10, B 2x10, B 2x10, B Red resistance band, 2x15, B 2x15, B Green resistance band at ankles, 5x20’, B Black resistance band, x20, B Cadence: 170 |
| Week 5-8 | Posterior lunge with glider Lateral lunge with glider Standing fire hydrant Single leg deadlift with single leg squat Tall kneeling palloff press with shoulder flexion |
2x10, B 2x10, B 2x10, B 2x10, B Black resistance band, x20, B |
| Week 8-12 | Double leg squat jumps Double leg squat jumps with 90 degrees rotation Single leg squat jumps with TRX Single leg squat jumps with opposite knee on plinth Box jumps down Single leg jumps on shuttle Gait retraining |
x20 x10, B x5, R x10, R 2x10, R bands, 3x12, B Cadence 168-172 |
Abbreviations: bilateral (B), central posterior to anterior mobilization (CPA), right lower extremity (R)
The first priority for treatment was to increase strength and stability in the hip, pelvis, and lumbar spine. The subject was non-irritable, and since the only complaint of pain was with running, pain was not the primary focus of the interventions.1 On the first visit, the subject started with single leg, closed chain exercises to focus on the stability from the lower extremity through the lumbar spine during functional movements,1 as seen in Figures 1, 2, and 3. The subject performed all of the single leg stability exercises on one leg prior to switching to the other leg and the therapist emphasized knee, pelvis and lumbar positioning throughout. The exercises were prescribed bilaterally secondary to the lack of motor control found on both sides during the examination.
Figure 1.
Single leg squat with TRX suspension system.
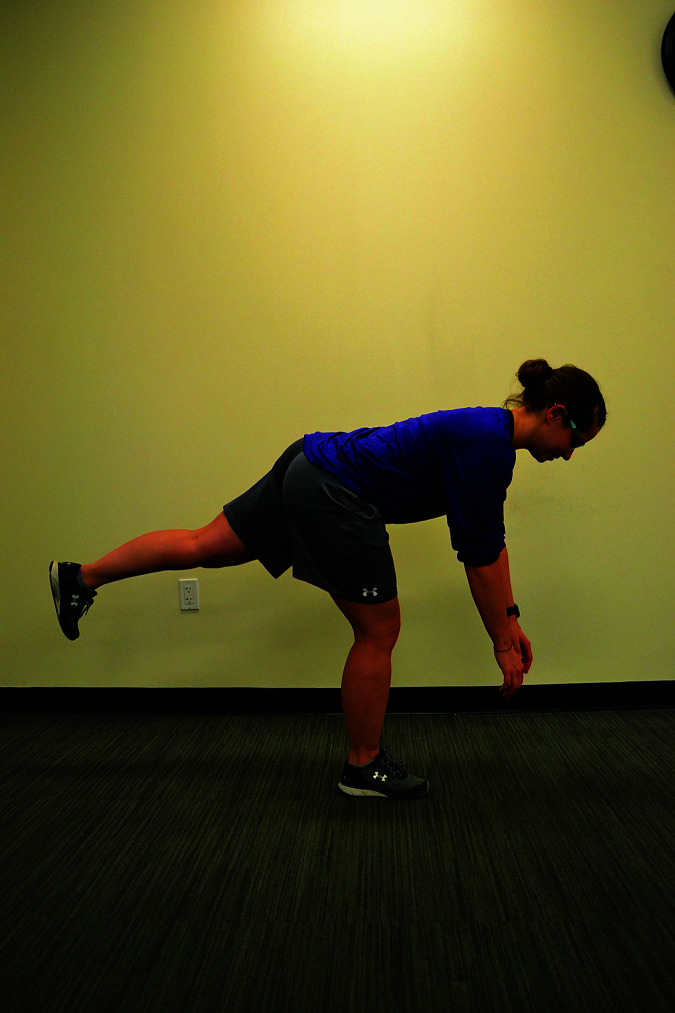
Figure 2.
Single leg dead lift.
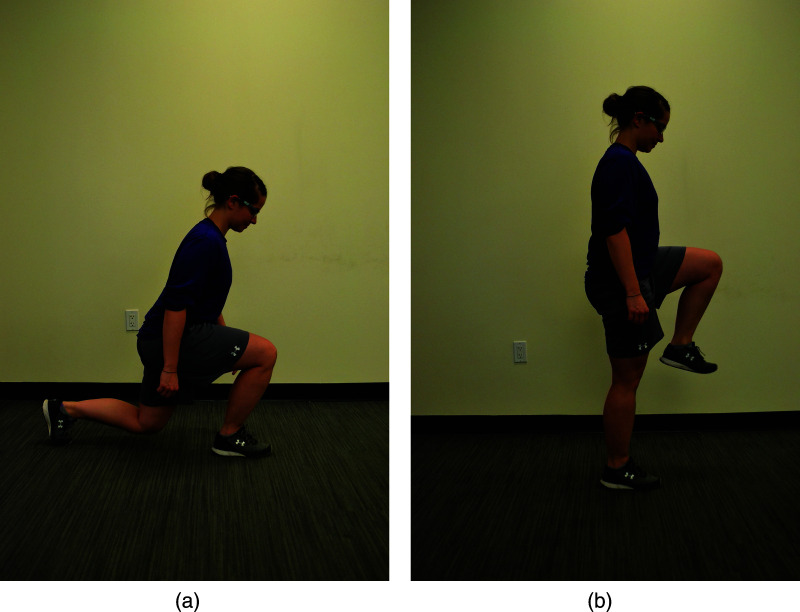
Figure 3.
(a) Starting position for posterior lunge with knee drive. (b) Ending position for posterior lunge with knee drive.
During the initial stages of physical therapy, the subject performed some single leg exercises with upper extremity support from the TRX suspension system (TRXtraining.com) to assist with balance and form. (Figure 1) During visit number two, core stabilization exercises were added,2,22 (Figures 4 and 5). The subject was in hook-lying, while marching and alternating leg lowering were performed, a blood pressure cuff was used for feedback, these exercises were selected based on the work of Brumitt, et al.23 The supine stabilization exercises chosen emphasized local core stabilization with global muscle activation to prevent sheering forces,23 addressing one theory of the cause of athletic pubalgia.3 Throughout the episode of care, the exercises utilized to target the stability of the entire lower extremity and the lumbopelvic complex were similar to those recommended by Hegedus et al1 and King et al.8
Figure 4.
Supine core exercise, marching while maintaining neutral pelvis, with use of blood pressure cuff for feedback.
Figure 5.
Supine core exercise, lower extremity extension while maintaining neutral pelvis, with use of blood pressure cuff for feedback.
Once the subject could easily complete the single leg exercises with the TRX system, she was advanced to unsupported activities. At this stage, the subject performed unsupported single leg exercises in front of a mirror for immediate visual feedback. When the subject could correctly perform the single leg squat, gait retraining was added to address the over striding and dynamic knee valgus in mid-stance. Work by Heiderscheit et al,24 showed that by increasing running cadence between 5% and 10% reduced over striding and decreased the hip adduction and dynamic knee valgus on the stance leg. Consistent with the work by Heiderscheit et al, the subject's running cadence was increased from 160 to 170 steps per minute (6.25%). This intervention was performed on the treadmill, at the same speed and incline used at examination, with intermittent use of an auditory metronome (EUMLab, Chengdu, China) to teach the subject the correct cadence. In the present study, the metronome was used intermittently so the subject would not develop a dependency on the auditory cues.
During treatment sessions, the authors of this study addressed the limitations in mobility found in the lumbar spine and hip musculature during the examination. To help normalize joint range of motion in the lumbar spine, manual therapy was provided beginning at the first visit.2 Central posterior to anterior mobs were applied, at grade III25 until a change in mobility of the segment was felt by the physical therapist. Trigger point release was performed on the iliopsoas to increase available range of hip extension.26 The physical therapist applied pressure to the muscle until a change in tissue tension was noted through palpation. Change in mobility was confirmed by repeating the range of motion testing performed on initial examination. The subject was taught to use a foam roll and lacrosse ball to maintain the range of motion gains between sessions.
The subject received education beginning on the first visit. On day one, the education focused on the importance of improving hip stability in the standing position for improved participation in functional activities and the importance of core dynamic stability to decrease stress on her pubic symphysis and hip. The subject received education throughout the course of care on the rationale for each intervention, proper form for the exercises, and home exercise prescription.
OUTCOMES
Beginning at week three, re-examination found improvements in the initial impairments. At week three, lumbar range of motion was within normal limits. By the end of the episode of care, there was an increase in strength of bilateral lower extremities during manual muscle testing, see Table 1. In addition, the subject reported improvement in pain with functional activities and increased the LEFS score, to 80/80. Despite an improved score on the LEFS, it did not reach the level of minimal detectable change (9 points).17
Functional changes were noted during the episode of care and at long-term follow up, one year after initiating physical therapy. Running gait was reassessed with the Hudl Technique application. The use of a metronome to increase cadence was successful in decreasing the subject's over striding during gait, noted by the decrease in distance between a line drawn down from the center of mass and the heel at initial contact. In addition, increased knee flexion was noted at initial contact. At five weeks post initial examination, the subject was running 5 kilometers (5k), three times per week with 0/10 pain. At 12 weeks (14 visits) the subject had returned to her baseline running of 25-30 miles per week with no complaints of pain. During a verbal follow up, one year after physical therapy, the subject noted she continued to self-progress her exercise program with a focus on single leg activities that challenged the hip, pelvis, and core for strength and position. She continued running without limitations and noted she had run her second fastest 5k time. Finally, she completed a follow up LEFS that was scored at 80/80.
The subject of this case report returned to her sport of choice, running, without surgical intervention. The subject was able to return to sport after 12 weeks of physical therapy, which was longer than outcomes described by other authors.4,8 The British Hernia Society's 2014 Position Statement suggested surgical intervention if pain had not been resolved after two months of physical therapy.7 This subject's return-to-participation time was in agreement with recommendations by Heiderscheit and McClinton.27
DISCUSSION
The purpose of this case report was to describe an intervention strategy focusing on gait retraining and hip and lumbopelvic stability for a female runner diagnosed with athletic pubalgia and a labral tear of the hip. The 45-year-old female runner successfully returned to running and did not have surgery. Athletic pubalgia has not been clearly defined and thus there is limited evidence for successful rehabilitation in the literature. In addition, most of the literature that does exist focuses on male athletes in sports that involve kicking, twisting, and/or sprinting, in contrast with this subject, a female distance runner.
Ellsworth et al4 noted dysfunction between the pelvis and the femur in individuals with athletic pubalgia, consistent with what the authors observed in this female runner. In this case report, the authors hypothesized that closed chain stability training of the hip and lumbopelvic unit would result in a decrease in pain on the numeric pain rating scale and functional improvements. Prior to starting physical therapy, the subject was performing strength training, but in an open chain position, without symptom relief or improvement in function. Having her perform exercises addressing single leg strength, stability, and progressing to single leg landing mechanics gradually exposed her to positions she would encounter with running. The authors hypothesized this would promote her to develop and improve her body awareness through challenging her to maintain lumbopelvic and knee control in a functional, closed chain position. The authors theorized that this improved stability would carry over to her running.
Running was the only functional activity that reproduced the subject's pain, therefore it was important to assess her gait and address her running as part of the intervention. Gait retraining is frequently cited in the literature for patellofemoral pain syndrome, but there is limited research in its application to those with athletic pubalgia or hip labral tears. Cadence retraining, with an increase of 5-10% from a subject's preferred cadence, has been shown to decrease energy absorption at the hip and peak hip adduction.24 In addition, work by Heiderscheit24 and Schubert28 showed cadence training decreased over striding and dynamic knee valgus in runners. Therefore, cadence retraining was deemed important, and was used in this case with the goal of decreasing the stress on the hip joint and musculature.
Surgical intervention for the athletic pubalgia and labrum was prescribed by the orthopedist as the first line of treatment to the subject in this study. Surgical correction of athletic pubalgia can be laparoscopic or open depending on surgeon training.7 The goals of surgical correction are to identify the abnormal structure, reduce tension through the affected structure, and restore the anatomy.7. Return to play is dependent on sport and type of surgical repair, but is reported between two and six months after surgery.3,10 Surgery for labral tears of the hip can include labral debridement, repair, or reconstruction.29 Average return to play time is 7.4 months after labrum repairs, with 66.7-84% of recreational athletes being able to return to sport.30 While the subject in this report did not have FAI (femoral acetabular impingement) that caused the labrum tear, it is a common concurrent pathology. Surgical intervention for individuals with FAI requires bone excision during arthroscopy to address the labrum.31
The subject in this report declined surgical intervention and after five months of self-prescribed exercises with an additional 12 weeks of physical therapy she was able to fully return to sport. Though she took longer to fully recover than was recommend by the British Hernia Society, she was making gradual improvements in her report of pain and return to function by the fifth week of physical therapy.
There are limitations specific to this case report. Ideally, on examination, a thigh thrust test9 or the six provocation tests, as described by Laslett, et al,32 should have been used to rule-out sacroiliac joint involvement and a FADIR to implicate the intra-articular hip joint dysfunction.1. An MRI, in isolation, should not be used for a diagnosis as a pathology noted in imaging may not be symptomatic.33 In addition, it would have been ideal to follow the terminology and test criteria set forth by the Doha agreement to isolate what structures contributed to the athletic pubalgia.34. As a single case report, the information is not generalizable and causality cannot be inferred.
CONCLUSIONS
This case report describes the use of gait retraining and stability training of the hip and lumbopelvic complex in a 45-year-old female with a medical diagnosis of athletic pubalgia and hip labral pathology. The subject avoided surgery and returned to running after 12 weeks of physical therapy and reported no functional limitations at a one-year follow-up. It would be beneficial to expand on this research to examine patterns of gait abnormalities in female runners with athletic pubalgia and/or hip labral tears and develop randomized controlled trials to determine best care based on examination findings. Since this case report was completed, King et al8 have published research suggesting the importance of the functional retraining similar to what was utilized herein.
REFERENCES
- 1.Hegedus EJ Stern B Reiman MP, et al. A suggested model for physical examination and conservative treatment of athletic pubalgia. Phys Ther Sport. 2013;14(1):3-16. [DOI] [PubMed] [Google Scholar]
- 2.Kachingwe AF Grech S. Proposed algorithm for the management of athletes with athletic pubalgia (sports hernia): A case series. J Orthop Sports Phys Ther. 2008;38(12):768-781. [DOI] [PubMed] [Google Scholar]
- 3.Elattar O Choi H Dills VD, et al. Groin injuries (athletic pubalgia) and return to play. Sports Health. 2016;8(4):313-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ellsworth AA Zoland MP Tyler TF. Athletic pubalgia and associated rehabilitation. Int J Sports Phys Ther. 2014;9(6):774-784. [PMC free article] [PubMed] [Google Scholar]
- 5.Oliveira ALd Andreoli CV Ejnisman B, et al. Epidemiological profile of patients diagnosed with athletic pubalgia. Rev Bras Ortop. 2016;51(6):692-696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hölmich P. Long-standing groin pain in sports people falls into three primary patterns, a “clinical entity” approach: A prospective study of 207 patients. Br J Sports Med. 2007;41(4):247-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheen AJ Stephenson BM Lloyd DM, et al. ‘Treatment of the sportsman's groin: British hernia society's 2014 position statement based on the Manchester consensus conference. Br J Sports Med. 2014;48(14):1079-1087. [DOI] [PubMed] [Google Scholar]
- 8.King E Franklyn-Miller A Richter C, et al. Clinical and biomechanical outcomes of rehabilitation targeting intersegmental control in athletic groin pain: Prospective cohort of 205 patients. Br J Sports Med. 2018;52(16):1054-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thorborg K Reiman MP Weir A, et al. Clinical examination, diagnostic imaging, and testing of athletes with groin pain: An evidence-based approach to effective management. J Orthop Sports Phys Ther. 2018;48(4):239-249. [DOI] [PubMed] [Google Scholar]
- 10.Kajetanek C Benoît O Granger B, et al. Athletic pubalgia: Return to play after targeted surgery. Orthop Traumatol Surg Res. 2018;104(4):469-472. [DOI] [PubMed] [Google Scholar]
- 11.Litwin DEM Sneider EB McEnaney PM, et al. Athletic pubalgia (sports hernia). Clin Sports Med. 2011;30(2):417-434. [DOI] [PubMed] [Google Scholar]
- 12.Kibler WB Press J Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36(3):189-198. [DOI] [PubMed] [Google Scholar]
- 13.Souza RB. An evidence-based videotaped running biomechanics analysis. Phys Med Rehabil Clin N Am. 2016;27(1):217-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pipkin A Kotecki K Hetzel S, et al. Reliability of a qualitative video analysis for running. J Orthop Sports Phys Ther. 2016;46(7):556-561. [DOI] [PubMed] [Google Scholar]
- 15.Kendall FP. Muscles: Testing and function with posture and pain. 5th ed. Baltimore: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 16.SFMA LLC. SFMA Seminar Manual 2011.
- 17.Binkley JM Stratford PW Lott SA, et al. The lower extremity functional scale (LEFS): Scale development, measurement properties, and clinical application. Phys Ther. 1999;79(4):371-383. [PubMed] [Google Scholar]
- 18.Hengeveld E Banks K, eds. Maitland's Peripheral Manipulation. 5th ed. Edinburgh: Churchill Livingstone; 2014. [Google Scholar]
- 19.Augustsson J Esko A Thomeé R Svantesson U. Weight training of the thigh muscles using closed versus open kinetic chain exercises: A comparison of performance enhancement. J Orthop Sports Phys Ther. 1998;27(1):3-8. [DOI] [PubMed] [Google Scholar]
- 20.Folland JP Williams AG. Morphological and neurological contributions to increased strength. Sports Med. 2007;37(2):145-168. [DOI] [PubMed] [Google Scholar]
- 21.Kraemer JW Ratamess AN. Fundamentals of resistance training: Progression and exercise prescription. Med Sci Sports Exerc. 2004;36(4):674-688. [DOI] [PubMed] [Google Scholar]
- 22.Cowan SM Schache AG Brukner P, et al. Delayed onset of transversus abdominus in long-standing groin pain. Med Sci Sports Exerc. 2004;36(12):2040-2045. [DOI] [PubMed] [Google Scholar]
- 23.Brumitt J Matheson JW Meira EP. Core stabilization exercise prescription, part I: Current concepts in assessment and intervention. Sports Health. 2013;5(6):504-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heiderscheit BC Chumanov ES Michalski MP, et al. Effects of step rate manipulation on joint mechanics during running. Med Sci Sports Exerc. 2011;43(2):296-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chesterton P Payton S McLaren S. Acute effects of centrally- and unilaterally-applied posterior-anterior mobilizations of the lumbar spine on lumbar range of motion, hamstring extensibility and muscle activation. J Back Musculoskelet Rehabil. 2018;31(6):1013-1023. [DOI] [PubMed] [Google Scholar]
- 26.Kojidi MM Okhovatian F Rahimi A, et al. Comparison between the effects of passive and active soft tissue therapies on latent trigger points of upper trapezius muscle in women: Single-blind, randomized clinical trial. J Chiropr Med. 2016;15(4):235–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heiderscheit B McClinton S. Evaluation and management of hip and pelvis injuries. Phys Med Rehabil Clin N Am. 2016;27(1):1-29. [DOI] [PubMed] [Google Scholar]
- 28.Schubert AG Kempf J Heiderscheit BC. Influence of stride frequency and length on running mechanics: A systematic review. Sports health. 2014;6(3):210-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Westermann RW Day MA Duchman KR Glass NA Lynch TS Rosneck JT. Trends in hip arthroscopic labral repair: An American board of orthopaedic surgery database study. Arthroscopy. 2019;35(5):1413-1419. [DOI] [PubMed] [Google Scholar]
- 30.O’connor M Minkara AA Westermann RW Rosneck J Lynch TS. Return to play after hip arthroscopy: A systematic review and meta-analysis. Am J Sports Med. 2018;46(11):2780-2788. [DOI] [PubMed] [Google Scholar]
- 31.Palmer AJR Ayyar Gupta V Fernquest S, et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: Multicentre randomised controlled trial. BMJ. 2019;364:l185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laslett M Aprill CN McDonald B, et al. Diagnosis of sacroiliac joint pain: Validity of individual provocation tests and composites of tests. Man Ther. 2005;10(3):207-218. Márquez WH, Gómez-Hoyos J, Gallo JA, et al. Prevalence of labrum and articular cartilage injuries of the hip on 3T magnetic resonance imaging of asymptomatic elite soccer players. Revista española de cirugía ortopédica y traumatología. 2019;63(2):77-85.16038856 [Google Scholar]
- 33.Weir A Brukner P Delahunt E, et al. Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med. 2015;49(12):768-774. [DOI] [PMC free article] [PubMed] [Google Scholar]