Abstract
Background:
Sports rehabilitation professionals often prescribe unstable objects for balance training. Unfortunately, there is a lack of measurement of balance confidence when incorporating these objects. Currently, there is no consensus on the optimal balance confidence measure or proposed progression of unstable objects. Understanding the influence of balance confidence on task performance using unstable objects may help professionals better prescribe a balance training program.
Purpose:
The primary purpose of this investigation was to explore the correlation between anticipated and actual balance confidence on different unstable objects during static double leg and single leg stance. The secondary purpose was to explore the correlation between anticipated and actual unstable object difficulty rankings.
Study Design:
Repeated measure observational, controlled trial.
Methods:
Sixty-five active, healthy adults (M = 35, F = 30) (mean age = 24.38 ± 3.56) underwent two testing sessions. During session one, participants took an online survey, rating their anticipated balance confidence after observing images of different unstable objects. During session two, participants stood on each unstable object under two conditions (static double leg stance and single leg stance) and rated their actual balance confidence. The main outcome measure was an ordinal balance confidence score adapted from the activities-specific balance confidence scale. Statistical analysis included subject demographic calculations and appropriate non-parametric tests.
Results:
For the double leg stance and single leg stance conditions, there was a very strong correlation between anticipated and actual balance confidence scores on the stable surface (ρ = 1.0, p = <.001). There was a weak correlation between scores for foam pad, air-filled discs, Bosu® (dome up), Bosu® (dome down), and wobble board for both conditions. For unstable object rankings, there was a very strong correlation between scores (ρ=1.0, p = <.001). The objects were ranked by perceived difficulty as follows: Level 1 (easy)- ground, Level 2- foam pad, Level 3- air-filled discs, Level 4- Bosu®, and Level 5 (difficult)- wobble board.
Conclusion:
Study findings suggest that actual measures of balance confidence may provide insight into a patient's confidence level and may help with prescribing and progressing their program. The suggested unstable object difficulty rankings may help professionals better match the objects to their patients to produce optimal outcomes.
Level of Evidence:
2c
Keywords: Balance, fall, motor control, proprioception, risk
INTRODUCTION
Balance training is a common intervention used during sports rehabilitation. Athletes or active individuals with musculoskeletal injury or concussion may undergo balance rehabilitation or an injury prevention program to improve their balance performance, postural control, and balance confidence.1,2,3 For lower extremity rehabilitation and injury prevention, unstable objects are often incorporated into balance training programs.4,5 Common unstable objects used include the Bosu® ball, air-filled discs, foam pads, and wobble boards.6 These objects are meant to create an unstable condition that challenges the individual's balance systems (visual, vestibular, somatosensory) during static and dynamic tasks and under different conditions (e.g. double and single leg stance).6,7
Several authors have examined the effects of progressive balance programs that were based upon task performance (e.g. advance when proficient at exercise) for injured and active healthy individuals.1,8,9,10 Evidence suggests that the level of difficulty (instability) of the unstable object is not indicative of balance improvements; thus, individuals may demonstrate improvements on different unstable objects.11,12 While task performance is a good clinical marker for progression, these studies did not consider the influence of an individual's balance confidence when using the different unstable objects. Low balance confidence can be a barrier to an individual's balance performance when the unstable object becomes more difficult.11,12
Balance confidence (i.e., perceived postural stability) can be anticipated or actual (during the task).13 Balance confidence has been a popular measure among community-dwelling older adults14 and older adults with medical conditions.15,16,17,18,19,20 There are several validated patient outcomes that use anticipated situational questions designed for older adults (e.g. walking up and down stairs). These types of questions may not capture the actual confidence level of the individual during the task. Individuals may answer questions based upon prior experience or estimated performance if they have not recently performed the activity.13 A lack of balance confidence is a high predictor of falls among older individuals.13 Furthermore, these outcomes may have a ceiling effect with active, younger adults since most can successfully perform the tasks presented in the questions.21,22
Rehabilitation professionals may progress individuals on unstable objects according to their own preferred methods or the patient's physical performance without addressing balance confidence. Currently, there is no universal consensus on the optimal progression of unstable objects for younger active, healthy adults and injured patients.23 Considering the influence of balance confidence on a patient's performance during their balance or injury prevention program is a novel concept to consider. To date, there are no investigations that have examined this topic. Most studies of this population have focused on return to play confidence or psychological readiness among individuals returning from lower extremity injuries.24,25 Addressing balance confidence during a training program may improve an individual's return to play confidence and provide insight into the appropriate programming progressions.
The first step in understanding the influences of balance confidence is to explore the correlation between anticipated and actual balance confidence and determine the best method to measure this construct. For example, an injured individual may demonstrate low balance confidence right before trying an unstable object (anticipated) but may gain higher confidence after they successfully perform a task on the object (actual). The rehabilitation professional may benefit from knowing which method is best for measuring balance confidence and from being able to rank the unstable objects based upon the patient's confidence level. The primary purpose of this investigation was to explore the correlation between anticipated and actual balance confidence on unstable objects during static double leg and single leg stance. The secondary purpose was to explore the correlation between anticipated and actual unstable object difficulty rankings.
METHODS
Subjects
Sixty-five young, active, healthy adults (M=35, F=30) (leg dominance: right = 57, left = 7) (mean age 24.38 ± 3.56 years) were recruited via convenience sampling (e.g., flyers). Recruited subjects reported participating in weekly recreational fitness activities (e.g. walking)26 and being familiar with common unstable objects. All participants reported using some type of unstable object as part of their fitness activities within the past 18 months of this study. Exclusion criteria included the presence of any musculoskeletal, neurologic, systemic, or metabolic disease that would affect balance or lower extremity function; the inability to avoid medications that may affect testing; or any other potential issue or factor that would prevent participation. This investigation was approved by the Institutional Review Board (IRB) at California State University Dominguez Hills (IRB # 19-143).
Procedures
Two investigators collected data for this investigation. Prior to data collection, a two-session pilot training was conducted to ensure consistency among the investigators. The primary investigator is a doctoral level physical therapist with over 13 years of experience and board certified in orthopedics. The second investigator is a doctoral level kinesiology researcher.
For data collection, all eligible participants signed the IRB-approved consent form before testing. All participants underwent two sessions of testing and were blinded from the results and other participants enrolled in the study. For Session 1 (anticipated), participants completed an online survey where they were shown pictures of unstable objects and then rated their anticipated balance confidence for each object. They then ranked the ground and unstable objects from easy to most difficult. All participants completed the survey and then underwent a 5 day “wash out” period of no testing. Participants then completed testing in Session 2 (actual) by rating their balance confidence while standing on the ground and unstable objects.
Session 1: Anticipated
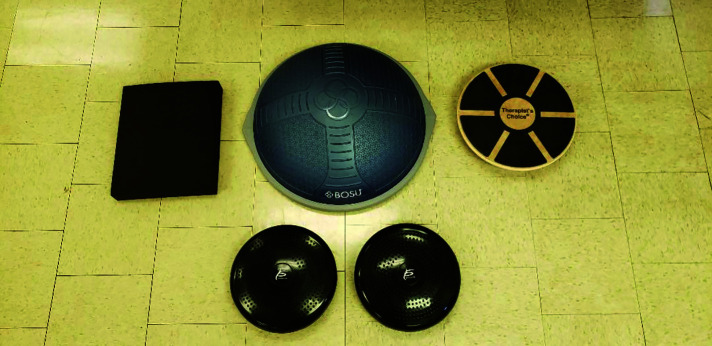
For Session 1, a 20-item online survey (SurveyMonkey® www.surveymonkey.com) included questions on participant demographics and questions related to five standing conditions: on a flat stable surface (floor of research lab: “ground”) and four different unstable objects (a foam pad, air-filled discs, Bosu®, and wobble board) (Figure 1). The survey was preset to randomize questions for each participant.
Figure 1.
Unstable objects used within the study.
After seeing a picture of each object, participants rated their predicted balance confidence (for each surface/object and stance condition) during double leg stance and single leg stance.27 Balance confidence was assessed using a numeric self-reported balance confidence score ranging from 0 to 100 scale (0-no confidence, 100-high confidence) (Figure 2). The numeric rating scale was adapted from the ordinal scale used in the Activities-specific Balance Confidence scale (ABC) questionnaire.27 The ABC is one of several validated patient outcomes that use situational questions designed for older adults.13 Ordinal type scales are reliable and valid outcomes commonly used to measure pain28,29,30 or other patient characteristics such as satisfaction rating or education level.31 The balance confidence score provides the professional with a simple numeric rating (e.g. 10, 20, ..100) of the individual's balance confidence before or during a task while standing on an unstable object. For the last question of the survey, participants ranked the difficulty level of the stable surface and each object from level 1 (“easy”) to level 5 (“difficult”) after completing each data collection session.
Figure 2.
Balance confidence score.
Session 2: Actual
For Session 2 (actual), participants were tested in the kinesiology laboratory using the same conditions on the ground and unstable objects they responded to in Session 1. Testing was conducted between the hours of 10 A.M. and 2 P.M.; participants were instructed to refrain from any strenuous activity for three hours prior to testing and from taking any medication that would interfere with testing. Participants wore comfortable clothing and athletic shoes during testing. Prior to data collection, the investigator reviewed the testing protocol with each participant and answered any questions. There were no practice trials conducted. For testing, the participants first stood on the ground and then on each of the four objects under the two static conditions: double and single leg stance. For double leg stance, participants stood with feet 12 inches apart and arms at their sides. For single leg stance, participants stood on their dominant leg (e.g. kicking leg) in a standard position with arms at their sides.32 Participants were not asked to focus their vision on any location but were asked to refrain from talking during testing. Participants completed one trial of each condition for the ground and four objects. Each condition lasted a total of 30 seconds in order to allow the participant to adjust to the unstable object.33,34 There was a 30-second rest period between conditions. The investigator was in immediate proximity to assist the participant if they lost their balance. If a loss of balance occurred, the participant could touch down the opposite lower extremity or reach out to the examiner for support. The examiner stopped the timer and immediately assisted participants until they regained their balance on the object. Testing resumed until 30 seconds was complete for each condition. Immediately following testing, participants rated their balance confidence for each condition; participants then ranked the ground and unstable objects from easy to most difficult. The unstable objects and conditions were randomized for each participant's testing session.
Statistical Analysis
Statistical analysis was performed using SPSS version 25.0 (IBM SPSS, Armonk, New York, USA). Subject descriptive data was calculated and reported as the mean and standard deviation (SD) for age, height, body mass, and body mass index (BMI). The correlation between Session 1 and Session 2 balance confidence scores and ranking of objects were calculated using the Spearman Rank correlation coefficient (95% confidence interval).35 The criteria for evaluating the correlation coefficient was as follows: 0.00-0.10 = negligible correlation; 0.10-0.39 = weak correlation; .40-.69 = moderate correlation; 0.70-0.89 = Strong correlation; and 0.90-1.00 = very strong correlation. Statistical significance was established at p<.05 for all measures.36
RESULTS
Sixty-five participants completed the study (Table 1). There were no adverse events or participant attrition during data collection.
Table 1.
Subject demographics (N=65).
| Characteristics | Age (years) | Height (cm) | Body Mass (kg) | BMI (kg/m2) |
|---|---|---|---|---|
| Subjects (N=65) (M=35, F=30) | 24.38 ± 3.56 (20-39) | 167.37 ± 9.60 (150-183) | 73.69 ± 16.16 (42-125) | 26.14 ± 4.55 (17-41) |
Data reported as mean ± SD; range (min-max); m=meters; BMI = body mass index; kg/m2 = kilograms-meter squared
Balance confidence scores: anticipated and actual
The relationship between both anticipated (Session 1) and actual (Session 2) balance confidence scores for the ground and unstable objects were calculated for the static double leg and single leg stance conditions. For double leg stance, there was a very strong correlation between anticipated and actual scores for standing on the ground (ρ=1.0, p = <.001). There was a weak correlation between scores for the foam pad (ρ=0.12, p = 0.34), air-filled discs (ρ=0.20, p = 0.11), Bosu® (dome up) (ρ=0.15, p = 0.23), Bosu® (dome down) (ρ=0.13, p = 0.30), and wobble board (ρ=0.20, p = 0.10) (Table 2).
Table 2.
Double leg stance: relationship among BCS scores (Session 1 and Session 2).
| Unstable Objects | Spearman rho (ρ) | 95% CI | p-value |
|---|---|---|---|
| Ground | 1.0 | - | *<.001 |
| Foam pad | 0.12 | 0.08-0.29 | 0.34 |
| Air-filled discs | 0.20 | 0.05-0.43 | 0.11 |
| Bosu® (dome up) | 0.15 | 0.10-0.38 | 0.23 |
| Bosu® (dome down) | 0.13 | 0.11-0.36 | 0.30 |
| Wobble board | 0.20 | 0.03-0.43 | 0.10 |
*IR: inter BCS = balance confidence score; *p-value significant at p<0.05
For single leg stance, there was a very strong correlation between anticipated and actual scores for standing on the ground (ρ=1.0, p = <.001). There was a weak correlation between scores for the foam pad (ρ=0.08, p = 0.54), air-filled discs (ρ=0.16, p = 0.21), Bosu® (dome up) (ρ=0.20, p = 0.11), Bosu® (dome down) (ρ=0.14, p = 0.27), and wobble board (ρ=0.15, p = 0.23) (Table 3).
Table 3.
Single leg stance: relationship among BCS Scores (Session 1 and Session 2).
| Unstable Object | Spearman rho (ρ) | 95% CI | p-value |
|---|---|---|---|
| Ground | 1.0 | - | *<.001 |
| Foam pad | 0.08 | 0.07-0.31 | 0.54 |
| Air-filled discs | 0.16 | 0.09-0.39 | 0.21 |
| Bosu® (dome up) | 0.20 | 0.05-0.41 | 0.11 |
| Bosu® (dome down) | 0.14 | 0.11-0.37 | 0.27 |
| Wobble board | 0.15 | 0.10-0.38 | 0.23 |
*IR: inter NPRS = numeric pain rating scale; *p-value significant at p<0.05
Difficulty ranking of objects
Upon completion of both sessions, participants ranked the unstable objects for easiest to hardest. Statistical analysis revealed an excellent relationship between both sessions for the unstable object rankings (ρ=1.0, p = <.001). The object rankings were based on the conditions with the highest agreement among participants for both sessions. The rankings were: level 1 (easy)- ground, level 2- foam pad, level 3- air-filled discs, level 4- Bosu®, and level 5 (difficult)- wobble board (Table 4).
Table 4.
Unstable object rankings of difficulty.
| Unstable Object (Difficulty Level) | Ground | Foam pad | Air-filled discs | Bosu® | Wobble Board |
|---|---|---|---|---|---|
| Level 5-Difficult | 5% (N=3) | 23% (N=15) | 72% (N=47) | ||
| Level 4 | 25% (N=16) | 52% (N=34) | 23% (N=15) | ||
| Level 3 | 70% (N=46) | 25% (N=16) | 5% (n=3) | ||
| Level 2 | 100% (N=65) | ||||
| Level 1-Easy | 100% (N=65) |
DISCUSSION
Sports rehabilitation professionals utilize unstable objects as part of a progressive balance program for injury rehabilitation and prevention. Professionals may prescribe a progressive balance program based on their preferred method without considering the influence of balance confidence. Low balance confidence can be a barrier to an individual's performance when the unstable object becomes more difficult.11,12 Balance confidence scales typically measure the anticipated balance confidence and do not capture the actual confidence level of the individual during the task.13 Rehabilitation professionals should consider measuring actual balance confidence while patients perform tasks on unstable objects.
Balance confidence scores: anticipated versus actual
This study measured the relationship between anticipated and actual balance confidence scores for stable and unstable surfaces. For standing on ground, there was a very strong correlation between anticipated and actual scores for both the double leg and single leg stance conditions (ρ=1.0, p = <.001). This suggests that individuals may feel confident when anticipating and when standing on the ground during both conditions. There was a weak correlation within the four unstable objects (ρ=0.08-0.20, p = 0.10-0.54) for both the double leg stance and single leg stance conditions. This suggests that individuals may not accurately anticipate their balance confidence. This can be a safety concern for patients with a pre-existing injury or poor balance who want to use an unstable object but may not have the physical abilities to do so safely. Similar situations have been reported in the fitness setting where individuals experience injuries from overexertion and improper use of equipment which may be from an inaccurate estimation of confidence.37,38
Based on the results of this study, rehabilitation professionals should have their patients perform a task on an unstable object and immediately rate their confidence while under direct supervision to ensure safety. Anticipated balance confidence may provide an inaccurate level of actual balance performance for certain patients. The ordinal balance confidence score may offer a simple method of documenting and tracking a patient's confidence before and during a standing task on an unstable object. Balance confidence may be the best determinant of patient performance and may help to build the patient's return to activity confidence. This is especially important with individuals recovering from musculoskeletal injury since they may already demonstrate low confidence with challenging activities due to fear of reinjury.11,12 This can also apply to active individuals who are using these objects for the first time.
Difficulty ranking for objects
A secondary analysis provided insight into individual perceptions about the difficulty of specific unstable objects under static standing conditions (double and single leg). This analysis identified an excellent relationship between both anticipated and actual sessions with the object difficulty rankings. Participants did not change their perception of the difficulty level of the unstable objects after completing both sessions. Subjective difficulty rankings from patients may help provide insight into their current perceptions about using specific unstable objects. However, not every patient may follow a standard progressive program due to their unique needs, physical abilities, balance confidence, and program goals.
Limitations
This investigation was considered exploratory. There are specific limitations to this investigation. First, this investigation tested young, active, healthy adults which limits the study generalizability. Second, the ABC questionnaire and adapted numeric rating scale have not been validated in healthy, young adults. Third, the unstable objects used in this study may not represent all the balance devices available in the rehabilitation setting. Different objects may have produced different outcomes among participants. Nevertheless, the study design was based on using objects that would not have a global floor or ceiling effect among the participants. Third, while the anticipated and actual balance confidence score and object rankings were studied, the interaction between balance confidence and task performance on each of the unstable objects was not studied. Fourth, this study only examined balance confidence using static double and single leg stance. Dynamic movements on the stable surface and unstable objects may have produced different outcomes among participants.
Clinical Relevance and Future Research
Considering the influence of balance confidence during injury rehabilitation, prevention, and performance programs using unstable objects is a novel concept. Sports rehabilitation professionals should consider measuring actual balance confidence prior to initiating balance exercises. An ordinal balance confidence score may provide an easy method of documenting a tracking a patient's progress as they use different objects under different conditions (e.g. static double or single leg stance).
Future research should explore the validity and reliability of the ordinal balance confidence score with different patient populations using unstable objects. Actual balance confidence during dynamic movements on unstable objects should also be studied since this investigation only measured static conditions. Future research should also explore the correlation between actual balance confidence, task performance, and return to play confidence among younger, active adults with different musculoskeletal injuries and concussions.
CONCLUSION
This was the first investigation to explore the relationship of balance confidence and unstable objects under different static conditions. A very strong correlation was found between anticipated and actual confidence on level ground for double and single limb stance in healthy adults; however, a weak correlation was found between anticipated versus actual confidence for the unstable object conditions. This novel topic should be considered by sports rehabilitation professionals when prescribing a balance program using these objects for different patients. An ordinal balance confidence score may offer an easy way to document and track a patient's progress with different objects. Measuring a patient's balance confidence may help rehabilitation professionals better prescribe and progress their balance training program.
REFERENCES
- 1.Brachman A Kamieniarz A Michalska J, et al. Balance training programs in athletes - a systematic review. J Human Kin. 2017;58:45-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Faizullin I Faizullina E. Effects of balance training on post-sprained ankle joint instability. Int J Risk Saf Med. 2015;27 Suppl 1:S99-s101. [DOI] [PubMed] [Google Scholar]
- 3.Wortmann MA Docherty CL. Effect of balance training on postural stability in subjects with chronic ankle instability. J Sport Rehabil. 2013;22(2):143-149. [DOI] [PubMed] [Google Scholar]
- 4.Paszkewicz J Webb T Waters B, et al. The effectiveness of injury-prevention programs in reducing the incidence of anterior cruciate ligament sprains in adolescent athletes. J Sport Rehabil. 2012;21(4):371-377. [DOI] [PubMed] [Google Scholar]
- 5.Noyes FR Barber-Westin SD. Neuromuscular retraining intervention programs: do they reduce noncontact anterior cruciate ligament injury rates in adolescent female athletes? Arthroscopy. 2014;30(2):245-255. [DOI] [PubMed] [Google Scholar]
- 6.Zemkova E. Instability resistance training for health and performance. J Tradit Complement Med. 2017;7(2):245-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lubetzky-Vilnai A McCoy SW Price R, et al. Young adults largely depend on vision for postural control when standing on a bosu ball but not on foam. J Strength Cond Res. 2015;29(10):2907-2918. [DOI] [PubMed] [Google Scholar]
- 8.Cug M Duncan A Wikstrom E. Comparative effects of different balance-training-progression styles on postural control and ankle force production: a randomized controlled trial. J Athl Train. 2016;51(2):101-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zech A Hubscher M Vogt L, et al. Balance training for neuromuscular control and performance enhancement: a systematic review. J Athl Train. 2010;45(4):392-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heleno LR, da Silva RA Shigaki L, et al. Five-week sensory motor training program improves functional performance and postural control in young male soccer players - A blind randomized clinical trial. Phys Ther Sport. 2016;22:74-80. [DOI] [PubMed] [Google Scholar]
- 11.Norris BS Medley A. The effect of balance confidence and context on functional reach ability in healthy older adults. Phys Med Rehabil. 2011;3(9):811-816. [DOI] [PubMed] [Google Scholar]
- 12.Blasco JM Tolsada C Beltran M, et al. Instability training, assessing the impact of level of difficulty on balance: A randomized clinical trial. Gait Posture. 2019;70:116-121. [DOI] [PubMed] [Google Scholar]
- 13.Landers MR Oscar S Sasaoka J, et al. Balance confidence and fear of falling avoidance behavior are most predictive of falling in older adults: prospective analysis. Phys Ther. 2016;96(4):433-442. [DOI] [PubMed] [Google Scholar]
- 14.Myers AM Powell LE Maki BE, et al. Psychological indicators of balance confidence: relationship to actual and perceived abilities. J Gerontol A Biol Sci Med Sci. 1996;51(1):M37-43. [DOI] [PubMed] [Google Scholar]
- 15.Nilsagard Y Carling A Forsberg A. Activities-specific balance confidence in people with multiple sclerosis. Mult Scler Int. 2012;2012:613925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee HK Altmann LJ McFarland N, et al. The relationship between balance confidence and control in individuals with parkinson's disease. Parkinsonism Relat Disord. 2016;26:24-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schinkel-Ivy A Wong JS Mansfield A. Balance Confidence Is Related to Features of Balance and Gait in Individuals with Chronic Stroke. J Stroke Cerebrovasc Dis. 2017;26(2):237-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schinkel-Ivy A Inness EL Mansfield A. Relationships between fear of falling, balance confidence, and control of balance, gait, and reactive stepping in individuals with sub-acute stroke. Gait Posture. 2016;43:154-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sihvonen S Kulmala J Kallinen M, et al. Postural balance and self-reported balance confidence in older adults with a hip fracture history. Gerontology. 2009;55(6):630-636. [DOI] [PubMed] [Google Scholar]
- 20.Stubbs B Schofield P Patchay S, et al. Musculoskeletal pain characteristics associated with lower balance confidence in community-dwelling older adults. Physiotherapy. 2016;102(2):152-158. [DOI] [PubMed] [Google Scholar]
- 21.Lajoie Y Gallagher SP. Predicting falls within the elderly community: comparison of postural sway, reaction time, the Berg balance scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch Gerontol Geriatr. 2004;38(1):11-26. [DOI] [PubMed] [Google Scholar]
- 22.Huang TT Wang WS. Comparison of three established measures of fear of falling in community-dwelling older adults: psychometric testing. Int J Nurs Stud. 2009;46(10):1313-1319. [DOI] [PubMed] [Google Scholar]
- 23.Klatt BN Carender WJ Lin CC, et al. A Conceptual framework for the progression of balance exercises in persons with balance and vestibular disorders. Phys Med Rehabil Int. 2015;2(4):1044. [PMC free article] [PubMed] [Google Scholar]
- 24.Kaplan Y Witvrouw E. When is it safe to return to sport after acl reconstruction? reviewing the criteria. Sports Health. 2019;11(4):301-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Corbett RO Keith TR Hertel J. Patient-reported outcomes and perceived confidence measures in athletes with a history of ankle sprain. J Sport Rehabil. 2019:1-6. [DOI] [PubMed] [Google Scholar]
- 26.Garber CE Blissmer B Deschenes MR et al. American college of sports medicine position stand. quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334-1359. [DOI] [PubMed] [Google Scholar]
- 27.Schepens S Goldberg A Wallace M. The short version of the activities-specific balance confidence (abc) scale: its validity, reliability, and relationship to balance impairment and falls in older adults. Arch Gerontol Geriatr. 2010;51(1):9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferraz MB Quaresma MR Aquino LR, et al. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol. 1990;17(8):1022-1024. [PubMed] [Google Scholar]
- 29.Hawker GA Mian S Kendzerska T, et al. Measures of adult pain: visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res. 2011;63 Suppl 11:S240-252. [DOI] [PubMed] [Google Scholar]
- 30.Bigatti SM Cronan TA. A comparison of pain measures used with patients with fibromyalgia. J Nurs Meas. 2002;10(1):5-14. [DOI] [PubMed] [Google Scholar]
- 31.Marateb HR Mansourian M Adibi P, et al. Manipulating measurement scales in medical statistical analysis and data mining: a review of methodologies. J Res Med Sci. 2014;19(1):47-56. [PMC free article] [PubMed] [Google Scholar]
- 32.Springer BA Marin R Cyhan T, et al. Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther. 2007;30(1):8-15. [DOI] [PubMed] [Google Scholar]
- 33.• • •
- 34.Vereeck L Wuyts F Truijen S, et al. Clinical assessment of balance: normative data, and gender and age effects. Int J Audiol. 2008;47(2):67-75. [DOI] [PubMed] [Google Scholar]
- 35.Weaver B Koopman R. An SPSS Macro to Compute Confidence Intervals for Pearson's Correlation. Quantit Methods Psych. 2014;10:29-39. [Google Scholar]
- 36.Schober P Boer C Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126(5):1763-1768. [DOI] [PubMed] [Google Scholar]
- 37.Gray SE Finch CF. The causes of injuries sustained at fitness facilities presenting to Victorian emergency departments - identifying the main culprits. Injury Epidemiol. 2015;2(1):6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gray SE Finch CF. Epidemiology of hospital-treated injuries sustained by fitness participants. Res Q Exerc Sport. 2015;86(1):81-87. [DOI] [PubMed] [Google Scholar]