Abstract
Background:
Several systematic reviews have evaluated the role of dual-task assessment in individuals with concussion. However, no systematic reviews to date have investigated dual-task protocols with implications for individuals with anterior cruciate ligament (ACL) injury or ACL reconstruction (ACLR).
Purpose:
To systematically review the evidence on dual-task assessment practices applicable to those with ACL deficiency/ACLR, specifically with the aim to identify motor-cognitive performance costs.
Study Design:
Systematic review
Methods:
A systematic literature review was undertaken on those with ACL-deficient or ACL-reconstructed knees performing dual-task activities. The following databases were searched from inception to June 8, 2018 including CINAHL, PsychInfo, PubMed, SPORTDiscus, Web of Science, and gray literature. Three primary search categories (knee, cognition, and motor task) were included. Only one reviewer independently performed the database search, data extraction, and scored each article for quality. All studies were assessed for quality and pertinent data were extracted, examined and synthesized.
Results:
Ten studies were included for analysis, all of which were published within the prior ten years. Performance deficits were identified in those with either ACL deficiency or ACLR while dual-tasking, such as prioritization of postural control at the expense of cognitive performance, impaired postural control in single limb stance, greater number of cognitive errors, and increased step width coefficient of variation while walking. No studies examined those with prior ACL injury or ACLR during tasks that mimicked ACL injury mechanisms such as jump-landing or single-leg cutting.
Conclusion:
The results of the current systematic review suggests that postural control, gait, and/or cognitive deficits exist when evaluated under a dual-task paradigm in those with ACL deficiency or ACLR. This systematic review highlights the need for future research on dual-task assessment for individuals who have sustained an ACL injury or undergone ACLR, specifically utilizing more difficult athletic movements.
Level of Evidence:
Level 3a
Keywords: ACL, cognition, dual-task, knee
INTRODUCTION
Approximately 8.6 million sports- and recreation-related injuries have occurred annually in the United States from 2011-2014, 42% of which involved the lower extremity (LE) for those over age five.1 In addition, anterior cruciate ligament (ACL) injuries are frequently encountered in athletic populations.2,3 Despite the high prevalence of ACL injuries, ACL reconstruction (ACLR) has less than desirable clinical outcomes. For example, a high percentage of athletes experience a second ACL injury after being cleared to return to sport,4 as well as failure to return to sports at their pre-injury level.5-7
Athletes tend to sustain ACL injuries when attending to a secondary task or object.8-10 Researchers and clinicians have attempted to account for the physical and cognitive demands of the real-world athletic environment when evaluating LE mechanics during drop vertical jump11-13 and single-leg cutting tasks14-17 under divided attention conditions. While this has not been investigated in a population who have sustained an ACL injury, two systematic reviews have examined knee mechanics in response to anticipation during single-leg cutting tasks in healthy individuals, indicating that suboptimal movement strategies ensue when pre-planning is not allowed.18,19 The role of anticipation, although relevant to athletic participation, should not be confused with the dual-task paradigm.
The dual-task paradigm involves the simultaneous performance of two tasks that can be performed and measured separately.20 One type of dual-tasking includes motor and cognitive task assessment. If attentional resources devoted to either task are diminished, a performance deficit may emerge in one or both tasks under dual-task conditions. This concept has been demonstrated in ACL-deficient soccer athletes who had a greater number of cognitive errors while in single- (SLS) and double-limb stance (DLS) when compared to a healthy control group, yet postural sway indices lacked a consistent directional response across both stance conditions.21 It has also been shown that a posture-first strategy is adopted by athletes with ACLR under dual-task conditions at the expense of increased reaction time and error ratios while completing an auditory Stroop task.22 Individuals with ACLR have demonstrated decreased SLS postural control under dual- versus single task conditions, yet no differences in cognitive performance were identified between groups.23 Therefore, physical and/or cognitive deficits may emerge under dual-task conditions in ACL-injured populations when compared to healthy individuals.
The cognitive changes that exist among clinical populations with LE injuries may underscore the importance of dual-task assessment. Functional magnetic resonance imaging identified altered sensorimotor cortical activation among those with ACL insufficiency at least six months post-injury when compared to healthy individuals.24 Neuroplastic changes that may persist for months to years after surgery and return to sport25,26 were identified during a simple motor task including joint motion (knee flexion/extension) for those with ACLR. Further, neurocognitive deficiencies in reaction time and visual processing speed have been shown to be predictive of future ACL injury in intercollegiate athletes.27
The data supporting an association between cognition and musculoskeletal injury, as well as the promising literature for dual-task assessment in those with concussion,28-31 suggests the need to examine the evidence for dual-task assessment in individuals who have sustained ACL injuries. Therefore, the purpose was to systematically review the evidence on dual-task assessment practices applicable to those with ACL deficiency/ACLR, specifically with the aim to identify motor-cognitive performance costs.
METHODS
Search Strategy
Only one reviewer independently performed the database search, data extraction, and scored each article for quality. The following databases were included in the search: CINAHL, PubMed, PsychInfo, SPORTDiscus, and Web of Science. The database search was limited to included articles published in the English language, from the time of the inception of each database through June 8, 2018. The search strategy utilized for this systematic review, including the navigation of gray-literature via Google search, can be found in the Appendix A. The search strategy included three primary search categories (knee, cognition, and motor task) and synonymous terms, along with Medical Subject Heading (MeSH) terms when appropriate. From the found articles, the principal investigator individually hand searched each reference list for other potentially relevant articles.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used to detail the process of article inclusion and exclusion.32 One researcher (BN) independently searched the databases and reviewed article titles and abstracts to identify potentially relevant studies. To be eligible, studies had to include adolescents and/or young adults, defined as ages 14- 18 and 18-45, respectively. Participant groups had to include individuals with history of ACL injury (any severity) or ACLR procedure. Once potentially relevant articles were identified, the principal investigator (BN) screened the full texts for additional inclusion criteria: (1) Assessment of balance, gait, jump landing, and/or a cutting maneuver under dual- and single-task conditions; (2) a cognitive task defined as arithmetic, auditory, and/or working memory; and (3) the use of LE performance measures. The following studies were excluded: (1) Case series or case studies; (2) interventional studies; and (3) populations with neurological conditions (concussion, dementia, etc.), amputations, or nontraumatic knee conditions (osteoarthritis).
Quality Review and Data Extraction
A modified version of the Downs and Black checklist,33 as previously applied,18 was used to evaluate study quality on a scale from 0-13. One reviewer (BN) independently performed data extraction and scored each article for quality. Data extraction categories followed those as previously described29 and included: authors, publication date, country, study design, eligibility and exclusion criteria, participant characteristics, motor and cognitive task assessment protocols, assessment timeframes, study results, and study resources. Effect sizes of dual versus single-task effect on lower extremity and/or cognitive performance were calculated when available, and reported as Cohen's d with the following criteria: < 0.2 (trivial), 0.2 – 0.49 (small), 0.5 – 0.79 (medium), and ≥ 0.8 (large).34
RESULTS
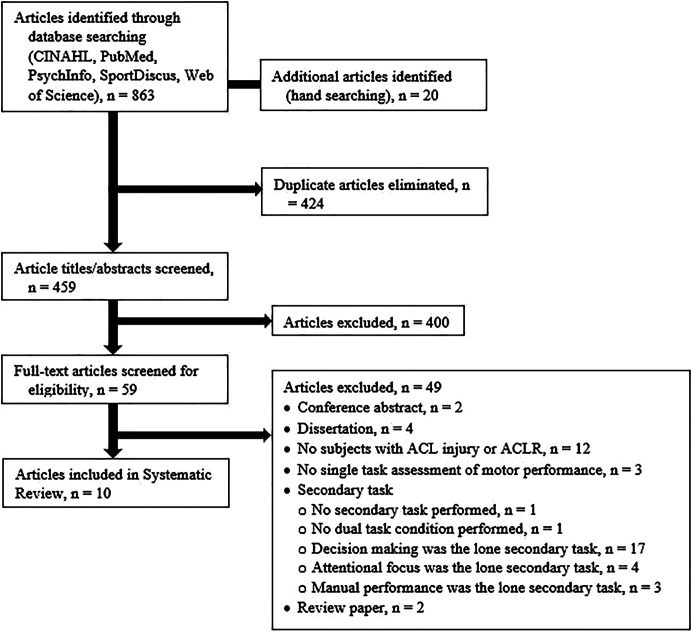
The initial database search yielded 863 articles, with an additional 20 articles located through hand searching. Following elimination of duplicate articles, 459 article titles/abstracts were screened, and, subsequently, 400 articles were excluded. Full-text screening of the remaining 59 articles yielded 10 articles to be included in the analysis. Figure 1 depicts a flow diagram of the systematic search strategy in accordance with PRISMA guidelines.32 The dual-task protocols lacked homogeneity across the included studies, which did not allow for a meta-analysis.
Figure 1.
Flow diagram of the systematic search strategy
Quality Review
Table 1 displays the itemized scoring results for study quality. Operational definitions of study quality assessment included low (0-4), moderate (5-8), and high (9-13), respectively. Most studies were of high quality (n = 9), while one study was of moderate quality (n = 1). Scoring ranged from 8-11 across all studies. Nine of the articles had similar author groups and/or affiliations. All articles were published within the prior ten years, which indicates this area of research is still in the relatively early stages of development.
Table 1.
Quality assessment of included studies.
| Modified Downs and Black Criteria | Akhbari et al41 | Lion et al39 | Mazaheri et al35 | Mohammadi-Rad et al40 | Mohammadi-Rad et al22 | Nazary-Moghadam et al36 | Nazary-Moghadam et al37 | Negahban et al21 | Negahban et al38 | Negahban et al23 |
|---|---|---|---|---|---|---|---|---|---|---|
| Clear objective(s) | + | + | + | + | + | + | + | + | + | + |
| Main outcomes clearly described | + | + | + | + | + | + | + | + | + | + |
| Participants clearly described | + | + | + | + | + | + | + | + | + | + |
| Task(s) clearly described | + | + | + | + | + | + | + | + | + | + |
| Main findings clearly described | - | + | + | + | + | + | + | + | + | - |
| Measures of random variability for main outcomes | + | + | + | + | + | + | + | + | + | + |
| Reporting of actual probability values, except where value is < 0.001 | - | + | - | + | + | + | + | - | - | - |
| Participants represent population | - | - | - | - | - | - | - | - | - | - |
| Included participants represent population | - | - | - | - | - | - | - | - | - | - |
| Planned analyses | + | + | + | + | + | + | + | + | + | + |
| Appropriate statistical tests | + | + | + | + | + | + | + | + | + | + |
| Accurate outcome measures | + | + | + | + | + | + | + | + | + | + |
| Sample size calculation | + | + | + | - | - | - | - | - | - | - |
| Total Score | 9 | 11 | 10 | 10 | 10 | 10 | 10 | 9 | 9 | 8 |
(+) present in study; (-) absent from study
Study Design
Participant eligibility and exclusion criteria, along with demographic information are listed in Table 2. The populations under investigation were young adults with mean age range of 23-28 years. All participant groups were described as athletes with soccer participation frequently documented. Five of the articles investigated individuals with an ACL-deficient knee (nonsurgical),21,35-38 four articles examined those with ACLR,22,23,39,40 and one included both types of ACL patient groups.41 The time since ACL injury (range 6 – 34 months) or ACLR surgery (mean range 11-14 months) was reported on several occasions. All articles were case control studies with control groups of healthy individuals matched according to current activity level/sport, sports background, age, gender, body mass index, height, and/or weight. Three of the included studies were investigations of reliability.
Table 2.
Descriptive characteristics of studies included in the systematic review.
| Study/Country | Design | Study Eligibility Criteria | Study Exclusion Criteria | Study Participants | Control group | Quality (0-13) |
|---|---|---|---|---|---|---|
| Akhbari et al41 Iran | Case control (reliability) | Injured athletes had returned to their sporting activity (soccer) | Vestibular or visual problems History of other orthopedic injuries in either limb over the past year (except meniscal injuries treated with non-invasive procedures) |
Male soccer athletes: n = 67; 23 ACL-deficient, 25 ACLR, 19 healthy controls; mean ± SD age, 26.6 ± 5.1 y, 28.2 ± 4.8 y, 27.6 ± 4.0 y. | NA | 9 |
| Lion et al39 Luxembourg | Case control | Age 15-35 y Unilateral ACLR Medically cleared to return to sport No history of neurological, visual, or vestibular disorders Control group: Healthy athletes participating in sports ≥ 3 hours per week; no history of knee or musculoskeletal disorders |
History of prior knee injuries History of musculoskeletal disorders affecting postural performance |
Athletes: n = 19; 14 males, 5 females, who underwent unilateral ACLR (time since surgery 9.2 ± 1.6 months); mean ± SD age, 24.8 ± 6.4 y | Healthy athletes: n = 21; 11 male, 10 female, mean ± SD age, 24.9 ± 3.7 y Matched according to age, gender, height, weight, and BMI | 11 |
| Mazaheri et al35 Netherlands | Case control | Age 15-40 y Nonsurgical, non-acute, complete ACL rupture with and without meniscal injury as confirmed by magnetic resonance imaging Time since injury 1-12 months Control group: Healthy participants without history of musculoskeletal injury in the back, neck or LE. |
Additional injury to the PCL, MCL, or LCL Injury to the contralateral LE Other musculoskeletal disorders Pain or difficulty with walking | Athletes with ACL-deficiency: n = 17 males; mean ± SD age, 28.5 ± 7.1 y | Healthy athletes: n = 19 males, mean ± SD age, 27.3 ± 6.6 y Matched according to age, gender, height, weight, and years of education |
10 |
| Mohammadirad et al40 Iran | Case control (reliability) | Athletes with unilateral ACLR were pain free, full weight bearing, functionally stable, had normal gait, and were provided clearance from their orthopedic surgeon for participation in the study Control group: No prior history of significant orthopedic injury (injury with symptoms lasting longer than 2 weeks duration) or balance condition |
History of known balance, vestibular, or visual problems, history of significant injury to either LE other than the ACL injury, or history of injury to any other knee ligaments at the time of the ACL tear over the past year | Athletes: n = 15; 14 males, 1 female, who underwent unilateral ACLR with hamstring autograft (time since surgery 12 ± 6 months); mean ± SD age, 26.0 ± 7.3 y | Healthy athletes: n = 15; 14 males, 1 female; mean ± SD age, 23.4 ± 6.5 y Matched according to age, gender, height, weight, and activity level |
10 |
| Mohammadi-Rad et al22 Iran | Case control | Athletes with unilateral ACLR within the past 6-12 months Followed similar postoperative rehabilitation protocol (no dual task training) |
History of significant pathology in any other joints or ligaments of the LEs | Athletes: n = 17; 16 males, 1 female, who underwent unilateral ACLR with hamstring autograft (time since surgery 14.1 ± 1.7 months); mean ± SD age, 26.8 ± 6.5 y | Healthy athletes: n = 17; 16 males, 1 female; mean ± SD age, 26.2 ± 7.3 y Matched according to age, gender, height, mass, and activity level |
10 |
| Nazary-Moghadam et al36 Iran | Case control | Unilateral, complete ACL tear (nonoperative treatment) | History of neurologic or orthopedic disorder History of auditory or visual deficiencies |
Young adults: n = 22 males with unilateral ACL-deficiency (time since injury 6-34 months); mean ± SD age, 26.0 ± 4.7 y | Healthy controls: n = 22 males; mean ± SD age, 24.3 ± 3.4 y Matched according to age, gender, height, weight, and physical activity prior to injury |
10 |
| Nazary-Moghadam et al37 Iran | Case control (reliability) | Nonsurgical, non-acute, complete ACL rupture with or without meniscal injury | History of serious neurological or musculoskeletal disorders History of falling Pain ≥ 3 on the Visual Analogue Scale Significant visual or auditory impairments |
Athletes: n = 14 males with unilateral ACL-deficiency (time since injury 19.7 ± 10.0 months); mean ± SD age, 27.1 ± 6.0 y | Healthy athletes: n = 14 males; mean ± SD age, 24.2 ± 4.0 y Matched according to age, gender, height, weight, and sport activity prior to injury |
10 |
| Negahban et al21 Iran | Case control | Nonsurgical, non-acute, complete ACL rupture with and without meniscal injury as confirmed by magnetic resonance imaging and clinical knee stability testing Pain no greater than two on the Visual Analogue Scale No injuries to the contralateral limb, neck, or back No history of ankle sprains on the ACL-deficient limb |
History of visual, vestibular, or neurological disorder History of auditory or cognitive (memory) impairment History of diabetes Use of any medication that could alter balance performance |
Male soccer athletes: n = 27 ACL-deficient; mean ± SD age, 26.7 ± 5.8 y | Male soccer athletes: n = 27 healthy controls; mean ± SD age, 26.3 ± 5.1 y Matched according to age, height, BMI, activity level, and sports background |
9 |
| Negahban et al38 Iran | Case control | Nonsurgical, non-acute, complete ACL rupture with and without meniscal injury as confirmed by magnetic resonance imaging and clinical knee stability testing Pain no greater than two on the Visual Analogue Scale No injuries to the contralateral limb, neck, or back No history of ankle sprains on the ACL-deficient limb |
History of visual, vestibular, or neurological disorder History of auditory or cognitive (memory) impairment History of diabetes Use of any medication that could alter balance performance |
Male soccer athletes: n = 27 ACL-deficient; mean ± SD age, 26.7 ± 5.8 y | Male soccer athletes: n = 27 healthy controls; mean ± SD age, 26.3 ± 5.1 y Matched according to age, height, BMI, activity level, and sports background |
9 |
| Negahban et al23 Iran | Case control | Age 17-45 years old >1 year since surgery Full AROM of surgical knee Full return to pre-injury activity level |
Concomitant injury to other knee ligaments at the time of ACL injury History of injury or surgery to the ankle and hip joints on the surgical limb History of injury or surgery to the nonsurgical limb History of recent neck and back pain History of vestibular or neurological disorders Uncorrected visual impairment Pain and joint effusion at the time of testing |
Young adults: n = 25 males who underwent unilateral ACLR with hamstring autograft (time since surgery 14.1 ± 1.7 months); mean ± SD age, 24.9 ± 3.8 y | Young adults: n = 25 healthy males; mean ± SD age, 24.9 ± 4.3 y Matched according to age, height, weight, and activity level |
8 |
Abbreviations: ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; AROM, active range of motion; BMI, body mass index; DLS, double limb stance; LE, lower extremity; SLS, single limb stance.
Dual-Task Assessment Protocols
Dual-task assessment methods and the key findings of included studies, along with effect sizes, are outlined in Appendix B. The number of dual-task assessment conditions in each study ranged from 3-17. Seven studies included motor task (single-task) assessment of balance performance, in positions of SLS,22,23,40,41 DLS,39 or both.21,38 Balance outcomes were measured via instrumented force platforms and software, which included center of pressure displacement, reaction time, latency, amplitude, regularity, complexity, sway velocity, and/or stability indices. In one study, an instrumented wobble board recorded contact frequency and time as a measure of balance performance.23 Balance conditions were also manipulated to include visual disturbances such as eyes open versus closed,21,22,38-40 varying levels of surface stability,21,22,38-40 and/or positional changes of the stance and non-stance knee.23
Walking gait was examined under single-task conditions on a motorized treadmill in three studies, which included varying stance width35 and velocity.36,37 Stance width during gait was manipulated to include narrow-base, defined as 50% of the distance between anterior superior iliac spine (ASIS) landmarks, and preferred step width.35 Gait velocity included self-selected, low (20% decrease), and high (20% increase) conditions.36,37 Gait outcomes were assessed by reflective makers and a 5-camera motion-analysis system, which included variability of step length, velocity, and/or width,35,36 in addition to hip and knee flexion ROM values.37 No studies evaluated landing or single-leg cutting mechanics under dual-task conditions in those with ACL injury or ACLR.
Three types of cognitive tasks were selected for the dual-task paradigm, which included an auditory Stroop task,22,36,37,40,41 arithmetic of varying difficulty levels,35,39 and backward digit span task of varying difficulty levels.21,23,38 The arithmetic conditions typically involved subtracting by either 3 or 7 as quickly and accurately as possible. Cognitive performance was evaluated in 90% of the included studies and typically expressed as an error ratio, response time, or the sum of correct/incorrect responses. Only one of the studies explicitly manipulated the prioritization of tasks.39
Study Outcomes
Postural control in single- and double-limb stance
DLS postural conditions yielded no significant differences in sway area and sway path between those with ACLR and healthy individuals, regardless of postural task difficulty.39 Both ACL-deficient and healthy individuals responded similarly with increased DLS postural sway under dual-task conditions; however the postural control of those with ACL-deficiency was not impaired to a greater extent under dual-task conditions when compared to healthy individuals.21
One study reported those with ACLR prioritized SLS postural control at the expense of cognitive performance under dual-task situations.22 However, this is in contrast to another study that examined postural sway in DLS.39 ACL-deficient athletes demonstrated greater center of pressure regularity in DLS and SLS compared to healthy individuals, hypothesized to indicate reduced adaptability of postural sway.38 SLS performance was impaired to a greater extent under dual- versus single-task conditions in young adults with ACLR, which was not observed in healthy individuals matched by age, height, weight, and activity level.23 Further, the ACLR group had varied SLS responses during three levels of cognitive task difficulty, which was not a trend seen in the control group; however, no differences in cognitive performance were shown between groups. Another study reported those with ACL-deficiency had an increased number of cognitive errors across DLS and SLS conditions when compared to a healthy control group matched according to age, height, BMI, activity level, and sports background.21
Walking gait
When walking at three different pre-selected velocities while performing an auditory task, those with ACL-deficiency demonstrated significantly increased step width coefficient of variation when compared to single-task conditions.36 This trend was not observed in a control group matched according to age, gender, height/weight, and prior physical activity level. Under narrow-base walking conditions, those with ACL-deficiency demonstrated decreased step length and increased step length variability during both single- and dual-task protocols when compared to a control group matched for age, gender, height/weight, and years of education.35 However, motor-cognitive performance costs were generally similar between the two groups when concurrently performing an arithmetic task.
DISCUSSION
Over half of the included studies assessed motor task performance through balance assessment, SLS and DLS under the dual-task paradigm – all of which included a participant group with ACLR or an ACL-deficient knee. These findings highlight the importance of selecting motor tasks that are sufficiently challenging to demand attentional resources during dual-task assessment. Motor tasks which are performed more automatically, such as DLS, may not be sensitive enough to identify postural control deficits in those with ACL injury.39 One may question the relevance of static SLS or DLS assessment for individuals returning to dynamic activities that require cutting, jumping, etc. However, no studies in the current systematic review examined dual-task cutting or jumping performance in those with ACL injury.
It has been demonstrated that in healthy populations, lower extremity mechanics were influenced by motor tasks that mimic noncontact ACL injury mechanisms under dual-task paradigms that involved a subtraction cognitive task.13,42 Similar trends were observed in other investigations with alternative secondary tasks, such as anticipatory or goal-oriented tasks.18,43 A drop-jump task with decision making resulted in decreased knee flexion angles at initial contact,43 while a systematic review highlighted suboptimal knee mechanics during single-leg cutting maneuvers performed under unplanned conditions.18 Goal-oriented tasks also demonstrated similar patterns of altered knee mechanics during drop vertical jump landing in response to an overhead goal, with decreased peak knee flexion angles and increased peak vertical ground reaction forces.12 Future studies should consider dual-task paradigms consisting of cutting and landing activities with a secondary task, which may include cognitive, anticipatory, or goal-oriented tasks.
The cognitive tasks in the included studies required auditory processing, computational skills, or working memory; all of which demand attentional resources to varying degrees. This may in part explain the variance in dual-task outcomes, as one cognitive task may place greater demands on attentional resources compared to another. It has been shown that adding a simple cognitive task can reduce center of pressure displacements in young adults; however, postural control can deteriorate with the application of more difficult cognitive tasks.44 Future research should examine the influence of cognitive task difficulty on sport-specific motor tasks.
One of the challenges with dual-task assessment is measuring the performance of the secondary task. Two of the secondary tasks excluded from this review were anticipatory and goal-oriented tasks, but these perhaps have greater external validity to the athletic environment compared to the cognitive tasks identified in the current study.12 This review highlights the value of capturing secondary task performance by recording cognitive errors, as those with ACL-deficiency displayed a greater number of cognitive errors without sacrificing balance performance when compared to healthy individuals.21 Measurement of cognitive performance deficits allows one to quantitatively appreciate the potential dual-task costs in spite of motor task performance preservation.
Several variables including patient populations, walking task difficulty, and the type of cognitive task selected for dual-task assessment may influence gait outcomes. Most dual-task gait (step length and velocity) and cognitive performance outcomes were similar between those with ACL-deficiency and healthy individuals when concurrently walking with narrow base of support and verbally counting backwards.35 This is in contrast to the findings of patients with ACL-deficiency showing increased step width variability when subjected to various walking speeds while performing an auditory Stroop task.36 It should be noted that none of the studies investigated dual-task gait outcomes in those with ACLR, which may provide insight into potential differences between patient groups. Researchers may wish to select motor tasks that emphasize frontal plane gait control for those with prior ACL injury.
From an intervention perspective, it has been shown that motor-cognitive dual-task training may result in enhanced gait, balance, and/or cognitive function in neurologic populations with motor-cognitive deficits.45 Others have supported single- and dual-task training to improve dual-task performance, however, conflicting evidence exists as to which type of training regimen is most effective.46,47 Finally, dual-task training may have greater benefits when compared to single-task training for sport skill development.48 Further research is needed to examine the effectiveness of motor-cognitive intervention programs in those susceptible to ACL injury with respect to enhancing lower extremity mechanics and motor skill development for injury prevention.
LIMITATIONS
The biggest limitation is that only one reviewer participated in study selection, data extraction, and scoring of study quality, which could have resulted in bias. The search strategy only included those studies with specific cognitive tasks, as systematic reviews already exist on the role of anticipation/decision-making for single-leg cutting mechanics.18,19
Additionally, most, if not all, of the methods used to measure motor task performance in the included studies were carried out in research laboratories and are not reproducible in most outpatient clinical settings, which limits generalizability to an extent. It would be advantageous to develop clinically feasible dual-task assessment strategies for motor tasks specific to noncontact ACL injury, in order to assist in return to sport decision making.
CONCLUSION
The addition of cognitive loading during single limb stance and walking gait revealed motor and/or cognitive performance costs in those with ACL injury compared to healthy individuals. Motor and cognitive task type and level of difficulty appear to be important considerations when assessing dual-task performance outcomes. No dual-task studies with ACL-deficient/ACLR patients were evaluated using more difficult athletic movements consistent with noncontact ACL injury mechanisms such as jump-landing and cutting. Given the low quantity and varying quality of the included studies, further research is needed to understand the influence of dual-tasking on motor and cognitive performance measures during athletic movements, as well as the implications for rehabilitation and return to sport testing after ACL injury.
APPENDIX A.
Search Strategy
CINAHL
|
SPORTDiscus
|
|
PsychINFO ((knee) OR (anterior cruciate ligament) OR (anterior cruciate ligament injury)) AND ((cognition) OR (dual task) OR (attention) OR (divided attention)) AND ((gait) OR (balance) OR (vertical jump biomechanics) OR (cutting)) |
|
PUBMED ((((((((((”psychomotor performance”[MeSH Terms]) OR “psychomotor performance”)) OR “gait”)) OR “balance”)) OR ((“postural balance”[MeSH Terms]) OR “postural balance”)) OR ((“drop vertical jump”) OR “cutting”)) AND ((((“cognition”) OR “Dual-task”) OR “attention”) OR “divided attention”)) AND ((((((“lower extremity”[MeSH Terms]) OR “hip”) OR “knee”) OR “ankle”) OR “leg”[MeSH Terms]) OR “lower extremity”) |
Web of Science
|
Google (Grey Literature Search)
|
APPENDIX B.
Dual-task assessment methods and key findings of studies included in the systematic review.
| Study | Dual-Task Assessment Protocol | Assessment Time Points | Study Results |
|---|---|---|---|
| Akhbari et al41 Iran | 3 conditions Single tasks: (1) Barefoot single limb stance (injured/surgical limbs of patients, and nondominant limbs of control group) with visual focus on a screen, in response to medium (6 °/s) and large (8 °/s) platform translations in the forward directions; (2) Auditory Stroop task reverse pitch recognition while seated Dual task: (1) Barefoot single limb stance (injured/surgical limbs of patients, and nondominant limbs of control group) with visual focus on a screen, in response to medium (6 °/s) and large (8 °/s) platform translations in the forward directions while completing an auditory Stroop task Prioritization of tasks: Participants were instructed to perform the Stroop task as accurately and quickly as possible (secondary task) Primary outcome assessed: Balance reactions (COP displacement: reaction time, latency, amplitude); Stroop task error ratio and response time |
Participants were assessed at 10.8 ± 3.2 months post injury for ACL deficient group, and 11.5 ± 2.5 months for ACLR group All three participant groups were re-tested 2-7 days after initial testing Randomized testing order |
Balance measures demonstrated moderate to very high intra-session and inter-session reliability under single- and dual-task situations Cognitive measures had low to high inter-session reliability for error ratio scores, and moderate to high reliability for response time. No significant performance differences for vast majority of balance and cognitive measures (test vs. re-test) across each group Resources needed for carrying out the study protocol are not readily available in most clinical settings (instrumented balance platform and software) |
| Lion et al39 Luxembourg | 8 conditions Single task: Barefoot DLS was performed for all conditions over 20 seconds duration; (1) DLS with eyes open; (2) DLS with eyes closed; (3) DLS with stable surface eyes open; (5) DLS with stable surface eyes closed; (5) DLS with foam surface eyes open; (6) DLS with foam surface eyes closed Dual task: (1) DLS with silent backward counting by seven with ‘posture first’ strategy; (2) DLS with silent backward counting by seven with ‘cognitive first’ strategy Prioritization of tasks: Participants were instructed prioritize posture or cognitive performance during separate test trials Primary outcome assessed: Balance performance as measured by two force platforms (sway area and sway path); cognitive task speed and accuracy |
Single session Randomized testing order |
No significant differences in DLS balance performance were identified between groups for any of postural conditions, regardless of difficulty No significant differences in cognitive performance were found between groups for any of the DLS postural conditions Resources needed for carrying out the study protocol are not readily available in most clinical settings (instrumented force platforms and software) |
| Mazaheri et al35 Netherlands | 6 conditions Single task: (1) Barefoot treadmill walking with preferred step width; (2) Barefoot walking with narrow-base (50% of distance between ASIS landmarks) Dual task: All walking conditions were performed with the following cognitive tasks: (1) Verbal backward counting in increments of 3; (2) Verbal backward counting in increments of 7 Prioritization of tasks: Participants were instructed to equally prioritize the motor and cognitive tasks Primary outcome assessed: Gait spatiotemporal parameters (mean and variability of step length/velocity); cognitive task sum of correct responses |
Single session (120 min) Randomized testing order |
ACL-deficient participants demonstrated decreased step length and increased variability in step length and velocity compared to the control group under the narrow-base walking condition The majority of gait and cognitive performance measures were similar between ACL-deficient participants and the control group under dual task conditions The injured limb of the ACL group demonstrated larger step length, where this trend was not observed in the control group Resources needed for carrying out the study protocol are not readily available in most clinical settings (reflective markers with 5-camera motion-analysis system and software) |
| Mohammadirad et al40 Iran | 8 conditions Single task: SLS was performed on the injured limb for all conditions over 30 seconds duration; (1) SLS with stability level 6 eyes open; (2) SLS with stability level 6 eyes closed; (3) SLS with stability level 8 eyes open; (4) SLS with stability level 8 eyes closed Dual task: (1) SLS with stability level 6 while performing an auditory Stroop task; (2) SLS stability level 8 while performing an auditory Stroop task Prioritization of tasks: Participants were instructed to verbally respond accurately and as quickly as possible to the auditory Stroop task while maintaining their balance Primary outcome assessed: Balance performance as measured by a Biodex Balance System (M-L, A-P, and overall stability indices); cognitive errors ratio and reaction time |
Retest session occurred 3-5 days after initial testing (120 min per subject) Randomized testing order |
Generally, moderate to high intersession and intersession reliability of balance performance was demonstrated among both groups as measured by the Biodex Balance System Cognitive performance measures demonstrated moderate to high reliability in ACLR and control participants Resources needed for carrying out the study protocol are not readily available in most clinical settings (instrumented balance platform and software) |
| Mohammadi-Rad et al22 Iran | 8 conditions Single task: SLS was performed on the injured limb for all conditions over 30 seconds duration; (1) SLS with stability level 6 eyes open; (2) SLS with stability level 6 eyes closed; (3) SLS with stability level 8 eyes open; (4) SLS with stability level 8 eyes closed Dual task: (1) SLS with stability level 6 while performing an auditory Stroop task; (2) SLS stability level 8 while performing an auditory Stroop task Prioritization of tasks: Participants were instructed to verbally respond accurately and as quickly as possible to the auditory Stroop task while maintaining their balance Primary outcome assessed: Balance performance as measured by a Biodex Balance System (M-L, A-P, and overall stability indices); cognitive error ratio and reaction time |
Single session (120 min) Randomized testing order |
ACLR participants prioritized postural performance at the expense of cognitive performance under dual task conditions when compared to healthy participants. Stroop task reaction time significantly increased for those with ACLR under dual task conditions (d = 0.8 – 1.0), as well as demonstrating higher error ratios (d = 0.6 – 1.0) Balance performance was not different between ACLR participants and the control group for the majority of balance conditions under dual task scenarios Resources needed for carrying out the study protocol are not readily available in most clinical settings (instrumented balance platform and software) |
| Nazary-Moghadam et al36 Iran | 6 conditions Single task: (1) Walking at self-selected velocity on a treadmill for 95 seconds duration; (2) Walking at low velocity (20% decrease); (3) Walking at high velocity (20% increase) Dual task: All walking conditions in addition to: (1) an auditory Stroop task Prioritization of tasks: No statement about task prioritization was included Primary outcome assessed: Gait performance (coefficient of variance for step length, step time, step width) |
Single session | Participants with ACL-deficiency demonstrated significantly decreased step width CV compared to healthy controls under single task conditions (d = 0.5) Participants with ACL-deficiency demonstrated significantly increased step width CV under dual task versus single task conditions (d = 0.3) Resources needed for carrying out the study protocol are not readily available in most clinical settings (reflective markers with 5-camera motion-analysis system and software) |
| Nazary-Moghadam et al37 Iran | 6 conditions Single task: (1) Walking at self-selected velocity on a treadmill; (2) Walking at low velocity (20% decrease); (3) Walking at high velocity (20% increase) Dual task: All walking conditions in addition to: (1) an auditory Stroop task Prioritization of tasks: No statement about task prioritization was included Primary outcome assessed: Gait performance (maximum/minimum hip and knee flexion ROM, total hip and knee ROM); cognitive error ratio and reaction time |
Retest session occurred 3-5 days after initial testing Randomized testing order |
Intrasession reliability in the ACL-deficient participants was high to very high in the majority of single and dual task conditions, and generally was superior when compared to the control group Intersession reliability was generally greater in ACL-deficient participants than the control group Resources needed for carrying out the study protocol are not readily available in most clinical settings (reflective markers with 5-camera motion-analysis system and software) |
| Negahban et al21 Iran | 17 conditions Single task: (1) DLS on a with eyes open on a rigid surface; (2) DLS with eyes closed on a rigid surface; (3) DLS with eyes closed on foam; (4) SLS eyes open on the injured limb; (5) SLS eyes open on the uninvolved limb; (6-7) Perform backward digit span task at maximal and easy levels of difficulty while seated Dual task: DLS and SLS tasks were performed while completing cognitive tasks; (1) Backward digit span task with maximal difficulty (full set of digits recalled plus 1); (2) Backward digit span task with easy level of difficulty (half of the digits) Prioritization of tasks: Participants were instructed to mentally rehearse the backward digit span task and focus on accuracy while performing the balance task of 30 seconds duration Primary outcome assessed: Balance performance measured by a Bertec balance platform (COP displacements A-P and M-L; sway velocity in A-P and M-L directions); cognitive errors |
Single session (120 min) Randomized testing order |
Both groups (ACL-deficient and control) demonstrated increased postural sway in DLS under dual versus single task conditions in all but one scenario (rigid surface – eyes closed), with small to large effect sizes noted in the ACL-deficient group (d = 0.3 – 0.9). ACL-deficient participants demonstrated increased postural sway across all DLS conditions when compared to the healthy control group; however, the addition of a cognitive task did not impair postural control in ACL-deficient participants to a greater degree when compared to the control group ACL-deficient participants had a significantly greater number of cognitive errors across seated, DLS, and SLS conditions when compared to the control group No significant differences in postural sway were noted between groups for the SLS condition, nor between limbs for the ACL-deficient group Resources needed for carrying out the study protocol are not readily available in most clinical settings (instrumented balance platform and software) |
| Negahban et al38 Iran | 10 conditions Single task: (1) DLS with eyes open on a rigid surface; (2) DLS with eyes closed on a rigid surface; (3) DLS with eyes closed on foam; (4) SLS eyes open on the injured limb; (5) SLS eyes open on the uninvolved limb Dual task: All DLS and SLS task conditions were performed while completing a backward digit span task with maximal difficulty (full set of digits recalled plus 1) Prioritization of tasks: Participants were instructed to mentally rehearse the backward digit span task and focus on accuracy while performing the DLS (30 sec) and SLS (20 sec) tasks Primary outcome assessed: Balance performance as measured by a Bertec balance platform (COP regularity and complexity, % determinism and Shannon entropy in A-P and M-L directions); cognitive errors |
Single session (90 min) Randomized testing order |
ACL-deficient participants demonstrated significantly greater COP regularity (decreased complexity) compared to healthy participants in both DLS and SLS Participants demonstrated decreased COP regularity with the addition of a cognitive task compared to single task conditions, with medium-large effect sizes (d = 0.5 – 1.1). Resources needed for carrying out the study protocol are not readily available in most clinical settings (instrumented balance platform and software) |
| Negahban et al23 Iran | 14 conditions Single task: (1) SLS on injured limb with straight knee; (2) SLS on injured limb with knee flexed 20 °; (3) SLS on uninjured limb with straight knee; (4) SLS on uninjured limb with knee flexed 20 °; (5-6) Perform backward digit span task at maximal and easy levels of difficulty while seated Dual task: All SLS task conditions were performed while completing two different cognitive tasks; (1) Backward digit span task with maximal difficulty (full set of digits recalled plus 1); (2) Backward digit span task with easy level of difficulty (half of the digits) Prioritization of tasks: No statement about task prioritization was included Primary outcome assessed: Balance performance measured by an instrumented wobble board (contact frequency and contact time); cognitive errors |
Single session Randomized testing order |
ACLR participants demonstrated decreased balance performance under dual-task conditions compared to single task, while this trend was not seen in the control group Contact time during SLS significantly increased for the ACLR group when a cognitive task was added, but no differences were seen between the easy and difficult cognitive task ACLR participants demonstrated significantly decreased balance performance when compared to the control group across most postural conditions ACLR participants demonstrated significantly greater contact frequency (decreased balance performance) on the injured versus uninjured limbs in both SLS positions Resources needed for carrying out the study protocol are not readily available in most clinical settings (instrumented wobble board and software) |
Abbreviations: A-P, anterior-posterior; ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; AROM, active range of motion; ASIS, anterior superior iliac spine; BMI, body mass index; COP, center of pressure; CV, coefficient of variation; DLS, double limb stance; LE, lower extremity; M-L, medial-lateral; SLS, single limb stance.
REFERENCES
- 1.Sheu Y Chen LH Hedegaard H. Sports- and recreation-related injury episodes in the United States, 2011–2014. Natl Health Stat Report. 2016;99:1-12. [PubMed] [Google Scholar]
- 2.Hootman JM Dick R Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319. [PMC free article] [PubMed] [Google Scholar]
- 3.Stanley LE Kerr ZY Dompier TP, et al. Sex differences in the incidence of anterior cruciate ligament, medial collateral ligament, and meniscal injuries in collegiate and high school sports: 2009-2010 through 2013-2014. Am J Sports Med. 2016;44(6):1565-1572. [DOI] [PubMed] [Google Scholar]
- 4.Paterno MV Rauh MJ Schmitt LC, et al. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ardern CL Taylor NF Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543-1552. [DOI] [PubMed] [Google Scholar]
- 6.Ardern CL Taylor NF Feller JA, et al. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015;43(4):848-856. [DOI] [PubMed] [Google Scholar]
- 7.Ardern CL Webster KE Taylor NF, et al. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596-606. [DOI] [PubMed] [Google Scholar]
- 8.Boden BP Torg JS Knowles SB, et al. Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med. 2009;37(2):252-259. [DOI] [PubMed] [Google Scholar]
- 9.Krosshaug T Nakamae A Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359-367. [DOI] [PubMed] [Google Scholar]
- 10.Olsen OE Myklebust G Engebretsen L, et al. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002-1012. [DOI] [PubMed] [Google Scholar]
- 11.Herman DC Barth JT. Drop-jump landing varies with baseline neurocognition: implications for anterior cruciate ligament injury risk and prevention. Am J Sports Med. 2016;44(9):2347-2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Almonroeder TG Kernozek T Cobb S, et al. Cognitive demands influence lower extremity mechanics during a drop vertical jump task in female athletes. J Orthop Sports Phys Ther. 2018;48(5):381-387. [DOI] [PubMed] [Google Scholar]
- 13.Dai B Cook RF, Meyer EA, et al. The effect of a secondary cognitive task on landing mechanics and jump performance. Sports Biomech. 2018;17(2):192-205. [DOI] [PubMed] [Google Scholar]
- 14.Almonroeder TG Kernozek T Cobb S, et al. Divided attention during cutting influences lower extremity mechanics in female athletes. Sports Biomech. 2017;13:1-13. [DOI] [PubMed] [Google Scholar]
- 15.Kipp K Brown TN McLean SG, et al. Decision making and experience level influence frontal plane knee joint biomechanics during a cutting maneuver. J Appl Biomech. 2013;29(6):756-762. [DOI] [PubMed] [Google Scholar]
- 16.McLean SG Lipfert SW van den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Med Sci Sports Exerc. 2004;36(6):1008-1016. [DOI] [PubMed] [Google Scholar]
- 17.Besier TF Lloyd DG Ackland TR, et al. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33(7):1176-1181. [DOI] [PubMed] [Google Scholar]
- 18.Almonroeder TG. The effects of anticipation on the mechanics of the knee during single-leg cuttig tasks: a systematic review Int J Sports Phys Ther. 2015;10(7):918-928. [PMC free article] [PubMed] [Google Scholar]
- 19.Brown SR Brughelli M Hume PA. Knee mechanics during planned and unplanned sidestepping: a systematic review and meta-analysis. Sports Med. 2014;44(11):1573-1588. [DOI] [PubMed] [Google Scholar]
- 20.McIsaac TL Lamberg EM Muratori LM. Building a framework for a dual task taxonomy. Biomed Res Int. 2015:591475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Negahban H Hadian MR Salavati M, et al. The effects of dual-tasking on postural control in people with unilateral anterior cruciate ligament injury. Gait Posture. 2009;30(4):477-481. [DOI] [PubMed] [Google Scholar]
- 22.Mohammadi-Rad S Salavati M Ebrahimi-Takamjani I, et al. Dual-tasking effects on dynamic postural stability in athletes with and without anterior cruciate ligament reconstruction. J Sport Rehabil. 2016;25(4):324-329. [DOI] [PubMed] [Google Scholar]
- 23.Negahban H Ahmadi P Salehi R, et al. Attentional demands of postural control during single leg stance in patients with anterior cruciate ligament reconstruction. Neurosci Lett. 2013;556:118-123. [DOI] [PubMed] [Google Scholar]
- 24.Kapreli E Athanasopoulos S Gliatis J, et al. Anterior cruciate ligament deficiency causes brain plasticity: a functional MRI study. Am J Sports Med. 2009;37(12):2419-2426. [DOI] [PubMed] [Google Scholar]
- 25.Grooms DR Page SJ Nichols-Larsen DS, et al. Neuroplasticity associated with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2017;47(3):180-189. [DOI] [PubMed] [Google Scholar]
- 26.Grooms DR Page SJ Onate JA. Brain activation for knee movement measured days before second anterior cruciate ligament injury: neuroimaging in musculoskeletal medicine. J Athl Train. 2015;50(10):1005-1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Swanik CB Covassin T Stearne DJ, et al. The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. Am J Sports Med. 2007;35(6):943-948. [DOI] [PubMed] [Google Scholar]
- 28.Grants L Powell B Gessel C, et al. Gait deficits under dual-task conditions in the concussed adolescent and young athlete population: a systematic review. Int J Sports Phys Ther. 2017;12(7):1011-1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kleiner M Wong L Dube A, et al. Dual-task assessment protocols in concussion assessment: a systematic literature review. J Orthop Sports Phys Ther. 2018;48(2):87-103. [DOI] [PubMed] [Google Scholar]
- 30.Lee H Sullivan SJ Schneiders AG. The use of the dual-task paradigm in detecting gait performance deficits following a sports-related concussion: a systematic review and meta-analysis. J Sci Med Sport. 2013;16(1):2-7. [DOI] [PubMed] [Google Scholar]
- 31.Register-Mihalik JK Littleton AC Guskiewicz KM. Are divided attention tasks useful in the assessment and management of sport-related concussion? Neuropsychol Rev. 2013;23(4):300-313. [DOI] [PubMed] [Google Scholar]
- 32.Moher D Liberati A Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336-341. [DOI] [PubMed] [Google Scholar]
- 33.Downs SH Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Commun H. 1998;52(6):377-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum Associates; 1988. [Google Scholar]
- 35.Mazaheri M Negahban H Soltani M, et al. Effects of narrow-base walking and dual tasking on gait spatiotemporal characteristics in anterior cruciate ligament-injured adults compared to healthy adults. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2528-2535. [DOI] [PubMed] [Google Scholar]
- 36.Nazary-Moghadam S Salavati M Esteki A, et al. Effect of dual-tasking on variability of spatiotemporal parameters in subjects with and without anterior cruciate ligament deficiency using linear dynamics. Phys Treat. 2015;4:213-220. [Google Scholar]
- 37.Nazary-Moghadam S Salavati M Esteki A, et al. Reliability of kinematic measures in subjects with anterior cruciate ligament deficiency during dual-task walking. J Bodyw Mov Ther. 2017;21(4):852-859. [DOI] [PubMed] [Google Scholar]
- 38.Negahban H Salavati M Mazaheri M, et al. Non-linear dynamical features of center of pressure extracted by recurrence quantification analysis in people with unilateral anterior cruciate ligament injury. Gait Posture. 2010;31(4):450-455. [DOI] [PubMed] [Google Scholar]
- 39.Lion A Gette P Meyer C, et al. Effect of cognitive challenge on the postural control of patients with ACL reconstruction under visual and surface perturbations. Gait Posture. 2018;60:251-257. [DOI] [PubMed] [Google Scholar]
- 40.Mohammadirad S Salavati M Takamjani IE, et al. Intra and intersession reliability of a postural control protocol in athletes with and without anterior cruciate ligament reconstruction: a dual-task paradigm. Int J Sports Phys Ther. 2012;7(6):627-636. [PMC free article] [PubMed] [Google Scholar]
- 41.Akhbari B Salavati M Ahadi J, et al. Reliability of dynamic balance simultaneously with cognitive performance in patients with ACL deficiency and after ACL reconstructions and in healthy controls. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3178-3185. [DOI] [PubMed] [Google Scholar]
- 42.Seymore KD Cameron SE Kaplan JT, et al. Dual-task and anticipation impact lower limb biomechanics during a single-leg cut with body borne load. J Biomech. 2017;65:131-137. [DOI] [PubMed] [Google Scholar]
- 43.Mache MA Hoffman MA Hannigan K, et al. Effects of decision making on landing mechanics as a function of task and sex. Clin Biomech (Bristol, Avon). 2013;28(1):104-109. [DOI] [PubMed] [Google Scholar]
- 44.Huxhold O Li SC Schmiedek F Lindenberger U. Dual-tasking postural control: aging and the effects of cognitive demand in conjunction with focus of attention. Brain Res Bull. 2006;69(3):294-305. [DOI] [PubMed] [Google Scholar]
- 45.Fritz NE Cheek FM Nichols-Larsen DS. Motor-cognitive dual-task training in persons with neurologic disorders: a systematic review. J Neurol Phys Ther. 2015;39(3):142-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pellecchia GL. Dual-task training reduces impact of cognitive task on postural sway. J Mot Behav. 2005;37(3):239-246. [DOI] [PubMed] [Google Scholar]
- 47.Ingriselli JM Register-Mihalik JK Schmidt JD, et al. Outcomes, utility, and feasibility of single task and dual task intervention programs: preliminary implications for post-concussion rehabilitation. J Sci Med Sport. 2014;17(6):580-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gabbett T Wake M Abernethy B. Use of dual-task methodology for skill assessment and development: examples from rugby league. J Sports Sci. 2011;29(1):7-18. [DOI] [PubMed] [Google Scholar]