Abstract
Background:
Less than 50% of those sustaining an anterior cruciate ligament (ACL) injury return to their preinjury level of sports participation or participate in competitive sport at two to seven years post ACL reconstruction (ACLR). After ACLR, it has been reported that frequency of subsequent ACL tears has reached as high as 31%.
Purpose:
The purpose of this case series was to evaluate return to sport and reinjury rates following the use of a criterion-based rehabilitation protocol with a final return to sport test that utilizes minimal equipment following ACL reconstruction.
Study Design:
Case series.
Methods:
Following ACL reconstruction, participants were included if they had a goal of returning to their pre-injury sport or level of activity, were between 16 and 50 years of age at the time of evaluation, had at least 25 physical therapy visits covered by insurance, and planned to complete physical therapy until clearance for return to sport.
Results:
Forty-three participants met the inclusion criteria and enrolled in the study. Twenty-one participants completed the full course of rehabilitation including passing their return to sport test and nineteen participants completed the two-year follow-up. Data obtained at two years indicated that 84% were able to return to their preinjury level of sports competition. A smaller percentage (16%) were able to return to a reduced level of sport and only one participant reported a second ACL injury.
Conclusion:
Participants that completed the full course of rehabilitation and passed return to sport testing had a larger percentage that were able to return to preinjury participation levels than currently reported in the literature. This case series did not exclude participants based on graft type, single vs double bundle procedure, ACL revision surgeries, nor concomitant procedures or injuries.
Level of Evidence:
Level 4
Keywords: anterior cruciate ligament, criterion-based rehabilitation, movement system, return to sport testing
INTRODUCTION
It is estimated that over 120,000 anterior cruciate ligament (ACL) injuries occur annually in the USA, with the majority occurring during high school and college.1 The ACL is often injured in sports participation, most commonly in a non-contact mechanism involving jumping, pivoting and cutting.2 The desire for a patient to return to cutting and pivoting sports is frequently cited as an indication for surgery, but actual return to sport rates are relatively low. Less than 50% return to their preinjury level of sports participation or continue to participate in competitive sport at two to seven years post ACLR.3 Ardern et al4 reports in a systematic review that while a larger percentage (83%) of athletes are able to return to some level of sport, only 63% are able to return to their previous level and an even smaller percentage (44%) return to competitive sport. It has also been found that younger athletes, males, and those athletes who participated in seasonal team sports were more likely to attempt return to sport by one year after ACL reconstruction.5 Currently, reinjury rates to the ipsilateral or contralateral ACL are relatively high (20-30%), but younger individuals who return to sport are at the highest risk.6-9
Since return to preinjury levels of function are relatively low and reinjury rates are high, clinicians are challenged to better prepare athletes to return to sport while also reducing the injury risk associated with returning to sport. The criteria used to inform return to sport decisions reported in research studies is most often based on time from surgery (60%) while factors such as muscle strength or hop testing are used less frequently (9-10%).6 The time from ACLR surgery to return to sport is about seven months, but timelines for can widely vary (2-24 months) for individual patients.4 Return to sport within the first year after surgery may not be advisable, as re-injury rates are highest during this time.6 Even in elite athletes, 83% returned to a preinjury level of sport between six and 13 months after surgery with a graft rupture rate of 5.2%.7 Moreover, time from surgery does not guarantee recovery as deficits in force development and absorption in single-limb vertical hopping were independent of time after surgery.8 It has also been found that females demonstrate asymmetries during both the landing and takeoff phase of the drop vertical jump maneuver two years after surgery.9
To better prepare athletes for return to sport, with a lessened reinjury risk, the authors created a five-phase ACLR rehabilitation protocol. The progression among phases with completion of a return to sport test is criterion-based and considers muscle strength, neuromuscular control, and task mastery. The emphasis on a criterion-based progression is different than what is often reported in the literature where time after surgery is the primary variable used.6 The purpose of this case series was to evaluate the return to sport and reinjury rates following the use of a criterion-based rehabilitation protocol with a final return to sport test that utilizes minimal equipment following ACL reconstruction. The authors hypothesized that the goal-oriented objective criterion-based program used in conjunction with time after surgery would best prepare the patient to return to their preinjury level of sports participation with a reduced rate of reinjury.
METHODS
Participants
Participants were informed of the study at their initial physical therapy evaluation. Written informed consent was obtained from all participants (and a legal guardian if younger than 18 years) prior to data collection and was approved by an institutional review board (IRB # PRO09030004). Participants were included if they had a goal of returning to their pre-injury sport or level of activity, were between 16 and 50 years of age at the time of evaluation, had at least 25 physical therapy visits covered by insurance, and planned to complete the criterion-based rehabilitation protocol in physical therapy until they were given clearance for return to sport by the physician based on the participant's results on the return to sport test. Participants were not excluded for any previous knee injury, concomitant knee injuries or procedures at the time of surgery, nor for the type of graft or reconstruction procedure they received. Patient reported outcomes were obtained at the first physical therapy evaluation visit and at the time for testing between each phase. Follow-up occurred at 12, 18, and 24 months post-surgery via phone call or email. At those time points, participants were asked about their level of sports participation as well as if any reinjuries occurred.
Scales and Surveys
Participants completed a battery of patient-reported outcomes at the onset of physical therapy, at progression to each new phase, and after completing the return to sport test. Participants completed the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, the Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), the Knee Outcome Survey Sports Activity Scale (KOS-Sports), and Numeric Pain Rating Scale (NPRS) to assess knee joint function and symptoms. Activity level was assessed via the Marx Activity Scale (Marx). Psychological readiness and belief in functional capacity were assessed via the Knee Activity Self-Efficacy Scale (KA-SES), the Knee Self-Efficacy Scale (K-SES), the Modified Self-Efficacy for Rehabilitation Outcome (MSERO), and the Tampa Scale for Kinesiophobia (TSK-11).
The IKDC consists of 18 questions in the domains of symptoms, functioning during activity of daily living and sports, current function of the knee, and participation in work and sports10 and has a high level of test-retest reliability (0.94).11 The KOS-ADL is a patient-reported measure of functional limitations imposed by pathological disorders and impairments of the knee during activities of daily living12 and reliability was found to be 85.8, mean validity score 76.0, and standardized response mean 1.1.13 The KOS-Sports measures symptoms and functional limitations experienced during sports activities.14 The Marx scale measures physical activity levels in patients as opposed to participation levels in sports, with a high reliability of 0.97.15 The NPRS ranges from 0 (no pain) to 10 (worst imaginable pain) and has been shown to be a reliable method of pain intensity assessment (ICC = 0.74-0.76).16,17 The KA-SES relates to the subject's perception of what everyday tasks he or she is able to accomplish.18 The K-SES assesses perceived self-efficacy regarding daily activities, sports and leisure activities, physical activities, and their knee function in the future. In patients with ACL injury, internal consistency was found to be 0.94, test-retest correlation was 0.73, and ICC was 0.75.19 The MSERO is modified from the Self-Efficacy for Rehabilitation Outcome Scale, which was shown to be valid and reliable in a population of participants after hip or knee arthroplasty.20 The questions on the MSERO involve the subject's perception of his or her ability to complete rehabilitation tasks.18 The TSK-11 was used to quantify pain-related fear of movement/reinjury and has an internal consistency of 0.79, a test-retest reliability of 0.81, and a responsiveness of 1.11.21 The TSK-11 for fear of injury is appropriate for use in the early postoperative phase and lower scores are found in patients reporting return to preinjury levels of sports participation.22 Scores on the TSK-11 and KA-SES were found to be significant predictors of IKDC subjective form scores.18
Strength and Functional Testing
Participants were screened throughout the rehabilitation process for strength, motor control, and capacity for plyometrics. Tests included, but are not limited to, a one-repetition maximum (1-RM) strength assessment for the quadriceps and leg, gait analyses, motor control with single leg squats, and performance with agility and jumping activities. While not all tests are validated measures, they are assessments that are commonly performed in physical therapy following ACL reconstruction.
Gait was assessed during fast treadmill walking for 15 minutes using a speed short of jogging (individual still demonstrates a double support phase). The physical therapist assessed for gait deviations such as an unequal stride length and hip hiking and the presence of pain.
Quality of movement was assessed with the step and hold test and single leg squats. The step and hold (Figure 1) is a low-level approximation of running to screen for abnormal mechanics with weight acceptance. The individual steps from the uninjured limb onto the injured limb, at least the distance of the individual's normal stride length. The individual is cued to imagine they are stepping over a puddle of water and to land with a heel-toe gait pattern to simulate walking and running without excessive stiffening or excessive knee flexion, loss of balance, or valgus collapse. Patients performed single leg squats to a specific degree of knee flexion without displaying loss of balance, contralateral hip drop, excessive femoral abduction or adduction where the knee moves inside or outside the border of the foot, excessive femoral internal rotation, or abnormal trunk movement. Piva et al. described these compensatory patterns in patients who had patellofemoral pain and found the assessment of quality of movement to have a moderate inter-tester reliability of 0.67.23 Weighted single leg squats were assessed in the later stages of the protocol. This is accomplished by holding dumbbells or wearing a weighted vest. Body weight is not part of the equation. For example, if the uninvolved limb could complete the task wearing a 20-pound weighted vest, the patient would need to complete the task on the involved side with at least 15 pounds.
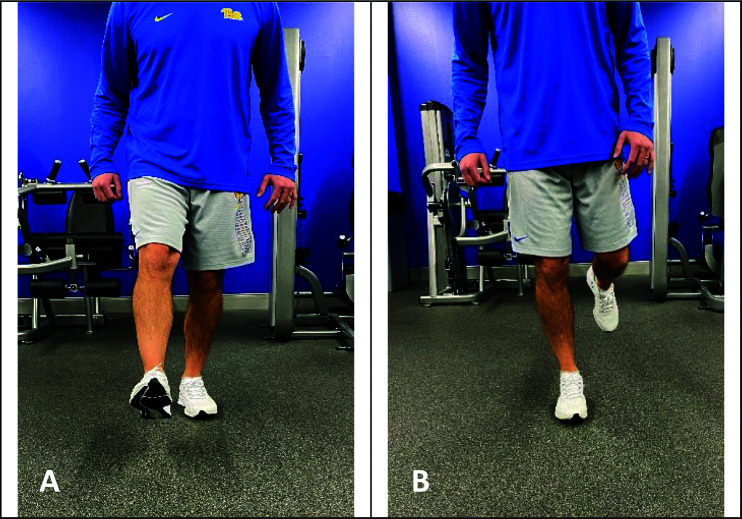
Figure 1.
In the step and hold exercise, the individual A) steps from the uninjured limb, B) onto the injured limb, at least the distance of the individual's normal stride length. The individual is cued to imagine they are stepping over a puddle of water and to land with a heel-toe gait pattern without excessive stiffening, knee flexion, loss of balance, or valgus collapse.
The modified Star Excursion Balance Test (SEBT) test is a measure of dynamic stability and neuromuscular control between limbs.24,25 Patients stand in the center of a “Y” on their involved side and reach as far as they can in an anterior, posteromedial and posterolateral direction while maintaining single leg stance. The maximum distance touched with the contralateral toe is measured. Reaches do not count if the patient loses their balance or puts more weight than a “toe tap” on the ground with the contralateral foot. Measuring the reach in the three designated directions had an ICC ranging from 0.84 to 0.87 and the assessment of limb length had an ICC of 0.99.26 Reach distance was normalized to the patient's limb length. Composite scores are from the sum of the three reaches divided by three times the patient's limb length and expressed as a percentage.
An electromechanical dynamometer is considered the gold standard for strength assessment due to superior reliability and high internal validity.26 However, many physical therapy clinics and athletic training rooms do not have an electromechanical dynamometer nor a hand-held dynamometer, so objective assessments of strength of the quadriceps and lower extremity was assessed via a 1-RM on a knee extension and leg press machine. The leg press can be used as a general measure of lower extremity strength, with contributions from the gluteal muscles, hamstrings and the triceps surae in addition to the quadriceps. 1-RM testing represents a valid means to assess leg muscle strength in vivo in both young and elderly men and women, with the strongest correlation found between 1-RM leg extension and isometric peak torque (r = 0.88; SEE = 0.06, 95% CI = 0.81-0.93).27
For the 1-RM leg extension, the individual is positioned in 90 ° hip and knee flexion with the resistance pad placed proximally to the malleoli. The individual is instructed to extend their knee as smoothly as possible to the designated amount of extension. Sinacore et al recently investigated the the absolute agreement of quadriceps muscle strength symmetry between limbs when measured with a leg extension task in a partial range and a full ROM in individuals with knee joint impairments. It was concluded that quadriceps symmetry is consistent when measured through either a full ROM or partial ROM, and that injured limbs and healthy limbs demonstrate similar relative strength in the range from 90-45 ° and from 90-0 ° and has an ICC of 0.67 and 0.62, respectively.28 For the 1-RM leg press, the individual is positioned on the leg press with the hip and knee being tested flexed to 90 °. The contralateral leg cannot assist in initiating the lift and cannot be on the floor or on the platform. The participant will continue to progress the weight lifted until they can no longer complete a full repetition for both the involved and uninvolved leg. The limb symmetry index for the leg press and knee extension test is calculated as the 1-RM load of the involved limb divided by the 1-RM load of the uninvolved limb expressed as a percentage for both the knee extension and leg press test.
Criterion-Based Functional Rehabilitation Protocol
The protocol that was used was introduced by Joreitz et al.29 and is presented in Appendix A. Participants progressed through the rehabilitation process in five phases, starting with becoming independent with activities of daily living (ADLs), and progressing to running, basic agility training, plyometrics, and rotational cutting and pivoting. Later stages of the rehabilitation program are individualized per the participant's requirements for their primary sport. An example is a volleyball player would have a larger rehabilitation emphasis placed on jumping compared to a soccer player who would have greater emphasis on cutting and agility tasks.
The criterion-based protocol serves multiple purposes. The first is to use objective criteria in conjunction with time after surgery as agreed upon per each individual surgeon, and not just time after surgery to progress through the rehabilitation process. To progress to the next phase, the participant must meet a set of objective criteria, which include mastery of the activities of each phase. Mastery is typically assessed through observation of the highest level of performance allowed in the progression. Failure to master the tasks of an individual phase is remediated with focused practice and instruction in proper technique. The inclusion of activity mastery as a pre-requisite for advancement to the next phase ensures that individuals take time to practice each skill and incorporate good movement patterns during dynamic tasks even if their strength and neuromuscular control would allow them to progress in multiple phases. Mastery of a task also includes participant reports of full confidence and no fear of reinjury with each new task.
A second purpose of the criterion-based protocol is to include strategies for prevention of ACL injury throughout the program with a focus on balance and proprioception, motor control, agility and plyometric training.30-35 A third purpose is to make this protocol generalizable to all clinical settings and to all individuals. The tests and measures can be applied with minimal specialized equipment and to all individuals regardless of surgical procedure. Specific attention is paid to concomitant injuries and/or procedures in that modifications to weight-bearing, range of motion (ROM) and RTS timeframes are made accordingly.
Phase one of the protocol begins immediately after surgery. The first four to six weeks focus on restoring ROM, patella mobility and quadriceps strength, decreasing inflammation, normalizing gait, and becoming independent with activities of daily living (ADLs). Exercises are then added for strength and stabilization of the hip and core. Exercise dosage for quadriceps strengthening via an open kinetic chain (OKC) knee extension and closed kinetic chain (CKC) leg press were determined by the DAPRE (Daily Adjustable Progressive Resistive Exercise) method of strengthening.36 Initially, OKC quadriceps exercises are performed in a restricted range of 90-45 ° to minimize strain on the healing ACL graft37,38 and patellofemoral joint stress.39 Risk of patella fracture after autogenous bone-patella tendon-bone (BPTB) or quadriceps tendon with bone block was reduced by delaying 1-RM testing until four months post-surgery.40 Once the 1-RM for quadriceps strength on the knee extension machine was established, knee extension resistance intensities were periodized to increase strength and hypertrophy.41 The authors were conscious of how many visits each patient was authorized to receive by their individual insurance. Therefore, participants presented 1-3x/week for physical therapy appointments based on their need in Phase 1. For example, some participants required more appointments if they were having difficulty regaining their ROM or quadriceps strength. Other participants who quickly regained their ROM, mobility, and quadriceps strength, minimized their visit usage in the early phase and relied on an extensive home exercise program.
For clearance to begin jogging, participants must demonstrate mastery of exercises in phase one by demonstrating the ability to perform 15 minutes of fast walking on the treadmill with normal gait at a speed just short of jogging. Additionally, participants must demonstrate 30 step and holds without loss of balance and good motor control as well as the ability to perform 10 single leg squats to 45 ° of knee flexion without compensation. The participant must score at least 80% LSI for the 1-RM on the knee extension machine in the range of 90-45 °, 80% LSI for the 1-RM on the leg press, and a 90% composite score on the modified SEBT. The participant must pass each of these tests and gain clearance from the surgeon before beginning to jog.
In Phase 2, participants continued lower extremity and core strengthening and started a jogging progression.42 The progression was based on each participant's comfort with jogging, signs and symptoms of inflammation (effusion, warmth, redness), joint pain, and display of normal gait pattern. The goal in this phase was to progress to at least two miles of continuous jogging and participants often performed their strengthening and jogging as part of a home exercise program to minimize the number of physical therapy visits utilized in this phase. Progression to phase three includes testing and mastery of running. Participants were required to complete two miles of continuous jogging at a self-selected speed with a normal gait pattern and without complaints of pain and signs and symptoms of inflammation. Participants also needed to score at least 85% LSI for the 1-RM on the knee extension machine in the range of 90-0 °, 85% LSI for the 1-RM on the leg press, and a 100% composite score on the modified SEBT. They also needed to demonstrate the ability to complete 10 single leg squats > 45 ° of knee flexion while holding ≥ 75% extra weight compared to the other side. This can be accomplished by holding dumbbells and/or wearing a weighted vest. Body weight is not part of the equation.
Phase 3 includes the addition of basic change of direction drills including forward/backward shuttle running, side shuffling, carioca, and “quick feet” drills using a ladder or hurdles in a forward and lateral direction. In this phase, the emphasis is placed on controlling the deceleration of the involved limb and moving in the frontal and transverse planes. Effort begins at approximately 50% speed and continues at that intensity level until the individual can complete the drills without hesitation or compensation during deceleration to change directions, as well as reporting 100% confidence in the knee at that speed. The individual should initially perform the agility progression under the supervision of their physical therapist or athletic trainer to monitor quality of movement patterns. Common compensation patterns include internal rotation or valgus collapse of the limb when planting the foot during, excessive stutter stepping when preparing to decelerate, and excessive absorption time of weight acceptance in lateral shuffling or carioca compared to the uninvolved side. Progression to phase four requires mastery of agility drills, ability to perform 10 consecutive weighted single leg squats to at least 60 ° of knee flexion with a limb symmetry index of at least 85%, and a LSI of 90% on 1-RM test for the leg press and knee extension test.
Phase 4 introduces double limb jumping. The authors recommend beginning with forward and vertical jumps at sub-maximal distances and heights, respectively. Cueing for proper technique, both when loading into the jump as well as when landing, is crucial to avoid dynamic valgus and side to side asymmetries in balance and control.30,31,43 When participants consistently jump with good form, progression of plyometrics include box jumps, lateral and rotational jumps. Jumping is also progressed from one single jump to continuous faster jumping. Progression to phase five requires mastery of plyometrics and the ability to perform 10 consecutive weighted single leg squats to at least 60 ° of knee flexion with a limb symmetry index of at least 90%.
Phase 5 introduces hopping and cutting. Hops are initiated and progressed in the same manner as jumping. Cutting progresses from jogging “S” curves, to planting the involved foot and cutting at 45 ° and progressing to cutting at 90 ° angles. In addition to demonstrating good form, participants must report full confidence and no fear of reinjury before progressing in speed of cutting. When participants can cut at full speed with good form, unanticipated cutting and agility drills should be practiced. Exercise selection should be primarily sport specific and individualized in this phase.44-47
Return to Sports Participation Testing Protocol
When the participant can perform all functional tasks at full speed with no compensation strategies and reports full confidence, they may take the return to sport test. A reassessment of 1-RM quadriceps strength is performed on the knee extension machine. We also utilize a battery of functional tests48-52 and start with the four most common hop tests described by Noyes et al.53 A single leg vertical hop is assessed using a Vertec System (Gill Athletics, Champaign, IL). This return to sports participation test introduces hopping in the frontal and transverse planes as criteria to return to practice. Participants hop on one leg as far as they can in a medial and a lateral direction. For example, when hopping on the right leg, medial hops would be to the left and lateral hops would be to the right. When hopping on the left leg, medial hops would be to the right and lateral hops would be to the left (Figure 2). Transverse plane hops included a vertical hop with medial and lateral rotation (Figure 3). Patients stood in the center of the “Y” used for the SEBT and were instructed to hop straight up in the air and spin/rotate in a medially and laterally rotating direction and control the landing. For example, when performing a medially rotating hop on the right leg, patients hopped vertically and spun/rotated to the left. They performed a single leg laterally rotating hop on the right leg by hopping vertically and spinning/rotating to the right and controlling the landing. The opposite occurred on the left leg with medially rotating hops to the right and laterally rotating hops spinning/rotating to the left. The amount of rotation for each hop was measured with a goniometer, with the stationary arm lined up with anteriorly projected line used for the SEBT and the moving arm of the goniometer bisected the patient's foot along the second metatarsal. The amount of rotation was compared bilaterally to calculate the LSI. The last two plyometric tests are the single and triple jump (with the take-off phase starting with two feet) for distance where the participant must land on one foot (Figure 4). A hopping trial was considered invalid if the participant landed with early touchdown of the contralateral limb, had loss of balance, touched the floor with any other part of their body, or had additional hops after landing.54
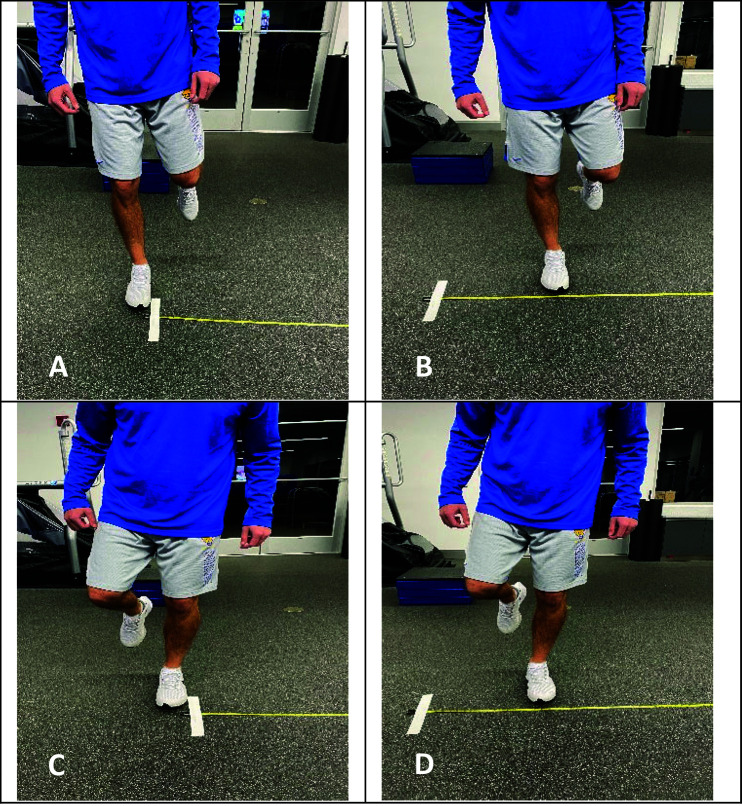
Figure 2.
Participants are instructed to hop on one leg as far as they can in a medial and a lateral direction. A) Right leg medial hop start position. B) Right leg medial hop end position. C) Left leg lateral hop start position. D) Left leg lateral hop end position.
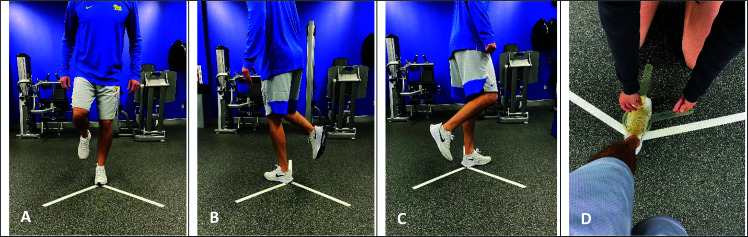
Figure 3.
For rotational hops, participants stood in the center of the “Y” used for the SEBT and were instructed to hop straight up in the air and spin/rotate in a medially and laterally rotating direction and control the landing. A) Left leg rotational hop starting position. B) Left leg medial rotating hop end position. C) Left leg lateral rotating hop end position. D) Measurement of the amount of rotation for each hop. The stationary arm of the goniometer is aligned parallel to the tape and the moving arm bisects the foot.
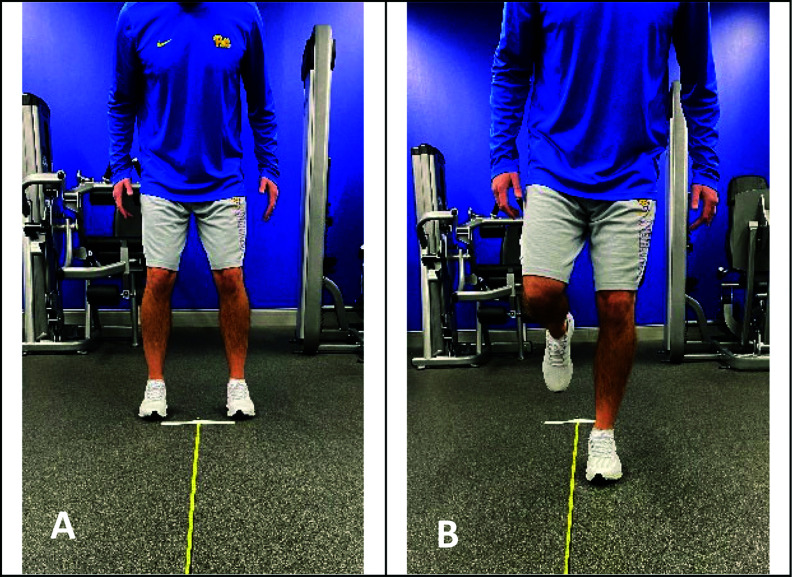
Figure 4.
For the single and triple broad jump, participants are instructed to A) start the jump with two feet, and then B) land on the single leg being tested. For the triple jump, the last jump will be landed on the single leg being tested.
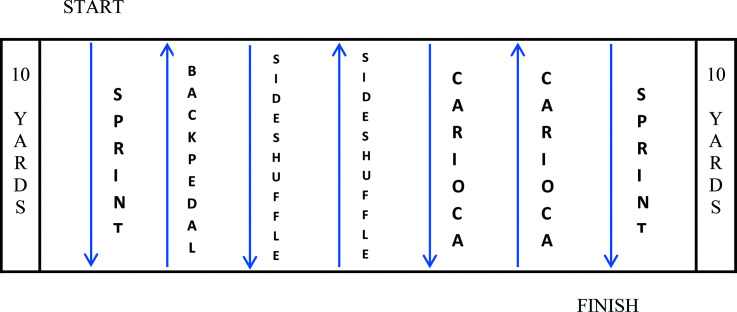
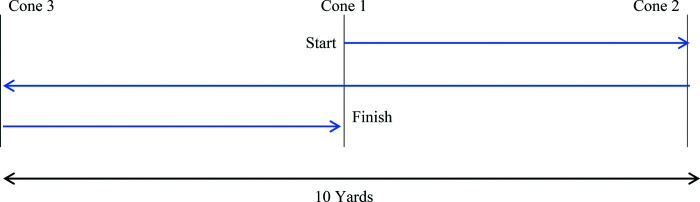
Two functional runs are utilized to assess for the presence of compensation strategies when changing directions at full speed. The lower-extremity functional run (Figure 5) is set up on a 10-yard course marked by 2 cones. The athlete begins with a 10-yard sprint followed by a 10-yard back-pedal, a 10-yard side-shuffle in each direction, a 10-yard carioca in each direction, and ends with a final 10-yard sprint. The pro-agility test (Figure 6) begins with the individual straddling the center line of a 10-yard course marked by three cones each five yards apart.54 The athlete must sprint five yards and touch the cone, change direction, sprint back 10 yards and touch the cone, change direction, and sprint back through the center line. The timer begins with the athlete's first movement to either end of the course and ends with the final crossing of the center line. These two functional runs are included for the physical therapist to evaluate for any abnormal movement patterns, or for subjective reports of hesitation, decreased confidence, and pain with change of direction movement patterns performed at full speed. Suggested time to complete each test is included as a reference, but only the quality of movement is assessed.55
Figure 5.
Participants will sprint 10 yards, then backpedal to the starting line; side-shuffle 10 yards and back; carioca 10 yards and back; and finally sprint 10 yards to the finish line. To pass this test, participants must run and change direction at full speed without any compensation patterns.
Figure 6.
Participants will start facing the tester straddling cone 1. When indicated, they will turn and sprint 5 yards and touch cone 2; then sprint 10 yards and touch cone 3; and finally, sprint 5 yards past cone 1. They will then repeat this test in reverse order (cone 1 to 3 to 2 to 1). To pass this test, participants must run and change direction at full speed without any compensation patterns.
Passing criteria is ≥ 90% LSI for all single-limb tests along with physician clearance. Passing the test allows the participant to return to unrestricted practice (if their sport is in-season). The function of the RTS test was to allow the participation in sports activity without any restrictions. When there were no impairments with full practice participation (either from the viewpoint of the participant, coach, or athletic trainer), they would be cleared to resume competition. This enabled adequate time to acclimate to full-speed practices with opposition and contact (when applicable). The rehabilitation protocol with return to sport test can be found as a supplemental file.
OUTCOMES
Participant demographic characteristics are presented in Table 1. Forty-three participants met the inclusion criteria and were enrolled in the study. However, only 21 participants (49%) completed the full course of rehabilitation including passing their return to sport test and 19 participants (44%) were available for the two-year follow-up. There were no statistically significant differences between those that completed or did not complete the program related to age, sex, graft type, or associated procedures. The average time from surgery to meeting the criteria to start jogging was four months (SD = 1.2 months). The average time from surgery to return to sport clearance was 10.6 months (SD = 4.4 months). One participant was excluded midway through her rehabilitation due to becoming pregnant, which was an exclusion criterion. Participant reported outcomes are listed in Table 2 for all participants enrolled. Tables 3 and 4 list the participant reported outcomes for the participants that completed the full course of rehabilitation and those that did not, respectively.
Table 1.
Patient Demographics.
| Enrolled (n = 43) | Completers (n = 21) | Non-completers (n = 22) | p-value Comparing Completers to Non-completers | |
|---|---|---|---|---|
| Age, mean ± SD | 27.2 ± 8.5 | 25.7 ± 8.3 | 28.9 ± 8.7 | 0.24 |
| Sex, n (%) | 0.41 | |||
| Male | 24 (56%) | 11 (52%) | 13 (66%) | |
| Female | 19 (44%) | 10 (48%) | 9 (41%) | |
| Mechanism of injury, n (%) | 0.13 | |||
| Contact | 8 (20%) | 2 (10%) | 6 (27%) | |
| Non-contact | 33 (80%) | 19 (90%) | 16 (73%) | |
| Graft type, n (%) | 1.00 | |||
| Allograft | 11 (26%) | 4 (19%) | 5 (23%) | |
| Autograft | 32 (74%) | 17 (81%) | 17 (77%) | |
| Graft source, n (%) | 0.85 | |||
| BPTB Autograft | 15 (35%) | 8 (38%) | 7 (32%) | |
| Quad Tendon Autograft | 9 (25%) | 6 (29%) | 3 (14%) | |
| Hamstring Autograft | 8 (22%) | 4 (19%) | 4 (25%) | |
| BPTB Allograft | 7 (16%) | 2 (10%) | 5 (23%) | |
| Tibialis Anterior Allograft | 3 (7%) | 1 (5%) | 2 (9%) | |
| Achilles Allograft | 1 (2%) | 0 (0%) | 1 (2%) | |
| Procedure, n (%) | 1.00 | |||
| Single Bundle | 40 (98%) | 20 (95%) | 22 (100%) | |
| Double bundle | 1 (2%) | 1 (5%) | 0 (0%) | |
| Associated meniscus procedure | 20 (49%) | 12 (57%) | 8 (40%) | 0.35 |
| Associated cartilage procedure | 4 (10%) | 2 (10%) | 2 (10%) | 1.00 |
| Associated MCL, LCL, or PCL procedure | 8 (20%) | 4 (19%) | 4 (20%) | 1.00 |
BPTB = bone patellar tendon bone; MCL = medial collateral ligament; LCL = lateral collateral ligament; PCL = posterior cruciate ligament
Table 2.
Patient Reported Outcome Measures (All Participants).
| Overall Group | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Phase 1 | Phase 2 | Phase 3 | Phase 4 | Phase 5 | Return to Sport | |||||||||||||
| N | Mean | Std | N | Mean | Std | N | Mean | Std | N | Mean | Std | N | Mean | Std | N | Mean | Std | |
| IKDC | 43 | 30.50 | 13.58 | 30 | 67.25 | 10.41 | 26 | 76.65 | 6.86 | 21 | 81.44 | 7.93 | 21 | 86.63 | 7.85 | 21 | 93.38 | 8.14 |
| KOS-ADL | 43 | 41.23 | 18.76 | 30 | 89.81 | 8.65 | 26 | 93.46 | 4.95 | 21 | 94.49 | 4.22 | 21 | 95.34 | 3.80 | 21 | 97.41 | 2.62 |
| KOS-Sports | 43 | 16.32 | 15.21 | 30 | 57.93 | 25.65 | 26 | 72.03 | 20.78 | 21 | 85.71 | 7.81 | 21 | 91.77 | 5.89 | 21 | 96.50 | 4.33 |
| Marx | 43 | Med = 13 | IQR = 5 | 30 | Med = 16 | IQR = 6 | 26 | Med = 12 | IQR = 11 | 21 | Med = 12 | IQR = 5 | 21 | Med = 13 | IQR = 4 | 21 | Med = 12 | IQR = 5 |
| Pain | 43 | Med = 6 | IQR = 4 | 30 | Med = 2 | IQR = 2 | 26 | Med = 1 | IQR = 2 | 21 | Med = 1 | IQR = 2 | 21 | Med = 1 | IQR = 1 | 21 | Med = 0 | IQR = 1 |
| KA-SES | 43 | 27.74 | 20.55 | 30 | 67.93 | 15.31 | 26 | 81.15 | 11.23 | 21 | 87.90 | 8.62 | 21 | 93.16 | 5.65 | 21 | 97.43 | 3.61 |
| K-SES-DA | 43 | 10.13 | 13.73 | 30 | 66.76 | 21.39 | 26 | 80.05 | 16.36 | 21 | 87.89 | 11.09 | 21 | 93.16 | 9.13 | 21 | 97.96 | 3.74 |
| K-SES-Sport | 43 | 6.93 | 11.27 | 30 | 48.20 | 18.53 | 26 | 59.31 | 15.70 | 21 | 62.67 | 12.75 | 21 | 69.16 | 10.53 | 21 | 77.90 | 3.25 |
| K-SES-PA | 43 | 5.58 | 11.44 | 30 | 52.11 | 22.15 | 26 | 67.69 | 21.08 | 21 | 81.51 | 13.81 | 21 | 89.65 | 9.74 | 21 | 96.83 | 4.31 |
| K-SES-KF | 43 | 84.30 | 19.88 | 30 | 82.33 | 22.80 | 26 | 89.81 | 12.80 | 21 | 92.74 | 10.46 | 21 | 94.74 | 7.63 | 21 | 95.48 | 6.60 |
| K-SES | 43 | 21.65 | 10.33 | 30 | 61.38 | 17.85 | 26 | 73.74 | 13.18 | 21 | 81.30 | 9.43 | 21 | 87.03 | 6.66 | 21 | 92.64 | 3.06 |
| MSERO | 43 | 88.63 | 14.71 | 30 | 96.60 | 4.34 | 26 | 98.81 | 1.72 | 21 | 99.29 | 1.27 | 21 | 99.58 | 1.07 | 21 | 99.81 | 0.68 |
| TSK-11 | 43 | 21.14 | 5.56 | 30 | 18.13 | 4.59 | 26 | 17.42 | 5.08 | 21 | 17.00 | 4.22 | 21 | 15.53 | 4.85 | 21 | 15.52 | 3.14 |
N = Number. Std = Standard deviation. Med = Median. IQR = Interquartile range. IKDC = International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form. KOS-ADL = Activities of Daily Living scale of the Knee Outcome Survey. KOS-Sports = Sports Activity Scales of the Knee Outcome Survey. Marx = Marx Activity Rating Scale. Pain = Numeric Pain Rating Scale. KA-SES = Knee Activity Self-Efficacy Scale. K-SES-DA = Knee Self-Efficacy Scale for Daily Activities. K-SES-Sport = Knee Self-Efficacy Scale for Sports and Leisure Activities. K-SES-PA = Knee Self-Efficacy Scale for Physical Activities. K-SES-KF = Knee Self-Efficacy Scale for Knee Function in the Future. K-SES-Knee Self-Efficacy Scale (total score). MSERO = Modified Self-Efficacy for Rehabilitation Outcome. TSK-11 = Shortened version of the Tampa Scale for Kinesiophobia.
Table 3.
Patient Reported Outcomes (Completers).
| Completers | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Phase 1 | Phase 2 | Phase 3 | Phase 4 | Phase 5 | Return to Sport | |||||||||||||
| N | Mean | Std | N | Mean | Std | N | Mean | Std | N | Mean | Std | N | Mean | Std | N | Mean | Std | |
| IKDC | 21 | 27.86 | 8.50 | 21 | 65.64 | 9.73 | 21 | 75.28 | 5.71 | 21 | 80.65 | 7.92 | 21 | 86.20 | 7.85 | 21 | 93.38 | 8.14 |
| KOS-ADL | 21 | 38.28 | 18.99 | 21 | 89.00 | 9.84 | 21 | 92.50 | 5.18 | 21 | 94.29 | 4.30 | 21 | 95.08 | 3.74 | 21 | 97.41 | 2.62 |
| KOS-Sports | 21 | 16.02 | 16.73 | 21 | 54.35 | 23.50 | 21 | 67.27 | 20.80 | 21 | 85.15 | 7.67 | 21 | 91.41 | 5.84 | 21 | 96.50 | 4.33 |
| Marx | 21 | Med = 15 | IQR = 4.5 | 21 | Med = 16 | IQR = 4 | 21 | Med = 14 | IQR = 4.5 | 21 | Med = 12 | IQR = 5 | 21 | Med = 13 | IQR = 4 | 21 | Med = 12 | IQR = 5 |
| Pain | 21 | Med = 6 | IQR = 3 | 21 | Med = 1 | IQR = 2 | 21 | Med = 1 | IQR = 2 | 21 | Med = 1 | IQR = 2 | 21 | Med = 1 | IQR = 1 | 21 | Med = 0 | IQR = 1 |
| KA-SES | 21 | 22.24 | 18.45 | 21 | 63.30 | 13.83 | 21 | 78.85 | 11.64 | 21 | 87.17 | 9.00 | 21 | 92.83 | 5.63 | 21 | 97.43 | 3.61 |
| K-SES-DA | 21 | 8.10 | 12.65 | 21 | 60.93 | 22.03 | 21 | 78.21 | 17.42 | 21 | 87.54 | 11.17 | 21 | 92.78 | 9.24 | 21 | 97.96 | 3.74 |
| K-SES-Sport | 21 | 5.05 | 8.62 | 21 | 44.00 | 17.85 | 21 | 55.80 | 16.02 | 21 | 62.22 | 13.34 | 21 | 68.78 | 10.70 | 21 | 77.90 | 3.25 |
| K-SES-PA | 21 | 4.29 | 7.35 | 21 | 43.83 | 17.46 | 21 | 63.33 | 21.49 | 21 | 80.19 | 14.24 | 21 | 89.07 | 9.69 | 21 | 96.83 | 4.31 |
| K-SES-KF | 21 | 81.43 | 25.56 | 21 | 77.38 | 26.11 | 21 | 88.00 | 13.97 | 21 | 91.81 | 11.04 | 21 | 94.44 | 7.74 | 21 | 95.48 | 6.60 |
| K-SES | 21 | 19.70 | 9.24 | 21 | 55.41 | 16.43 | 21 | 70.84 | 13.24 | 21 | 80.56 | 9.67 | 21 | 86.62 | 6.60 | 21 | 92.64 | 3.06 |
| MSERO | 21 | 89.62 | 13.77 | 21 | 97.00 | 3.83 | 21 | 98.70 | 1.66 | 21 | 99.33 | 1.33 | 21 | 99.56 | 1.10 | 21 | 99.81 | 0.68 |
| TSK-11 | 21 | 22.05 | 5.56 | 21 | 19.30 | 4.90 | 21 | 17.45 | 5.37 | 21 | 16.78 | 4.02 | 21 | 15.78 | 4.86 | 21 | 15.52 | 3.14 |
N = Number. Std = Standard deviation. Med = Median. IQR = Interquartile range. IKDC = International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form. KOS-ADL = Activities of Daily Living scale of the Knee Outcome Survey. KOS-Sports = Sports Activity Scales of the Knee Outcome Survey. Marx = Marx Activity Rating Scale. Pain = Numeric Pain Rating Scale. KA-SES = Knee Activity Self-Efficacy Scale. K-SES-DA = Knee Self-Efficacy Scale for Daily Activities. K-SES-Sport = Knee Self-Efficacy Scale for Sports and Leisure Activities. K-SES-PA = Knee Self-Efficacy Scale for Physical Activities. K-SES-KF = Knee Self-Efficacy Scale for Knee Function in the Future. K-SES-Knee Self-Efficacy Scale (total score). MSERO = Modified Self-Efficacy for Rehabilitation Outcome. TSK-11 = Shortened version of the Tampa Scale for Kinesiophobia.
Table 4.
Patient Reported Outcomes (Non-Completers).
| Phase 1 | Phase 2 | Phase 3 | Phase 4 | Phase 5 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | Std | N | Mean | Std | N | Mean | Std | N | Mean | Std | N | Mean | Std | |
| IKDC | 22 | 33.03 | 16.93 | 10 | 70.46 | 11.49 | 6 | 81.23 | 8.89 | 3 | 86.21 | 7.54 | 1 | 94.25 | . |
| KOS-ADL | 22 | 44.05 | 18.54 | 10 | 91.43 | 5.67 | 6 | 96.67 | 2.15 | 3 | 95.71 | 4.29 | 1 | 100 | . |
| KOS-Sports | 22 | 16.61 | 14.00 | 8 | 66.43 | 30.12 | 6 | 87.88 | 11.07 | 3 | 89.09 | 9.45 | 1 | 98.18 | . |
| Marx | 22 | 12.45 | 4.18 | 10 | 9.70 | 6.75 | 6 | 6.17 | 3.43 | 3 | 7.67 | 2.31 | 1 | 13.00 | . |
| Pain | 22 | 33.00 | 21.47 | 10 | 77.20 | 14.44 | 6 | 88.83 | 4.92 | 3 | 92.33 | 4.51 | 1 | 99.00 | . |
| KA-SES | 22 | 12.08 | 14.71 | 10 | 78.43 | 14.91 | 6 | 86.19 | 11.27 | 3 | 90.00 | 12.70 | 1 | 100 | . |
| K-SES-DA | 22 | 8.73 | 13.29 | 10 | 56.60 | 17.77 | 6 | 71.00 | 6.54 | 3 | 65.33 | 10.07 | 1 | 76.00 | . |
| K-SES-Sport | 22 | 6.82 | 14.38 | 10 | 68.67 | 21.90 | 6 | 82.22 | 11.72 | 3 | 89.44 | 8.55 | 1 | 100 | . |
| K-SES-PA | 22 | 87.05 | 12.31 | 10 | 92.25 | 8.45 | 6 | 95.83 | 4.65 | 3 | 98.33 | 1.44 | 1 | 100 | . |
| K-SES-KF | 22 | 23.51 | 11.16 | 10 | 73.32 | 14.82 | 6 | 83.41 | 7.52 | 3 | 85.76 | 7.73 | 1 | 94.55 | . |
| K-SES | 22 | 87.68 | 15.82 | 10 | 95.80 | 5.37 | 6 | 99.17 | 2.04 | 3 | 99.00 | 1.00 | 1 | 100 | . |
| MSERO | 22 | 20.27 | 5.54 | 10 | 15.80 | 2.86 | 6 | 17.33 | 4.41 | 3 | 18.33 | 6.11 | 1 | 11.00 | . |
| TSK-11 | 22 | 33.03 | 16.93 | 10 | 70.46 | 11.49 | 6 | 81.23 | 8.89 | 3 | 86.21 | 7.54 | 1 | 94.25 | . |
N = Number. Std = Standard deviation. Med = Median. IQR = Interquartile range. IKDC = International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form. KOS-ADL = Activities of Daily Living scale of the Knee Outcome Survey. KOS-Sports = Sports Activity Scales of the Knee Outcome Survey. Marx = Marx Activity Rating Scale. Pain = Numeric Pain Rating Scale. KA-SES = Knee Activity Self-Efficacy Scale. K-SES-DA = Knee Self-Efficacy Scale for Daily Activities. K-SES-Sport = Knee Self-Efficacy Scale for Sports and Leisure Activities. K-SES-PA = Knee Self-Efficacy Scale for Physical Activities. K-SES-KF = Knee Self-Efficacy Scale for Knee Function in the Future. K-SES-Knee Self-Efficacy Scale (total score). MSERO = Modified Self-Efficacy for Rehabilitation Outcome. TSK-11 = Shortened version of the Tampa Scale for Kinesiophobia.
At the two-year follow-up, 16 of the 19 (84%) returned to their preinjury level of sports competition and 3 (16%) returned to a reduced level of sports participation (Table 5). At the two-year follow-up, only one participant suffered a reinjury. He returned to his previous level of sports participation and had a second ACL injury due to a non-contact injury playing basketball, where his knee twisted upon landing on an opponent's foot.
Table 5.
Return to Sport and Reinjury Outcomes.
| 2-Year Follow-up Data (n = 19) | |
| Returned to Preinjury Level of Sports Participation | Returned to Reduced Level of Sports Participation |
| n = 16 (84%) | n = 3 (16%) |
At the time of return to sport, measures for the IKDC, KOS-ADL, KOS-Sports, KA-SES, K-SES, and MSERO were all >90%. Typically, 90% is used as a long-term goal for patient reported outcomes in outpatient physical therapy. All participants, who completed their physical therapy, met that goal for reports related to activities of daily living and function. Median Marx score was 12 (out of a possible 16), indicating that the participants were running, cutting, decelerating, and pivoting 2-3 times per week. Median pain rating was 0 (out of 10). Average TSK-11 scores at return to sport were 15.52, with 11 being the best possible score.
DISCUSSION
Following ACLR, reasons for lower return to sport rates and high re-injury rates are multifactorial, but a rehabilitation program that does not fully prepare patients to participate in sport is a substantial modifiable factor. Our goal with this case series was to determine if a highly structured and criterion-based rehabilitation protocol that included progressive activity and required minimal equipment would provide equal or better return to previous level of sports participation and reinjury rates than those currently reported in the literature. Unfortunately, only 49% of the participants completed the rehabilitation progression. Despite numerous efforts to contact those that were lost to follow-up, the authors were unable to ascertain the reason why they stopped coming to physical therapy, whether or not they returned to sports participation, or if they suffered a reinjury. This did not allow for comparisons of between-group differences in the early phases of physical therapy in those that completed the full course of physical therapy and those that did not. However, each participant that completed their rehabilitation returned to some level of sports participation and 84% to their pre-injury level with only one re-injury. Although it is a small sample size, our return to sport and reinjury rates are similar, if not better than averages reported in the literature.
In the present study, specific objective criteria for strength and functional testing, including mastery of the previous phase's activities, were used to progress to the next phase as well as permit return to sports participation. Various reviews have been published looking at the requirements and factors used in return to sport decision making following ACLR. Time after surgery is listed as the primary factor and some studies do not include any criteria used to clear patients for return to sports participation. A small number included strength and hop tests in their criteria.56-58 The European Board of Sport Rehabilitation recommended including strength and hop testing to ensure some basic levels of performance.59 The goal was to include objective assessments in conjunction with time after surgery to determine readiness to return to sports participation.
This protocol uses time after surgery, strength and functional assessments, as well as physician clearance (based on their exam) to clear a participant to return to a running program. Rambaud et al60 reviewed the criteria used to permit the return to running after ACL reconstruction. Of the 201 included studies, 198 (99%) used time after surgery as part of or the only criteria used to start running. Thirty studies (15%) used a strength assessment as criteria and 13 (6%) used a performance test as part of the criteria. The authors postulated the possibility that time after surgery is thought of as the only necessary criteria for return to running but that there is a lack of valid and reliable ways to assess readiness to return to running. 1-RM testing on a knee extension machine has excellent interrater/intrarater reliability (ICC = 0.90 and 0.96)61 and Piva et al.23 reported moderate values of reliability with assessing the quality of movement with a step-down task. The authors of the current study chose to implement a single leg squat and step and hold test as they are more closely related to the mechanics of running but chose to use Piva's criteria to assess quality for standardization. In addition, running greatly increases loads on the knee joint compared to walking, so we implemented a fast walking assessment to ensure that the knee could tolerate more loading without increases in inflammation. The participants’ surgeons preferred to delay starting to run until four months after surgery, with the rule of no sooner than three months. The participants were required to meet all the functional criteria to begin running before the surgeon would be agreeable to it. Coincidentally, this did occur at an average of four months. The median time to return to running reported by Rambaud et al60 was 12 weeks. The authors of the current study advocate including the use of objective strength and functional testing in addition to time after surgery for clearance to start running.
Time to return to sport can vary across studies following ACLR. In the present study, average time to complete physical therapy, pass the return to sport test, and be cleared by the physician was 10.6 months. Grindem et al.62 assessed 106 participants as part of the Delaware-Oslo ACL cohort who intend to return to level I or II sports. Seventy-four of the 83 (89%) participants who previously participated in Level I sports returned to their pre-injury level of participation within two years of ACLR, with a median of eight months. It was interesting however, that only 18 of the 74 (24%) that returned to level I sports participation actually passed their RTS test. By requiring the use of a criterion-based rehabilitation protocol, used in conjunction with time after surgery, the course of physical therapy lasted 2 months longer than what was reported by Grindem et al.62
Of the 19 participants that completed their course of physical therapy, passed their RTS test, and were available for the two-year follow-up, only one participant sustained a reinjury (11%). This number is below the reported data of those sustaining an ipsilateral or contralateral reinjury following ACLR. 6-9 It has been reported that for every month up to nine months that return to sport was delayed, participants had a reduced reinjury rate of 51%. In that same study, 21 (38%) of the 55 participants who failed RTS criteria suffered a reinjury whereas only one of the 18 (5.6%) who passed RTS testing suffered a reinjury. This reinforces the importance of having and passing objective testing in addition to waiting at least nine months to return to sport. The average time for return to sports participation in our study was 10.6 months. Kyritsis et al.51 assessed 158 professional male athletes for the likelihood of ACL graft rupture after return to sport. A battery of strength and functional tests was used to determine discharge criteria, which was >90% LSI for quadriceps strength and hop tests, full completion of on-field sports-specific rehabilitation and <11 seconds for a running T-test. The results showed that athletes not meeting the discharge criteria before returning to professional sport had a four times greater risk of sustaining an ACL graft rupture compared to those that met all six RTS criteria.
Paterno et al.63 recently reported that TSK-11 scores ≥ 17 were four times more likely to report lower levels of activity and scores ≥19 at the time of RTS were 13 times more likely to suffer a second ACL injury within two years after RTS. Participants in the current study who completed their physical therapy had a mean TSK-11 score of 15.52 which is below this threshold and thus, were likely to have a higher activity level and not suffer a second ACL injury within two years after RTS, per Paterno et al.63
Schmitt et al found that >15% asymmetries in quadriceps strength at the time of return to sport are associated with worse performance on measures of function and performance in young, active individuals following ACL reconstruction. It was also found that those with quadriceps strength deficits less than 10% demonstrated functional performance64 and movement patterns with walking and jogging similar to uninjured individuals.65 It has been shown that using a battery of tests, as opposed to just one, is better able to discriminate strength differences between the involved and uninvolved leg after ACL reconstruction.59,66,67 The authors of the current study chose strength assessments that utilized equipment found in most physical therapy clinics and high schools to which athletic trainers would have access. This included isolating the quadriceps with a knee extension machine, measuring total lower extremity strength with a leg press, and a dynamic test with motor control qualities in the single leg squat.
Participants in this study had a variety of graft types including bone-patellar tendon-bone (BPTB), hamstring, or quadriceps autografts, or soft tissue allografts. Some also had concomitant cartilage, ligamentous, or meniscal procedures, as well as revision ACL reconstructions. To the authors’ knowledge, this is the first paper to summarize return to sport and reinjury outcomes that did not exclude participants based on graft type, single vs double bundle procedure, ACL revision surgeries, nor concomitant procedures or injuries. Of the participants that completed PT and returned to sport, Table 1 shows that 16 (80%) received an autograft and 4 (20%) received an allograft. The most commonly used autografts were a BPTB (35%) and a quadriceps tendon (30%). There was not a statistically significant difference in graft type or concomitant procedures between individuals who completed the study versus those who did not complete the study. Of the group that completed the study, 12 (57%) had an associated meniscus procedure, 2 (10%) had an associated cartilage procedure, and 4 (19%) had an associated ligament procedure. All graft types and concomitant procedures were included because so few patients have an isolated ACLR and graft selection continues to evolve. The authors designed a protocol to have the most possible external validity, especially considering concomitant procedures and graft type typically influence the rehabilitation process the most during the immediate post-operative phase. Once the decision has been made to allow a patient to begin running, surgery specific factors are considerably less important than patient performance.
A question that remains is how to best prepare athletes to return to sports participation and ultimately their previous level of performance following ACL reconstruction. The majority of patients are given a predetermined set of physical therapy visits covered by insurance, which presents case management challenges. If ROM and/or strength impairments persist in the early phases of rehabilitation, more visits need to be utilized to prevent complications such as arthrofibrosis68 which means fewer are available for subsequent functional training. Some clinics offer cash-based physical therapy services or group exercise programs to bridge the gap from rehabilitation to training. Many high school and collegiate athletes also work with their athletic trainer. Collaboration between the physical therapist and athletic trainer allows for a higher volume of treatment sessions, both during the acute management period and during sport specific training. Having clearly defined criteria for progression should improve the consistency of care, regardless of provider. The authors also advocate entering an ACL injury prevention program following clearance to return to sport. A structured program of plyometrics, neuromuscular and sport specific training will help bridge the gap between returning to sports participation and reaching the previous level of performance.
The number of participants that were lost to follow-up is a substantial limitation of this study. Twenty-two participants (51%) did not complete the full course of rehabilitation. Despite numerous efforts, participants were not able to be contacted to ascertain the reason for self-discharge. Changes in lifestyle, such as wishing to no longer participate in competitive sports, the financial burden of insurance co-payments, time required for physical therapy appointments, dissatisfaction with physical therapy services, or participants becoming satisfied with their knee function and no longer wish to continue physical therapy may have led to the self-discharges. This has changed the authors clinical practice and led to having more discussions with patients about their goals and motivations throughout the course of care. Two participants (10%) that completed rehabilitation were not able to be reached for their two-year follow-up. This did not allow for reporting on return to sports participation status nor reinjury occurrence data on them.
After this protocol was created, Sinacore et al.69 demonstrated that 1-RM knee extension testing was a fair alternative to isokinetic testing but that it overestimated quadriceps strength. He also found that 1-RM testing on the leg press should not be used to assess quadriceps strength in the absence of isokinetic testing. If 1-RM knee extension testing is going to be used to assess for >80% quadriceps strength on isokinetic testing, 83% LSI should be used. Similarly, a 96% LSI should be the criteria when the goal is >90% quadriceps strength on isokinetic dynamometry. The 1-RM on the leg press involved all of the lower extremity muscles but overestimated quadriceps strength and resulted in poor specificity for identifying individuals who had not achieved the criteria for advancing activity according to an electromechanical dynamometer (gold standard). Therefore, the authors recommend that clinicians not utilize a leg press as a surrogate measure for quadriceps strength, but instead utilize a leg extension machine (90-45 °) and increase the threshold for quadriceps LSI values to inform return to running (83% versus traditional 80%) and to return to sports participation (96% versus traditional 90%).
CONCLUSION
The present case series is the first, to the authors’ knowledge, to evaluate a criterion-based rehabilitation program following ACL reconstruction that utilizes minimal equipment and does not exclude participants based on graft type used, or those with concomitant injuries or procedures. Sixteen participants (84%) returned to their preinjury level of sports participation. This is a higher percentage than reported by Ardern3 but attention should be drawn to the small sample size, as return to sports participation data was not available on 28 initially enrolled participants. Only one of the 16 (6%) suffered a reinjury in the two years following surgery, which is a smaller percentage compared to previously reported data.70-73 For those that completed the program and returned to sport, participant reported outcomes demonstrated high levels of function in activities of daily living, sports participation and low levels of pain and fear of movement. The authors propose that this protocol serve as a foundation for future research that utilizes a criterion-based program that requires minimal equipment and does not exclude participants based on graft type or previous injuries.
Appendix A
Anterior Cruciate Ligament Reconstruction Functional Rehabilitation Protocol
Activities of Daily Living Guidelines Following Surgery
Patients may begin the following activities at the timeframes indicated (unless otherwise specified by the physician):
No bathing or submerging the wound in water until the sutures have been removed, the scabs have fallen off, and the skin is completely closed.
Showering is allowed after the surgical dressing is removed; a waterproof dressing is not needed as the incision can get wet. A shower seat is advised to avoid falls.
The brace will be locked in extension for gait and sleep for the first week.
Use of crutches and brace for ambulation for 4-6 weeks. Must be cleared by physician and/or physical therapist to begin walking without assistive devices.
Weight-bearing as tolerated immediately after surgery unless otherwise instructed.
- For R knee surgery, no driving for 4-6 weeks. As long as they are in the brace, patients are medically liable if in an accident. For L knee surgery, patients may drive after 1 week as long as they have an automatic and have stopped taking narcotics.
- Must pass driving test for R knee: While sitting, complete 8 fast foot taps over shoe then stand up
Brace and Crutch Use Guidelines
Patients will be WBAT after surgery. The post-operative brace is locked in extension initially for the first week with the exception that it may be unlocked for post-op exercises and continuous passive motion (CPM) machine use. It is unlocked for walking once the patient reaches full knee hyperextension, usually 1 week post-op.
BRACE IS DISCONTINUED WHEN:
The patient is at least 4-6 weeks post-op
- The patient has full and equal passive and active knee hyperextension and >100 ° flexion
- Active knee extension is measured via straight leg raise
The patient demonstrates normal pain-free walking without an increase in swelling
CRUTCHES ARE DISCONTINUED WHEN:
The patient will initially be WBAT with 2 crutches for 4 weeks; they will then transition to one crutch before walking without the crutches over the next 2 weeks
The patient has full and equal passive and active knee hyperextension and >100 ° flexion
The patient is able to walk and maintain the knee in full extension without use of assistive device (i.e. does not walk with “bent knee” gait pattern)
The patient has no increased knee pain or swelling with independent weightbearing
Special weightbearing guidelines for concomitant procedures
The brace will be worn at least 6 weeks for combined ACL/MCL procedures, concomitant meniscal repairs, and microfracture procedures
MENISCUS REPAIR: Patients that also undergo a meniscus repair procedure will be NWB for 4 weeks, 50% WB for 2 weeks, then WBAT after 6 weeks
MICROFRACTURE or ARTICULAR CARTILAGE PROCEDURE: Patients that also undergo a microfracture or articular cartilage procedure will be NWB for 4 weeks, 50% WB for 2 weeks, then WBAT after 6 weeks
Estimated Return to Sport Milestones (based on graft healing time and passing functional testing):
| Jogging | Low-level Agility | Jumping | Cutting | Return to Sport | |
|---|---|---|---|---|---|
| Bone-Patellar Tendon-Bone Autograft | 4-5 months | 5-6 months | 6-7 months | 7-8 months | 9 + months |
| Hamstring/Quad Tendon Autograft | 4-5 months | 5-6 months | 6-7 months | 7-8 months | 9 + months |
| Bone-Patellar Tendon-Bone Allograft | 5-6 months | 6-7 months | 7-8 months | 8-9 months | 10 + months |
| Soft Tissue Allograft | 5-6 months | 6-7 months | 7-8 months | 8-9 months | 10-12 + months |
These times are estimated based on graft healing and are dependent upon the patient passing functional testing in physical therapy that assesses strength and neuromuscular control. These times may be longer if the patient also had a concomitant procedure such as a meniscal repair, microfracture/articular cartilage procedure and other ligament injury or procedure.
Phase 1: Initial Post-Op Care
Goals for Phase 1 include restoration of ROM and mobility, management of pain and edema, and initiation of strengthening with emphasis on the quadriceps. The post-operative brace may be removed for treatment. Closed kinetic chain (CKC) exercises should initially be performed in the range of 0-45 ° of flexion and open kinetic chain (OKC) knee extension exercises should stay in the protected range of 90-60 ° of flexion. Exercises should include but are not limited to:
Weeks 1-4:
4-way patella mobilization
High intensity neuromuscular electrical stimulation
Exercises to regain hyperextension – hamstring and gastrocnemius stretching, prone hang, manual overpressure, seated heel props with bag hang and/or with cuff weights
- Exercises to regain full flexion – heelslides, posterior tibial mobilizations
- Flexion is limited to 90 ° for 4 weeks with concomitant meniscus repairs
Early strengthening – quad sets in full knee hyperextension, 4-way straight leg raises, terminal knee extension (CKC), mini-squats, isometric quadriceps setting at 90 ° and 60 ° of knee flexion
Balance and proprioception exercises – progressing from weight shifting during bilateral stance progressing to unilateral stance exercises on stable and unstable surfaces, with eyes open and eyes closed
Gait training – weight-shifts (side to side and forward/backward)
Progress strengthening to include – leg press (single leg), OKC knee extension from 90-60 ° with ankle cuff weights, step-ups, step-downs, bridges, hamstring curls, wall slides
No OKC hamstring curls with concomitant meniscal repair or hamstring autograft for first 6 weeks
Goals at 2 weeks post-op include:
Passive and active hyperextension (as measured when doing a straight leg raise) should be equal to the uninvolved side and flexion >100 °
Reduced pain and swelling (rated 2 + or less via Stroke Test)
If SLR doesn't reach neutral extension (0 °) by 2 weeks post-op, increase frequency of PT and notify the physician
Goals at 4 weeks post-op include:
Full flexion (unless ROM restriction from concomitant meniscus repair)
No active inflammation (i.e. no increased pain, swelling or warmth) as a result of exercise. Swelling should be rated 1 + or less via Stroke Test
Preparation for full weightbearing and independent gait
The patient's visit frequency will be set by the PT for 1-3 times per week. If the patient is not meeting the range of motion milestones or if they are having difficulty with regaining quadriceps control/have a knee extensor lag, the physician should be notified and visit frequency should increase.
Weeks 4-16:
Stretching
Cardio – bike, elliptical
Gait training on treadmill progressing to fast treadmill walking
Aquatic therapy (if available)
Progress lower extremity strengthening, with emphasis on quadriceps
Perturbation training
Weeks 12-20:
CKC exercises should be progressed to ∼60-75 ° of knee flexion provided that this does not cause any patellofemoral pain.
OKC exercises should be progressed to full range 90-0 ° provided that this does not cause any patellofemoral pain.
Prepare to pass screening exam to begin running
Goal at 4-6 months post-op (depending on graft type): PASS SCREENING TEST TO BEGIN RUNNING
No abnormal gait patterns while walking as fast as they can on the treadmill for 15 minutes
30 step and holds without loss of balance or excessive motion outside of the sagittal plane
10 consecutive single leg squats to 45 ° of knee flexion without loss of balance, abnormal trunk movement, Trendelenburg sign, femoral IR or the knee deviating medially causing the tibial tuberosity to cross an imaginary vertical line over the medial border of the foot
≥ 80% 1-repetition maximum (1-RM) on the leg press (90-0 °)
≥ 80% 1-repetition maximum (1-RM) on the knee extension machine (90-45 °)
≥ 90% composite score on Y-balance test. Composite score = (anterior reach + posteromedial reach + posterolateral reach)/(3 x limb length)
Phase 2: Running
Begin jogging on a treadmill or a track when the patient passes the screening exam AND is cleared by the physician. Running should begin at slow, comfortable speeds for short durations and distances. The patient may progress in speed, time and distance as long as there is no development or increase in pain, swelling, warmth, or gait deviations. See Running Progression Guidelines handout.
The patient should be seen by the physical therapist once every 2-3 weeks while running tolerance and endurance progresses. Aggressive strengthening should continue in preparation to pass the screening test to begin agility drills.
Patients who undergo a Quadriceps tendon autograft with bone plug will need an x-ray at their 6 month post-op visit in order to be cleared for electromechanical dynamometer testing to ensure healing of the harvest site.
Goals at 5-7 months post-op: PASS SCREENING TEST TO BEGIN
LOW-LEVEL AGILITY DRILLS
≥ 85% 1-RM on the leg press (90-0 °)
≥ 85% 1-RM on the knee extension machine (90-0 °) or Biodex testing if available
10 consecutive single leg squats >45 ° of knee flexion without loss of balance, abnormal trunk movement, Trendelenburg sign, femoral IR or the knee deviating medially causing the tibial tuberosity to cross an imaginary vertical line over the medial border of the foot while holding ≥ 75% extra weight compared to the other side (dumbbells, weight vest, etc.) Body weight is not part of the equation
100% composite score on Y-balance test. Composite score = (anterior reach + posteromedial reach + posterolateral reach)/(3 x limb length)
Be able to run 2 miles continuously without pain, swelling, warmth or gait deviations
Phase 3: Agility Training
When the patient passes the screening exam AND is cleared by the physician, they may begin agility drills that include lateral shuffling, forward/backward shuttle runs, carioca, and ladder drills.
Physical therapy should focus on elimination of compensation patterns, particularly when the patient decelerates. Aggressive strengthening should continue in preparation to pass the screening test to begin jumping.
Goals at 6-8 months post-op: PASS SCREENING TEST TO BEGIN JUMPING
≥ 90% 1-RM on the leg press (90-0 °)
≥ 90% 1-RM on the knee extension machine (90-0 °) or Biodex testing if available
10 consecutive single leg squats to 60 ° of knee flexion without loss of balance, abnormal trunk movement, Trendelenburg sign, femoral IR or the knee deviating medially causing the tibial tuberosity to cross an imaginary vertical line over the medial border of the foot while holding ≥ 85% extra weight compared to the other side (dumbbells, weight vest, etc.). Body weight is not part of the equation
No compensation patterns with deceleration during agility drills performed at near 100% effort
Phase 4: Jumping (Two Feet)
When the patient passes the screening exam AND is cleared by the physician, begin jumping. Jumping is with 2 feet, both taking off and landing.
Jumps should start with single vertical jumps and the physical therapist should watch for medial collapse of the knees both when loading into the jump and landing from the jump. When the patient demonstrates consistent equal weightbearing when landing, progress with forward, side to side, rotating, and box jumps. As the patient demonstrates consistent good form, progress from single jumps to consecutive jumps.
Physical therapy should focus on teaching the patient soft, athletic landings and avoidance of compensation strategies. Aggressive strengthening should continue in preparation to pass the screening test to begin hopping and cutting.
Goals at 7-9 months post-op: PASS SCREENING TEST TO BEGIN CUTTING AND HOPPING
10 consecutive single leg squats to 60 ° without loss of balance, abnormal trunk movement, Trendelenburg sign, femoral IR or the knee deviating medially causing the tibial tuberosity to cross an imaginary vertical line over the medial border of the foot while holding ≥ 90% extra weight compared to the other side (dumbbells, weight vest, etc.). Body weight is not part of the equation
No display of medial collapse of the knees when loading into or landing from jumps, and equal weight distribution when initiating and landing the jumps
Phase 5: Hopping (Single Leg) and Cutting
When the patient passes the screening exam AND is cleared by the physician, they may begin hopping and cutting. Hopping is with 1 foot, both taking off and landing. Hopping should follow the same progression as jumping.
Patients should first practice running in an “S” pattern, then progress to 45 ° cuts, and then to sharper angles. Pivoting and cut and spinning should begin when the patient is competent with cutting at sharp angles. Patients should be able to tolerate cutting, pivoting and cut and spinning at full speed before practicing unanticipated cutting. The patient should not progress their speed if they demonstrate any excessive knee medial deviation or express a lack of confidence when cutting.
Sprinting should begin with transitions from running directly into sprinting short distances. Distance should be progressed to sprinting a 40 yard dash, then a 100 yard dash, and finally sprints to fatigue.
Physical therapy should focus on improving the form and speed of hopping and cutting. Aggressive strengthening should continue in preparation to return to sports participation.
Goals at 9-12 months: PREPARE TO TAKE RETURN TO SPORTS TEST
Display a normal running pattern that does not increase pain, swelling, or warmth
Practice and display no hesitation or compensation strategies during agility drills (particularly when decelerating) when performed at 100% effort
Practice and display normal loading (no medial knee collapse) and soft, athletic landings from all jumps and hops
Practice and display no hesitation or compensation strategies during cutting drills (particularly when decelerating) when performed at perceived 100% effort
Returning to Sports Participation
The patient should be able to perform all agility, plyometric, and cutting exercises at full speed without compensation patterns or complaints of pain, swelling, or warmth. Exercises should include anticipated and unanticipated cutting and jumping.
Physical therapy should be geared on sport specific training as per the patient's sport and position.
The patient may return to sports participation when they pass the ACL Return to Sports Test AND receive clearance by the physician.
Anterior Cruciate Ligament Reconstruction Return to Sport Test
Name: ____________________________________________________ Date:_________________
Single broad jump, landing on one foot - Involved/Uninvolved Distance = _______/_______ = _______
Triple broad jump, landing last jump on one foot –
Involved/Uninvolved Distance = _______ /_______ = _______
Single leg forward hop - Involved/Uninvolved Distance = _______ /_______ = _______
Single leg triple hop - Involved/Uninvolved Distance = _______ /_______ = _______
Single leg triple crossover hop - Involved/Uninvolved Distance = _______ /_______ = _______
Timed 6-meter single leg hop – Uninvolved/Involved Time = _______ /_______ = _______
Single leg lateral hop - Involved/Uninvolved Distance = _______ /_______ = _______
Single leg medial hop - Involved/Uninvolved Distance = _______ /_______ = _______
Single leg medial rotating hop - Involved/Uninvolved Distance = _______ /_______ = _______
Single leg lateral rotating hop - Involved/Uninvolved Distance = _______ /_______ = _______
Single leg vertical hop - Involved/Uninvolved Height = _______ /_______ = _______
- 10 yard Lower Extremity Functional Test
- Sprint/back-peddle, Shuffle, Carioca, Sprint
- Must perform at perceived full speed and not display hesitation or compensation strategies when decelerating
- Recommended goal for males: 18-22 seconds; females: 20-24 seconds
- 10 yard Pro-agility Run
- Both directions
- Must perform at perceived full speed and not display hesitation or compensation strategies when decelerating
- Recommended goal for males: 4.5-6.0 seconds; females: 5.2-6.5 seconds
Criteria to Return to Practice:
MD clearance
Pass Return to Sport Test with ≥90% results for each test.
Criteria to Return to Competition:
MD clearance
Tolerate full practice sessions with opposition and contact (if applicable) performed at 100% effort without any increased pain, increased effusion, warmth, or episodes of giving way.
REFERENCES
- 1.Gornitzky AL Lott A Yellin JL Fabricant PD Lawrence JT Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med. 2016; 44(10): 2716-2723. [DOI] [PubMed] [Google Scholar]
- 2.Griffin LY Agel J Albohm MJ et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000; 8(3): 141-150. [DOI] [PubMed] [Google Scholar]
- 3.Ardern CL Taylor NF Feller JA Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012; 40(1): 41-48. [DOI] [PubMed] [Google Scholar]
- 4.Ardern CL Webster KE Taylor NF Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011; 45(7): 596-606. [DOI] [PubMed] [Google Scholar]
- 5.Ardern CL Webster KE Taylor NF Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011; 39(3): 538-543. [DOI] [PubMed] [Google Scholar]
- 6.van Eck CF Schkrohowsky JG Working ZM Irrgang JJ Fu FH. Prospective analysis of failure rate and predictors of failure after anatomic anterior cruciate ligament reconstruction with allograft. Am J Sports Med. 2012; 40(4): 800-807. [DOI] [PubMed] [Google Scholar]
- 7.Lai CCH Ardern CL Feller JA Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018; 52(2): 128-138. [DOI] [PubMed] [Google Scholar]
- 8.Myer GD Martin Jr L Ford KR et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012; 40(10): 2256-2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paterno MV Ford KR Myer GD Heyl R Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sports Med. 2007; 17(4): 258-262. [DOI] [PubMed] [Google Scholar]
- 10.Anderson AF Irrgang JJ Kocher MS Mann BJ Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006; 34(1): 128-135. [DOI] [PubMed] [Google Scholar]
- 11.Irrgang JJ Anderson AF Boland AL et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001; 29(5): 600-613. [DOI] [PubMed] [Google Scholar]
- 12.Irrgang JJ Snyder-Mackler L Wainner RS Fu FH Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998; 80(8): 1132-1145. [DOI] [PubMed] [Google Scholar]
- 13.Marx RG Jones EC Allen AA et al. Reliability, validity, and responsiveness of four knee outcome scales for athletic patients. J Bone Joint Surg Am. 2001; 83(10): 1459-1469. [DOI] [PubMed] [Google Scholar]
- 14.Chhabra A Cha PS Rihn JA et al. Surgical management of knee dislocations. Surgical technique. J Bone Joint Surg Am. 2005; 87 Suppl 1(Pt 1): 1-21. [DOI] [PubMed] [Google Scholar]
- 15.Marx RG Stump TJ Jones EC Wickiewicz TL Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001; 29(2): 213-218. [DOI] [PubMed] [Google Scholar]
- 16.Cleland JA Childs JD Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008; 89(1): 69-74. [DOI] [PubMed] [Google Scholar]
- 17.Mintken PE Glynn P Cleland JA. Psychometric properties of the shortened disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009; 18(6): 920-926. [DOI] [PubMed] [Google Scholar]
- 18.Jones D Rivett J Wolfe M Chmielewski T. The association of fear of movement/reinjury and self-efficacy with function in patients after knee injury. Orthop Pract. 2008; 20: 193-199. [Google Scholar]
- 19.Thomee P Wahrborg P Borjesson M Thomee R Eriksson BI Karlsson J. A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sport. 2006; 16(3): 181-187. [DOI] [PubMed] [Google Scholar]
- 20.Waldrop D Lightsey Jr OR Ethington CA Woemmel CA Coke AL. Self-efficacy, optimism, health competence, and recovery from orthopedic surgery. J Counsel Psych. 2001; 48(2): 233-238. [Google Scholar]
- 21.Woby SR Roach NK Urmston M Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005; 117(1-2): 137-144. [DOI] [PubMed] [Google Scholar]
- 22.George SZ Lentz TA Zeppieri Jr G Lee D Chmielewski TL. Analysis of shortened versions of the Tampa Scale for Kinesiophobia and Pain Catastrophizing Scale for patients following anterior cruciate ligament reconstruction. Clin J Pain. 2012; 28(1): 73-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piva SR Fitzgerald K Irrgang JJ et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musc Disorders. 2006; 7(1): 33-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gribble PA Hertel J Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012; 47(3): 339-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Herrington L Hatcher J Hatcher A McNicholas M. A comparison of Star Excursion Balance Test reach distances between ACL deficient patients and asymptomatic controls. Knee. 2009; 16(2): 149-152. [DOI] [PubMed] [Google Scholar]
- 26.Abernethy P Wilson G Logan P. Strength and power assessment-issues controversies and challenges. Sports Med. 19(6): 401-419. [DOI] [PubMed] [Google Scholar]
- 27.Verdijk LB Van Loon L Meijer K Savelberg HH. One-repetition maximum strength test represents a valid means to assess leg strength in vivo in humans. J Sport Sci. 2009; 27(1): 59-68. [DOI] [PubMed] [Google Scholar]
- 28.Sinacore A Evans A Lynch B Joreitz R Irrgang JJ Lynch AD. Partial range of motion 1-repetition maximum testing of the quadriceps identifies strength asymmetries similar to full-range testing. J Orthop Sports Phys Ther. 2017; 47(1): A214. [DOI] [PubMed] [Google Scholar]
- 29.Joreitz R Lynch A Rabuck S Lynch B Davin S Irrgang J. Patient-specific and surgery-specific factors that affect return to sport after ACL reconstruction. Int J Sports Phys Ther. 2016; 11(2): 264. [PMC free article] [PubMed] [Google Scholar]
- 30.Di Stasi S Myer GD Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013; 43(11): 777-A711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hewett TE Di Stasi SL Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013; 41(1): 216-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hewett TE Myer GD Ford KR Paterno MV Quatman CE. The 2012 ABJS Nicolas Andry Award: The sequence of prevention: a systematic approach to prevent anterior cruciate ligament injury. Clin Orthop Rel Res. 2012; 470(10): 2930-2940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mandelbaum BR Silvers HJ Watanabe DS et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005; 33(7): 1003-1010. [DOI] [PubMed] [Google Scholar]
- 34.Myer GD Ford KR Brent JL Hewett TE. An integrated approach to change the outcome part II: targeted neuromuscular training techniques to reduce identified ACL injury risk factors. J Strength Cond Res. 2012; 26(8): 2272-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Risberg MA Holm I Myklebust G Engebretsen L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007; 87(6): 737-750. [DOI] [PubMed] [Google Scholar]
- 36.Knight KL. Quadriceps strengthening with the DAPRE technique: Case studies with neurological implications. J Orthop Sports Phys Ther. 1990; 12(2): 66-71. [DOI] [PubMed] [Google Scholar]
- 37.van Melick N van Cingel RE Brooijmans F et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016; 50(24): 1506-1515. [DOI] [PubMed] [Google Scholar]
- 38.Escamilla RF MacLeod TD Wilk KE Paulos L Andrews JR. ACL strain and tensile forces for weight-bearing and non-weight bearing exercises after ACL reconstruction: a guide to exercise selection. J Orthop Sports Phys Ther. 2012; 42(3): 208-220. [DOI] [PubMed] [Google Scholar]
- 39.Steinkamp LA Dillingham MF Markel MD Hill JA Kaufman KR. Biomechanical considerations in patellofemoral joint rehabilitation. Am J Sports Med. 1993; 21(3): 438-444. [DOI] [PubMed] [Google Scholar]
- 40.Piva SR Childs JD Klucinec BM Irrgang JJ Almeida GJ Fitzgeiald GK. Patella fracture during rehabilitation after bone-patellar tendon-bone anterior cruciate ligament reconstruction: 2 case reports. J Orthop Sports Phys Ther. 2009; 39(4): 278-286. [DOI] [PubMed] [Google Scholar]
- 41.Ratamess NA Alvar BA Evetoch TE et al. Progression models in resistance training for healthy adults. Med Sci Sports Exer. 2009; 41(3): 687-708. [DOI] [PubMed] [Google Scholar]
- 42.Adams D Logerstedt D Hunter-Giordano A Axe MJ Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012; 42(7): 601-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paterno MV Schmitt LC Ford KR et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010; 38(10): 1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bizzini M Hancock D Impellizzeri F. Suggestions from the field for return to sports participation following anterior cruciate ligament reconstruction: soccer. J Orthop Sports Phys Ther. 2012; 42(4): 304-312. [DOI] [PubMed] [Google Scholar]
- 45.Kokmeyer D Wahoff M Mymern M. Suggestions from the field for return-to-sport rehabilitation following anterior cruciate ligament reconstruction: alpine skiing. J Orthop Sports Phys Ther. 2012; 42(4): 313-325. [DOI] [PubMed] [Google Scholar]
- 46.Waters E. Suggestions from the field for return to sports participation following anterior cruciate ligament reconstruction: basketball. J Orthop Sports Phys Ther. 2012; 42(4): 326-336. [DOI] [PubMed] [Google Scholar]
- 47.Verstegen M Falsone S Orr R Smith S. Suggestions from the field for return to sports participation following anterior cruciate ligament reconstruction: American football. J Orthop Sports Phys Ther. 2012; 42(4): 337-344. [DOI] [PubMed] [Google Scholar]
- 48.Fitzgerald GK Lephart SM Hwang JH Wainner MRS. Hop tests as predictors of dynamic knee stability. J Orthop Sports Phys Ther. 2001; 31(10): 588-597. [DOI] [PubMed] [Google Scholar]
- 49.Myer GD Schmitt LC Brent JL et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011; 41(6): 377-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reid A Birmingham TB Stratford PW Alcock GK Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007; 87(3): 337-349. [DOI] [PubMed] [Google Scholar]
- 51.Kyritsis P Bahr R Landreau P Miladi R Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016; 50(15): 946-951. [DOI] [PubMed] [Google Scholar]
- 52.Cascio BM Culp L Cosgarea AJ. Return to play after anterior cruciate ligament reconstruction. Clin Sport Med. 2004; 23(3): 395-408. [DOI] [PubMed] [Google Scholar]
- 53.Noyes FR Barber SD Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991; 19(5): 513-518. [DOI] [PubMed] [Google Scholar]
- 54.Stewart PF Turner AN Miller SC. Reliability, factorial validity, and interrelationships of five commonly used change of direction speed tests. Scand J Med Sci Sports. 2014; 24(3): 500-506. [DOI] [PubMed] [Google Scholar]
- 55.Hoffman J. NSCA's Guide to Program Design. Human Kinetics; 2011.
- 56.Barber-Westin SD Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011; 27(12): 1697-1705. [DOI] [PubMed] [Google Scholar]
- 57.Harris JD Abrams GD Bach BR et al. Return to sport after ACL reconstruction. Orthopedics. 2014; 37(2): e103-e108. [DOI] [PubMed] [Google Scholar]
- 58.Burgi CR Peters S Ardern CL et al. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br J Sports Med. 2019; 53(18): 1154-61. [DOI] [PubMed] [Google Scholar]
- 59.Thomeé R Kaplan Y Kvist J et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumat Arthrosc. 2011; 19(11): 1798-1805. [DOI] [PubMed] [Google Scholar]
- 60.Rambaud AJ Ardern CL Thoreux P Regnaux J-P Edouard P. Criteria for return to running after anterior cruciate ligament reconstruction: a scoping review. Br J Sports Med. 2018; 52(22): 1437-1444. [DOI] [PubMed] [Google Scholar]
- 61.Kvist J. Intra-and interrater reliability of the establishment of one repetition maximum on squat and seated knee extension. J Strength Cond Res. 2007; 21(3): 801-807. [DOI] [PubMed] [Google Scholar]
- 62.Grindem H Snyder-Mackler L Moksnes H Engebretsen L Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016; 50(13): 804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Paterno MV Flynn K Thomas S Schmitt LC. Self-Reported Fear Predicts Functional Performance and Second ACL Injury After ACL Reconstruction and Return to Sport: A Pilot Study. Sports Health. 2018; 10(3): 228-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Schmitt LC Paterno MV Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012; 42(9): 750-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lewek M Rudolph K Axe M Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech. 2002; 17(1): 56-63. [DOI] [PubMed] [Google Scholar]
- 66.Gustavsson A Neeter C Thomeé P et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumat Arthrosc. 2006; 14(8): 778-788. [DOI] [PubMed] [Google Scholar]
- 67.Neeter C Gustavsson A Thomeé P Augustsson J Thomeé R Karlsson J. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg Sports Traumat Arthrosc. 2006; 14(6): 571-580. [DOI] [PubMed] [Google Scholar]
- 68.Shelbourne KD Patel DV Martini DJ. Classification and management of arthrofibrosis of the knee after anterior cruciate ligament reconstruction. Am J Sports Med. 1996; 24(6): 857-862. [DOI] [PubMed] [Google Scholar]
- 69.Sinacore JA Evans AM Lynch BN Joreitz RE Irrgang JJ Lynch AD. Diagnostic accuracy of handheld dynamometry and 1-repetition-maximum tests for identifying meaningful quadriceps strength asymmetries. J Orthop Sports Phys Ther. 2017; 47(2): 97-107. [DOI] [PubMed] [Google Scholar]
- 70.Shelbourne KD Gray T Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. The Am J Sports Med. 2009; 37(2): 246-251. [DOI] [PubMed] [Google Scholar]
- 71.Salmon L Russell V Musgrove T Pinczewski L Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005; 21(8): 948-957. [DOI] [PubMed] [Google Scholar]
- 72.Leys T Salmon L Waller A Linklater J Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012; 40(3): 595-605. [DOI] [PubMed] [Google Scholar]
- 73.Pinczewski LA Lyman J Salmon LJ Russell VJ Roe J Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007; 35(4): 564-574. [DOI] [PubMed] [Google Scholar]