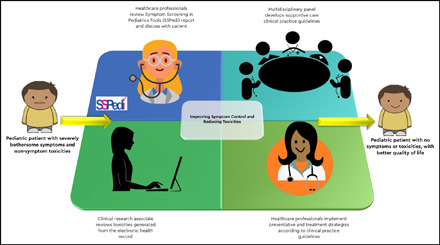
Visual Abstract
Abstract
The continuing improvement in pediatric cancer survival over time is largely attributable to the availability of intensive therapies. Increasing attention has been focused on addressing the physical and psychosocial impacts of cancer and cancer treatments. Evidence from adult oncology suggests that routine symptom screening and feedback to health care providers can improve patient-clinician communication, reduce distress, and improve quality of life and may even increase survival. Many questions remain regarding implementation of routine symptom screening in pediatric cancer care, including the best symptom assessment instrument and the reporter type and feasibility of integration with electronic health records (EHRs). Nonsymptom adverse events are also important, for both routine clinical care and adverse event reporting for patients enrolled in clinical trials. However, traditional mechanisms for reporting adverse events lead to substantial inaccuracies and are labor intensive. An automated approach for abstraction from EHRs is a potential mechanism for improving accuracy and reducing workload. Finally, identification of symptom and nonsymptom toxicities must be paired with prophylactic and therapeutic strategies. These strategies should be based on clinical practice guidelines that synthesize evidence and use multiprofessional, multidisciplinary expertise to place this evidence in clinical context and create recommendations. How best to implement clinical practice guidelines remains a challenge, but EHR order sets and alerts may be useful. In summary, although survival is excellent for pediatric patients receiving cancer therapies, more focus is needed on identification of symptoms and nonsymptom toxicities and their management. The EHR may be useful for promoting better supportive care through these mechanisms.
Learning Objectives
Understand the importance of routine symptom screening for pediatric patients with hematological malignancies
Understand the importance of rigorously developed supportive care clinical practice guidelines
Clinical case
A 12-year-old girl who had completed chemotherapy for acute myeloid leukemia (AML) 6 months ago presented with bone marrow relapse and was enrolled in a clinical trial. She stated that she felt “terrible” during most of her initial treatment and asked whether this next treatment would make her feel even worse. Her parents were with her and asked whether there was anything that could be done to help her cope with the toxicities that they were expecting with the new treatment plan. During the first cycle of chemotherapy, she developed bacteremia and most likely had pulmonary aspergillosis. The clinical research associate was uncertain how to report these toxicities accurately.
Introduction
Pediatric cancer care has benefitted from decades of successive clinical trials, resulting in continual improvement in survival for children and adolescents with cancer. Currently, >82% of pediatric patients with cancer survive at least 5 years after diagnosis.1 Although precision medicine and targeted therapies are promising approaches,2 the foundation of pediatric cancer treatment remains conventional chemotherapy, surgery, and radiotherapy. There has been increasing recognition that these therapies have an adverse impact on pediatric patients and negatively affect their quality of life.3 Consequently, increasing attention has been turned toward addressing the physical and psychosocial effects of cancer and cancer treatments. This article focuses on measuring symptoms and nonsymptom toxicities, in the context of both routine care and clinical trials, and also addresses the implementation of evidence-based prophylactic and therapeutic strategies to reduce these toxicities.
Symptom screening in routine care
Evidence supporting the hypothesis that routine symptom screening could improve outcomes first emerged in the adult cancer literature. Observational studies suggested that routine collection of patient-reported outcomes would improve patient-clinician communication,4 reduce distress,5 and improve quality of life.6 The strongest evidence supporting the importance of routine symptom screening came from randomized trials. In one trial, 766 adults with metastatic solid tumors were randomized into a routine symptom screening group or a standard-of-care group. The routine symptom screening group reported 12 common symptoms at clinic visits, and those with computers also received weekly e-mail prompts. Patients in the intervention group had significantly improved quality of life, fewer emergency department visits, and fewer hospitalizations than those in the standard-of-care control group.6 In a follow-up analysis, median overall survival was 31.2 months (95% confidence interval, 24.5-39.6) in the routine symptom screening group vs 26.0 months (95% confidence interval, 22.1-30.9) in the standard-of-care group (P = .03).7 These studies set the stage for routine symptom screening in pediatric patients with cancer.
The choice of instrument to use for routine symptom screening has been addressed in 3 systematic reviews of system assessment scales used in pediatric patients with cancer.8-10 Scales most commonly used were the Memorial Symptom Assessment Scale (MSAS) 10-18, the MSAS 7-12, the Symptom Distress Scale, and the Symptom Screening in Pediatrics Tool (SSPedi). In the most recent systematic review,9 more than half of the identified studies involved electronic administration of the symptom assessment scale, which is likely to be well received in pediatric populations.
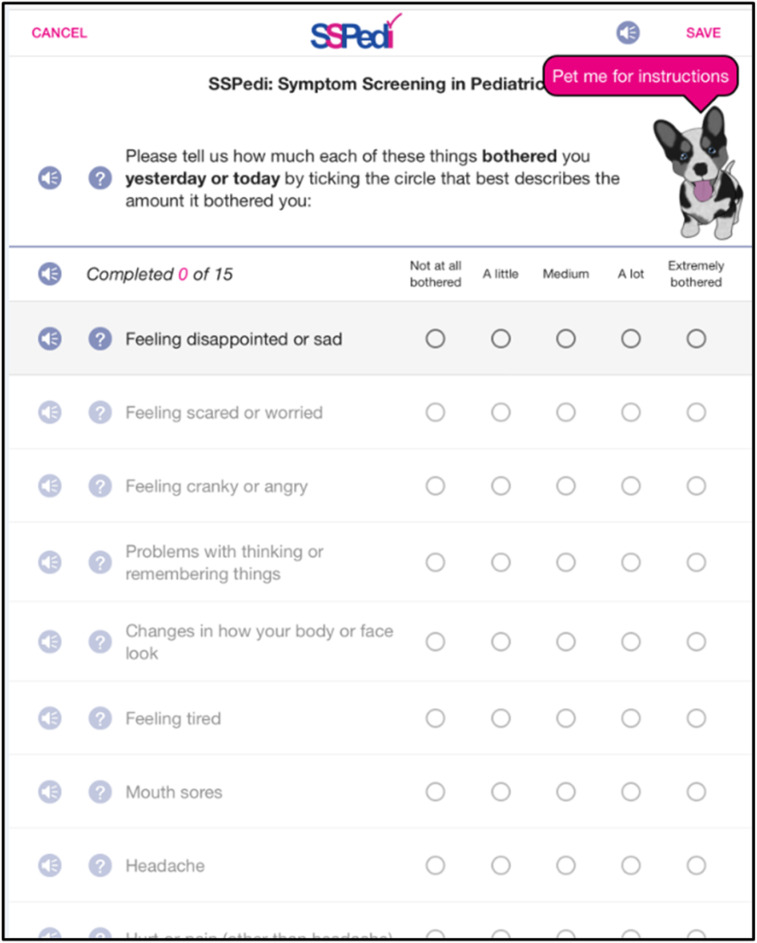
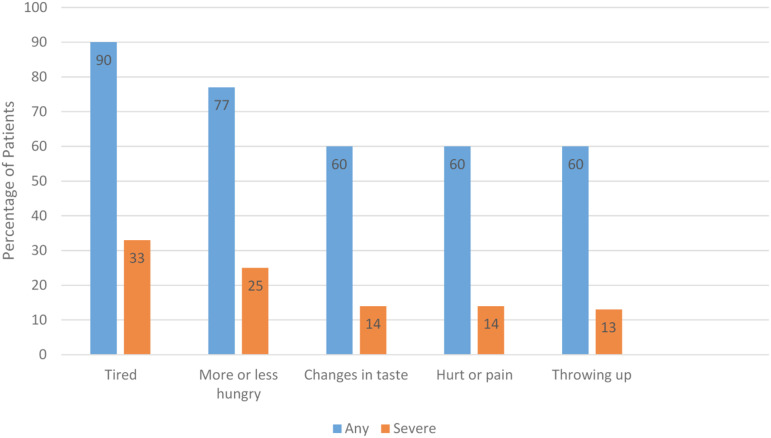
SSPedi is a self-reported, 15-item symptom screening tool created specifically for children receiving cancer treatments (Figure 1). It measures the extent of discomfort of 15 symptoms as follows: disappointment or sadness, fear or worry, cranky or angry disposition, problems with concentration or memory, bodily or facial changes, fatigue, mouth sores, headache, other pain, tingling or numbness, vomiting, changes in appetite, changes in taste, constipation, and diarrhea. SSPedi is available in paper-based and electronic formats, with the latter having an audio feature that provides oral reading of the entire instrument or specific questions. In a multicenter study conducted in Canada and the United States, SSPedi was reliable (internal consistency, test-retest reliability, and interrater reliability), valid (construct validity), and responsive to change in 502 English-speaking children 8 to 18 years of age who were receiving cancer therapies.3 It has been translated into Spanish and French.11 The most commonly reported bothersome symptoms are shown in Figure 2. A self-report version for children 4 to 7 years of age (mini-SSPedi12) and a proxy-report version for children 2 to 18 years of age13 have also been developed.
Figure 1.
Symptom screening in a pediatrics tool.
Figure 2.
Most common severely bothersome symptoms among inpatients 8 to 18 years of age. Adapted from Johnston et al.39
Once an instrument has been identified, an important question is whether it is the best reporter of the pediatric patient’s symptoms for clinical implementation. It has long been recognized that the patient is the best reporter of symptoms.14 However, in pediatric cancer care, there are many scenarios where pediatric patients either cannot or will not report their symptoms. Such scenarios include children who are too young, those with cognitive impairment, or those who are too ill.15 Thus, an ideal symptom screening approach must be flexible enough to allow for different types of reporter. We have proposed a novel method for symptom reporting that involves a structured dyadic approach. This approach may be particularly useful in young children.16 Whether the approach is feasible and valid, however, remains to be answered.
Another important issue is the mechanism by which symptoms are collected and reported to health care professionals, with the 2 broad options being stand-alone systems or integration into electronic health records (EHRs; Table 1). There are many advantages of incorporating symptom data into EHRs, such as efficiency of integration into the workflow of clinicians and ability to link documented symptoms to orders for intervention. Some vendors (eg, Epic Systems Corporation; Verona, WI) have developed programs that enable the capture of patient-reported outcomes. However, these programs generally have not had modules that are specific to pediatric patients. Advantages of using stand-alone systems include agility in development and modification and compatibility across health systems with programs from different EHR vendors.
Table 1.
Leveraging EHRs for symptom screening, identification of nonsymptom toxicities, and improving CPG-concordant care
| Target areas | Components |
|---|---|
| Facilitate symptom screening | Allow patient self-report or proxy report to track symptoms |
| Allow health care professionals to view symptom scores | |
| Automated capture of toxicities | Extraction of data directly from the EHR |
| Clean data to ensure complete data capture | |
| Remove false results | |
| Grade toxicities according to standard grading systems | |
| Enhance guideline-concordant supportive care | Order sets consistent with CPGs |
| Build alerts when symptoms or other toxicities are identified | |
| Incorporate management recommendations into alerts |
Finally, many practical questions remain to be addressed, including the ideal frequency for reminders, treatment periods during which symptoms should be elicited, and the best approach to providing results of symptom screening to health care professionals. These questions are likely to be addressed through the next generation of clinical trials. Nonetheless, the status of symptom screening in pediatric cancer is currently at the interface between research and clinical implementation, and this pendulum is likely to swing toward clinical implementation in the future.
Capturing nonsymptom toxicities in clinical practice and clinical trials
Capture of nonsymptom toxicities presents a range of different challenges. Documentation of toxicities by clinicians is crucial for understanding a patient’s experience during treatment. Identification of adverse events (AEs) has been guided for many trials and patients by the United States National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE).17 The CTCAE was developed in 1983 to standardize reporting of AEs across clinical trials.18-20 However, over time, it has increased in complexity, and the most recent version, CTCAE v5, includes more than 800 AEs.17,20 Although this complexity increases the potential for more granular reporting, it also raises concern about potential variation in approaches to identifying toxicities. Some individuals may report specific signs or symptoms, whereas others may report a syndrome that encompasses many individual toxicities. For example, tumor lysis syndrome could be reported as the syndrome; as individual components of hyperkalemia, hyperphosphatemia, hypocalcemia, and hyperuricemia; or as both. CTCAE may also be inappropriately used, depending on the subjective or complex nature of the definitions.21 Variation in reporting approaches and interpretation causes difficulties in determining accurate toxicity rates for specific chemotherapy regimens. Further, CTCAE definitions cause particular challenges for pediatric patients, despite the addition of pediatric-specific criteria beginning with CTCAE v3.0.20 For example, many CTCAE definitions rely on activities of daily living, which vary widely by age and patient, especially among children who meet developmental milestones at different ages.20
For patients enrolled in National Cancer Institute cooperative group trials, reporting of AEs is mandatory. AE rates reported from clinical trials may be the only source of information regarding the toxicity of specific chemotherapy combinations. In these circumstances, trial AE rates are the only data source that guides clinicians and patients regarding potential treatment-related toxicities. On clinical trials, AE capture is typically performed via manual medical record review and reporting by clinical research associates (CRAs). This process is labor intensive and is only one of many responsibilities that CRAs have.22 Studies have shown that, despite the effort devoted to it, toxicities are underreported.23,24 One study demonstrated that AE reports in a trial for pediatric AML had less than 50% sensitivity for 8 of 12 clinically relevant AEs when compared with the gold-standard chart abstraction.25 This underreporting means that clinicians do not have an accurate understanding of toxicity rates and therefore cannot truly prepare patients for potential toxicity during therapy. Further, phase 3 clinical trials typically report the highest grade of toxicity experienced during each chemotherapy course, but the grade may not fully represent the experience of the patient, especially those receiving prolonged oral chemotherapy, such as children with acute lymphoblastic leukemia who are in maintenance therapy. Efforts must be implemented to capture and describe toxicity profiles over time.
Similar to the benefits of using EHRs to collect symptom data from patients, EHRs may be leveraged to improve capture of nonsymptom toxicities recorded by clinicians (Table 1). Automated ascertainment that extracted laboratory data directory from the EHR, cleaned and processed the data, and graded laboratory-identified AEs according to CTCAE criteria had high accuracy at a single institution.26 This automated R package, ExtractEHR, was implemented at 3 hospitals to obtain laboratory result data and described accurate rates of laboratory-identified AEs by chemotherapy course for pediatric patients undergoing therapy for acute lymphoblastic leukemia or AML.27 Work is ongoing using the same package to capture non–laboratory-identified toxicities in pediatric patients with leukemia across multiple centers. Some institutions have integrated AE capture systems into the EHR to alert clinicians and track AEs over time, although no study on this approach has been published from pediatric centers.28 Trigger tools to alert clinicians to AEs have also been tested, but a recent study reported low positive predictive value when using a medication-based trigger.29 Further tailoring of such tools is needed realize clinical benefit.
Accurate capture of nonsymptom toxicities is crucial for understanding the patient’s experience and ultimately implementing measures to reduce toxicity. EHR-based ascertainment has the potential to standardize approaches to capture of AE and reduce the manual effort required for reporting. If implemented widely, this approach would improve accuracy and efficiency and free CRAs to capture more complex toxicities or to perform other responsibilities. This improved knowledge of AEs would also educate clinicians, improve identification of AEs for patients in clinical practice, and provide a resource clinicians can use to guide patients regarding toxicities that may occur during therapy.
Interventions to improve symptoms
Preventing toxicity and relieving symptoms is essential in the holistic care of children undergoing cancer therapy and their families. Delivering this care, triggered by symptom scores or toxicity assessment or by a predicted high probability that problems will occur, should be informed by the same high quality of evidence that underpins cancer care. This belief is the basis for the development of high-quality supportive care clinical practice guidelines (CPGs).
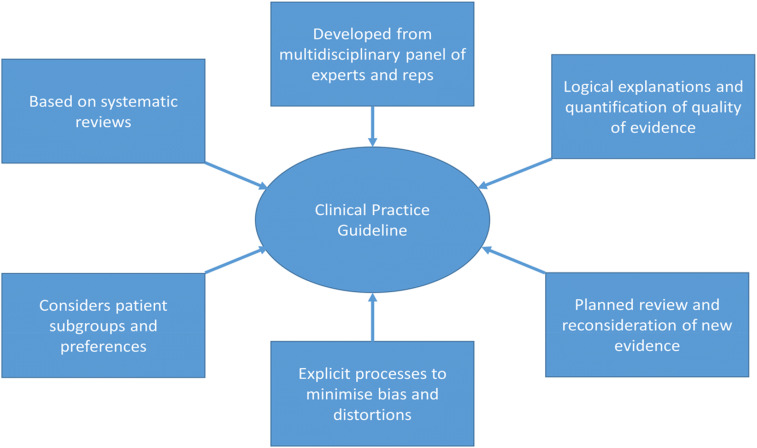
CPGs are implementable pieces of evidence synthesis30 (Figure 3). They define the clinical situation to be addressed; use explicit and comprehensive methods to search for and appraise the risk of bias of studies that address clinical situations; and with multiprofessional, multidisciplinary expertise, place these elements in clinical context to aid in recommending action (or inaction) and in defining areas of needed research. Guidance documents, from narrative reviews to expert position statements, vary in the rigor of their development and in the transparency in decision making. They require experts to offer their expertise during development, but their views are considered in the context of the evidence, and the trail of thinking is laid bare, rather than hidden in wise pronouncements. CPGs are not just meta-analyses, although high-quality evidence synthesis with systematic reviews and similar studies are the bricks from which they are built.
Figure 3.
Definition of a CPG. Adapted from Graham et al.40
CPGs should be patient centered, valid, accessible, and practical. Assessing which outcomes and experiences are of greatest importance to families and clinicians has been prioritized in the development of many supportive care CPGs, including the following: avoiding death from toxicity31; shortening the hospital stay32; and minimizing pain,33 mucositis,34 nausea,35 and fatigue.36 CPG validity can be assessed by using a formal assessment tool (such as AGREE II [Appraisal of Guidelines for Research and Evaluation])37 or by using guidelines endorsed by an organization that has undertaken such an assessment.
Implementation of guidelines, that is, converting their bald academic recommendations into something the clinical team can act on, is a separate skill. Local knowledge and significant leadership are needed to change the behaviors of a clinical team. A series of studies have been undertaken to assess how well CPGs effect change and the best techniques for the assessment, but much more research is needed.38 Tools such as integrated care pathways, prepopulated test order sets, and 1-touch prescription protocols linked to other elements of the EHR can help (Table 1). Patient-led interaction and high-quality education linked to emotional motivation may be effective as well. Printing a flowsheet, e-mailing a 20-page document to the clinical team, or silently placing it in an online library wastes the clinician’s time and breaks the hearts of the EHR developers, as well as reducing the chances of it being clinically implemented an improving symptoms.
Back to the clinical case
The patient’s hospital had adopted a systematic approach to routine symptom screening in the ambulatory and inpatient settings. Fatigue, nausea, and changes in taste were quickly deemed extremely bothersome. Based on the hospital’s clinical pathways, routine physical exercise with a physiotherapist was implemented. Adherence to a CPG for prevention of nausea and treatment guidance was closely monitored. Several approaches to managing the changes in taste were provided, although this symptom was less well controlled. The hospital also implemented an automated AE capture system, and reports were validated by the patient’s attending physician. She completed relapse therapy and reported her experience was much better in comparison with the initial therapy, even though the second treatment had been more intensive.
References
- 1.Canadian Cancer Society’s Steering Committee on Cancer Statistics. Canadian Cancer Statistics. Toronto, ON, Canada: Canadian Cancer Society; 2011. [Google Scholar]
- 2.Forrest SJ, Geoerger B, Janeway KA. Precision medicine in pediatric oncology. Curr Opin Pediatr. 2018;30(1):17-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dupuis LL, Johnston DL, Baggott C, et al. Validation of the Symptom Screening in Pediatrics Tool in children receiving cancer treatments. J Natl Cancer Inst. 2018;110(6):661-668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang LY, Manhas DS, Howard AF, Olson RA. Patient-reported outcome use in oncology: a systematic review of the impact on patient-clinician communication. Support Care Cancer. 2018;26(1):41-60. [DOI] [PubMed] [Google Scholar]
- 5.Berry DL, Hong F, Halpenny B, et al. Electronic self-report assessment for cancer and self-care support: results of a multicenter randomized trial. J Clin Oncol. 2014;32(3):199-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial [published correction appears in J Clin Oncol. 2016;34(18):2198]. J Clin Oncol. 2016;34(6):557-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA. 2017;318(2):197-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dupuis LL, Ethier MC, Tomlinson D, Hesser T, Sung L. A systematic review of symptom assessment scales in children with cancer. BMC Cancer. 2012;12(1):430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.OʼSullivan C, Dupuis LL, Sung L. A review of symptom screening tools in pediatric cancer patients. Curr Opin Oncol. 2015;27(4):285-290. [DOI] [PubMed] [Google Scholar]
- 10.Dupuis LL, Cook S, Robinson PD, Tomlinson D, Vettese E, Sung L. Optimizing symptom control in children and adolescents with cancer. Pediatr Res. 2019;86(5):573-578. [DOI] [PubMed] [Google Scholar]
- 11.Larouche V, Revon-Rivière G, Johnston D, et al. Translating the Symptom Screening in Pediatrics Tool (SSPedi) into French and among French-speaking children receiving cancer treatments, evaluating understandability and cultural relevance in a multiple-phase descriptive study. BMJ Open. 2020;10(4):e035265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tomlinson D, Hyslop S, Stein E, et al. Development of mini-SSPedi for children 4-7 years of age receiving cancer treatments. BMC Cancer. 2019;19(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hyslop S, Dupuis LL, Baggott C, et al. Validation of the proxy version of Symptom Screening in Pediatrics Tool in children receiving cancer treatments. J Pain Symptom Manage. 2018;56(1):107-112. [DOI] [PubMed] [Google Scholar]
- 14.Upton P, Lawford J, Eiser C. Parent-child agreement across child health-related quality of life instruments: a review of the literature. Qual Life Res. 2008;17(6):895-913. [DOI] [PubMed] [Google Scholar]
- 15.Johnston DL, Nagarajan R, Caparas M, et al. Reasons for non-completion of quality of life evaluations in pediatric acute myeloid leukemia: a report from the health related Children’s Oncology Group. PLoS One. 2013;8(9):e74549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tomlinson D, Plenert E, Dadzie G, et al. Discordance between pediatric self-report and parent proxy-report symptom scores and creation of a dyad symptom screening tool (co-SSPedi). Cancer Med. 2020;9(15)3235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) v5.0. Available at: https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm. 2017. Accessed date 14 Oct 2020.
- 18.Trotti A, Bentzen SM. The need for adverse effects reporting standards in oncology clinical trials. J Clin Oncol. 2004;22(1):19-22. [DOI] [PubMed] [Google Scholar]
- 19.Gwede CK, Johnson DJ, Daniels SS, Trotti A. Assessment of toxicity in cooperative oncology clinical trials: the long and short of it. J Oncol Manag. 2002;11(2):15-21. [PubMed] [Google Scholar]
- 20.Miller TP, Fisher BT, Getz KD, et al. Unintended consequences of evolution of the Common Terminology Criteria for Adverse Events. Pediatr Blood Cancer. 2019;66(7):e27747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang S, Liang F, Tannock I. Use and misuse of common terminology criteria for adverse events in cancer clinical trials. BMC Cancer. 2016;16(1):392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roche K, Paul N, Smuck B, et al. Factors affecting workload of cancer clinical trials: results of a multicenter study of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2002;20(2):545-556. [DOI] [PubMed] [Google Scholar]
- 23.Sivendran S, Latif A, McBride RB, et al. Adverse event reporting in cancer clinical trial publications. J Clin Oncol. 2014;32(2):83-89. [DOI] [PubMed] [Google Scholar]
- 24.Scharf O, Colevas AD. Adverse event reporting in publications compared with sponsor database for cancer clinical trials. J Clin Oncol. 2006;24(24):3933-3938. [DOI] [PubMed] [Google Scholar]
- 25.Miller TP, Li Y, Kavcic M, et al. Accuracy of adverse event ascertainment in clinical trials for pediatric acute myeloid leukemia. J Clin Oncol. 2016;34(13):1537-1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miller TP, Li Y, Getz KD, et al. Using electronic medical record data to report laboratory adverse events. Br J Haematol. 2017;177(2):283-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller TP, Getz KD, Demissei B, et al. Rates of laboratory adverse events by chemotherapy course for pediatric acute leukemia patients within the Leukemia Electronic Abstraction of Records Network (LEARN) [abstract]. Blood. 2019;134(suppl 1). Abstract 333. [Google Scholar]
- 28.Lencioni A, Hutchins L, Annis S, et al. An adverse event capture and management system for cancer studies. BMC Bioinformatics. 2015;16(suppl 13):S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Call RJ, Burlison JD, Robertson JJ, et al. Adverse drug event detection in pediatric oncology and hematology patients: using medication triggers to identify patient harm in a specialized pediatric patient population. J Pediatr. 2014;165(3):447-452 e444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dupuis LL, Robinson PD, van de Wetering MD, et al. ; Members of the iPOG Network. Lexicon for guidance terminology in pediatric hematology/oncology: a white paper. Pediatr Blood Cancer. 2020;67(4):e28170. [DOI] [PubMed] [Google Scholar]
- 31.Lehrnbecher T, Fisher BT, Phillips B, et al. Guideline for antibacterial prophylaxis administration in pediatric cancer and hematopoietic stem cell transplantation. Clin Infect Dis. 2020;71(1):226-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lehrnbecher T, Robinson P, Fisher B, et al. Guideline for the management of fever and neutropenia in children with cancer and hematopoietic stem-cell transplantation recipients: 2017 update. J Clin Oncol. 2017;35(18):2082-2094. [DOI] [PubMed] [Google Scholar]
- 33.Loeffen EAH, Mulder RL, Font-Gonzalez A, et al. Reducing pain and distress related to needle procedures in children with cancer: A clinical practice guideline. Eur J Cancer. 2020;131:53-67. [DOI] [PubMed] [Google Scholar]
- 34.Sung L, Robinson P, Treister N, et al. Guideline for the prevention of oral and oropharyngeal mucositis in children receiving treatment for cancer or undergoing haematopoietic stem cell transplantation. BMJ Support Palliat Care. 2017;7(1):7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paw Cho Sing E, Robinson PD, Flank J, et al. Classification of the acute emetogenicity of chemotherapy in pediatric patients: a clinical practice guideline. Pediatr Blood Cancer. 2019;66(5):e27646. [DOI] [PubMed] [Google Scholar]
- 36.Robinson PD, Oberoi S, Tomlinson D, et al. Management of fatigue in children and adolescents with cancer and in paediatric recipients of haemopoietic stem-cell transplants: a clinical practice guideline. Lancet Child Adolesc Health. 2018;2(5):371-378. [DOI] [PubMed] [Google Scholar]
- 37.Brouwers MC, Kho ME, Browman GP, et al. ; AGREE Next Steps Consortium. Development of the AGREE II, part 1: performance, usefulness and areas for improvement. CMAJ. 2010;182(10):1045-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Robinson PD, Dupuis LL, Tomlinson G, Phillips B, Greenberg M, Sung L. Strategies facilitating practice change in pediatric cancer: a systematic review. Int J Qual Health Care. 2016;28(4):426-432. [DOI] [PubMed] [Google Scholar]
- 39.Johnston DL, Hyslop S, Tomlinson D, et al. Describing symptoms using the Symptom Screening in Pediatrics Tool in hospitalized children with cancer and hematopoietic stem cell transplant recipients. Cancer Med. 2018;7(5):1750-1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidlines. In: Graham R, Mancher M, Miller Wolman D, Greenfield S, Steinberg E, eds. Clinical Practice Guidelines We Can Trust. Washington, DC: National Academies Press; 2011. Available at: https://www.ncbi.nlm.nih.gov/pubmed/24983061. [PubMed] [Google Scholar]