Visual Abstract
Abstract
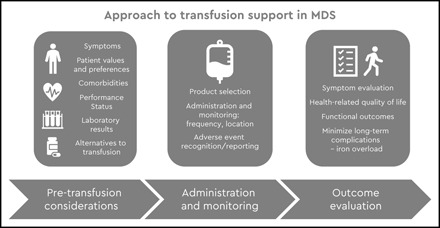
Patients with myelodysplastic syndromes (MDS) often need extended periods of red blood cell or platelet transfusion support, with the goal to manage symptoms of anemia and thrombocytopenia, respectively, and improve quality of life. Many questions about the optimal approach to transfusion management in MDS, especially in the outpatient setting, remain unanswered, including hemoglobin and platelet thresholds for transfusion. Restrictive transfusion approaches are often practised, but whether these are appropriate for outpatients with MDS, who are often older and may be frail, is not known. Current schedules for transfusion-dependent patients are burdensome, necessitating frequent visits to hospitals for sample collection and blood administration. Questions of optimal schedule and dosage are being explored in clinical trials, including the recently completed REDDS study. Patient-reported outcomes and functional assessments are increasingly being incorporated into research in this area so that we can better understand and improve transfusion support for patients with MDS.
Learning Objectives
Understand the goals of outpatient transfusions for patients with myelodysplastic syndromes (MDS)
Review current evidence supporting optimal management of outpatient transfusions for patients with MDS
Identify priority areas for future research in transfusion supportive care for MDS
Introduction
Anemia and thrombocytopenia in patients with myelodysplastic syndromes
Anemia is essentially universal in patients with myelodysplastic syndromes (MDS), and symptoms and signs of anemia, such as fatigue and dyspnea, are common presenting features.1-4 Palpitations, headache, anxiety, insomnia, pain, and weakness are also described by patients, and these contribute to the well-documented findings that anemia is also associated with poorer health-related quality of life (QoL) in MDS.1,4
Both the presence and degree of anemia are important in MDS, and these have been incorporated into prognostic scores.5,6 Malcovati et al5 demonstrated that hemoglobin <90 g/L in men and <80 g/L in women was independently associated with worse overall survival and with both nonleukemic and cardiac causes of death. Oliva et al7,8 reported that degree of anemia correlated with cardiac hypertrophy and remodeling, which may help explain the worse cardiac outcomes for anemic patients, although undoubtedly other factors contribute, including cardiac dysfunction from disease-related iron dysregulation and transfusion-related iron overload.7-9 These data do not tell us whether we can modify these outcomes by applying a different transfusion policy.
Thrombocytopenia is also very common in MDS, with up to two-thirds of patients having platelet counts <100 × 109/L at diagnosis; 5% to 20% of patients have severe thrombocytopenia depending on the definition used (<20 or <10 × 109/L).1,10,11 Thrombocytopenia in MDS is commonly multifactorial; platelet dysfunction is also common but often not recognized.10 Presence and degree of thrombocytopenia are both associated with worse prognosis in terms of survival and progression to acute leukemia. In day-to-day management, the primary concern related to thrombocytopenia is risk of bleeding. Minor bleeding is common, and bleeding is variably reported as the cause of death in 5% to 24% of patients with MDS in different studies.11
In the context of these cytopenias, 50% to 90% of patients with MDS will need red blood cell (RBC) transfusions, and many become RBC transfusion dependent; 30% to 50% of patients will need ≥1 platelet transfusion.1-3,12 With data indicating a high but variable burden of transfusion dependency in this patient population, this review addresses recent research findings to help clinicians answer the questions: How do I decide whether a transfusion is needed for my patient, and if it is, how is it best delivered, in accordance with the principles of patient blood management? Key considerations include the following:
The role of transfusion among the currently available therapeutic options for MDS
The aims of, and optimal processes for delivering and monitoring, transfusion supportive care with a focus on patient QoL
Where does transfusion fit among the currently available therapeutic options for MDS?
Therapeutic approaches for MDS include those directed at ameliorating the underlying bone marrow disease or managing the resulting cytopenias. These options include growth factors such as erythropoiesis-stimulating agents (ESAs) or granulocyte colony-stimulating factor; hypomethylating agents such as azacitidine; immunosuppression or immunomodulation (eg, lenalidomide); chemotherapy; and allogeneic hematopoietic stem cell transplantation, the only current curative option.1,9 Many novel agents, including molecularly targeted therapies, are in trials or coming into clinical practice. Recently, luspatercept has been shown to minimize anemia and RBC transfusion requirements, with 38% of luspatercept-treated lower-risk patients with MDS and ring sideroblasts becoming transfusion independent for ≥8 of the first 24 weeks on study, compared with 13% in the placebo arm, and with up to one-third of responders remaining transfusion independent for ≤48 weeks.13 Starting disease-modifying therapy (DMT) earlier can be associated with better clinical outcomes, but these therapies are not yet widely used in routine practice, mostly because of problems with cost or tolerability.14
As a result, many patients with MDS, especially those with lower-risk disease, are managed with supportive care alone, including transfusion, often for months to years.1-3,15-18 Therefore, even as new therapies emerge into practice, transfusion is likely to continue to be a central part of MDS management for the foreseeable future.
What are the aims of transfusion supportive care in MDS?
The main goals of transfusion supportive care are outlined in Table 1. RBC transfusions are given primarily to prevent serious complications of anemia, both acute and chronic, including heart failure and myocardial infarction.1,15-17,19 Other reasons for transfusion are to manage broader consequences of bone marrow failure, including fatigue and other symptoms related to anemia, and to prevent and manage of bleeding related to thrombocytopenia, aiming to improve patient QoL. However, data on the optimal timing to start transfusions in MDS are lacking, and transfusion is usually introduced on the basis of symptoms and falling blood counts.
Table 1.
Goals of RBC and platelet transfusion in MDS
| Transfusion type | Goal of transfusion | Measured by | Desired outcomes |
|---|---|---|---|
| Red cell transfusion |
|
|
|
| Platelet transfusion |
|
|
|
Various definitions of RBC transfusion dependency in MDS have been proposed, recently reviewed by Germing et al.1 These include requirements for 2 RBCs per month, RBC transfusion three or more times in a year, and other variations which include minimum numbers of RBCs or admissions per defined time period – with these definitions being variably applicable either in the routine clinical management setting, in analysis of administrative datasets, or for determining entry or response criteria for clinical trials.2,18,20 Transfusion intensity can be further described as low (3 to 7 RBCs per 16 weeks) or high (≥8 RBC per 16 weeks), and patients can be described either as not being transfusion dependent or as having low, medium, or high transfusion burden or dependency. These definitions can be helpful for research purposes but are probably less useful in day-to-day practice, except for the purpose of prognostication.
Management of transfusion dependency in MDS is a real conundrum: Transfusions are given with the aim of relieving symptoms, and indeed they can do so, but they provide only transient benefits related to the circulating lifespan of the transfused cells. They also carry the risks of both transfusion-related adverse effects and MDS-associated consequences: If you have MDS, being anemic or thrombocytopenic makes things worse for you, but being RBC or platelet transfusion dependent has itself been shown to be associated with worse prognosis, regardless of when it develops and even at low dose density.1,20 This association may relate in part to the underlying disease (the worse the ineffective hemopoiesis, the worse the consequences and the worse the prognosis) but also to the transfusion and its sequelae.
What is optimal transfusion support in MDS? Is it the same for all patients?
The principles of patient blood management (PBM), such as those described by the International Society of Blood Transfusion21 as “an evidence-based, multidisciplinary approach aimed at optimising the care of patients . . . put(ting) the patient at the heart of decisions made around blood transfusion, promoting appropriate use of blood and blood components and the timely use of alternatives where available,” remind us to be patient-focused. Transfusion decisions and processes should be undertaken with the patient’s active participation. We cannot simply apply a one-size-fits-all approach, but how do we determine the right approach and know how to advise an individual patient with MDS? Furthermore, hematologists are trying to balance care of each patient with efforts to minimize risks and costs and make best use of precious community blood supplies. Unfortunately, as outlined in Table 2, we still have many more questions than answers on how best to do this.
Table 2.
Important questions that need answers in optimizing transfusion support for patients with MDS
| Red cell transfusion |
|---|
| 1. To what degree does anemia (hemoglobin below the reference range, a laboratory result) need to be corrected to see clinical benefit? |
| 2. When should RBCs be transfused in MDS? What are the optimal hemoglobin thresholds and targets? Are they applicable to all patients, or are there subgroups, such as older patients or those with cardiovascular or respiratory comorbidities, who need special consideration? |
| 3. What is the optimal RBC transfusion schedule? Is a more stable hemoglobin better (should we aim to avoid the peaks and troughs of hemoglobin), and if so, why, and how can we achieve it? |
| 4. What is the optimal RBC product for transfusion in MDS (eg, improved oxygen delivery or lifespan, or degree of RBC antigen matching)? |
| Platelet transfusion |
| 5. Does degree of thrombocytopenia correlate with health-related QoL? Are there outcomes other than bleeding that are important? |
| 6. To what degree does thrombocytopenia (platelet count below the reference range, a laboratory result) need to be corrected to see clinical benefit? |
| 7. What should be the recommended platelet transfusion thresholds and targets? Are they applicable to all patients, or are there subgroups who need special consideration? |
| 8. What is the optimal platelet product for transfusion in MDS? How can platelet wastage (related to short shelf-life) be minimized? |
| 9. What alternatives to platelet transfusions can be used to reduce bleeding? |
| All transfusions |
| 10. What transfusion-related outcomes matter to patients, and how can they be measured (eg, using patient-reported outcomes) and prioritized? |
| 11. How can patients be more meaningfully involved in transfusion decision-making, the transfusion process, and monitoring of transfusion outcomes, including adverse events? |
| 12. What tools should we use to measure clinical need for and outcomes of transfusion? |
| 13. What are the clinical and community burdens (including costs and complications) of anemia, thrombocytopenia, and transfusion in MDS? |
| 14. How can the outpatient transfusion process be improved to optimize the patient experience, streamline health care delivery, and reduce costs? |
| 15. Is home transfusion an option, and if so, when and for which patients? |
The need for high-quality data applicable to hematology/oncology, including MDS, was noted by the International Consensus Conference on PBM22 and is reflected in current national and international clinical guidelines, where most recommend individualizing therapy but can provide only limited specific guidance on management, including hemoglobin and platelet transfusion thresholds.15,16,23 The impact of this current uncertainty on MDS transfusion management was documented in a recent practice survey of Australian and New Zealand hematologists.24
Consider the following cases. How would you approach the transfusion decision for each patient? What factors would influence your decision?
Case 1: A 80-year-old woman with low- to intermediate-risk MDS who lives at home with her husband presents to clinic for review. She has no past history of cardiovascular disease, and her renal function is normal. She denies any symptoms of fatigue or dyspnea. She has previously had a trial of erythropoietin for management of anemia, with no response. Her most recent blood tests included a hemoglobin concentration of 85 g/L. You consider whether to administer an RBC transfusion.
Case 2: A 63-year-old man with low- to intermediate-risk MDS who lives at home with his wife presents to the clinic for review. His past history is significant for a myocardial infarction 1 year earlier. He has no chest pain, dyspnea, or fatigue. His most recent blood tests showed a hemoglobin concentration of 78 g/L and normal renal function. You consider whether to administer an RBC transfusion.
Case 3: A 68-year-old woman with intermediate-risk MDS who lives alone presents to the clinic for review. She reports exertional dyspnea and fatigue but says these features have been long-standing. She has no history of cardiovascular disease, and physical examination reveals no signs of cardiac failure. Her renal function is normal. Her last RBC transfusion was 4 weeks ago. At what hemoglobin threshold would you initiate an RBC transfusion?
Choosing hemoglobin thresholds for RBC transfusion
Although nearly 20,000 patients have been enrolled in randomized trials comparing different hemoglobin thresholds, these have been almost exclusively in the acute anemia setting, most often in critical care or cardiac surgery, and often aimed at addressing primary outcomes of short-term (eg, in hospital) mortality. It is inappropriate to extrapolate the results from these trials to recommend a “restrictive” policy in transfusion-dependent MDS.
Unfortunately, few transfusion trials have been conducted for patients with hematological malignancies, and no studies have looked at hemoglobin threshold or outcomes studies for chronically transfused patients with other blood diseases with cytopenias, such as aplastic anemia or myelofibrosis.22,25 A recent study of adults undergoing hematopoietic stem cell transplantation showed that a restrictive (hemoglobin [Hb] <70 g/L) threshold for RBC transfusion was safe and delivered the same QoL outcomes as a liberal (Hb <90 g/L) strategy; however, patients were young (median age 57 years), the setting was primarily hospital-based (and median hospital length of stay was 23 days) with follow-up to 100 days, and patients had short-term transfusion needs.26 There are challenges in extrapolating these trial data, or data from other chronically anemic patients (including those with renal impairment, now generally managed with ESAs) to patients with MDS in the community, because a significant number of patients with MDS have comorbidities such as cardiovascular disease. We do not know whether a more liberal transfusion policy is indicated for patients with cardiac disease, including in the setting of MDS specifically.27
With this uncertainty in mind, an international group recently conducted the Red Blood Cell Transfusion Schedule in Myelodysplastic Syndromes (REDDS) pilot trial in transfusion-dependent MDS. Patients were assigned to a restrictive (Hb 80 g/L, to maintain hemoglobin 85 to 100 g/L) or liberal (Hb 105 g/L, maintaining 110 to 125 g/L) threshold for RBC transfusion, with health-related QoL measured via the EORTC QLQ-C30 and EQ-5D-5L.28 The primary outcome (adherence to assigned study arm) was shown to be feasible, and the protocol for outpatient transfusion was successfully implemented across multiple sites internationally. The investigators noted several additional points: Patients assigned to the liberal transfusion arm received about twice as many RBCs as the restrictive arm, and the time interval between transfusions was shorter for patients in the liberal arm. This has implications for both patients and transfusion services, given the need for more visits and more blood bank activities. A post hoc exploratory analysis suggested that the 5 main QoL domains were improved for participants in the liberal arm, supporting the need for additional research to elucidate the impact of different RBC transfusion policies. Finally, the REDDS analysis highlighted the need to consider not just hemoglobin concentration but also swings of amplitude, as demonstrated in an earlier modeling analysis.29
Additional research is needed, and a number of other studies are registered (Canada [NCT 02099669], France [NCT03643042], and the international REDDS2 trial [ACTRN12619001053112p]). However, larger studies of transfusion thresholds in MDS will be challenging, with limited numbers of potentially eligible patients at any given site.
If improved QoL is an aim of RBC transfusion in MDS, when and how should we measure it?
Most trials of RBC transfusion thresholds have used short-term mortality as the primary outcome. Trials of interventions to address anemia, such as ESAs, have mostly measured increase in hemoglobin as a trial outcome. Although this measurement is convenient and inexpensive, it does not tell the whole story, and we need to look at the clinical impact on patients, particularly functional outcomes and QoL, through relief of symptoms for which the intervention is being given. This also applies to RBC transfusion. Documentation of patient-reported outcomes (PROs) via patient-reported outcome measures (PROMs) is being included more routinely in clinical trials and practice. Functional outcomes are particularly important for outpatients who are managing their physical ADLs as well as the social and community aspects of their lives.
Table 3 summarizes clinical studies that have assessed QoL and functional outcomes related to RBC transfusion for patients with MDS.28-34 In addition to the REDDS pilot trial,28 a few observational studies have measured the impact of RBC transfusion on QoL or functional outcomes, and 1 small randomized trial compared RBCs of different storage age. In the RETRO study (which included patients with a range of hematology/oncology diagnoses including MDS), RBC transfusion was associated with improvement in some (fatigue, walk distance) but not all (dyspnea) outcomes, particularly if hemoglobin was maintained at ≥80 g/L 1 week after transfusion.30 In a subsequent analysis from the RETRO study, Bruhn et al31 studied the impact of RBC transfusions over 4 weeks on patient-reported fatigue via serial FACIT-Fatigue scores and noted improvement in early post-transfusion scores, without real change after that. Notably, responses varied widely between patients. Chan et al.32 used a variety of tools to study QoL after RBC transfusion for medical patients, of whom some had MDS. Worse pretransfusion QoL scores predicted post-transfusion improvement. These observations are also supported by trials that have shown improved QoL for patients with MDS with higher hemoglobin, regardless of how it is achieved (eg, in the Nordic study where patients received darbepoetin with or without granulocyte colony-stimulating factor or transfusion, or both, to achieve a target Hb of ≥120 g/L).35
Table 3.
Studies of the impact of RBC transfusion on QoL and functional outcomes in MDS
| Study | Patients | Study design | Intervention | Outcomes assessed | Comments |
|---|---|---|---|---|---|
| Bruhn et al31 2020 | 204 outpatients >50 y with hematological or cancer-related diagnosis (40 with MDS) | Observational study | Assessed before RBC transfusion and at days 3, 7, and 28 after RBC transfusion | FACIT-Fatigue | Patients with greater fatigue at baseline had early improvement in fatigue after RBC transfusion but no significant change between day 3 and day 28 after RBC transfusion |
| Caocci et al29 2007 | 32 patients with MDS, 20 received RBC transfusion | Observational study | Measured the association between amplitude of Hb fluctuations with QoL over 1 mo | EORTC QLQC30, patient self-report | Lower variation in Hb correlated with better QoL and lower fatigue; transfusion-free patients reported better QoL and less fatigue than transfused patients |
| Chan et al32 2018 | 101 patients receiving RBC transfusion (inpatients and outpatients), 40 with hematological diagnosis | Observational study | Measured QoL before RBC transfusion and day 1 and day 7 after RBC transfusion | Short Form 12 Version 2 | Greater increase in QoL observed in patients with worse baseline QoL scores; transfusion trigger was not associated with change in QoL |
| FACT-Anemia | |||||
| Hsia et al33 2016 | 20 transfusion-dependent adults (11 with MDS) | Randomized trial (n-of-1 design) | Fresh (<7 d of storage) vs standard-issue (up to 42 d of storage) RBC transfusion | FACT-An, 3 questions on a visual analog scale | No difference in QoL between fresh and standard-issue RBC; no clinically significant improvement in QoL after RBC transfusion (whether fresh or standard) |
| Patient self-report | |||||
| Jansen et al34 2020 | 19 patients with transfusion-dependent MDS | Randomized trial | Liberal (Hb transfusion trigger <97 g/L) vs restrictive (<73 g/L) RBC transfusion protocol | EuroQoL5D, Multidimensional Fatigue Inventory | Terminated prematurely because of slow recruitment |
| No significant differences in symptoms, QoL scores, or cardiovascular outcomes | |||||
| Oliva et al7 2005 | 39 patients with MDS | Observational, cross-sectional study | Cross-sectional study of cardiac and QoL assessment according to transfusion dependence | QOL-E, cardiac echocardiography | Worse QoL in transfused patients compared with nontransfused; higher rates of cardiac remodeling in transfusion-dependent group; cardiac remodeling associated with lower mean Hb levels and older age; each unit of Hb increase predicted a 49% reduction in risk of remodeling |
| St Lezin et al30 2019 | 221 outpatients >50 y with hematological or cancer-related diagnosis (40 with MDS) | Observational study | Assessed before RBC transfusion and 1 wk after RBC | FACIT-Fatigue Scale, FACIT-Dyspnea Scale, 6-min walk test (6MWT) | Clinically important improvement in fatigue or 6MWT but not dyspnea 1 wk after RBC in 70%; patients who maintained Hb 80 g/L at 1 wk, who had not received cancer therapy and who did not need hospitalization, showed clinically important increases in mean 6MWT distance |
| Stanworth et al28 2020 | 38 patients with transfusion-dependent MDS | Randomized trial | Liberal (maintain Hb 100-125 g/L) vs restrictive (maintain Hb 85-100 g/L) RBC transfusion protocol | EQ-5D EORTC QLQC30 | Post hoc exploratory analysis suggested improved QoL (global health, physical functioning, fatigue, and dyspnea) |
In addition to inclusion of PROs in clinical trials, implementation of PROMs in routine clinical practice is increasingly gaining interest. Use of PROMs to inform cancer care has been shown to improve outcomes including QoL, survival, and emergency department visits in other cancers. However, few studies have been done in hematological cancer, and to our knowledge none are specific to transfusion management. Extrapolating from other cancers, potential benefits from routine use of PROMs include improved accuracy of symptom assessment, improved patient–clinician communication, shared medical decision making, and improved QoL.36 The choice of PROM is important for both clinical studies and practice, because there is different information to be gained from generic QoL tools such as the EQ5D (which are generally simple and fast to complete and permit comparisons across different conditions) with data obtained from condition-specific (eg, MDS) or symptom-specific (eg, anemia) tools, which tend to be more targeted and comprehensive but where data may be more difficult to obtain. We should also distinguish between information gained from completing a standard questionnaire compared with providing a description of experience in the patient’s own words (eg, data that may be generated from individual interviews or focus groups).4 Moreover, it should be recognized that patient and physician perceptions may differ substantially, either in emphasis (what is relevant to one may not be important to the other) or the importance attributed to it. For example, in one study physicians tended to give more positive scores about QoL than did their patients with MDS, and patients placed greater importance on the disruption to daily life by frequent hospital visits for transfusion than did physicians.37
The question of hemoglobin thresholds for RBC transfusion has been further highlighted by feedback from patients with MDS. A large, multicountry survey presented at ASH 2018 reported that 40% of patients with MDS wished they had received RBC transfusions at higher hemoglobin thresholds than they currently were, suggesting that patients are aware of and concerned about the impact of anemia and how it is managed.38
More research is needed to elucidate the relationship between anemia and thrombocytopenia and the range of symptoms being reported (including where there may be interactions) before and after transfusion. As this field develops, we can expect to see objectively recorded functional outcomes and PROs being considered absolutely central to the evaluations of both new agents and supportive care interventions, and we can also anticipate that new technologies such as wearable devices (eg, smart watches) will be more widely used for continuous monitoring and capture of these data.
The outpatient transfusion process
The recent REDDS trial illustrated the high frequency with which transfusion-dependent MDS outpatients need hospitalization.28 Not surprisingly, the need for multiple visits is a major burden and disruption for transfusion-dependent patients with MDS. Many aspects of our current outpatient transfusion policies have been designed to fit the needs of busy clinics and transfusion departments rather than the needs of patients. However, the optimal way to deliver outpatient transfusion services is not known. The REDDS findings indicate the need for additional studies to evaluate the impacts and costs of changing transfusion policies, because changes would have important implications for patients (frequent travel and clinic visits) and hospitals alike.
For some patients, transfusions on weekends, or even at home, might be an option. It is unclear how widespread is the use of home transfusion services for patients with MDS; however, these have been described, and where adequately resourced they may help reduce the travel and attendance burden for selected patients.39
Other considerations
Transfusion complications in transfused patients with MDS range from common febrile reactions to uncommon but more serious adverse effects. Few reliable data are available on rates of these complications in patients with MDS, but many cases have been reported to hemovigilance programs, perhaps reflecting the high transfusion exposures in these patients. Transfusion-associated circulatory overload (TACO) is a particular concern for older adults, many of whom have cardiorespiratory comorbidities. Whether transfusing fewer units at a time, or more slowly, or accompanied by prophylactic diuretics reduces TACO risk for patients with MDS is not known.
Identifying and managing transfusion reactions in the outpatient setting can be difficult; these events are easily missed between visits or attributed to other causes, and patients need specific instructions on whom to contact and what to report. Many transfusion adverse events are process-related, and the complexity of the multiple interconnecting clinical and laboratory processes contributes to errors and delays. Efforts to simplify the outpatient transfusion process may reduce these hazards.
Alloimmunization to RBC antigens is a major concern, with most studies describing rates of 10% to 23% in transfusion-dependent patients with MDS, but much higher rates have been reported.40-42 Alloimmunization appears to correlate with total RBC exposure and exposure to platelet units unmatched for RBC antigens, rather than inherent immunogenicity of the RBC units or the known immune dysregulation present in the underlying MDS, but it is probably multifactorial. A significant proportion of alloimmunized patients also develop autoantibodies, which may compound hemolytic complications.40 A wide variety of RBC antibody specificities have been reported, but antibodies to K and the Rh system antigens (especially anti-E) are the most common; therefore, providing RBCs negative for these antigens may be sufficient to minimize alloimmunization for most patients.42 However, more extensive matching, including genotyping, may confer additional benefit and is being increasingly used in routine practice before chronic transfusion programs.43 In retrospective studies, azacitidine use has been reported to reduce rates of RBC alloimmunization.44
Iron overload is commonly identified in transfusion-dependent MDS, caused by the dual problems of ineffective hemopoiesis or deranged iron metabolism from MDS and iron loading from transfused RBCs.1,9 The toxic effects of labile plasma iron seem to play an important role in end-organ damage. Ferritin levels have traditionally been monitored to document iron overload, and an elevated level has been shown to be an independent risk factor for mortality. However, hyperferritinemia is not specific for iron overload and is starting to be supplemented by monitoring of other parameters in trials and clinical practice.
Iron chelation has been reported to reduce transfusion requirements and should be considered early for patients who become transfusion dependent.1 However, determining who is a candidate for chelation can be difficult; for instance, higher-risk patients needing greater transfusion intensity will become iron loaded more quickly but may not benefit from chelation because of their shorter survival. Furthermore, chelation success still depends on compliance with therapy, but delivering tolerable, clinically effective and cost-effective iron chelation has been challenging, particularly until the advent of oral agents, and all chelation agents carry costs and the risk of adverse effects.
Guidelines variably recommend commencing chelation at ferritin >1,000 μg/L or after receipt of 20 to 30 U of RBCs. The recent TELESTO trial randomly assigned 225 patients with low- to intermediate-risk MDS who had received 15 to 75 U of RBCs before study entry to deferasirox or placebo.45 Because of slow recruitment, the trial was changed from a phase 3 to phase 2 trial. Event-free survival (worsening cardiac and liver function, need for hospitalization for congestive heart failure, acute myeloid leukemia transformation) was improved in the treatment group; adverse events were common. Longer follow-up in this study will be interesting, because few patients were followed at later time points, and it remains to be seen whether these results will be taken up in routine practice, because historically chelation rates have been low in MDS, especially for older and frail patients, even though chelation improves clinical outcomes.46
A few words about platelet transfusions in MDS
Up to 50% of patients need some platelet transfusion support. Routine prophylaxis (to prevent bleeding) with platelet transfusion for patients with MDS and thrombocytopenia who are not undergoing intensive therapy is not recommended, but few reliable data exist on how commonly this is performed in practice or how effective platelet transfusions are.10-12 There is no international definition of platelet transfusion dependency in the MDS setting.
Dosing of platelet transfusion has largely been extrapolated from studies of other hematological malignancies. In a retrospective review of outpatient platelet transfusions, where 57% of the patients had leukemia or MDS, there was no clear advantage in transfusing 2 U of platelets compared with 1 U.47 In a recent analysis from the South Australian MDS Registry, 9% of all patients (and 30% of women receiving DMT, compared with only 5% of men receiving DMT) who received a platelet transfusion developed immune-mediated refractoriness to platelet transfusions and needed HLA-matched platelets for future transfusion support, increasing the risks of bleeding and the costs and complexity of care.12
One approach to severe thrombocytopenia in MDS is to offer routine tranexamic acid. A number of randomized trials are testing the safety of tranexamic acid in acute settings of hematological malignancies, although none are specifically recruiting outpatients with MDS.
Conclusion—and the way forward
New understanding of the MDS disease process and the availability of novel therapies offer the prospect of major advances in management and outcomes for patients over the coming years. However, transfusion is still an important part of MDS supportive care. Although blood components are safe in most countries, they carry substantial risks and costs, and patients who are chronically transfused are recurrently exposed to these hazards. We need to make every management decision, including each transfusion decision, carefully, guided by the available evidence and the principles of PBM to deliver personalized MDS and transfusion therapy based on an individual patient’s needs and with their participation.48 We also need to monitor the impact of our transfusion therapy, including the effects on QoL. Many questions remain, some of which are summarized in Table 2. By designing and contributing to high-quality, patient-centered research using a range of approaches, including clinical registries to provide real-world practice and outcome data, and performing well-conducted clinical trials incorporating PROs and functional assessments, we can strengthen the evidence base to guide our practice and improve outcomes for transfused patients with MDS.
Acknowledgments
The authors thank Simon Stanworth, Allison Mo, Robert Weinkove, and Devendra Hiwase for helpful discussions.
References
- 1.Germing U, Oliva EN, Hiwase D, Almeida A. Treatment of anemia in transfusion-dependent and non-transfusion-dependent lower-risk MDS: current and emerging strategies. HemaSphere. 2019;3(6):e314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McQuilten ZK, Polizzotto MN, Wood EM, Sundararajan V. Myelodysplastic syndrome incidence, transfusion dependence, health care use, and complications: an Australian population-based study 1998 to 2008. Transfusion. 2013;53(8):1714-1721. [DOI] [PubMed] [Google Scholar]
- 3.DeZern AE, Binder G, Rizvi S, et al. . Patterns of treatment and costs associated with transfusion burden in patients with myelodysplastic syndromes. Leuk Lymphoma. 2017;58(11):2649-2656. [DOI] [PubMed] [Google Scholar]
- 4.Ryblom H, Hast R, Hellström-Lindberg E, Winterling J, Johansson E. Self-perception of symptoms of anemia and fatigue before and after blood transfusions in patients with myelodysplastic syndromes. Eur J Oncol Nurs. 2015;19(2):99-106. [DOI] [PubMed] [Google Scholar]
- 5.Malcovati L, Hellström-Lindberg E, Bowen D, et al. ; European Leukemia Net. Diagnosis and treatment of primary myelodysplastic syndromes in adults: recommendations from the European LeukemiaNet. Blood. 2013;122(17):2943-2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hiwase DK, Singhal D, Strupp C, et al. . Dynamic assessment of RBC-transfusion dependency improves the prognostic value of the revised-IPSS in MDS patients. Am J Hematol. 2017;92(6):508-514. [DOI] [PubMed] [Google Scholar]
- 7.Oliva EN, Dimitrov BD, Benedetto F, D’Angelo A, Nobile F. Hemoglobin level threshold for cardiac remodeling and quality of life in myelodysplastic syndrome. Leuk Res. 2005;29(10):1217-1219. [DOI] [PubMed] [Google Scholar]
- 8.Oliva EN, Schey C, Hutchings AS. A review of anemia as a cardiovascular risk factor in patients with myelodysplastic syndromes. Am J Blood Res. 2011;1(2):160-166. [PMC free article] [PubMed] [Google Scholar]
- 9.Platzbecker U. Treatment of MDS. Blood. 2019;133(10):1096-1107. [DOI] [PubMed] [Google Scholar]
- 10.Li W, Morrone K, Kambhampati S, Will B, Steidl U, Verma A. Thrombocytopenia in MDS: epidemiology, mechanisms, clinical consequences and novel therapeutic strategies. Leukemia. 2016;30(3):536-544. [DOI] [PubMed] [Google Scholar]
- 11.Vijenthira A, Premkumar D, Callum J, et al. . The management and outcomes of patients with myelodysplastic syndrome with persistent severe thrombocytopenia: an observational single centre registry study. Leuk Res. 2019;76:76-81. [DOI] [PubMed] [Google Scholar]
- 12.Cheok KPL, Chhetri R, Wee LYA, et al. . The burden of immune-mediated refractoriness to platelet transfusions in myelodysplastic syndromes [published online ahead of print 9 September 2020]. Transfusion. [DOI] [PubMed] [Google Scholar]
- 13.Fenaux P, Platzbecker U, Mufti GJ, et al. . Luspatercept in patients with lower-risk myelodysplastic syndromes. N Engl J Med. 2020;382(2):140-151. [DOI] [PubMed] [Google Scholar]
- 14.Cogle CR, Reddy SR, Chang E, et al. . Early treatment initiation in lower-risk myelodysplastic syndromes produces an earlier and higher rate of transfusion independence. Leuk Res. 2017;60:123-128. [DOI] [PubMed] [Google Scholar]
- 15.Killick SB, Carter C, Culligan D, et al. ; British Committee for Standards in Haematology. Guidelines for the diagnosis and management of adult myelodysplastic syndromes. Br J Haematol. 2014;164(4):503-525. [DOI] [PubMed] [Google Scholar]
- 16.Fenaux P, Haase D, Sanz GF, Santini V, Buske C; ESMO Guidelines Working Group. Myelodysplastic syndromes: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25(suppl 3):iii57-iii69. [DOI] [PubMed] [Google Scholar]
- 17.Ramsey SD, McCune JS, Blough DK, et al. . Patterns of blood product use among patients with myelodysplastic syndrome. Vox Sang. 2012;102(4):331-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Platzbecker U, Fenaux P, Adès L, et al. . Proposals for revised IWG 2018 hematological response criteria in patients with MDS included in clinical trials. Blood. 2019;133(10):1020-1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mastaglio F, Bedair K, Papaemmanuil E, et al. . Impact of socioeconomic status on disease phenotype, genomic landscape and outcomes in myelodysplastic syndromes. Br J Haematol. 2016;174(2):227-234. [DOI] [PubMed] [Google Scholar]
- 20.de Swart L, Smith A, Johnston TW, et al. . Validation of the revised international prognostic scoring system (IPSS-R) in patients with lower-risk myelodysplastic syndromes: a report from the prospective European LeukaemiaNet MDS (EUMDS) registry. Br J Haematol. 2015;170(3):372-383. [DOI] [PubMed] [Google Scholar]
- 21.International Society of Blood Transfusion. Available at: https://www.isbtweb.org/working-parties/clinical-transfusion/. Accessed 30 May 2020.
- 22.Mueller MM, Van Remoortel H, Meybohm P, et al. ; ICC PBM Frankfurt 2018 Group. Patient blood management: recommendations from the 2018 Frankfurt Consensus Conference. JAMA. 2019;321(10):983-997. [DOI] [PubMed] [Google Scholar]
- 23.Estcourt LJ, Birchall J, Allard S, et al. ; British Committee for Standards in Haematology. Guidelines for the use of platelet transfusions. Br J Haematol. 2017;176(3):365-394. [DOI] [PubMed] [Google Scholar]
- 24.Mo A, McQuilten ZK, Wood EM, Weinkove R. Red cell transfusion thresholds in myelodysplastic syndromes: a clinician survey to inform future clinical trials. Intern Med J. 2017;47(6):695-698. [DOI] [PubMed] [Google Scholar]
- 25.Estcourt LJ, Malouf R, Trivella M, Fergusson DA, Hopewell S, Murphy MF. Restrictive versus liberal red blood cell transfusion strategies for people with haematological malignancies treated with intensive chemotherapy or radiotherapy, or both, with or without haematopoietic stem cell support. Cochrane Database Syst Rev. 2017;1(1):CD011305 10.1002/14651858.CD011305.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tay J, Allan DS, Chatelain E, et al. . Liberal versus restrictive red blood cell transfusion thresholds in hematopoietic cell transplantation: a randomized, open label, phase III, noninferiority trial. J Clin Oncol. 2020;38(13):1463-1473. [DOI] [PubMed] [Google Scholar]
- 27.Carson JL, Stanworth SJ, Alexander JH, et al. . Clinical trials evaluating red blood cell transfusion thresholds: an updated systematic review and with additional focus on patients with cardiovascular disease. Am Heart J. 2018;200:96-101. [DOI] [PubMed] [Google Scholar]
- 28.Stanworth SJ, Killick S, McQuilten ZK, et al. ; REDDS Investigators. Red cell transfusion in outpatients with myelodysplastic syndromes: a feasibility and exploratory randomised trial. Br J Haematol. 2020;189(2):279-290. [DOI] [PubMed] [Google Scholar]
- 29.Caocci G, Baccoli R, Ledda A, Littera R, La Nasa G. A mathematical model for the evaluation of amplitude of hemoglobin fluctuations in elderly anemic patients affected by myelodysplastic syndromes: correlation with quality of life and fatigue. Leuk Res. 2007;31(2):249-252. [DOI] [PubMed] [Google Scholar]
- 30.St Lezin E, Karafin MS, Bruhn R, et al. ; NHLBI Recipient Epidemiology and Donor Evaluation Study (REDS)-III Program. Therapeutic impact of red blood cell transfusion on anemic outpatients: the RETRO study. Transfusion. 2019;59(6):1934-1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bruhn R, Karafin MS, Hilton JF, et al. . Early and sustained improvement in fatigue-related quality of life following red blood cell transfusion in outpatients. Qual Life Res. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chan KLL, Mak WMV, Tam YH, Lee KKH. Factors affecting patient-reported outcomes after red blood cell transfusion in medical patients. Transfusion. 2018;58(1):158-167. [DOI] [PubMed] [Google Scholar]
- 33.Hsia CC, Mahon JL, Seitelbach M, Chia J, Zou G, Chin-Yee IH. Use of n-of-1 (single patient) trials to assess the effect of age of transfused blood on health-related quality of life in transfusion-dependent patients. Transfusion. 2016;56(5):1192-1200. [DOI] [PubMed] [Google Scholar]
- 34.Jansen AJG, van den Bosch J, Te Boekhorst PAW, Schipperus MR, Beckers EAM. Results of the prematurely terminated TEMPLE randomized controlled trial in patients with myelodysplastic syndrome: liberal versus restrictive red blood cell transfusion threshold. Transfusion. 2020;60(4):879-881. [DOI] [PubMed] [Google Scholar]
- 35.Nilsson-Ehle H, Birgegård G, Samuelsson J, et al. . Quality of life, physical function and MRI T2* in elderly low-risk MDS patients treated to a haemoglobin level of ≥120 g/L with darbepoetin alfa ± filgrastim or erythrocyte transfusions. Eur J Haematol. 2011;87(3):244-252. [DOI] [PubMed] [Google Scholar]
- 36.Efficace F, Gaidano G, Lo-Coco F. Patient-reported outcomes in hematology: is it time to focus more on them in clinical trials and hematology practice? Blood. 2017;130(7):859-866. [DOI] [PubMed] [Google Scholar]
- 37.Oliva EN, Finelli C, Santini V, et al. . Quality of life and physicians’ perception in myelodysplastic syndromes. Am J Blood Res. 2012;2(2):136-147. [PMC free article] [PubMed] [Google Scholar]
- 38.Buckstein R, Starkman R, Lin Y, et al. . Forty percent of MDS patients wish they received red blood cell transfusions at higher hemoglobin thresholds than they currently are: a multinational transfusion audit. Blood. 2018;132(suppl 1):3092. [Google Scholar]
- 39.Niscola P, Tendas A, Giovannini M, et al. . Transfusions at home in patients with myelodysplastic syndromes. Leuk Res. 2012;36(6):684-688. [DOI] [PubMed] [Google Scholar]
- 40.Singhal D, Kutyna MM, Chhetri R, et al. . Red cell alloimmunization is associated with development of autoantibodies and increased red cell transfusion requirements in myelodysplastic syndrome. Haematologica. 2017;102(12):2021-2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chhetri R, Wee LYA, Sinha R, et al. . Red cell autoimmunization and alloimmunization in myelodysplastic syndromes: prevalence, characteristic and significance. Haematologica. 2019;104(10):e451-e454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lin Y, Saskin A, Wells RA, et al. . Prophylactic RhCE and Kell antigen matching: impact on alloimmunization in transfusion-dependent patients with myelodysplastic syndromes. Vox Sang. 2017;112(1):79-86. [DOI] [PubMed] [Google Scholar]
- 43.Guelsin GA, Rodrigues C, Visentainer JE, et al. . Molecular matching for Rh and K reduces red blood cell alloimmunisation in patients with myelodysplastic syndrome. Blood Transfus. 2015;13(1):53-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ortiz S, Orero MT, Javier K, et al. . Impact of azacitidine on red blood cell alloimmunisation in myelodysplastic syndrome. Blood Transfus. 2017;15(5):472-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Angelucci E, Li J, Greenberg P, et al. ; TELESTO Study Investigators. Iron chelation in transfusion-dependent patients with low- to intermediate-1-risk myelodysplastic syndromes: a randomized trial. Ann Intern Med. 2020;172(8):513-522. [DOI] [PubMed] [Google Scholar]
- 46.Hoeks MPA, Middelburg RA, Romeijn B, Blijlevens NMA, van Kraaij MGJ, Zwaginga JJ. Red blood cell transfusion support and management of secondary iron overload in patients with haematological malignancies in the Netherlands: a survey. Vox Sang. 2018;113(2):152-159. [DOI] [PubMed] [Google Scholar]
- 47.Gehrie EA, Frank SM, Visagie M, et al. . One-unit compared to two-unit platelet transfusions for adult oncology outpatients. Vox Sang. 2019;114(5):517-522. [DOI] [PubMed] [Google Scholar]
- 48.Buckstein RJ. Integrating patient-centered factors in the risk assessment of MDS. Hematology (Am Soc Hematol Educ Program). 2019;2019(1):373-380. [DOI] [PMC free article] [PubMed] [Google Scholar]


