Visual Abstract
Abstract
“Monoclonal gammopathy of clinical significance” (MGCS) is the term used to describe nonmalignant monoclonal gammopathies causing important disease. MGCS is the differential diagnosis for any patient presenting with what appears to be a monoclonal gammopathy of undetermined significance but is also experiencing other unexplained symptoms. Broadly, these conditions can be separated into symptoms and signs referable to the nerves, the kidneys, and the skin. The first step in making these diagnoses is to consider them. With a particular condition in mind, the next step is to order those tests that can help confirm or dismiss a particular diagnosis. Nearly all of the renal and dermatologic conditions are diagnosed by renal and skin biopsies, respectively. The importance of a highly competent renal pathologist and dermatopathologist cannot be underestimated. Biopsy is less specific for the neuropathic conditions. Because several of the MGCSs are syndromes, recognizing other manifestations is also key. Treatment recommendations for many of these conditions are anecdotal because of their rarity, but for several of the conditions, IV immunoglobulin, rituximab, and plasma cell–directed therapy are the best options.
Learning Objectives
• Recognize the differential diagnosis for a monoclonal gammopathy with peripheral neuropathy, skin abnormalities, or renal disease
• Diagnose MGCS
Clinical case
Approximately 18 months before diagnosis and at age 67, a man began experiencing anorexia, nausea, vomiting, and weight loss. By 12 months before diagnosis, he had lost 25 kg. An extensive nondiagnostic evaluation was performed, including thyrotropin, antineutrophil cytoplasmic autoantibodies, antinuclear antibodies, endoscopies, gastric emptying studies, and positron emission tomography–computed tomography. Seven months before diagnosis, an immunoglobulin Aλ monoclonal gammopathy was found. Over the ensuing months, this patient developed sensorimotor peripheral neuropathy, progressive muscle weakness, volume overload, and pseudogout. He was admitted to our hospital, where a diagnosis was made. In addition to the preceding presentations, he had malnutrition and anasarca (Table 1). His Eastern Cooperative Oncology Group performance status was 4.
Table 1.
Baseline characteristics, interpretation, and resolution for patient case
| Characteristics | At diagnosis | Comment | After therapy |
|---|---|---|---|
| Demyelinating PN | Classic for POEMS syndrome | Walks with AFOs; still foot drop | |
| Nausea, vomiting, anorexia | Due to adrenal insufficiency | Promptly resolved | |
| Hb, g/dL | 8.6 | Due to adrenal insufficiency, hypothyroidism and chronic disease; unusual to have cytopenias in POEMS | Normalized |
| Platelets, ×109/L | 109 | ||
| Albumin, g/dL | 2.3 | ||
| Creatinine, g/dL | 2.3 | Hypovolemia, diuretic use | |
| M spike | IgA λ | IFE positive | IFE positive |
| IgA, mg/dL | 536 | Elevated | Normal range |
| κ-FLC, mg/dL | 8.26 | Acute renal insufficiency and POEMS syndrome: polyclonal FLC elevation common. | |
| λ FLC, mg/dL | 13.2 | ||
| FLC ratio | 0.626 | ||
| TSH/T4, IU/L, ng/dL | 9.5/0.4 | Hypothyroidism | Replaced |
| Cortisol | 3.3 | Hypoadrenalism | |
| Plasma VEGF, pg/mL | 320 | ULN 86 pg/mL: consistent with POEMS | Normalized |
| IL-6, pg/mL | 62.9 | Bed sores due to chronic debility | |
| Urine 24-h protein, mg | 381 | AKI versus POEMS | |
| BMPC, % | 10 (λ) | On the high side for POEMS syndrome | <5%, but still clonal |
| RVSP, mmHg | 64 | Moderate pulmonary hypertension | Normalized |
| DLCO | Normal | Normal | |
| CT skeletal survey | Bones negative, but ascites, effusions, anasarca | >85% patients with bone lesions | Resolved |
| ECOG PS | 4 | 0-1 |
AFOs, ankle foot orthotics; AKI, acute kidney injury; BMPC, bone marrow plasma cells; CT, computed tomography; DLCO, diffusion capacity of carbon monoxide; ECOG, Eastern Cooperative Oncology Group; FLC, immunoglobulin free light chains; Hb, hemoglobin; IFE, immunofixation; IgA, immunoglobulin A; IL-6, interleukin-6; POEMS, polyradiculoneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, and skin changes; PN, peripheral neuropathy; PS, performance status; RVSP, right ventricular systolic pressure; T4, thyroxine; TSH, thyrotropin; ULN, upper limit of normal; VEGF, vascular endothelial growth factor.
Introduction
The term “monoclonal gammopathy of clinical significance” (MGCS) was coined subsequent to monoclonal gammopathy of renal significance (MGRS) when it became increasingly apparent that a term was required for a patient with a small B-cell clone and small monoclonal proteins that were causing serious and even life-threatening disease (Figure 1A).1,2 Monoclonal gammopathy of “undetermined significance” (MGUS) is a misnomer for these conditions. Some patients with MGCS have sufficient clonal burden to satisfy the definition of smoldering multiple myeloma or smoldering Waldenstrom macroglobulinemia. In short, MGCS is a monoclonal gammopathy featuring two main characteristics: a quiescent underlying clone and symptoms that are related to the monoclonal immunoglobulin or to the clone itself by mechanisms other than the tumor burden. The MGCSs are best divided into different systems that are affected, the most common of which are kidney, nerve, and skin, recognizing that in some cases there is overlap due to a systemic, multiorgan presentation and/or course.
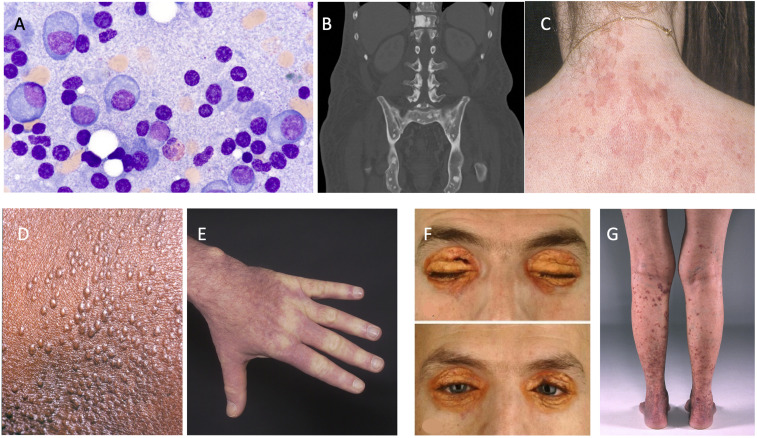
Figure 1.
Part of the monoclonal gammopathy of clinical significance spectrum. (A) Bone marrow plasma cells (original magnification, 100×). (B) Osteosclerotic lesions of POEMS syndrome (polyradiculoneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, and skin changes). (C) Schnitzler syndrome. (D and E) Scleromyxedema. (F) Necrobiotic xanthogranuloma. (G) Cryoglobulinemia vasculitis.
Neurologic MGCS
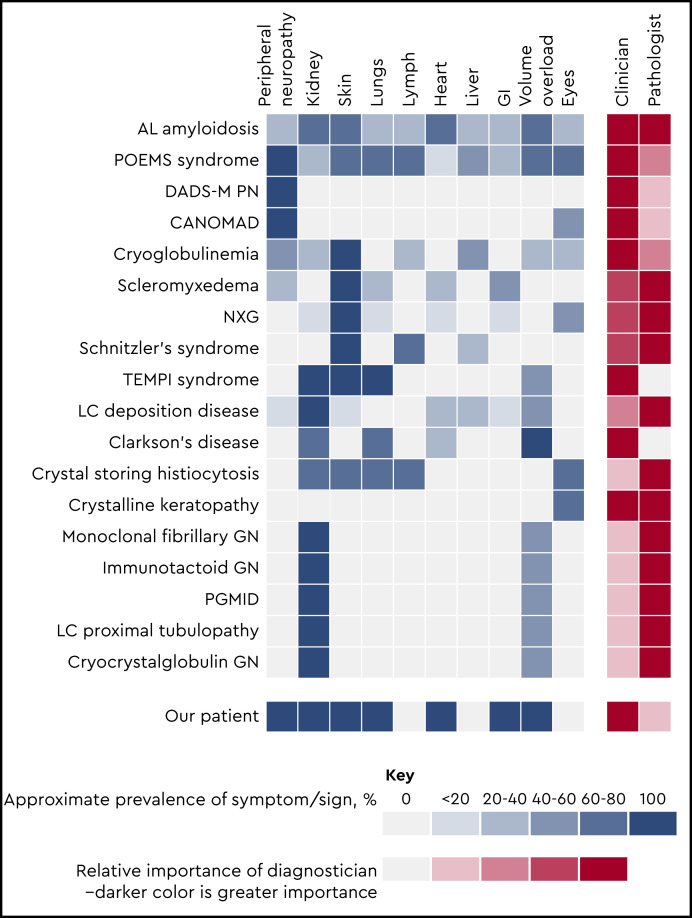
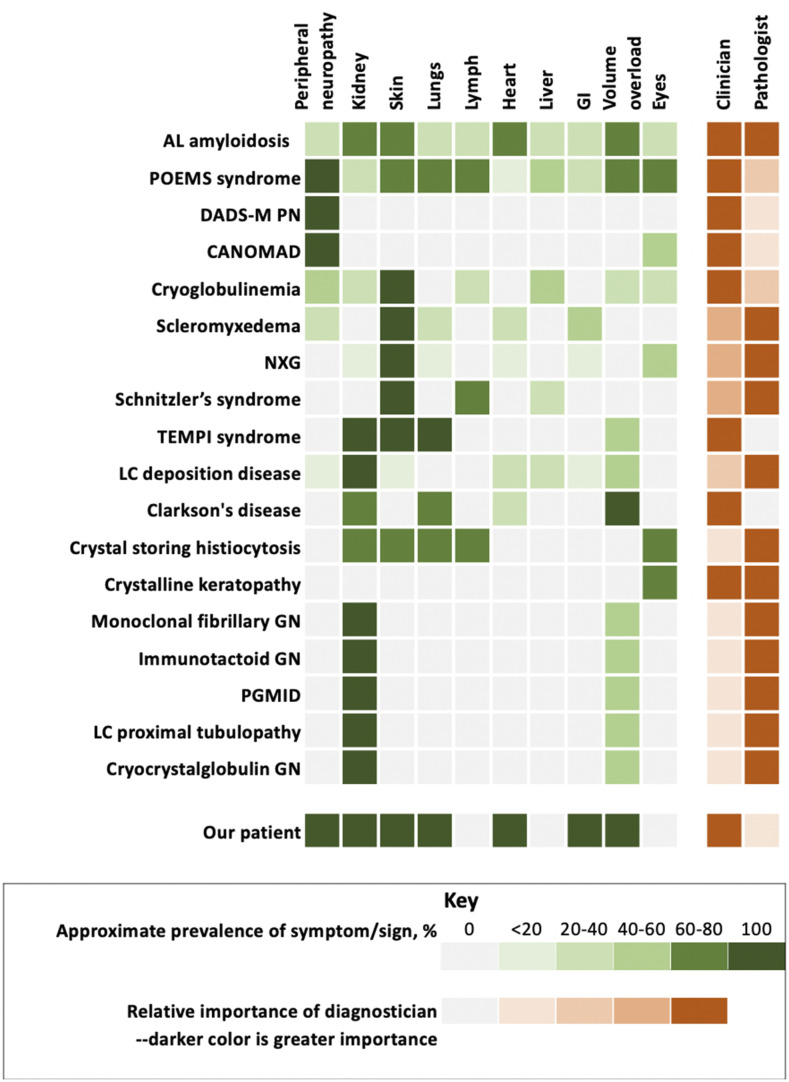
The major MGCS considerations for a patient with neuropathy include (Figure 2) amyloid light-chain (AL) amyloidosis, POEMS syndrome (polyradiculoneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, and skin changes), cryoglobulinemia, CANOMAD (chronic ataxic neuropathy, ophthalmoplegia, immunoglobulin M [IgM] paraprotein, cold agglutinins, and disialosyl antibodies), and DADS-M (distal acquired demyelinating symmetric neuropathy with M protein [formerly known as “MGUS-associated peripheral neuropathy”]). The first three are diseases with multiple systemic manifestations, whereas the last two are primarily in the nervous system only.
Figure 2.
Monoclonal gammopathy of clinical significance and organ system involvement. CANOMAD, chronic ataxic neuropathy, ophthalmoplegia, immunoglobulin M paraprotein, cold agglutinins, and disialosyl antibodies; DADS-M-PN, distal acquired demyelinating symmetric neuropathy with M protein; GN, glomerulonephritis; LC, light chain; NXG, necrobiotic xanthogranuloma; PGMID, proliferative glomerulonephritis with monoclonal immune deposition; POEMS, polyradiculoneuropathy, organomegaly, endocrinopathy, monoclonal protein, skin changes.
POEMS syndrome
POEMS syndrome is the acronym for polyradiculoneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, and skin changes.3 It is a rare condition with a prevalence of 3 per 1 million. Median age at presentation is in the 50s, and there are slightly more men than women affected. Symptoms and signs refer to the acronym as well as features covered by another acronym, PEST, which includes papilledema, extravascular volume overload, sclerotic bone lesions (Figure 1B), thrombocytosis, and erythrocytosis. Other elements not covered in either of the acronyms are elevated vascular endothelial growth factor, pulmonary hypertension, reduced diffusion capacity of carbon monoxide, and arterial and venous thromboembolisms (Table 2). The dominant symptom in this disease is a progressive length-dependent ascending sensorimotor demyelinating peripheral neuropathy.
Table 2.
Diagnostic criteria for five selected syndromes
| POEMS syndrome*3 | Schnitzler syndrome†‡16 | Necrobiotic xanthogranuloma§21 | Scleromyxedema18 | TEMPI syndrome23 |
|---|---|---|---|---|
| Mandatory major criteria | Obligate criteria | Major criteria | 1. Generalized papular and sclerodermoid eruption | Major criteria |
| 1. Polyneuropathy (typically demyelinating) | 1. Chronic urticarial rash | 1. Cutaneous papules, plaques, and/or nodules, most often yellow or orange in color | 2. Evidence of monoclonal gammopathy | 1. Telangiectasias |
| 2. Monoclonal plasma cell-proliferative disorder (almost always λ) | 2. Monoclonal IgM or IgG | 2. Histopathological features demonstrating palisading granulomas with lymphoplasmacytic infiltrate and zones of necrobiosis. Variably present cholesterol clefts and/or giant cells | 3. Microscopic triad associating dermal mucin deposition, thickened collagen, and fibroblast proliferation or an interstitial granuloma annulare–like pattern | 2. Monoclonal gammopathy |
| Major criteria | Minor criteria | 3. Elevated erythropoietin and erythrocytosis | ||
| 3. Castleman disease|| | 3. Recurrent fever¶ | Minor criteria | ||
| 4. Sclerotic bone lesions | 4. Objective findings of abnormal bone remodeling with or without bone pain# | Minor criteria | 4. Absence of thyroid disease | 4. Perinephric fluid |
| 5. Vascular endothelial growth factor elevation | 5. A neutrophilic dermal infiltrate on skin biopsy** | 3. Periorbital distribution of cutaneous lesions | 5. Intrapulmonary shunting | |
| Minor criteria | 6. Leukocytosis and/or elevated CRP†† | 4. Paraproteinemia, most often IgG-λ, plasma cell dyscrasia, and/or other associated lymphoproliferative disorder | 6. Other: venous thrombosis | |
|
CRP, C-reactive protein; IgG-λ, immunoglobulin G-λ; POEMS, polyneuropathy, organomegaly, endocrinopathy, M protein, skin changes; TEMPI, telangiectasias, elevated erythropoietin and erythropoiesis, monoclonal gammopathy, perinephric fluid, intrapulmonary shunting.
POEMS syndrome diagnosis is confirmed when both of the mandatory major criteria, 1 of the 3 other major criteria, and 1 of the 6 minor criteria are present.
Definite diagnosis of Schnitzler syndrome: if IgM, both obligate criteria and at least 2 minor criteria; if IgG, both obligate criteria and 3 minor criteria.
Probable diagnosis of Schnitzler syndrome: if IgM, both obligate criteria and 1 minor criteria; if IgG, both obligate criteria and 2 minor criteria.
For necrobiotic xanthogranuloma diagnosis, both major criteria and at least 1 minor criterion, applicable only in the absence of foreign body, infection, or other identifiable cause.
There is a Castleman disease variant of POEMS syndrome that occurs without evidence of a clonal plasma cell disorder that is not accounted for in this table. This entity should be considered separately.
Must be >38°C and otherwise unexplained. Occurs usually—but not obligatory—together with the skin rash.
As assessed by bone scintigraphy, magnetic resonance imaging, or elevation of bone alkaline phosphatase.
Corresponds usually to the entity described as “neutrophilic urticarial dermatosis,” absence of fibrinoid necrosis, and significant dermal edema.
Neutrophils >10 000/mm3 and/or CRP >30 mg/L.
Because of the high prevalence of diabetes mellitus and thyroid abnormalities, this diagnosis alone is not sufficient to meet this minor criterion.
Approximately 50% of patients will have bone marrow changes that distinguish it from a typical monoclonal gammopathy of undetermined significance or myeloma bone marrow. Anemia and/or thrombocytopenia are distinctively unusual in this syndrome unless Castleman disease is present.
Adverse risk factors in this disease are age, pleural effusion, reduced estimated glomerular filtration rate, pulmonary hypertension, coexisting Castleman disease, and lack of complete hematologic response to plasma cell–directed therapy.4 Autologous stem cell transplant (ASCT) is a favored therapy, but lenalidomide and dexamethasone are also active (Table 3).5,6 Data associated with use of proteasome inhibitors and daratumumab are emerging. Overall survival in patients with POEMS syndrome is excellent with plasma cell–directed therapy, with estimated 10-year survivorship at 79%.
Table 3.
Treatments
| Conditions | Therapy |
|---|---|
| POEMS syndrome | First line: most experience with ASCT and lenalidomide/dexamethasoneFirst line: if only 1-2 bone lesions and negative bone marrow, radiation |
| DADS-M-PN | First line: IVIGSecond line: rituximab |
| CANOMAD | First line: IVIG or plasmapheresisSecond line: rituximab |
| SLOMN | First line: IVIGSecond line: plasma cell–directed therapy |
| Light chain deposition disease | First line: most experience with ASCT and bortezomib/dexamethasone |
| PGMID | First line: rituximabSecond line: bortezomib/dexamethasone |
| Monoclonal fibrillary glomerulonephritis | First line: unknown |
| Immunotactoid GN | First line: rituximab or clone directed therapy |
| Inclusions/crystalline deposits | First line: may consider clone-directed therapy |
| Cryoglobulinemia | First line: treat underlying cause (eg, HCV, CTD, PCD); for severe cases, plasmapheresis, high-dose methylprednisolone, and/or cyclophosphamide may be consideredSecond line: rituximab |
| Scleromyxedema | First line: IVIGSecond line: add lenalidomide or bortezomib |
| Necrobiotica xanthogranuloma | First line: IVIGSecond line: may consider clone-directed therapy |
| Schnitzler syndrome | First line: anti–IL-1 monoclonal therapeuticsSecond line: Waldenstrom macroglobulinemia therapy |
| TEMPI syndrome | First line: plasma cell–directed therapy |
| Clarkson disease | Prophylactic IVIG |
| Crystal-storing histiocytosis29 | First line: observationSecond line: may consider clone-directed therapy |
| Monoclonal gammopathy keratopathy | No treatment required |
These treatments are based on case series and not on high levels of evidence.
ASCT, autologous stem cell transplant; CANOMAD, chronic ataxic neuropathy, ophthalmoplegia, immunoglobulin M paraprotein, cold agglutinins, and disialosyl antibodies; CTD, connective tissue disease; DADS-M-PN, distal, acquired, demyelinating, symmetric neuropathy with M protein; GN, glomerulonephritis; HCV, hepatitis C virus; IL-1, interleukin-1; IVIG, intravenous immunoglobulin; PCD, plasma cell disorder; PGMID, proliferative glomerulonephritis with monoclonal immune deposition; POEMS, polyradiculoneuropathy, organomegaly, endocrinopathy, monoclonal protein, skin changes; SLOMN, sporadic late-onset nemaline myopathy.
DADS-M
IgM monoclonal gammopathy accounts for ∼60% of neuropathies associated with monoclonal gammopathy.7 Patients are more often male and in their 50s to 80s. They present with a distal, demyelinating symmetric neuropathy. Sensory ataxia is the most common sign. The diagnosis is one of exclusion. Even in the presence of a monoclonal gammopathy, other explanations, such as inherited neuropathies, diabetes, alcoholism, and drug use, should be ruled out.
Pathologic studies have identified demyelination and widened myelin lamellae with IgM deposits in the widened lamellae of myelin fibers and myelin debris contained in Schwann cells and macrophages. Despite the fact that these M proteins may bind to myelin-associated glycoprotein (MAG) or other gangliosides, anti-MAG antibodies are not specific for peripheral neuropathy, and reduction in anti-MAG antibody titers with rituximab or other anti-CD20 antibodies has not correlated with clinical improvement. Treatments include IV immunoglobulin (IVIG) and rituximab.
CANOMAD
CANOMAD is a rare condition characterized by a chronic neuropathy with sensory ataxia and IgM disialosyl antibodies.8 Patients may or may not have motor weakness involving oculomotor and bulbar muscles or cold agglutinins. The most frequently targeted gangliosides are CD1b, GD3, GT1b, and GQ1b. Both axonal and demyelinating patterns have been recognized. The most effective therapies are IVIG, rituximab, and plasmapheresis.
Sporadic late-onset nemaline myopathy
Sporadic late-onset nemaline myopathy is a rare muscle disease that can be associated with a monoclonal protein or HIV infection.9 It is not a neuropathy, but it does cause significant motor dysfunction. On biopsy, muscle fibers accumulate nemaline rods, and there is no associated inflammation. Patients present with predominantly proximal or axial muscle weakness, including respiratory muscle weakness. Treatment strategies include IVIG and plasma cell–directed therapies, including ASCT.
Our patient had a symmetrical, ascending, demyelinating, sensorimotor peripheral neuropathy, along with systemic signs. The multisystemic nature of his disease made CANOMAD and DADS-M unlikely. Although AL amyloidosis and cryoglobulinemia are multisystemic diseases, the former is associated with a small-fiber neuropathy and the latter with an axonal neuropathy due to vasculitis.
Monoclonal gammopathy of renal significance
MGRS is a group of disorders in which a monoclonal immunoglobulin secreted by a nonmalignant or premalignant B-cell or plasma cell clone causes renal damage. As shown in Figure 2, several conditions are renal only, whereas others potentially have systemic features. All MGRS diagnoses without other systemic features are made by a renal pathologist (Figure 2). With the exception of C3 glomerulopathy with monoclonal gammopathy and thrombotic microangiopathy, the other MGRSs are broken into “nonorganized monoclonal immunoglobulin deposits” and “organized” monoclonal immunoglobulin deposits.10 The nonorganized deposits include monoclonal immunoglobulin deposition disease and proliferative glomerulonephritis with monoclonal immune deposits. In contrast, the organized deposits are categorized as (1) fibrillar deposits, which include AL amyloidosis and monoclonal fibrillary glomerulonephritis; (2) microtubular deposits, which include immunotactoid glomerulonephritis and cryoglobulinemia glomerulonephritis; and (3) inclusions or crystalline deposits, which include light chain proximal tubulopathy, crystal-storing histiocytosis, and cryocrystalglobulin glomerulonephritis.
This classification allows for a uniform vocabulary among nephrologists, renal pathologists, and hematologists such that diagnostic algorithms can be constructed and natural history and therapeutic interventions can be analyzed (Table 3). Although renal transplant can be considered in these patients, there is risk for recurrence.11 Which diseases respond best to which plasma cell or lymphoproliferative disease–directed therapies is still a work in progress. The most data exist on light chain deposition disease (LCDD), so that topic is described next.
LCDD
LCDD shares similarities with AL amyloidosis in that both are immunoglobulin deposition diseases. Both can rarely involve immunoglobulin heavy chains as well. LCDD is less common than AL amyloidosis, less likely to involve other organs, and more often is due to a κ-restricted light chain (immunoglobulin kappa variable 4 [IGKV4]) and to present with impaired creatinine clearance. The median plasmacytosis in the bone marrow is ∼10%.12,13 Immunofluorescence of the kidney biopsy reveals linear deposits of the involved monoclonal immunoglobulin along tubular basement membranes and along glomerular basement membranes. Electron microscopy shows that these deposits have a granular appearance.
Treatment is similar to that used for patients with AL, and survival tends to be better because it is unusual for patients with LCCD to have cardiac involvement. Although our patient had reduced renal function and mild proteinuria, no renal biopsy was performed. The renal injury was presumed to be due to hypotension and exuberant application of diuretics. Significant renal disease is rare in POEMS syndrome, but numerous pathologic changes have been reported, including membranoproliferative glomerulonephritis–like lesions, microangiopathic lesions, mesangiolytic lesions, and even immunotactoid lesions.
Cutaneous MGCSs
Cutaneous MGCSs include Schnitzler syndrome, scleromyxedema, necrobiotic xanthogranuloma (NXG), TEMPI syndrome (telangiectasias, elevated erythropoietin and erythropoiesis, monoclonal gammopathy, perinephric fluid, intrapulmonary shunting), cryoglobulinemia, systemic capillary leak syndrome (SCLS), and POEMS syndrome.
Schnitzler syndrome
Schnitzler syndrome is characterized primarily by chronic urticaria (Figure 1C) and the presence of an IgM monoclonal gammopathy. Interleukin (IL)-1β plays a critical role in in the disease. Aberrant NLRP3 inflammasome signaling and cytokine pathway dysregulation also play a role. Schnitzler syndrome can rarely be associated with an IgG monoclonal gammopathy. Other features and diagnostic criteria are shown in Figure 2 and Table 2.14-16 Although the presence of a dermal neutrophilic infiltrate on skin biopsy became a minor criterion with the Strasbourg revision, such a biopsy finding is nonspecific, and its relative importance in the diagnostic criteria has been questioned. Therapy with anakinra, an anti–IL-1 antibody, is quite effective (Table 3). More novel anti–IL-1 antibodies, such as rilonacept and canakinumab, have also been effective.17 Following C-reactive protein can be helpful in monitoring this disease.
Scleromyxedema
Scleromyxedema is characterized by generalized papular and sclerodermoid cutaneous eruptions (Figure 1D-E) and is typically associated with an IgG monoclonal gammopathy.18 Extracutaneous involvement can include the nervous system, joints, gastrointestinal system, and heart (Figure 2). The infiltrates are composed of mucin. How the monoclonal protein induces fibroblast proliferation is not well understood. The science behind the pathology is gradually emerging through skin transcriptome analyses and the study of peripheral blood immune cells. Transforming growth factor-β is overexpressed. Other proteins, including collagen Ia and several interferon-inducible proteins, are also overexpressed.19,20 Diagnostic criteria are shown in Table 2. IVIG is considered first-line therapy, with plasma cell–directed therapy (eg, lenalidomide or bortezomib) added if no response is achieved or more severe disease develops (Table 3).20
NXG
NXG is a non–Langerhans cell histiocytosis typically associated with monoclonal proteins attributable to plasma cell disorders or lymphoproliferative disorders. The mean age of presentation is 62 years, with a slight predominance of women.21 The classic presentation is yellow-to-orange papules, plaques, and/or nodules involving the eyelids (Figure 1F). Cutaneous lesions may also be found on other locations of the face, the trunk, and the extremities. NXG plaques can occasionally be pruritic and also painful if they ulcerate. Extracutaneous involvement includes the eye, heart, gastrointestinal tract, liver, and lung but is relatively rare (Figure 2). A French group has suggested an association between monoclonal gammopathy and both hyperlipidemic and nonhyperlipidemic xanthomatosis and suggested that the association can be strengthened if complement levels, especially C4, are low.22
On biopsy of NXG, palisading granulomas with nonclonal lymphoplasmacytic infiltrate and zones of necrobiosis are seen. Cholesterol clefts and large bizarre foreign body giant cells are also classic. The pathogenesis of the disease is unknown, but it has been speculated that there is a monoclonal protein–lipoprotein interaction. Diagnostic criteria have been proposed (Table 2). The leading differential diagnosis is necrobiosis lipoidica, which is a necrotizing skin condition that can occur in patients with diabetes mellitus or rheumatoid arthritis. In contrast to monoclonal gammopathy–associated hyperlipidemic and nonhyperlipidemic xanthomatosis, CD163-positive foam cells and Touton giant cells are seen but typically without necrobiosis. Treatment with IVIG is one of the most promising therapies, but limited success has also been reported with plasma cell–directed therapies, intralesional triamcinolone, and antimalarials.
TEMPI syndrome
TEMPI syndrome is a rare acquired disorder characterized by the features that comprise the acronym: telangiectasias, elevated erythropoietin and erythrocytosis, monoclonal gammopathy, perinephric fluid collections, and intrapulmonary shunting.23 The underlying pathophysiology is not understood, but it is clear that plasma cell–directed therapy reverses the clinical manifestations.
Telangiectasias involving the face and upper body and erythrocytosis comprise the most common presentation. Unlike the erythrocytosis of polycythemia rubra vera and of POEMS syndrome, patients with TEMPI syndrome have a high erythropoietin level.24 These patients develop progressive hypoxia. The pulmonary shunting is not evident on high-resolution computed tomography of the chest and is best demonstrated by 99mTc macroaggregated albumin scintigraphy. The perinephric fluid collections have the same electrolyte composition as serum. Proposed diagnostic criteria are shown in Table 2. Unlike POEMS syndrome, there is no bias in clonality for λ-restricted clones, and there are no features of a myeloproliferative neoplasm.
Plasma cell–directed therapy appears to be useful, specifically bortezomib, daratumumab, lenalidomide, and high-dose melphalan. All of the features can improve upon achievement of complete hematologic response (Table 3).
Cryoglobulinemia
Cryoglobulinemia is a multisystem disease that can affect almost any organ system, but cutaneous manifestations are almost always present (Figure 1G). Type I cryoglobulins arise from clonal plasma cell proliferative disorders or lymphoproliferative disorders. Type II and type III cryoglobulins may be related to plasma cell disorders or lymphoporliferative disorders but are more often due to infections such as hepatitis C virus and connective tissue disorders.25
Manifestations and disease severity are quite variable. Type I cryoglobulins more often cause occlusive symptoms due to occlusion of capillary lumina, and vasculitis is uncommon.25 Patients report cold-induced skin symptoms, including purpura, livedo, and cold urticaria. Ulceration can occur. Less than one-third of patients will have renal involvement, but up to 50% may have peripheral neuropathy. In contrast, in type II/III cryoglobulinemia or mixed cryoglobulinemia, small-vessel vasculitis is the major mechanism driving morbidity. Skin symptoms, including purpura, occur in the vast majority of patients; arthralgia is also very common in peripheral neuropathy followed by renal involvement.
The aim of treatment of cryoglobulinemia is to treat the underlying cause. For patients with hepatitis C virus, who comprise the majority of type II and III cases, sustained virologic responses can be achieved in >50% with antiviral therapy. For patients not responding to antiviral therapy, rituximab and other immunosuppressants can play an important role in treating vasculitis. For disease driven by autoimmune disease, rituximab and corticosteroids are the best first-line options. Plasmapheresis can be used in patients with severe end organ damage and/or refractory disease.26 Other disease modifiers, including corticosteroids and cyclophosphamide, can also play a role in therapy, especially in patients with severe end organ damage.
Idiopathic SCLS (Clarkson disease)
This devastating disease was first described in 1960. SCLS is characterized capillary leak resulting in sudden-onset shock and anasarca caused by plasma extravasation (up to 70% of total plasma volume). The diagnostic triad is composed of the “3 Hs,” which occur in the absence of secondary causes of these findings: hypotension, hemoconcentration, and hypoalbuminemia. Sixty-eight percent of adult patients with SCLS have monoclonal proteins, most commonly IgG-κ. Details of the limited understanding of disease mechanisms of the vascular endothelial hyperpermeability of SCLS can be found in a review published elsewhere.27
The differential diagnosis for an acute attack includes sepsis, anaphylaxis, and hereditary angioedema. Treatment at the time of an acute attack is supportive with fluid resuscitation until flare subsides, which typically occurs over the course of a few days. Empiric prophylaxis with IVIG is recommended because it has been demonstrated that there are fewer attacks in those patients managed as such.28
POEMS syndrome
Our patient had POEMS syndrome evolving over the course of nearly 18 months. His first symptoms were those of adrenal insufficiency and peripheral neuropathy. His characteristics and his course are summarized in Figure 2 and Table 1. His case exemplifies the importance of an extensive review of systems in patients with a monoclonal protein and other unexplained conditions. A focused review of systems prompts additional testing from scans to disease-oriented blood work and/or biopsies. By the time he was diagnosed, our patient had a performance score of 4 and was bedridden with bedsores. With adrenal and thyroid replacement and plasma cell clone-directed therapy, his life has returned to nearly normal, though he does still use ankle foot orthotics. Had the syndrome not been considered, he would have died. Five years later, he continues to enjoy life.
In summary, MGCSs are a constellation of diseases associated with clonal—but not malignant–B cells or plasma cells that produce monoclonal proteins and pathology through diverse, often ill-defined mechanisms. Similar end organ damage can occur in the context of malignant plasma cell or B-cell clonal disorders, but these are no longer MGCSs, but rather the cancer with associated disease (eg, myeloma with associated cryoglobulinemia). The most commonly affected organs among patients with MGCS are the kidney, nerve, and skin. A thorough discussion of all of the MGCSs is beyond the scope of this article, but Table 4 highlights some of the most recent and relevant references pertaining to MGCS. Some MGCSs predominantly affect only one organ, and others are systemic diseases affecting multiple organ systems. In order to help patients, these diagnoses and the severity of the symptoms must be considered so that appropriate therapy may be instituted. Conversely, not every patient with a monoclonal gammopathy and an unexplained symptom or sign has MGCS, given the high prevalence of true MGUS, especially with advancing age. In many instances, the appropriate therapy is clone-directed therapy, even though there is no malignancy; in others, data indicate that therapies such as IVIG, rituximab, or anti–IL-1 antibodies are most appropriate. The treating physician should strive to assign causality before proceeding with clone-directed therapy.
Table 4.
Selected relevant references
| Conditions | References |
|---|---|
| Neurologic POEMS syndrome Distal acquired demyelinating symmetric neuropathy with monoclonal protein (DADS-M) Chronic ataxic neuropathy, ophthalmoplegia, IgM paraprotein, cold agglutinins, and disialosyl antibodies (CANOMAD) Sporadic late-onset nemaline myopathy (SLOMN) | 3-6,7,8,9 |
| Renal10 AL amyloidosis Monoclonal immunoglobulin deposition disease Proliferative glomerulonephritis with monoclonal immunoglobulin deposition (PGMID) Monoclonal fibrillary glomerulonephritis Monoclonal fibrillary glomerulonephritis Cryoglobulinemia Immunotactoid glomerulonephritis Acquired Fanconi syndrome and other light chain proximal tubulopathies Crystal-storing histiocytosis C3 glomerulonephritis Monoclonal gammopathy–associated thrombotic microangiopathy | 30,12,13,11,31,32,25,26,33,34,29,35,36 |
| Dermatologic Schnitzler syndrome Scleromyxedema Necrobiotica xanthogranuloma Hyperlipidemic and nonhyperlipidemic xanthomatosis TEMPI syndrome Acquired cutis laxa Neutrophilic dermatosis Clarkson disease (systemic capillary leak syndrome) Macroglobulinosis | 14-17,18-20,21,22,22,23,37,38,27,28,39 |
| Other Monoclonal gammopathy keratopathy Acquired C1 inhibitor deficiency Acquired von Willebrand disease Cold agglutinin disease | 40,41,42,43 |
A single category was chosen for systemic diseases. See Figure 2, which demonstrates multiorgan involvement.
AL, amyloid light chain; POEMS, polyradiculoneuropathy, organomegaly, endocrinopathy, monoclonal protein, skin changes; TEMPI, telangiectasias, elevated erythropoietin and erythropoiesis, monoclonal gammopathy, perinephric fluid, intrapulmonary shunting.
References
- 1.Leung N, Bridoux F, Hutchison CA, et al. ; International Kidney and Monoclonal Gammopathy Research Group. Monoclonal gammopathy of renal significance: when MGUS is no longer undetermined or insignificant. Blood. 2012;120(22):4292-4295. [DOI] [PubMed] [Google Scholar]
- 2.Fermand JP, Bridoux F, Dispenzieri A, et al. . Monoclonal gammopathy of clinical significance: a novel concept with therapeutic implications. Blood. 2018;132(14):1478-1485. [DOI] [PubMed] [Google Scholar]
- 3.Dispenzieri A. POEMS syndrome: 2019 update on diagnosis, risk-stratification, and management. Am J Hematol. 2019;94(7):812-827. [DOI] [PubMed] [Google Scholar]
- 4.Wang C, Huang XF, Cai QQ, et al. . Prognostic study for overall survival in patients with newly diagnosed POEMS syndrome. Leukemia. 2017;31(1):100-106. [DOI] [PubMed] [Google Scholar]
- 5.D’Souza A, Lacy M, Gertz M, et al. . Long-term outcomes after autologous stem cell transplantation for patients with POEMS syndrome (osteosclerotic myeloma): a single-center experience. Blood. 2012;120(1):56-62. [DOI] [PubMed] [Google Scholar]
- 6.Zhao H, Huang XF, Gao XM, et al. . What is the best first-line treatment for POEMS syndrome: autologous transplantation, melphalan and dexamethasone, or lenalidomide and dexamethasone? Leukemia. 2019;33(4):1023-1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaudhry HM, Mauermann ML, Rajkumar SV. Monoclonal gammopathy-associated peripheral neuropathy: diagnosis and management. Mayo Clin Proc. 2017;92(5):838-850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yuki N, Uncini A. Acute and chronic ataxic neuropathies with disialosyl antibodies: a continuous clinical spectrum and a common pathophysiological mechanism. Muscle Nerve. 2014;49(5):629-635. [DOI] [PubMed] [Google Scholar]
- 9.Naddaf E, Milone M, Kansagra A, Buadi F, Kourelis T. Sporadic late-onset nemaline myopathy: clinical spectrum, survival, and treatment outcomes. Neurology. 2019;93(3):e298-e305. [DOI] [PubMed] [Google Scholar]
- 10.Leung N, Bridoux F, Batuman V, et al. . The evaluation of monoclonal gammopathy of renal significance: a consensus report of the International Kidney and Monoclonal Gammopathy Research Group. Nat Rev Nephrol. 2019;15(1):45-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Said SM, Cosio FG, Valeri AM, et al. . Proliferative glomerulonephritis with monoclonal immunoglobulin G deposits is associated with high rate of early recurrence in the allograft. Kidney Int. 2018;94(1):159-169. [DOI] [PubMed] [Google Scholar]
- 12.Joly F, Cohen C, Javaugue V, et al. . Randall-type monoclonal immunoglobulin deposition disease: novel insights from a nationwide cohort study. Blood. 2019;133(6):576-587. [DOI] [PubMed] [Google Scholar]
- 13.Kourelis TV, Nasr SH, Dispenzieri A, et al. . Outcomes of patients with renal monoclonal immunoglobulin deposition disease. Am J Hematol. 2016;91(11):1123-1128. [DOI] [PubMed] [Google Scholar]
- 14.Gusdorf L, Asli B, Barbarot S, et al. . Schnitzler syndrome: validation and applicability of diagnostic criteria in real-life patients. Allergy. 2017;72(2):177-182. [DOI] [PubMed] [Google Scholar]
- 15.Rowczenio DM, Pathak S, Arostegui JI, et al. . Molecular genetic investigation, clinical features, and response to treatment in 21 patients with Schnitzler syndrome. Blood. 2018;131(9):974-981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simon A, Asli B, Braun-Falco M, et al. . Schnitzler’s syndrome: diagnosis, treatment, and follow-up. Allergy. 2013;68(5):562-568. [DOI] [PubMed] [Google Scholar]
- 17.Krause K, Bonnekoh H, Ellrich A, et al. . Long-term efficacy of canakinumab in the treatment of Schnitzler syndrome. J Allergy Clin Immunol. 2020;145(6):1681-1686.e5. [DOI] [PubMed] [Google Scholar]
- 18.Rongioletti F, Merlo G, Carli C, et al. . Histopathologic characteristics of scleromyxedema: a study of a series of 34 cases. J Am Acad Dermatol. 2016;74(6):1194-1200. [DOI] [PubMed] [Google Scholar]
- 19.Mecoli CA, Talbot CC Jr, Fava A, et al. . Clinical and molecular phenotyping in scleromyxedema pretreatment and posttreatment with intravenous immunoglobulin. Arthritis Care Res (Hoboken). 2020;72(6):761-767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahévas T, Arnulf B, Bouaziz JD, et al. . Plasma cell-directed therapies in monoclonal gammopathy-associated scleromyxedema. Blood. 2020;135(14):1101-1110. [DOI] [PubMed] [Google Scholar]
- 21.Nelson CA, Zhong CS, Hashemi DA, et al. . A multicenter cross-sectional study and systematic review of necrobiotic xanthogranuloma with proposed diagnostic criteria. JAMA Dermatol. 2020;156(3):270-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Szalat R, Arnulf B, Karlin L, et al. . Pathogenesis and treatment of xanthomatosis associated with monoclonal gammopathy. Blood. 2011;118(14):3777-3784. [DOI] [PubMed] [Google Scholar]
- 23.Sykes DB, O’Connell C, Schroyens W. The TEMPI syndrome. Blood. 2020;135(15):1199-1203. [DOI] [PubMed] [Google Scholar]
- 24.Rosado FG, Oliveira JL, Sohani AR, et al. . Bone marrow findings of the newly described TEMPI syndrome: when erythrocytosis and plasma cell dyscrasia coexist. Mod Pathol. 2015;28(3):367-372. [DOI] [PubMed] [Google Scholar]
- 25.Desbois AC, Cacoub P, Saadoun D. Cryoglobulinemia: an update in 2019. Joint Bone Spine. 2019;86(6):707-713. [DOI] [PubMed] [Google Scholar]
- 26.Galli M, Monti G, Marson P, et al. . Recommendations for managing the manifestations of severe and life-threatening mixed cryoglobulinemia syndrome. Autoimmun Rev. 2019;18(8):778-785. [DOI] [PubMed] [Google Scholar]
- 27.Druey KM, Parikh SM. Idiopathic systemic capillary leak syndrome (Clarkson disease). J Allergy Clin Immunol. 2017;140(3):663-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xie Z, Chan EC, Long LM, Nelson C, Druey KM. High-dose intravenous immunoglobulin therapy for systemic capillary leak syndrome (Clarkson disease). Am J Med. 2015;128(1):91-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dogan S, Barnes L, Cruz-Vetrano WP. Crystal-storing histiocytosis: report of a case, review of the literature (80 cases) and a proposed classification. Head Neck Pathol. 2012;6(1):111-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Merlini G, Dispenzieri A, Sanchorawala V, et al. . Systemic immunoglobulin light chain amyloidosis. Nat Rev Dis Primers. 2018;4(1):38. [DOI] [PubMed] [Google Scholar]
- 31.van Kruijsdijk RCM, Abrahams AC, Nguyen TQ, Minnema MC, Jacobs JFM, Limper M. Clone-directed therapy for proliferative glomerulonephritis with monoclonal immunoglobulin depositions: is it always necessary? Two case reports and literature review. J Nephrol. 2020;33(3):611-617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nasr SH, Vrana JA, Dasari S, et al. . DNAJB9 is a specific immunohistochemical marker for fibrillary glomerulonephritis. Kidney Int Rep. 2018;3(1):56-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nasr SH, Fidler ME, Cornell LD, et al. . Immunotactoid glomerulopathy: clinicopathologic and proteomic study. Nephrol Dial Transplant. 2012;27(11):4137-4146. [DOI] [PubMed] [Google Scholar]
- 34.Vignon M, Javaugue V, Alexander MP, et al. . Current anti-myeloma therapies in renal manifestations of monoclonal light chain-associated Fanconi syndrome: a retrospective series of 49 patients. Leukemia. 2017;31(1):123-129. [DOI] [PubMed] [Google Scholar]
- 35.Chauvet S, Frémeaux-Bacchi V, Petitprez F, et al. . Treatment of B-cell disorder improves renal outcome of patients with monoclonal gammopathy-associated C3 glomerulopathy. Blood. 2017;129(11):1437-1447. [DOI] [PubMed] [Google Scholar]
- 36.Ravindran A, Go RS, Fervenza FC, Sethi S. Thrombotic microangiopathy associated with monoclonal gammopathy. Kidney Int. 2017;91(3):691-698. [DOI] [PubMed] [Google Scholar]
- 37.Jachiet M, Harel S, Saussine A, et al. ; Groupe d’Etude des Dermatoses Associées à une Immunoglobuline Monoclonale. Cutis laxa associated with monoclonal gammopathy: 14 new cases and review of the literature. J Am Acad Dermatol. 2018;79(5):945-947. [DOI] [PubMed] [Google Scholar]
- 38.Szalat R, Monsel G, Le Goff W, et al. . The spectrum of neutrophilic dermatoses associated with monoclonal gammopathy: association with IgA isotype and inflammatory profile. J Am Acad Dermatol. 2015;73(5):809-820. [DOI] [PubMed] [Google Scholar]
- 39.Camp BJ, Magro CM. Cutaneous macroglobulinosis: a case series. J Cutan Pathol. 2012;39(10):962-970. [DOI] [PubMed] [Google Scholar]
- 40.Milman T, Kao AA, Chu D, et al. . Paraproteinemic keratopathy: the expanding diversity of clinical and pathologic manifestations. Ophthalmology. 2015;122(9):1748-1756. [DOI] [PubMed] [Google Scholar]
- 41.Gobert D, Paule R, Ponard D, et al. . A nationwide study of acquired C1-inhibitor deficiency in France: characteristics and treatment responses in 92 patients. Medicine (Baltimore). 2016;95(33):e4363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dicke C, Schneppenheim S, Holstein K, et al. . Distinct mechanisms account for acquired von Willebrand syndrome in plasma cell dyscrasias. Ann Hematol. 2016;95(6):945-957. [DOI] [PubMed] [Google Scholar]
- 43.Swiecicki PL, Hegerova LT, Gertz MA. Cold agglutinin disease. Blood. 2013;122(7):1114-1121. [DOI] [PubMed] [Google Scholar]