Abstract
Background:
Despite the substantial role indoor exposure has played in heat wave–related mortality, few epidemiological studies have examined the health effects of exposure to indoor heat. As a result, knowledge gaps regarding indoor heat–health thresholds, vulnerability, and adaptive capacity persist.
Objective:
We evaluated the role of indoor heat exposure on mortality and morbidity among the elderly ( of age) in Houston, Texas.
Methods:
Mortality and emergency hospital admission data were obtained through the Texas Department of State Health Services. Summer indoor heat exposure was modeled at the U.S. Census block group (CBG) level using building energy models, outdoor weather data, and building characteristic data. Indoor heat–health associations were examined using time-stratified case-crossover models, controlling for temporal trends and meteorology, and matching on CBG of residence, year, month, and weekday of the adverse health event. Separate models were fitted for three indoor exposure metrics, for individual lag days 0–6, and for 3-d moving averages (lag 0–2). Effect measure modification was explored via stratification on individual- and area-level vulnerability factors.
Results:
We estimated positive associations between short-term changes in indoor heat exposure and cause-specific mortality and morbidity [e.g., circulatory deaths, (95% CI: 1.03, 1.30)]. Associations were generally positive for earlier lag periods and weaker across later lag periods. Stratified analyses suggest stronger associations between indoor heat and emergency hospital admissions among African Americans compared with Whites.
Discussion:
Findings suggest excess mortality among certain elderly populations in Houston who are likely exposed to high indoor heat. We developed a novel methodology to estimate indoor heat exposure that can be adapted to other U.S. locations. In locations with high air conditioning prevalence, simplified modeling approaches may adequately account for indoor heat exposure in vulnerable neighborhoods. Accounting for indoor heat exposure may improve the estimation of the total impact of heat on health. https://doi.org/10.1289/EHP6340
Introduction
Extreme heat is a leading cause of weather-related human mortality worldwide (Basu 2009; Basu and Malig 2011; Basu and Samet 2002; Benmarhnia et al. 2015; Braga et al. 2002; Bunker et al. 2016; Gasparrini et al. 2015; Hajat and Kosatky 2010; Kovats et al. 2004; Laaidi et al. 2012). Extreme heat is also associated with increases in the number of hospital admissions and emergency visits due to heat-related cardiovascular disease, respiratory disease, and heat stroke/dehydration (Anderson et al. 2013; Cheng et al. 2014; Lin et al. 2009; Michelozzi et al. 2009; O’Lenick et al. 2017; Winquist et al. 2016; Ye et al. 2012). A cross-section of this literature reveals that children, the elderly, and individuals with chronic health conditions are particularly vulnerable. Studies on heat-related deaths during heat-wave events have reported that decedents were more likely to succumb to heat in their own home (CDC 2013a; Fouillet et al. 2006) and that poor, socially isolated, and elderly populations are at the greatest risk for heat-related mortality (Fouillet et al. 2006; Kaiser et al. 2007; Semenza et al. 1996). These findings implicate indoor environments as a place where exposure to hazardous temperatures occurs and suggest that the risk of heat-related health outcomes is not borne equally by all members of society. However, the vast majority of heat–health studies do not account for exposure to harmful indoor temperatures and typically assess health risks among the general population. Given that individuals, particularly the elderly, spend of their time indoors (Klepeis et al. 2001), health risk analyses that do not include estimates of personal/indoor heat exposure likely underestimate the impact of heat on health and result in underinformed risk assessments, policies, and intervention measures concerning heat exposure (Kuras et al. 2017).
However, because indoor environments are largely dependent on outdoor conditions—as well as properties of the built environment, occupant behavior, and characteristics of individual buildings (e.g., construction, design, and the functioning of heating, ventilation, and air-conditioning systems)—quantifying associations between indoor heat and human health presents a considerable research challenge. Notably, occupant behavior and the ability or willingness to use climate control are dominant influences on indoor thermal comfort (Frey et al. 2014; Klepeis et al. 2017; Kuras et al. 2017). Therefore, estimating indoor exposure for an epidemiological study requires either direct measurements in buildings and information on occupant behavior or simulations of indoor environments based on a detailed understanding of how outdoor temperatures impact indoor environments for different types of building construction, high-resolution (temporal and spatial) meteorological data, and access to large-scale computational resources. Owing to the analytical challenges and complexity of estimating indoor thermal comfort, few studies have investigated relationships between indoor heat and health, and, to date, a population-based study design has not been used to examine the effects of modeled indoor heat on human health.
Among the studies that have investigated relationships between indoor heat and health, results suggest that certain populations experience elevated indoor temperatures, even in cities with a high prevalence of central air conditioning (AC) (Uejio et al. 2016; White-Newsome et al. 2012), and that increases in indoor temperatures may be connected to a variety of health effects, including respiratory emergency calls (Uejio et al. 2016), sleep disturbance (van Loenhout et al. 2016), and cognitive decline (Cedeño Laurent et al. 2018), as well as declines in respiratory function (McCormack et al. 2016). These studies are overwhelmingly cohort based, with indoor measurements taken directly from the home of the affected individual. Using a population-based study design may capture a more complete picture of the impact of heat, indoors and outdoors, on health. However, there are very real barriers to implementing a population-based design, and they primarily stem from the unique analytical challenge of estimating daily indoor thermal comfort at the household and neighborhood level. Thus, there are knowledge gaps in our understanding of the impacts of heat on health, and this is an area of research with considerable potential for growth.
To address this knowledge gap, the research presented here introduces a novel methodology that uses building energy models, parcel-level (building) data, and hourly meteorological data to estimate daily indoor heat exposure for use in a population health study. This work is part of a larger interdisciplinary study, Heat and Ozone in Metropolitan Environments: Assessing Indoor Risks (HOME-AIR) (Sailor et al. 2015). Here, we integrate multiple data products generated by the HOME-AIR study to estimate the impacts of indoor heat exposure on mortality and morbidity among the elderly population in Houston, Texas. The overall project design and data integration follow a conceptual and analytical framework developed by our research team for the HOME-AIR project (O’Lenick et al. 2019).
We selected Houston as the ideal location to develop our methodology because of Houston’s aging population, intensifying urban heat island effect, and socioeconomic disparity. Our previous work in Houston reported that the presence/absence of central AC was a significant determinant of spatial variation in heat vulnerability, and that increases in the percentage of the population of age led to significant increases in expected heat risk at the U.S. Census block group (CBG) level (Heaton et al. 2014). In addition, despite widespread AC prevalence in Houston, a population survey on heat vulnerability during the 2011 summer reported that 37% of respondents felt too hot in their home, and 20% of respondents reported heat-related symptoms in the summer of 2011 (Hayden et al. 2017). Given these findings, we hypothesized that indoor heat exposure has a significant influence on negative health outcomes, particularly for older populations who tend to spend a considerable amount of time indoors. We also hypothesized that observed associations between heat and health will vary across health outcome definitions, indoor heat exposure metrics, lag periods, and vulnerability factors. In this study, indoor heat–health associations were estimated using time-stratified case-crossover models. Separate models were fitted for three indoor exposure metrics, for individual lag days 0 through 6, and for 3-d moving averages (lag 0–2). Effect measure modification was explored via stratification on individual- and area-level vulnerability factors. Few studies have estimated the health impacts of indoor heat among vulnerable populations, and, to our knowledge, this is the first study to use building energy models to estimate daily indoor heat exposure for use in an epidemiological model.
Methods
Study Area
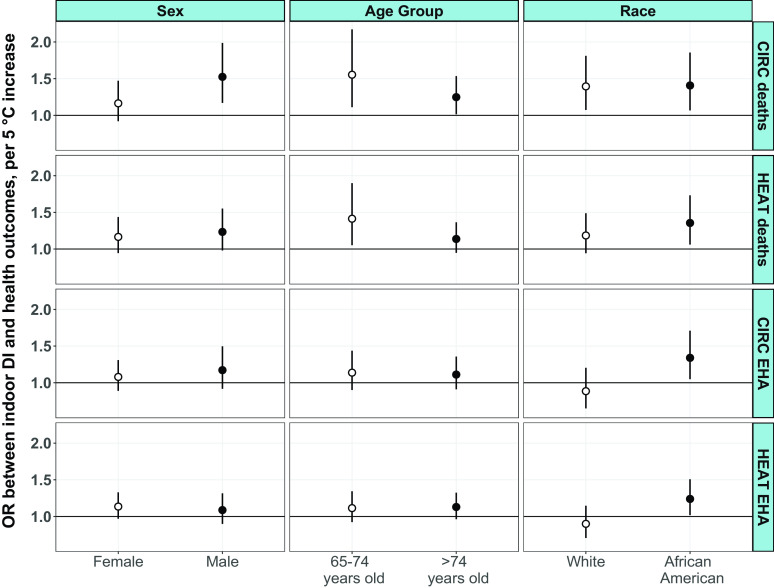
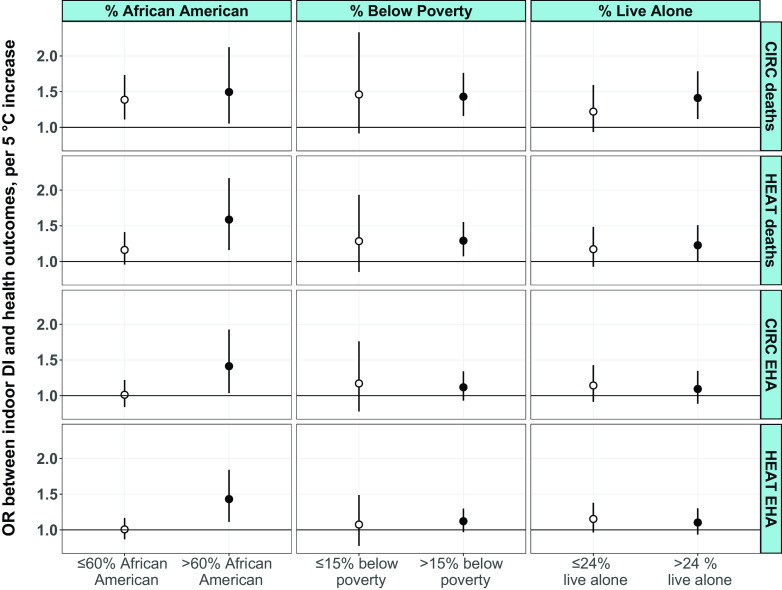
Our study area, Houston, is the largest city in Texas and the fourth largest in the United States, with a 2018 population of 2.3 million (U.S. Census Bureau 2018). Houston is located in Harris County on the gulf coastal plain in southern Texas. Coupled with Houston’s growth, diversity, and hot summer climate come challenges such as an aging population, educational and income disparities, projected increases in high heat stress days and nights (Oleson et al. 2015), and heat-related mortality (Marsha et al. 2018; Rohat et al. 2019). For analyses, our study area was limited to Harris County in Houston, Texas (Figure 1), and the geographic boundary was determined by the availability of health outcome data, meteorological data, ozone concentration data, and Harris County tax assessor data. In 2010, Harris County comprised 2,144 CBGs, with an average population of 2,000. CBGs were included in analyses if they contained any residential buildings. Figure 2 shows the percentage of residential and nonresidential buildings within Harris County CBG boundaries. Eighty-six CBGs were excluded from analyses because all buildings within these block groups were identified as nonresidential (e.g., industrial, church, hospital, university). Sixteen CBGs with residential buildings were excluded because residential buildings could not be categorized into one of 108 building archetypes used in our indoor modeling work. Excluded CBGs with residential buildings () appeared to be randomly distributed across Houston and, based on the 2010–2014 American Community Survey (ACS) data, were relatively affluent (average median income was approximately ). Four residential CBGs in the western part of Harris County were excluded because meteorological data were not available. In total, 2,038 (of 2,144) Harris County CBGs were represented in our analyses.
Figure 1.
Overall map of our study area. Analyses were performed separately for all of Harris County and for City of Houston residents.
Figure 2.
Percentage of residential buildings in Harris County U.S. Census block groups (CBGs) from 2017 Harris County Appraisal District Real and Personal Property Database. Hatched areas represent CBGs excluded from analyses because all buildings within these CBGs were identified as nonresidential or because residential buildings could not be categorized into building archetypes used in our indoor modeling.
Mortality and Morbidity Data
We obtained individual-level mortality data for Harris County residents from death certificate records provided by the Texas Department of State Health Services from 2000 to 2015. We obtained statewide hospital admission data from the Texas Department of State Health Services from 2004 to 2013. We restricted hospital admission data to only those admissions that were coded as urgent or emergency. Emergency hospital admission data were included in analyses if the patient was a Harris County resident who was admitted to a hospital in Harris County, Fort Bent County, Montgomery County, Brazoria County, Galveston County, Liberty County, Waller County, Chambers County, or Austin County. Texas requires all hospitals to submit claims on all discharged inpatients. Thus, this data set represents all eligible residents of Harris County who were admitted to any hospital between 2004 and 2013 in the aforementioned counties.
Relevant data elements on death certificate and emergency hospital admission records included date of admission or death, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM; CDC 2013b) or International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10; WHO 2016) diagnosis codes, age, race, sex, CBG of patient residence, and longitude/latitude of decedent residence. Texas Department of State Health Services provided CBG of residence as a variable for extraction in their hospital admission records, and this variable was used to identify the CBG of residence based on 2010 U.S. Census boundaries. To identify the deceased’s CBG of residence, we spatially overlayed 2010 CBG boundaries to geocoded addresses. Health outcomes of interest were identified using primary ICD-9-CM and ICD-10 diagnosis codes for all circulatory diseases (CIRC; ICD-9-CM codes 390–459, ICD-10 codes I00–I99), all respiratory diseases (ICD-9-CM codes 460–519; ICD-10 codes J00–J99), and a broad health outcome grouping, hereafter referred to as heat related (HEAT), which was created by combining primary diagnoses for circulatory, respiratory, renal (ICD-9-CM codes 580–593; ICD-10 codes N00–N20), and heat stroke/heat exhaustion diagnosis sets (ICD-9-CM codes 992.0–992.9; ICD-10 codes T67.0–T67.9, X30). The HEAT outcome grouping includes any diagnoses plausibly related to heat exposure and for which evidence exists in the literature. We restricted our analysis to the summer months (June–September) and to the elderly population ( of age). The University Corporation for Atmospheric Research (UCAR) and the Texas Department of State Health Services institutional review boards approved this study and granted exemption from informed consent requirements. Ethics approval for human subjects research at the National Center for Atmospheric Research (NCAR) was obtained by the UCAR IRB (IRB00006222) through the Texas Department of State Health Services IRB (14-053), and the University of Texas–Health Science Center Committee for the Protection of Human Subjects (HSC-SPH-14-0783).
Ambient Ozone Concentration and Meteorological Data
We obtained hourly observations of ozone during the summer season (June to September, 2000–2015) from the Texas Commission on Environmental Quality monitoring network for all 86 monitoring sites within the spatial domain of our study area. We then employed ordinary kriging to generate continuous surfaces of daily 8-h maximum ozone concentrations at a spatial resolution of (Michael et al. 2019). Hourly meteorological conditions for the summer months (June–September) from 2000–2015 in the Houston Metropolitan area were modeled at spatial resolution using the High-Resolution Land Data Assimilation System (HRLDAS) (Monaghan et al. 2014). Briefly, the HRLDAS model uses the meteorological monitoring network in Houston and further accounts for land surface, soil properties, and urban geometry (e.g., road surfaces, building types) by coupling an urban canopy model with an offline version of the Noah land surface model (Monaghan et al. 2014). Monaghan et al. (2014) compared the hourly HRLDAS modeled air temperatures to measurements from 17 weather stations across Houston; average biases were during afternoon hours and during nighttime, and centered root-mean-square errors (RMSEs) were about during afternoon hours and during nighttime. Daily minimum, maximum, and mean ambient dry-bulb temperature and maximum ambient dew point temperature were computed from the hourly HRLDAS outputs. Ozone and meteorological metrics used in epidemiological analyses were estimated for each CBG in our study area by using the values closest to the centroid of each CBG. Figure 3 presents summer (June–September) average daily minimum temperature across all CBGs and illustrates the urban heat island effect in Houston.
Figure 3.
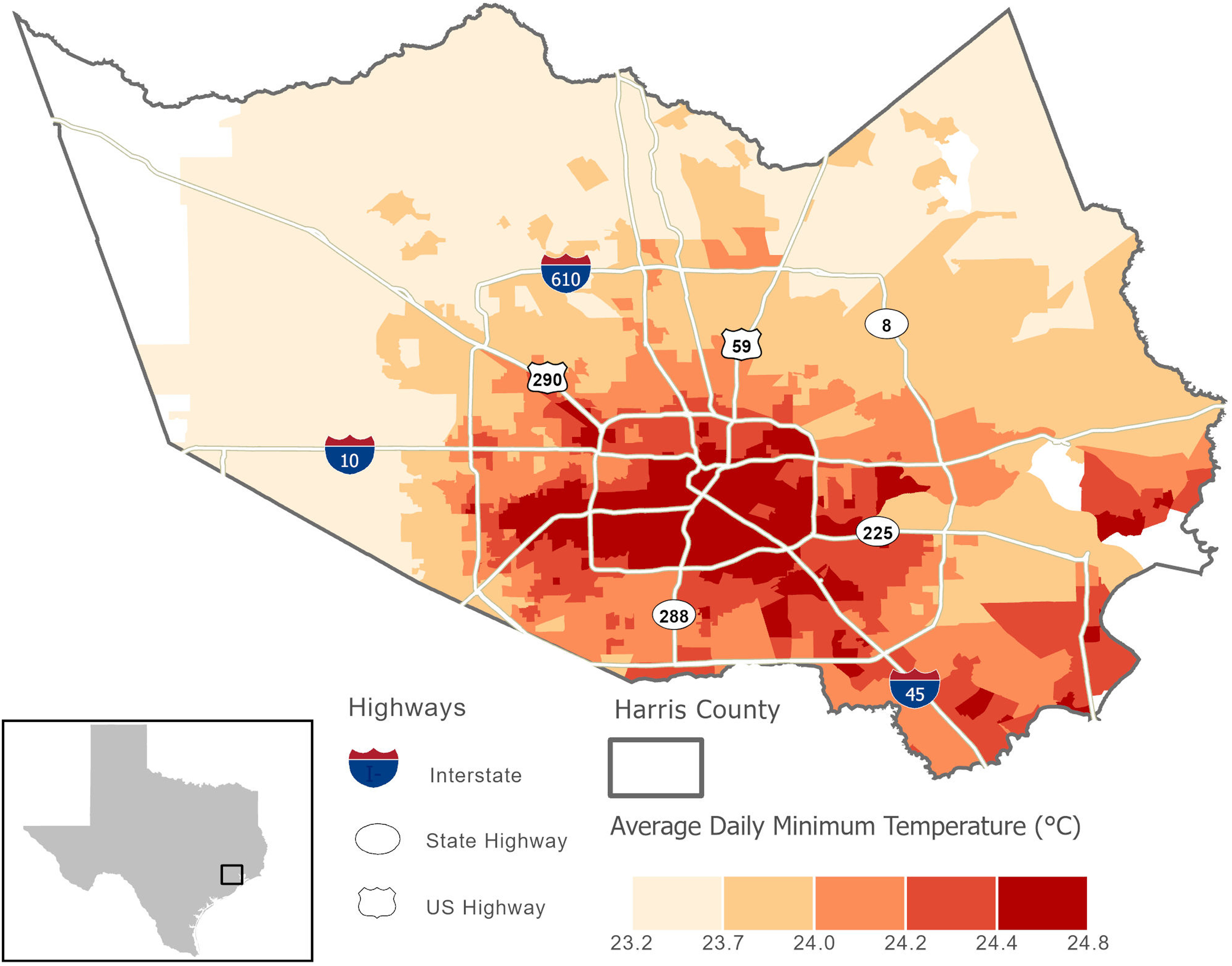
Average daily minimum ambient temperature across U.S. Census block groups in Houston (June–September, 2000–2015). HRLDAS weather data were not available in the blank areas. HRLDAS, High-Resolution Land Data Assimilation System.
Hourly HRLDAS estimates were also used as inputs into the indoor thermal comfort model, as described in the “Modeling Exposure to Indoor Heat” section. For this purpose, we divided our study area into five local climate subregions (Figure S1). Although we had access to meteorological data through HRLDAS at a spatial resolution, it would be too computationally expensive to use the full HRLDAS data set for the indoor modeling. Therefore, we created local climate subregions to resolve spatial differences in local meteorology based on distance from the shore as well as potential urban heat island effects in the city center. Identification of the five local climate subregions was informed by a Houston-based study that demonstrated that distance to the coastline was the most important determinant of daily maximum and daily mean temperatures, whereas intensity of development was the greatest determinant for daily minimum temperature (Zhou et al. 2014). We used major roads to define approximate boundaries of each subregion and maintained internal structure with the CBGs (Figure S1). Hourly data from HRLDAS models were aggregated to each local climate subregion. The result was hourly meteorological data at the local climate subregion scale for the summer months (June–September) from 2000 to 2015. Key weather variables required for the indoor thermal comfort model are dry-bulb temperature, relative humidity, dew point temperature, global solar radiation (direct and indirect), and wind speed.
Modeling Exposure to Indoor Heat
Building energy models.
Whole-building energy models are extensively use by engineers, architects, and researchers in the building science field to assess energy performance and thermal comfort in buildings (Hensen and Lamberts 2011). These models use physics-based equations to calculate thermal loads on different zones within a building in response to outdoor signals and occupant behavior, and they account for all modes of heat and mass transfer between indoors and outdoors (e.g., heat transfer through walls and windows, air exchange). EnergyPlus, a whole-building energy simulation program developed by the U.S. Department of Energy (https://energyplus.net/) is among the most used tools in the literature over the last decade (Baniassadi et al. 2018a; Ramakrishnan et al. 2017). Numerous studies have validated individual modules of EnergyPlus (Gu 2007; Loutzenhiser et al. 2009; Mateus et al. 2014; Shrestha and Maxwell 2011; Tabares-Velasco et al. 2012; Witte et al. 2001; Crawley et al 2001; Yu et al. 2014), and the entire model has been validated based on American National Standards Institute/American Society of Heating, Refrigerating and Air Conditioning Engineers (ANSI/ASHRAE) Standard 140 (Crawley et al. 2004; Henninger and Witte 2010). Thus, EnergyPlus was our preferred building energy model to estimate daily thermal conditions inside buildings across our study area.
Half-hourly measurements of indoor and outdoor environmental conditions (i.e., temperature, humidity, and carbon dioxide) from the homes of elderly Houstonians () during the 2016 and 2017 summer months were used to parameterize EnergyPlus for modeling indoor thermal conditions in Houston (Baniassadi et al. 2018c). We validated EnergyPlus for residential buildings by comparing EnergyPlus output with measured indoor parameters for four homes in Houston, Texas, and Phoenix, Arizona (Sailor et al. 2019). In our tests, we measured indoor temperature rise after an interruption to central AC (intentional or due to power outage) in these four homes. EnergyPlus models predicted indoor temperature with an RMSE of 0.4°C, 0.4°C, 0.5°C, and 0.6°C for the four buildings. In line with previous validation studies, this shows that EnergyPlus is capable of accurately predicting indoor air temperature.
Archetype generation.
Simulating daily indoor conditions for individual buildings was not feasible in this study because of the large study area. However, results of past studies suggest that the thermal performance of buildings is mostly determined by a limited number of variables such as size, building construction and design, and type of building (detached house vs. apartment building) (Alam et al. 2016; Baniassadi et al. 2018b; Chvatal and Corvacho 2009; McLeod et al. 2013; Nahlik et al. 2017; Ramakrishnan et al. 2017; Ren et al. 2014). This makes it possible to use archetype building models to represent buildings with relatively similar characteristics. Accordingly, we used the 2017 Harris County Appraisal District (HCAD) Real and Personal Property Database to generate archetype building models representing the study area’s residential building stock. The HCAD database included building variables such as prevalence of central AC, square footage, number of floors, exterior wall type, and qualitative descriptions of the construction, which were used to assess building envelop properties. Building envelop properties determine to what degree the indoor space is thermally isolated from the outdoors, and valuations for envelop properties were used to help us relate the thermal performance of archetype buildings to air-exchange rates, insulation, and solar transmittance (Table S1).
We created building archetypes based on the following categories for each of the following variables: we considered four classes of exterior wall type (brick/masonry, concrete block, brick/veneer, and wood frame), three classes of height (1-, 2-, and 3-story buildings), three classes of size (, , and ), and three classes of construction quality (low, medium, and high). Although the resulting set of 108 archetypes excludes some attributes (e.g., 4-story buildings), it represents 97% of residential buildings within our study domain.
Indoor Thermal Comfort Models
Once the archetypes and EnergyPlus model parameters (Table S2) were defined, hourly meteorological data from each local climate subregion was used with EnergyPlus (version 8.8.0) to model hourly indoor thermal comfort for all archetypes for the entire analysis period. Occupant behavior regarding window opening and AC usage was included in the indoor modeling work. However, we did not vary behavior across individuals and chose conservative behaviors that were plausible. For example, in buildings without AC, active occupants were assumed to open windows when the outdoor temperature is 2°C cooler than indoors. In buildings with central AC, we assumed occupants kept their homes at a constant, comfortable temperature. The result of the EnergyPlus indoor temperature model ( time-steps each summer) was a time series of hourly indoor temperature and relative humidity data for all archetypes during the entire analysis period. To estimate indoor thermal comfort at the CBG level, we calculated the percentage of residential buildings that correspond to each archetype in each CBG. We used these percentages to weight the hourly time series of indoor dry-bulb temperature and relative humidity for each CBG. Hourly values of indoor temperature and relative humidity were used to estimate the following daily exposure metrics: daily maximum indoor temperature, daily minimum indoor temperature, and daily maximum indoor discomfort index (DI). Because Houston has a humid subtropical climate, we chose to estimate the DI to account for the effect of humidity on adverse health outcomes. Although the term heat index is commonly used to communicate outdoor heat-related health risks, we chose the DI because it was specifically developed for indoor environments and was previously determined to be the best available metric for the indoor environment (Baniassadi et al. 2018a; Baniassadi and Sailor 2018). DI is the average of dry-bulb and wet-bulb temperature, and indoor DI was calculated using Equation 1.
| (1) |
where is the dry-bulb temperature, and is the wet-bulb temperature reported by (Stull 2011).
CBGs that reported 100% prevalence of central AC (), were assigned daily indoor temperature values of 23°C and daily indoor DI values of 20°C. Indoor heat metrics within these CBGs did not vary over time, and did not contribute to the estimation of associations between indoor heat and health. Ultimately, our indoor thermal comfort model outputted a weighted time series of estimated daily indoor heat exposure for the summer months during our study period (2000–2015) for all CBGs in our study area.
Statistical Analyses
Associations between indoor heat exposure and adverse health events were assessed using conditional logistic regression in single-exposure, time-stratified case-crossover models, matching on the CBG of subject (hospital patient or decedent) residence, year, month, and weekday of the adverse health event. We examined three metrics of indoor heat exposure for their effect on health outcomes: daily maximum indoor temperature, daily minimum indoor temperature, and daily maximum DI, described previously. Associations between indoor heat exposure and health were assessed for single lag days (lag 0 through lag 6) and for 3-d moving averages for lags 0–2. Separate models were fitted for each exposure metric and its respective lag day or moving average. Because specific diagnoses may have different relationships with indoor heat exposure compared with broader outcome definitions, we also fitted separate models for circulatory disease, respiratory disease, and any heat-related disease processes. In the main analyses, we examined mortality and emergency hospital admission data separately to evaluate the differences between these end points. All models controlled for maximum ambient temperature and maximum ambient dew point temperature (in degrees Celsius), modeled as cubic polynomials to account for possible nonlinear relationships with health outcomes. We chose to control for maximum values of temperature and dew point temperature because of their known impacts on health and because these metrics may represent outdoor exposures in Houston that pose a higher risk for acute heat stress on a given day (Heaton et al. 2015). Models included additional control for days on which federal holidays were observed and day of the warm season, modeled as a smooth function with monthly knots across the summer season (June–September). An interaction term between year and day of the warm season was also included to capture between-year differences.
In stratified analyses, we evaluated whether individual factors or area-level socio-demographics modified associations between health outcomes and 3-d moving averages of indoor heat exposure metrics. For the individual factors, models were stratified by the following strata: male or female sex; White or African American race, and age group (65–74 y, and ). Health records with missing information on sex, race, or age group were excluded from stratified analyses. Less than 0.5% of records within outcome groupings were excluded due to missing demographic information. For area-level socio-demographic factors, models were stratified a priori by median cut points of continuous CBG-level percentage of households living below the federal poverty line ( and ), and CBG-level percentage of the population living alone ( and ). We also stratified models by and CBG-level African American population, representing neighborhoods with a concentrated minority population. CBG-level socio-demographic data were obtained from the ACS 5-y (2010–2014) summary file. Effect measure modification analyses were restricted to health events among City of Houston residents and to the following health outcomes: circulatory deaths, circulatory hospitalizations, heat-related deaths, and heat-related hospitalizations. Evidence of significant effect modification was assessed by estimating the degree of heterogeneity between stratum-specific odds ratios (ORs) in pairwise comparisons (Kaufman and MacLehose 2013).
Primary epidemiological analyses explored health risks across CBGs that were considered part of the City of Houston in 2010 (1,522 CBGs), whereas secondary analyses explored health risks across all Harris County CBGs (2,038 CBGs). By design, the case-crossover approach controls for individual time-invariant confounders given that case and control days are compared for the same person. We also note that the above model assumes a) adverse health events for different individuals are independent, conditional on the variables in the model; b) all confounder effects are CBG-specific; and c) a linear association between indoor heat exposure and the log odds of an adverse health event. For all models, we estimated ORs and 95% confidence intervals (CIs) for changes in indoor exposure (e.g., maximum indoor temperature, minimum indoor temperature, and maximum indoor DI). The primary temperature increment evaluated was a 5°C increase in indoor heat exposure, representing an approximate interquartile range increase in indoor heat exposure from the 25th percentile to the 75th percentile (e.g., 23°C to 28°C).
Attributable deaths.
For the purpose of reporting actionable results to our stakeholders (i.e., the Houston Health Department), we estimated for each CBG the total number of excess heat-related deaths that could be plausibly attributable to exposure to high indoor heat. Heat-related deaths were the broadest health outcome grouping used in this study and included primary diagnoses of circulatory, respiratory, renal, and heat stroke/heat exhaustion diagnosis sets (ICD-9-CM/ICD-10 codes itemized in Table 1). For each day and each CBG, attributable number (AN) of heat-related deaths were estimated using Equation 2.
| (2) |
where is the total number of deaths in CBG on day that could be plausibly related to heat exposure (defined in Table 1 as heat-related), and represents the log odds from our conditional logistic regression models. For the attributable death calculation, is defined as the log odds between 3-d moving averages of indoor DI and heat-related deaths. DI represents the difference in estimated daily indoor DI for each CBG compared with a reference value of 20°C. The average number of attributable deaths in each CBG was given by the sum of the contributions from all the days of the series.
Table 1.
Descriptive statistics for health outcome data for Harris County and the City of Houston (June–September, 2000–2015).
| Health outcome groups | ICD-9-CM codes | ICD-10 codes | Harris Countya | City of Houstonb | ||||
|---|---|---|---|---|---|---|---|---|
| Total deaths () | Total EHAs () | Total deaths () | Total EHAs () | Mean daily deaths () | Mean daily EHAs () | |||
| Heat-related (HEAT) | 390–519; 580–593; 992 | I00–I99; J00–J99; N00–N20; T67.0–T67.9, X30 | 32,043 | 54,152 | 23,809 | 42,395 | 12 | 35 |
| Circulatory (CIRC) | 390–459 | I00–I99 | 24,513 | 34,484 | 18,330 | 27,277 | 9 | 22 |
| Respiratory (RESP) | 460–519 | J00–J99 | 5,806 | 14,832 | 4,159 | 11,320 | 2 | 9 |
Note: CBG, U.S. Census block group; CIRC, diseases of the circulatory system; EHA, emergency hospital admissions; HEAT, heat-related outcomes; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification diagnostic codes; ICD-10, International Classification of Diseases, 10th Revision diagnostic codes; RESP, diseases of the respiratory system.
Data are from all valid CBGs in the study area ().
Data are from all valid CBGs in the study area ().
Sensitivity analyses.
In sensitivity analyses, we considered models that controlled for daily 8-h maximum ozone concentrations [modeled using a linear term for the 3-d moving average (lag 0–2) concentration of ozone]. Results of models controlling for ozone were compared with primary models using maximum indoor DI and maximum indoor temperature with the same lag structure as ozone concentrations. We also performed a series of sensitivity analyses to assess the evidence for health effects related to maximum indoor DI compared with models that did not include indoor exposure data. Specifically, we used likelihood ratio tests (LRTs) to evaluate whether the inclusion of 3-d moving averages of maximum indoor DI made a significant contribution to model fit compared with a model that only included 3-d moving averages of ambient maximum temperature and ambient maximum dew point temperature. We also explored the sensitivity of our primary model to covariate control by fitting models with and without control for ambient meteorological factors. Finally, we fitted models with only one temperature indicator and compared estimated associations from models with indoor DI only to models with ambient maximum temperature only. Sensitivity analyses were restricted to heat-related deaths and heat-related hospitalizations among City of Houston residents.
In the present article, analyses that produce -values of are considered statistically significant. However statistical significance was only one factor we considered when interpreting results. Positive associations are indicative of an . All analyses were performed using R (version 3.4.0; R Development Core Team). We executed case-crossover models with strata based on individual cases using the clogit function of the survival package in R.
Results
Table 1 presents descriptive statistics of all health outcome groupings explored in this analysis. Health outcome groupings were created using primary ICD-9-CM and ICD-10 diagnostic codes. This study included a total of 32,043 deaths (June–September, 2000–2015) and 54,152 emergency hospital admissions (June–September, 2004–2013) for any heat-related illnesses among Harris County residents of age (Table 1). The relatively low number of mean daily counts reported in Table 1 reflect the specificity of our outcome groupings and our focus on the population.
During 2000–2015, summer season (June–September) daily maximum ambient temperatures modeled by HRLDAS ranged from 21.1°C to 47.8°C. Daily maximum indoor temperatures estimated by our indoor thermal comfort models ranged from 23°C to 48.5°C (Table 2). On average, CBGs near Houston’s urban center had higher indoor maximum temperatures (Figure S2) and greater variability in daily indoor maximum temperatures (Figure S3). CBGs with no daily variation in indoor heat () did not contribute to the estimation of associations between indoor heat and health.
Table 2.
Descriptive statistics for daily meteorological and indoor exposure metrics in Houston (June–September, 2000–2015).
| Daily ozone (ppb), meteorological and indoor exposure metrics (°C) | Min | p25 | Median | p75 | Max | |
|---|---|---|---|---|---|---|
| Max ambient temperature | 21.1 | 32.5 | 34.3 | 36.2 | 47.8 | |
| Min ambient temperature | 8.7 | 23.5 | 24.5 | 25.3 | 29.2 | |
| Max ambient dew point temperature | 7.60 | 23.4 | 24.4 | 25.3 | 37.2 | |
| Indoor max DI | 20.0 | 20.0 | 20.2 | 23.4 | 37.1 | |
| Indoor max temperature | 23.0 | 23.0 | 23.2 | 27.0 | 48.5 | |
| Indoor min temperature | 23.0 | 23.0 | 23.1 | 24.0 | 30.6 |
Note: Data are from all valid U.S. Census block groups in the study area (). DI, discomfort index; max, maximum; min, minimum; p25, 25th percentile; p75, 75th percentile; SD, standard deviation.
Daily maximum ambient temperature and daily maximum ambient dew point temperature were weakly correlated with daily indoor heat exposure metrics for the Harris County study area (Spearman’s of ; Table S3). To evaluate potential issues with collinearity in our models, we estimated day-to-day correlations between daily ambient maximum temperature and daily indoor heat metrics within each CBG. Figures S4–S6 illustrate the spatial variation and degree of correlation between indoor heat metrics and ambient maximum temperature within each CBG. These maps demonstrate that the strength of correlation depended on the choice of indoor heat metric, the prevalence of central AC within a CBG, and other characteristics of the built environment that modify the indoor environment (Figures S4–S6). Within CBGs, the highest correlations were observed between indoor maximum temperature and outdoor maximum temperature (Spearman’s of ; Figure S4). Spearman correlations were moderate to moderately high for indoor minimum temperature (Spearman’s of 0.43–0.74; Figure S5) and indoor maximum DI (Spearman’s of 0.55–0.76; Figure S6). Indoor heat exposure metrics were found to be weakly to moderately correlated with common indicators of socioeconomic status (Spearman’s of ; Table S4) and highly correlated with the percentage of households without central AC (Spearman’s of 0.92–1.0; Table S4). In addition, indoor temperature metrics were highly correlated with each other (Spearman’s of 0.93–1.00; Table S3).
Overall Analyses
Associations between HEAT and CIRC health outcomes and indoor heat exposure for our study area are reported in Table 3. We estimated statistically significant positive associations between HEAT and CIRC health outcomes and indoor heat, particularly when health outcomes were defined using mortality data compared with emergency hospital admission data [e.g., CIRC deaths, lag 0–2, OR per 5°C maximum indoor (95% CI: 1.10, 1.57)]. Associations were generally positive for earlier lag periods (lag 0 through lag 2) and weaker across later lag days (lags 3 through 6). Associations between indoor heat exposure and emergency hospitalizations were weaker and often not statistically significant compared with associations between indoor heat exposure and mortality. ORs also tended to be slightly attenuated for Harris County, compared with the City of Houston, although differences in magnitude were very small and did not affect overall interpretations (Table 3). Central AC prevalence was significantly lower (two-sample -test ) in City of Houston neighborhoods () compared with Harris County neighborhoods that are not in the City of Houston (). Given our indoor heat modeling approach, City of Houston residents, on average, would have been assigned a higher daily indoor heat exposure, which may partially account for the observed stronger associations. Across all exposure metrics, increases in indoor heat were associated with increases in the odds of death due to circulatory disease (Table 3). Associations between respiratory mortality and respiratory morbidity and all metrics of indoor thermal comfort were weak and consistent with the null (Table S5).
Table 3.
Odds ratios (95% confidence intervals) between select health outcomes and indoor heat exposure metrics (per 5°C) for City of Houston (COH) and Harris County residents (June–September, 2000–2015).
| Heat metric/lags | HEAT diagnoses (COH) | HEAT diagnoses (Harris County) | CIRC diagnoses (COH) | CIRC diagnoses (Harris County) | ||||
|---|---|---|---|---|---|---|---|---|
| Mortality | EHA | Mortality | EHA | Mortality | EHA | Mortality | EHA | |
| Indoor max DI (°C) | ||||||||
| Lag | ||||||||
| 0 | 1.18 (1.05, 1.34) | 1.05 (0.96,1.16) | 1.13 (1.01, 1.27) | 1.05 (0.96, 1.14) | 1.27 (1.10, 1.46) | 1.04 (0.92, 1.16) | 1.19 (1.04, 1.35) | 1.04 (0.93, 1.16) |
| 1 | 1.15 (1.02, 1.30) | 1.13 (1.03, 1.24) | 1.12 (1.00, 1.26) | 1.10 (1.00, 1.20) | 1.22 (1.06, 1.41) | 1.13 (1.01, 1.28) | 1.18 (1.04, 1.35) | 1.10 (0.98, 1.23) |
| 2 | 1.01 (0.89, 1.14) | 1.03 (0.94, 1.14) | 1.01 (0.90, 1.13) | 1.01 (0.92, 1.10) | 1.06 (0.92, 1.21) | 1.04 (0.92, 1.17) | 1.04 (0.92, 1.19) | 1.01 (0.91, 1.13) |
| 3 | 0.98 (0.86, 1.10) | 1.04 (0.94, 1.14) | 1.01 (0.90, 1.13) | 1.02 (0.94, 1.12) | 0.99 (0.86, 1.13) | 1.04 (0.92, 1.17) | 1.02 (0.90, 1.17) | 1.03 (0.92, 1.15) |
| 4 | 0.94 (0.83, 1.06) | 0.98 (0.89, 1.07) | 0.97 (0.86, 1.09) | 0.95 (0.87, 1.04) | 0.96 (0.84, 1.10) | 0.98 (0.88, 1.10) | 0.97 (0.85, 1.11) | 0.94 (0.84, 1.05) |
| 5 | 0.95 (0.84, 1.08) | 0.96 (0.88, 1.05) | 0.96 (0.85, 1.08) | 0.92 (0.85, 1.04) | 0.96 (0.83, 1.10) | 0.98 (0.87, 1.10) | 0.98 (0.86, 1.12) | 0.93 (0.84, 1.04) |
| 6 | 0.90 (0.80, 1.02) | 0.95 (0.87, 1.04) | 0.90 (0.81, 1.02) | 0.94 (0.86, 1.02) | 0.90 (0.79, 1.04) | 0.97 (0.86, 1.08) | 0.91 (0.80, 1.03) | 0.93 (0.84, 1.04) |
| 0–2 | 1.20 (1.02, 1.40) | 1.12 (0.99, 1.26) | 1.14 (0.99, 1.32) | 1.08 (0.97, 1.21) | 1.31 (1.10, 1.57) | 1.12 (0.96, 1.30) | 1.22 (1.04, 1.44) | 1.08 (0.94, 1.24) |
| Indoor max temp (°C) | ||||||||
| Lag | ||||||||
| 0 | 1.11 (1.02, 1.20) | 1.03 (0.97, 1.09) | 1.08 (1.00, 1.17) | 1.03 (0.97, 1.09) | 1.14 (1.04, 1.25) | 1.03 (0.95, 1.11) | 1.10 (1.01, 1.20) | 1.03 (0.96, 1.11) |
| 1 | 1.08 (1.00, 1.17) | 1.08 (1.02, 1.15) | 1.07 (0.99, 1.15) | 1.07 (1.01, 1.14) | 1.12 (1.02, 1.23) | 1.10 (1.02, 1.18) | 1.10 (1.01, 1.20) | 1.08 (1.01, 1.16) |
| 2 | 0.98 (0.91, 1.06) | 1.03 (0.97, 1.10) | 0.98 (0.91, 1.06) | 1.02 (0.96, 1.08) | 1.01 (0.92, 1.11) | 1.05 (0.97, 1.13) | 1.00 (0.92, 1.09) | 1.03 (0.96, 1.11) |
| 3 | 0.97 (0.89, 1.05) | 1.03 (0.97, 1.10) | 0.99 (0.92, 1.07) | 1.03 (0.97, 1.09) | 0.98 (0.89, 1.07) | 1.05 (0.97, 1.13) | 1.00 (0.92, 1.09) | 1.04 (0.97, 1.12) |
| 4 | 0.94 (0.87, 1.02) | 1.00 (0.94, 1.07) | 0.95 (0.88, 1.03) | 0.99 (0.93, 1.05) | 0.96 (0.88, 1.05) | 1.01 (0.94, 1.09) | 0.96 (0.88, 1.05) | 0.99 (0.92, 1.06) |
| 5 | 0.95 (0.88, 1.03) | 0.99 (0.93, 1.05) | 0.95 (0.88, 1.03) | 0.97 (0.92, 1.02) | 0.97 (0.88, 1.06) | 0.99 (0.92, 1.07) | 0.98 (0.90, 1.06) | 0.97 (0.90, 1.04) |
| 6 | 0.93 (0.86, 1.01) | 0.99 (0.94, 1.05) | 0.93 (0.86, 1.00) | 0.98 (0.92, 1.03) | 0.93 (0.85, 1.02) | 0.99 (0.92, 1.07) | 0.93 (0.85, 1.01) | 0.97 (0.90, 1.04) |
| 0–2 | 1.10 (0.99, 1.22) | 1.08 (0.99, 1.17) | 1.07 (0.98, 1.18) | 1.07 (0.99, 1.15) | 1.16 (1.03, 1.30) | 1.09 (0.99, 1.21) | 1.11 (1.00, 1.24) | 1.08 (0.98, 1.19) |
| Indoor min temp (°C) | ||||||||
| Lag | ||||||||
| 0 | 1.11 (0.90, 1.36) | 1.06 (0.91, 1.23) | 1.03 (0.85, 1.24) | 1.03 (0.90, 1.18) | 1.26 (1.00, 1.58) | 0.97 (0.80, 1.16) | 1.16 (0.93, 1.44) | 0.95 (0.80, 1.13) |
| 1 | 1.23 (1.01, 1.51) | 1.04 (0.90, 1.20) | 1.18 (0.97, 1.42) | 0.99 (0.86, 1.14) | 1.30 (1.03, 1.63) | 1.02 (0.85, 1.22) | 1.22 (0.98, 1.51) | 0.98 (0.83, 1.17) |
| 2 | 1.08 (0.88, 1.33) | 1.07 (0.92, 1.24) | 1.08 (0.89, 1.31) | 1.03 (0.90, 1.18) | 1.13 (0.90, 1.43) | 1.05 (0.88, 1.26) | 1.13 (0.91, 1.40) | 1.01 (0.85, 1.20) |
| 3 | 1.02 (0.83, 1.25) | 0.99 (0.85, 1.14) | 1.04 (0.86, 1.25) | 0.95 (0.83, 1.09) | 1.05 (0.83, 1.32) | 0.98 (0.82, 1.18) | 1.07 (0.86, 1.33) | 0.94 (0.79, 1.11) |
| 4 | 0.92 (0.75, 1.12) | 0.99 (0.86, 1.14) | 0.96 (0.80, 1.16) | 0.93 (0.81, 1.06) | 0.93 (0.74, 1.17) | 0.98 (0.82, 1.17) | 1.00 (0.81, 1.24) | 0.91 (0.77, 1.08) |
| 5 | 0.93 (0.76, 1.14) | 0.98 (0.85, 1.13) | 0.95 (0.79, 1.15) | 0.95 (0.83, 1.08) | 0.90 (0.72, 1.13) | 1.02 (0.85, 1.21) | 0.93 (0.75, 1.15) | 0.99 (0.84, 1.17) |
| 6 | 1.10 (0.90, 1.35) | 1.02 (0.88, 1.17) | 1.10 (0.91, 1.33) | 1.02 (0.89, 1.17) | 1.03 (0.82, 1.29) | 1.07 (0.89, 1.28) | 1.02 (0.83, 1.27) | 1.07 (0.91, 1.27) |
| 0–2 | 1.22 (0.95, 1.57) | 1.09 (0.90, 1.31) | 1.15 (0.90, 1.45) | 1.02 (0.86, 1.22) | 1.37 (1.03, 1.82) | 1.02 (0.81, 1.29) | 1.26 (0.97, 1.66) | 0.97 (0.78, 1.21) |
Note: Mortality data were available 2000–2015; EHA data were available 2004–2013. Odds Ratios were derived from single-exposure, time-stratified case-crossover models (conditional logistic regression), that matched on census block group of subject residence, year, month, and weekday of the adverse health event. Models controlled for federal holidays, day of the warm season, maximum ambient temperature and maximum ambient dew point temperature (in degrees Celsius, modeled as cubic polynomials). CIRC, diseases of the circulatory system; COH, City of Houston; DI, discomfort index; EHA, emergency hospital admission; HEAT, heat-related illnesses; max, maximum; min, minimum; temp, temperature.
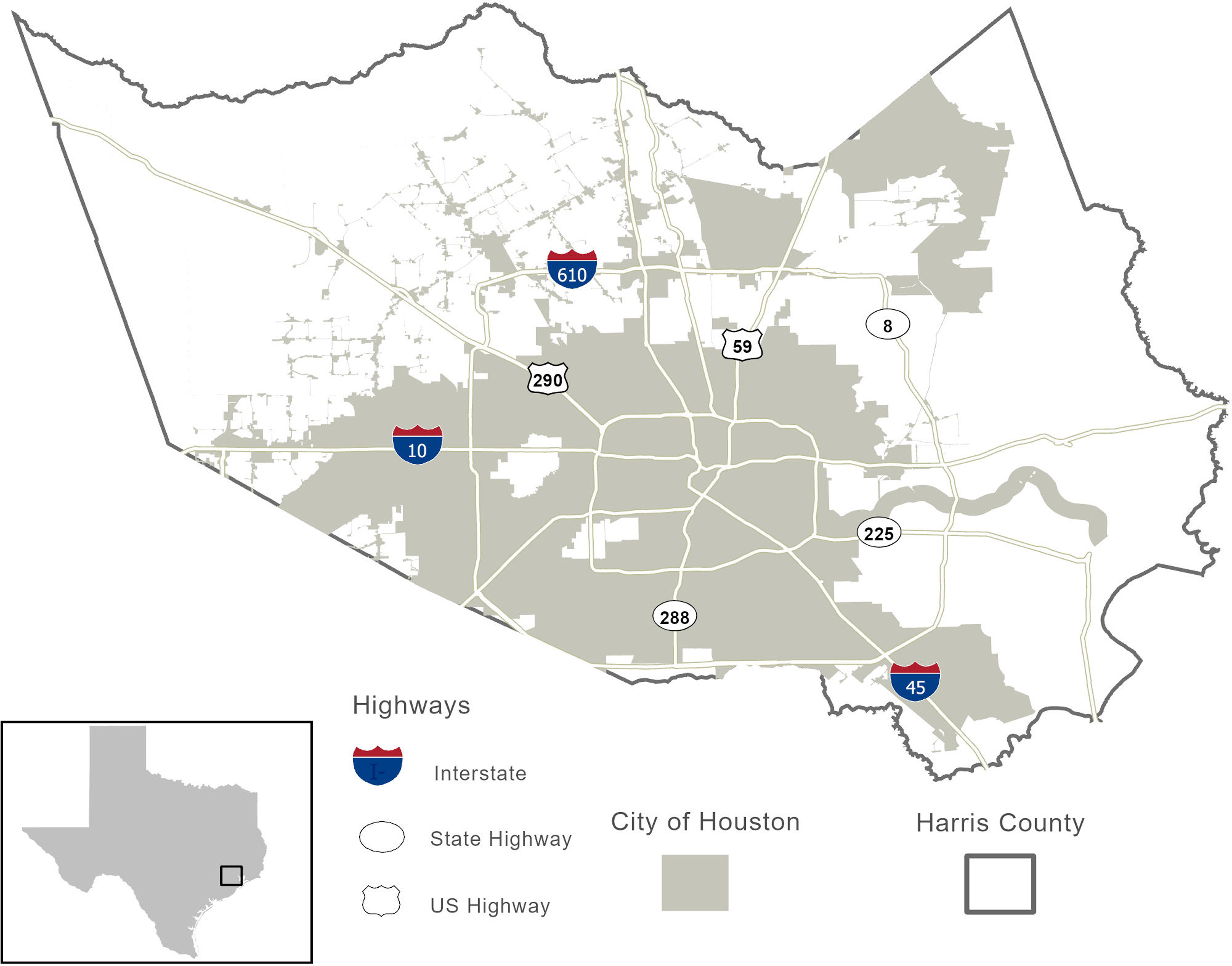
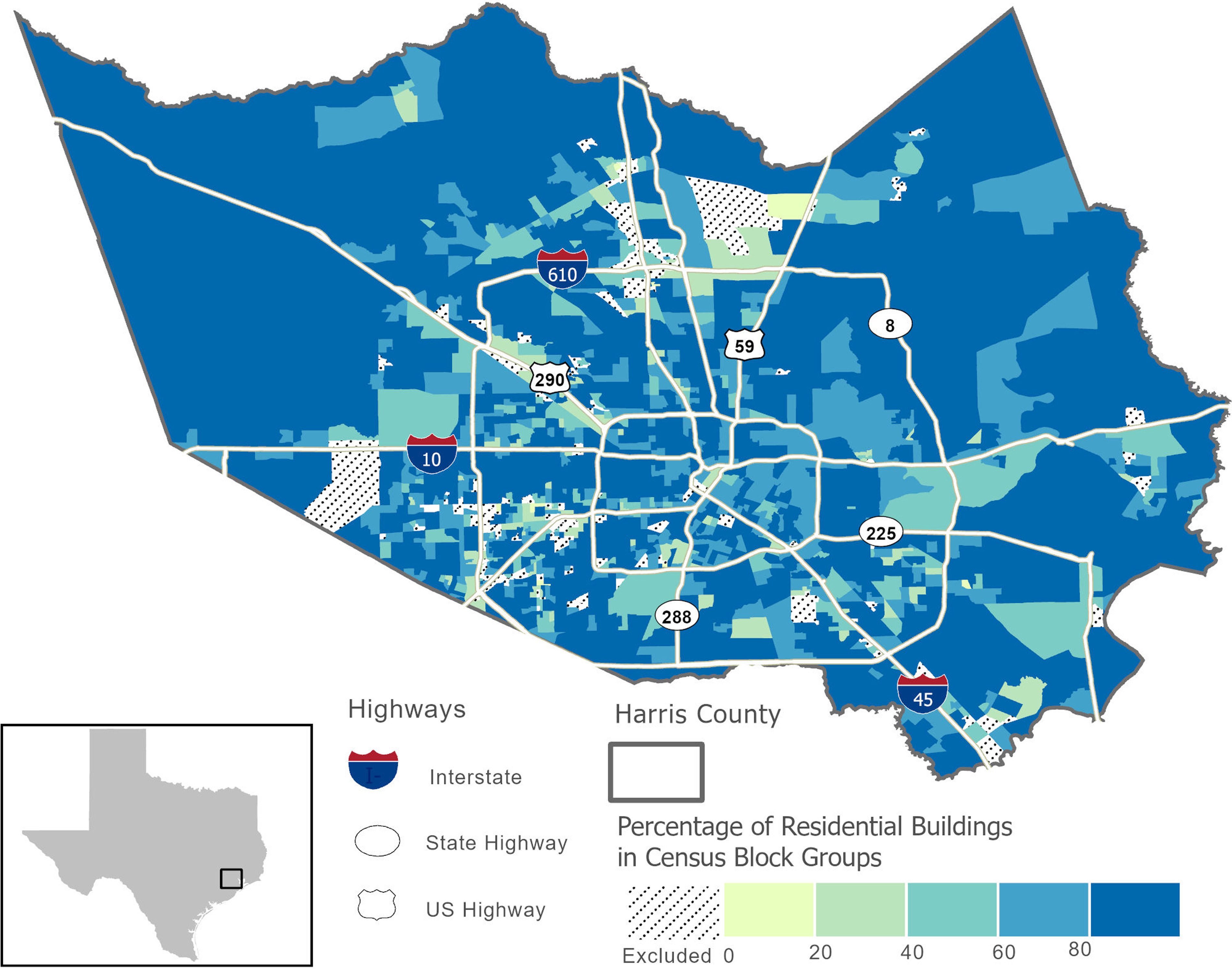
Effect Measure Modification Analyses
Table 4 and Figures 4 and 5 present ORs between 3-d moving averages of maximum indoor DI and health outcomes from effect measure modification analyses. The results presented in Table 4 and Figures 4 and 5 are largely representative of findings from effect measure modification analyses that used dry-bulb temperature metrics (maximum indoor temperature and minimum indoor temperature) for indoor heat exposure (Figures S7 and S8, Tables S8 and S9). We did not observe effect modification of indoor heat–mortality associations by individual or area-level factors. However, with regard to emergency hospital admissions, stratified analyses suggested that African American populations were more likely to be admitted to the hospital after indoor heat exposure compared with White populations. For example, when examining effect modification by patient race, statistically significant differences in ORs between White and African American strata were observed at the 0.05 level for circulatory and heat-related emergency hospital admissions when indoor heat exposure was defined using 3-d moving averages of maximum DI. This pattern was not observed when considering mortality outcomes (Figure 4, Table 4). Likewise, at the neighborhood level, we observed significantly stronger associations between 3-d moving averages of indoor heat exposure and health outcomes in neighborhoods that were predominantly () African American compared with neighborhoods with fewer African Americans () (Figure 5; Table 4; Figures S7 and S8; Tables S8 and S9). We did not find statistical evidence for effect modification by subject sex (male vs. female), advanced age (), percentage living below the federal poverty level, or the percentage of the elderly population living alone (Figures 4 and 5; Table 4).
Table 4.
Odds ratios (95% confidence intervals) between 3-d moving averages of maximum DI and health outcomes stratified by individual and neighborhood factors for City of Houston residents (June–September, 2000–2015).
| Strata | CIRC deaths | -Valuea | HEAT deaths | -Valuea | CIRC EHA | -Valuea | HEAT EHA | -Valuea |
|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||
| Female | 1.16 (0.92, 1.47) | 1.17 (0.95, 1.44) | 1.08 (0.89, 1.31) | 1.14 (0.97, 1.33) | ||||
| Male | 1.52 (1.17, 1.99) | 0.13 | 1.23 (0.98, 1.55) | 0.72 | 1.17 (0.92, 1.50) | 0.60 | 1.09 (0.90, 1.32) | 0.73 |
| Age group (y) | ||||||||
| 65–74 | 1.55 (1.11, 2.17) | 1.41 (1.05, 1.90) | 1.14 (0.90, 1.44) | 1.11 (0.92, 1.34) | ||||
| 1.25 (1.01, 1.53) | 0.28 | 1.14 (0.95, 1.36) | 0.22 | 1.11 (0.91, 1.36) | 0.88 | 1.13 (0.96, 1.32) | 0.91 | |
| Race | ||||||||
| White | 1.39 (1.07, 1.81) | 1.19 (0.94, 1.49) | 0.89 (0.65, 1.20) | 0.90 (0.71, 1.15) | ||||
| African American | 1.41 (1.07, 1.86) | 0.96 | 1.36 (1.06, 1.73) | 0.43 | 1.34 (1.05, 1.71) | 0.04 | 1.24 (1.02, 1.51) | 0.04 |
| CBG percentage African Americanb | ||||||||
| 1.39 (1.11, 1.73) | 1.16 (0.96, 1.41) | 1.01 (0.84, 1.22) | 1.01 (0.87, 1.17) | |||||
| 1.49 (1.05, 2.12) | 0.72 | 1.59 (1.16, 2.17) | 0.1 | 1.41 (1.04, 1.93) | 0.07 | 1.43 (1.11, 1.84) | 0.02 | |
| CBG percentage below povertyc | ||||||||
| 1.46 (0.91, 2.33) | 1.28 (0.85, 1.93) | 1.17 (0.78, 1.76) | 1.07 (0.78, 1.49) | |||||
| 1.43 (1.16, 1.76) | 0.94 | 1.29 (1.07, 1.55) | 0.9 | 1.12 (0.93, 1.34) | 0.83 | 1.12 (0.97, 1.30) | 0.82 | |
| CBG percentage living aloned | ||||||||
| 1.22 (0.93, 1.59) | 1.17 (0.93, 1.48) | 1.14 (0.92, 1.43) | 1.15 (0.96, 1.38) | |||||
| 1.41 (1.12, 1.78) | 0.42 | 1.23 (1.00, 1.51) | 0.77 | 1.09 (0.89, 1.35) | 0.78 | 1.10 (0.93, 1.30) | 0.72 | |
Note: Mortality data were available 2000–2015; EHA data were available 2004–2013. Odds Ratios were derived from single-exposure, time-stratified case-crossover models (conditional logistic regression), that matched on U.S. CBG of subject residence, year, month, and weekday of the adverse health event. Models controlled for federal holidays, day of the warm season, maximum ambient temperature and maximum ambient dew point temperature (in degrees Celsius, modeled as cubic polynomials). CBG, U.S. Census block group; CIRC, diseases of the circulatory system; EHA, emergency hospital admission; HEAT, heat-related illnesses; OR, odds ratio.
Statistical evidence for effect modification was assessed by estimating the degree of heterogeneity between stratum-specific ORs in pairwise comparisons (Kaufman and MacLehose 2013). Referent groups for each stratum were female sex, 65- to 74-y-old age group, White race, African American, poverty, live alone.
CBG-level percentage of households living below the federal poverty line.
CBG percentage of the population living alone.
CBG percentage of the population that identifies as African American.
Figure 4.
Estimated ORs and 95% CIs per 5°C increase between 3-d moving averages of maximum indoor DI and health outcomes stratified by individual factors for City of Houston residents (June–September, 2000–2015). ORs were derived from single-exposure, time-stratified case-crossover models (conditional logistic regression), that matched on U.S. Census block group of subject residence, year, month, and weekday of the adverse health event. Models controlled for maximum ambient temperature and maximum ambient dew point temperature (°C) with cubic polynomials, federal holidays, day of the warm season, modeled as a smooth function with monthly knots across the summer season (June–September). An interaction term between year and day of the warm season was also included to capture between-year differences. Mortality data were available 2000–2015; EHA data were available 2004–2013. See Table 4 for corresponding numeric data. Note: CI, confidence interval; CIRC, circulatory diagnoses; DI, discomfort index; EHA, emergency hospital admissions; HEAT, heat-related diagnoses; OR, odds ratio.
Figure 5.
Estimated ORs and 95% CIs per 5°C increase between 3-d moving averages of maximum indoor DI and health outcomes stratified by U.S. Census block group (CBG) socio-demographic factors for City of Houston residents (June–September, 2000–2015). ORs were derived from single-exposure, time-stratified case-crossover models (conditional logistic regression) that matched on CBG of subject residence, year, month, and weekday of the adverse health event. Models controlled for maximum ambient temperature and maximum ambient dew point temperature (°C) with cubic polynomials, federal holidays, day of the warm season, modeled as a smooth function with monthly knots across the summer season (June–September). An interaction term between year and day of the warm season was also included to capture between-year differences. Mortality data were available 2000–2015; EHA data were available 2004–2013. See Table 4 for corresponding numeric data. Note: CI, confidence interval; CIRC, circulatory diagnoses; DI, discomfort index; EHA, emergency hospital admissions; HEAT, heat-related diagnoses; OR, odds ratio.
Attributable Deaths and Risk Communication
Although reporting ORs is ideal for summarizing the association between indoor heat and health, such relative measures of association offer limited information on the actual health burden of indoor heat and are not very useful to HOME-AIR stakeholders in the City of Houston. Therefore, we report an estimate of the excess number of heat-related deaths (outcome defined in Table 1) attributable to indoor heat for each CBG in our study area. By providing this information, City of Houston public health practitioners can better understand which populations are at greater risk of heat-related health effects and which neighborhoods experience the greatest health burden—information that is critical for the planning and evaluation of public health interventions. Figure 6 shows the average number of excess heat-related deaths attributable to exposure to high indoor heat for each CBG in Harris County. This risk map demonstrates that populations living in neighborhoods that are predominately nonwhite, of lower socioeconomic status, and with less prevalence of central AC have the greatest risk of dying due to indoor heat exposure compared with other populations. Based on Figure 6, neighborhoods in East Houston and North Central Houston appear most vulnerable to indoor heat. Between 2000 and 2015, we estimate that excess deaths (95% CI: 358, 6,116) among the population were attributable to exposure to indoor heat during the summer months. This translates to (95% CI: 22, 382) excess deaths in the population each summer due to high indoor heat.
Figure 6.
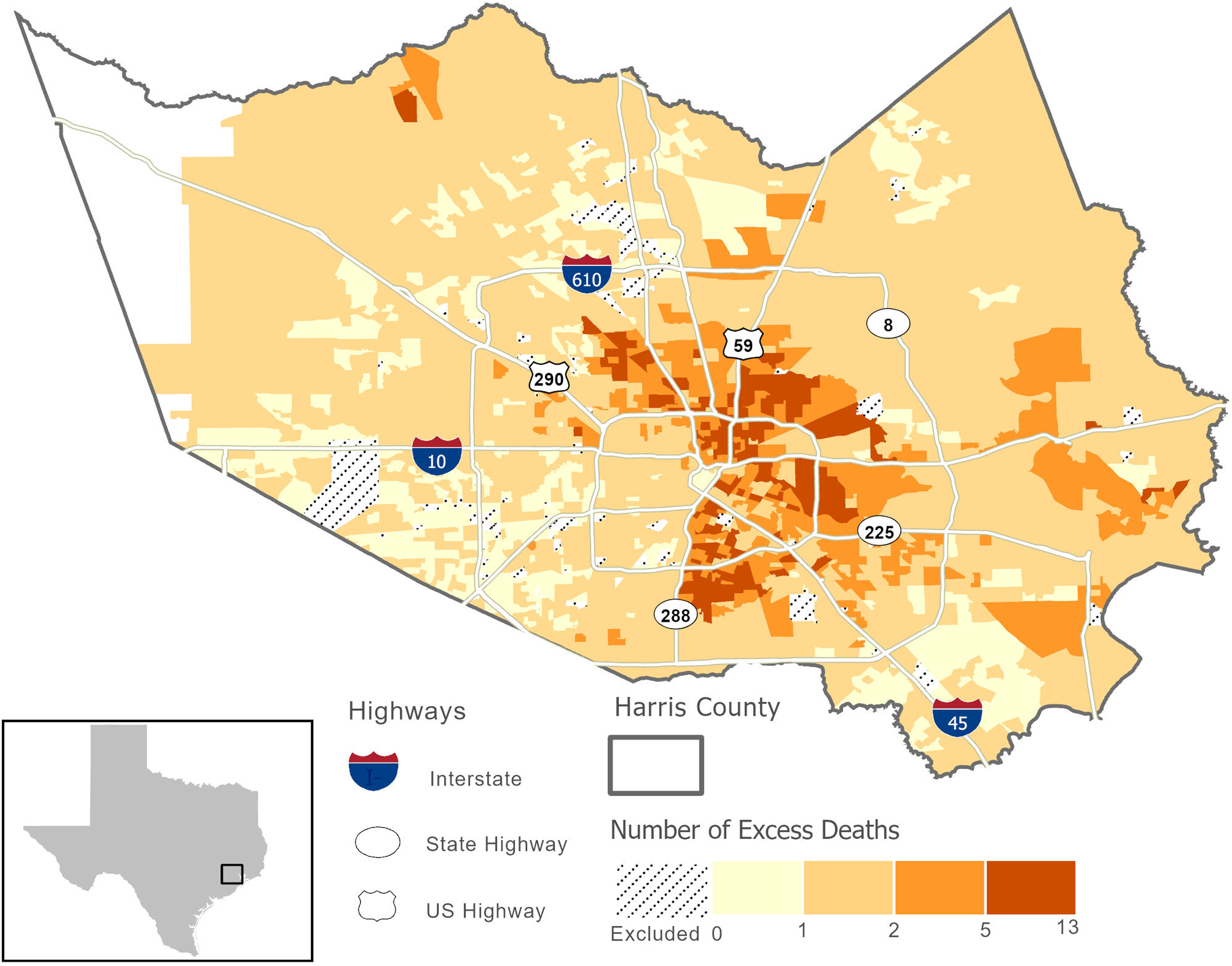
Estimated number of heat-related deaths attributable to exposure to high indoor heat during the summer months (June–September) for each U.S. Census block group (CBG) in Harris County between 2000 and 2015. To map the estimated number of deaths across our study area, we used effect estimates between heat and mortality for City of Houston residents. Hatched areas represent CBGs excluded from analyses because all buildings within these CBGs were identified as nonresidential or because residential buildings could not be categorized into building archetypes used in our indoor modeling.
Sensitivity Analyses
We performed a series of sensitivity analyses to assess whether indoor heat effect estimates would change when controlling for daily ozone concentrations and, importantly, to explore whether the inclusion of indoor heat exposure made a significant impact on model fit. Indoor heat exposure effect estimates were not sensitive to the addition of daily 8-h maximum ozone concentrations to primary models (Table S6), suggesting that ambient ozone (or unmeasured confounders) were not contributing significantly to the observed effect estimates between indoor heat and health. Based on these findings, we did not include control for ambient ozone in primary epidemiological models.
We used LRTs to compare primary models with models that did not include a term for indoor heat exposure. Based on LRTs and -values, when examining heat-related deaths, primary models performed marginally better than models without indoor heat exposure terms (). LRTs and -values from sensitivity analyses are reported in Table S7.
The primary model used throughout this analysis included an indicator of indoor heat as the exposure metric and controlled for ambient maximum temperature, ambient dew point temperature, and time-varying confounders. We controlled for outdoor heat exposure to compare hypothetical individuals with the same outdoor temperature to those with higher indoor heat exposure. However these variables may be highly correlated. To assess any issues due to possible collinearity, we fitted models that removed ambient meteorological control and compared estimated associations and confidence intervals. For mortality outcomes, mean ORs from primary models were larger [e.g., OR per 1°C maximum indoor (95% CI: 1.00 1.07) compared with models that removed ambient temperature control [e.g., OR per 1°C maximum indoor (95% CI: 0.99, 1.05), and standard error estimates were very similar across model configurations (Table S10). When estimating associations between indoor heat and hospital admissions, mean ORs and 95% CIs were the same regardless of meteorological control (Table S10). These findings suggest that potential collinearity between explanatory variables did not overly influence mean effect estimates nor their associated uncertainties.
Given that our study population likely spends the majority of their time indoors at home, we compared estimated associations from models with an indoor heat metric only (no ambient temperature control) to models with ambient maximum temperature as the exposure of interest. Table S11 reports ORs and 95% CIs from these analyses. For heat-related mortality and heat-related hospital admission outcomes, models that included indoor DI only estimated larger associations [e.g., HEAT deaths, OR per 1°C maximum indoor (95% CI: 0.994, 1.051)] than models that fit ambient maximum temperature as the exposure of interest [e.g., HEAT deaths, OR per 1°C maximum (95% CI: 0.987, 1.004)]. These findings suggest that indoor heat metrics may be more relevant for the population in Houston compared with ambient heat metrics.
Discussion
In the present study, we used a novel methodology to estimate daily indoor heat exposure and a TS-CCO approach to evaluate the short-term effects of indoor heat exposure on health outcomes among older adults in the Houston metropolitan area. Few studies have estimated the health impacts of indoor heat among vulnerable populations, and, to our knowledge, this is the first study to use building energy models to estimate daily indoor heat exposure for use in an epidemiological model. The modeling approach presented in this research can help inform future studies, and the findings add to the small, yet growing body of literature on climate-related health effects among sensitive subpopulations.
Overall Analyses
In overall analyses, we estimated statistically significant associations between indoor heat and adverse health outcomes, especially for circulatory and any heat-related deaths among City of Houston residents of age. Despite some evidence for increases in respiratory distress due to ambient heat exposure (Anderson et al. 2013; Gronlund et al. 2014; Lin et al. 2009; McCormack et al. 2016; Winquist et al. 2016), we did not find evidence of an association between respiratory diseases and short-term exposure to indoor heat in the present study. This may be due to the small number of cases in the respiratory outcome group (Table 1) and to limited power to detect associations. It is also possible that ambient exposure is more relevant for respiratory disease given that ambient heat exposure may also involve exposure to outdoor pollutants, many of which are well-known respiratory irritants.
For all exposure metrics, associations were consistently weaker for emergency hospital admissions compared with mortality outcomes. These findings differ from a recent Houston-based study on the 2011 heat wave that reported stronger associations between heat waves and emergency department visits compared with mortality outcomes (Zhang et al. 2015). It is possible that many of the heat-related deaths occurred at home and would, therefore, have a stronger relationship with indoor conditions. Unfortunately, we do not have data on where deaths occurred or if a patient admitted to the hospital was at home or elsewhere prior to the health event. In addition, earlier lag periods were the most important exposure periods from a health standpoint. These findings align with the ambient heat–health literature that often report stronger associations between heat and mortality/morbidity for earlier lag periods (Anderson and Bell 2009; Guo et al. 2017; Ye et al. 2012). In the present study, ORs between indoor heat and mortality were largest on lag day 0 and decreased over subsequent lag days. For emergency hospital admissions, ORs usually peaked around lag day 1 and decreased over subsequent lag days. Although estimates from single day lags likely correlate with one another, and differences may be due to chance, there also appears to be a robust cumulative effect of indoor heat on mortality as evidenced by the increasing strength of association for 3-d moving average periods. These findings suggest that the elderly are at risk for increased mortality when temperatures are high, on average, for several days. For the elderly population in Houston, Heaton et al. (2019) reported different lagged effects of heat depending on age: For example, persons closer to 65 years of age did not appear overly vulnerable to heat across lag days 0 through 3. However, for persons near 78 years of age, high heat was associated with increases in mortality on lag day 0, and persons of age were impacted by heat at all lag periods examined (lags 0 through 3) (Heaton et al. 2019). Owing to data limitations, we could not stratify our models by age; however, the use of a 3-d moving average (lag day 0–2) metric allowed us to capture exposure across these earlier lag periods and the cumulative effect of prolonged exposure to high heat across the population.
When comparing our findings to recent U.S.-based studies, and a Houston study in particular, patterns of association between indoor heat and mortality (e.g., positive associations at early lag periods) largely align with associations reported in the ambient heat–mortality literature (Anderson and Bell 2009; Basu 2009; Gasparrini and Armstrong 2011). However differences in the magnitude of the reported associations are noted. For example, Anderson and Bell (2009) reported a 3.0% (95% CI: 2.4%, 3.6%) increase in mortality risk across 107 U.S. communities comparing the 99th and 90th percentile temperatures (Anderson and Bell 2009); Basu and Malig (2011) reported an increased risk of 4.3% (95% CI: 3.4%, 5.2%) per 5.6°C increase in ambient apparent temperature in California (Basu and Malig 2011). Notably, Zhang et al. (2015) reported an excess risk of mortality of only 0.1% (95% CI: , 7.8%) due to the 2011 heat wave in the Houston population. Using stricter heat wave definitions, excess risk of mortality increased to 6.3% (, 54.8%) (Zhang et al. 2015) In contrast, excess risks of mortality per 5°C increase in indoor heat exposure reported here for City of Houston residents range from 10% (95% CI: , 22%) to 22% (95% CI: , 57%) depending on the indoor heat metric [e.g., an increase in heat-related mortality risk of 20% (95% CI: 2%, 40%) per 5°C indoor DI]. Differences in magnitude between this study and previous ambient heat–health studies can be attributed to many factors, including modeling approach, exposure metrics, scaling factors, and time-period, as well as the generalizability of the findings to other age groups and locations. Although there are important differences between this study and the study by Zhang et al. (2015), we estimated associations between heat and mortality for a similar population. Thus, differences in magnitude of excess risk of mortality may reflect the relative importance of capturing indoor exposure among older adults in Houston who likely spend the majority of their time indoors and at home.
Indoor Heat Metrics
When comparing findings across three different indoor heat exposure metrics (i.e., indoor maximum DI, maximum indoor temperature, and minimum indoor temperature), we observed several important similarities across these metrics. Namely, patterns of association tended to be similar for indoor DI and indoor maximum temperature and largely tracked with overall findings (i.e., weak associations with emergency hospital admissions, stronger associations in early lag periods) (Table 3). In the ambient heat–health literature, it is considered best practice to account for the impact of humidity on health either by including it in the main exposure metric (e.g., apparent temperature) or by controlling for it in the model. In the present study, we used indoor DI to account for the influence of indoor humidity on the association between indoor heat and health. Although the DI was determined to be the best available metric for the indoor environment for this type of analysis (Baniassadi et al. 2018a; Baniassadi and Sailor 2018), it is uncommonly used by the general public to assess personal heat exposure. However, smart home devices and/or simple phone or tablet apps can translate dry-bulb temperature and relative humidity (commonly reported on thermostats or smart home devices) into more meaningful exposure metrics such as the DI in real time. If access to a thermostat/outdoor thermometer and smart phone is limited, it would be challenging for the average person to determine their indoor heat exposure, both broadly speaking and in the context of the DI.
With the exception of circulatory deaths, ORs between minimum indoor temperature and health outcomes were weak and consistent with the null. It is worth noting that one possible explanation for attenuated estimates and wide CIs could be due to less variability in indoor minimum temperature across time and space compared with the other indoor heat metrics (standard deviation of 1.1 compared with 3.8 for maximum indoor temperature; Table 2). For all three exposure metrics, an increase in indoor heat was associated with an increase in the odds of death due to circulatory disease (Table 3) and suggest that elevated indoor temperatures/indoor heat exposure may play a role in disease processes that lead specifically to circulatory-related deaths. Disease processes in our circulatory-outcome group included high blood pressure, ischemic heart disease, myocardial infarction, heart failure, and stroke. When exposed to extreme heat, older adults have an altered response (compared with younger adults) during passive heating that manifests as attenuated blood flow and attenuated cardiac output, resulting in excess central cardiovascular strain, impaired thermoregulation, and attenuated evaporative heat loss (Kenney et al. 2014). These heat-induced stressors on the cardiorespiratory system could initiate a cascade that leads to circulatory mortality or morbidity, particularly for individuals with underlying circulatory disease. In our data, circulatory diseases made up the majority of total hospitalizations (64%) and deaths (77%) within the heat-related outcome grouping (Table 1) and may partially explain why the magnitudes and patterns of association were similar for circulatory and heat-related mortality/morbidity when comparing ORs for a given indoor heat metric, lag period, and study area. In the present analysis, only primary causes of mortality/morbidity were considered. Given that deaths due to circulatory diseases were statistically significant with indoor heat exposure metrics, the use of only primary causes of death could underestimate associations between indoor heat and mortality.
Relationship between Indoor Heat, Ozone, and Indoor Pollutants/Allergens
In the present study we did not consider tropospheric ozone as a confounder of the ambient temperature–health relationship, rather we considered it to be along the causal pathway (a causal intermediate) and influenced by ambient temperature (see directed acyclic graph; Figure S9A). Similar assessments on the role of tropospheric ozone in studies of temperature and health have been reported (Buckley et al. 2014; Reid et al. 2012). However, when evaluating the relationship between indoor heat and health, we did consider the possibility that ambient ozone may be penetrating indoors, especially if occupants are opening their windows to cool their homes. This may be especially true in CBGs with low prevalence of central AC. Under this scenario, indoor ozone levels could be elevated and coincide with high indoor heat, and this co-occurrence would likely be differential across CBGs and socioeconomic subgroups and may have differentially impacted health for population subgroups. Although ozone was not considered a confounder of the relationship between indoor temperature and health in the present study, controlling for ozone in health models may control for confounding by other unmeasured factors (see directed acyclic graph; Figure S9B). In sensitivity analyses, we observed nominal changes in effect estimates (Table S6) when controlling for ambient ozone, indicating that ozone (or unmeasured confounders) was not contributing significantly to estimated associations between indoor heat and health.
Related to the discussion above, whereas it is likely that other indoor environmental factors (e.g., particulate matter, household allergens, indoor gaseous pollutants) contribute to adverse health outcomes among our study population, we did not consider them to be confounders of the indoor heat–health relationship because they would be unlikely to influence indoor temperatures, either directly or indirectly. However, ambient temperature, and, by extension, indoor temperature, may affect particulate matter levels, mold growth, and aerosol chemistry of the indoor environment. These unmeasured indoor environmental factors could be considered on the causal pathway (causal intermediates) between indoor heat and health. Therefore, we assume that the associations we estimated between indoor heat and health reflect the total effect of indoor heat on health, including that which may be mediated by indoor environmental factors. Furthermore, one of the advantages of using the TS-CCO design is that it inherently controls for an individual’s time-invariant confounders given that case and control days are compared for the same person. For example, we could assume that unmeasured time-invariant confounders (e.g., proximity to roadway, occupation, cooking habits) would be relatively stable over time, and thus any potential confounding effects would be controlled for within the TS-CCO model.
Effect Measure Modification Analyses
In stratified analyses, associations between indoor heat and emergency hospital admissions were significantly stronger among African Americans compared with Whites and among residents of CBGs with higher proportions of African Americans. However, these differences should be interpreted with care because they may be at least partly due to differences in hospital utilization rates between White and African American residents. Although it is outside the scope of this study to investigate mechanisms underlying heat vulnerability by race/ethnicity, previous studies have reported evidence of heat-related health disparities between White and African American populations that were hypothesized to be due in part to AC access (O’Neill et al. 2003, 2005). Gronlund observed that, in the United States, race intersects with additional indicators of vulnerability and argued that disparities in heat-associated mortality and morbidity may be attributed to additional factors such as low socioeconomic status, lack of transportation, preexisting health conditions, and living in areas of intense urban development (Gronlund 2014). Houston is considered one of the most diverse cities in the country; a better understanding of how race and ethnicity intersect with heat-related health outcomes is critical to public health intervention efforts and should be an active area of research, particularly in southern U.S. cities. We were able to compare estimated health effects between White and African American residents, but there were too few cases in other race/ethnicity categories. We did not find statistical evidence for effect modification by sex (male vs. female), advanced age ( years old), percentage living below the federal poverty level, or the percentage of the elderly population living alone. Although we evaluated effect modification by neighborhood-level percentage below poverty and percentage living alone, individual-level measures might have been better indicators of vulnerability. In general, our ability to evaluate effect modification was limited by the small numbers of outcomes within the subgroups of interest.
Considerations for Future Analyses
Although LRTs demonstrated some model improvement by including indoor heat exposure, the differences were marginally significant. In addition, modeled indoor heat was very highly correlated with the percentage of households without central AC (Spearman’s of 0.92–1.0; Table S4). This is, in part, because data on variation in AC functionality and operation was not available. Nevertheless, one could argue that these findings suggest that in cities with high AC prevalence, simplified modeling approaches may adequately account for potential indoor heat exposure in vulnerable neighborhoods and could be employed to evaluate the impact of indoor heat on health. For example, when AC prevalence is high, a reasonable alternative to complex indoor modeling could be to include fine-scale AC prevalence as an effect modifier of the ambient temperature–health association. These are important findings given the intensive nature of the modeling performed for this study and the engineering expertise needed to inform EnergyPlus models. Although a simplified approach would greatly reduce the computational burden, and perhaps be more accessible to a greater number of researchers, it may not be appropriate for all study locations. For example, in locations with lower AC prevalence (e.g., Boston, Portland) other housing characteristics such as insulation level become more relevant, and detailed indoor modeling would be more impactful. Future building energy and indoor heat modeling research could elucidate alternative modeling approaches and help inform indoor heat–health analyses, particularly in study locations with low AC prevalence.
In addition, the indoor modeling approach undertaken for this study would have benefited greatly from additional data, which would have allowed indoor heat exposure to vary over time in neighborhoods with 100% central AC prevalence. Data that could be used to improve estimation and reduce exposure misclassification error include building or area-level window AC prevalence, the occurrence of any power outages over the study period, AC functionality and operational status, and occupant behavior and ability/willingness to use central AC, as well as more detailed data on housing characteristics and vegetative cover near residences. Unfortunately, these data are not easily accessible and may be very challenging to obtain, especially at the household level.
Limitations
Our ability to examine the impact of indoor heat on health among the elderly population was facilitated by a long 16-y study period; rich, patient-level data; and a novel methodology to model daily indoor heat exposure. Importantly, we validated the building models used in this study against measured data from four residential units in two cities (Houston and Phoenix) under different outdoor temperature profiles (Sailor et al. 2019). However, additional considerations should be acknowledged when interpreting results. First, this study considered many different statistical hypotheses, and we did not make adjustments to statistical significance to account for multiple testing. Therefore, it is possible that small differences in effect across different lag days and indoor heat metrics may be the result of chance. We did not consider secondary or tertiary causes of mortality/morbidity; magnitudes and patterns of association could differ with the use of secondary and tertiary diagnoses. In addition, our indoor heat models used ambient meteorological data that were averaged to the area level (climate subregions). Nevertheless, dividing the study area into five subregions for building models provided some spatial variation in the weather data input for the building energy models and gave us a higher resolution than the established typical meteorological year method that is the standard approach in building energy compliance simulations (Bhandari et al. 2012). Related to our indoor modeling process, three types of aggregation in this study may have induced exposure misclassification error: a) aggregating meteorological data to the local climate subregion scale; b) distilling thousands of different building configurations into 108 building archetypes; and c) weighting of indoor exposure metrics to the CBG level. We expect exposure misclassification error from these sources to be minimal and nondifferential across our study population given that our analysis related daily changes in indoor temperature to health outcomes and that day-to-day variation in ambient and indoor temperature/heat exposure for the entire study area was well captured by our methods.
Although the present study aspired to account for different types of occupant behavior in our indoor modeling work, we did not have the necessary data to capture spatial variation in window operation among different age and income groups, nor did we have an understanding of how other behaviors that influence indoor heat exposure (e.g., temperature settings, use of curtains/blinds, response to power outages) vary for our study population. However, EnergyPlus is capable of modeling a wide range of occupant behavior, and detailed household level survey data can be used to inform operation schemes, and model a variety of experiences (O’Lenick et al. 2019). Perhaps the most problematic assumption—resulting in a conservative estimate of the impact of indoor heat exposure on health—with our indoor heat model is that a building with central AC will always be adequately cooled. We know this assumption is not valid because a population-based survey we performed among the elderly population reported that approximately 20% of older Houstonians feel too hot in their homes despite having centralized AC. Undersized AC units resulting in poor performance, financial constraints, or maladaptive behaviors may prevent our study population from using their central AC to keep their homes adequately cooled. However, this study was not able to account for different factors influencing AC utilization and assumed that buildings with central AC were kept at a constant, comfortable temperature. We expect this type of exposure misclassification to bias toward the null and underestimate the effect of indoor heat on health. Another impact of this assumption is that it resulted in no temporal variation in indoor heat values for CBGs that reported 100% prevalence of central AC. These CBGs did not contribute to the estimation of association between indoor heat and health and may have impacted the generalizability of our findings. Ongoing work by our research group is exploring ways to examine stochastic elements in indoor modeling and capture the effect of AC systems that are undersized or otherwise performing poorly (Baniassadi et al. 2020). Future work will integrate estimates of conditions in homes with partially functioning AC to more accurately represent indoor environmental conditions.
Conclusion
Despite findings from heat wave–mortality studies that implicate indoor environments as a place where hazardous exposure to heat occurs, very few population-based heat–health studies account for indoor heat exposure. Thus, the impact of heat on health is likely underestimated and knowledge gaps regarding indoor heat–health thresholds, vulnerability, and adaptive capacity remain. In this analysis, we outline a novel methodology to estimate indoor heat exposure and explore the impacts of indoor heat on mortality and morbidity among the elderly population in Houston, Texas. Our findings suggest that short-term exposures to high indoor heat are associated with increased adverse health outcomes, especially deaths, among the older Houston population. Additional key findings from this study include the following: a) in study locations with high AC prevalence, simpler modeling approaches than the one presented here may adequately account for potential indoor heat exposure; b) additional data is necessary to better understand variation in indoor thermal conditions, particularly for homes with central AC; and c) certain populations and demographic groups experience high indoor heat. These exposures are important to consider to develop more informed risk assessments and better estimate the total impact of heat on health.
In Houston, ambient heat has been associated with increases in emergency hospitalizations (Zhang et al. 2015), increases in 911 calls (Heaton et al. 2015), and increased mortality (Chien et al. 2016; Heaton et al. 2019). Global and regional climate models suggest that Houston will have more heat stress days and nights (Oleson et al. 2015), and Houston is expected to experience increases in nonaccidental mortality above historical reference periods due to future climate and demographic shifts (Marsha et al. 2018; Rohat et al. 2019). Given the projected impacts in Houston and across the United States, a better understanding of the interactions between indoor and outdoor temperature, population vulnerability, and adaptive capacity is necessary to protect human health.
Supplementary Material
Acknowledgments
C.R.O., A.B., A.M., M.H.H, C.W., D.J.S., and O.V.W. designed the study and directed its implementation. A.B., R.M., A.M., J.B., C.W., P.J.C., and J.H. provided exposure data, analytical design and modeling assistance. X.Y. and K.Z. provided inpatient hospital data. C.R.O., A.B., R.M., X.Y., P.J.C., J.H., and P.H. analyzed the data. C.R.O., A.B., K.Z., D.J.S., and O.V.W. interpreted the results. P.H. provided graphic support. C.R.O., A.B., R.M., J.B., X.Y., M.H.H., C.W., A.M., P.J.C., K.Z., J.H., D.J.S., and O.V.W. wrote the manuscript.
We thank the Houston Health Department, especially D. Banerjee and V. Nepal, for their assistance in recruiting participants for our indoor air modeling validation study and for providing valuable insights into local public health responses to heat and air quality.
This research was supported by the U.S. Environmental Protection Agency (EPA) under award 83575401. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. EPA. Further, U.S. EPA does not endorse the purchase of any commercial products or services mentioned in this manuscript. The National Center for Atmospheric Research (NCAR) is sponsored by the National Science Foundation.
Data used in this study include hospital discharge data, death certificate data, American Community Survey (ACS) data, daily estimates of indoor heat exposure, and ozone concentration and weather data at the CBG level in Houston, Texas. NCAR institutional review board protocols and data use agreements with the Texas Department of State Health Services prevent sharing of the health data outside the research team. Daily weather and ozone concentration data were generated by the NCAR team; the outputs are available through NCAR’s Research Data Archive. Indoor heat exposure data were modeled by researchers at Arizona State University; the outputs are available through NCAR’s Research Data Archive. ACS data are publicly available through the U.S. Census Bureau.
References
- Alam M, Sanjayan J, Zou PXW, Stewart MG, Wilson J. 2016. Modelling the correlation between building energy ratings and heat-related mortality and morbidity. Sustain Cities Soc 22:29–39, 10.1016/j.scs.2016.01.006. [DOI] [Google Scholar]
- Anderson BG, Bell ML. 2009. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology 20(2):205–213, PMID: 19194300, 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML, Peng RD. 2013. Heat-related emergency hospitalizations for respiratory diseases in the Medicare population. Am J Respir Crit Care Med 187(10):1098–1103, PMID: 23491405, 10.1164/rccm.201211-1969OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baniassadi A, Heusinger J, Sailor DJ. 2018a. Energy efficiency vs resiliency to extreme heat and power outages: the role of evolving building energy codes. Build Environ 139:86–94, 10.1016/j.buildenv.2018.05.024. [DOI] [Google Scholar]
- Baniassadi A, Sailor DJ. 2018. Synergies and trade-offs between energy efficiency and resiliency to extreme heat—a case study. Build Environ 132:263–272, 10.1016/j.buildenv.2018.01.037. [DOI] [Google Scholar]
- Baniassadi A, Sailor DJ, Crank PJ, Ban-Weiss GA. 2018b. Direct and indirect effects of high-albedo roofs on energy consumption and thermal comfort of residential buildings. Energy Build 178:71–83, 10.1016/j.enbuild.2018.08.048. [DOI] [Google Scholar]
- Baniassadi A, Sailor DJ, O’Lenick CR, Wilhelmi OV, Crank PJ, Chester MV, et al. 2020. Effectiveness of mechanical air conditioning as a protective factor against indoor exposure to heat among the elderly. ASME J Eng Sustain Build Cities 1(1):011005, 10.1115/1.4045678. [DOI] [Google Scholar]
- Baniassadi A, Sailor DJ, Olenick CR. 2018c. Indoor air quality and thermal comfort for elderly residents in Houston TX—a case study. In: Proceedings of the 7th International Building Physics Conference. Zhang J, Bogucz E, Davidson C, Krietmeyer E, eds. 23–26 September 2018. Syracuse, NY: International Building Physics Conference, 787–792. [Google Scholar]
- Basu R. 2009. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health 8:40, PMID: 19758453, 10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R, Malig B. 2011. High ambient temperature and mortality in California: exploring the roles of age, disease, and mortality displacement. Environ Res 111(8):1286–1292, PMID: 21981982, 10.1016/j.envres.2011.09.006. [DOI] [PubMed] [Google Scholar]
- Basu R, Samet JM. 2002. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev 24(2):190–202, PMID: 12762092, 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- Benmarhnia T, Deguen S, Kaufman JS, Smargiassi A. 2015. Review article: vulnerability to heat-related mortality: a systematic review, meta-analysis, and meta-regression analysis. Epidemiology 26(6):781–793, PMID: 26332052, 10.1097/EDE.0000000000000375. [DOI] [PubMed] [Google Scholar]
- Bhandari M, Shrestha S, New J. 2012. Evaluation of weather datasets for building energy simulation. Energy Build 49:109–118, 10.1016/j.enbuild.2012.01.033. [DOI] [Google Scholar]
- Braga ALF, Zanobetti A, Schwartz J. 2002. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect 110(9):859–863, PMID: 12204818, 10.1289/ehp.02110859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley JP, Samet JM, Richardson DB. 2014. Commentary: does air pollution confound studies of temperature? Epidemiology 25(2):242–245, PMID: 24487206, 10.1097/EDE.0000000000000051. [DOI] [PubMed] [Google Scholar]
- Bunker A, Wildenhain J, Vandenbergh A, Henschke N, Rocklöv J, Hajat S, et al. 2016. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 6:258–268, PMID: 27211569, 10.1016/j.ebiom.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (Centers for Disease Control and Prevention). 2013a. Heat illness and deaths–New York City, 2000–2011. MMWR Morb Mortal Wkly Rep 62:617–621, PMID: 23925170. [PMC free article] [PubMed] [Google Scholar]
- CDC. 2013b. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). http://www.cdc.gov/nchs/icd/icd9cm.htm [accessed 23 November 2020].
- Cedeño Laurent JG, Williams A, Oulhote Y, Zanobetti A, Allen JG, Spengler JD. 2018. Reduced cognitive function during a heat wave among residents of non-air-conditioned buildings: an observational study of young adults in the summer of 2016. PLoS Med 15(7):e1002605, PMID: 29990359, 10.1371/journal.pmed.1002605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng J, Xu Z, Zhu R, Wang X, Jin L, Song J, et al. 2014. Impact of diurnal temperature range on human health: a systematic review. Int J Biometeorol 58(9):2011–2024, PMID: 24535132, 10.1007/s00484-014-0797-5. [DOI] [PubMed] [Google Scholar]
- Chien LC, Guo Y, Zhang K. 2016. Spatiotemporal analysis of heat and heat wave effects on elderly mortality in Texas, 2006–2011. Sci Total Environ 562:845–851, PMID: 27110995, 10.1016/j.scitotenv.2016.04.042. [DOI] [PubMed] [Google Scholar]
- Chvatal KMS, Corvacho H. 2009. The impact of increasing the building envelope insulation upon the risk of overheating in summer and an increased energy consumption. J Build Perform Simul 2(4):267–282, 10.1080/19401490903095865. [DOI] [Google Scholar]
- Crawley DB, Lawrie LK, Pedersen CO, Winkelmann FC, Witte MJ, Strand RK, et al. 2004. EnergyPlus: new, capable, and linked. J Archit Plann Res 21(4):292–302. https://www.jstor.org/stable/43030706 [accessed 24 November 2020]. [Google Scholar]
- Crawley DB, Linda KL, Frederick CW, Walter FB, Y JH, Curtis OP, Richard KS , et al. 2001. EnergyPlus: creating a new-generation building energy simulation program. Energy and Buildings 33(4):319–331. 10.1016/S0378-7788(00)00114-6. [DOI] [Google Scholar]
- Fouillet A, Rey G, Laurent F, Pavillon G, Bellec S, Guihenneuc-Jouyaux C, et al. 2006. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health 80(1):16–24, PMID: 16523319, 10.1007/s00420-006-0089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frey SE, Destaillats H, Cohn S, Ahrentzen S, Fraser MP. 2014. Characterization of indoor air quality and resident health in an Arizona senior housing apartment building. J Air Waste Manag Assoc 64(11):1251–1259, PMID: 25509546, 10.1080/10962247.2014.937513. [DOI] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B. 2011. The impact of heat waves on mortality. Epidemiology 22(1):68–73, PMID: 21150355, 10.1097/EDE.0b013e3181fdcd99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. 2015. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386(9991):369–375, PMID: 26003380, 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronlund CJ. 2014. Racial and socioeconomic disparities in heat-related health effects and their mechanisms: a review. Curr Epidemiol Rep 1(3):165–173, PMID: 25512891, 10.1007/s40471-014-0014-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS. 2014. Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006. Environ Health Perspect 122(11):1187–1192, PMID: 24905551, 10.1289/ehp.1206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu L. 2007. Airflow network modeling in EnergyPlus. In: Proceedings, 10th International Building Performance Simulation Association Conference and Exhibition. 3–6 September 2007. Cocoa, FL: Florida Solar Energy Center/University of Central Florida, 964–972. [Google Scholar]
- Guo Y, Gasparrini A, Armstrong BG, Tawatsupa B, Tobias A, Lavigne E, et al. 2017. Heat wave and mortality: a multicountry, multicommunity study. Environ Health Perspect 125(8):087006, PMID: 28886602, 10.1289/EHP1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat S, Kosatky T. 2010. Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health 64(9):753–760, PMID: 19692725, 10.1136/jech.2009.087999. [DOI] [PubMed] [Google Scholar]
- Hayden MH, Wilhelmi OV, Banerjee D, Greasby T, Cavanaugh JL, Nepal V, et al. 2017. Adaptive capacity to extreme heat: results from a household survey in Houston, Texas. Weather Clim Soc 9(4):787–799, 10.1175/WCAS-D-16-0125.1. [DOI] [Google Scholar]
- Heaton MJ, Olenick CR, Wilhelmi O. 2019. Age-specific distributed lag models for heat-related mortality. Environmetrics 30(7):e2561, 10.1002/env.2561. [DOI] [Google Scholar]
- Heaton MJ, Sain SR, Greasby TA, Uejio CK, Hayden MH, Monaghan AJ, et al. 2014. Characterizing urban vulnerability to heat stress using a spatially varying coefficient model. Spat Spatiotemporal Epidemiol 8:23–33, PMID: 24606992, 10.1016/j.sste.2014.01.002. [DOI] [PubMed] [Google Scholar]
- Heaton MJ, Sain SR, Monaghan AJ, Wilhelmi OV, Hayden MH. 2015. An analysis of an incomplete marked point pattern of heat-related 911 calls. J Am Stat Assoc 110(509):123–135, 10.1080/01621459.2014.983229. [DOI] [Google Scholar]
- Henninger RH, Witte MJ. 2010. EnergyPlus Testing with Building Thermal Envelope and Fabric Load Tests from ANSI/ASHRAE Standard 140–2007. EnergyPlus version 6.0.0.023. Prepared for U.S. Department of Energy. https://labeee.ufsc.br/sites/default/files/disciplinas/ECV4202_EnergyPlus%20testing%20with%20Ashrae140.pdf [accessed 24 November 2020].
- Hensen JE, Lamberts RE. 2011. Building Performance Simulation for Design and Operation. 1st ed London, UK: Spon. [Google Scholar]
- Kaiser R, Le Tertre A, Schwartz J, Gotway CA, Daley WR, Rubin CH. 2007. The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am J Public Health 97(suppl 1):S158–S162, PMID: 17413056, 10.2105/AJPH.2006.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman JS, MacLehose RF. 2013. Which of these things is not like the others? Cancer 119(24):4216–4222, PMID: 24022386, 10.1002/cncr.28359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney WL, Craighead DH, Alexander LM. 2014. Heat waves, aging, and human cardiovascular health. Med Sci Sports Exerc 46(10):1891–1899, PMID: 24598696, 10.1249/MSS.0000000000000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klepeis NE, Bellettiere J, Hughes SC, Nguyen B, Berardi V, Liles S, et al. 2017. Fine particles in homes of predominantly low-income families with children and smokers: key physical and behavioral determinants to inform indoor-air-quality interventions. PLoS One 12(5):e0177718, PMID: 28545099, 10.1371/journal.pone.0177718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klepeis NE, Nelson WC, Ott WR, Robinson JP, Tsang AM, Switzer P, et al. 2001. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol 11(3):231–252, PMID: 11477521, 10.1038/sj.jea.7500165. [DOI] [PubMed] [Google Scholar]
- Kovats RS, Hajat S, Wilkinson P. 2004. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occup Environ Med 61(11):893–898, PMID: 15477282, 10.1136/oem.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuras ER, Richardson MB, Calkins MM, Ebi KL, Hess JJ, Kintziger KW, et al. 2017. Opportunities and challenges for personal heat exposure research. Environ Health Perspect 125(8):085001, PMID: 28796630, 10.1289/EHP556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laaidi K, Zeghnoun A, Dousset B, Bretin P, Vandentorren S, Giraudet E, et al. 2012. The impact of heat islands on mortality in Paris during the August 2003 heat wave. Environ Health Perspect 120(2):254–259, PMID: 21885383, 10.1289/ehp.1103532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R. 2009. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 20(5):738–746, PMID: 19593155, 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- Loutzenhiser PG, Manz H, Moosberger S, Maxwell GM. 2009. An empirical validation of window solar gain models and the associated interactions. Int J Therm Sci 48(1):85–95, 10.1016/j.ijthermalsci.2008.01.011. [DOI] [Google Scholar]
- Marsha A, Sain SR, Heaton MJ, Monaghan AJ, Wilhelmi OV. 2018. Influences of climatic and population changes on heat-related mortality in Houston, Texas, USA. Clim Change 146(3–4):471–485, 10.1007/s10584-016-1775-1. [DOI] [Google Scholar]
- Mateus NM, Pinto A, Carrilho da Graça G. 2014. Validation of EnergyPlus thermal simulation of a double skin naturally and mechanically ventilated test cell. Energy Build 75:511–522, 10.1016/j.enbuild.2014.02.043. [DOI] [Google Scholar]
- McCormack MC, Belli AJ, Waugh D, Matsui EC, Peng RD, Williams DL, et al. 2016. Respiratory effects of indoor heat and the interaction with air pollution in chronic obstructive pulmonary disease. Ann Am Thorac Soc 13(12):2125–2131, PMID: 27684429, 10.1513/AnnalsATS.201605-329OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod RS, Hopfe CJ, Kwan A. 2013. An investigation into future performance and overheating risks in Passivhaus dwellings. Build Environ 70:189–209, 10.1016/j.buildenv.2013.08.024. [DOI] [Google Scholar]
- Michael R, O’Lenick CR, Monaghan A, Wilhelmi O, Wiedinmyer C, Hayden M, et al. 2019. Application of geostatistical approaches to predict the spatio-temporal distribution of summer ozone in Houston, Texas. J Expo Sci Environ Epidemiol 29(6):806–820, PMID: 30451934, 10.1038/s41370-018-0091-4. [DOI] [PubMed] [Google Scholar]
- Michelozzi P, Accetta G, De Sario M, D’Ippoliti D, Marino C, Baccini M, et al. 2009. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med 179(5):383–389, PMID: 19060232, 10.1164/rccm.200802-217OC. [DOI] [PubMed] [Google Scholar]
- Monaghan AJ, Hu L, Brunsell NA, Barlage M, Wilhelmi OV. 2014. Evaluating the impact of urban morphology configurations on the accuracy of urban canopy model temperature simulations with MODIS. J Geophys Res Atmos 119(11):6376–6392, 10.1002/2013JD021227. [DOI] [Google Scholar]
- Nahlik MJ, Chester MV, Pincetl SS, Eisenman D, Sivaraman D, English P. 2017. Building thermal performance, extreme heat, and climate change. J Infrastruct Syst 23(3):04016043, 10.1061/(ASCE)IS.1943-555X.0000349. [DOI] [Google Scholar]
- O’Lenick CR, Wilhelmi OV, Michael R, Hayden MH, Baniassadi A, Wiedinmyer C, et al. 2019. Urban heat and air pollution: a framework for integrating population vulnerability and indoor exposure in health risk analyses. Sci Total Environ 660:715–723, PMID: 30743957, 10.1016/j.scitotenv.2019.01.002. [DOI] [PubMed] [Google Scholar]
- O’Lenick CR, Winquist A, Chang HH, Kramer MR, Mulholland JA, Grundstein A, et al. 2017. Evaluation of individual and area-level factors as modifiers of the association between warm-season temperature and pediatric asthma morbidity in Atlanta, GA. Environ Res 156:132–144, PMID: 28342349, 10.1016/j.envres.2017.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill MS, Zanobetti A, Schwartz J. 2003. Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol 157(12):1074–1082, PMID: 12796043, 10.1093/aje/kwg096. [DOI] [PubMed] [Google Scholar]
- O’Neill MS, Zanobetti A, Schwartz J. 2005. Disparities by race in heat-related mortality in four US cities: the role of air conditioning prevalence. J Urban Health 82(2):191–197, PMID: 15888640, 10.1093/jurban/jti043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oleson KW, Monaghan A, Wilhelmi O, Barlage M, Brunsell N, Feddema J, et al. 2015. Interactions between urbanization, heat stress, and climate change. Clim Change 129(3–4):525–541, 10.1007/s10584-013-0936-8. [DOI] [Google Scholar]
- Ramakrishnan S, Wang X, Sanjayan J, Wilson J. 2017. Thermal performance of buildings integrated with phase change materials to reduce heat stress risks during extreme heatwave events. Appl Energy 194:410–421, 10.1016/j.apenergy.2016.04.084. [DOI] [Google Scholar]
- Reid CE, Snowden JM, Kontgis C, Tager IB. 2012. The role of ambient ozone in epidemiologic studies of heat-related mortality. Environ Health Perspect 120(12):1627–1630, PMID: 22899622, 10.1289/ehp.1205251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Z, Wang X, Chen D. 2014. Heat stress within energy efficient dwellings in Australia. Archit Sci Rev 57(3):227–236, 10.1080/00038628.2014.903568. [DOI] [Google Scholar]
- Rohat G, Wilhelmi O, Flacke J, Monaghan A, Gao J, Dao H, et al. 2019. Characterizing the role of socioeconomic pathways in shaping future urban heat-related challenges. Sci Total Environ 695:133941, PMID: 31756866, 10.1016/j.scitotenv.2019.133941. [DOI] [PubMed] [Google Scholar]
- Sailor DJ, Baniassadi A, O’Lenick CR, Wilhelmi OV. 2019. The growing threat of heat disasters. Environ Res Lett 14(5):054006, 10.1088/1748-9326/ab0bb9. [DOI] [Google Scholar]
- Sailor DJ, Hu H, Wilhelmi O, Banerjee D. 2015. Indoor-outdoor environmental coupling and exposure risk to extreme heat and poor air quality during heat waves. In: Proceedings of the 9th International Conference on Urban Climate jointly with 12th Symposium on the Urban Environment 20–24 July 2015. Boston, MA: International Association for Urban Climate/American Meteorological Society; http://www.meteo.fr/cic/meetings/2015/ICUC9/LongAbstracts/bph2-1-4601436_a.pdf [accessed 24 November 2020]. [Google Scholar]
- Semenza JC, Rubin CH, Falter KH, Selanikio JD, Flanders WD, Howe HL, et al. 1996. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med 335(2):84–90, PMID: 8649494, 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- Shrestha SS, Maxwell G. 2011. Empirical validation of building energy simulation software: EnergyPlus. In: Proceedings of Building Simulation 2011: 12th Conference of International Building Performance Simulation Association 14–16 November 2011. Sydney, Australia: International Building Performance Simulation Association, 2935–2942. [Google Scholar]
- Stull R. 2011. Wet-bulb temperature from relative humidity and air temperature. J Appl Meteorol Climatol 50(11):2267–2269, 10.1175/JAMC-D-11-0143.1. [DOI] [Google Scholar]
- Tabares-Velasco PC, Christensen C, Bianchi M. 2012. Verification and validation of EnergyPlus phase change material model for opaque wall assemblies. Build Environ 54:186–196, 10.1016/j.buildenv.2012.02.019. [DOI] [Google Scholar]
- U.S. Census Bureau. 2018. U.S. Census Bureau: quick facts, Houston, Texas. https://www.census.gov/quickfacts/houstoncitytexas [accessed 2 October 2019].
- Uejio CK, Tamerius JD, Vredenburg J, Asaeda G, Isaacs DA, Braun J, et al. 2016. Summer indoor heat exposure and respiratory and cardiovascular distress calls in New York City, NY, U.S. Indoor Air 26(4):594–604, PMID: 26086869, 10.1111/ina.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Loenhout JAF, le Grand A, Duijm F, Greven F, Vink NM, Hoek G, et al. 2016. The effect of high indoor temperatures on self-perceived health of elderly persons. Environ Res 146:27–34, PMID: 26710340, 10.1016/j.envres.2015.12.012. [DOI] [PubMed] [Google Scholar]
- White-Newsome JL, Sánchez BN, Jolliet O, Zhang Z, Parker EA, Dvonch JT, et al. 2012. Climate change and health: indoor heat exposure in vulnerable populations. Environ Res 112:20–27, PMID: 22071034, 10.1016/j.envres.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (World Health Organization). 2016. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. http://apps.who.int/classifications/icd10/browse/2016/en [accessed 23 November 2020].
- Winquist A, Grundstein A, Chang HH, Hess J, Sarnat SE. 2016. Warm season temperatures and emergency department visits in Atlanta, Georgia. Environ Res 147:314–323, PMID: 26922412, 10.1016/j.envres.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte MJ, Henninger RH, Glazer J, Crawley DB. 2001. Testing and validation of a new building energy simulation program. In: Proceedings of Building Simulation 2001 13–15 August 2001. Rio de Janeiro, Brazil: International Building Performance Simulation Association. [Google Scholar]
- Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S. 2012. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect 120(1):19–28, PMID: 21824855, 10.1289/ehp.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu T, Heiselberg P, Lei B, Pomianowski M. 2014. Validation and modification of modeling thermally activated building systems (TABS) using EnergyPlus. Build Simul 7(6):615–627, 10.1007/s12273-014-0183-6. [DOI] [Google Scholar]
- Zhang K, Chen TH, Begley CE. 2015. Impact of the 2011 heat wave on mortality and emergency department visits in Houston, Texas. Environ Health 14:11, PMID: 25627975, 10.1186/1476-069X-14-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou W, Ji S, Chen TH, Hou Y, Zhang K. 2014. The 2011 heat wave in Greater Houston: effects of land use on temperature. Environ Res 135:81–87, PMID: 25262079, 10.1016/j.envres.2014.08.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.