Abstract
OBJECTIVE:
To describe characteristics of the full population of women who participated in the Zika Contraception Access Network program in Puerto Rico during the virus outbreak and to examine factors associated with removal of a long-acting reversible contraception (LARC) method by a Zika Contraception Access Network provider during the program’s duration (May 2016– September 2017).
METHODS:
We conducted an observational cohort study. The Zika Contraception Access Network program was designed to increase access to contraception services in Puerto Rico for women who chose to prevent pregnancy during the Zika virus outbreak as a primary strategy to reduce adverse Zika virus–related pregnancy and birth outcomes. Among program participants, an observational cohort of women served by the Zika Contraception Access Network Program, we describe their demographic and program-specific characteristics, including contraceptive method mix before and after the program. We also report on LARC removals by Zika Contraception Access Network providers during the program. We examined factors associated with LARC removal using multivariable logistic regression.
RESULTS:
A total of 29,221 women received an initial Zika Contraception Access Network visit during the program. Ninety-six percent (27,985) of women received same-day provision of a contraceptive method and 70% (20,381) chose a LARC method. While the program was active, 719 (4%) women who chose a LARC at the initial visit had it removed. Women with a college degree or higher were more likely to have their LARC removed (adjusted prevalence ratio [aPR] 1.24); breastfeeding women (aPR 0.67) and those using a LARC method before Zika Contraception Access Network (aPR 0.55) were less likely to have their LARC removed.
CONCLUSION:
The Zika Contraception Access Network program was designed as a short-term response for rapid implementation of contraceptive services in a complex emergency setting in Puerto Rico and served more than 29,000 women. The Zika Contraception Access Network program had high LARC uptake and a low proportion of removals by a Zika Contraception Access Network provider during the program. A removal-inclusive design, with access to removals well beyond the program period, maximizes women’s reproductive autonomy to access LARC removal when desired. This model could be replicated in other settings where the goal is to increase contraception access.
The Zika Contraception Access Network was an emergency response intervention established to increase access to contraception among women who chose to prevent pregnancy during the 2016–2017 Zika virus outbreak in which Puerto Rico reported the highest number of Zika virus cases in the United States.1,2 Zika virus infection during pregnancy can cause severe brain abnormalities, including micro-cephaly, and eye defects.3 Strategies to prevent Zika virus infection in pregnant women include the elimination of mosquitos in the environment, prevention of mosquito bites, protection of pregnant women from sexual transmission of the Zika virus, and prevention of pregnancy among women who choose to delay or avoid pregnancy during the Zika virus outbreak.4
Access to contraception in Puerto Rico before the Zika Contraception Access Network was limited by reduced availability of the full-range of reversible contraceptive methods, high out-of-pocket costs, insufficient health care provider reimbursement, barriers that limited same-day provision, lack of patient education, and shortage of providers trained in insertion, removal, and management of long-acting reversible contraception (LARC), which includes intrauterine devices (IUDs) and contraceptive implants.5 Additionally, before the Zika virus outbreak, the estimated proportion of unintended pregnancies was higher in Puerto Rico than the United States (65% vs 45%).5,6 These predicates, coupled with the high caseload of Zika virus in Puerto Rico during the 2016–2017 outbreak, led to the development of the Zika Contraception Access Network program, a short-term emergency response that trained a network of physicians across Puerto Rico to provide client-centered contraceptive counseling and same-day access to the full-range of reversible contraceptive methods at no cost for women who chose to prevent pregnancy.1,7
The Zika Contraception Access Network program was designed to increase access to contraception by removing identified barriers and providing the full range of reversible contraceptive methods at no cost to promote high contraception uptake including LARC placement.1,7 Strategies were incorporated to mitigate potential coercion and facilitate evidence-based practices in contraception service delivery.8,9 Concerns of health care provider coercion of women when LARC methods are promoted over other methods or the refusal to remove LARC methods, have highlighted the importance that contraception access programs, whether in stable or complex emergency contexts, are client-centered and that the women have reproductive autonomy to choose what method best fits their needs and have access to removal when requested.10–12 Given the historical context of coerced sterilization and unethical testing of oral contraceptives in Puerto Rico13–15 and concerns for reproductive coercion,16,17 the Zika Contraception Access Network program incorporated ethical considerations, safeguards, and best practices frame works for contraception service delivery, including offering the full range of reversible contraceptive methods and having a removal-inclusive component to allow women who chose a LARC method through the Zika Contraception Access Network and obtain a removal from any Zika Contraception Access Network provider during or beyond the lifetime of the program at no cost to her.7
We previously described the Zika Contraception Access Network program design, implementation activities, and baseline characteristics of the first 21,124 women who participated in the Zika Contraception Access Network.1 Here we describe characteristics of the full population of women served by the Zika Contraception Access Network (N529,221) and examine factors associated with removal of a LARC method by a Zika Contraception Access Network provider during the program’s duration (May 2016– September 2017).
METHODS
This article reports on data analyzed from an observational cohort of women served by the Zika Contraception Access Network program. The methods used to design and implement the Zika Contraception Access Network program have been reported previously,1,7 and will be briefly described. The Zika Contraception Access Network program was designed to address gaps in contraception access and service provision in Puerto Rico as a preventive measure to reduce Zika virus–related adverse pregnancy and birth outcomes. The development of the Zika Contraception Access Network was multifaceted and included several program development and implementation strategies to rapidly remove barriers to contraception access across Puerto Rico’s health system.
Given the identified gaps in contraceptive access and service provision,5 it was necessary to strengthen capacity among health care providers and staff in contraception knowledge, client-centered contraceptive counseling, and initiation and management of LARC, including the insertion and removal procedures. Before the Zika Contraception Access Network, none of the participating clinics routinely provided levonorgestrel-releasing IUDs or contraceptive implants, and access to copper IUDs was limited. The Zika Contraception Access Network program recruited physicians and clinic staff from all areas of the island, who practiced in private and publicly-funded clinics and were interested in becoming part of the network of trained Zika Contraception Access Network providers to address the needs of women who chose to delay or prevent pregnancy during the Zika virus outbreak.1 Posttraining, a Zika Contraception Access Network program staff member and a family planning specialist proctored providers and clinic staff to ensure delivery of high quality care.1
At the initial Zika Contraception Access Network visit, physicians and clinic staff recorded women’s demographic information, reproductive and contraception histories, and the contraceptive method chosen. To eliminate cost barriers, all Zika Contraception Access Network services were provided to women at no cost.
Data were submitted without personal identifying information to the Zika Contraception Access Network program and entered into a REDCap database hosted on a secure server at the Centers for Disease Control and Prevention.18 Descriptive statistics on program participants were generated. Unadjusted and adjusted prevalence ratios with 95% CIs were estimated to examine factors associated with removal of a LARC method by a Zika Contraception Access Network provider while the Zika Contraception Access Network program was active. We examined effect modification by age group. Data were analyzed using SAS-callable SUDAAN 11.0.0, a statistical software package for analyzing correlated data, to account for clustering of patients within clinic-provider dyads. Reasons for discontinuation were tabulated from the program database.
The Zika Contraception Access Network programmatic data were determined to be nonresearch public health practice thus did not require review from the Institutional Review Board nor necessitate Office of Management and Budget Paperwork Reduction Act approval.
RESULTS
The results reported here include all data ultimately available for Zika Contraception Access Network patients seen during the program, including new initial Zika Contraception Access Network visits and any missing data from the 17-month implementation period. From May 4, 2016, to September 23, 2017, a total of 29,221 women received an initial Zika Contraception Access Network visit during the program (Table 1). The mean age of participants was 26 years old and the age range was 12–54 years (data not shown). Most women were married or had a partner (56%) and had more than a high school education (60%). Half (52%) of women had public insurance, and 5% reported having no insurance. About 58% of women had at least one previous live birth, 95% reported not wanting to conceive in the next year, and 96% received a contraceptive method on the day of their initial visit.
Table 1.
Characteristics of All Women Who Participated in the Zika Contraception Access Network and Women Who Received a LARC Method at the Initial Zika Contraception Access Network Visit
| Patient Characteristics | All Women | Received LARC |
|---|---|---|
| Age (y) | ||
| Younger than 20 | 6,436/29,221 (22.0) | 4,365/20,381 (21.4) |
| 21–24 | 8,433/29,221 (28.9) | 6,018/20,381 (29.5) |
| 25–34 | 10,556/29,221 (36.1) | 7,395/20,381 (36.3) |
| Older than 35 | 3,497/29,221 (12.0) | 2,407/20,381 (11.8) |
| Relationship status | ||
| Single | 12,532/29,221 (42.9) | 8,430/20,381 (41.4) |
| Married or partnered | 16,247/29,221 (55.6) | 11,686/20,381 (57.3) |
| Education | ||
| Less than 12 y | 11,238/29,221 (38.5) | 7,810/20,381 (38.3) |
| College degree | 17,520/29,221 (60.0) | 12,293/20,381 (60.3) |
| Insurance status | ||
| Private or other | 11,783/29,221 (40.3) | 8,074/20,381 (39.6) |
| Public | 15,216/29,221 (52.1) | 10,689/20,381 (52.5) |
| None | 1,585/29,221 (5.4) | 1,188/20,381 (5.8) |
| Previous live birth | ||
| 0 | 11,463/29,221 (39.2) | 6,835/20,381 (33.5) |
| 1 or more | 16,992/29,221 (58.2) | 13,046/20,381 (64.0) |
| Breastfeeding at time of initial visit | ||
| No | 23,919/29,221 (81.9) | 16,262/20,381 (79.8) |
| Yes | 4,644/29,221 (15.9) | 3,679/20,381 (18.1) |
| Clinic type where initial visit occurred | ||
| CHC | 5,703/29,221 (19.5) | 3,509/20,381 (17.2) |
| Private practice or other | 23,518/29,221 (80.5) | 16,872/20,381 (82.8) |
| Did not want to conceive in the next year | 27,845/29,221 (95.3) | 19,606/20,381 (96.2) |
| Received same-day provision of a reversible contraceptive method | 27,985/29,221 (95.8) | 20,381/20,381 (100.0) |
| Effectiveness of contraceptive method used before Z-CAN* | ||
| None | 13,225/29,221 (45.3) | 9,284/20,381 (45.6) |
| Least | 8,680/29,221 (29.7) | 6,432/20,381 (31.6) |
| Moderately | 5,923/29,221 (20.3) | 3,593/20,381 (17.6) |
| Most | 1,075/29,221 (3.7) | 872/20,381 (4.3) |
| Effectiveness of contraceptive method provided at initial Z-CAN visit* | ||
| None | 1,236/29,221 (4.2) | — |
| Least | 816/29,221 (2.8) | — |
| Moderately | 6,788/29,221 (23.2) | — |
| Most | 20,381/29,221 (69.8) | 20,381/20,381 (100.0) |
| LARC type provided at initial Z-CAN visit | ||
| LNG-IUD | 9,316/20,381 (45.7) | |
| Copper IUD | 2,960/20,381 (14.5) | |
| ETN implant | 8,105/20,381 (39.8) |
LARC, long-acting reversible contraception; CHC, Community Health Center; Z-CAN, Zika Contraception Access Network; LNG, levonorgestrel; IUD, intrauterine device; ETN, etonogestrel.
Data are n/N (%).
Proportions may not add to 100% owing to missing data.
Least effective contraceptive methods include male and female condoms, withdrawal, sponge, fertility awareness methods, and spermicides. Moderately effective contraceptive methods include injectables, pills, patch, ring, and diaphragm. Most effective contraceptive methods include intrauterine devices, implants, and partner sterilization. Sterilized women were not eligible for Z-CAN services. Methods provided by Z-CAN included intrauterine devices, implants, injectables, pills, patch, ring, and male condoms.
Before their initial Zika Contraception Access Network visit, most women used either no method (45%) or one of the least effective contraceptive methods (30%), which includes condoms, withdrawal, sponge, fertility awareness methods, and spermicides. Only 4% of women used one of the most effective methods (male sterilization, IUD, or implant). At their visit, more than two thirds of women (70%) chose a most effective method (IUD or implant); 23% chose a moderately effective method (injectable, pills, patch, or ring); 3% chose a least effective method (condoms only); and 4% left without a method of contraception. Of those who left without a contraceptive method (n51,236), the most common reasons included: the woman was undecided on method preference or not ready to receive the method that day (42%), a pregnancy could not be ruled out (22%), or the desired method was not in stock (9%).
Among women who chose a LARC method (n520,381), the distribution of patient characteristics was similar to the distribution described above for all women served by the Zika Contraception Access Network (Table 1), although statistical testing was not conducted. Additionally, 46% chose a levonorgestrel-releasing IUD, 40% chose an etonogestrel implant, and 15% chose a copper IUD. While the program was active, 719 women who had a LARC method inserted at their initial Zika Contraception Access Network visit had the method removed by a Zika Contraception Access Network provider (4%) (Table 2). Women were more likely to have a LARC removal if they had a college degree or higher compared with women with a high school education or less after adjustment for all other characteristics (Table 2). Women who were breastfeeding at the time of the initial visit compared with those who were not, and women who were using a LARC method before the Zika Contraception Access Network compared with women using no method before the Zika Contraception Access Network, were less likely to have a LARC removal. Age, relationship status, insurance status, parity, and clinic type where the initial visit occurred were not associated with LARC removal by a Zika Contraception Access Network provider during the program. Associations did not vary by age group. The most common reasons for removal were irregular bleeding and pelvic pain (Table 3).
Table 2.
Factors Associated With Removal of a Long-Acting Reversible Contraception Method* During the Zika Contraception Access Network Program (May 4, 2016–September 23, 2017) Among 20,381 Women Who Received a Long-Acting Reversible Contraception Method at the Initial Visit
| Characteristics | Removal (n=719) |
No Removal (n=19,662) |
Unadjusted PR (95% CI) |
Adjusted PR (95% CI)† |
|---|---|---|---|---|
| Age (y) | ||||
| Younger than 20 | 144/705 (20.4) | 4,221/19,480 (21.7) | Referent | Referent |
| 21–24 | 214/705 (30.4) | 5,804/19,480 (29.8) | 1.08 (0.89–1.31) | 0.99 (0.80–1.24) |
| 25–34 | 276/705 (39.2) | 7,119/19,480 (36.6) | 1.13 (0.93–1.38) | 1.01 (0.80, 1.27) |
| Older than 35 | 71/705 (10.1) | 2,336/19,480 (12.0) | 0.89 (0.69–1.15) | 0.78 (0.59–1.03) |
| Relationship status | ||||
| Single | 304/705 (43.0) | 8,126/19,411 (42.0) | Referent | Referent |
| Married or partnered | 401/705 (56.9) | 11,285/19,411 (58.0) | 0.95 (0.80–1.13) | 0.97 (0.81–1.17) |
| Education | ||||
| Less than 12 y | 241/703 (34.3) | 7,569/19,400 (39.0) | Referent | Referent |
| College or graduate degree | 462/703 (65.7) | 11,831/19,400 (61.0) | 1.22 (1.04–1.43)‡ | 1.24 (1.03–1.48)‡ |
| Insurance status | ||||
| Private or other | 288/697 (41.3) | 7,786/19,254 (40.4) | Referent | Referent |
| Public | 361/697 (51.8) | 10,328/19,254 (53.6) | 0.95 (0.77–1.16) | 0.99 (0.79–1.23) |
| None | 48/697 (6.9) | 1,140/19,254 (5.9) | 1.13 (0.83–1.55) | 1.18 (0.86–1.62) |
| Previous live birth | ||||
| 0 | 242/697 (34.7) | 6,593/19,184 (34.4) | Referent | Referent |
| 1 or more | 455/697 (65.3) | 12,591/19,184 (65.6) | 0.99 (0.83–1.17) | 1.15 (0.94–1.40) |
| Breastfeeding at time of initial visit | ||||
| No | 605/703 (86.1) | 15,657/19,238 (81.4) | Referent | Referent |
| Yes | 98/703 (13.9) | 3,581/19,238 (18.6) | 0.72 (0.58–0.88)‡ | 0.67 (0.54–0.84)‡ |
| Effectiveness of contraceptive method used before Z-CAN§ | ||||
| None | 318/710 (44.8) | 8,966/19,471 (46.1) | Referent | Referent |
| Least | 232/710 (32.7) | 6,200/19,471 (31.8) | 1.05 (0.87–1.27) | 1.02 (0.84–1.22) |
| Moderately | 141/710 (19.9) | 3,452/19,471 (17.7) | 1.15 (0.94–1.40) | 1.08 (0.88–1.33) |
| Most | 19/710 (2.7) | 853/19,471 (4.4) | 0.64 (0.42–0.97)‡ | 0.55 (0.33–0.90)‡ |
| Clinic type where initial visit occurred | ||||
| CHC | 111/719 (15.4) | 3,398/19,662 (17.3) | Referent | Referent |
| Private practice or other | 608/719 (84.6) | 16,264/19,662 (82.7) | 1∙14 (0.90–1.44) | 1∙08 (0.85–1.38) |
PR, prevalence ratio; Z-CAN, Zika Contraceptive Access Network; CHC, Community Health Center.
Data are n/N (%) unless otherwise specified.
Removed and reported by a Z-CAN provider.
Each characteristic in the table was adjusted for all other characteristics.
95% CI does not include 1.
Least effective contraceptive methods include male and female condoms, withdrawal, sponge, fertility awareness methods, and spermicides. Moderately effective contraceptive methods include injectables, pills, patch, ring, and diaphragm. Most effective contraceptive methods include intrauterine devices (IUDs), implants, and partner sterilization. Sterilized women were not eligible for Z-CAN services.
Table 3.
Reasons for Long-Acting Reversible Contraception Method Removal During the Zika Contraception Access Network Program
| Reason for Removal | All LARC Methods (n=580)* |
LNG IUD (n=290) |
Copper IUD (n=79) |
ETN Implant (n=211) |
|---|---|---|---|---|
| Irregular bleeding | 180 (31) | 79 (27) | 27 (34) | 74 (35) |
| Pelvic pain | 99 (17) | 80 (28) | 17 (22) | 2 (1) |
| Arm pain | 7 (1) | 0 (0) | 0 (0) | 7 (3) |
| Decreased libido | 3 (1) | 0 (0) | 0 (0) | 3 (1) |
| Desires pregnancy | 16 (3) | 8(3) | 1 (1) | 7 (3) |
| Does not like method | 28 (5) | 17 (6) | 8 (10) | 3 (1) |
| Headache | 14 (2) | 4(1) | 0 (0) | 10 (5) |
| Mood changes | 15 (3) | 4(1) | 0 (0) | 11 (5) |
| Pain with sex | 7 (1) | 4(1) | 3 (4) | 0 (0) |
| Pelvic infection | 12 (2) | 11 (4) | 1 (1) | 0 (0) |
| Weight gain | 14 (2) | 5 (2) | 0 (0) | 9 (4) |
| Other† | 185 (32) | 78 (27) | 22 (28) | 85 (40) |
LARC, long-acting reversible contraception; LNG, levonorgestrel; IUD, intrauterine device; ETN, etonogestrel.
Eighty-five LNG IUD partial expulsions, fifty Copper IUD partial expulsions, one ETN implant expulsion, and three broken implants were excluded (Fig. 1).
Other reasons included abnormal discharge, acne, allergic reaction, anemia, back pain, breast cancer, burning sensation, cavernous sinus thrombosis, dizziness, doesn’t want a contraceptive method, owing to program ending, fatigue, fear of breast cancer, hair loss, increased blood pressure, itching, leg pain, menopause symptoms, nausea, not sexually active, other medical reason, ovarian cyst, partner feels strings, partner got a vasectomy, patient desires sterilization, patient diagnosed with lupus, patient feels strings, patient removed IUD accidentally, physician notes illegible/unclear, physician recommendation, pregnant, religious reasons, skin infection, skin rash, thinking about other options, unspecified side effects, urinary tract infection, uterine fibroids, vaginal dryness, weight loss.
DISCUSSION
The Zika Contraception Access Network program served more than 29,000 women in a 17-month period by prioritizing increased access to contraception as a primary strategy to reduce Zika virus–related adverse pregnancy and birth outcomes. There was high LARC uptake in a largely LARC naïve system and low LARC discontinuation over the lifetime of the program, demonstrating that when barriers to contraception are minimized and a client-centered contraception counseling model is prioritized, women will often choose a most effective reversible method of contraception. The Zika Contraception Access Network also demonstrated that it is feasible to rapidly develop and implement a contraception access program in the setting of a public health emergency. The Zika response in Puerto Rico, through the Zika Contraception Access Network program, not only increased, but equalized access to contraception for all women and families who chose to prevent pregnancy in the context of Zika virus by reducing identified contraception access barriers such as cost, availability of providers and methods, and expanded service sites across all five public health regions of the island in partnership with diverse health facilities.
Seventy percent of Zika Contraception Access Network program participants chose a LARC method. This contrasts sharply with the 4% of women who used a most effective method (LARC or male sterilization) before the Zika Contraception Access Network program. The LARC uptake seen in the Zika Contraception Access Network program is consistent with other demonstration projects with a similar focus on decreasing common barriers to contraception.19,20 Studies describing other contraception access programs in complex public health emergency settings are limited,12 but it is reasonable to consider that the presence of a devastating birth defect may have influenced women’s choice to elect a most effective method of contraception during the period of the Zika virus outbreak. Only 4% of LARC users presented for a removal; however, data on the rate of LARC removal are limited postprogram, and data collection and analysis from the Zika Contraception Access Network patient follow-up at 6-, 24-, and 36- months are underway. Of women who received a LARC removal from a Zika Contraception Access Network provider, the most common reasons for removal were irregular bleeding and pelvic pain in implant and IUD users, respectively, which are similar to reasons for removal seen in other studies.19 The Contraceptive CHOICE project, which had an overall 75% LARC uptake, reported 7% discontinuation within the first 6 months of use and 13% at 12 months.21,22 Women who participated in the Zika Contraception Access Network reported high satisfaction with Zika Contraception Access Network services and receipt of the method they were most interested in,1 both of which influence continuation overall.23 The vast majority of women who accessed Zika Contraception Access Network services did not want to be pregnant for at least a year and that, coupled with fear of the birth defects associated with Zika virus could have influenced the desire to continue. It is also possible that women who chose to discontinue a LARC method experienced difficulty accessing removal services, although this is unlikely during the Zika Contraception Access Network program period.
Women with a college degree were more likely, and those who were breastfeeding or who had used a LARC previously were less likely to have their device removed during the program period, but none of the other characteristics examined were associated with removal. Prior studies have found lower rather than higher patient education levels to be associated with LARC discontinuation in unadjusted models.21,24 Our finding that women with higher education were more likely to have their device removed may be because college educated women in Puerto Rico may have better access to ongoing reproductive health services and may also have more financial resources to support a pregnancy. No other studies reported on breastfeeding or prior contraceptive use as characteristics associated with LARC discontinuation. As pregnancy desire is a reported reason for discontinuing contraception, including LARC methods,25,26 postpartum women breastfeeding may be highly motivated to avoid another pregnancy thus less likely to remove their device. Similarly, it is not surprising that women with prior experience using LARC, thus greater awareness of what use entails including potential side effects, would be less likely to discontinue their device. There are limited data on characteristics of LARC discontinuation overall and on barriers and strategies to ensure access to LARC removal, including in the setting of complex emergencies. More research is needed to better understand factors related to LARC discontinuation and barriers to LARC removal. As LARCs become a standard part of family planning programs in humanitarian crisis, early stages and protracted crisis settings,27 strategies and safeguards to prevent reproductive coercion and promote reproductive autonomy that are incorporated into program design are critical to meet the reproductive needs of women.
Consistent with the principles of shared decision-making and contraceptive method choice, the Zika Contraception Access Network program trained participating network physicians in client-centered counseling and procured the full range of reversible methods before implementing services as an ethical commitment and key principles of the program.1 In addition to ensuring access to full range of methods, the Zika Contraception Access Network included a removal-inclusive component that incorporated several strategies to ensure access to no cost removal (up to 10 years) after the Zika Contraception Access Network program ended. Understanding that without access to LARC removal after the program ended, women’s reproductive autonomy to control the discontinuation of their contraceptive method could be challenging given the identified access barriers before the Zika Contraception Access Network program. To mitigate the potential risk of limited access to LARC removals, the Zika Contraception Access Network developed a safety net to ensure LARC removal after the program ended. The safety net included a bundled LARC insertion and removal reimbursement at the time of insertion to cover future removal costs by that provider and communications channels to assist women to find a Zika Contraception Access Network physician or clinic for removal. The Zika Contraception Access Network program also developed formal agreements with select Zika Contraception Access Network champion providers for consultation and services for any complicated LARC removals and, if necessary, to provide routine removals.7 Furthermore, part of the Zika Contraception Access Network monitoring and evaluation plan includes following a cohort of participants for 3 years, in part to assess desire for and access to LARC removal after the program, and what barriers women encountered. As part of this evaluation, the Zika Contraception Access Network patient follow-up survey at 24- and 36- months includes a pop-up notice that survey participants can click on to alert the Zika Contraception Access Network program if they have had or are having issues with LARC removal (eg, identifying a Zika Contraception Access Network physician to remove LARC, Zika Contraception Access Network physician charging for LARC removal). This allows Zika Contraception Access Network program staff to assist women in real time, clarify what the effect of the Zika Contraception Access Network was years after the program, determine whether or not the safety net was successful, and highlight lessons that can be garnered from these experiences and shared with Puerto Rico agencies and partners as they continue to build sustainable contraceptive services.
The Zika Contraception Access Network program has several strengths. The Puerto Rico Zika virus outbreak response is a Zika virus epidemic response that robustly incorporates contraception as a medical countermeasure to reduce unintended pregnancy among women who chose to delay pregnancy to mitigate the adverse risks of the Zika virus. Moreover, the Zika Contraception Access Network incorporated a removal-inclusive component and developed a safety net for up to 10 years after the program ended to ensure that participants who selected a LARC method had access to no-cost removal even after the program ended. Furthermore, strengths of the analysis included that we were able to ascertain information on contraceptive method mix before the program to allow us to compare it with contraceptive method mix as part of the Zika Contraception Access Network. Additionally, Zika Contraception Access Network program staff worked with participating Zika Contraception Access Network physicians to ensure complete and timely submission of data, which resulted in limited missing data for most variables. This allowed the Zika Contraception Access Network program to have mostly complete data for nearly all women served. The Zika Contraception Access Network program also had several limitations. The LARC removals in this report were those recorded during implementation of the program and are from program data collected by Zika Contraception Access Network providers; this may not reflect all the removals during the program by non– Zika Contraception Access Network providers, nor does it reflect removals after the program ended, although longer term follow up is underway.
The Zika Contraception Access Network program incorporated several innovative and longer-term components meant to mitigate the potential risks of a brief contraception access program with anticipated high LARC uptake. The removal-inclusive strategies, including development of champion providers and implementation of a 10-year safety net for women to seek help with removals, if needed, or address other issues related to the program, require continuous communication with Zika Contraception Access Network providers and intermittent social media communications to reach participants, all to support women who were a part of the Zika Contraception Access Network. These efforts will ideally continue to drive provider interest in continuing to provide high-quality contraceptive services and support women’s demand for these services as Puerto Rico aims to implement sustainable contraception programs. The Zika Contraception Access Network program is a model program that demonstrated that contraception can be part of a rapid response to a public health emergency, and that similar programs can be put rapidly into place with fidelity and brought to scale while maintaining high-quality care.
Fig. 1.
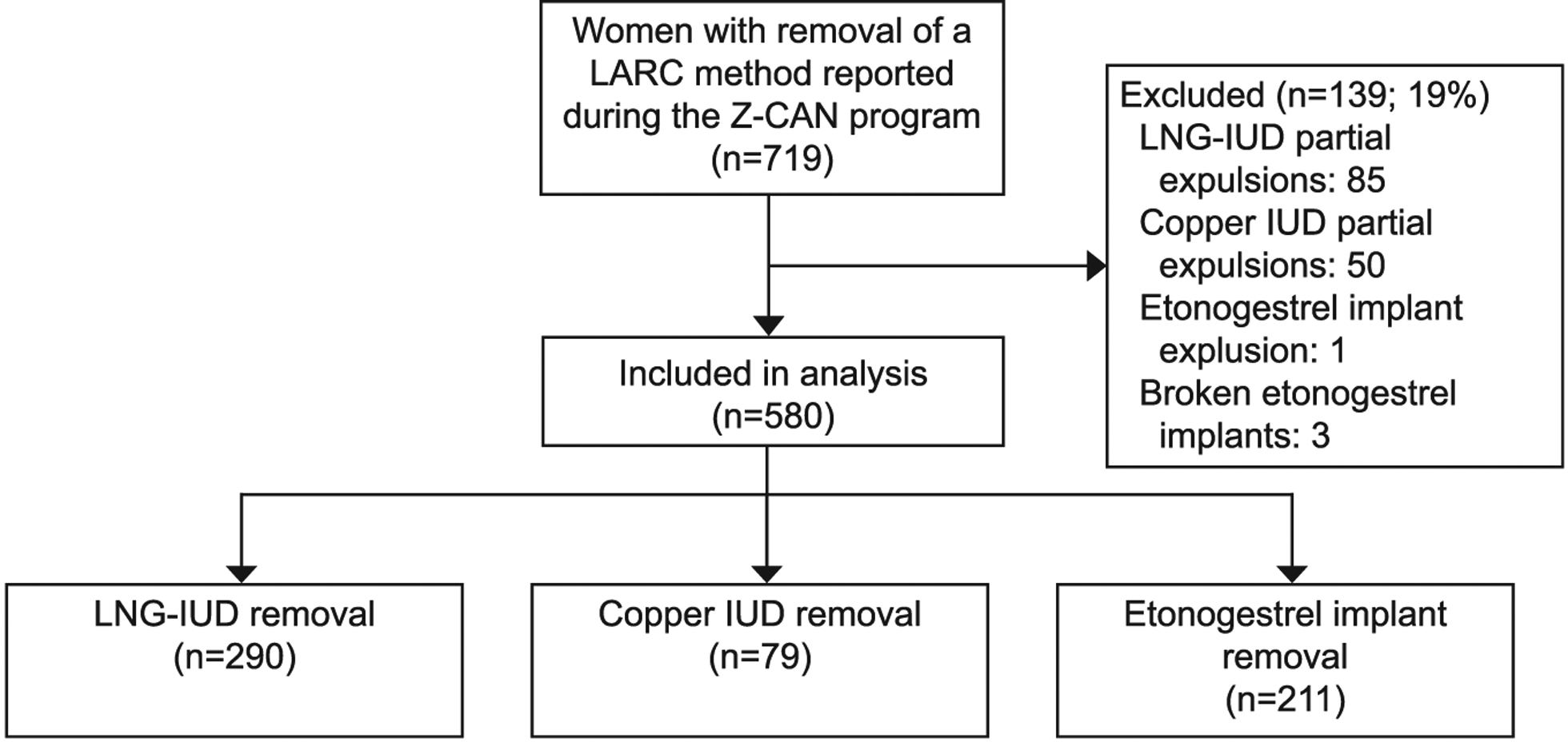
Flow chart of exclusions. LARC, long-acting reversible contraception; Z-CAN, Zika Contraception Access Network; LNG-IUD, levonorgestrel-releasing intrauterine device.
Lathrop. Factors Associated With LARC Removal. Obstet Gynecol 2020.
Acknowledgments
This project was funded by the National Foundation for the Centers for Disease Control and Prevention, Inc. (CDC Foundation). Funding for the Z-CAN program via the CDC Foundation was made possible by the Bill & Melinda Gates Foundation, Bloomberg Philanthropies, the William and Flora Hewlett Foundation, the Pfizer Foundation, and the American College of Obstetricians and Gynecologists. The CDC Foundation also secured large-scale donations, offers of contraceptive products, support tools, and services from Bayer, Allergan, Medicines360, Americares and Janssen Pharmaceuticals, Inc., Merck & Co., Inc., Mylan, the Pfizer Foundation, Teva Pharmaceuticals, Church & Dwight Co., Inc., RB, Power to Decide (formerly The National Campaign to Prevent Teen and Unplanned Pregnancy), Upstream USA, and Market Vision, Culture Inspired Marketing. Power to Decide allowed us to use some of their educational materials, Upstream conducted the first provider training, and Market Vision developed the Z-CAN communications campaign. None of these organizations were involved in the actual study design, data collection or analysis, or writing the paper.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention. In addition, the views and conclusions in this document are those of the authors and should not be interpreted as representing the opinions or policies of the CDC Foundation.
The authors thank Carla Agosto, Juan L. Cantres, Jeamy Rodriguez Cross, Megan T. Frey, Martha Canellas Garcia, Luz Marilyn Colon Lopez, Brian D. Montalvo Martinez, Charity Ntansah, Elvin Class Rodriguez, Madelyn Rodriguez, Stephanie Rivera, and Yari Vale, who were on the team of many who made the program work, and Margaret A. Honein and Judith Monroe for providing high-level support of the concept of Z-CAN.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has confirmed compliance with the journal’s requirements for authorship.
REFERENCES
- 1.Lathrop E, Romero L, Hurst S, Bracero N, Zapata LB, Frey MT, et al. The Zika Contraception Access Network: a feasibility programme to increase access to contraception in Puerto Rico during the 2016–17 Zika virus outbreak. The Lancet Public Health 2018;3:e91–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lozier M, Adams L, Flores Febo M, Torres-Aponte J, Bello-Pagan M, Ryff KR, et al. Incidence of Zika virus disease by age and sex—Puerto Rico, November 1, 2015–October 20, 2016. MMWR Morb Mortal Wkly Rep 2016;65:1219–23. [DOI] [PubMed] [Google Scholar]
- 3.Olson SM, Delaney A, Jones AM, Carr CP, Liberman RF, Forestieri NE, et al. Updated baseline prevalence of birth defects potentially related to Zika virus infection. Birth Defects Res 2019;111:938–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Zika virus: prevention and transmission. Available at: https://www.cdc.gov/zika/prevention/index.html. Retrieved September 20, 2019.
- 5.Tepper NK, Goldberg HI, Vargas Bernal MI, Rivera B, Frey MT, Malave C, et al. Estimating contraceptive needs and increasing access to contraception in response to the Zika virus disease outbreak—Puerto Rico, 2016. MMWR Morb Mortal Wkly Rep 2016:65:311–4. [DOI] [PubMed] [Google Scholar]
- 6.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. New Engl J Med 2016;374:843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romero L, Koonin LM, Zapata LB, Hurst S, Mendoza Z, Lathrop E. Contraception as a medical countermeasure to reduce adverse outcomes associated with Zika virus infection in Puerto Rico: the Zika contraception access network program. Am J Public Health 2018;108:S227–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curtis KM, Tepper NK, Jatlaoui TC, Berry-Bibee E, Horton LG, Zapata LB, et al. US medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep 2016;65:1–103. [DOI] [PubMed] [Google Scholar]
- 9.Curtis KM, Jatlaoui TC, Tepper NK, Zapata LB, Horton LG, Jamieson DJ, et al. US selected practice recommendations for contraceptive use, 2016. MMWR Recomm Rep 2016;65:1–66. [DOI] [PubMed] [Google Scholar]
- 10.Gubrium AC, Mann ES, Borrero S, Dehlendorf C, Fields J, Geronimus AT, et al. Realizing reproductive health equity needs more than long-acting reversible contraception (LARC). Am J Public Health 2016;106:18–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JA, Kramer RD, Ryder KM. Provider bias in long-acting reversible contraception (LARC) promotion and removal: perceptions of young adult women. Am J Public Health 2016;106:1932–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rattan J, Noznesky E, Curry DW, Galavotti C, Hwang S, Rodriguez M. Rapid contraceptive uptake and changing method mix with high use of long-acting reversible contraceptives in crisis-affected populations in Chad and the Democratic Republic of the Congo. Glob Health Sci Pract 2016;4:S5–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boring CC, Rochat RW, Becerra J. Sterilization regret among Puerto Rican women. Fertil Steril 1988;49:973–81. [PubMed] [Google Scholar]
- 14.Briggs L Discourses of forced sterilization in Puerto Rico: the problem with the speaking subaltern. Differences J Fem Cult Stud 1998;10:30–3. [Google Scholar]
- 15.The Puerto Rico pill trials. Available at: http://www.pbs.org/wgbh//amex/pill/peopleevents/e_puertorico.html. Retrieved September 1, 2019. [Google Scholar]
- 16.Briggs L Contraceptive programs: the risk of coercion. Womens Health J 1994:52–3. [Google Scholar]
- 17.Gomez AM, Fuentes L, Allina A. Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health 2014;46:171–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol 2010;203:115.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health 2014;46:125–32. [DOI] [PubMed] [Google Scholar]
- 21.Grunloh DS, Casner T, Secura GM, Peipert JF, Madden T. Characteristics associated with discontinuation of long-acting reversible contraception within the first 6 months of use. Obstet Gynecol 2013;122:1214–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McNicholas C, Madden T, Secura G, Peipert JF. The contraceptive CHOICE project round up: what we did and what we learned. Clin Obstet Gynecol 2014;57:635–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dehlendorf C, Henderson JT, Vittinghoff E, Grumbach K, Levy K, Schmittdiel J, et al. Association of the quality of interpersonal care during family planning counseling with contraceptive use. Am J Obstet Gynecol 2016;215:78.e1–9. [DOI] [PubMed] [Google Scholar]
- 24.Phillips SJ, Hofler LG, Modest AM, Harvey LF, Wu LH, Hacker MR. Continuation of copper and levonorgestrel intrauterine devices: a retrospective cohort study. Am J Obstet Gynecol 2017;217:57.e1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diedrich JT, Zhao Q, Madden T, Secura GM, Peipert JF. Three-year continuation of reversible contraception. Am J Obstet Gynecol 2015;213:662.e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simmons RG, Sanders JN, Geist C, Gawron L, Myers K, Turok DK. Predictors of contraceptive switching and discontinuation within the first 6 months of use among Highly Effective Reversible Contraceptive Initiative Salt Lake study participants. Am J Obstet Gynecol 2019;220:376.e1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization/UNFPA. UNHCR Inter-agency field manual on reproductive health in humanitarian settings. Geneva, Switzerland: WHO; 2010. [Google Scholar]


