Abstract
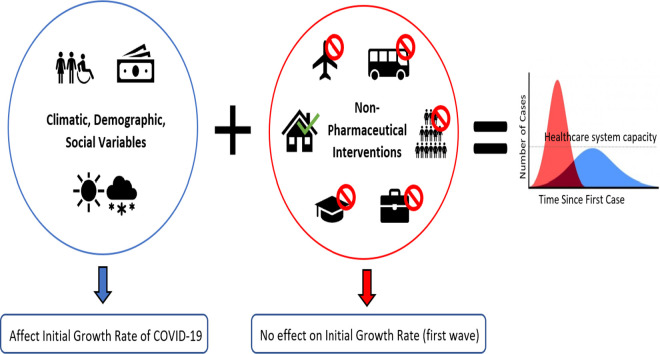
On March 11, 2020 the World Health Organization announced that the COVID-19 disease developed into a global pandemic. In the present paper, we aimed at analysing how the implementation of Non-Pharmaceutical Interventions (NPI) as well as climatic, social, and demographic variables affected the initial growth rate of COVID-19. In more detail, we aimed at identifying and assessing all the predictors in a whole picture of the COVID-19 outbreak and the effectiveness of the response of the countries to the pandemic. It can be expected, indeed, that there is a subtle and complex interplay among the various parameters. As such, we estimated the initial growth rate of COVID-19 for countries across the globe, and used a multiple linear regression model to study the association between the initial growth rate and NPI as well as pre-existing country characteristics (climatic, social and demographic variables measured before the current epidemic began). We obtained a mean initial growth rate of 0.120 (SD 0.076), in the range 0.023–0.315. Ten (8 pre-existing country characteristics and 2 NPI) out of 29 factors considered (21 pre-existing country characteristics and 8 NPI) were associated with the initial growth of COVID-19. Population in urban agglomerations of more than 1 million, PM2.5 air pollution mean annual exposure, life expectancy, hospital beds available, urban population, Global Health Security detection index and restrictions on international movement had the most significant effects on the initial growth of COVID-19. Based on available data and the results we obtained, NPI put in place by governments around the world alone may not have had a significant impact on the initial growth of COVID-19. Only restrictions on international movements had a relative significance with respect to the initial growth rate, whereas demographic, climatic, and social variables seemed to play a greater role in the initial growth rate of COVID-19.
Keywords: COVID-19, Epidemic growth rate, Non-pharmaceutical interventions, Climatic variables, Social variables, Demographic variables
Graphical abstract
1. Introduction
On December 31, 2019, the Wuhan Municipal Health Commission in mainland China reported a group of cases of pneumonia with unknown aetiology (later termed as Coronavirus Disease 2019, COVID-19) in Wuhan, Hubei Province (WHO, 2020). However, it has been hypothesized that the first human infections may have occurred earlier than December, in November 2019 or even before then (Andersen et al., 2020). This outbreak was likely to commence in a poultry and seafood market in a city with a population of 11 million people (IPAC, 2020). The earliest 59 suspected cases were admitted to Jinyintan Hospital which was designated to isolate and treat them. On January 23, 2020, authorities in China closed off the city. Planes, trains, buses, subways and ferry services were suspended (IPAC, 2020). The city of Huanggang, China, was also placed on lock-down. On January 24, 2020 travelling to 10 cities was restricted affecting 50 million people. Public transit and other modes of transportation were also suspended in neighbouring cities (IPAC, 2020).
The responsible infectious agent was identified in an emerging coronavirus, named as “Severe Acute Respiratory Syndrome Coronavirus Type 2” (SARS-CoV-2). Similar to SARS-CoV and MERS-CoV, with which it shares a common genetic basis, the emerging coronavirus has a zoonotic origin, with a human-to-human transmission (Tiwari et al., 2020). On January 30, 2020, the World Health Organization (WHO) announced a public health emergency of international concern (PHEIC) due to the novel coronavirus. This decision was made due to concern of further global spread after cases being confirmed in 4 other countries (Japan, Vietnam, Germany, and the United States) (WHO, 2020). From February 5 up to late March 2020, forty major airlines have cancelled or reduced flights to China. On February 19 and 21, 2020, coronavirus cases were reported in Italy and Iran, without a direct relation to China. Travel restrictions were imposed in South Korea and Iran as well (IPAC, 2020). On March 11, 2020 the WHO announced that the COVID-19 disease had developed into a global pandemic (WHO, 2020).
As of May 13, 2020, 188 countries were affected by the virus. In an effort to slow the spread of COVID-19 and flatten the epidemiological curve, given the absence of effective vaccines and drugs and the quickly contagious nature of the virus (Ferguson et al., 2020; Imai et al., 2020) many countries have responded by implementing non pharmaceutical interventions (NPI) which include: school and workplace closures, cancellation of public events and gatherings, stay-at-home orders, and international and domestic travel restriction. Even if single measures alone are not enough, a comprehensive package of interventions can result in a significant control of the disease (Nussbaumer-Streit et al., 2020; Sjödin et al., 2020). However, due to socio-economic and political factors, various countries have decided to enforce NPI in a less stringent and intensive way, in the effort to cause less economic damages and losses, choosing a mitigation strategy (which slows but not eliminates the spread of the virus) rather than a suppression one (aimed at eradicating the disease) (Ferguson et al., 2020; Imai et al., 2020).
Besides the various responses to the pandemic in terms of public health policies, differences in the outcome of flattening the curve could be explained taking into account an array of climatic, social and demographic parameters, including temperature, weather (Tosepu et al., 2020) and pollution (Copat et al., 2020; Riccò et al., 2020), country development, income and gross domestic product (Lippi et al., 2020; Mukherji, 2020), and population ageing (Petretto and Pili, 2020), among others. Concerning climatic factors, a positive association between COVID-19 cases and 14-day lagged temperature was found, whereas a negative association between COVID-19 cases and 14-day lagged wind speed could be detected. Furthermore, higher rates of COVID-19 cases were reported where absolute humidity was in the range 5–10 g/m3 (Islam et al., 2020a). Pollutants, such as PM2.5 and NO2 and to a lesser extent PM10, have been found to contribute to COVID-19 and mortality rate, as potential triggers (Copat et al., 2020). The COVID-19 induced death rate was reported to be positively associated with economic variables, such as the countries' gross domestic products (Lippi et al., 2020), income, and Gini's inequality index (Mukherji, 2020). Moreover, social and health parameters, including old age, male gender, ethnicity, comorbidities (diabetes, cancer and other chronic-degenerative disorders) have been found to correlate with COVID-19 fatality rate.
The growth rate of an infectious disease for a country is an important measure of how it spreads in the country and the time at which the peak value occurs. It is usually estimated by fitting the cumulative number of cases of the initial growth phase of the disease to exponential, logistic, Richard's and delayed logistic models (Chowell et al., 2003; Ma et al., 2014; Mills et al., 2004; Roberts and Heesterbeek, 2007; Nishiura et al., 2009). Since the number of cumulative cases for COVID-19, initially grows exponentially, but eventually slows and approaches a limit, the dynamics is qualitatively similar to that of a logistic curve. Thus, we estimate the growth rate of COVID-19 for the first ‘wave’ for each country by applying the logistic model and using the least-squares fitting method.
As previously mentioned, and briefly over-viewed, several studies have performed various analyses with the objective of identifying predictors of the outbreak and the effectiveness of the response of the different countries to the pandemic. However, to the best of our knowledge, no investigation has assessed all the variables in a whole picture, whereas it can be expected that there is a subtle and complex interplay among the various parameters. Moreover, it has not been done in a systematic way at the global level, utilizing a cross-country approach. As such, we aim at analysing how the implementation of NPI as well as climatic, social, and demographic variables affected the growth rate of COVID-19, to shed light on the covariates which may have a larger influence on the initial growth and should therefore be investigated further at both the global and national/sub-national scales. This work is not meant to be exhaustive or definitive, but rather to help reveal baseline epidemiological differences across countries, shape the direction of further research on COVID-19 and potential future outbreaks, and understand infectious disease transmission in general.
2. Material and methods
The data was collected on July 29, 2020 and used in a correlational study to determine the effects of government interventions as well as demographic, social, and climatic variables on the growth rate of COVID-19.
2.1. The growth rate of COVID-19
The growth rate of COVID-19 for the first ‘wave’ for each country was estimated by fitting the rate of change in cumulative cases of a logistic growth model to daily confirmed cases data obtained from Our World in Data Coronavirus (COVID-19) Cases dataset using the least-squares fitting method (https://ourworldindata.org/coronavirus-data). We chose a logistic model because mechanistic models (like compartmental ones, such as the Susceptible-Infectious-Recovered/Removed or SIR model and its variants) require a complex parametrization procedure, which is characterized by a high degree of uncertainty, especially during the early phases of a pandemic, due to the lack of detailed data. Phenomenological models, instead, being data-driven, do not suffer from such shortcomings. Moreover, among the four most commonly employed phenomenological models (namely, exponential, Richards, logistic and delayed logistic models), the logistic one tends to outperform (Ma et al., 2014). Logistic models have been utilized to model COVID-19 epidemic growth, using generalized equations to capture different growth curves in various countries (following an exponential growth in the Americas and in Australia, and a power law growth in most European countries) (Bertozzi et al., 2020; Pelinovsky et al., 2020). For instance, Wu and colleagues (Wu et al., 2020), employing different models (namely, the logistic growth model and its generalized variant, the generalized growth model and the generalized Richards model) showed the feasibility of utilizing the logistic model for COVID-19 predictive modelling purposes. The model is, indeed, able to provide reliable estimations of the upper and lower bounds of COVID-19 related scenarios. Moreover, in several studies logistic models represent a basic essential component for building more sophisticated models, based, for example, on machine learning and other artificial intelligence techniques (Pelinovsky et al., 2020; Zreiq et al., 2020).
More in detail, in the logistic model, the cumulative number of cases c(t) is assumed to satisfy the following equation:
where K is the epidemic size which c(t) approaches, r is the speed of the epidemic growth (the response variables). Solving this, we have that:
where c(0) is the initial number of cases. The change in cumulative cases that is fitted to the 7-day rolling mean of daily confirmed cases is given as I(t) = c(t + t) − c(t), where t is a small increment in time, which we choose to be one day. The change in cumulative cases is chosen instead of the cumulative number of cases because observations drawn from the same cumulative curve are correlated. From a mathematical perspective, cumulative and change in cumulative curves carry the same information, but from a statistical perspective, they do not. Most curve fitting algorithms (including least square fitting) assume that the errors in individual observations are statistically independent. This assumption is not true for cumulative curves, where each observation contains all of the cases from prior observations. We truncate all time series on the day with the highest daily count, because some countries have lingered near peak daily count for much longer than a logistic growth model would predict, which would pull the model peak later than the actual date of peak incidence and thereby underestimate r. We included all countries with at least a 6-day period of at least 30 daily cases as of April 23, 2020, after truncating at the peak. We eliminated countries whose logistic growth model R 2 was less than 0.94. Some countries do not report daily cases, may have variable reporting delays, and may have changed reporting methods resulting in dramatic spikes in cases for particular dates. To account for these inaccuracies, we used the 7-day rolling average (right aligned) for daily cases (https://ourworldindata.org/coronavirus-data). To estimate the growth rate, we used the scipy.optimize.curve_fit function in Python.
2.2. Non-pharmaceutical interventions
We consulted the Our World in data Policy Responses to the Coronavirus Pandemic datasets to extract the various NPI implemented, which include: school and workplace closures, cancellation of public events and gatherings, stay-at-home orders, and international and domestic travel restriction (https://ourworldindata.org/coronavirus-data). Each NPI is an indicator recorded on an ordinal scale where the larger the index, the stricter the policy. The mean of each NPI was taken from the date of the first known case to the date of maximum new cases for each country (although any country that has begun a second wave may have the NPI averaged from the first known case to a short time span after the maximum).
The NPI index can be found here https://github.com/OxCGRT/covid-policy-tracker/blob/master/documentation/codebook.md.
2.3. Climatic, social, and demographic variables
The data for the climatic, social, and demographic variables were extracted from the World Bank website (http://datatopics.worldbank.org/universal-health-coverage/coronavirus/). These are pre-existing country characteristics which can impact the growth phases of COVID-19, although not implying causation. We did not attempt to include all possibly relevant covariates because of high correlations even among a limited set, and because the limited number of countries dictate that a small subset should be preselected in order to retain sufficiently positive degrees of freedom for statistical analyses. For each predictor, we used the most recent available data, which ranged from 2000 to 2019. The climatic, social, and demographic factors used are presented in Table 2.
Table 2.
Climatic, social, and demographic factors.
| Variable type | Predictors |
|---|---|
| Demographic |
|
| Disease |
|
| Economic |
|
| Environmental |
|
| Habitat |
|
| Health |
|
| Social |
|
2.4. Statistical analysis
Data with highly skewed distributions were log-transformed and all distributions were centered and standardized. The covariates are standardized for effect comparisons. After compiling the variables, we model the relationship between the covariates and initial growth rate of COVID-19 using a multiple linear regression model. To achieve this, we use the lm() function in RStudio1.2.5033. The general formula of a multiple linear regression model is given as follows:
where, for i = 1 to n observations:
y i= response variable
β 0= constant term (y-intercept).
β j(j from 1 to p) = slope coefficients for each explanatory variable.
ε=the model's error term (also known as the residuals).
To ensure that our covariates provide unique or independent information in the regression model, we removed covariates with severe correlation with other covariates in the model. To this end, we calculate the variance inflation factor (VIF) of the covariates using the VIF() function in RStudio1.2.5033. This function takes as input a linear regression and calculates the variance inflation factor of the covariates. We sequentially eliminated covariates with the highest VIF from the model until the VIF of all covariates was less than 5. Following VIF analysis, we performed both forward and backward stepwise variable selection, using the function step in RStudio1.2.5033. For the range of models to examined in the stepwise search, we instruct the algorithm to consider all models from the constant model, to the model with all the covariates.
3. Results
3.1. Estimation of initial growth rate
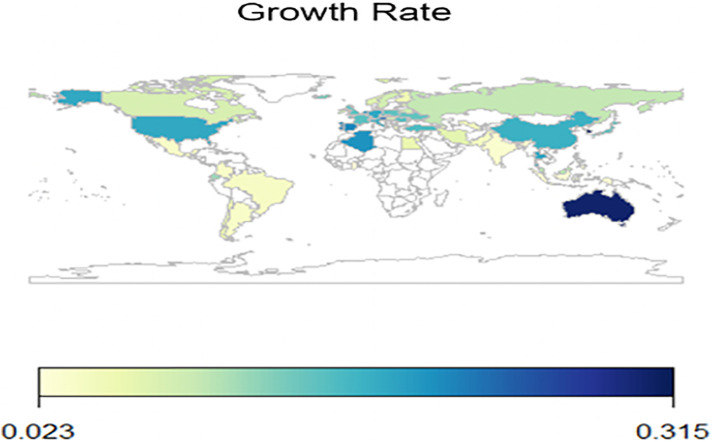
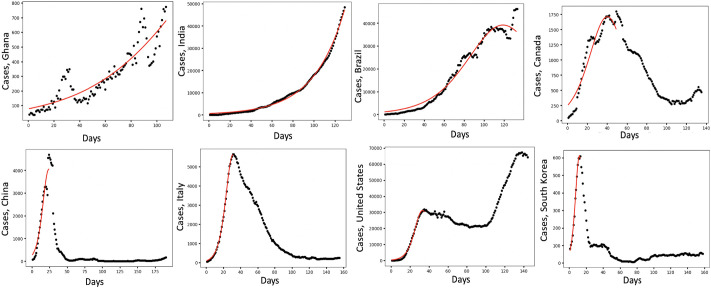
Fig. 1 shows a map of the initial growth of COVID-19 across countries. The plotted estimate at each time is based on a fitting window from time t = 0 until peak time. Fig. 2 pictorially illustrates the COVID-19 time-course dynamics in 8 countries, those with the lowest initial growth rate (first four) and those with the highest initial growth rate (last four). Figs. S1–S4 show growth curves fitted to the observed time series for daily confirmed cases for all the remaining countries considered. Only countries whose logistic growth model had an R 2 of greater 0.94 were considered. For the countries considered, the growth rate has maximum values in South Korea, Australia and Luxemburg, with 0.315, 0.302 and 0.275, respectively, and minimum values in Ghana, Indonesia, and Panama with 0.023, 0.028, 0.030, respectively. The mean initial growth rate is 0.120 with a standard deviation of 0.076. Ecuador (0.117), Belgium (0.134) and Iceland (0.136) initial growth rate are closest to the mean initial growth rate of COVID-19.
Fig. 1.
Estimated initial growth rate of COVID-19 across the globe. White countries are not included in our analysis.
Fig. 2.
The time course dynamics of COVID-19 in countries with the lowest initial growth rate (first four) and those with highest initial growth rate (last four). Countries are arranged from top left to bottom right in order of increasing initial growth rate. The black dots represent measured incidence data and the red line simulated data. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.2. Statistical analysis
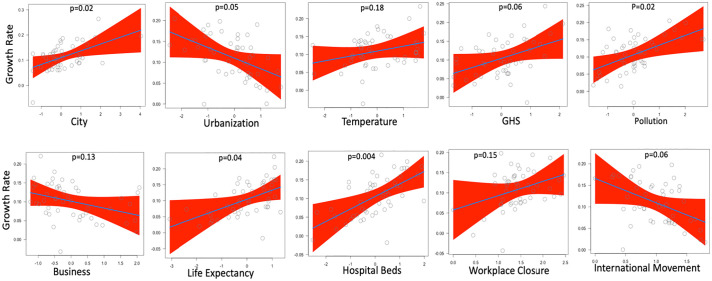
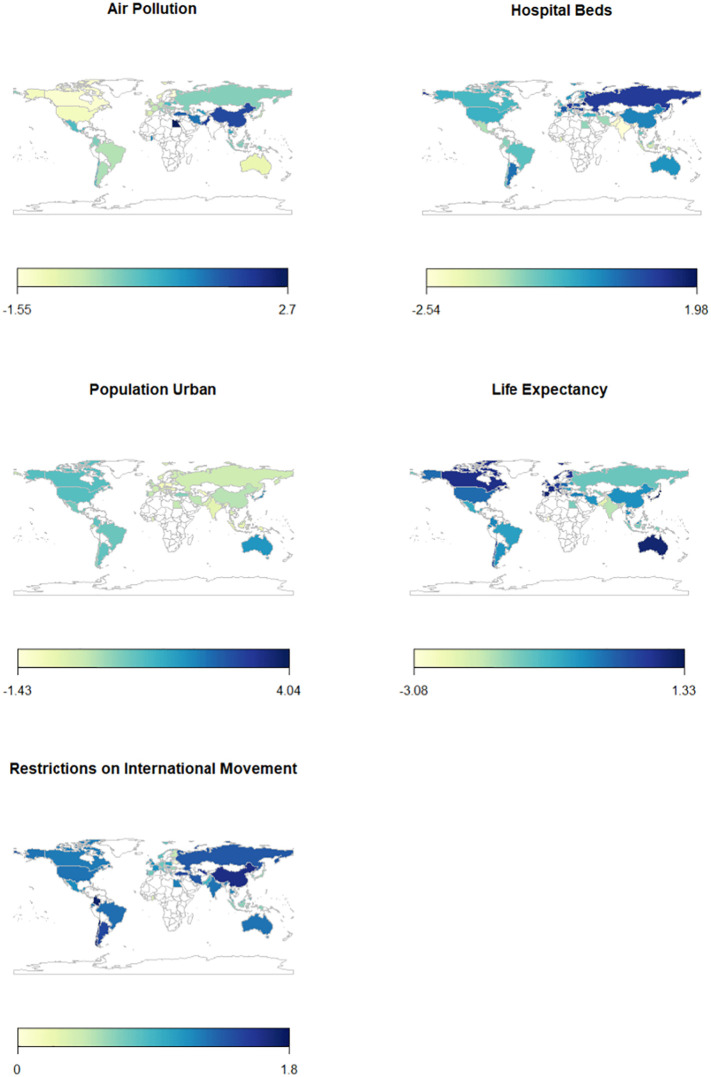
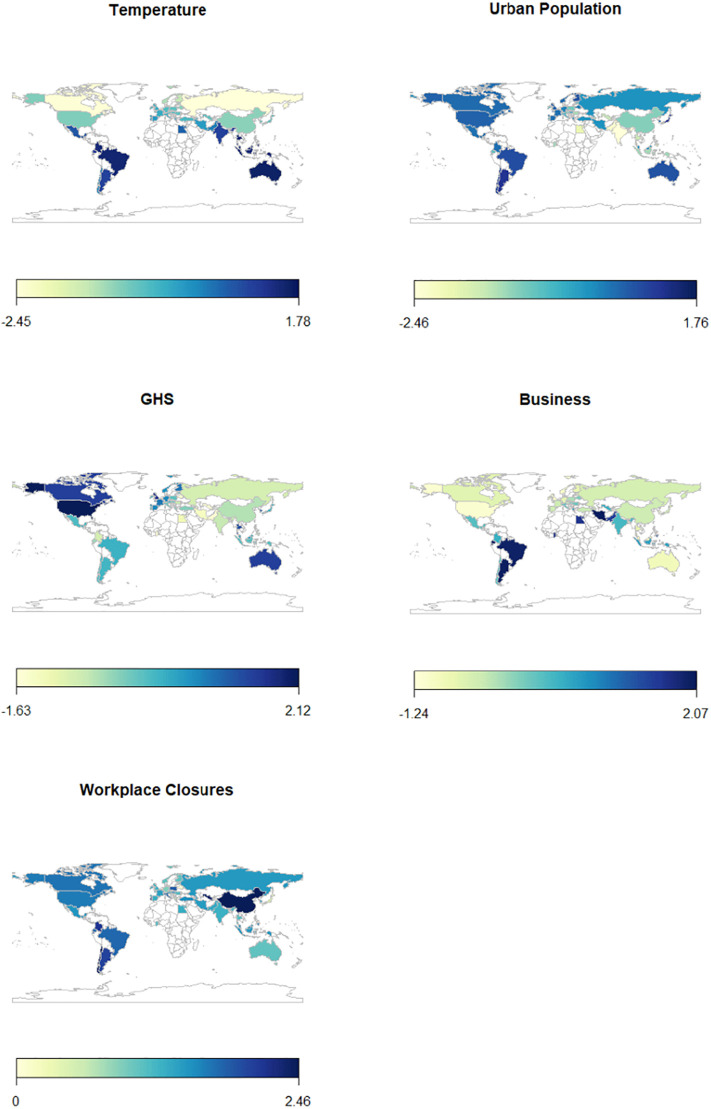
After performing VIF analysis and stepwise variable selection, the following covariates were removed: Air transport, Precipitation, Mortality rate from lower respiratory infections, Mortality rate from infectious and parasitic diseases, Nurses and midwives, Government Internet filtering in practice, Public transit closures, International travel controls, Public transit closures, Restrictions on gatherings, School closure, Stay-at-home requirements, Population total, Median age, Population aged 65 and older, GDP per capita, and Diabetes prevalence. Fitting the remaining covariates in Table 1, Table 2 to a multiple linear regression model, we obtained the results presented in Fig. 3 and Table 3 . The model has an overall P-value of 2.089e-06, a multiple R-squared value of 0.6633 and an adjusted R-squared value of 0.5734. These statistical values indicate that the model has a good explanatory power. The variables with positive correlation to growth rate are: Population in urban agglomerations of more than 1 million, Temperature, Global Health Security detection index, PM2.5 air pollution mean annual exposure, Life expectancy, Hospital beds available, and Workplace closures. Those with a negative correlation to growth rate are: Urban population, Ease of doing business index, and Restrictions on international movement. The most significant variables are Population in urban agglomerations of more than 1 million (p = 0.0235), PM2.5 air pollution mean annual exposure (p = 0.0155), Life expectancy (p = 0.0351), and Hospital beds available (p = 0.0038). Relative to other NPI in this model, Restrictions on international movements was the only significant variable with a p-value of p = 0.0617. Finally, Fig. 4, Fig. 5 show world heat maps of variables under study with a strong significant and moderate significant relationship to the initial growth rate of COVID-19, respectively.
Table 1.
Descriptions and/or index explanations of each NPI.
| NPI | Scale | Description |
|---|---|---|
| School closures | 0 | No measures taken |
| 1 | Recommended closing (not enforced) | |
| 2 | Required closing of only certain levels (e.g. public schools, high schools…) | |
| 3 | Required closing of all levels | |
| Workplace closures | 0 | No measures taken |
| 1 | Recommended closing and/or work from home (not enforced) | |
| 2 | Required closing and/or work from home only for certain sectors or categories of workers | |
| 3 | Required closing and/or work from home for all but for essential workplaces (grocery…) | |
| Cancellation of public events (public events) | 0 | No measures taken |
| 1 | Recommended cancelling (but not enforced) | |
| 2 | Required cancelling public events | |
| Restrictions on gatherings (gatherings) | 0 | No restrictions |
| 1 | Restrictions on very large gatherings of over 1000 people | |
| 2 | Restrictions on gatherings between 101 and 1000 people | |
| 3 | Restrictions on gatherings between 11 and 100 people | |
| 4 | Restrictions on gatherings of 10 people or less | |
| Public transit closures (public transit) | 0 | No measures taken |
| 1 | Recommended closing or significantly reducing volume/route/means of transportation that are available | |
| 2 | Required closing | |
| Stay-at-home requirements (stay-at-home) | 0 | No measures taken |
| 1 | Recommended not leaving the house (but not enforced) | |
| 2 | Required not leaving the house with exception of essential trips (grocery.) or daily exercise | |
| 3 | Required not leaving the house with very little exception (ex: one person leaves at a time, once per week…) | |
| Restrictions on International movement (restriction of movement between cities/countries) (International Movement) | 0 | No measures taken |
| 1 | Recommended not to travel between regions/cities (but not enforced) | |
| 2 | Restriction of internal movement | |
| International travel controls (restrictions on international travel (foreign travellers, not citizens) (Ban on Foreigners) | 0 | No restrictions |
| 1 | Screening at arrivals | |
| 2 | Quarantine arrivals for some or all regions | |
| 3 | Ban arrivals from some regions. | |
| 4 | Total border closure or ban on all regions |
Fig. 3.
The association between the initial growth rate of COVID-19 and the covariates selected using stepwise variable section and VIF.
Table 3.
Summary of the multiple regression analysis results.
| Estimate | Std. error | t-value | p-value | |
|---|---|---|---|---|
| Intercept | 0.115906 | 0.023965 | 4.836 | 2.21e-05 |
| City | 0.026936 | 0.011409 | 2.361 | 0.0235 |
| Urbanization | 0.025540 | 0.012826 | −1.991 | 0.0537 |
| Temperature | 0.013683 | 0.009923 | 1.379 | 0.1760 |
| GHS | 0.024504 | 0.012827 | 1.910 | 0.0637 |
| Pollution | 0.028141 | 0.011109 | 2.533 | 0.0155 |
| Business | 0.018335 | 0.11787 | −1.556 | 0.1281 |
| Life expectancy | 0.028414 | 0.012999 | 2.186 | 0.0351 |
| Hospital beds | 0.033400 | 0.010831 | 3.084 | 0.0038 |
| Workplace closure | 0.035366 | 0.023912 | 1.479 | 0.1474 |
| International movement | 0.056492 | 0.029346 | −1.925 | 0.0617 |
Fig. 4.
World heat maps of variables under study with a significant relationship to the initial growth rate of COVID-19.
Fig. 5.
World heat maps of variables with a non significant relationship to the initial growth rate of COVID-19.
4. Discussion
The NPI put in place by governments alone do not seem to explain the growth rate of COVID-19. Based on the available data, our results show that growth rate is mostly explained by demographic, climatic, and social variables. This can be due to the fact that the measures were put in place after the growth rate has begun. The most significant variables were Population in urban agglomerations, Air pollution, Life expectancy, and Hospital beds. Compared to other NPI in this model, Restrictions on international movement were borderline significant.
The Population in urban agglomeration of more that 1 million has a positive correlation and a significant effect on the growth rate of COVID-19. This is true particularly for territories in the Americas and in Australia (Fig. 4, Fig. 5). According to the CDC COVID-19 Response Team, COVID-19 is transmitted primarily by respiratory droplets, so population density might play a significant role in transmission (CDC COVID Response Team, 2020). Keeping a safe distance from other people can pose a challenge with higher population densities and it has been shown that contact rate is proportional to population density (Rocklöv and Sjödin, 2020). This finding is in line with some studies which found a moderate association between population density and COVID-19 spread in a number of countries including India (Bhadra et al., 2020), and Algeria (Kadi and Khelfaoui, 2020) or utilizing mathematical modelling (Rader et al., 2020). However, other studies could not replicate such results, finding, on the contrary, an inverse (Hamidi et al., 2020) or no association (Carozzi et al., 2020).
Air pollution also has a positive correlation and a significant effect on growth rate. Air pollution is a catalyst in the transmission of COVID-19. PM can act as a carrier of virus particles and spread the virus over 2 m of distance (Sharma and Balyan, 2020). Some areas characterized by high levels of air pollutions, such as India, China, Italy, Russia, Chile and Qatar (Fig. 4, Fig. 5), have, indeed, reported higher rates of COVID-19 cases, especially severe ones, with respect to territories with less pollution (Paital and Agrawal, 2020). On the other hand, evidence for previous coronavirus outbreaks is highly conflicting with some studies, such as an important cluster randomized controlled trial (Carrión et al., 2019) failing to find any correlation between household pollution and infant viral carriage.
Life expectancy has a positive correlation and has a significant effect on the growth rate of COVID-19. This can be explained by comparing high-income vs. low-income countries. Although high-income countries have a longer life expectancy, this means that there is an ageing population with many more people that are 70 years old or greater (Schellekens and Sourrouille, 2020). It has been shown that elderly people have a higher infection and death rate (Chen et al., 2020) while younger people have shown milder symptoms and even asymptomatic infection (Velavan and Meyer, 2020). A recently published meta-analysis that has pooled together more than half million of COVID-19 cases from different countries (China, Italy, Spain, UK, and New York State, USA) has shown the impact of age on mortality, identifying the threshold of age greater than 50 years and, in particular, greater than 60 years. This is parallel to our results that show a positive correlation between life expectancy and growth rate of COVID-19, especially in North America, Europe, China and Australia (Fig. 4, Fig. 5). On the other hand, the spread of the virus is expected to have a negative effect on life expectancy, inverting the secular increasing trend (Marois et al., 2020).
The number of hospital beds available has a significant effect on the growth rate of COVID-19 and was also found to be positively correlated. On the one hand, one could expect that countries with higher numbers of beds per hospital may have experienced less pressure and strain, with less need to implement drastic and stringent measures. On the other hand, it has been shown that exceeding the number of hospital beds and other health care capacities available can increase the spread of COVID-19. This may also lead to a decrease in quality of care which leads to inadequate access to ventilators and increase the case-fatality ratio (Li et al., 2020). Our analysis shows a particularly strong correlation in areas such as North America, China, Russia and Australia (Fig. 4, Fig. 5). This is in line with a study (Karaca-Mandic et al., 2020) conducted in the USA that shows that an increase in non-intensive care unit (ICU) bed use was associated with more COVID-19 deaths.
Among the NPI implemented by governmental authorities, only Restrictions on international movements were found to be borderline significant. This is in line with a study, that has shown that these restrictions likely have an effect on the containment of the epidemic in Wuhan China in the early stages of COVID-19 (Tian et al., 2020).
All the other variables selected in the final model (namely, temperature, GHS, workplace closures, urban population, and business closure) may not have a strong significant impact on the initial growth rate of COVID-19 (Fig. 5).
In our study, temperature has a positive but not a very significant correlation with the initial growth rate. This finding is in partial contrast with the available literature that shows, for instance, that normal and maximum temperature are positively and significantly correlated with the number of COVID-19 cases (Menebo, 2020). Moreover, temperature, in particular, warm and wet climates could counteract, or at least mitigate, the spread of COVID-19 transmission, even though this variable alone could explain only a little portion of the variability in the viral spread and the level of evidence was deemed to be low (Mecenas et al., 2020).
Concerning the GHS, in our investigation, this index has a positive correlation to the initial growth rate and matches the fact the higher the GHS of a country, the more prepared it is to deal with an epidemic. At the global level, its average score is 40.2 out of 100, indicating the global preparedness to potential pandemics and outbreaks is weak. Even though there is a certain degree of variability in the index with high-income countries having an average value of 51.9, all countries should develop and implement more robust resilience and response plans.
Regarding the urban population, we have found that it has a negative correlation to the initial growth rate. Spatio-temporal modelling studies have shown that COVID-19 did not remain confined to gentrified settings but spread quickly from urban areas to rural ones (Paul et al., 2020). This could explain, at least partially, the lack of statistical significance of this variable.
Concerning NPI, our study shows that measures such as those concerning Businesses, or Workplace closure are not correlated to a significant control of the growth rate. These results are not in line with that found by Ferguson et al., showing that if school/workplace transmission accounts for an assumed 50–60% of transmission, then policies such as school closure should be quite effective (Ferguson et al., 2020). However, the existing scholarly literature reports also contrasting findings: for instance, social distancing has been found to mitigate the spread of COVID-19 (Islam et al., 2020b; Vokó and Pitter, 2020), whereas other scholars could not replicate such findings (Wagner et al., 2020). Such conflicting results may depend on different methods employed, time periods studied as well as on the sample of countries selected. Moreover, it should be emphasized that most of these studies are ecological studies, which are afflicted by the so-called ecological bias and do not correct or adjust for confounding variables, or are based on specific modelling assumptions.
In conclusion, there exist contrasting findings concerning the drivers and predictors of COVID-19 spread. The current study aimed at investigating all variables altogether at a global level, using a systematic and reproducible approach. However, despite these strengths, the present study suffers from a number of limitations that should be properly acknowledged. The major shortcoming is given by the assumption of a constant growth rate, whereas it has been widely acknowledged that the growth rate of COVID-19 changes over time, which could be affected by various epidemiological, social, economic, and NPI factors, resulting in a change of the growth rate over time for different countries. Future studies should replicate the present findings utilizing time-varying values of the growth rate.
5. Conclusion
Based on available data and the results obtained, NPI put in place by governments around the world alone may not explain the initial growth rate of COVID-19, whereas demographic, climatic, and social variables play a greater role in the initial growth rate of the virus, although restrictions on international movement relative to other NPI had a relative significance in terms of the growth rate.
CRediT authorship contribution statement
J.D.K. designed research; all authors conducted literature search and data collection; J.D.K. and J.D. analyzed data; and all authors wrote the paper.
Declaration of competing interest
The authors declare no competing financial interest.
Acknowledgments
Acknowledgement
J.D.K. acknowledges support from Canada's International Development Research Centre (IDRC) (Grant No. 109559-001), N.L.B. acknowledges support from the Canadian Institute of Health Research (CIHR) 2019 Novel Coronavirus (COVID-19) rapid research program and J.D. acknowledges support from the York University, Faculty of Science York Science Scholars Award.
Editor: Jay Gan
References
- Andersen K.G., Rambaut A., Lipkin W.I., Holmes E.C., Garry R.F. The proximal origin of SARS-Cov-2. Nat. Med. 2020;26(4):450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertozzi A.L., Franco E., Mohler G., Short M.B., Sledge D. The challenges of modeling and forecasting the spread of COVID-19. PNAS. 2020;117:16732–16738. doi: 10.1073/pnas.2006520117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhadra A., Mukherjee A., Sarkar K. Model. Earth Syst; Environ: 2020. Impact of Population Density on Covid-19 Infected and Mortality Rate in India. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carozzi F., Provenzano S., Roth S. IZA Discussion Papers 13440. Labor Economics (IZA); Institute of: 2020. Urban density and COVID-19. [Google Scholar]
- Carrión D., Kaali S., Kinney P.L., Owusu-Agyei S., Chillrud S., Yawson A.K., Quinn A., Wylie B., Ae-Ngibise K., Lee A.G., Tokarz R., Iddrisu L., Jack D.W., Asante K.P. Examining the relationship between household air pollution and infant microbial nasal carriage in a Ghanaian cohort. Environ Int. 2019;133(Pt A):105150. doi: 10.1016/j.envint.2019.105150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Li T., Ye Y., Chen Y., Pan J. Impact of fundamental diseases on patients with COVID-19. Disaster Medicine and Public Health Preparedness. 2020:1–6. doi: 10.1017/dmp.2020.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowell G., Fenimore P., Castillo-Garsow M., Castillo-Chavez C. SARS outbreaks in Ontario, Hong Kong and Singapore: the role of diagnosis and isolation as a control mechanism. J. Theor. Biol. 2003;224(1):1–8. doi: 10.1016/S0022-5193(03)00228-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copat C., Cristaldi A., Fiore M., Grasso A., Zuccarello P., Signorelli S.S., Conti G.O., Ferrante M. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review. Environ. Res. 2020;191:110129. doi: 10.1016/j.envres.2020.110129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson N.M., Laydon D., Nedjati-Gilani G., Imai N., Ainslie K., Baguelin M., Bhatia S., Boonyasiri A., Cucunubá Z., Cuomo-Dannenburg G., Dighe A., Origatti I., Fu H., Gaythorpe K., Green W., Hamlet A., Hinsley W., Okell L.C., Van Elsland S.…Verity R. 2020. Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. [Google Scholar]
- Hamidi S., Sabouri S., Ewing R. Does density aggravate the COVID-19 pandemic? J. Am. Plan. Assoc. 2020;86(4):495–509. [Google Scholar]
- Imai N., Gaythorpe K., Abbott S., Bhatia S., Van Elsland S., Prem K., Liu Y., Ferguson N.M. Adoption and impact of non-pharmaceutical interventions for COVID-19. Wellcome Open Research. 2020;5(59) doi: 10.12688/wellcomeopenres.15808.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IPAC . 2020. Coronavirus (COVID-19)https://ipac-canada.org/coronavirus-resources.php Retrieved from. [Google Scholar]
- Islam N., Bukhari Q., Jameel Y., Shabnam S., Erzurumluoglu A.M., Siddique M.A., Massaro J.M., D’Agostino R.B., Sr. COVID-19 and climatic factors: a global analysis. Environ. Res. 2020;110355 doi: 10.1016/j.envres.2020.110355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam N., Sharp S.J., Chowell G., Shabnam S., Kawachi I., Lacey B., Massaro J.M., D’Agostino R.B., White M. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. 2020:m2743. doi: 10.1136/bmj.m2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadi N., Khelfaoui M. Population density, a factor in the spread of COVID-19 in Algeria: statistic study. Bull Natl Res Cent. 2020;44(1):138. doi: 10.1186/s42269-020-00393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaca-Mandic P., Sen S., Georgiou A., Zhu Y., Basu A. Association of COVID-19-related hospital use and overall COVID-19 mortality in the USA. J. Gen. Intern. Med. 2020 doi: 10.1007/s11606-020-06084-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R., Rivers C., Tan Q., Murray M.B., Toner E., Lipsitch M. Estimated demand for US hospital inpatient and intensive care unit beds for patients with COVID-19 based on comparisons with Wuhan and Guangzhou, China. JAMA Netw. Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.8297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi G., Henry B.M., Mattiuzzi C., Bovo C. The death rate for COVID-19 is positively associated with gross domestic products: coronavirus and gross domestic product. Acta Bio Med. 2020;91(2):224–225. doi: 10.23750/abm.v91i2.9514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J., Dushoff J., Bolker B.M., Earn D.J. Estimating initial epidemic growth rates. Bull. Math. Biol. 2013;76(1):245–260. doi: 10.1007/s11538-013-9918-2. [DOI] [PubMed] [Google Scholar]
- Marois G., Muttarak R., Scherbov S. Assessing the potential impact of COVID-19 on life expectancy. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0238678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mecenas P., Bastos R.T.D.R.M., Vallinoto A.C.R., Normando D. Effects of temperature and humidity on the spread of COVID-19: a systematic review. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0238339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menebo M.M. Temperature and precipitation associate with COVID-19 new daily cases: a correlation study between weather and COVID-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020;737:139659. doi: 10.1016/j.scitotenv.2020.139659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills C.E., Robins J.M., Lipsitch M. Transmissibility of 1918 pandemicinfluenza. Nature. 2004;432(7019):904–906. doi: 10.1038/nature03063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherji N. 2020. The Social and Economic Factors Underlying the Incidence of COVID-19 Cases and Deaths in US Counties. (MedRxiv) [Google Scholar]
- Nishiura H., Castillo-Chavez C., Safan M., Chowell G. Transmission potential of the new influenza A(H1N1) virus and its age-specificity in Japan. Eurosurveillance. 2009;14(22) doi: 10.2807/ese.14.22.19227-en. [DOI] [PubMed] [Google Scholar]
- Nussbaumer-Streit B., Mayr V., Dobrescu A.I., Chapman A., Persad E., Klerings I., Wagner G., Siebert U., Ledinger D., Zachariah C., Gartlehner G. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst. Rev. 2020;4(4) doi: 10.1002/14651858.CD013574.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paital B., Agrawal P.K. Air pollution by NO2 and PM2.5 explains COVID-19 infection severity by overexpression of angiotensin-converting enzyme 2 in respiratory cells: a review. Environ Chem Lett. 2020 doi: 10.1007/s10311-020-01091-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul R., Arif A.A., Adeyemi O., Ghosh S., Han D. Progression of COVID-19 from urban to rural areas in the United States: a spatiotemporal analysis of prevalence rates. J. Rural. Health. 2020;36(4):591–601. doi: 10.1111/jrh.12486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelinovsky E., Kurkin A., Kurkina O., Kokoulina M., Epifanova A. Logistic equation and COVID-19. Chaos Solitons Fractals. 2020;140:110241. doi: 10.1016/j.chaos.2020.110241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petretto D.R., Pili R. Ageing and COVID-19: what is the role for elderly people? Geriatrics. 2020;5(2):25. doi: 10.3390/geriatrics5020025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rader B., Scarpino S.V., Nande A., Hill A.L., Adlam B., Reiner R.C. Crowding and the shape of COVID-19 epidemics. Nat. Med. 2020:1–6. doi: 10.1038/s41591-020-1104-0. [DOI] [PubMed] [Google Scholar]
- Riccò M., Ranzieri S., Balzarini F., Bragazzi N.L., Corradi M. SARS-Cov-2 infection and air pollutants: correlation or causation? Sci. Total Environ. 2020;734:139489. doi: 10.1016/j.scitotenv.2020.139489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts M.G., Heesterbeek J.A. Model-consistent estimation of the basic reproduction number from the incidence of an emerging infection. J. Math. Biol. 2007;55(5–6):803–816. doi: 10.1007/s00285-007-0112-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocklöv J., Sjödin H. High population densities catalyse the spread of COVID-19. Journal of Travel Medicine. 2020;27(3) doi: 10.1093/jtm/taaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schellekens P., Sourrouille D. 2020. COVID-19 Mortality in Rich and Poor Countries: A Tale of Two Pandemics? (Policy Research Working Papers) [Google Scholar]
- Sharma A.K., Balyan P. Indian J Public Health; 2020. Air Pollution and COVID-19: Is the Connect Worth its Weight? [DOI] [PubMed] [Google Scholar]
- Sjödin H., Wilder-Smith A., Osman S., Farooq Z., Rocklöv J. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. Eurosurveillance. 2020;25(13) doi: 10.2807/1560-7917.ES.2020.25.13.2000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H., Liu Y., Li Y., Wu C., Chen B., Kraemer M.U., Li B., Cai J., Xu B., Yang Q., Wang B., Yang P., Cui Y., Song Y., Zheng P., Wang Q., Bjornstad O.N., Yang R., Grenfell B.…Dye C. Science; 2020. The impact of transmission control measures during the first 50 days of the COVID-19 epidemic in China. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari R., Dhama K., Sharun K., Iqbal Yatoo M., Malik Y.S., Singh R., Michalak I., Sah R., Bonilla-Aldana D.K., Rodriguez-Morales A.J. COVID-19: animals, veterinary and zoonotic links. Vet. Q. 2020;40(1):169–182. doi: 10.1080/01652176.2020.1766725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Ahmad L.O., Lestari H., Bahar H., Asfian P. Correlation between weather and COVID-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020;725:138436. doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velavan T.P., Meyer C.G. The COVID-19 epidemic. Tropical Med. Int. Health. 2020;25(3):278–280. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vokó Z., Pitter J.G. The effect of social distance measures on COVID-19 epidemics in Europe: an interrupted time series analysis. GeroScience. 2020;42(4):1075–1082. doi: 10.1007/s11357-020-00205-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner A.B., Hill E.L., Ryan S.E., Sun Z., Deng G., Bhadane S., Martinez V.H., Wu P., Li D., Anand A., Acharya J., Matteson D.S. 2020. Social Distancing has Merely Stabilized COVID-19 in the US. Stat (International Statistical Institute) p. e302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. WHO timeline - COVID-19.https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19 Retrieved from. [Google Scholar]
- Wu K., Darcet D., Wang Q., Sornette D. Generalized logistic growth modeling of the COVID-19 outbreak: comparing the dynamics in the 29 provinces in China and in the rest of the world. Nonlinear Dyn. 2020;101:1561–1581. doi: 10.1007/s11071-020-05862-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zreiq R., Kamel S., Boubaker S., Al-Shammary A.A., Algahtani F.D., Alshammari F. Generalized Richards model for predicting COVID-19 dynamics in Saudi Arabia based on particle swarm optimization algorithm. AIMS Public Health. 2020;7(4):828–843. doi: 10.3934/publichealth.2020064. [DOI] [PMC free article] [PubMed] [Google Scholar]