Abstract
Objective
To describe telemedicine utilization in neurosurgery at a single tertiary institution to provide outpatient care during the coronavirus disease 2019 (COVID-19) pandemic, with 315 telemedicine visits performed by the neurosurgery department.
Patients and Methods
In response to the COVID-19 pandemic national stay-at-home orders and postponed elective surgeries, we converted upcoming clinic visits into telemedicine visits and rescheduled other patients thought not to be markedly affected by surgical postponement. We reviewed the charts of all patients who had telehealth visits from April 1 through April 30, 2020, and collected demographic information, diagnosis, type of visit, and whether they received surgery; a satisfaction questionnaire was also administered.
Results
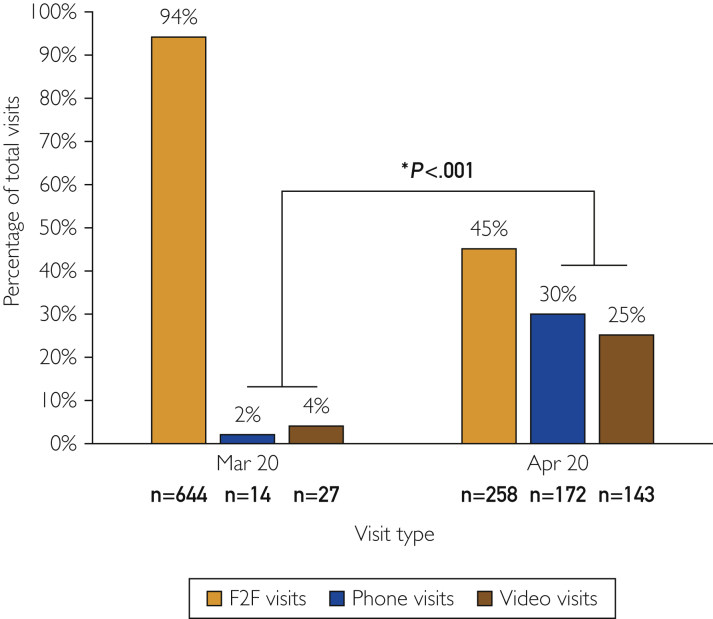
In March 2020, 94% (644 of 685) of the neurosurgery clinic visits were face-to-face, whereas in April 2020, 55% (315 of 573) of the visits were telemedicine (P<.001). In April, of the 315 telemedicine visits, 172 (55%) were phone consults and 143 (45%) video consults; 101 (32%) were new consults, 195 (62%) return visits, and 18 (6%) postoperative follow-up. New consults were more likely to be video with audio than return visits and postoperative follow-up (P<.001). Only 39 patients (12%) required surgery. Ninety-one percent of the questionnaire respondents were very likely to recommend telemedicine.
Conclusion
Rapid implementation of telemedicine to evaluate neurosurgery patients became an effective tool for preoperative consultation, postoperative and follow-up visits during the COVID-19 pandemic, and decreased risks of exposure to severe acute respiratory syndrome coronavirus 2 to patients and health care staff. Future larger studies should investigate the cost-effectiveness of telemedicine used to triage surgical from nonsurgical patients, potential cost-savings from reducing travel burdens and lost work time, improved access, reduced wait times, and impact on patient satisfaction.
Abbreviations and Acronyms: CD, compact disc; CMS, Centers for Medicare & Medicaid Services; COVID-19, coronavirus disease 2019; EMR, electronic medical record; HIPPA, Health Insurance Portability and Accountability Act; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
The novel coronavirus (severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]) pandemic significantly affected routine neurosurgery patient care flow and health care systems around the globe.1,2 As the number of coronavirus disease 2019 (COVID-19) cases was increasing, on March 13, 2020, the American College of Surgeons with the Surgeon General and Centers for Medicare & Medicaid Services (CMS) recommended to postpone elective surgeries.3, 4, 5 Hospitals implemented several measures to prevent the spread of the virus, such as temperature checks for patients and employees as well as no-visitor policies. To continue to provide quality care while minimizing the risk of exposure to SARS-CoV-2 and cross-infecting patients and health care workers and reduce the use of needed personal protective equipment, telemedicine emerged quickly as a tool to balance the need to triage patients who needed urgent neurosurgery from those whose surgeries could be postponed and reevaluate those patients shortly thereafter as the pandemic evolved.6
Telemedicine was defined by the World Health Organization7 as follows:
The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
Telemedicine was first introduced in the late 19th century when telephone calls were used to reduce superfluous office visits.8 Since then, the spread of high-speed broadband and cellular connectivity, combined with high-resolution video capability from laptops and smartphones, has facilitated high-resolution, low-latency audiovisual consultations. In neurosurgery, telemedicine has mainly been used for teleconsults in neurological emergencies such as triaging traumatic brain injury and in telestroke for weighing risks and benefits of local thrombolytic therapy administration.9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19
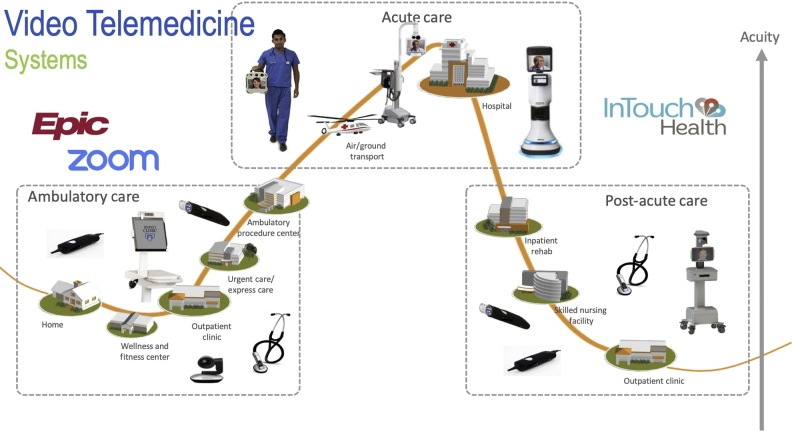
During the COVID-19 pandemic, neurosurgical practices were negatively affected by the government mandates to cease elective surgeries combined with national stay-at-home orders, resulting in a considerable drop in outpatient visits. To minimize the deterioration of patients without COVID-19; to assess and triage new patients in need of semi-urgent, urgent, or more emergent surgery; to maintain follow-ups; and to minimize the risk of exposure to SARS-CoV-2, our neurosurgery department rapidly implemented telemedicine consults (Figure 1). The goal of this study was to report our neurosurgery department’s experience at a single institution located in the state of Florida with telemedicine during the COVID-19 pandemic. We wanted to test the hypothesis that telemedicine safely and effectively triages and follows neurosurgical patients. We summarize the necessary requirements to incorporate telemedicine in the outpatient neurosurgical practice beyond the current pandemic.
Figure 1.
Video telemedicine implementation by our neurosurgery department for ambulatory care, acute care, and post–acute care.
Patients and Methods
During the early part of the COVID-19 pandemic, to minimize the risk of exposure to SARS-CoV-2, our neurosurgery department performed an evaluation and triage of the upcoming outpatient clinic visits. Relevant imaging films were obtained for new consults, referrals, and follow-ups and evaluated by a physician. We implemented telemedicine not only to maintain follow-up of patients during government-issued stay-at-home orders but also to keep providing quality care to neurosurgical patients in need of a new evaluation. Furthermore, patients who were considered not in need of urgent surgery were converted to telemedicine or rescheduled if not considered at risk of significant impact by a postponement.
Neurosurgery Telemedicine Visit
Telemedicine visits were conducted in 2 ways: video with audio or telephone only. Video visits were conducted via the application Zoom (Zoom Video Communications, Inc.), which was integrated with our electronic medical record (EMR) Epic (Epic Systems Corporation), was compatible with Health Insurance Portability and Accountability Act (HIPPA) regulations during COVID-19, and was familiar among our physicians as our department has been using it for our virtual teaching conferences for residents and fellows, multidisciplinary boards, and meetings.
After scheduling the video consult, patients received an e-mail with attached instructions on how to access their video appointment (a copy of the instructions is available in the Supplemental Appendix, available online at http://www.mcpiqojournal.org). They were offered the possibility to perform a video test call with Mayo Clinic customer assistance staff. Creation of a Patient Online Services account and download of the Zoom app were required before the visit. To initiate their video consult, patients simply had to go in the “Appointments” section of their Patient Online Services account and click “Begin Video Appointment,” which redirected them to a secured Zoom meeting where they were greeted by a Mayo Clinic staff member who connected them with their health care provider (a neurosurgeon in this case). A certified medical interpreter was available for international and non–English-speaking patients. Given the multiple participant capability of Zoom, the interpreter joined the video encounter and helped facilitate the consult.
A major role in neurosurgical visits was the ability to review relevant neuroimaging studies. Normally patients are instructed to bring to the clinic the compact disc (CD) of imaging obtained at outside facilities, so that they can be uploaded into our EMR for the physician’s review. To obtain outside imaging for telemedicine consults, we implemented several measures: the external imaging facility could push images directly to our picture archiving and communication system; patients could receive a link through which they could upload the CDs into our system via a cloud-based secure imaging system (AMBRA, Ambra Health); or patients could mail the CDs to our clinic and we uploaded them into the EMR. During the telemedicine video consult, the capability to share the screen with Zoom allowed physicians to review images with patients and drawing on the screen allowed for effective communication.
Although some physical examination maneuvers could not be adequately performed via telemedicine, most urgent neurosurgical conditions can be readily detected using the combination of a detailed history and video evaluation of strength, coordination, and cognitive and cranial nerve function combined with relevant neuroimaging. Awadallah et al20 also validated a neurological examination via audiovisual telemedicine consisting of 22 items.
Demographic Characteristics and Telemedicine Visit Information
All patients who had a telemedicine visit in our neurosurgery department from April 1 through April 30, 2020, were included in this study. In this time period, we found 315 telemedicine encounters. We collected clinical data from the EMR Epic. These data included demographic information, diagnosis, type of visit (new consult/return visit/postoperative follow-up), type of telemedicine encounter (video and audio/audio only), surgical subspecialty (spine/cranial/vascular/functional), whether patients had surgery after their visit, name/type of the procedure, whether they had a return face-to-face visit, and whether they were admitted to the emergency department.
Satisfaction Questionnaire
To measure patient satisfaction after a telemedicine visit, a study assistant who was not involved in the patient’s care administered a questionnaire via phone or e-mail. The survey included questions on overall satisfaction with the telemedicine encounter, satisfaction with telemedicine technology, ease of talking to a care provider over video/phone, and likelihood of recommending telemedicine visits. The results of the satisfaction questionnaire were compared with those of an historical control group comprising patients who received a questionnaire after a face-to-face encounter in our neurosurgery department during quarter 1 of 2019.
Statistical Analyses
Descriptive statistics were calculated for demographic and clinical factors by using the median as a measure of central tendency and the interquartile range as a measure of dispersion. Comparisons of categorical variables were performed using the chi-square test. All tests were performed at a significance level of .05. All analyses were performed using SPSS version 21 (IBM Corporation).
Results
Telemedicine Visits
During the month of April, our neurosurgery department performed 315 telemedicine visits, of which 172 (55%) were phone consults and 143 (45%) video consults. One hundred one (32%) were new consults, 195 (62%) return visits, and 18 (6%) postoperative follow-ups. Seventy-six percent of new consults were video consults, whereas for return visits only 32% were video consults and most was phone consults (68%). New consults were more likely to be video with audio than return visits and postoperative follow-ups (P<.001), which were predominantly phone calls. During the month of March 2020, 94% of the neurosurgery clinic visits were face-to-face as compared with April 2020, in which 55% of the visits were telemedicine (P<.001) (Figure 2). Two hundred twenty-eight (72%) were spine consults, 61 (19%) cranial, 14 (5%) vascular, and 12 (4%) functional consultations.
Figure 2.
Neurosurgery visit volumes by visit type during the months of March and April 2020. Volume of telemedicine in April compared with March 2020 (P<.001). F2F = face-to-face visits.
Patient Population
The median age of patients was 62 years with an interquartile range of 52 to 72 years; the range was 19 to 90 years. One hundred fifty-eight patients (50%) were male (Table 1). Two hundred forty patients (76%) resided in the state of Florida; 65 (21%) were out of state, and we had patients residing in 18 states: Alabama, Arkansas, Colorado, Georgia, Illinois, Indiana, Kentucky, Louisiana, Massachusetts, Maryland, Missouri, New York, Oklahoma, Pennsylvania, South Carolina, Tennessee, Virginia, and West Virginia. Ten patients (3%) were international; 3 were new evaluations; and 7 were follow-ups. We had international patients from 7 countries: Mexico, Canada, Argentina, Brazil, Colombia, El Salvador, and Guatemala. None of the international patients required transfer for surgery. The median distance from our hospital for US patients was 100 mi (1 mi = 1.609344 km) with an interquartile range of 24 to 234 mi.
Table 1.
| Characteristic | Value |
|---|---|
| Age (y) | 62 (52-72) |
| Male sex | 158 (50) |
| Instate patients | 240 (76) |
| Out-of-state patients | 65 (21) |
| International patients | 10 (3) |
| Distance from the hospital (mi) | 100 (25-234) |
| Telemedicine visits | 315 |
| Phone consults | 172 (55) |
| Video consults | 143 (45) |
| New consults | 101 (32) |
| Phone consults | 24 (24) |
| Video consults | 77 (76) |
| Return visits | 195 (62) |
| Phone consults | 133 (68) |
| Video consults | 62 (32) |
| Postoperative follow-ups | 18 (6) |
| Phone consults | 14 (78) |
| Video consults | 4 (22) |
| Surgical subspecialty | |
| Cranial | 61 (19) |
| Functional | 12 (4) |
| Spine | 228 (72) |
| Vascular | 14 (5) |
| Patient who required surgery | 39 (12) |
| Surgical patients who came for F2F before surgery | 21 (54) |
| ED admissions | 0 (0) |
ED = emergency department; F2F = face-to-face.
Data are presented as median (interquartile range) or as No. (percentage).
Surgical Cases
Of this group, 39 patients (12%) met the requirements for surgery that was in the category of semi-urgent, urgent, or more emergent, thus representing a surgical yield of 12% for telemedicine encounters. Thirty (77%) were spine cases, 5 (13%) functional, and 4 (10%) cranial. Of the 39 patients who underwent surgery, 21 (54%) came to the clinic for a face-to-face visit before surgery. None of the 315 patients presented to the emergency department after the telemedicine consultation. Excluding the 21 patients who came for an in-person visit before their surgery, 0 patients required a face-to-face consult because of an incomplete telemedicine assessment. From the 258 face-to-face visits during the month of April, 106 patients underwent surgery for a 41% surgical yield. Patients who had face-to-face visits were more likely to require surgery (P<.001), as explained by the patient selection that was made for in-person encounters.
Satisfaction Questionnaire Results
Fifty-six patients responded to the satisfaction questionnaire after their telemedicine encounter. Fifty-one patients (91%) rated their overall visit assessment as very good. When the same question was asked to patients in our neurosurgery department after a face-to-face visit during quarter 1 of 2019, 240 of 273 respondents (88%) rated the assessment very good. There was no statistically significant difference in overall satisfaction between the patients who were seen via telemedicine in April 2020 compared with the historical control of in-person visits during quarter 1 of 2019 (P=.50) (Figure 3). Fifty-one respondents (91%) were very likely to recommend telemedicine; 45 (80%) said it was very easy talking to a care provider via telemedicine (Table 2).
Figure 3.
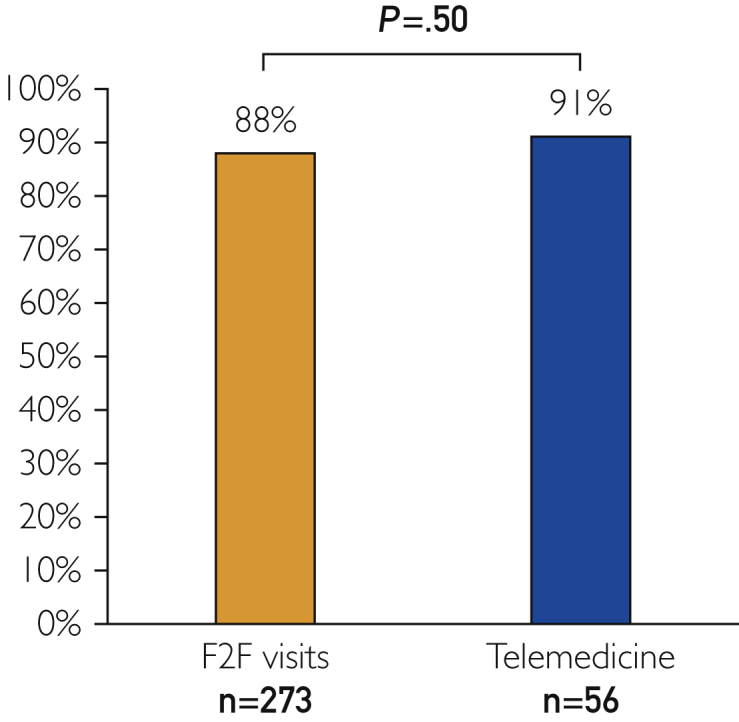
Percentage of patients who responded very good to the overall assessment question in the satisfaction questionnaire. Face-to-face (F2F) visits from an historical control group of neurosurgical patients from quarter 1 of 2019. Telemedicine encounters from April 2020. No statistically significant difference, P=.50.
Table 2.
Satisfaction Questionnaire
| Item | Telemedicine | Face-to-face | P value |
|---|---|---|---|
| Total respondents | 56 | 273 | |
| Overall assessment – very good | 51 (91) | 240 (88) | .50 |
| Talking to a care provider via telemedicine – very easy | 45 (80) | – | |
| Very likely to recommend telemedicine | 51 (91) | – |
Discussion
In this study, we report our preliminary experience at a single institution in the Department of Neurosurgery providing telemedicine care for new neurosurgical patients as well as maintaining follow-up via telemedicine during the COVID-19 pandemic. Until the month of March 2020, our practice was almost entirely face-to-face. To respond to stay-at-home government orders and decrease the risk of exposing patients and health care workers to SARS-CoV-2, we rapidly and extensively implemented telemedicine in our practice and it represented 55% of the visits performed by our neurosurgery department in the month of April 2020.
Regulatory Requirements
Presently, telemedicine capability is more widely accessible with lower technological barriers to adoption; there remain questions regarding the short-term to long-term regulatory environment. Several beneficial regulatory changes were implemented in response to the COVID-19 pandemic, which allowed many to implement telemedicine so rapidly in the United States. Before COVID-19, CMS allowed only telemedicine reimbursement for visits delivered to patients in rural health professional shortage areas (HPSA) at designated originating sides, which did not include homes.21 Under the Coronavirus Preparedness and Response Supplemental Appropriations Act and Section 1135 waiver, in response to the COVID-19 pandemic, CMS eased restrictions and allowed reimbursement for telemedicine services delivered to patients at home.22 Most private insurers rapidly followed suit.23 During COVID-19, coding and billing for telemedicine thus far appears to mirror the evaluation and management codes used in face-to-face time evaluation and management. In the long-term, obtaining a reimbursement equal or close to an in-person visit will be crucial in facilitating the adoption of telemedicine beyond this pandemic. Another key restriction before COVID-19 was the fact that for some states physicians were required to have a license in the state where the patient was located. During the COVID-19 pandemic, CMS eased the state licensure regulations to allow easier use of cross-state telemedicine.24
Privacy and confidentiality concerns remain present with the risk of data loss or hacking.25 CMS, however, allowed the adoption of telemedicine and eased restrictions, which allowed the use of non–HIPPA-compliant applications (such as FaceTime and WhatsApp). The Office of Civil Rights is also exercising its enforcement discretion to not impose penalties for HIPAA violations against health care providers in connection with their good faith provision of telehealth using communication technologies during the COVID-19 nationwide public health emergency.26 Nonetheless, we still strongly recommend use of a HIPPA-compliant software to perform telemedicine encounters, as we did with Zoom, integrated in our EMR Epic.
Benefits of Telemedicine During the COVID-19 Pandemic
Telemedicine played a key role in our response to the COVID-19 pandemic. It allowed us not only to minimize physical contacts and maintain social distancing practices but also to keep providing care for patients in need of a new evaluation or follow-up. As indicated by the escalation in the number of telemedicine visits during the month of April, the easing of restrictions by CMS allowed for a rapid diffusion of virtual consults. We generally encountered interest in patients in performing a telemedicine encounter. Our patients had a median age of 62 years, and the oldest patient who received a video visit was 90 years old. We did not encounter resistance in adopting the new technology from neurosurgery physicians. As reported in a retrospective review assessing factors associated with rates of telemedicine adoption, usability, local technical support, and appropriate training were critical factors to maximize telemedicine adoption.27 Our hospital system provided technical support for our staff and used an application that was already familiar to them, as routinely used for our teaching conferences and meetings. Another potential limitation is that not every neurosurgical practice may be able to shift the mode of visitation to telemedicine or have the same level of resources as we were able to implement in our department.
Our Experience
We were able to effectively use telemedicine for return visits, postoperative follow-up, and new consults for US as well as international patient. Being a destination medical center, we provided care via telemedicine not only to patients residing in the state of Florida (240 [76%]) but also to patients from 18 other states (65 [21%]). The median distance from the hospital for US patients was 100 mi; thanks to telemedicine, patients were able to avoid travel burdens and lost work hours. Telemedicine also allowed us to maintain follow-up and evaluate new international patients during a time when international travel almost came to a halt. We assessed 10 international patients during the month of March, mainly from Central America and South America. When the health care provider did not speak Spanish, a medical interpreter facilitated the encounter.
Patient Satisfaction
Most patients were satisfied with the telemedicine encounter. Ninety-one percent of the questionnaire respondents said they were overall very satisfied, and they would very likely recommend telemedicine. When compared to the historical control of in-person visits during quarter 1 of 2019, there was no statistically significant difference in overall satisfaction between the patients who were seen via telemedicine in April 2020 (P>.05)
Areas of Future Development
An aspect that still needs further development is the neurological physical examination performed via telemedicine. Remote diagnostic assessment is slower than a bedside assessment and relies on good lighting, sufficient room for the patient to move, and often the help of another person in positioning the camera for appropriate visualization. For spine consults, it is possible, by sharing the screen with Zoom, to share a pain diagram that the patient can draw on to represent the location of their pain. The importance of the clinical history, patterns of weakness and/or numbness, and presence or absence of radicular symptoms or neurological deficits were all reemphasized via telemedicine similar to the in-person examination. We were successfully able to perform 77 video encounters for new patients, 13 patients (17%) required surgery, and only 9 of those (69%) came for a face-to-face visit as part of their preoperative work-up.
Telemedicine emerged from this pandemic as an effective tool to provide quality care without the need of patients coming in person to the hospital and the added benefit in these circumstances of decreasing the exposure risk to SARS-CoV-2. Easing regulation and allowing for broader reimbursement helped obtaining a widespread implementation of virtual consults. If legal and regulatory barriers revert to their pre-pandemic status, we feel this would seriously hinder the future of telemedicine. A potential pitfall in the future is the possibility of nonpracticing neurosurgeons performing telemedicine visits for monetary purposes; that is why, as it was in our series, we advocate for actual practicing neurosurgeons to conduct telemedicine consults.
There are several potential benefits of telemedicine for patients—beyond the current pandemic—and they include reduced travel time and costs, less wait time, reduced time off from work, potentially improved access, patient satisfaction, and cost-savings for patients and hospitals that could decrease their overhead costs. Telemedicine could be especially beneficial for patients seeking expert opinions at tertiary medical centers far from their place of residence. Future emphasis should be placed on the policy and regulation barriers, licensing requirements, interoperable electronic data, potential for data theft, and billing and reimbursement.
Conclusion
We report our single department and institution experience using telemedicine during COVID-19 to provide outpatient care for neurosurgical patients. We describe the methods used by our institution, relevant regulatory requirements, and potential pitfalls and areas for further development. Most of our patients were satisfied with their encounter and would recommend telemedicine visits, and none of them had to come to an in-person visit because of incomplete evaluation or examination. During the COVID-19 pandemic, telemedicine has quickly emerged as an essential tool to balance social distancing and cross-infection with many other potential benefits that we hope will last long after this pandemic is resolved. In our experience, telemedicine can safely and effectively triage and follow up neurosurgical patients.
Footnotes
Potential Competing Interests: The authors report no competing interests.
Supplemental material can be found online at: http://www.mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.Zhu N., Zhang D., Wang W. China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P., Yang X.-L., Wang X.-G. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.COVID-19: recommendations for management of elective surgical procedures. American College of Surgeons website. https://www.facs.org/about-acs/covid-19/information-for-surgeons
- 4.Stahel P.F. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. 2020;14:8. doi: 10.1186/s13037-020-00235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CMS releases recommendations on adult elective surgeries, non-essential medical, surgical, and dental procedures during COVID-19 response. Centers for Medicare & Medicaid Services website. https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental
- 6.De Biase G., Freeman W., Elder B. Path to reopening surgery in the COVID-19 pandemic: neurosurgery experience [published online ahead of print June 30, 2020] https://doi.org/10.1016/j.mayocpiqo.2020.06.003 Mayo Clin Proc Innov Qual Outcomes. [DOI] [PMC free article] [PubMed]
- 7.World Health Organization . vol 2. World Health Organization; Geneva: 2010. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth.https://www.who.int/goe/publications/goe_telemedicine_2010.pdf (Global Observatory for eHealth Series). Accessed September 8, 2020. [Google Scholar]
- 8.Nesbitt T.S. National Academies Press (US); Washington, DC: 2012. The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. [PubMed] [Google Scholar]
- 9.LaMonte M.P., Bahouth M.N., Hu P. Telemedicine for acute stroke: triumphs and pitfalls. Stroke. 2003;34(3):725–728. doi: 10.1161/01.STR.0000056945.36583.37. [DOI] [PubMed] [Google Scholar]
- 10.Freeman W.D. Implementation of mobile health tools. JAMA. 2014;311(14):1448. doi: 10.1001/jama.2014.1109. [DOI] [PubMed] [Google Scholar]
- 11.Freeman W.D., Vatz K.A. The future of neurology. Neurol Clin. 2010;28(2):537–561. doi: 10.1016/j.ncl.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 12.Freeman W.D., Vatz K.A., Demaerschalk B.M. Telemedicine in 2010: robotic caveats. Lancet Neurol. 2010;9(11):1046. doi: 10.1016/S1474-4422(10)70261-1. [DOI] [PubMed] [Google Scholar]
- 13.Freeman W.D., Barrett K.M., Vatz K.A., Demaerschalk B.M. Future neurohospitalist: teleneurohospitalist. Neurohospitalist. 2012;2(4):132–143. doi: 10.1177/1941874412450714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barrett K.M., Pizzi M.A., Kesari V. Ambulance-based assessment of NIH Stroke Scale with telemedicine: a feasibility pilot study. J Telemed Telecare. 2017;23(4):476–483. doi: 10.1177/1357633X16648490. [DOI] [PubMed] [Google Scholar]
- 15.Cheshire W.P., Barrett K.M., Eidelman B.H. Patient perception of physician empathy in stroke telemedicine [published online ahead of print January 27, 2020] https://doi.org/10.1177/1357633X19899237 J Telemed Telecare. [DOI] [PubMed]
- 16.Rubin M.N., Barrett K.M., Freeman W.D. Teleneurosonology: a novel application of transcranial and carotid ultrasound. J Stroke Cerebrovasc Dis. 2015;24(3):562–565. doi: 10.1016/j.jstrokecerebrovasdis.2014.09.032. [DOI] [PubMed] [Google Scholar]
- 17.Tipton P.W., D’Souza C.E., Greenway M.R.F. Incorporation of telestroke into neurology residency training: “time is brain and education”. Telemed J E Health. 2020;26(8):1035–1042. doi: 10.1089/tmj.2019.0184. [DOI] [PubMed] [Google Scholar]
- 18.Mahato D., De Biase G., Ruiz-Garcia H.J. Impact of facility type and volume on post-surgical outcomes following diagnosis of WHO grade II glioma. J Clin Neurosci. 2018;58:34–41. doi: 10.1016/j.jocn.2018.10.078. [DOI] [PubMed] [Google Scholar]
- 19.Yoon J.W., Wanderman N.R., Kerezoudis P. Enterobacter infection after spine surgery: an institutional experience. World Neurosurg. 2019;123:e330–e337. doi: 10.1016/j.wneu.2018.11.169. [DOI] [PubMed] [Google Scholar]
- 20.Awadallah M., Janssen F., Körber B., Breuer L., Scibor M., Handschu R. Telemedicine in general neurology: interrater reliability of clinical neurological examination via audio-visual telemedicine. Eur Neurol. 2018;80(5-6):289–294. doi: 10.1159/000497157. [DOI] [PubMed] [Google Scholar]
- 21.Medicare telemedicine health care provider fact sheet. Centers for Medicare & Medicaid Services website. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- 22.Wright J.H., Caudill R. Remote treatment delivery in response to the COVID-19 pandemic. Psychother Psychosom. 2020;89(3):130–132. doi: 10.1159/000507376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Health insurance providers respond to coronavirus (COVID-19). America’s Health Insurance Plans (AHIP) website. https://www.ahip.org/health-insurance-providers-respond-to-coronavirus-covid-19/
- 24.Additional background: sweeping regulatory changes to help U.S. healthcare system address COVID-19 patient surge. Centers for Medicare & Medicaid Services website. https://www.cms.gov/newsroom/fact-sheets/additional-backgroundsweeping-regulatory-changes-help-us-healthcare-system-address-covid-19-patient
- 25.American Association of Neurological Surgeons Congress of Neurological Surgeons Joint Cerebrovascular Section Joint Section on Neurotrauma and Critical Care. Position Statement on Telemedicine. American Association of Neurological Surgeons. https://www.aans.org/-/media/Files/AANS/Advocacy/PDFS/Position-Statements/AANS-CNS-Telemedicine-Position-Statement-2017-FINAL.ashx?la=en&hash=0A2FC4AF703C584CC3A0B230C2FD3A30468E9C36
- 26.Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. U.S. Department of Health & Human Services website. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html
- 27.Broens T.H.F., Huis in’t Veld R.M.H.A., Vollenbroek-Hutten M.M.R., Hermens H.J., van Halteren A.T., Nieuwenhuis L.J.M. Determinants of successful telemedicine implementations: a literature study. J Telemed Telecare. 2007;13(6):303–309. doi: 10.1258/135763307781644951. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.