Abstract
Background
The high incidence of work-related diseases and injuries among day-laborers and workers with no legal contracts (informal workers) has received the attention of the Thai authorities. Workers' low occupational health literacy (OHL) has been reasoned as one contributing factor. Absence of a valid tool has prevented assessment of informal workers' OHL. The aim of this study was to create a valid and reliable Occupational Health Literacy Scale within the context of Thai working culture (TOHLS-IF).
Methods
This study used the mixed method approach to develop TOHLS-IF. Questions were generated using in-depth interviews and an extensive review of the literature. Experts' assessment confirmed the content validity of TOHLS-IF. The scales of its psychometric properties were assessed in a sample of 400 informal workers using cluster random sampling.
Results
The final version of the TOHLS-IF comprises 38 items within 4 dimensions: Ability to Gain Access, Understanding, Evaluation, and Use of occupational health and safety information. Factor analysis identified items explaining 50.22% of the total variance. The final confirmatory analysis confirmed the model estimates were satisfactory for the construct. TOHLS-IF demonstrated a high internal consistency and satisfactory reliability (Cronbach's alpha = .98).
Conclusion
The TOHLS-IF is a valid and reliable instrument to assess informal workers' OHL. The structural dimensions of this instrument are based on the concept of health literacy and Thai culture. Thai health professionals are encouraged to benefit from this instrument to assess their workers' OHL and apply findings as guidelines for effective occupational health and safety interventions.
Keywords: Instrument, Occupational health literacy, Scale development, Thai informal workers
1. Introduction
The concept of health literacy has been well established. In accordance with the World Health Organization, people who are health literate are not only simply able to read health information but also able to understand and use information in ways that promote and maintain health [1]. The World Health Organization definition suggests that health literacy is an outcome of health promotion and disease prevention [2,3]. Kickbusch quoted two definitions of health literacy. The first focuses on the “ability to perform basic reading and numerical skills required to function in the health-care environment.” The second is “the capacity to obtain, interpret and understand basic health information and services and the competence to use such information and services to enhance health” [4]. Therefore, health literacy comprises skills and competencies that individuals develop to search, comprehend, evaluate, and use health information and services to make informed choices, reduce health risks, and increase quality of life.
Health literacy is linked to a spectrum of health conditions and health-care concepts including occupational health and safety issues; the latter two are specifically important aspect in prevention of work-related disease and injuries. Rauscher and Myers [5] defined the concept of occupational health literacy (OHL) as the degree to which workers have the capacity to obtain, communicate, process, and understand occupational health and safety information and services in making appropriate health decisions in their workplaces. Studies have founded that workers with poor occupational health lite racy have a higher incidence of work-related injuries, illnesses, and fatalities [6,7]. Workers in informal sector, especially in low- and middle-income countries, are quite vulnerable to occupational health hazards and work-related injuries due to their limited OHL [8,9].
In Thailand, informal workers are extremely important to Thailand's economy. In accordance with the 2019 employment survey by the National Statistical Office, the informal workers account for 54.3 % of Thailand's workforce [10]. Economic productivity of the informal workers has been estimated at 60-70% of Thailand's GDP [11]. Per the definition of the Thailand National Statistical Office, an informal worker is “a person of at least 15 years of age, whose employment is neither protected nor regulated by the Thai social security system [10]. In general, informal workers are either self-employed or are hourly wage earners; in addition, they do not have a set regular working hours and most likely either work at home or in the service, construction or material transfer industries. Informal workers mostly are comprised of unskilled workforces, young and old individuals in a community, as well as immigrant groups. Workforce are more likely to be low educated and have low socioeconomic background; therefore, many can be at elevated risk of low health literacy. In general, training educational and safety resources are neither available nor accessible to many informal workers; the lack of education and safety resources make this segment of the population more vulnerable to occupational related injuries, occupationally related adverse health conditions, and even death [12].
Unfortunately, many of these occupationally related injuries and health conditions are not reported or underreported. Some describe this underreporting as “suffering in silence” [13]. Regardless of literacy or immigration status, in Thailand, all workers are protected by the National Workplace Rights [14]. However, most vulnerable workers due to fear of losing their jobs do not report their work-related injuries; whereas others, do not have the knowledge how to document and process their reports or how to seek health-care services when injured at work. The inability of vulnerable workers to advocate for themselves often leads to disparities in occupational health outcomes. Moreover, poor or inadequate hazard communication training for workers with low health literacy exacerbates these health inequalities [15].
Assessing health literacy is the first step in protecting people from potential occupational health hazards [7]. For the last decade, several health literacy instruments have been developed in different countries including Thailand [[16], [17], [18]]. In addition, a number of subject-specific literacy concepts, such as oral health literacy, nutrition literacy, and mental health literacy also have been developed [[19], [20], [21]]. Although these literacy concepts require acquisition of different skills, abilities, and knowledge, they all are built on the foundation of, and are closely related to, the general concept of health literacy. Furthermore, none contribute to the concept of health literacy in the domain of occupational health and safety.
A Search in literature supports a paucity of valid and acceptable instrument for assessment of OHL. The latest Thai OHL instrument has been developed to assess OHL of informal and legal workers in work settings in large urban settings such as Bangkok [22]. Its application might not be valid in other settings, such as rural areas or smaller cities; therefore, we developed and validated an OHL scale specifically for Thai workers in the informal sectors. The Thai Occupational Health Literacy Scale for Informal Workers is consistent with the concept of health literacy. This concept was introduced by Sørensen et al. [2] and evaluates cognitive aptitudes of an individual in gaining access to, understanding, evaluating, and applying of health information. Assessing OHL can yield to a better understanding about the competency of workers about the crucial role of occupational health and work safety in their own overall health and well-being. Therefore, findings can be conduits for developing effective and appropriate interventions at workplace to improve health literacy of workers.
2. Materials and methods
2.1. Development process
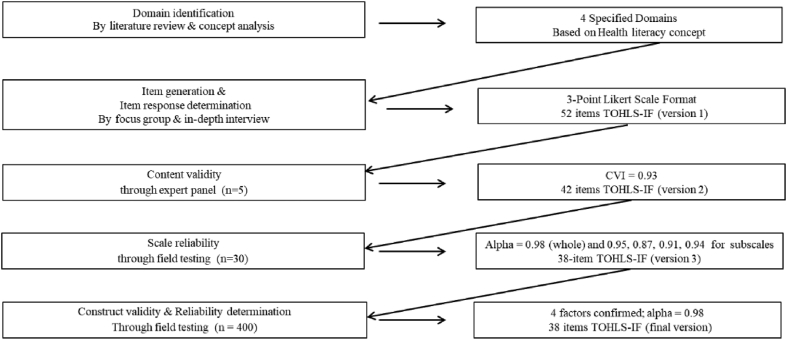
The guideline and the development of the instrument was developed based on scientific advice and suggestions of an expert in the field of OHL [[23], [24], [25]]. To address the objective of the study, we implemented a mixed method study (Fig. 1). The initial step was the domain identification and item generation using deductive and inductive methods [26]. The deductive methods involved domain identification and item generation which were based on an extensive literature review and pre-existing scales [[26], [27], [28]]. The inductive method was used to collect qualitative information about the construct of the instrument. One focus group and multiple in-depth interviews were held to collect qualitative data about the contents of the survey and the development of the initial pool of questions. A total of 30 informal workers from various work settings, were purposively sampled to participate in the focus group. All workers were recruited from one province (Chiang Mai) in the northern region of Thailand. This step was followed by assessment and evaluation of the initial pool of items by a panel of five experts to ascertain the desired construct [29]. The panel was selected based on their expertise in the areas of occupational health and instrument development. The criteria used by the experts for retention or deletion of items included clarity of expression, face validity, and appropriateness for the construct being measured.
Fig. 1.
Stages and results of the development and psychometric evaluation of the Thai Occupational Health Literacy Scale for Informal Workers (TOHLS-IF).
After item reduction and modification, the remaining items were used to draft of the first version of TOHLS-IF. This version was returned to the panel for validation of face and content validity. In addition, the panel validated the item response determination on a 3-point scale (1 = not relevant, 2 = somewhat relevant, and 3 = high relevant). The content validity index of the revised version (Version 2) was computed [4,28,29]. Sociodemographic questions were added to Version 2 before field testing the instrument for its reliability. In addition, the clarity of items and the length of time required to complete the instrument was evaluated. Furthermore, we sought participants' inputs about the response scales. Finally, psychometric analysis was performed to assess construct validity and reliability of Version 2. The instrument was modified accordingly and the latest version, Version 3, was field validated.
For the purpose of field validation, multicluster random sampling was used to recruit a total of 420 informal workers. The number of participants was calculated based on item-to-participant ratio of at least 1:10 [[30], [31], [32], [33]]. Based on previous data about response rate of self-administered survey in Thai public health studies, the total number of participants then was inflated by 10% (n = 40) to account for incomplete or no-response participation [34]. The inclusion and exclusion criteria are as follow; members of the community were eligible to participate if: (A) they were working with no legal work contracts; (B) If they had worked with no legal work contracts for a minimum of 6 months before participating in the study; (C) if they were 15 years or older; (D) if they were willing to participate in the study. Members of the community who were business owners were excluded from the study. We recruited community volunteers who were prominent members of the community to distribute the questionnaires.
Informal workers holding immigrant status (n = 34) were also recruited to participate in our study. For these participants, data were collected using in-person interview method; in addition, a translator was present during the interviews in case of limited or inability to communicate in Thai language; however, most of the immigrant workers were able to communicate in Thai because of their long-term residency in Thailand.
2.2. Data analysis
Construct validity of TOHLS-IF was evaluated using exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The factor structure of the scale was examined by EFA, which is a highly powerful and widely applied procedure for construct validation; however, it involves a high degree of subjectivity [35]. To avoid this bias, we applied a factor loading cutoff point of 0.30 [36,37]. Values for Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy were used to assess the suitability of data for factorization. The criterion for loading and cross loading was set at 0.4; items with loading below this value and cross loading over this value were deleted. CFA was used to cross validate the factor structure derived from EFA. The CFA was performed based on the variance–covariance matrix using the analysis of moment of structure (AMOS) statistical package for testing the factor model [38].
A number of indices was used to assess the goodness of fit test of the CFA model. The indices included root means square error of approximation (RMSEA), goodness of fit index (GFI), adjusted goodness of fit index (AGFI), comparative fit index (CFI), and normal fit index (NFI) [39]. The internal consistency was established by calculating Cronbach's alpha coefficients [40].
2.3. Research ethics
This study was approved by the Institutional Review Board of the Faculty of Nursing, Chiang Mai University, Thailand (Approval # 049/2017). Written informed consents were obtained from all participants. Participation was anonymous, confidential, and on a voluntary basis.
3. Results
The initial scale development was domain identification, derived from the well-established health literacy concept [2], and founded on: accessibility, understandability, evaluability, and utilization of occupational health and safety (OHS) information and services. The themes that emerged from the qualitative data were used to build the first version of the instrument. The first version contained a total of 52 items. Result from the content validation evaluation of Version 1 of the TOHLS-IF was 0.93. Based on the experts' inputs, 10 of the items were removed due to redundancy of content. In addition, five of the remaining 42 items were modified to enhance clarity and simplicity of item content. Item response determination, which was initially addressed by the focus group, also was suggested by the panel of experts. The initially developed 3-points Likert scale format was retained. After Version 2 was field tested, we decided to eliminate 4 additional items. Thus, the third version, which is the final version of the TOHLS-IF, consisted of 38 items, 4 factors.
The final version was field tested; A total of 402 of 420 participants (95.7% response rate) returned their completed questionnaires; however, two of the questionnaires were eliminated due to incomplete answers, resulting 400 to be analyzed. A total of 156 (39%) of participants were male and 244 (61%) were female. The average age was 42.5 (range: 16-60) years of age. A total of 26 (6.5%) of the participants lacked formal education; 113 (28%) had completed elementary education, 74 (18.5%) were educated at 9th grade formal education, 54 (13.5%) had completed high school education, and 135 (33.5%) had either vocational or college education. The average duration of working experience was 10 (range: 6 months-19 years) years.
The scale reliability with Cronbach's Alpha for subscales ranged between 0.87 and 0.96; the reliability for the entire scale was calculated at 0.98 (Fig. 1). The 38 items were subjected to EFA to assess the factorial validity of the scale. The KMO measure of sampling adequacy was 0.986 and Bartlett's test of sphericity was 1310.586 (p = 000, df 44) which suggested that data were suitable for factor analysis [41,42]. Table 1 shows a four-factor solution, including 38 items, explaining 50.22% of the total item variance in the database had been captured. Factor 1 (7 items), “Access to OHS Information and Services” had factor loading between 0.57 and 0.73, accounted for 14.84% of the variance. Factor 2 (15 items), “Understanding of OHS Information”, had factor loading between 0.40 and 0.69, and accounted for 12.94 % of the variance. Factor 3 (4 items), “Evaluation of OHS Information”, had factor loading between 0.62 and 0.79 that accounted for 12.70% of the variance. Finally, Factor 4 (12 items), “Use of OHS Information and Services”, had factor loading between 0.45 and 0.69 and accounted for 9.75 % of the variance.
Table 1.
Exploratory factor analysis of 38-item of the Thai Occupational Health Literacy Scale for Informal Workers (TOHLS-IF)
| Domain/item | Component |
|||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Factor 1: Ability to gain access to OHS1information | ||||
|
.61 | |||
|
.56 | |||
|
.70 | |||
|
.70 | |||
|
.64 | |||
|
.73 | |||
|
.57 | |||
| Factor 2: Understand OHS information | ||||
|
.41 | |||
|
.42 | |||
|
.40 | |||
|
.41 | |||
|
.59 | |||
|
.55 | |||
|
.66 | |||
|
.69 | |||
|
.68 | |||
|
.61 | |||
|
.48 | |||
|
.68 | |||
|
.50 | |||
|
.51 | |||
|
.45 | |||
| Factor 3: Evaluation of OHS information | ||||
|
.71 | |||
|
.78 | |||
|
.79 | |||
|
.62 | |||
| Factor 4: Use of OHS information | ||||
|
.66 | |||
|
.67 | |||
|
.67 | |||
|
.52 | |||
|
.65 | |||
|
.50 | |||
|
.45 | |||
|
.63 | |||
|
.69 | |||
|
.62 | |||
|
.57 | |||
|
.54 | |||
| Eigenvalue | 5.64 | 4.92 | 4.83 | 3.70 |
| % of variance | 14.84 | 12.94 | 12.70 | 9.75 |
| Cumulative % | 14.84 | 27.77 | 40.47 | 50.22 |
Note: Extraction method: Principal Component Analysis. Rotation method: Varimax with Kaiser Normalization; 1OHS: Occupational Health Safety.
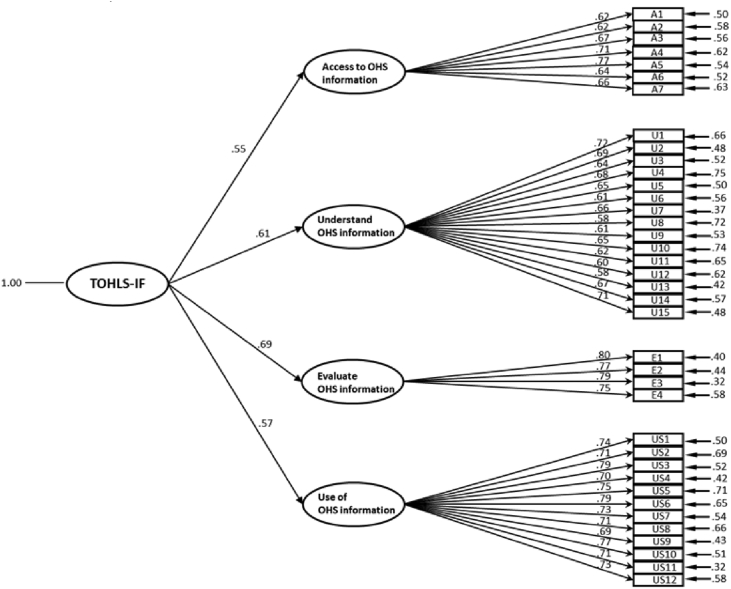
The CFA with maximum likelihood method was used and yielded the same four-factor structure. As presented in Table 2, several CFA fit indices (χ2/df < 3.00, RMSEA < 0.06, CFI > 0.95, NFI, GFI, and AGFI > 0.90) indicated goodness of fit for the model [[42], [43], [44]]. Results yielded Model 4 as the best fit and supported the assumption of dimensionality of that these 4 factors for the scale. The hierarchical model with factor loadings and the standardized maximum likelihood parameter estimates are presented (Fig. 2). The Standardized loadings of all items were higher than 0.50, fluctuating between 0.58 and 0.80, demonstrating that the observed variable sufficiently reflect its construct latent variable [44]. The fitness of the estimated model was considered as acceptable because the result of multiple indices yielded at satisfactory levels.
Table 2.
Model fit in confirmatory factor analysis (CFA)
| Model | χ2 | df | χ2/df | RMSEA | Goodness of fit statistics |
|||
|---|---|---|---|---|---|---|---|---|
| GFI | AGFI | CFI | NFI | |||||
| 1 | 2439.92∗∗∗ | 659 | 3.70 | 0.05 | 0.75 | 0.72 | 0.95 | 0.93 |
| 2 | 1126.55∗∗∗ | 609 | 1.85 | 0.05 | 0.88 | 0.83 | 0.98 | 0.96 |
| 3 | 1042.08∗∗∗ | 603 | 1.73 | 0.04 | 0.88 | 0.85 | 0.98 | 0.97 |
| 4 | 977.13∗∗∗ | 602 | 1.62 | 0.04 | 0.99 | 0.86 | 0.99 | 0.97 |
Note: ∗∗∗p < .0001, RMSEA = root means square error of approximation, GFI = goodness of fit index, AGFI = adjusted goodness of fit index, CFI = comparative fit index and NFI = normal fit index.
Fig. 2.
Confirmatory factor analysis based on 38 items and 4 factors.
4. Discussion
This study is the first, to the best of our knowledge, to report on the development and validation of a socioculturally specific instrument to evaluate OHL. In the development of item pool, the theme emerged from extensive review of health literacy literature. Findings were used to build on the related constructs and were applied as guideline for the development of the item pool. In addition, information that was gleaned during interviews was used to fine-tune the instrument.
The items were generated from the perspectives of informal workers from a wide range of workplaces. This approach ascertained the content validity of the tool at the beginning of the study. The process also identified appropriate key words and language that were understandable by the targeted population. In the development of the scale, the item pool was validated by experts, selected for their expertise in the area of occupational health and safety, as well as instrument development. This approach most likely strengthened the face and content validity of the scale [26,27].
In the assessment of the psychometric properties of the TOHLS-IF, the evidence of the construct validity was supported by EFA and CFA. An EFA using the maximum likelihood procedure with oblique rotation was performed to determine the number of factors. The Bartletts test of sphericity reached statistical significance (P = .000). The KMO measure of sampling adequacy was considered as very good (.896) and supported their retention in the analysis [41,42]. Given that the data were normally distributed, a maximum likelihood factor extraction with oblique rotation was conducted to determine the number of factors and the extent of interfactor correlation. The eigenvalues suggested four-factor solutions, which accounted for 50.22% of the total variance. Factor 1 (Ability to gain access to OHS information) contained 7 items, Factor 2 (Understanding OHS information) contained 15 items, Factor 3 (Evaluation of OHS information) contained 4 items, and Factor 4 (Use of OHS information) contained 12 items (Table 1). The items revealed high factor loadings higher than .50 without any one item indicating a significant cross loading. Moreover, all factor loadings were significant, and the items showed high communalities (mean item communality = .61) [45].
CFA was used to validate the EFA-derived factor structures of the scale [35,36]. To discuss the model fit of CFA, the criteria of the various model fit indices were considered. It has been suggested that the RMSEA values less than 0.05 should be considered as good, between 0.05 and 0.08 as acceptable, between 0.08 and 0.1 as marginal, and values greater than 0.1 as poor [43]. Therefore, the values of .04 in this study indicate a good fit. The GFI and the CFI values in Model 4 were greater than 0.9 and the AGFI value was close to 0.9; these values indicate a relatively good fit [43]. For the Normal Fit Idex (NFI), our finding was over the good fit which concurs with previous work [43]. Overall, the calculated indices values support the notion of a good fit for the instrument and provide the confirmatory evidence for the factor structure.
Finally, the internal consistency of the scale and its 4 subscales, as measured by Cronbach's alpha, were all greater than 0.9, indicating highly satisfactory [44]. Generally, if α > 0.9, the internal consistency, is considered as excellent, whereas, 0.7 < α < 0.9, as good [46]. Results from the analysis support the notion of acceptable reliability for both the overall instrument and each subdimension. The individuals who contributed to our study were recruited using the multicluster random sampling technique; they were representatives of the heterogeneous population of Thai informal workers. Therefore, generalizability of the study results is quite good.
In sum, the TOHLS-IF can be considered as a valid and reliable instrument in assessing the OHL among Thai informal workers. Use of this instrument can enable occupational health personnel to identify valuable information for the improvement of workers' health and safety. However, because our instrument was developed using empirical data from informal working population of Thailand, caution should be exercised when considering the use of the TOHLS-IF in other informal workforce with different working characteristics, health-care context, and cultural norms and values. For example, the question of “whether workers received occupational health and safety information from a health-care volunteer” might not be applicable in other countries with no health-care volunteer system. It is recommended further studies should be conducted in other cultures and work settings with the objective of developing OHL scales tailored for each specific setting.
Conflicts of interest
All contributing authors have no conflict of interest to declare.
Acknowledgments
This research has been supported by Thai Health Promotion Foundation (ThaiHealth). The authors would like to thank all study participants for their cooperation. A special thanks to Dr. Azadeh Stark for technical suggestions and assistance with drafting of this manuscript.
References
- 1.World Health Organization (WHO) Presented at the 7th Global Conference on Health Promotion, Shanghai, China [Internet] 2016. Health literacy and health behavior.www.who.int/healthpromotion/conferences/9gchp/health-literacy/en/ [cited 2019 May 12]. Available from: [Google Scholar]
- 2.Sørensen K., Van den Broucke S., Fullam J. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health [Internet] 2012:12–80. doi: 10.1186/1471-2458-12-80. [cited 2019 May 15]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21stcentury. Health Promot Int. 2000;15:259–267. [Google Scholar]
- 4.Kickbusch I.S. Health literacy: addressing the health and education divide. Health Promot Int [Internet] 2001;16(3):289–297. doi: 10.1093/heapro/16.3.289. https://academic.oup.com/heapro/article/16/3/289/653857 [cited 2019 May 22]; Available from: [DOI] [PubMed] [Google Scholar]
- 5.Rauscher K.J., Myers D.J. Socioeconomic disparities in the prevalence of work-related injuries among adolescents in the United States. J Adolesc Health. 2008;42(1):50–57. doi: 10.1016/j.jadohealth.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 6.National Occupational Research Agenda (NORA) 2010. Health disparities in manufacturing.www.cdc.gov/niosh/docs/2010-146/pdfs/2010-146.pdf (Publication no. 2010-146) [cited 2019 May 15]. Available from: [Google Scholar]
- 7.Department of Health and Human Services (HHS) HHS; Washington, D.C.: 2016. Quick guide to health literacy [Internet]www.health.gov/communication/literacy/quickguide/factsbasic.html [cited 2019, May 14]. Available from: [Google Scholar]
- 8.International Labour Organization (ILO), Informal economy: a hazardous activity. [cited 2019 May 22]. Available from: https://www.ilo.org/safework/areasofwork/hazardous-work/WCMS_110305/lang--en/index.htm.
- 9.Rockefeller Foundation . 2013. Report. Health vulnerabilities of informal workers [Internet]https://assets.rockefellerfoundation.org/app/uploads/20130528214745/Health-Vulnerabilities-of-Informal-Workers.pdf [cited 2019 May 28]. Available from: [Google Scholar]
- 10.National Statistical Office (NSO), Ministry of Digital Economy and Society, Thailand . 2018. The informal employment survey; p. 131. (in Thai) [Google Scholar]
- 11.Office of the National Economic and Social Development Council (NESDC), Thailand . 2019. A report on social situation and outlook.https://www.nesdc.go.th/ewt_dl_link.php?nid=5491&filename=socialoutlookreport [cited 2020 Mar 14]. Available from: (in Thai) [Google Scholar]
- 12.Wong B.K. Building a health literate workplace. Workplace Health Saf. 2012;60(8):363–369. doi: 10.1177/216507991206000806. quiz 370. [DOI] [PubMed] [Google Scholar]
- 13.Kriebel D., Jacobs M.M., Markkanen P., Tickner J. Lowell Center for Sustainable Production at University of Massachusetts Lowell; 2011. Lessons learned: solutions for workplace safety and health.www.sustainableproduction.org/Lessons.php [cited 2019 May 22]. Available from: [Google Scholar]
- 14.Jun-on N. 2013. Management of labour in the informal sector in Thailand.http://library.senate.go.th/document/Ext5360/5360123_0002.PDF (in Thai). Available from: [Google Scholar]
- 15.Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Crotty K. Low health literacy and health outcomes: an updated systematic review. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 16.Cutilli C.C., Bennett I.M. Understanding the health literacy of America: results of the national assessment of adult literacy. Orthop Nurs. 2009;28(1):27–34. doi: 10.1097/01.NOR.0000345852.22122.d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sørensen K. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU) Eur J Public Health. 2015;25(6):1053–1058. doi: 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roma M. 2018. Health Systems Research Institute (HSRI). National health literacy survey 2017, Thailand (Phase 1) (in Thai). Available from: Report No. hs2438.pdf. [Google Scholar]
- 19.Sabbahi D.A., Lawrence H.P., Limeback H., Rootman I. Development and evaluation of an oral health literacy instrument for adults. Community Dent Oral Epidemiol. 2009;37(5):451–462. doi: 10.1111/j.1600-0528.2009.00490.x. [DOI] [PubMed] [Google Scholar]
- 20.Gibbs H., Chapman-Novakofski K. Establishing content validity for the nutrition literacy assessment instrument. Prev Chronic Dis. 2013;10:E109. doi: 10.5888/pcd10.120267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Azizi N., Karimy M., Abedini R., Armoon B., Montazeri A. Development and validation of the health literacy scale for workers. Int J Occup Environ Med. 2019;10(1):30–39. doi: 10.15171/ijoem.2019.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoryuenyong C., Cheryklinput N., Chiangkhong A. Health literacy for occupational diseases prevention among workers in Bangkok Metropolitan: development and validation of health literacy scale. Kuakarun J Nurs. 2019;26(2):7–21. (in Thai) [Google Scholar]
- 23.De Vellis R.F. 2nd ed. SAGE Publications; University of North Carolina, Chapel Hill (USA): 2016. Scale development: theory and application; p. 280. [Google Scholar]
- 24.Nunnally J.C. 2nd ed. McGraw-Hill; New York (NY): 1978. Psychometric theory; p. 701. [Google Scholar]
- 25.Netemeyer R.G., Bearden W.O., Sharma S. Sage Publications; California (CA): 2003. Scaling procedures: issues and applications; p. 224. [Google Scholar]
- 26.Morgado F.F.R., Meireles J.F.F., Neves C.M., Amaral A.C.S., Ferreira M.E.C. Scale development: ten main limitations and recommendations to improve future research practices. Psicol Reflex E Critia. 2018;30:3. doi: 10.1186/s41155-016-0057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hinkin T.R. 1998. A brief tutorial on the development of measures for use in survey questionnaires [Internet]http://scholarship.cornell.edu/articles/521 [cited 2019 May 18]. Available from: [Google Scholar]
- 28.Boateng G., Neilands T.B., Frongillo E.A., Megar-Quinonez H.R., Yong S.L. Best practice for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. 2018;6:149. doi: 10.3389/fpubh.2018.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davis L.L. Instrument review: getting the most from a panel of experts. Appl Nurs Res. 1992;5(4):194–197. [Google Scholar]
- 30.MacCallum R.C., Widaman K.F., Preacher K.J., Hong S. Sample size in factor analysis: the role of model error. Multivariate Behav Res. 2001;36:611–637. doi: 10.1207/S15327906MBR3604_06. [DOI] [PubMed] [Google Scholar]
- 31.Osborne J.W., Costello A.B. Sample size and subject to item ratio in principal components analysis. Pract Assess Res Eval. 2004;9(11) http://PAREonline.net/getvn.asp?v=9&n=11 (cited 2019 May 22). Available from: [Google Scholar]
- 32.Meade A.W., Bauer D.J. Power and precision in confirmatory factor analytic tests of measurement invariance. Struct Equ Model. 2007;14(4):611–635. [Google Scholar]
- 33.Kyriazos T.A. Applied psychometrics: sample size and sample power considerations in factor Analysis (EFA, CFA) and SEM in general. Psychology. 2018;9:2207–2230. [Google Scholar]
- 34.Sombutteera K., Thavornpitak Y. Response rate and factors associating mailed questionnaire: response rate in nursing sciences and public health research. KKU Res J. 2015;15(1):105–113. (in Thai) [Google Scholar]
- 35.Polit D.F., Beck C.T. 5th ed. Lippincott Company; Philadelphia (PA): 2006. Essential of nursing research: methods, appraisal, and utilization; p. 758. [Google Scholar]
- 36.Waltz C., Strickland O., Lenz E. 5th ed. Springer Publishing Company; New York (NY): 2010. Measurement in nursing and health research; p. 634. [Google Scholar]
- 37.Hinkle D.E., Jurs S.G., Wiersma W. 2nd ed. Houghton Mifflin; Boston (MA): 1988. Applied statistics for the behavioral sciences; p. 682. [Google Scholar]
- 38.Arbuckle J. Amos Development Cooperation; Chicago, IL: 2010. Amos 17.0 users’ guide. [Google Scholar]
- 39.Bentler P.M., Chou C.P. Practical issues in structural modeling. Sociol Methods Res. 1987;16(1):78–117. [Google Scholar]
- 40.Cronbach L.J. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 41.Kaiser H.F. An index of factorial simplicity. Psychometrika. 1974;39(1) doi: 10.1007/BF02291575. (cited 2019 May 30). Available from: [DOI] [Google Scholar]
- 42.Bartlett M.S. A note on the multiplying factors for various chi square approximation. J R Stac Soc. 1954:296–298. (series B) [Google Scholar]
- 43.Bentler P.M., Bonett D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. [Google Scholar]
- 44.Schreiber J.B., Nora A., Stage F.K., Barlow E.A., King J. Reporting structural equation modeling and confirmatory factor Analysis results: a review. J Educ Res. 2006;99:323–338. [Google Scholar]
- 45.Polit D.F., Beck C.T. The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health. 2006;29:489–497. doi: 10.1002/nur.20147. [DOI] [PubMed] [Google Scholar]
- 46.Horn J.L. On the internal consistency reliability of factors. Multivariate Behav Res. 1969;4:115–125. [Google Scholar]