Abstract
In 2013, DSM-5 urged for further research on non-suicidal self-injury (NSSI) and defined NSSI disorder (NSSI-D) for the first time separate from borderline personality disorder (BPD). However, research on the comorbidity between NSSI-D and BPD symptoms is still scarce, especially in adolescent populations. The current study selected 347 adolescents who engaged at least once in NSSI (78.4% girls, Mage = 15.05) and investigated prevalence, comorbidity, gender differences, and bridge symptoms of NSSI-D and BPD. Network analysis allowed us to visualize the comorbidity structure of NSSI-D and BPD on a symptom-level and revealed which bridge symptoms connected both disorders. Our results supported NSSI-D as significantly distinct from, yet closely related to, BPD in adolescents. Even though girls were more likely to meet the NSSI-D criteria, our findings suggested that the manner in which NSSI-D and BPD symptoms were interconnected, did not differ between girls and boys. Furthermore, loneliness, impulsivity, separation anxiety, frequent thinking about NSSI, and negative affect prior to NSSI were detected as prominent bridge symptoms between NSSI-D and BPD. These bridge symptoms could provide useful targets for early intervention in and prevention of the development of comorbidity between NSSI-D and BPD. Although the current study was limited by a small male sample, these findings do provide novel insights in the complex comorbidity between NSSI-D and BPD symptoms in adolescence.
Keywords: non-suicidal self-injury (NSSI), NSSI disorder, adolescence, comorbidity, DSM-5, borderline personality disorder, network analysis
Introduction
Non-suicidal Self-Injury (Disorder)
Non-Suicidal Self-Injury (NSSI) is defined as the socially unacceptable, intentional, and direct injury of one's own body tissue without suicidal intent (1). Common methods of NSSI include cutting, burning, or carving one's own skin (2). In community samples, pooled estimates suggest that 17.2% of adolescents, 13.4% of young adults, and 5.5% of adults report a lifetime history of NSSI (3). In clinical samples, lifetime prevalence rises to 60% in adolescence and 65–80% in adulthood (4, 5). The high prevalence rates of NSSI are alarming, as the behavior has been linked to several mental health conditions. For instance, NSSI is associated with depression, anxiety, rumination, feelings of stigma and shame, and low levels of help seeking (6–8). Moreover, 50–75% of those with a history of NSSI make a suicide attempt at some point in their life (9). Research has shown how NSSI can occur with virtually any mental disorder, although comorbidity rates are particularly high for anxiety and mood disorders, post-traumatic stress disorder, substance use disorder, eating disorders, and personality disorders (10–12). The high prevalence rates and significant mental health implications underscore the necessity for an improved understanding of NSSI (13).
The need for further research on NSSI was formally emphasized with the inclusion of NSSI disorder (NSSI-D) as a “condition requiring further research” in Section III of DSM-5 (14). The newly proposed disorder included six provisional diagnostic criteria (14). First, criterion A specifies that NSSI has to occur for at least 5 days in the past 12 months. Second, criterion B states that the individual must engage in NSSI for one or more of these reasons: to relieve negative thoughts or feelings (B1), to resolve interpersonal difficulties (B2), or to induce a positive state (B3). Third, criterion C indicates that NSSI must be preceded by either negative thoughts or feelings (C1a), conflicts with others (C1b), preoccupation with the behavior that is difficult to resist (C2), or recurrent thoughts about the behavior (C3). Finally, socially acceptable behaviors are excluded (criterion D), the behavior must cause significant distress or interference in the individual's daily life (criterion E), and should not occur solely in the context of another mental disorder (criterion F).
Although research on NSSI has mainly focused on adults and college students, adolescents seem to be particularly at-risk for an NSSI-D diagnosis (3). Based on the limited available data, it has been estimated that 5.6–7.6% of adolescents are eligible for an NSSI-D diagnosis in community samples, compared to 0.2–3% of (young) adults (15–17). Moreover, it has been found that 37.7% of community adolescents with a lifetime history of NSSI meet all six NSSI-D criteria (17). In most studies, the diagnosis was more common in girls than in boys (16). These results may be subject to change, as discussion regarding the exact formulation and clinical relevance of some of the diagnostic criteria and NSSI-D as a separate disorder is still ongoing (17–20). For instance, a recent study suggested that the NSSI-D frequency cut-off should be raised from 5 days to at least 10 days in the past year to clinically meaningful (21, 22). However, a review of 16 empirical studies using the current DSM-5 criteria already found preliminary support for a distinct NSSI-D diagnosis, independent of other closely related mental disorders (16). For instance, in one of the reviewed studies, 80% of adolescents who met the current NSSI-D criteria did not meet criteria for Borderline Personality Disorder (BPD), thus indicating that NSSI-D can occur independently of BPD (23, 24). The distinction between NSSI(-D) and BPD is particularly relevant because NSSI has been historically intertwined with BPD as a prototypical symptom of the disorder (11). More specifically, before the release of DSM-5, NSSI was only mentioned in the DSM as a criterion for BPD.
Borderline Personality Disorder
BPD is a severe mental disorder that is generally typified by four core features: affective instability, identity problems, negative or unstable interpersonal relationships, and impulsivity or recurrent self-harm (14). Individuals diagnosed with BPD tend to experience strong emotions and can be particularly sensitive to rejection (25), they are more likely to suffer from severe psychosocial impairment such as intense conflict and tumultuous relationships (26), and show high mortality rates due to suicide, with up to 10% of BPD patients committing suicide (27). Epidemiological studies have shown that BPD prevalence rates peak in late adolescence and range from 2 to 3.2% in community adolescents (28, 29), 11% in adolescent outpatients, and 33–49% in adolescent inpatients (30–32). In community samples, most studies suggest an equal prevalence in adolescent boys and girls (28, 33). In clinical samples, prevalence rates are typically cited as higher among girls than boys, although it has been argued that this might be an artifact of sampling or diagnostic biases (34, 35). Importantly, adolescents with BPD are more likely than adults to show “acute” BPD symptoms, such as suicidal ideation and recurrent NSSI (36). Around 61% of adolescents with BPD pathology have engaged in NSSI at least once, making “recurrent NSSI and suicidal behavior” the most commonly met diagnostic criterion for BPD in adolescence (34, 37). In this young at-risk age group, the comorbidity between BPD and NSSI is complex (38). For instance, displaying BPD symptoms indicates greater severity of NSSI based on several parameters (36) such as a younger age of NSSI onset (37, 39), more frequent NSSI episodes (40), and a higher likelihood of repetitive NSSI (41). NSSI in adolescence is considered a key precursor for, or even indicator of, BPD, especially when repetitive and long-lasting NSSI is present (42). Severity of NSSI (i.e., earlier age of onset and longer duration of the behavior) is a risk factor for later BPD (43). On the other hand, the majority of adolescents engaging in NSSI do not meet the criteria for BPD (44, 45). To improve our understanding of comorbidity, the field could benefit from adopting a symptom-level approach of the comorbidity between NSSI-D and BPD. This could clarify whether or not NSSI-D and BPD symptoms cluster together and, most importantly, detect which symptoms drive the high co-occurrence between both diagnoses. Network theory offers a compelling new direction because of its clear symptom-level conceptualization of comorbidity and its statistical tools to model and visualize the approach (46).
Network Theory as an Innovative View on Comorbidity of Mental Disorders
In 2013, Borsboom and Cramer introduced network theory, a conceptual framework asserting that mental disorders are networks of symptoms influencing each other, rather than symptom sets being caused by an underlying disease entity (47). The network theory innovated analysis of comorbidity (48), because it states that a symptom can directly activate one or more symptoms in other disorder's network, which thus links disorders to each other without the assumption of a latent comorbidity factor. The accompanying statistical technique, network analysis, allows researchers to model and visualize these symptom associations to illuminate the nosology and comorbidity of mental disorders (47).
In network analysis, the graphical output represents each symptom by a node. Nodes that tend to co-occur in the data are joined together by connecting edges, which results in a web-like constellation or network (47). If a group of nodes cluster more strongly among each other than with other nodes, that group is defined as a community (49, 50). A community structure analysis therefore offers an innovative way of detecting whether or not the symptoms in a network form statistically discernible symptom clusters (i.e., in our study, an NSSI-D community and a BPD community). Interestingly, certain edges can bridge two disorders by running from a node belonging to one theoretically defined cluster (e.g., NSSI-D) to a node belonging to another cluster (e.g., BPD). These between-cluster nodes are aptly referred to as bridge symptoms (46). Bridge symptoms are powerful tools in studying comorbidity, as they provide valuable information regarding the spread of activation between disorders. Specifically, the presence of an identified bridge symptom might indicate a heightened risk for the onset of an additional disorder, or, if both disorders are already present, the bridge symptom might play a role in maintaining the spread of activation between them (51). Albeit connections in networks do not necessarily reflect causal structures, edges can be indicative of potential mutual or directed causal relationships (52, 53). If this is the case, “deactivating” a bridge symptom, for instance by intervention or medication, could be regarded as cutting a crucial connection between comorbid disorders. In other words, successfully treating a bridge symptom could result in a decrease in symptom-level associations both within- and between-disorders (46, 51). Up until recently, researchers had to rely on subjective visual inspection of a network to detect bridge symptoms (46). However, in 2019 Jones et al. developed and validated a quantitative index to identify bridge symptoms and to measure their centrality between theoretically defined clusters.
Research Aims and Hypotheses
Embracing these state-of-the-art techniques, the aim of the present study was fourfold: (1) describe prevalence rates of (the comorbidity between) NSSI-D and BPD symptomatology, (2) investigate whether or not NSSI-D and BPD can be distinguished from one another in a network structure, (3) explore potential gender differences in (the comorbidity of) the NSSI-D and BPD network, and (4) identify specific bridge symptoms through which pathology is most likely to spread between NSSI-D and BPD symptom clusters. First, concerning prevalence rates, we tentatively hypothesized that the percentage of individuals scoring above the BPD cut-off in the current sample (i.e., community adolescents engaging in NSSI) would be between percentages found in community adolescents [i.e., 2–3.2%, (28, 29)] and in adolescent outpatients [i.e., 11%, (30)]. Concerning the second research aim, we hypothesized based on a review of the empirical NSSI-D literature (16) that NSSI-D and BPD symptoms (nodes) would split into at least two statistically discernible communities without symptoms from NSSI-D belonging to the BPD community or vice versa. Regarding the third research aim, we expected more girls than boys to be eligible for an NSSI-D diagnosis (16), but we did not expect gender differences in the percentage of boys and girls scoring above the BPD cut-off in this sample (28, 33). To the best of our knowledge, no research is currently available on gender differences in the comorbidity between BPD and NSSI-D symptomatology. Lastly, as no previous research is currently available on potential bridge symptoms between NSSI-D and BPD, no specific hypotheses could be formulated.
Materials and Methods
Procedure
The current study is part of a research project in which eight secondary schools took part, all located in Flanders, Belgium (17). Across all eight schools, we contacted the parents of 3,483 students and distributed informed consent forms among them. A total of 2,313 (66.4%) students received active parental consent and were subsequently invited to partake in the study. The 2,162 (93.5%) students who agreed to participate received an assent form, a questionnaire booklet, and an envelope. The data collection took place during school hours, with the researchers present at all time. After signing the assent form and filling out all questionnaires, the students returned these documents in a sealed envelope to the researchers. Students who were absent on the day of assessment were contacted by e-mail to complete an online version of the study. All participants received a movie ticket as compensation, as well as a letter with contact details of the school counselor and several mental health services. The study was approved by the Ethics Committee at the University of Leuven.
Participants
Out of the 2,162 participating students, we selected only those who reported having ever engaged in NSSI (i.e., “I have at least once engaged in self-injury without the intent to die”) and who completed the BPD questionnaire. This resulted in a final sample of 347 students (78.4% female) between the ages of 12 and 20 (M = 15.05, SD = 1.83). The vast majority of students identified as Belgian (93.1%). About half of the students lived with both parents (53.0%, n = 184), the remaining students had divorced parents and/or lived in a blended family (40.4%, n = 132) or indicated to have another home environment (9%, n = 31).
Measures
Non-suicidal Self-Injury Disorder
Lifetime NSSI was assessed using the single-item screening measure “Have you ever engaged in self-injury without an intent to die?” Those who answered affirmatively responded to follow-up questions regarding frequency and recency of NSSI, current NSSI, age of NSSI onset, and different NSSI behaviors (i.e., scratching, carving, cutting, burning, rubbing the skin, self-hitting, pricking/piercing the skin, and banging the head). Additionally, a set of questions assessing DSM-5 criteria for NSSI-D was included. We used questions that explicitly assessed all NSSI-D criteria (A, B, C, D, E, and F), with the wording of these items matching the DSM-5 criteria as closely as possible [see Buelens et al. (17) for an overview of the exact questions]. Furthermore, since previous research indicated that criterion C1 contains two elements that are considerably different from each other (17), we additionally split criterion C1 into C1a (negative feelings or thoughts) and C1b (conflicts with others) to assess this symptom more accurately. We used a dichotomous approach when describing prevalence rates [i.e., fulfilling (1) or not fulfilling (0) the criterion], while we used the continuous scores on each criterion in the network analyses. For all DSM-5 criteria together, a KR-20 reliability coefficient of 0.667 was found, which is close to the 0.7 cut-off for acceptable internal consistency (54).
Borderline Personality Disorder Symptomatology
The brief Borderline Personality Features Scale for Children [BPFSC-11; (55)] was used to assess BPD symptomatology. The questionnaire consists of 11 items scored on a 5-point Likert scale ranging from 0 (never true for me) to 4 (always true for me) and results in a unidimensional sum score ranging from 0 to 44 or mean score ranging from 0 to 4 (56). A higher mean score indicates more BPD symptomatology. The BPFSC-11 had a Cronbach's alpha of 0.79 in the current study, which is comparable to previous research (56). Next to the continuous mean score, we created a dichotomous cut-off score (1 = above the BPD cut-off, 0 = below the BPD cut-off) as recommended by previous sensitivity and specificity analyses on the BPFSC-11, which indicated the ideal cut-off value to be 34 out of the maximum sum score of 44 (55). We used the dichotomous score when describing percentages of adolescents scoring above and below the cut-off, while we used the continuous BPD score in the network analyses. The BPFSC-11 does not include items assessing NSSI.
Statistical Analyses
To address the first research aim, we used SPSS version 26 (57) to conduct descriptive analyses and compute prevalence rates of (the comorbidity between) NSSI-D and BPD symptoms. Research aims two to four were addressed using R (58) to conduct network analyses. For these analyses, participants who had six or more missing values were removed (n = 10) and the remaining 22 missing values out of the 7,751 datapoints were imputed using the mice R package (59).
As the second research aim was to investigate whether or not NSSI-D and BPD would occur as statistically discernible clusters of symptoms (nodes), we modeled a weighted, undirected graphical LASSO network using qgraph (60). We used the Extended Bayesian Information Criterion (EBIC), with the γ hyperparameter at 0.25, to set the amount of LASSO regularization (61). We then conducted a community structure analysis using the Walktrap algorithm, as implemented in the igraph R package (62, 63). Expected influence (EI) was used as a centrality measure, as it accounts for the presence of potential negative edges in the network by not taking the absolute value of edges before summing them (46, 64). The robustness (accuracy and stability) was tested by the bootstrapping procedure in the bootnet R package (65, 66). This procedure estimates a 95% confidence interval around the edges to estimate accuracy and provides a correlation-stability (CS) coefficient to assess whether or not the centrality indices (e.g., EI) are stable enough to be interpreted (65, 66). Namely, the CS-coefficient represents the proportion of participants that can be removed from the sample in case-dropping bootstrap resamples, such that the resulting EI indices have a 95% probability to correlate ≥ 0.7 with the original EI index (65). As a rule of thumb, a CS-coefficient below 0.25 indicates insufficient stability and warns against interpreting the centrality indices. A CS-coefficient above 0.50 indicates good stability (66).
To address the third research aim concerning potential gender differences in the network, we used the Network Comparison Test (NCT, γ = 0.25) from the NetworkComparisonTest R package (67) to investigate if the network structure and global strength were significantly different between boys and girls in the sample. The NCT allows us to assess the difference between the male and the female network based on network invariance, global strength invariance, edge invariance and centrality invariance.
Finally, to reach the fourth research aim, we used the networktools R package (68) to detect bridge symptoms between NSSI-D and BPD. As we were interested in the comorbidity between these two disorders, we specified to the network model which symptoms belonged to NSSI-D and which symptoms belonged to BPD. We then used bridge EI as a centrality measure to indicate which symptoms operate as bridges between the two theoretically defined symptom sets (64). We computed the CS-coefficient for bridge EI using the same case-dropping bootstrap resample as described above.
Results
Descriptive Statistics
Non-suicidal Self-Injury
At the moment of assessment, 4.6% (n = 16) of participants reported having engaged in NSSI that same day and/or the day before, 8.9% (n = 31) reported having engaged in NSSI a couple of days ago, 11.8% (n = 41) a week ago, 11.5% (n = 40) a month ago, 35.2% (n = 122) several months ago, and 27.1% (n = 94) reported having engaged in NSSI over a year ago. Three participants did not answer this question. A total of 20.7% (n = 72) of the participants described themselves as “currently engaging in NSSI.” The most common methods of NSSI were cutting and carving one's own skin, with 53.0% (n = 184) and 51.0% (n = 177) of the sample indicating that they engaged in these behaviors at least once. The other behaviors were hitting (30.8%, n = 107), scratching (26.5%, n = 92), head banging (25.4%, n = 88), pricking/piercing (23.1%, n = 80), rubbing (11.8%, n = 41), and burning the skin (8.4%, n = 29). The mean age of NSSI onset was 12.87 years (SD = 2.03), which did not significantly differ between boys (Mage = 12.76, SD = 2.23) and girls [Mage = 12.90, SD = 1.98; F(1, 332) = 1.456, p = 0.619].
Non-suicidal Self-Injury Disorder
Buelens et al. (17) provides more details on the diagnostic NSSI-D criteria in this sample. In short, a total of 37.8% (n = 131) of the participants adhered to all DSM-5 criteria for NSSI-D, whereas 59.9% (n = 208) was at least one criterion short of being eligible for an NSSI-D diagnosis. 2.3% (n = 8) of participants could not be classified on absence of presence of NSSI-D due to missing data on the NSSI-D criteria. When considered dichotomously, criterion A was met by 51.6% of the sample, criterion B by 86.9%, criterion C by 97.9%, criterion D by 100%, criterion E by 78.6%, and criterion F by 99.1% of the sample. Significantly more girls were eligible for an NSSI-D diagnosis (n = 111 out of 265 girls, 41.89%) compared boys (n = 20 out of 74 boys, 27.03%) according to the assessed DSM-5 criteria [X2(1) = 5.39, p = 0.020].
Borderline Personality Disorder
The mean score for BPD symptomatology was 2.16 (SD = 0.66) and was significantly higher for girls (M = 2.22, SD = 0.64) than boys [M = 1.95, SD =0.70; F(1, 344) = 1.30, p = 0.002]. There was no significant effect of age [F(8, 337) = 0.709, p = 0.684] on the mean score for BPD symptomatology. We additionally performed analyses using the dichotomous cut-off variable (1 = above the BPD cut-off, 0 = below the BPD cut-off). A total of 6.6% (n = 23) of the sample scored above the BPD cut-off, 93.1% (n = 323) scored below the cut-off, and 0.3% (n = 1) could not be classified due to missing data. Although a higher percentage of girls (n = 21 out of 271 girls, 7.75%) scored above the BPD cut-off compared to boys (n = 2 out of 75 boys, 2.67%), this difference did not reach statistical significance [X2 (1) = 2.45, p = 0.118].
Comorbidity
In the cross tabulation of NSSI-D and BPD (Table 1), all adjusted standardized residuals exceeded |2|, indicating significant discrepancies between the observed and expected frequencies. Out of the 23 participants who scored above the BPD cut-off, 60.87% (n = 14) met the NSSI-D diagnosis as well, the remaining 39.13% (n = 9) did not meet the criteria for an NSSI-D diagnosis. Out of the 131 participants who met the NSSI-D diagnosis, 10.68% (n = 14) scored above the BPD cut-off as well, while 89.31% (n = 117) scored below the BPD cut-off. These differences were statistically significant [X2 (1) = 5.08, p = 0.024], with a higher probability to observe NSSI-D in the BPD group.
Table 1.
Cross tabulation of NSSI-D and BPD.
| BPD | No BPD | Total | |
|---|---|---|---|
| NSSI-D | 14 (2.3) | 117 (−2.3) | 131 |
| No NSSI-D | 9 (−2.3) | 198 (2.3) | 207 |
| Total | 23 | 315 |
NSSI-D, Non-suicidal self-injury disorder; BPD, Borderline personality disorder.
Adjusted standardized residuals are in parentheses.
Number of participants in this category are in bold.
Table 2 shows the Pearson correlations between all NSSI-D criteria and all BPD symptoms.
Table 2.
Correlation coefficients between all study variables.
| Strong | Back | Miss | Leave | Change | Lonely | Hurt | Letdown | Mean | Careless | Nothink | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 0.136* | 0.219** | 0.230** | 0.188** | 0.134* | 0.261** | 0.172** | 0.148** | 0.007 | 0.046 | 0.105 |
| B1 | 0.077 | 0.198** | 0.186** | 0.228** | 0.166** | 0.259** | 0.157** | 0.184** | 0.071 | 0.119* | 0.043 |
| B2 | 0.037 | 0.118* | 0.058 | 0.123* | 0.07 | 0.095 | 0.014 | 0.01 | 0.042 | 0.026 | 0.073 |
| B3 | 0.105 | 0.074 | 0.151** | 0.086 | 0.065 | 0.065 | 0.103 | 0.072 | 0.074 | 0.005 | 0.123* |
| C1a | 0.185** | 0.308** | 0.252** | 0.276** | 0.163** | 0.291** | 0.210** | 0.258** | 0.117* | 0.173** | 0.164** |
| C1b | 0.213** | 0.181** | 0.108* | 0.159** | 0.121* | 0.099 | 0.168** | 0.194** | 0.037 | 0.109* | 0.178** |
| C2 | 0.231** | 0.265** | 0.245** | 0.189** | 0.206** | 0.216** | 0.231** | 0.151** | 0.079 | 0.163** | 0.165** |
| C3 | 0.128* | 0.321** | 0.344** | 0.246** | 0.146** | 0.389** | 0.172** | 0.192** | −0.005 | 0.174** | 0.110* |
| E1 | 0.136* | 0.096 | 0.184** | 0.151** | 0.073 | 0.116* | 0.119* | 0.121* | 0.052 | 0.129* | 0.152** |
| E2 | 0.155** | 0.169** | 0.159** | 0.220** | 0.077 | 0.193** | 0.141** | 0.130* | 0.105 | 0.163** | 0.251** |
| E3 | 0.125* | 0.119* | 0.152** | 0.147** | 0.071 | 0.135* | 0.132* | 0.128* | 0.099 | 0.061 | 0.195** |
| E4 | 0.164** | 0.058 | 0.126* | 0.153** | 0.043 | 0.091 | 0.091 | 0.114* | 0.05 | 0.063 | 0.049 |
p < 0.05.
p < 0.01.
Significant correlations are marked in bold. For the full legend, see Figure 1.
Graphical Network Analysis
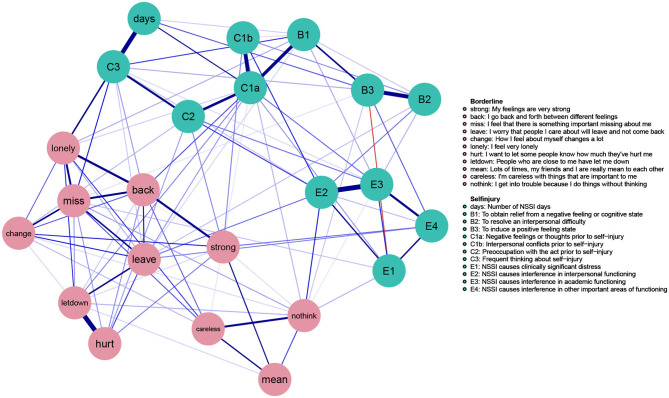
Figure 1 visualizes the EBIC gLASSO network (γ =0.25) based on the 12 NSSI-D items (in green) and the 11 BPD items (in pink). Positive regularized edges are depicted in blue, negative regularized edges are in red. The exact values of each edge, as well as the bootstrapped confidence intervals are reported in Supplementary Table 1. All 99 edges in this network were positive, with the exception of a small negative edge (−0.09) between B3 (I engage in NSSI to induce a positive feeling state) and E1 (NSSI causes clinically significant distress), a small negative edge (−0.02) between C1b (I engage in NSSI to obtain relief from a negative feeling of cognitive state) and B1 (interpersonal conflict takes place prior to NSSI), as well as a small edge (−0.01) between nodes lonely and strong. Regarding the stability of the centrality measures, the CS-coefficient as calculated by the case-dropping bootstrap resample was 0.65 for EI and 0.401 for bridge EI. Thus, the CS-coefficient for EI stayed above the desired 0.50 threshold and the coefficient for bridge EI remained well-above the lower limit of 0.25, making it justifiable to interpret EI results for this network (66), albeit with some caution in the case of bridge EI. Regarding overall EI, nodes C1a (negative feelings prior to NSSI) C3 (frequent thinking about NSSI), E2 (NSSI causes interference in interpersonal functioning), back (I go back and forth between different feelings), and miss (I feel that something important is missing about me) had the highest expected influence in the full network (see the second panel of Figure 3). These five symptoms thus had strong and numerous connections to other symptoms and acted as hubs connecting otherwise disparate symptoms to one another (46). The lowest EI was found for mean (lots of times, my friends and I are really mean to each other) and E1 (NSSI causes clinically significant distress), indicating that both symptoms operated in the periphery of the network, with few and/or weak connections to other symptoms (46).
Figure 1.
Full gLASSO network.
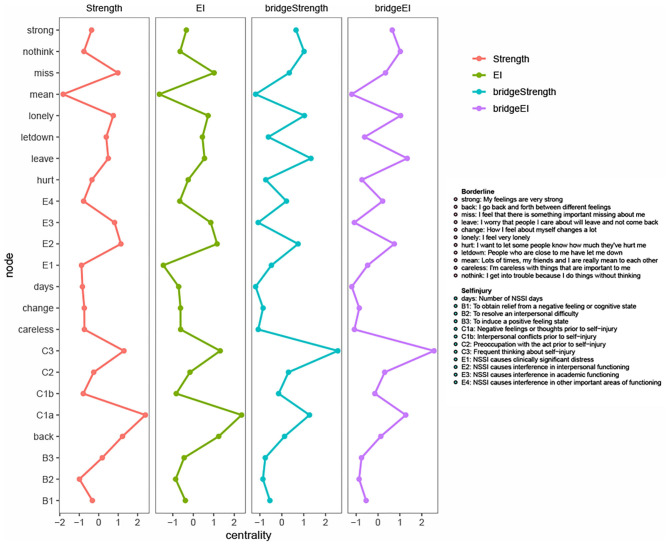
Figure 3.
(Bridge) strength and (bridge) expected influence. Centrality measures are visualized using standardized values to facilitate comparison. The x-axis represents standardized centrality values, the y-axis represents each node. The full definition of each node can be found in the legend. EI, expected influence.
Community Structure Analysis
Upon visual inspection (Figure 1), the NSSI-D items clearly clustered together at the top half of the network while the BPD items clustered together at the lower half of the network. Even though both sets of symptoms were substantially interrelated with each other, no NSSI-D symptoms were nested within the group of BPD symptoms or vice versa.
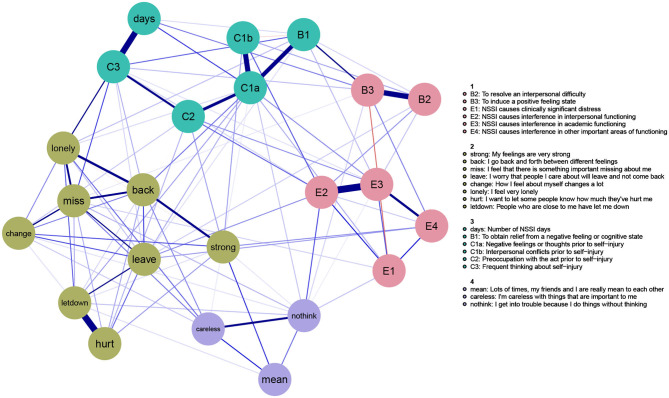
The results of the community structure analysis (Figure 2) corroborated this visual interpretation of the network. Namely, our results showed two communities consisting exclusively of NSSI-D symptoms and two communities consisting exclusively of BPD symptoms, without any overlap (i.e., no NSSI-D symptoms were part of a BPD community or vice versa). For NSSI-D, the E-criteria [NSSI causes clinical (E1), interpersonal (E2), academic (E3), other (E4) distress], and two of the B-criteria [engaging in NSSI to resolve interpersonal difficulties (B2) or to induce a positive state (B3)] formed one community (see Figure 2, depicted in pink). The remaining criteria [engaging in NSSI to relieve negative feelings/thoughts (B1); number of NSSI days (A, days); negative feelings (C1a), conflicts (C1b), preoccupation with NSSI (C2), and frequent thinking about NSSI (C3)] constituted the third NSSI-D community (depicted in blue). Regarding BPD, the impulsivity symptoms (I'm careless with things that are important to me (Careless) and I get into trouble because I do things without thinking (nothink) grouped together with my friends and I are really mean to each other (mean) into the first BPD community (depicted in purple). The second BPD community (depicted in green) consisted of the remaining BPD symptoms.
Figure 2.
Community structure gLASSO network.
Gender Differences in the Network
The network invariance test indicated no significant differences in network structure (M = 0.46, p = 0.215) and no significant differences between girls and boys in global strength across networks (girls: 9.23, boys: 0, s = 9.23, p = 0.243). However, these results should be interpreted cautiously, as the lack of a significant gender differences might be a result of low power due to the small number of boys in our sample (21.6%, n = 75).
Bridge Symptoms
Figure 3 summarizes the standardized centrality measures for each of the 23 symptoms included in the network. For the sake of completeness, we included both strength centrality and expected influence (EI). However, because of the small proportion of negative edges in the network, strength centrality and EI were nearly identical for the overall measures (rstrngxEI = 0.98) and exactly identical for the bridge measures (rstrngxEI = 1), because all negative edges connected nodes within the same cluster. Importantly however, as the CS-coefficient for bridge EI was below the 0.50 threshold, the results below should be interpreted with some caution.
The highest bridge EI was found for C1a (negative feelings or thoughts prior to NSSI), C3 (frequent thinking about NSSI), leave (I worry that people I care about will leave and not come back), lonely (I feel very lonely), and nothink (I get into trouble because I do things without thinking). This could indicate that these five nodes might have many and/or strong inter-cluster edges bridging the theoretically defined clusters of NSSI-D and BPD symptoms. The lowest bridge EI was found for days (number of NSSI days), E4 (NSSI causes interference in other important areas of functioning), mean (my friends and I are really mean to each other) and careless (I'm careless with things that are important to me). This might indicate that these four nodes did not play a significant role in connecting NSSI-D and BPD symptoms. This could either be due to overall low EI (as is the case for mean), or to being mainly connected to nodes within the same cluster (as is the case for careless in the BPD cluster and E4 and days in the NSSI-D cluster). The latter could indicate that these symptoms are potentially less relevant in the comorbidity between NSSI-D and BPD, even though they could play a considerable role within each disorder.
Discussion
In 2013, DSM-5 urged for further research on NSSI-D and represented NSSI for the first time distinct from BPD (14). However, research on the comorbidity between NSSI-D and BPD symptoms is still scarce, especially in adolescent populations, where the symptoms of both disorders tend to be more acute and more prevalent than in adulthood (36). Therefore, the current study selected 347 adolescents who engaged at least once in NSSI to address four research aims regarding prevalence, comorbidity, gender differences, and bridge symptoms of NSSI-D and BPD.
First, our results showed that 6.6% in this specific sample (i.e., community adolescents with a history of NSSI) scored above the BPD cut-off, which turned out to be higher than the 2–3% previously found in community adolescents (28, 29), but lower than the 11% previously found in outpatient adolescents (30). Regarding the co-occurrence of BPD with NSSI-D, our results showed that 60.87% of adolescents who scored above the BPD cut-off were eligible for an NSSI-D diagnosis as well. To the best of our knowledge, the current study is the first to report the co-occurrence of BPD with NSSI-D in community adolescents. Previous research, however, did already indicate that out of those adolescents who presented with BPD symptomatology, 61% had at least once engaged in NSSI (34, 37). Considering the reverse direction (i.e., the co-occurrence of NSSI-D with BPD), our results showed that 37.14% of adolescents eligible for NSSI-D scored above the BPD cut-off as well. This percentage is just below the 44.4% reported recently by Zetterqvist et al. (69). The slight difference might be due to the fact that our study investigated community adolescents, whereas Zetterqvist et al. studied adolescent outpatients.
Second, to investigate comorbidity in more detail, we modeled the symptoms of NSSI-D and BPD together in one network of inter-symptom relations. The network showed how NSSI-D and BPD symptoms were closely interrelated, with a total of 98 connections running to and from the 23 symptoms included in the network. Despite this interconnectedness, a community structure analysis revealed that NSSI-D and BPD symptoms reliably split into separate communities, where no symptoms from NSSI-D ended up in the BPD community nor vice versa. These results confirm earlier research, which found NSSI-D to occur both together with and independently of BPD (16, 69). As a previous study showed that the overlap between BPD and NSSI-D is similar to the overlap between BPD and other disorders (24), these findings seem to strengthen the validity of distinct, yet related diagnoses (24, 69). Two additional findings emerged from the community structure analysis regarding the clustering of symptoms within NSSI-D. First, criterion B1 (engaging in NSSI to relieve negative feelings/thoughts) did not group together with the other B-criteria, but rather formed a community with the A-criterion (number of NSSI days) and C-criteria [i.e., negative feelings (C1a), conflicts (C1b), preoccupation with NSSI (C2), and frequent thinking about NSSI (C3)]. This could be due to the particularly strong edge connecting engaging in NSSI to relieve negative feelings/thoughts (B1) and experiencing negative thoughts/feelings prior to NSSI (C1a), which reflects previous research with this sample reporting an almost complete overlap of B1 with C1a (17). Second, criterion A (the number of days one engaged in NSSI in the last year) showed relatively low EI and very low bridge EI. This is likely due to the strong connection of criterion A with C3 (frequent thinking about NSSI, even when it is not acted upon): the variance in the number of days seems to be explained to a large extent by the thoughts one has regarding NSSI.
Third, we investigated potential gender differences in (the comorbidity of) NSSI-D and BPD symptoms. Confirming our hypotheses based on previous literature (16, 28, 33), the current study found significantly more girls than boys being eligible for an NSSI-D diagnosis, but no significant gender difference in the BPD cut-off. Moreover, our results showed no significant gender differences in the network of NSSI-D and BPD symptoms. This could indicate that the overall comorbidity structure of NSSI-D and BPD, as well as the strength of the connections between the symptoms, remains alike for boys and girls in a community sample. Thus, even though girls are more likely to meet the NSSI-D criteria, our results tentatively suggest that the manner in which NSSI-D and BPD symptoms are interconnected does not differ between girls and boys. Importantly however, the lack of a significant gender differences in the current study could also be ascribed to the particularly small number of males in our sample.
Fourth, the current study identified the five bridge symptoms through which pathology was most likely to spread to or from NSSI-D and BPD symptoms: negative feelings/thoughts prior to NSSI (C1a), frequent thinking about NSSI (C3), separation anxiety (leave), loneliness (lonely), and impulsivity (nothink). The identification of bridge symptoms can clarify why comorbidities occur in some adolescents, but not in others (70). For instance, our results showed I feel very lonely (lonely) to be one of the five main bridge symptoms connecting BPD to NSSI-D symptoms (i.e., high bridge EI). If future research could replicate this finding, it could indicate that an adolescent who feels very lonely would be at greater risk for NSSI-D compared to an adolescent with equally severe BPD features, but who does not feel particularly lonely (70). Loneliness standing out as a potential bridge between BPD and NSSI-D symptoms is supported by earlier work, which reported elevated loneliness in NSSI (71, 72) and BPD (73–75), potentially due to the association of loneliness with depression as a comorbid diagnosis for NSSI and BPD (76). Moreover, previous studies suggested that being alone increases self-reflection (77) which, for at-risk adolescents, could trigger an emotional cascade of rumination, depressive feelings, and potentially NSSI (6).
Relatedly, our results showed that the BPD symptom I feel very lonely had its strongest connection to NSSI-D with frequent thinking about NSSI (C3), which in itself showed up as one of the five strongest bridge symptoms (i.e., high bridge EI). Thus, frequent thinking about NSSI (C3) potentially operates as an important gateway from NSSI-D to BPD. In addition, our results revealed how this symptom was highly influential -and sufficiently stable- in the overall network (i.e., high EI). In other words, frequent thinking about NSSI (C3) additionally acted as a central hub in the overall network, with strong and numerous connections to symptoms of both NSSI-D and BPD. Noteworthy, previous research has shown that teaching coping skills to reduce and resist frequent NSSI thoughts and urges is a key component of successful treatment for NSSI (78, 79).
Similarly, experiencing negative thoughts or feelings prior to engaging in NSSI (C1a) showed up as one of the five main bridge symptoms (i.e., high bridge EI) as well as one of the most influential symptoms in the overall network (i.e., high EI). This neatly aligns with previous research indicating that, on the one hand, engaging in NSSI to relieve negative thoughts and feelings is the most commonly reported function of NSSI (80, 81) and, on the other hand, adolescents with BPD features tend to report particularly strong negative emotions (25).
Finally, BPD symptoms I worry that people will leave and not come back (leave) and I get into trouble because I do things without thinking (nothink) showed a different pattern: unlike C1a and C3 these symptoms did not stand out in the overall network (i.e., they showed moderate EI), but they did come up as the final two main bridge symptoms (i.e., high bridge EI) connecting BPD to NSSI-D. These bridge symptoms, BPD symptoms referring to separation anxiety (leave) and impulsivity (nothink), thus could indicate that very anxious or very impulsive adolescents would be at greater risk for NSSI-D, compared to adolescents with equally severe BPD features, but who show less separation anxiety or are less impulsive. This finding extents previous research reporting that separation from parents before the age of 15 increases risk for NSSI and that, among all BPD features, impulsivity showed the strongest association with NSSI frequency (82).
The current study adhered to several recommendations stemming from the extensive discussion on network replicability (83, 84). We provided robustness checks (accuracy and stability) with a bootstrapping procedure and, where necessary, warranted against overinterpreting results with insufficient stability. Despite these precautions, our research was not without limitations. First, our sample size, relatively small considering the high statistical power necessary for these analyses, could have led to increased instability in the LASSO network. Particularly the small number of males in our sample, a common issue when researching both NSSI-D and BPD (34, 35), is likely to be the underlying reason for the insignificant gender differences in the network. Future research with larger sample sizes and more equal numbers of boys and girls should aim to replicate this analysis. Second, NSSI-D showed low internal consistency and measuring NSSI-D and BPD solely with self-report questionnaires is limited and could result in reporting bias (85). However, NSSI is typically secretive (86) and parents or teachers are often unaware of the adolescent's engagement in the behavior (87), which makes NSSI(-D) difficult to assess by other informants. Future research could embrace a multi-method approach and include diagnostic clinical interviews to allow for differential diagnostics and/or behavioral measures to assess NSSI-D and BPD more accurately. Third, our results might not be generalizable to clinical, particularly inpatient, samples. Fourth, both NSSI(-D) and BPD symptoms show high comorbidity with other diagnoses, such as major depressive disorder, substance use disorders, anxiety disorders, and eating disorders (76). Future research could aim to replicate our findings while additionally controlling for other diagnostic comorbidity. Finally, the cross-sectional nature of our data limits the conclusions that can be drawn. Future longitudinal research will allow us to make stronger assumptions regarding long-term symptom interactions and, noteworthy, directionality and causality. Namely, by using time-series data on a group level or on an individual level, specific nodes could be targeted by experimental manipulations to test for causality in the network (70).
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee at the University of Leuven (G-2017 01 755). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
TB was involved in the conception, design of the study, the acquisition, initial analysis, interpretation of the data, the drafting, and revisions of the manuscript. GC made substantial contributions to the analysis, interpretation of the data, and was involved in the revisions of the manuscript. KL and LC were involved in the funding acquisition, conception and design of the study, and revisions of the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Annabel Bogaerts, Kaat Buelens, Nina Palmeroni, Ine Triangl, Lotte Verboven, and Margaux Verschueren for their help with the data collection.
Footnotes
Funding. This research was funded by Fonds Wetenschappelijk Onderzoek (FWO, Belgium; grant number G062117N).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.580922/full#supplementary-material
References
- 1.International Society for the Study of Self-Injury What Is Self-Injury? (2018). Available online at: https://itriples.org/about-self-injury/what-is-self-injury (accessed July 07, 2020).
- 2.Klonsky ED, Victor SE, Saffer BY. Nonsuicidal self-injury: what we know, and what we need to know. Can J Psychiatry. (2014) 59:565–8. 10.1177/070674371405901101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life-Threatening Behav. (2014) 44:273–303. 10.1111/sltb.12070 [DOI] [PubMed] [Google Scholar]
- 4.Andrewes HE, Hulbert C, Cotton SM, Betts J, Chanen AM. Relationships between the frequency and severity of non-suicidal self-injury and suicide attempts in youth with borderline personality disorder. Early Intervent Psychiatry. (2019) 13:194–201. 10.1111/eip.12461 [DOI] [PubMed] [Google Scholar]
- 5.Brickman LJ, Ammerman BA, Look AE, Berman ME, McCloskey MS. The relationship between non-suicidal self-injury and borderline personality disorder symptoms in a college sample. Borderline Personality Disorder Emotion Dysregulation. (2014) 1:14. 10.1186/2051-6673-1-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buelens T, Luyckx K, Gandhi A, Kiekens G, Claes L. Non-suicidal self-injury in adolescence: longitudinal associations with psychological distress and rumination. J Abnormal Child Psychol. (2019) 47:1569–81. 10.1007/s10802-019-00531-8 [DOI] [PubMed] [Google Scholar]
- 7.Burke TA, Piccirillo ML, Moore-Berg SL, Alloy LB, Heimberg RG. The stigmatization of nonsuicidal self-injury. J Clin Psychol. (2019) 75:481–98. 10.1002/jclp.22713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moran P, Coffey C, Romaniuk H, Olsson C, Borschmann R, Carlin JB, et al. The natural history of self-harm from adolescence to young adulthood: a population-based cohort study. Lancet. (2012) 379:236–43. 10.1016/S0140-6736(11)61141-0 [DOI] [PubMed] [Google Scholar]
- 9.Nock MK, Joiner TE, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res. (2006) 144:65–72. 10.1016/j.psychres.2006.05.010 [DOI] [PubMed] [Google Scholar]
- 10.Cipriano A, Cella S, Cotrufo P. Nonsuicidal self-injury: a systematic review. Front Psychol. (2017) 8:1–14. 10.3389/fpsyg.2017.01946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Møhl B. Assessment and Treatment of Non-Suicidal Self-Injury. New York, NY: Routledge; (2019). 10.4324/9780429296352 [DOI] [Google Scholar]
- 12.Buelens T, Luyckx K, Verschueren M, Schoevaerts K, Dierckx E, Depestele L, et al. Temperament and character traits of female eating disorder patients with(out) non-suicidal self-injury. J Clin Med. (2020) 9:1207. 10.3390/jcm9041207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mullins-Sweatt SN, Lengel GJ, Grant DM. Non-suicidal self-injury: the contribution of general personality functioning. Personal Mental Health. (2013) 7:56–68. 10.1002/pmh.1211 [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders. 5th ed Washington, DC: American Psychiatric Association; 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- 15.Kiekens G, Hasking P, Claes L, Mortier P, Auerbach RP, Boyes M, et al. The DSM-5 nonsuicidal self-injury disorder among incoming college students: prevalence and associations with 12-months mental disorders and suicidal thoughts and behaviors. Depress Anxiety. (2018) 35:629–37. 10.1002/da.22754 [DOI] [PubMed] [Google Scholar]
- 16.Zetterqvist M. The DSM-5 diagnosis of nonsuicidal self-injury disorder: a review of the empirical literature. Child Adoles Psychiatry Mental Health. (2015) 9:31 10.1186/s13034-015-0062-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buelens T, Luyckx K, Kiekens G, Gandhi A, Muehlenkamp JJ, Claes L. Investigating the DSM-5 criteria for non-suicidal self-injury disorder in a community sample of adolescents. J Affect Disord. (2020) 260:314–22. 10.1016/j.jad.2019.09.009 [DOI] [PubMed] [Google Scholar]
- 18.Ammerman BA, Jacobucci R, McCloskey MS. Reconsidering important outcomes of the nonsuicidal self-injury disorder diagnostic criterion A. J Clin Psychol. (2019) 75:1084–97. 10.1002/jclp.22754 [DOI] [PubMed] [Google Scholar]
- 19.Brausch AM, Muehlenkamp JJ, Washburn JJ. Nonsuicidal self-injury disorder: does Criterion B add diagnostic utility? Psychiatry Res. (2016) 244:179–84. 10.1016/j.psychres.2016.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghinea D, Edinger A, Parzer P, Koenig J, Resch F, Kaess M. Non-suicidal self-injury disorder as a stand-alone diagnosis in a consecutive help-seeking sample of adolescents. J Affect Disord. (2020) 274:1122–5. 10.1016/j.jad.2020.06.009 [DOI] [PubMed] [Google Scholar]
- 21.Ammerman BA, Jacobucci R, Kleiman EM, Muehlenkamp JJ, McCloskey MS. Development and validation of empirically derived frequency criteria for NSSI disorder using exploratory data mining. Psychol Assess. (2017) 29:221–31. 10.1037/pas0000334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muehlenkamp JJ, Brausch AM, Washburn JJ. How much is enough? J Consult Clin Psychol. (2017) 85:611–9. 10.1037/ccp0000209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.In-Albon T, Ruf C, Schmid M. Proposed diagnositic criteria for the DSM-5 of nonsuicidal self-injury in female adolescents: diagnostic and clinical correlates. Psychiatry J. (2013) 2013:159208. 10.1155/2013/159208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glenn CR, Klonsky ED. Nonsuicidal self-injury disorder: an empirical investigation in adolescent psychiatric patients. J Clin Child Adoles Psychol. (2015) 42:496–507. 10.1080/15374416.2013.794699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stiglmayr CE, Grathwol T, Linehan MM, Ihorst G, Fahrenberg J, Bohus M. Aversive tension in patients with borderline personality disorder: a computer-based controlled field study. Acta Psychiatr Scand. (2005) 111:372–9. 10.1111/j.1600-0447.2004.00466.x [DOI] [PubMed] [Google Scholar]
- 26.Lazarus SA, Cheavens JS, Festa F, Zachary Rosenthal M. Interpersonal functioning in borderline personality disorder: a systematic review of behavioral and laboratory-based assessments. Clin Psychol Rev. (2014) 34:193–205. 10.1016/j.cpr.2014.01.007 [DOI] [PubMed] [Google Scholar]
- 27.Homan KJ, Sim LA, Fargo JD, Twohig MP. Five-year prospective investigation of self-harm/suicide-related behaviors in the development of borderline personality disorder. Personal Disord. (2017) 8:183–8. 10.1037/per0000169 [DOI] [PubMed] [Google Scholar]
- 28.Zanarini MC, Horwood J, Wolke D, Waylen A, Fitzmaurice G, Grant BF. Prevalence of DSM-IV borderline personality disorder in two community samples: 6,330 English 11-year-olds and 34,653 American adults. J Personal Disord. (2011) 25:607–19. 10.1521/pedi.2011.25.5.607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leung S-W, Leung F. Construct validity and prevalence rate of borderline personality disorder among Chinese adolescents. J Personal Disord. (2009) 23:494–513. 10.1521/pedi.2009.23.5.494 [DOI] [PubMed] [Google Scholar]
- 30.Chanen AM, Jackson HJ, McGorry PD, Allot KA, Clarkson V, Yuen HP. Two-year stability of personality disorder in older adolescent outpatients. J Personal Disord. (2004) 18:526–41. 10.1521/pedi.18.6.526.54798 [DOI] [PubMed] [Google Scholar]
- 31.Ha C, Balderas JC, Zanarini MC, Oldham J, Sharp C. Psychiatric comorbidity in hospitalized adolescents with borderline personality disorder. J Clin Psychiatry. (2014) 75:e457–64. 10.4088/JCP.13m08696 [DOI] [PubMed] [Google Scholar]
- 32.Levy KN, Becker DF, Grilo CM, Mattanah JJF, Garnet KE, Quinlan DM, et al. Concurrent and predictive validity of the personality disorder diagnosis in adolescent inpatients. Am J Psychiatry. (1999) 156:1522–8. 10.1176/ajp.156.10.1522 [DOI] [PubMed] [Google Scholar]
- 33.Livesley WJ, Larstone R. Handbook of Personality Disorders: Theory, Research, and Treatment. 2nd edn. The Guildford Press; (2018). [Google Scholar]
- 34.Kaess M, Brunner R, Chanen A. Borderline personality disorder in adolescence. Pediatrics. (2014) 134:782–93. 10.1542/peds.2013-3677 [DOI] [PubMed] [Google Scholar]
- 35.Skodol AE, Bender DS. Why are women diagnosed borderline more than men? Psychiatric Quart. (2003) 74:349–60. 10.1023/A:1026087410516 [DOI] [PubMed] [Google Scholar]
- 36.Stead VE, Boylan K, Schmidt LA. Longitudinal associations between non-suicidal self-injury and borderline personality disorder in adolescents: a literature review. Borderline Personal Disord Emotion Dysregul. (2019) 6:1–12. 10.1186/s40479-019-0100-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zanarini MC, Frankenburg FR, Ridolfi ME, Jager-Hyman S, Hennen J, Gunderson JG. Reported childhood onset of self-mutilation among borderline patients. J Personal Disord. (2006) 20:9–15. 10.1521/pedi.2006.20.1.9 [DOI] [PubMed] [Google Scholar]
- 38.Hessels CJ, Laceulle OM, van Aken MAG, Resch F, Kaess M. Differentiating BPD in adolescents with NSSI disorder: the role of adverse childhood experiences and current social relationships. Borderline Personal Disord Emotion Dysregul. (2018) 5:1–11. 10.1186/s40479-018-0097-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klonsky ED, Olino TM. Identifying clinically distinct subgroups of self-injurers among young adults: a latent class analysis. J Consult Clin Psychol. (2008) 76:22–7. 10.1037/0022-006X.76.1.22 [DOI] [PubMed] [Google Scholar]
- 40.Jacobson CM, Muehlenkamp JJ, Miller AL, Turner JB. Psychiatric impairment among adolescents engaging in different types of deliberate self-harm. J Clin Child Adoles Psychol. (2008) 37:363–75. 10.1080/15374410801955771 [DOI] [PubMed] [Google Scholar]
- 41.Muehlenkamp JJ, Ertelt TW, Miller AL, Claes L. Borderline personality symptoms differentiate non-suicidal and suicidal self-injury in ethnically diverse adolescent outpatients. J Child Psychol Psychiatry Allied Discipl. (2011) 52:148–55. 10.1111/j.1469-7610.2010.02305.x [DOI] [PubMed] [Google Scholar]
- 42.Nakar O, Brunner R, Schilling O, Chanen A, Fischer G, Parzer P, et al. Developmental trajectories of self-injurious behavior, suicidal behavior and substance misuse and their association with adolescent borderline personality pathology. J Affect Disord. (2016) 197:231–8. 10.1016/j.jad.2016.03.029 [DOI] [PubMed] [Google Scholar]
- 43.Groschwitz RC, Plener PL, Kaess M, Schumacher T, Stoehr R, Boege I. The situation of former adolescent self-injurers as young adults: a follow-up study. BMC Psychiatry. (2015) 15:1. 10.1186/s12888-015-0555-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chanen AM, Kaess M. Developmental pathways to borderline personality disorder. Curr Psychiatry Rep. (2012) 14:45–53. 10.1007/s11920-011-0242-y [DOI] [PubMed] [Google Scholar]
- 45.Chanen AM, Thompson K. Preventive strategies for borderline personality disorder in adolescents. Curr Treat Opt Psychiatry. (2014) 1:358–68. 10.1007/s40501-014-0029-y [DOI] [Google Scholar]
- 46.Jones PJ, Ma R, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res. (2019) 0:1–15. 10.1080/00273171.2019.1614898 [DOI] [PubMed] [Google Scholar]
- 47.Borsboom D, Cramer AOJ. Network analysis: an integrative approach to the structure of psychopathology. Ann Rev Clin Psychol. (2013) 9:91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- 48.Eaton NR. Latent variable and network models of comorbidity: toward an empirically derived nosology. Social Psychiatry Psychiatric Epidemiol. (2015) 50:845–9. 10.1007/s00127-015-1012-7 [DOI] [PubMed] [Google Scholar]
- 49.Kendler KS, Aggen SH, Flint J, Borsboom D, Fried EI. The centrality of DSM and non-DSM depressive symptoms in Han Chinese women with major depression. J Affect Disord.(2018) 227:739–44. 10.1016/j.jad.2017.11.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Newman MEJ, Girvan M. Finding and evaluating community structure in networks. Phys Rev E. (2004) 69:026113. 10.1103/PhysRevE.69.026113 [DOI] [PubMed] [Google Scholar]
- 51.Afzali MH, Sunderland M, Teesson M, Carragher N, Mills K, Slade T. A network approach to the comorbidity between posttraumatic stress disorder and major depressive disorder: the role of overlapping symptoms. J Affect Disord. (2017) 208:490–6. 10.1016/j.jad.2016.10.037 [DOI] [PubMed] [Google Scholar]
- 52.Costantini G, Perugini M. A framework for testing causality in personality research. Eur J Personality. (2018) 32:254–68. 10.1002/per.2150 [DOI] [Google Scholar]
- 53.Epskamp S, Waldorp LJ, Mõttus R, Borsboom D. The Gaussian graphical model in cross-sectional and time-series data. Multivariate Behav Res. (2018) 53:453–80. 10.1080/00273171.2018.1454823 [DOI] [PubMed] [Google Scholar]
- 54.Cortina JM. What is coefficient alpha? J Appl Psychol. (1993) 78:98–104. 10.1037/0021-9010.78.1.98 [DOI] [Google Scholar]
- 55.Sharp C, Steinberg L, Temple J, Newlin E. An 11-item measure to assess borderline traits in adolescents: refinement of the BPFSC using IRT. Personal Disord. (2014) 5:70–8. 10.1037/per0000057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fossati A, Sharp C, Borroni S, Somma A. Psychometric properties of the borderline personality features scale for children-11 (BPFSC-11) in a sample of Community Dwelling Italian Adolescents. Eur J Psychol Assess. (2019) 35:70–7. 10.1027/1015-5759/a000377 [DOI] [Google Scholar]
- 57.IBM Corp IBM SPSS Statistics for Windows. IBM Corp; (2019). [Google Scholar]
- 58.R core team R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; (2019). [Google Scholar]
- 59.van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Statist Softw. (2011) 45:i03 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 60.Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph : network visualizations of relationships in psychometric data. J Statist Softw. (2012) 48:i04 10.18637/jss.v048.i04 [DOI] [Google Scholar]
- 61.Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Method. (2018) 23:617–6. 10.1037/met0000167 [DOI] [PubMed] [Google Scholar]
- 62.Golino H, Christensen AP. EGAnet: Exploratory Graph Analysis—A Framework for Estimating the Number of Dimensions in Multivariate Data Using Network Psychometrics. (R Package Version 0.8.0). (2020). [Google Scholar]
- 63.Pons P, Latapy M. Computing communities in large networks using random walks. In Yolum, T. Güngör, F. Gürgen, Özturan C, editors. Computer and Information Sciences—ISCIS 2005. Heidelberg; Berlin: Springer; (2005). p. 84–293. 10.1007/11569596_31 [DOI] [Google Scholar]
- 64.Robinaugh DJ, Millner AJ, McNally RJ. Identifying highly influential nodes in the complicated grief network. J Abnormal Psychol. (2016) 125:747–57. 10.1037/abn0000181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Costantini G, Richetin J, Preti E, Casini E, Epskamp S, Perugini M. Stability and variability of personality networks. Personal Individual Differences. (2019) 136:68–78. 10.1016/j.paid.2017.06.011 [DOI] [Google Scholar]
- 66.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Method. (2018) 50:195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.van Borkulo CD, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, Borsboom D, et al. Comparing network structures on three aspects: a permutation test. Physiology. (2017) 34:38569 10.13140/RG.2.2.29455.38569 [DOI] [PubMed] [Google Scholar]
- 68.Jones PJ. Networktools: Tools for Identifying Important Nodes in Networks. (2020). [Google Scholar]
- 69.Zetterqvist M, Perini I, Mayo LM, Gustafsson PA. Nonsuicidal self-injury disorder in adolescents: clinical utility of the diagnosis using the clinical assessment of nonsuicidal self-injury disorder index. Front Psychiatry. (2020) 11:1–10. 10.3389/fpsyt.2020.00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jones PJ, Mair P, Riemann BC, Mugno BL, McNally RJ. A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. J Anxiety Disord. (2018) 53:1–8. 10.1016/j.janxdis.2017.09.008 [DOI] [PubMed] [Google Scholar]
- 71.Gandhi A, Luyckx K, Goossens L, Maitra S, Claes L. Association between non-suicidal self-injury, parents and peers related loneliness, and attitude towards aloneness in flemish adolescents: an empirical note. Psychol Belgica. (2018) 58:3–12. 10.5334/pb.385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang Q, Wang H, Liu X. Loneliness, non-suicidal self-injury, and friendship quality among Chinese left-behind adolescents: the role of parent-child cohesion. J Affect Disord. (2020) 271:193–200. 10.1016/j.jad.2020.03.112 [DOI] [PubMed] [Google Scholar]
- 73.Liebke L, Bungert M, Thome J, Hauschild S, Gescher DM, Schmahl C, et al. Loneliness, social networks, and social functioning in borderline personality disorder. Personal Disord. (2017) 8:349–56. 10.1037/per0000208 [DOI] [PubMed] [Google Scholar]
- 74.Pucker HE, Temes CM, Zanarini MC. Description and prediction of social isolation in borderline patients over 20 years of prospective follow-up. Personal Disord. (2019) 10:383–8. 10.1037/per0000337 [DOI] [PubMed] [Google Scholar]
- 75.Zanarini MC, Frankenburg FR, Reich DB, Silk KR, Hudson JI, McSweeney LB. The subsyndromal phenomenology of borderline personality disorder: a 10-year follow-up study. Am J Psychiatry. (2007) 164:929–35. 10.1176/ajp.2007.164.6.929 [DOI] [PubMed] [Google Scholar]
- 76.Turner BJ, Dixon-Gordon KL, Austin SB, Rodriguez MA, Zachary Rosenthal M, Chapman AL. Non-suicidal self-injury with and without borderline personality disorder: differences in self-injury and diagnostic comorbidity. Psychiatry Res. (2015) 230:28–35. 10.1016/j.psychres.2015.07.058 [DOI] [PubMed] [Google Scholar]
- 77.Goossens L. Affinity for aloneness in adolescence and preference for solitude in childhood: linking two research traditions. In: RJ Coplan, JC Bowker, editors. The Handbook of Solitude: Psychological Perspectives on Social Isolation, Social Withdrawal, and Being Alone. Malden, MA: Wiley Blackwell; (2014). p. 150–66. 10.1002/9781118427378.ch9 [DOI] [Google Scholar]
- 78.Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder. JAMA Psychiatry. (2015) 72:475. 10.1001/jamapsychiatry.2014.3039 [DOI] [PubMed] [Google Scholar]
- 79.Turner BJ, Austin SB, Chapman AL. Treating nonsuicidal self-injury: a systematic review of psychological and pharmacological interventions. Can J Psychiatry. (2014) 59:576–85. 10.1177/070674371405901103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nock MK, Cha C. Psychological models of non-suicidal self-injury. In: Nock MK, editor. Understanding Non-suicidal Self-Injury: Origins, Assessment and Treatment. Washington, DC: American Psychological Association; (2009). p. 65–77. 10.1037/11875-000 [DOI] [Google Scholar]
- 81.Nock MK, Favazza AR. Nonsuicidal self-injury: definition and classification. In: Nock MK, editor. Understanding Nonsuicidal Self-Injury: Origins, Assessment, and Treatment. Washington, DC: American Psychological Association; (2009). p. 9–18. 10.1037/11875-001 [DOI] [Google Scholar]
- 82.You J, Leung F, Lai CM, Fu K. The associations between non-suicidal self-injury and borderline personality disorder features among Chinese adolescents. J Personal Disord. (2012) 26:226–37. 10.1521/pedi.2012.26.2.226 [DOI] [PubMed] [Google Scholar]
- 83.Borsboom D, Fried EI, Epskamp S, Waldorp LJ, van Borkulo CD, van der Maas HLJ, et al. False alarm? A comprehensive reanalysis of “evidence that psychopathology symptom networks have limited replicability” by Forbes, Wright, Markon, and Krueger (2017). J Abnormal Psychol. (2017) 126:989–99. 10.1037/abn0000306 [DOI] [PubMed] [Google Scholar]
- 84.Forbes MK, Wright AGC, Markon KE, Krueger RF. Evidence that psychopathology symptom networks have limited replicability. J Abnormal Psychol. (2017) 126:969–88. 10.1037/abn0000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Podsakoff PM, MacKenzie SB, Lee J-Y, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- 86.Baetens I, Claes L, Muehlenkamp J, Grietens H, Onghena P. Non-suicidal and suicidal self-injurious behavior among flemish adolescents: a web-survey. Archiv Suicide Res. (2011) 15:56–67. 10.1080/13811118.2011.540467 [DOI] [PubMed] [Google Scholar]
- 87.Baetens I, Claes L, Onghena P, Grietens H, Van Leeuwen K, Pieters C, et al. The effects of nonsuicidal self-injury on parenting behaviors: a longitudinal analyses of the perspective of the parent. Child Adoles Psychiatry Mental Health. (2015) 9:2. 10.1186/s13034-015-0059-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.