Abstract
Background
Burnout among primary care clinicians (PCPs) is associated with negative health and productivity consequences. The Veterans Health Administration (VA) embedded mental health specialists and care managers in primary care to manage common psychiatric diseases. While challenging to implement, mental health integration is a team-based care model thought to improve clinician well-being.
Objective
To examine the relationships between PCP-reported burnout (and secondarily, job satisfaction) and mental health integration at provider and clinic levels
Design
Analysis of 286 cross-sectional surveys in 2012 (n = 171) and 2013 (n = 115)
Participants
210 PCPs in one VA region
Main Measures
Outcomes were PCP-reported burnout (Maslach Burnout Inventory emotional exhaustion subscale), and secondarily, job satisfaction. Two independent variables represented mental health integration: (1) PCP-specialty communication rating and (2) proportion of clinic patients who saw integrated specialists. Using multilevel regression models, we examined PCP-reported burnout (and job satisfaction) and mental health integration, adjusting for PCP characteristics (e.g., gender), PCP ratings of team functioning (communication, knowledge/skills, satisfaction), and organizational factors.
Key Results
On average, PCPs reported high burnout (29, range = 9–54) across all VA healthcare systems. In total, 46% of PCPs reported “very easy” communication with mental health; 9% of primary clinic patients had seen integrated specialists. Burnout was not significantly associated with mental health communication ratings (β coefficient = − 0.96, standard error [SE] = 1.29, p = 0.46), nor with proportion of clinic patients who saw integrated specialists (β = 0.02, SE = 0.11, p = 0.88). No associations were observed with job satisfaction either. Among study participants, PCPs with poor team functioning, as exhibited by low team communication ratings, reported high burnout (β = − 1.28, SE = 0.22, p < 0.001) and low job satisfaction (β = 0.12, SE = 0.02, p < 0.001).
Conclusions
As currently implemented, primary care and mental health integration did not appear to impact PCP-reported burnout, nor job satisfaction. More research is needed to explore care model variation among clinics in order to optimize implementation to enhance PCP well-being.
KEY WORDS: burnout, primary care, mental health, communication, veterans
INTRODUCTION
Burnout, or the sense of being overwhelmed and emotionally exhausted,1, 2 among the primary care workforce can be harmful for both patients and clinicians.3 National surveys have found that more than half of physicians reported at least one burnout symptom,4 and “frontline” VA specialties, especially those that provide primary care, were most severely affected.5 When primary care clinicians (PCPs) are unwell, patient care and healthcare system performance can be suboptimal6—consisting of reported medical errors,7 low quality of care,8 poor patient satisfaction,9 and low-functioning primary care teams.10, 11 Importantly, clinician burnout has the potential to lower job satisfaction and increase job turnover, which can be costly to health systems.12 Accordingly, there has been a call to address clinician well-being as part of a “quadruple aim” approach to optimize primary care delivery.13
Team-based care models have been implemented to improve patient outcomes, while also supporting clinician well-being.14 The Veterans Health Administration (VA) implemented two such models of primary care practices nationally to improve both the physical and mental healthcare of patients: (1) Primary Care Mental Health Integration15 and (2) Patient Aligned Care Team (patient-centered medical home).16 Mental health integration first began in 2007. Informed by evidence-based collaborative care models, embedded mental health specialists, care managers, and PCPs jointly manage common psychiatric disease in primary care. In 2010, patient-centered medical home implementation further supported the aim to care for most mild-to-moderate mental/behavioral health problems directly in primary care. One VA region used an evidence-based quality improvement approach to facilitate medical home adoption, which decreased face-to-face visits (increase non-face-to-face care),17 improved patient-provider communication,18 and reduced primary care workforce burnout over time.19
While many have studied the relationship between PCP burnout and patient-centered medical home implementation, few have examined the potential additional contributions of mental health integration. Primary care patients with psychiatric disease require comprehensive services to better accommodate their needs. Coordinating their needs among various specialties can be “difficult”20 and their overall costs of care to health systems can be high.21 As such, care models that aim to systematically integrate the physical location and clinical workflow of both specialties may improve communication, and thus make care coordination less overwhelming (i.e., induce less burnout), between primary care and mental health specialties. In fact, mental health integration has been found to be associated with greater patient22 and clinician satisfaction.23 One cross-sectional survey found that fully integrated care, when compared with care with minimal integration and colocation, was associated with some components of clinician burnout (higher personal accomplishment and lower depersonalization) but not emotional exhaustion.24
To our knowledge, no study has examined the dissemination and implementation of mental health integration over time and found an association with PCP-reported burnout, and ultimately job satisfaction. In particular, emotional exhaustion is important to monitor in PCPs because it manifests first before full burnout syndrome develops1, 2 and is tied to job dissatisfaction and turnover.25 In addition, we do not know if purported team-based care effects on clinician well-being are observed in both VA patient-centered medical home and mental health integration care models as synergistically implemented across healthcare systems. Using 2-year survey data obtained in one VA region, this study examined the relationships between PCP-reported burnout and mental health integration both at the provider level (PCP-rated communication with mental health specialty) and at the clinic level (level of engagement in mental health integration programs for each PCP clinic). Secondarily, we examined the association between mental health integration variables and PCP-reported job satisfaction. We hypothesized that high PCP ratings of mental health specialty communication and high clinic engagement with integrated care programs would be positively associated with job satisfaction, and inversely associated with burnout.
METHODS
Study Design and Participants
The VA implemented (1) Primary Care Mental Health Integration15 in 2007 and (2) Patient Aligned Care Team (patient-centered medical home)16 in 2010. The Veterans Assessment and Improvement Laboratory (VAIL) facilitated medical home implementation using evidence-based quality improvement methods across one southwest VA region.26 As part of its evaluation, the RAND Corporation administered the VAIL-Patient Centered Care Clinician Survey with approximately 130 items assessing PCP experiences with medical home implementation from November 30, 2011, to March 30, 2012 (wave 1, fiscal year [FY] 2012), and August 1, 2013, to January 15, 2014 (wave 2, FY2013).19 During each survey wave, all PCPs according to VA’s electronic Primary Care Management Module were invited to complete the surveys online or to request a mail version.
In this study, we examined 286 cross-sectional survey responses from 210 PCPs in 17 clinics within four Southern California healthcare systems (FY2012 n = 171, response rate = 54%) (FY2013 n = 115, response rate = 48%). We did not include responses from PCPs in one healthcare system due to reorganizations in their mental health integration programs during our study period.
Dependent Variable
PCPs, that is physicians, nurse practitioners, or physician assistants, reported burnout symptoms via the Maslach Burnout Inventory (MBI), emotional exhaustion subscale2 (α = 0.86). The 9 items included statements such as “I feel emotionally drained from my work” and “I feel burned out from my work.” Six-point scale responses ranged from “never” (0) to “every day” (6) and has been categorized as low (0–18), medium (18–25), and high (27–54).27 To minimize participation burden, the survey did not include the full sub-scales for cynicism and professional efficacy. The survey also measured past month job satisfaction with a single item, “Overall, I am satisfied with my job,” rated on a 5-point Likert scale.
Two Key Independent Variables
First, we asked PCPs, “How easy is it for you to communicate [in person, by phone, or electronically] with the following types of health services providers?” This survey question was developed to understand PCP-specialist communication and has been compared with VA clinician interviews.28 While the response list included a variety of specialists, we examined only PCP-rated communication with “mental/behavioral health” specialists, which was found to be the highest of all specialties, presumably due to the availability of integrated care.28 Three-point Likert scale responses ranged from “very easy” (0) to “not at all easy” (3).
Second, for each PCP, we calculated his/her clinic’s engagement in PC-MHI programs, defined as the proportion of primary care patients who saw integrated mental health specialists during each fiscal year. It represents the reach of integrated care services in primary care clinics, is a performance metric used across the VA, and has been described in prior research.29, 30 We ascertained clinic patients who received PC-MHI services from nationally designated electronic PC-MHI encounter codes (534 and 539).
Covariates
Similar to a prior study,27 we controlled for the effect of team functioning on PCP burnout10, 11 by adjusting for the following three survey measures: (1) team communication, (2) team knowledge and skills, and (3) team satisfaction. First, we measured team communication via 4 items from the Survey of Organizational Attributes for Primary Care31 (α = 0.80), such as “In this clinic, co-workers from different clinical or administrative backgrounds frequently interact to solve quality of care problems.” Five-point Likert scale responses ranged from “strongly disagree” (0) to “strongly agree” (5) and were aggregated from 0 to 20. Second, we examined team knowledge and skills using 6 items from the Team Diagnostic Survey32 (α = 0.77), such as “Everyone in this team has the special skills that are needed for team work.” Five-point Likert scale responses were aggregated from 0 to 30. Third, we asked PCPs to rate the following statement again on a 5-point Likert scale: “Overall, I am satisfied with the help I receive from my teamlet.”
We examined additional clinician- and organizational-level characteristics, which may affect PCP-reported burnout.33 Clinician characteristics included age, gender, provider type (i.e., physician versus non-physician), full-time to near full-time status (i.e., practicing more than 3 days per week), and years in practice at the VA. We did not control for race/ethnicity due to lack of variation among PCPs in our study. We accounted for whether or not a clinic was participating in the evidence-based quality improvement intervention, which was previously found to influence clinician burnout.19
Analysis
We described the level of PCP-reported burnout, and secondarily job satisfaction, in fiscal years 2012 and 2013, and in total. Burnout rates were aggregated across and stratified by healthcare systems, to examine organizational-level variation. In bivariate analysis, we dichotomized our two key independent variables, that is PCP-rated communication with mental health specialty and his/her clinic’s engagement in mental health integration programs. We used logistic regression models to examine their unadjusted associations between all study variables.
Using multilevel linear regression models, we examined the relationship between PCP-reported burnout, and secondarily job satisfaction, and our two key independent variables. Both mental health integration variables were examined separately and then together in regression models. If we identified a relationship between PCP-rated communication with mental health specialty and his/her clinic’s engagement in mental health integration programs, we intended to perform a mediation analysis with our burnout outcome and both key independent variables. Adjusted models also controlled for PCP-reported team functioning, and both clinician- and organizational-level characteristics. We included two random effects, provider and clinic, in the mixed model. This accounted for provider responses in, at most, two survey waves and for clustering of providers within a clinic. Survey weighting was applied to provider role and clinic site in both waves to correct for non-response bias.
In sensitivity analysis, we examined multilevel logistic regression models with PCP-reported burnout, and secondarily job satisfaction, dichotomized as low–medium versus high to assess the robustness of our findings. Given the organizational nature of clinician burnout,34 we also stratified adjusted regression models by healthcare system to examine for variation across VA healthcare systems. We determined significance using a two-tailed α of 0.05 and analyzed data in SAS, version 9.4 (SAS Institute Inc., Cary, NC). The VA Greater Los Angeles Institutional Review Board approved this study (PCC-2013101432).
RESULTS
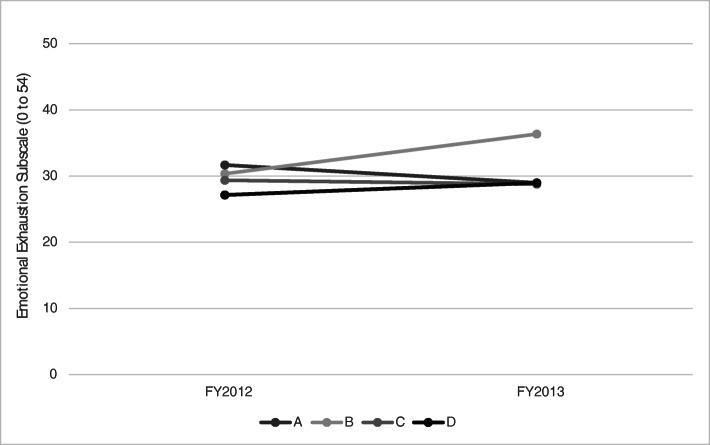
On average, PCPs reported high levels of burnout (29, range 9–54), which did not significantly increase over the two study years. We observed no significant difference in aggregated burnout levels across healthcare systems over time (mean 27 to 32 in 2012, p = 0.64; 29 to 36 in 2013, p = 0.23) (Fig. 1). On average, PCP rated job satisfaction as 3.6 (range = 1–5).
Figure 1.
Average levels of PCP-reported burnout by VA healthcare system over time. Each line represents aggregated primary care clinician (PCP)-reported burnout levels (via the Maslach Burnout Inventory, Emotional Exhaustion subscale) in one of four VA healthcare systems studied during each survey administration over two fiscal years (FY). 16%, 13%, 28%, and 43% of PCPs were from VA Healthcare System A, B, C, and D, respectively.
Participating PCPs were mostly female (57%), non-Hispanic White (91%), and physicians (72%). On average, they were 49 years of age, practiced 10 years in the VA, and were in clinic 3 days a week. Mean PCP ratings for team functioning were 12 (range = 4–20) for communication, 22 (range = 8–30) for knowledge and skills, and 3.6 (range = 1–5) for satisfaction.
Our two key mental health integration variables did not appear to have a relationship with each other; thus, no mediation analysis was performed. Approximately half of PCPs reported that communication with mental health specialists was “very easy” (mean = 2; range = 1–4). In unadjusted analyses, the first key independent variable appeared to be associated with clinician burnout (p = 0.03) and team functioning (communication, p = 0.002; knowledge and skills, p = 0.02; satisfaction, p = 0.01). On average, study clinics where PCPs practiced had 9% of their primary clinic patients seeing integrated mental health specialists (mean = 9%; range = 0–36%). The second key independent variable was not associated with any other study variables (Table 1).
Table 1.
PCP Burnout/Job Satisfaction and Clinician/Organizational Factors by Mental Health Integration
| Total | Communication with mental health specialists | Proportion of clinic patients who saw integrated provider | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Not “very easy” | “Very easy” | p value | 8% (median) or less | More than 8% | p value | |||
| Maslach Burnout Inventory | |||||||||
| Emotional exhaustion subscale (average, 0–54) | 265 | 29 | 30 | 27 | 0.03 | * | 31 | 29 | 0.87 |
| Job satisfaction (average, 1–5) | 273 | 3.6 | 3.5 | 3.8 | 0.07 | 3.5 | 3.6 | 0.91 | |
| Mental health integration | |||||||||
| Mental health communication (% very easy) | 248 | 46% | – | – | – | 51% | 46% | 0.80 | |
| Proportion of clinic patients who saw integrated provider (%) | 286 | 9% | 9% | 9% | 0.91 | – | – | – | |
| Clinician characteristics | |||||||||
| Age (average, years) | 258 | 49 | 49 | 49 | 0.77 | 51 | 50 | 0.80 | |
| Gender (% female) | 262 | 57% | 47% | 49% | 0.78 | 54% | 50% | 0.93 | |
| Non-Hispanic White (%) | 139 | 91% | 91% | 89% | 0.32 | 100% | 89% | 0.78 | |
| Physician (%) | 286 | 72% | 70% | 75% | 0.53 | 55% | 75% | 0.78 | |
| > 10 years of practice at VA (%) | 279 | 43% | 50% | 49% | 0.85 | 24% | 50% | 0.59 | |
| > 3 days per week in clinic (%) | 269 | 49% | 48% | 43% | 0.56 | 81% | 44% | 0.67 | |
| Clinician self-reported measures | |||||||||
| Team functioning - communication (average, 0–20) | 271 | 12 | 12 | 13 | <.001 | ‡ | 14 | 12 | 0.73 |
| Team functioning - knowledge and skills (average, 0–30) | 274 | 22 | 21 | 22 | 0.02 | * | 23 | 21 | 0.71 |
| Team functioning - satisfaction (average, 0–5) | 262 | 3.6 | 3.5 | 3.9 | 0.01 | † | 4.2 | 3.6 | 0.62 |
| Organizational characteristics | |||||||||
| Evidence-based quality improvement program (%) | 265 | 57% | 49% | 67% | 0.06 | 0% | 60% | – | |
Differences between groups were tested for significance using simple logistic regression models
*p < 0.05
†p < 0.01
‡p < 0.001
In fully adjusted regression analyses, PCP-reported burnout was not significantly associated with mental health communication ratings (beta coefficient [β] = − 0.96, standard error [SE] = 1.29, p = 0.46), nor with affiliated clinic’s engagement in mental health integration (β = 0.02, SE = 0.11, p = 0.88). Null findings were mostly unchanged across all models, including subpopulation analyses for each individual healthcare system (Table 2). Similarly, PCP-rated job satisfaction was not significantly associated with mental health communication ratings (β = 0.005, SE = 0.13, p = 0.97), nor with affiliated clinic’s engagement in mental health integration (β = 0.005, SE = 0.01, p = 0.63) (Table 3).
Table 2.
Adjusted Associations Between PCP-Reported Burnout and Mental Health Integration
| β (SE) | β (SE) | β (SE) | β (SE) | |
|---|---|---|---|---|
| Mental health integration | ||||
| Mental health communication (“very easy”) | − 2.34 (1.30) | − 2.89 (1.35)* | − 0.44 (1.22) | − 0.96 (1.29) |
| Proportion of clinic patients who saw integrated specialists | 0.03 (0.11) | 0.06 (0.13) | − 0.006 (0.10) | 0.02 (0.11) |
| Clinician characteristics | ||||
| Age | – | − 0.11 (0.09) | – | − 0.07 (0.08) |
| Gender (female) | – | 2.51 (1.72) | – | 2.60 (1.50) |
| Physician | – | − 0.32 (2.06) | – | − 0.93 (1.85) |
| > 10 years of practice at VA | – | − 1.48 (1.81) | – | − 1.70 (1.60) |
| >3 days per week in clinic | – | 0.52 (1.52) | – | − 0.76 (1.39) |
| Clinician self-reported measures | ||||
| Team functioning - communication (0–20) | – | – | − 1.29 (0.20)‡ | − 1.28 (0.22)‡ |
| Team functioning - knowledge and skills (0–30) | – | – | − 0.04 (0.19) | − 0.008 (0.20) |
| Team functioning - satisfaction (0–5) | – | – | − 1.63 (0.68)* | − 1.39 (0.73) |
| Organizational characteristics | ||||
| Evidence-based quality improvement program (%) | – | – | – | − 1.35 (2.09) |
β, beta coefficient; SE, standard error
We reported coefficients (and standard errors) from multilevel linear regression models that predicted PCP-reported burnout using our two key mental health integration variables, controlling for all clinician and organization-level covariates as listed on the table
*p < 0.05
†p < 0.01
‡p < 0.001
Table 3.
Associations Between PCP-Rated Job Satisfaction and Mental Health Integration
| β (SE) | β (SE) | β (SE) | β (SE) | |
|---|---|---|---|---|
| Mental health integration | ||||
| Mental health communication (“very easy”) | 0.14 (0.14) | 0.22 (0.14) | − 0.06 (0.12) | 0.005 (0.13) |
| Proportion of clinic patients who saw integrated provider | 0.003 (0.01) | 0.001 (0.01) | 0.006 (0.01) | 0.005 (0.01) |
| Clinician characteristics | ||||
| Age | – | 0.01 (0.01) | – | 0.008 (0.008) |
| Gender (female) | – | − 0.47 (0.19)* | – | − 0.4 (0.15)* |
| Physician | – | − 0.26 (0.22) | – | − 0.29 (0.18) |
| > 10 years of practice at VA | – | 0.09 (0.19) | – | 0.11 (0.16) |
| > 3 days per week in clinic | – | − 0.31 (0.16) | – | − 0.21 (0.14) |
| Clinician self-reported measures | ||||
| Team functioning - communication (0–20) | – | – | 0.14 (0.02)‡ | 0.12 (0.02)‡ |
| Team functioning - knowledge and skills (0–30) | – | – | 0.02 (0.02) | 0.02 (0.02) |
| Team functioning - satisfaction (0–5) | – | – | 0.31 (0.07)‡ | 0.28 (0.07)‡ |
| Organizational characteristics | ||||
| Evidence-based quality improvement program (%) | – | – | – | − 0.15 (0.18) |
SE, standard error
We reported coefficients (and standard errors) from multilevel linear regression models that predicted PCP-rated job satisfaction using our two key mental health integration variables, controlling for all clinician and organization-level covariates as listed on the table
*p < 0.05
†p < 0.01
‡p < 0.001
Among model covariates, we found only team functioning to be consistently associated with PCP-reported burnout. Among study participants, PCPs reporting low team communication ratings (β = − 1.28, SE = 0.22, p < 0.001), and PCPs reporting low team satisfaction (for certain models), had high levels of burnout (Table 2). In parsimonious iterations of our models, we noted female gender and younger age (and/or < 10 years in VA practice) to be correlated with the highest levels of PCP-reported burnout. We did not observe any changes in PCP-reported burnout over time in our fully adjusted regressions, nor in our results for each individual healthcare system (data not shown). Similar patterns were observed for PCP-reported job satisfaction—low team communication ratings (β = 0.12, SE = 0.02, p < 0.001), low team satisfaction ratings (β = 0.28, SE = 0.07, p < 0.001), and female gender (β = − 0.4, SE = 0.15, p = 0.46) were associated with low job satisfaction (Table 3).
DISCUSSION
As locally implemented, care models that integrated primary care and mental health specialties did not appear to influence PCP-reported burnout, nor job satisfaction, in the VA. While half of study PCPs reported that communication with mental health specialists was “very easy,” the clinics where they practiced varied in their level of program engagement, e.g., the proportion of patients who saw integrated mental health specialists. Nonetheless, neither factor independently nor together appeared to influence PCP-reported burnout or job satisfaction. Interestingly, we did not observe a significant relationship between PCP-rated mental health communication and their clinic’s engagement in mental health integration. In theory, improved cross-specialty communication and integration should mitigate burnout; in practice, however, our study did not replicate the significant relationship between integrated care and burnout, as had been found in a previous study.24 Team-based care has generally demonstrated positive associations with clinician well-being,14 but, in the case of mental healthcare integration, it may be attenuated by increased workload related to newly discovered mental health disease among primary care patients.35 Also, the construct of mental health integration can be challenging to measure, as clinic arrangements (e.g., specialty staffing, communication methods) vary from site to site.36 Future research should explore variation in mental health integration models among clinics—for example, triangulate the extent of evidence-based depression care management implementation as recorded in administrative data with qualitative data from leadership and from clinic staff—in order to optimize care models to additionally enhance PCP well-being.
Regardless of healthcare system where they practice, PCPs reported high levels of burnout, which did not decrease over time, consistent with prior VA research.5 Emotional exhaustion was observed across all PCPs—physicians, nurse practitioners, and physicians’ assistants—and, as expected, at levels higher than previously reported when including primary care staff.37 Across the literature, PCP-reported burnout has been shown to be a chronic rather than a transient condition and commonly persists over time.38 This is extrapolated to mean that PCPs who reported high emotional exhaustion (relative to their peers) during this survey will continue to do so. On average, PCPs rated job satisfaction as only mid-range. As such, interventions aimed at addressing important factors that contribute to burnout are sorely needed in order to target improved PCP and other clinician well-being, in the VA and more broadly.39
Clinician burnout, and correspondingly job satisfaction, is complex and, for VA PCPs specifically, it appears to be most strongly associated with team functioning. In our study and extant literature,10, 11, 27 team functioning (specifically, communication) was again a significant contributor to clinician well-being. While some studies report age and gender to be associated with clinician burnout,27, 33, 37 we observed these associations to be sporadic in our study. When present, however, we found that women exhibited higher burnout, and lower job satisfaction, than men in our study. We also observed young age (correspondingly, fewer years in VA practice) to influence PCP-reported burnout, or vice versa—burnout may encourage early retirement. Taken together, health systems should consider strengthening PCPs’ communication with other primary care team members by optimizing fidelity to evidence-based integrated care models (e.g., depression care management), and possibly directing efforts first at women and at younger PCPs (or PCPs new to the VA system), in order to achieve the lowest aggregated levels of clinician burnout.
This study had a few limitations. Survey results highlight associations noted within PCPs of one VA region at one point in time and do not imply causality (or direction of a relationship). While provider response rates are comparable with those of other studies,10, 11 PCPs who did not participate in the survey may exhibit different burnout or job satisfaction levels than those who did. We reported results from two waves of surveys administered over approximately 2 years, but burnout results are likely to be stable over time.38 While we examined PCP-reported burnout via the Maslach Burnout Inventory’s central domain of emotional exhaustion, other studies have favored other domains like depersonalization, such as becoming more callous toward patients.34 Based on prior research,28–30 we chose to examine mental health integration at both the provider-level and the clinic-level yet each method has its own strengths and limitations. For example, the proportion of primary care patients who saw integrated mental health specialists may approximate the overall level of program engagement, which may be unevenly distributed across individual PCPs. Because we incorporated use of both survey and administrative data, the overlap in time periods is noted to be approximate, and not exact. Despite having multiple data sources, there may still be unmeasured variables, such as inundation with technology,40 that may influence clinician well-being in our study.
All in all, PCPs were emotionally exhausted, and reported mediocre satisfaction with their jobs, across different VA healthcare systems in our study region. As broadly implemented across multiple primary care practices, current care models to integrate primary care and mental health specialties did not appear to be associated with clinician burnout. In 2019, the National Academy of Medicine (NAM) has recommended in a consensus study that healthcare organizations focus on redesigning work systems to prevent and reduce clinician burnout and foster professional well-being.6 As the VA strives to redesign clinical services in an effort to achieve high-quality population-based care, it should also consider taking heed of NAM’s recommendations to measure and conduct interventions to tackle reductions in burnout within the primary care workforce serving veterans. Health systems would do well to examine team-based care models as currently implemented to ensure the optimization of both patient outcomes and clinician well-being.
Acknowledgments
This work was undertaken as part of the Veterans Assessment & Improvement Laboratory (VAIL) for Patient-Centered Care (XVA 65–018).
Funding
Funding is provided by the VA Office of Primary Care to support and evaluate VA’s transition to a patient-centered medical home. Dr. Leung was funded by Career Development Award Number IK2 HX002867 from the United States Department of Veterans Affairs Health Services Research & Development Service.
Compliance with Ethical Standards
Disclaimer
These views represent the opinions of the authors and not necessarily those of the VA or the US government.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103–111. doi: 10.1002/wps.20311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maslach C, Jackson SE, Leiter MP, Schaufeli WB, Schwab RL. Maslach burnout inventory. Palo Alto, CA: Consulting psychologists press; 1986. [Google Scholar]
- 3.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 5.Rinne ST, Mohr DC, Swamy L, Blok AC, Wong ES, Charns MP. National Burnout Trends Among Physicians Working in the Department of Veterans Affairs. J Gen Intern Med. 2020. [DOI] [PMC free article] [PubMed]
- 6.In: Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington (DC); 2019. [PubMed]
- 7.Hall LH, Johnson J, Watt I, Tsipa A, O'Connor DB. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS One. 2016;11(7):e0159015. doi: 10.1371/journal.pone.0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salyers MP, Bonfils KA, Luther L, et al. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis. J Gen Intern Med. 2017;32(4):475–482. doi: 10.1007/s11606-016-3886-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panagioti M, Geraghty K, Johnson J, et al. Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis. JAMA Intern Med. 2018;178(10):1317–1330. doi: 10.1001/jamainternmed.2018.3713. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 10.Willard-Grace R, Hessler D, Rogers E, Dube K, Bodenheimer T, Grumbach K. Team structure and culture are associated with lower burnout in primary care. J Am Board Fam Med. 2014;27(2):229–238. doi: 10.3122/jabfm.2014.02.130215. [DOI] [PubMed] [Google Scholar]
- 11.Helfrich CD, Dolan ED, Simonetti J, et al. Elements of team-based care in a patient-centered medical home are associated with lower burnout among VA primary care employees. J Gen Intern Med. 2014;29(Suppl 2):S659–666. doi: 10.1007/s11606-013-2702-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buchbinder SB, Wilson M, Melick CF, Powe NR. Estimates of costs of primary care physician turnover. Am J Manag Care. 1999;5(11):1431–1438. [PubMed] [Google Scholar]
- 13.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith CD, Balatbat C, Corbridge S, et al. Implementing optimal team-based care to reduce clinician burnout. NAM Perspectives. 2018.
- 15.Post EP, Metzger M, Dumas P, Lehmann L. Integrating mental health into primary care within the Veterans Health Administration. Fam Syst Health. 2010;28(2):83–90. doi: 10.1037/a0020130. [DOI] [PubMed] [Google Scholar]
- 16.Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19(7):e263–272. [PubMed] [Google Scholar]
- 17.Yoon J, Chow A, Rubenstein LV. Impact of medical home implementation through evidence-based quality improvement on utilization and costs. Med Care. 2016;54(2):118–125. doi: 10.1097/MLR.0000000000000478. [DOI] [PubMed] [Google Scholar]
- 18.Huynh A, Lee M, Rose D, Stockdale S, Wang M, Rubenstein L. Evaluation of Changes in Patient-Provider Communication in Evidence-Based Quality Improvement Sites Using a Non-randomized Stepped Wedge Design. HSR&D/QUERI National Conference; July 18-20, 2017. Arlington, VA; 2017.
- 19.Meredith LS, Batorsky B, Cefalu M, et al. Long-term impact of evidence-based quality improvement for facilitating medical home implementation on primary care health professional morale. BMC Fam Pract. 2018;19(1):149. doi: 10.1186/s12875-018-0824-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hahn SR, Kroenke K, Spitzer RL, et al. The difficult patient: prevalence, psychopathology, and functional impairment. J Gen Intern Med. 1996;11(1):1–8. doi: 10.1007/BF02603477. [DOI] [PubMed] [Google Scholar]
- 21.Zulman DM, Chee CP, Wagner TH, et al. Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System. BMJ Open. 2015;5(4):e007771. doi: 10.1136/bmjopen-2015-007771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525. doi: 10.1002/14651858.CD006525.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levine S, Unutzer J, Yip JY, et al. Physicians' satisfaction with a collaborative disease management program for late-life depression in primary care. Gen Hosp Psychiatry. 2005;27(6):383–391. doi: 10.1016/j.genhosppsych.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Zubatsky M, Pettinelli D, Salas J, Davis D. Associations Between Integrated Care Practice and Burnout Factors of Primary Care Physicians. Fam Med. 2018;50(10):770–774. doi: 10.22454/FamMed.2018.655711. [DOI] [PubMed] [Google Scholar]
- 25.Meredith LS, Schmidt Hackbarth N, Darling J, et al. Emotional exhaustion in primary care during early implementation of the VA's medical home transformation: Patient-aligned Care Team (PACT) Med Care. 2015;53(3):253–260. doi: 10.1097/MLR.0000000000000303. [DOI] [PubMed] [Google Scholar]
- 26.Rubenstein LV, Stockdale SE, Sapir N, et al. A patient-centered primary care practice approach using evidence-based quality improvement: rationale, methods, and early assessment of implementation. J Gen Intern Med. 2014;29(2):589–597. doi: 10.1007/s11606-013-2703-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim LY, Rose DE, Soban LM, et al. Primary care tasks associated with provider burnout: findings from a veterans health administration survey. J Gen Intern Med. 2018;33(1):50–56. doi: 10.1007/s11606-017-4188-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zuchowski JL, Rose DE, Hamilton AB, et al. Challenges in referral communication between VHA primary care and specialty care. J Gen Intern Med. 2015;30(3):305–311. doi: 10.1007/s11606-014-3100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leung LB, Yoon J, Rubenstein LV, et al. Changing Patterns of Mental Health Care Use: The Role of Integrated Mental Health Services in Veteran Affairs Primary Care. J Am Board Fam Med. 2018;31(1):38–48. doi: 10.3122/jabfm.2018.01.170157. [DOI] [PubMed] [Google Scholar]
- 30.Leung LB, Yoon J, Escarce JJ, et al. Primary Care-Mental Health Integration in the VA: Shifting Mental Health Services for Common Mental Illnesses to Primary Care. Psychiatr Serv. 2018;69(4):403–409. doi: 10.1176/appi.ps.201700190. [DOI] [PubMed] [Google Scholar]
- 31.Ohman-Strickland PA, John Orzano A, Nutting PA, et al. Measuring organizational attributes of primary care practices: development of a new instrument. Health Serv Res. 2007;42(3 Pt 1):1257–1273. doi: 10.1111/j.1475-6773.2006.00644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wageman R, Hackman JR, Lehman E. Team diagnostic survey: Development of an instrument. J Appl Behav Sci. 2005;41(4):373–398. doi: 10.1177/0021886305281984. [DOI] [Google Scholar]
- 33.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 34.Leiter MP, Maslach C. Latent burnout profiles: A new approach to understanding the burnout experience. Burn Res. 2016;3(4):89–100. doi: 10.1016/j.burn.2016.09.001. [DOI] [Google Scholar]
- 35.Leung LB, Rubenstein LV, Yoon J, et al. Veterans Health Administration Investments In Primary Care And Mental Health Integration Improved Care Access. Health Aff (Millwood) 2019;38(8):1281–1288. doi: 10.1377/hlthaff.2019.00270. [DOI] [PubMed] [Google Scholar]
- 36.Leung LB, Rose D, Stockdale S, et al. Regional Adoption of Primary Care-Mental Health Integration in Veterans Health Administration Patient-Centered Medical Homes. J Healthc Qual. 2019. [DOI] [PubMed]
- 37.Meredith LS, Hackbarth NS, Darling J, et al. Emotional exhaustion in primary care during early implementation of the VA’s medical home transformation: Patient-aligned Care Team (PACT) Med Care. 2015;53(3):253–260. doi: 10.1097/MLR.0000000000000303. [DOI] [PubMed] [Google Scholar]
- 38.Schaufeli WB, Maassen GH, Bakker AB, Sixma HJ. Stability and change in burnout: A 10-year follow-up study among primary care physicians. J Occup Organ Psychol. 2011;84(2):248–267. doi: 10.1111/j.2044-8325.2010.02013.x. [DOI] [Google Scholar]
- 39.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 40.Are U. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Intern Med. 2018;169:50–51. doi: 10.7326/M18-0139. [DOI] [PubMed] [Google Scholar]