Abstract
Objective
The purpose of this study was to investigate the feasibility of recruiting, randomizing, enrolling, and collecting outcome data on veteran patients with chronic low back pain (CLBP) who undergo an 8-week, active exercise class with mindfulness (yoga class) and without (stretching class).
Methods
United States veterans with CLBP based on inclusion/exclusion criteria were randomized to 1 of 2 groups. The study design was a pilot randomized controlled trial. Twenty CLBP patients attended a yoga class or stretching class once per week for 8 weeks at the Veterans Affairs Rochester Outpatient Center, Rochester, New York. The following measurements were obtained: recruitment or enrollment data, compliance data to include class attendance and home exercise, and compliance data regarding ability to collect outcome measures at baseline and at completion. Outcome measures included pain (PEG), quality of life (PROMIS Global Health Survey), self-efficacy (2-item questionnaire), fear avoidance belief, catastrophizing, and social engagement in addition to qualitative clinician open-ended questions postintervention.
Results
Forty-five veterans were queried regarding interest in participation. Of these, 34 (76%) met the study's criteria. Twenty (44%) agreed to participate and were consented, randomized, and enrolled in the study. Initial and final outcome measures were obtained for each participant (100%). Forty percent attended more than 80% of the sessions for both yoga and stretching groups.
Conclusion
This pilot study demonstrated feasibility of recruiting, enrolling, and collecting outcome data on CLBP veteran patients participating in yoga and stretching class. The data from this pilot will inform the development of a randomized, comparative effectiveness study of yoga with and without mindfulness in the management of CLBP.
Key Indexing Terms: Low Back Pain, Chronic Pain, Yoga, Veterans, Mindfulness, Exercise, Pain Management
Introduction
Background
Chronic low back pain (CLBP) is a multifactorial public health dilemma affecting millions of people worldwide. It is also a significant factor leading to disability in the United States and worldwide1 costing billions of dollars annually in lost productivity and loss of wages, and it is the second most common reason for physician visits.2 Veterans have higher rates of chronic pain than the general population, with back pain being the most commonly reported.3 Despite widely accepted clinical guidelines, there remains widespread inappropriate use of imaging, rest, spinal injections, surgery, and opioid prescriptions4 in the civilian and military veteran populations. Many veterans with CLBP may have coexisting diagnoses, such as generalized anxiety, PTSD, and major depression, which affect their perception and management of pain. The presence of psychosocial factors is a major predictor of chronicity of pain.5 Often catastrophizing, fear avoidance behaviors, and substance abuse6 delay or inhibit recovery from back pain and return to normal activity, leading to increased social isolation. Given these significant comorbidities, the management of CLBP requires a biopsychosocial approach. Current back pain guidelines emphasize self-management and promote exercise7 such as yoga.8,9 Yoga is becoming more popular in the United States10 and is used for both wellness and management of specific medical conditions. Hatha Yoga, the form of yoga most commonly practiced in the United States, uses physical exercise and mental focus that is intended to improve strength, flexibility, and balance in the body and the mind. Rooted in meditation, yoga uses breathing techniques to promote mindfulness as the body moves through different physical postures. The mindfulness practices associated with yoga, such as self-introspection, non-judgmental awareness, and self-acceptance, may affect the psychological aspects of CLBP. Additionally, the supportive group setting of a yoga class may also affect the social aspects of CLBP in creating a supportive social network for people who might otherwise be isolated, thereby improving the patient's overall chronic pain experience. Yoga is also a form of active exercise utilizing stretching combined with body weight strengthening postures, which may improve CLBP.
Several yoga studies for CLBP have shown a reduced pain intensity and pain-related disability, whereas others have suggested yoga can improve biopsychosocial factors related to chronic pain.11,12 More recently, a 2018 report by the Agency for Healthcare Research and Quality evaluating yoga for low back pain concluded yoga improved short-term and intermediate (defined as 1-6 months) pain and function.13 Although research on yoga interventions is rapidly growing,14 much of the literature is inconclusive due to the weakness in study design,15 specifically concerning appropriate control groups.16 In evaluating any intervention, it is important to have a comparable control group to better understand the mechanism of the intervention. Of 128 randomized control trials included in Park et al's16 systematic review of comparison groups in yoga research, 30 used physical exercise, and 4 used what was considered sham yoga or stretching. However, review of these 4 studies indicated the “sham yoga” was indeed simply stretching, with no description of utilizing yoga postures for comparison.16 Furthermore, none of these studies evaluated CLBP. Although the literature suggests that yoga has the potential to alleviate low back pain,14,17, 18, 19, 20, 21 the long-term goal of this project was to create a study design that would enable the evaluation of the mechanism by which yoga is effective for CLBP. The authors chose this topic given the popularity of yoga in the United States,22 the fact that yoga is currently mandated at all Veterans Affairs (VA) facilities under the Whole Health Initiative,23 and that it was recommended by the VA State of the Art conference that there be further research in this area.24 The data generated in our current study will inform the design of a larger randomized controlled trial to evaluate the mechanism of yoga. Specifically, is the clinical effectiveness of yoga related simply to the stretching and strengthening exercises, mindfulness or is it some combination of the 2?
Feasibility Objectives
To assess the feasibility of recruiting, enrolling, randomizing, and collecting outcomes at baseline and 8 weeks postintervention on 20 CLBP veteran patients using 2 evidence-based interventions: a mindfulness-based exercise program (yoga) or an exercise program without mindfulness (stretching class).
Methods
Trial Design
A randomized controlled trial design to evaluate the feasibility of recruitment and data collection to inform a larger randomized controlled trial investigating the mechanism of yoga's effect on CLBP.
This project was approved by the Syracuse VA Medical Center Institutional Review Board, Syracuse, New York (initial approval date: November 27, 2018; approval number: 1135250).
There were no changes to methods after pilot trial commencement.
Participants
Inclusion Criteria
Veterans between the ages of 18 to 89 years of either sex with lower back pain for >12 weeks who had the ability to exercise independently were included in the study.
Exclusion Criteria
Subjects were excluded if they were currently enrolled in or maintained a home meditation practice; if they were currently involved in a mindfulness or cognitive behavioral therapy group; if they had participated in a structured group yoga program within the previous 3 months; if there was any radiographic or examination evidence of cauda equina syndrome, spinal neoplasia or metastatic disease, destructive joint pathology such as rheumatoid arthritis, bowel/bladder dysfunction (associated with the back pain), progressive lumbosacral radiculopathy (as evidenced by worsening of objective neurological symptoms over a 2-4 week period of time as defined by loss of strength and/or onset of neurologically mediated bowel/bladder symptoms) (stable radiculopathy was not excluded), progressive myelopathy or neurogenic claudication (as evidenced by worsening of objective neurological symptoms over a 2-4 week period of time as defined by loss of strength and/or onset of neurologically mediated bowel/bladder symptoms and an increase in objective upper motor neuron signs such as hyperreflexia); or any absolute contraindications to exercise such as unstable angina, uncontrolled symptomatic heart failure, or acute systemic infection. Subjects were excluded if they had an open workers’ compensation or no-fault case or had undergone spinal surgery in the previous 6 months.
Enrollment Procedures
All patients who presented to the Chiropractic Clinic as either a new consult or an established patient between January 2018 and March 2018 and who met the inclusion/exclusion criteria were approached concerning their willingness to participate in the study. Participation in the study was voluntary and did not affect or alter any chiropractic evaluation or treatment plans. If interested, the patient was provided an informed consent document and a HIPAA form, which were reviewed and signed the same day. The patient was given details regarding their respective intervention including times of classes, expectation for home practice that began after their first in-person group class, and all handouts and logs for the home practice consistent with the respective groups.
Randomization
A computer-generated randomization table, used to determine which intervention the patient participated in after consent, was received and outcome measures completed. The computer-generated randomization table was referenced, and the patient was informed of their allocated group by the consenting clinician on the same day. Neither patient nor clinician were blinded after assignment to interventions.
Interventions
Yoga
Participants randomized to the yoga intervention were asked to attend 1, 1-hour yoga class per week for 8 weeks. The classes were timed, each starting and ending on the hour. Classes were offered every Monday and Friday. Participants were provided with a mat and block for use during the class. The classes were instructed by registered yoga teachers, with 1 teaching and demonstrating while the other teacher assisted with modifications or further instructions on an individualized basis during the class. Yoga classes included yoga postures, breathing exercises, relaxation practices, and mindfulness cueing in addition to self-awareness practices. Participants were reminded throughout the practice to be aware of how they were feeling and to fully engage physically and mentally in all aspects of the class. Participants were given a home practice instruction packet and home practice log. The instruction packet contained descriptions on how to safely perform similar yoga postures and how to modify if needed. Participants were encouraged to practice at home 3 times a week for 30 minutes in addition to the 1-hour group class per week. The home instruction packet also included a guided meditation practice to be done in conjunction with the home yoga. At the end of the eighth class, participants were given outcome measures to complete. If a participant did not attend the eighth class, verbal answers to outcome measures were recorded via a phone call at the end of the study.
Stretching
Participants enrolled in the stretching intervention were asked to attend 1, 1-hour stretching class per week for 8 weeks. The classes were timed, each starting and ending on the hour. Classes were offered every Monday and Friday. Participants were provided with a mat and block for use during the class. The classes were instructed by registered yoga teachers, with 1 teaching and demonstrating, while the other teacher assisted with modifications or further instructions on an individualized basis during the class. The stretching class included similar yoga postures to the other intervention; however, it purposely excluded any verbal reminders regarding mindfulness, being in the present moment, breathing exercises, relaxation practices, or self-awareness reminders. Conversely, the participants were encouraged to engage in conversation with each other to avoid opportunities for mindfulness. Participants were given a home practice instruction packet and a home practice log specific to stretching (yoga postures) only. The instruction packet contained descriptions on how to safely perform similar yoga postures and how to modify if needed. Participants were encouraged to practice at home 3 times a week for 30 minutes in addition to the 1-hour group class per week. At the end of the eighth class, participants were given outcome measures to complete. If a participant did not attend the eighth class, verbal answers to outcome measures were recorded via a phone call at the end of the study.
Treating Clinician
Both yoga therapy and stretching therapy were delivered by 2 licensed chiropractors, each of whom were registered yoga teachers.
Concomitant Interventions
For the purpose of this study, the patients were permitted to continue with usual health care for their CLBP including but not limited to chiropractic, acupuncture, or physical therapy.
Outcomes
Primary outcomes were collected at baseline and after the last session. Those veterans who did not attend the eighth session were called, and verbal answers to outcome measure questionnaires were recorded at the end of the study. The outcome measures were chosen to inform the investigators about potential changes in quality of life, pain, and psychosocial factors. We chose to utilize abbreviated psychosocial questions to decrease participant burden including the following:
-
•
PROMIS Global Health Scale is a quality of life tool developed by the Patient Reported Outcome Measurement Information System. This scale provides an overall index score for quality of life and includes components of a patient's perception of their physical and mental health. This form was recently validated in comparison to the EuroQual.25
-
•
PEG is an ultra-brief, three-item scale derived from the Brief Pain Inventory. Evidence supports it as a reliable and valid measure of pain among primary care patients with chronic musculoskeletal pain. The PEG appears comparable to the Brief Pain Inventory in terms of responsiveness to change.26
-
•
Psychosocial questions included a 2-question self-efficacy questionnaire27; a catastrophizing question, “I feel that my back pain is terrible and it's never going to get any better”; a fear avoidance question, “It's not really safe for a person with my back problem to be physically active”; and a behavioral disengagement question, “Due to my chronic back pain, I no longer engage in activities that are enjoyable and pleasant.”
At the conclusion of the study, both study clinicians answered the following open-ended questions:
-
•
What were the barriers to recruitment and enrollment of participants?
-
•
What were the barriers to collecting outcomes?
-
•
What barriers were encountered in regard to carrying out the group classes?
-
•
What were the barriers to patient accountability?
-
•
Did you feel the classes were well received by the patients or did you encounter any constructive feedback from patients?
Feasibility criteria
The following criteria defined feasibility for this study: complete baseline and postintervention outcome measures in at least 90% of all recruited subjects; enrollment of at least 50% of eligible patients to be consented and randomized to 1 of 2 groups; and 100% of clinicians completing qualitative questions postintervention.
Data Analysis
Given that this is a pilot study, simple descriptive statistics were used for patient characteristics including age, sex, body mass index, and scores on outcome measures.
Sample size
Although a feasibility study does not require a sample size calculation, we had anticipated recruiting 20 patients over the course of 1 month who presented to the chiropractic clinc and met our inclusion/exclusion criteria. Typically, the chiropractic clinic sees approximately 35 new patients and 70 follow-up patients per month, and we felt it was reasonable to recruit and enroll 20 by the end of 4 weeks.
Ethical aspects
The informed consent document clearly described to the participant the intention of the study being feasibility. It details “(T)he purpose of this study is to evaluate the feasibility of performing a larger trial comparing 2 different types of interventions for your CLBP. The 2 interventions are an 8-week mindfulness-based exercise class (yoga) and an 8-week exercise class (stretching class). We would ultimately like to compare the 2 interventions for their efficacy; however, this study is a pilot study conducted simply to assess the feasibility of enrolling, randomizing, and conducting a multi-week exercise class.” The study was approved by the VA Institutional Review Board.
Results
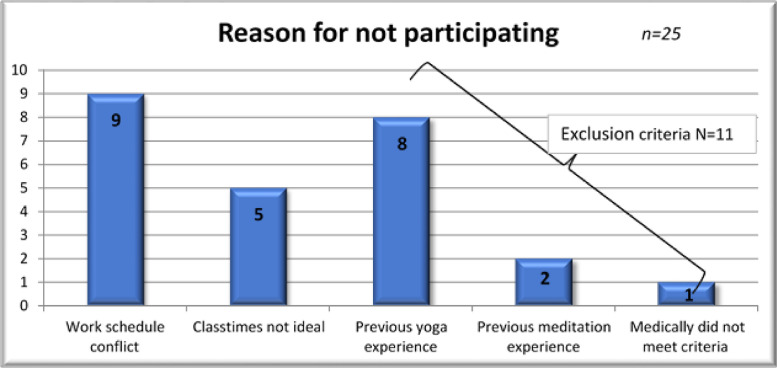
During a 4-week period, 45 veterans with CLBP presenting to the Chiropractic Clinic were queried regarding their interest in participating in our feasibility study. Of these patients, 34 (76%) met the study's inclusion and exclusion criteria. Of those who met the criteria, 20 (59%) agreed to participate and were consented, randomized, and enrolled in the study. Ten participants were randomized into the yoga group and 10 into the stretching group. Of these 20, initial and final outcome measures were obtained for each participant (100%). The most common reasons for not participating in the study were not being able to attend at the times the classes occurred, previous yoga or meditation experience, or working during class times (Fig 1).
Fig 1.
Details regarding a screening patient's reason for not participating in pilot study (n = 25).
The patients’ demographics are reported in Table 1. The average age of the yoga group (n = 10) was 51.7 (standard deviation [SD] = 14.9), and the stretching group (n = 10) was 50.3 (SD = 16.9). The average body mass index of the yoga group was 32.83 (SD = 3.67), and the stretching group was 30.90 (SD = 6.0). The average PEG score out of 30 points of the yoga group was 12.75 (SD = 6.18), and the stretching group was 13.7 (SD = 7.67).
Table 1.
A Comparison of the Population Baseline Characteristics Between the Yoga Group (n = 10) and Stretching Group (n = 10) for the Number of Subjects by Sex and Age, Body Fat, and Pain Mean (Standard Deviation) And Median
| Yoga group n = 10 | Stretching group n = 10 | |
|---|---|---|
| Sex | ||
| Male, n | 8 | 9 |
| Female, n | 2 | 1 |
| Age, y | ||
| Mean (SD) | 51.7 (14.9) | 50.3 (16.9) |
| Median | 54 | 47 |
| Body mass index | ||
| Mean (SD) | 32.83 (3.67) | 30.90 (6.0) |
| Median | 32.68 | 32.41 |
| Pain, PEG out of 30 points | ||
| Mean (SD) | 12.75 (6.18) | 13.7 (7.67) |
| Median | 14.5 | 14 |
SD, standard deviation.
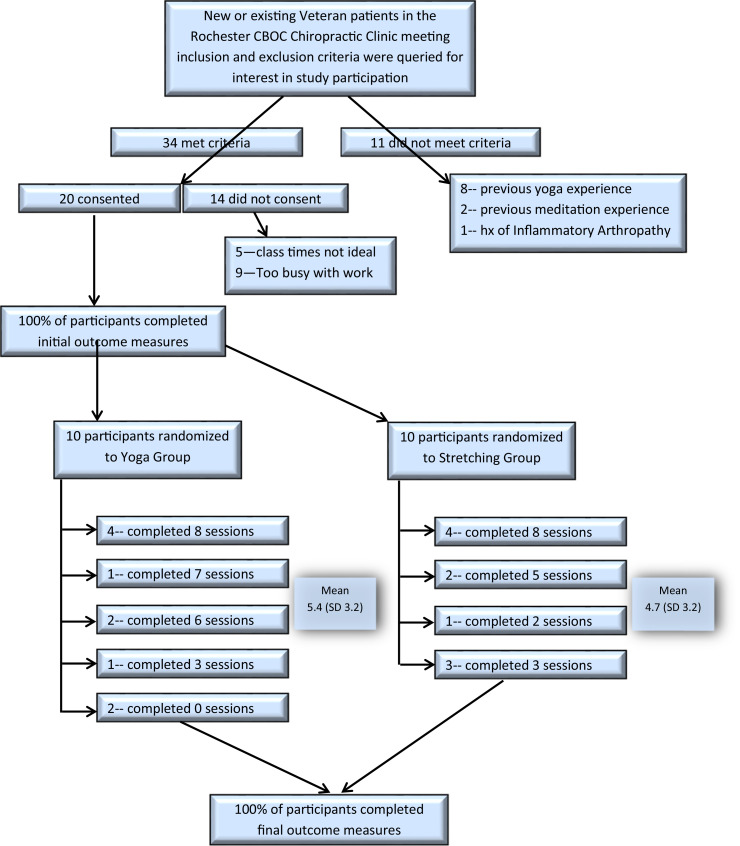
The average number of classes completed for the yoga group was 5.4 (SD = 3.24) and stretching 4.7 (SD = 3.20). The yoga group averaged 2.52 days per week with an average of 20.37 minutes per home practice, whereas the stretching group averaged 2.32 days per week of home practice with an average practice time of 17.56 minutes. There were 2 participants in the yoga group who did not attend any of the classes, and all participants in the stretching group attended at least 1 class. Altogether, there were 11 participants who attended 6 or more classes (7 in yoga, 4 in stretching). There were 8 who attended all 8 sessions (4 in yoga and 4 in stretching, or 40% per group) (Fig 2). Reasons for attending less than 8 sessions were fear of hurting oneself, time constraints, change in work schedule, the death of a family member, being on vacation, or other unrelated health problems.
Fig 2.
Yoga pilot study flow chart.
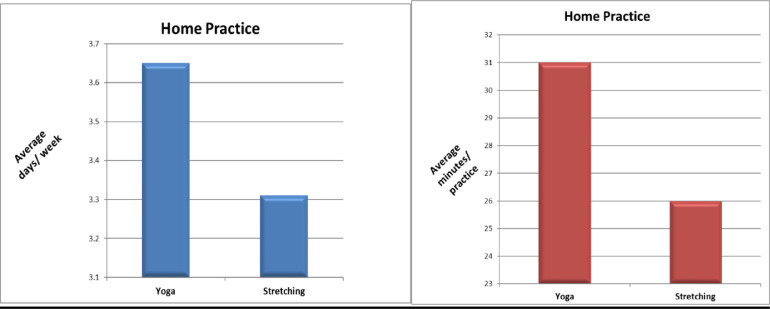
There were 4 participants in the yoga group and 2 in the stretching group who averaged 3 or more days of home practice and 30 minutes or more of practice per session. There were 6 people who averaged over 20 minutes in the yoga group and 6 in the stretching group. There were 2 participants in yoga and 4 in the stretching group who did no home practice at all (Fig 3).
Fig 3.
A comparison of home practice average minutes per practice and average days per week of both groups (yoga n = 10) (stretching n = 10).
Postintervention Clinician Open-Ended Questions
What were the barriers to recruitment and enrollment of participants?
The primary perceived barrier noted by both clinicians was a larger group of veterans having prior experience with yoga or meditation. This originally excluded 8 veterans. We attempted to account for this with an amendment to the protocol stating, “no active engagement in a structured yoga or meditation class within the past 3 months.” The amendment was approved; however, in the interim they were able to recruit 20 veterans who had no prior yoga or meditation experience. They also felt the class time being mid-day limited the number of participants available because of work conflicts.
What were the barriers to collecting outcomes?
The clinicians felt the limited time allotted for participants to complete outcome measures at baseline was challenging, as the enrollment was embedded into a typical chiropractic visit time slot of 30 minutes. Additionally, they anticipated outcome collection to be more challenging than it proved to be. With the foresight of including or allowing phone collection of outcomes postintervention in the original informed consent, they were able to collect outcomes on 100% of participants. There were 5 veterans whom they did need to call to complete post-treatment outcome measures.
What barriers were encountered in regard to carrying out the group classes?
The clinicians felt the size of the room utilized for classes limited the number of participants per class creating a barrier to larger enrollment. Additionally, they noted that although they would have been able to fit more participants in the room, a few veterans made it clear they were uncomfortable if another participant's mat was too close to theirs, limiting their enjoyment of the class. In addition, veterans in general did not like the instructor walking behind them. A few of them voiced concern for PTSD symptoms being provoked unknowingly. Additionally, it was challenging when a participant showed up late to the yoga group after the beginning integration breathing poses had begun, as it disrupted other participants. They did attempt to use the distraction as a learning opportunity to encourage the participants to use their breathing techniques to bring an awareness back to their own self and to use this technique off the mat in their daily lives as well.
What were the barriers to patient accountability?
There was no monetary incentive for patients to complete all 8 classes and no incentive to complete home care exercises, which created a barrier to accountability. This led to a wide spectrum of compliance primarily depending on each participants interest.
Did you feel the classes were well received by the patients or did you encounter any constructive feedback from patients?
The clinicians did feel the classes were well received by the veterans. Many who were apprehensive to try yoga and may have had a preconceived notion that yoga classes are only for flexible or athletic body types surprised themselves with their ability to participate in the entire class, learning modifications as needed. The constructive feedback they received primarily focused on the limited space of the room and the limitations of the class times for veterans who worked.
Harms
Although there were no reported harms during the study for any participants, of note 1 participant did not return after the first class for fear of hurting themselves with exercise.
Discussion
Exercise is a safe and moderately effective treatment for CLBP28; however, the literature remains limited in understanding the types and duration of exercises that are more beneficial than others.29 The majority of studies currently in the literature evaluating yoga for CLBP utilized a type of yoga that incorporated a physical posture and exercise component. It can be concluded that yoga has the potential to alleviate low back pain4,17, 18, 19, 20, 21 and is noninferior to other conservative options.20 There remains contention, however, regarding the therapeutic mechanism of yoga's effectiveness,16 as the literature is limited in defining the specific and nonspecific therapeutic mechanisms of the intervention. The goal of our project was to determine whether the mindfulness aspect of yoga contributes to improvement of CLBP in veterans, and although this project is only a first step, it has helped to inform the design of a future trial. In reviewing the literature, it appears that this study is the only one to teach yoga poses without mindfulness as an active comparison to a yoga intervention.16 Other studies have used physical therapy, calisthenics, or other dis-similar active interventions, and others have used inactive comparators.
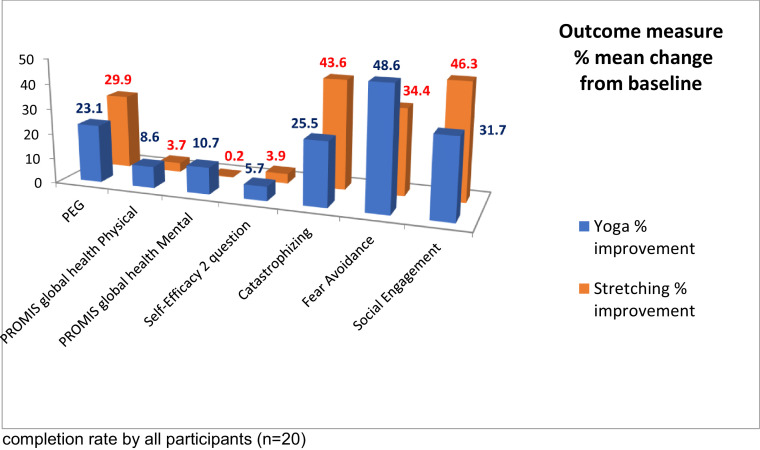
The purpose of this feasibility study was to investigate the ability to recruit, enroll, and collect outcomes on 20 patients with CLBP randomized to 1 of 2 interventions. We were able to achieve both primary and secondary objectives for this study with 100% completion rate of outcome measures. This was a feasibility study and, therefore, statistical analysis was limited to descriptive statistics; it is interesting that on average both groups showed improvement in postintervention outcome assessments. (Fig 4 and Table 2). Because the study sample sizes are too small to demonstrate any clinical significance between the 2 groups, there were clearly responders that eagerly took to attending regular classes and engaging in self-care. The data from the current project will inform the design of a larger, prospective randomized controlled trial assessing a biopsychosocial treatment approach for veterans with CLBP.
Fig 4.
A comparison of postintervention outcome measure % mean change from baseline with 100% completion rate by all participants (n = 20).
Table 2.
A Comparison of Outcome Measures Collected at Baseline and Postintervention Between Yoga Group (n = 10) and Stretching Group (n = 10) for Mean (Standard Deviation)
| Outcomes | Measurement time | Yoga (SD) | Stretching (SD) |
|---|---|---|---|
| PEG | Pre | 13 (6.18) | 14 (7.70) |
| Post | 10 (6.80) | 10 (7.43) | |
| GH physical | Pre | 41 (3.98) | 42 (5.92) |
| Post | 44 (5.40) | 43 (6.63) | |
| GH mental | Pre | 46 (6.68) | 47 (10.23) |
| Post | 50 (8.00) | 48 (13.77) | |
| Self-efficacy | Pre | 9 (2.70) | 8 (3.50) |
| Post | 9 (2.41) | 8 (3.75) | |
| Catastrophizing | Pre | 5 (2.83) | 6 (1.65) |
| Post | 4(1.78) | 3 (2.60) | |
| Fear avoidance | Pre | 4 (2.88) | 3 (3.01) |
| Pre | 2 (2.49) | 2 (3.25) | |
| Behavioral disengagement | Pre | 4 (3.00) | 5 (3.13) |
| Post | 3 (2.90) | 3 (3.41) |
GH, Global Health PROMIS tool; SD, standard deviation.
Limitations
The study was limited by its small sample size. Logistical barriers such as timing of the classes, size of the room, and additional time needed during a typical chiropractic visit to include administering research consent documents and outcome measures were also identified as limitations in this study.
Generalizability
This pilot study does not create generalizable knowledge. Further studies are necessary to better understand the specific and nonspecific mechanisms of yoga in the management of CLBP.
Future Studies
Future appropriately powered trials need to be performed that address the identified barriers during this pilot, which include the timing or availability of the classes to improve accessibility and clarification of definitions of inclusion/exclusion criteria to assure no bias, while still allowing enough people to be enrolled. Additionally, given the pragmatic nature in the methodology of this study, future studies should consider a more stringent yoga protocol in terms of scripting the classes for consistent delivery. Although we recognize a limitation to scripting the classes to include identical postures and movements across both groups lessens the translational interpretation to a real-world setting, it is important in the early phase of yoga literature to create reproduceable studies for validation. Additionally, we will track concomitant interventions in a future study to determine whether certain types of care are confounders and will also assess expectations and beliefs before randomization.
Objectives of Future/Larger RCT
The objectives of a future trial would be to assess the clinical effects of yoga versus stretching in veterans experiencing CLBP using a randomized controlled design. The overall purpose of this study is to evaluate the mechanism by which yoga is effective for CLBP.
Conclusion
It is feasible to enroll, randomize, and collect data on veterans who participate in a trial design that evaluates yoga with and without mindfulness. The strength of the current study is that it has demonstrated that veterans with CLBP are willing and able to participate in the current study design. The most important part of the study was the identification of potential barriers that must be acknowledged before initiating a larger trial. Although no statistical significance was noted between groups, it is important to note that all the participating veterans demonstrated improvements. Given the subjective role of socialization being an important factor in the therapeutic effects, future trials should consider both quantitative and qualitative assessment of socialization. We feel that this study is an important first step in better understanding why those who participate in yoga programs show improvement in pain, and further study will help to refine interventions that will have a greater therapeutic benefit.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): LR, PD, NE
Design (planned the methods to generate the results): LR, PD, NE
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): LR
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): LR, NE
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): LR, NE
Literature search (performed the literature search): NE
Writing (responsible for writing a substantive part of the manuscript): LR
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): LR, PD
Other (list other specific novel contributions):
Practical Applications.
-
•
This study addresses the limitations of previous yoga studies lacking an appropriate and similar comparison control group.
-
•
This was a novel design comparing yoga (which consisted of typical yoga exercise postures to include meditative breathing instruction, self-introspection, and non-judgmental awareness) to yoga exercise postures alone without the mindfulness aspects.
-
•
Although this pilot study was not powered for comparative effectiveness of the interventions, it proved feasibility of performing the larger RCT.
Alt-text: Unlabelled box
References
- 1.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Atkinson C, Bhalla K. The state of US Health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goulet JL, Kerns RD, Bair M. The musculoskeletal diagnosis cohort: examining pain and pain care among veterans. Pain. 2016;157(8):1696–1703. doi: 10.1097/j.pain.0000000000000567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Foster NE, Anema JR, Cherkin D. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–2383. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 5.Cohen SP, Gallagher RM, Davis SA, Griffith SR, Carragee EJ. Spine-area pain in military personnel: a review of epidemiology, etiology, diagnosis, and treatment. Spine J. 2012;12(9):833–842. doi: 10.1016/j.spinee.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 6.Vallerand AH, Cosler P, Henningfield JE, Galassini P. Pain management strategies and lessons from the military: A narrative review. Pain Res Manag. 2015;20(5):261–268. doi: 10.1155/2015/196025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19(12):2075–2094. doi: 10.1007/s00586-010-1502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qaseem A, Wilt TJ, McLean RM, Forciea MA. Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 9.Chou R, Deyo R, Friedly J. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017;166(7):493–505. doi: 10.7326/M16-2459. [DOI] [PubMed] [Google Scholar]
- 10.Wang CC, Li K, Choudhury A, Gaylord S. Trends in yoga, tai chi, and qigong use among US adults, 2002-2017. Am J Public Health. 2019;109(5):755–761. doi: 10.2105/AJPH.2019.304998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wieland LS, Skoetz N, Pilkington K, Vempati R, D'Adamo CR, Berman BM. Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst Rev. 2017;1(1) doi: 10.1002/14651858.CD010671.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang DG, Holt JA, Sklar M, Groessl EJ. Yoga as a treatment for chronic low back pain: A systematic review of the literature. J Orthop Rheumatol. 2016;3(1):1–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Skelly AC, Chou R, Dettori JR. Agency for Healthcare Research and Quality (US); Rockville (MD): 2018. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review. [PubMed] [Google Scholar]
- 14.Goode AP, Coeytaux RR, McDuffie J. An evidence map of yoga for low back pain. Complement Ther Med. 2016;25:170–177. doi: 10.1016/j.ctim.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 15.Coeytaux RR, McDuffie J, Goode A. Department of Veterans Affairs (US); Washington, DC: 2014. Evidence Map of Yoga for High-Impact Conditions Affecting Veterans. [PubMed] [Google Scholar]
- 16.Park CL, Groessl E, Maiya M. Comparison groups in yoga research: a systematic review and critical evaluation of the literature. Complement Ther Med. 2014;22(5):920–929. doi: 10.1016/j.ctim.2014.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Posadzki P, Ernst E. Yoga for low back pain: a systematic review of randomized clinical trials. Clin Rheumatol. 2011;30(9):1257–1262. doi: 10.1007/s10067-011-1764-8. [DOI] [PubMed] [Google Scholar]
- 18.Tilbrook HE, Cox H, Hewitt CE. Yoga for chronic low back pain: a randomized trial. Ann Intern Med. 2011;155(9):569–578. doi: 10.7326/0003-4819-155-9-201111010-00003. [DOI] [PubMed] [Google Scholar]
- 19.Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005;143(12):849–856. doi: 10.7326/0003-4819-143-12-200512200-00003. [DOI] [PubMed] [Google Scholar]
- 20.Saper RB, Lemaster C, Delitto A. Yoga, physical therapy, or education for chronic low back pain: A randomized noninferiority trial. Ann Intern Med. 2017;167(2):85–94. doi: 10.7326/M16-2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Groessl EJ, Liu L, Chang DG. Yoga for military veterans with chronic low back pain: A randomized clinical trial. Am J Prev Med. 2017;53(5):599–608. doi: 10.1016/j.amepre.2017.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Report. 2015;(79):1–16. [PMC free article] [PubMed] [Google Scholar]
- 23.Gaudet T, Kligler B. Whole health in the whole system of the Veterans Administration: How will we know we have reached this future state? Altern Complement Med. 2019;25(S1):S7–S11. doi: 10.1089/acm.2018.29061.gau. [DOI] [PubMed] [Google Scholar]
- 24.Kligler B, Bair MJ, Banerjea R. Clinical policy recommendations from the VHA state-of-the-art conference on non-pharmacological approaches to chronic musculoskeletal pain. J Gen Intern Med. 2018;33(Suppl 1):16–23. doi: 10.1007/s11606-018-4323-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schalet BD, Rothrock NE, Hays RD. Linking physical and mental health summary scores from the Veterans RAND 12-Item Health Survey (VR-12) to the PROMIS(®) Global Health Scale. J Gen Intern Med. 2015;30(10):1524–1530. doi: 10.1007/s11606-015-3453-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krebs EE, Lorenz KA, Bair MJ. Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J Gen Intern Med. 2009;24(6):733–738. doi: 10.1007/s11606-009-0981-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nicholas MK, McGuire BE, Asghari A. A 2-item short form of the Pain Self-efficacy Questionnaire: development and psychometric evaluation of PSEQ-2. J Pain. 2015;16(2):153–163. doi: 10.1016/j.jpain.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 28.Carey TS. Comparative effectiveness studies in chronic low back pain: Progress and goals. Arch Intern Med. 2011;171(22):2026–2027. doi: 10.1001/archinternmed.2011.519. [DOI] [PubMed] [Google Scholar]
- 29.Hayden JA, van Tulder MW, Malmivaara AV, Koes BW. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142(9):765–775. doi: 10.7326/0003-4819-142-9-200505030-00013. [DOI] [PubMed] [Google Scholar]