Abstract
Rationale & Objective
Hyperkalemia is a common electrolyte abnormality of chronic kidney disease and heart failure associated with increased mortality and morbidity. We aimed to assess the long-term economic burden of hyperkalemia.
Design
Observational cohort study using a Japanese nationwide hospital claims database (April 1, 2008, to September 30, 2018).
Setting & Population
: Patients 18 years or older with at least 1 serum potassium value (N = 1,208,894).
Exposures
Hyperkalemia defined with the presence of at least 2 serum potassium values ≥ 5.1 mmol/L.
Outcome Measures
Direct health care costs and resource use in patients with hyperkalemia within and after 12 months from first hyperkalemia episodes.
Analytical Approach
Health care costs and resource use were compared with propensity score–matched or nonmatched normokalemic controls. Multivariable regression analysis was performed to examine factors associated with health care costs.
Results
27,534 patients with hyperkalemia and 233,098 normokalemic controls were studied. Mean ± SD age was 73±13 years in patients with hyperkalemia; among them, 59% and 35% had chronic kidney disease and heart failure, respectively. In the propensity score–matched cohort (n = 5,859 in each group), average numbers of hospitalizations per patient per year in patients with hyperkalemia within and after 12 months were 1.2 and 1.6 times higher, respectively, compared with those in patients with normokalemia. The total cost per patient in patients with hyperkalemia was higher than for controls, with mean differences of $8,611 (95% CI, $8,046-$9,175) within 12 months and $5,150 (95% CI, $4,733-$5,566) after 12 months. The number of repeat hyperkalemic episodes was the factor with the strongest association with long-term health care costs, whereas severity of hyperkalemia was not associated.
Limitations
This study used secondary data; therefore, residual confounders may not be fully excluded.
Conclusions
Hyperkalemia was associated with significant long-term economic burden with frequent hospitalizations due to recurrent episodes, indicating the importance of hyperkalemia treatment for the sake of reducing health economic burdens and clinical complications.
Index Words: Hyperkalemia, chronic kidney disease (CKD), heart failure (HF), healthcare cost, health economics
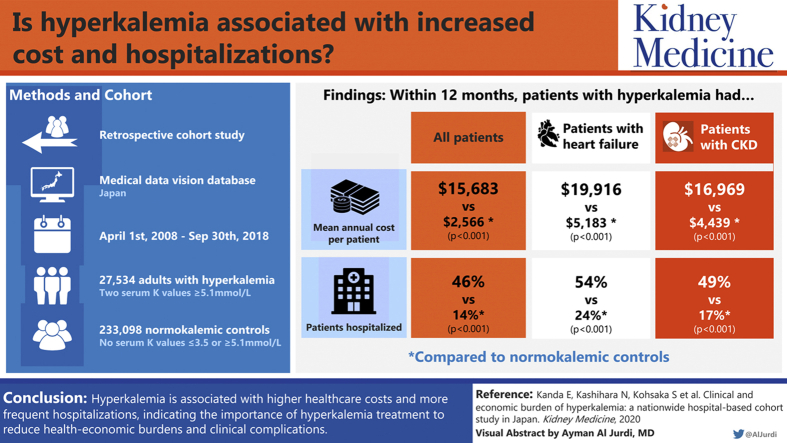
Graphical abstract
Plain-Language Summary.
Hyperkalemia is a common electrolyte level abnormality associated with increased mortality and morbidity. We conducted an observational cohort study using a Japanese nationwide hospital claims database to assess long-term health care costs and resource use in patients with hyperkalemia compared with normokalemia. Based on propensity score–matching analyses, we found increased numbers of hospitalizations in hyperkalemic patients, resulting in higher total health care cost per patient by $8,611 within 12 months and $5,150 after 12 months. The number of repeat hyperkalemic episodes was the most significant factor associated with long-term health care costs. Hyperkalemia was associated with significant long-term economic burden with frequent hospitalizations due to recurrent episodes, indicating the importance of hyperkalemia treatment for the sake of reducing health economic burdens and clinical complications.
Hyperkalemia, characterized as abnormally elevated serum potassium levels, is a common electrolyte abnormality of chronic kidney disease (CKD), heart failure (HF), diabetes mellitus (DM), and in patients who are treated with renin-angiotensin-aldosterone system (RAAS) inhibitors that is associated with increased mortality and morbidity.1, 2, 3 Hyperkalemia is often asymptomatic but sometimes results in muscle weakness, paralysis, life-threatening cardiac arrhythmias, and sudden death.4 Common treatments for hyperkalemia include diet restriction, downtitration/discontinuation of RAAS inhibitor treatment, use of diuretics, hemodialysis, and glucose-insulin injection. Potassium binders have also been used to treat both episodic and chronic hyperkalemia.4, 5, 6 However, patients often experience recurrent hyperkalemic episodes.7,8
Recently, hyperkalemia is increasingly recognized as a potential marker that may reflect the general conditions of patients.9 Studies have reported a U-shaped association between serum potassium levels and adverse clinical outcomes.7,10, 11, 12, 13 In addition to the prognosis of patients, hyperkalemia can lead to significant increases in health care costs. Despite the substantial data for epidemiology, practice patterns, and long-term prognoses, there is limited information about the economic burden of hyperkalemia. Previous studies have shown an increased numbers of hospitalizations and emergency visits and longer duration of hospital stays. However, evaluation of the health care costs and resource usse was performed in relatively short periods (eg, within 12 months), and the long-term economic burden remains to be elucidated.14, 15, 16 Moreover, given the differences in health care systems, it is important to assess the economic burden of hyperkalemia in disparate regions.
In this study, we investigated long-term health care costs and resource use in patients with hyperkalemia using one of the largest hospital claims databases in the Japanese health care system, in which the comprehensive health care cost information can be captured based on the single-insurer system. To assess hyperkalemia-associated costs, we examined health care costs and resource use in patients with hyperkalemia and compared that with propensity score–matched patients with normal serum potassium level ranges. Furthermore, we assessed contributing factors to the health care cost in patients with hyperkalemia to identify the high-risk profile of patients who are likely to incur higher health care costs.
Methods
Data Source
The data used for this study were extracted from the Medical Data Vision (MDV), one of the largest hospital claims databases in Japan. MDV collects hospital claims data with a diagnostic and procedural coding system that includes individual drug prescriptions, procedures, examinations, and laboratory data. Data collection began in April 2008. As of September 2018, MDV consisted of 25,570,000 individual patient records from 374 hospitals across all geographic regions in Japan. MDV uses International Classification of Diseases, Tenth Revision (ICD-10) coding.
Study Design and Patient Selection
This was a retrospective cohort study to assess health care costs and resource use. We extracted patients 18 years and older whose records included at least 1 serum potassium value within the study period of April 1, 2008, to September 30, 2018. Excluded from the analysis were patients who could not be followed up 12 months after the index date, patients with a cancer diagnosis, and patients undergoing dialysis before the index date. Patients with hyperkalemia were defined as patients who had at least 2 serum potassium values ≥ 5.1 mmol/L within the 12-month interval during the study period, based on the definition used in previous studies.7,17 A 12-month interval was selected for the 2 serum potassium measurements to enroll patients who were likely to have persistent hyperkalemia and were continuously treated in clinical practice. Hyperkalemia episodes were defined as episodes with serum potassium values ≥ 5.1 mmol/L. We also extracted patients with no record of serum potassium levels ≤ 3.5 mmol/L or ≥5.1 mmol/L as normokalemic controls. To assess economic burden in patients with high-risk comorbid conditions, we extracted 4 separate cohorts of patients with hyperkalemia and normokalemic controls from the database, overall, chronic kidney disease (CKD), HF, and patients without CKD/HF. The index date for patients with hyperkalemia was set as the date of their first episode of hyperkalemia. Normokalemic controls were followed up after their first visit for at least 12 months from their initial hospital record or at their first diagnosis of CKD or HF. Each individual was followed up until their emigration from the database, death, or the end of the study period, whichever came first.
Covariates and Health Economic Outcomes
Subgroups of known high-risk comorbid conditions associated with hyperkalemia, including CKD, HF, DM, and hypertension,4,5,18 were defined using the recorded ICD-10 codes and estimated glomerular filtration rate (Table S1). CKD stages were categorized based on estimated glomerular filtration rates. Other comorbid conditions were also collected based on ICD-10 diagnoses to calculate the Charlson Comorbidity Index score (Table S2). Considering commonly used intervals of drug prescriptions in Japanese clinical practice, information for drug treatments was collected from 120 days before the index date. RAAS inhibitor treatment (ie, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and mineralocorticoid receptor antagonists) and drugs for kidney diseases, including erythropoiesis-stimulating agents (ESAs), phosphate binders, active vitamin D, uremic toxin absorbents, sodium bicarbonate, and potassium binders, were collected from the medical records.
Direct health care costs and resource use within 12 months from the index date and after 12 months until the end of patient follow-up were collected based on hospital activity records. Health care costs for all prescriptions, medical examinations, procedures, operations, and other costs were summarized and described within and after 12 months. Health care costs were also summarized as cost per hospitalization, outpatient visit, or emergency visit. All unit costs were calculated based on the national medical fee points table issued by the Japan’s Ministry of Health, Labour, and Welfare for each calendar year in which the resource use occurred. Health care costs were converted to US dollars using Organisation for Economic Co-operation and Development exchange rates based on purchasing-power parities from 2017; thus, US $1 equaled 102.470 Japanese yen.19 We also collected the number of all-cause hospitalizations, rehospitalizations (defined as hospitalization within 30 days from the discharge of a prior hospitalization), emergency visits, and outpatient visits. Lengths of stay per hospital admission were also assessed for patients who had at least 1 hospitalization.
Statistical Analysis
Continuous variables were reported as mean, standard deviation, and median. Frequency and percentage were used to document categorical measures of interest. We calculated 95% CIs for mean values. Patients with hyperkalemia were stratified by the number of hyperkalemia episodes recorded within 12 months after their first episode. Analyses of health care costs and resource use after 12 months were conducted by re-indexing the patient follow-up at 12 months after the original index date.
To measure differences in health care costs and resource use considering substantially different patient characteristics, we built a propensity score–matched cohort of patients with hyperkalemia and controls. We developed a propensity score for having hyperkalemia using these covariates: age, sex, index year, lengths of follow-up, prescription of RAAS inhibitor, other drugs associated with hyperkalemia, diuretics, antidiabetic medications, presence of comorbid conditions (including CKD stage, HF, DM, hypertension, dyslipidemia, atrial fibrillation or atrial flutter, valvular heart disease, acute kidney injury, sepsis, or peripheral edema), Charlson Comorbidity Index score, and history of hospitalization of 3 or more consecutive days before the index date using a multivariable logistic regression model. Patients with hyperkalemia were matched 1:1 with normokalemic controls based on the developed propensity score, with a caliper width of 0.1. The validity of propensity score matching was assessed by evaluating standardized differences of patient characteristics. A standardized difference > 0.1 was considered as a significant imbalance between the 2 groups after propensity score matching.
In addition, we performed multivariable regression analysis using generalized linear models with gamma distribution to assess factors associated with health care costs in patients with hyperkalemia.20,21 Covariates included in the model were CKD, HF, DM, hypertension, dyslipidemia, age (ie, 18-44, 45-64, 65-74, and ≥75 years), serum potassium level (5.1-5.4, 5.5-5.9, and ≥6.0 mmol/L), Charlson Comorbidity Index score, hospital admission at index date, history of hospitalization for 3 or more consecutive days 12 months before the index date, sex, use of RAAS inhibitors, and use of serum potassium-lowering drugs including diuretics and potassium binders for health care costs within 12 months. The number of hyperkalemia episodes within 12 months was added to the model after 12 months.
All statistical analyses were performed using SAS software, version 9.4 (SAS Institute). The study followed STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) reporting guidelines (Item S1). Because patient records were already anonymized and deidentified, informed consent was not obtained. Use of deidentified data was in accordance with local regulations. This study was reviewed and approved by an independent ethics committee (Clinical Research Promotion Network Japan: 2440023).
Results
We identified 74,974 patients with hyperkalemia and 469,016 normokalemic controls from the total of 1,208,894 patients who had at least 1 serum potassium measurement. After excluding patients who could not be followed up for 12 months (18,594 with hyperkalemia vs 158,965 controls), patients who had already undergone dialysis by the index date (2,999 with hyperkalemia vs 148 controls), and patients who had a cancer diagnosis during the study period (25,847 with hyperkalemia vs 76,805 controls), we included the following numbers of patients (hyperkalemia vs controls) in each cohort: (1) overall, 27,534 versus 233,098; (2) CKD, 16,133 versus 15,287; (3) HF, 9,674 versus 27,628; and (4) without CKD/HF, 7,049 versus 187,012. Patient flow diagrams of each cohort are depicted in Figure S1. Baseline characteristics of hyperkalemic patients and controls are summarized in Table 1.
Table 1.
Characteristics of Patients With Hyperkalemia and Normokalemic Controls
| Overall |
CKD |
HF |
Without CKD/HF |
|||||
|---|---|---|---|---|---|---|---|---|
| Hyperkalemia (N = 27,534) | Normokalemia (N = 233,098) | Hyperkalemia (N = 16,133) | Normokalemia (N = 15,287) | Hyperkalemia (N = 9,674) | Normokalemia (N = 27,628) | Hyperkalemia (N = 7,049) | Normokalemia (N = 187,012) | |
| Mean age, y | 73 ± 13 | 60 ± 17 | 73 ± 13 | 68 ± 14 | 77 ± 12 | 69 ± 13 | 69 ± 15 | 58 ± 17 |
| Age group | ||||||||
| 18-64 y | 6,471 (24%) | 125,579 (54%) | 3,576 (22%) | 5,288 (35%) | 1,460 (15%) | 8,748 (32%) | 2,240 (32%) | 109,102 (58%) |
| 65-79 y | 11,397 (41%) | 82,505 (35%) | 6,850 (42%) | 6,968 (46%) | 3,573 (37%) | 12,738 (46%) | 2,942 (42%) | 61,610 (33%) |
| 80+ y | 9,666 (35%) | 25,014 (11%) | 5,707 (35%) | 3,031 (20%) | 4,641 (48%) | 6,142 (22%) | 1,867 (26%) | 16,300 (9%) |
| Male sex | 15,167 (55%) | 107,586 (46%) | 9,109 (56%) | 8,617 (56%) | 5,042 (52%) | 15,786 (57%) | 3,857 (55%) | 81,797 (44%) |
| Length of follow-up, mo | 34.8 ± 24.9 | 44.2 ± 23.4 | 37.5 ± 24.3 | 44.1 ± 21.9 | 29.8 ± 23.8 | 42.9 ± 25.2 | 33.1 ± 25.8 | 43.0 ± 22.4 |
| Serum potassium at index date, mmol/L | 5.4 ± 0.5 | 4.2 ± 0.3 | 5.4 ± 0.5 | 4.3 ± 0.3 | 5.4 ± 0.5 | 4.2 ± 0.3 | 5.4 ± 0.5 | 4.2 ± 0.3 |
| Serum potassium group | ||||||||
| ≥5.1-<5.5 mmol/L | 19,647 (71%) | 0 (0%) | 11,221 (70%) | 0 (0%) | 6,730 (70%) | 0 (0%) | 5,261 (75%) | 0 (0%) |
| ≥5.5-<6.0 mmol/L | 5,644 (21%) | 0 (0%) | 3,460 (21%) | 0 (0%) | 2,082 (22%) | 0 (0%) | 1,313 (19%) | 0 (0%) |
| ≥6.0-<6.5 mmol/L | 1,346 (5%) | 0 (0%) | 898 (6%) | 0 (0%) | 508 (5%) | 0 (0%) | 261 (4%) | 0 (0%) |
| ≥6.5-<7.0 mmol/L | 488 (2%) | 0 (0%) | 314 (2%) | 0 (0%) | 200 (2%) | 0 (0%) | 104 (1%) | 0 (0%) |
| ≥7.0 mmol/L | 409 (1%) | 0 (0%) | 240 (1%) | 0 (0%) | 154 (2%) | 0 (0%) | 110 (2%) | 0 (0%) |
| CKD | 16,133 (59%) | 11,898 (5%) | 16,133 (100%) | 15,287 (100%) | 6,394 (66%) | 2,827 (10%) | 0 (0%) | 0 (0%) |
| Stage 1 | 200 (1%) | 1,086 (9%) | 200 (1%) | 1,173 (8%) | 47 (1%) | 106 (4%) | 0 (0%) | 0 (0%) |
| Stage 2 | 1,140 (7%) | 3,821 (32%) | 1,140 (7%) | 4,514 (30%) | 331 (5%) | 674 (24%) | 0 (0%) | 0 (0%) |
| Stage 3a | 2,655 (16%) | 4,652 (39%) | 2,655 (16%) | 6,586 (43%) | 975 (15%) | 1,244 (44%) | 0 (0%) | 0 (0%) |
| Stage 3b | 4,128 (26%) | 1,815 (15%) | 4,128 (26%) | 2,345 (15%) | 1,787 (28%) | 620 (22%) | 0 (0%) | 0 (0%) |
| Stage 4 | 4,745 (29%) | 379 (3%) | 4,745 (29%) | 430 (3%) | 2,060 (32%) | 137 (5%) | 0 (0%) | 0 (0%) |
| Stage 5 | 3,265 (20%) | 145 (1%) | 3,265 (20%) | 239 (2%) | 1,194 (19%) | 46 (2%) | 0 (0%) | 0 (0%) |
| HF | 9,674 (35%) | 19,021 (8%) | 6,394 (40%) | 3,182 (21%) | 9,674 (100%) | 27,628 (100%) | 0 (0%) | 0 (0%) |
| Diabetes | 11,344 (41%) | 25,602 (11%) | 7,717 (48%) | 6,893 (45%) | 4,190 (43%) | 5,261 (19%) | 2,163 (31%) | 15,947 (9%) |
| Hypertension | 18,105 (66%) | 71,517 (31%) | 12,196 (76%) | 9,915 (65%) | 7,582 (78%) | 20,344 (74%) | 3,082 (44%) | 43,168 (23%) |
| Dyslipidemia | 7,439 (27%) | 32,603 (14%) | 5,057 (31%) | 5,360 (35%) | 3,129 (32%) | 9,087 (33%) | 1,292 (18%) | 18,997 (10%) |
| Charleson Comorbidity Index score | 1.1 ± 1.2 | 0.5 ± 0.8 | 1.1 ± 1.2 | 0.9 ± 1.0 | 1.3 ± 1.2 | 1.0 ± 1.1 | 1.0 ± 1.2 | 0.4 ± 0.7 |
| RAASi treatment | 12,102 (44%) | 34,012 (15%) | 8,314 (52%) | 6,090 (40%) | 5,793 (60%) | 10,669 (39%) | 1,710 (24%) | 18,127 (10%) |
| ACEi | 2,414 (9%) | 4,631 (2%) | 1,649 (10%) | 825 (5%) | 1,494 (15%) | 2,091 (8%) | 227 (3%) | 1,945 (1%) |
| ARB | 8,906 (32%) | 29,169 (13%) | 6,391 (40%) | 5,254 (34%) | 3,587 (37%) | 8,151 (30%) | 1,332 (19%) | 16,272 (9%) |
| MRA | 3,688 (13%) | 2,410 (1%) | 2,401 (15%) | 559 (4%) | 2,840 (29%) | 1,851 (7%) | 303 (4%) | 418 (0.2%) |
| Thiazide diuretics | 567 (2%) | 1,616 (1%) | 481 (3%) | 349 (2%) | 240 (2%) | 354 (1%) | 43 (1%) | 811 (0.4%) |
| Loop diuretics | 5,247 (19%) | 3,020 (1%) | 3,693 (23%) | 756 (5%) | 3,724 (38%) | 2,146 (8%) | 383 (5%) | 380 (0.2%) |
Note: Values expressed as mean ± standard deviation or number (percent).
Abbreviations: ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CKD, chronic kidney disease; HF, heart failure; MRA, mineralocorticoid receptor antagonist; RAASi, renin-angiotensin-aldosterone system inhibitor.
Health Care Cost
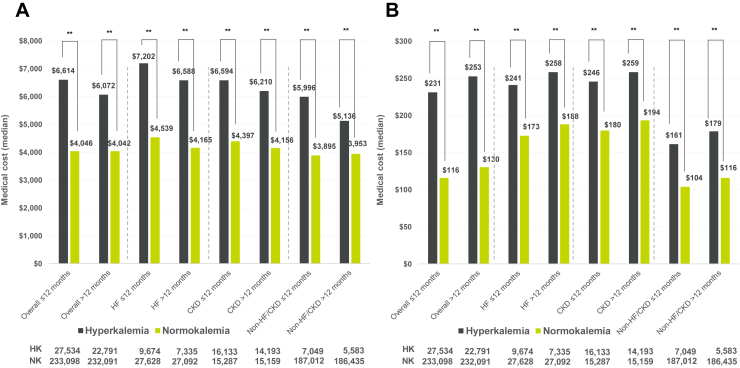
Figure 1 shows inpatient and outpatient costs within and after 12 months of follow-up in patients with hyperkalemia and controls. Median inpatient and outpatient costs per visit were 1.6 and 2 times higher in patients with hyperkalemia within 12 months (inpatient, $6,614 [interquartile range (IQR), $3,584-$12,977] vs $4,046 [IQR, $2,046-$7,699]; outpatient, $231 [IQR, $88-$380] vs $116 [IQR, $49-$230]) and 1.5 and 2 times higher after 12 months (inpatient, $6,072 [IQR, $3,409-$11,434] vs $4,042 [IQR, $2,165-$7,382]; outpatient, $253 [IQR, $141-$388] vs $130 [IQR, $57-$258]) in the overall cohort (all P < 0.001).
Figure 1.
Inpatient and outpatient costs within and after 12 months of follow-up overall and in cohorts of chronic kidney disease (CKD), heart failure (HF), and patients without CKD/HF diagnoses (Non-HF/CKD). (A) Inpatient and (B) outpatient cost (median). ∗∗P < 0.001 versus normokalemia by Wilcoxon rank sum test. Abbreviations: HK, hyperkalemia; NK, normokalemia.
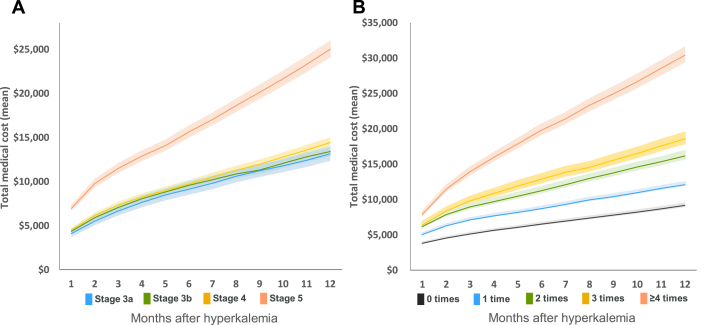
Table 2 summarizes total health care costs and resource use per patient within and after 12 months. Mean total costs in patients with hyperkalemia and controls were $15,683 (95% CI, $15,428-$15,938) versus $2,566 (95% CI, $2,541-$2,591) within 12 months and $9,884 (95% CI, $9,682-$10,085) versus $1,947 (95% CI, $1,927-$1,967) after 12 months (both P < 0.001), respectively. Among patients with hyperkalemia, patients with HF and/or CKD had higher total health care costs than patients without CKD and HF (Fig S2). Total health care costs were the highest in the subgroup with stage 5 CKD, with a mean of $25,006 (95% CI, $24,033-$25,980) within 12 months (Fig 2A). Total health care costs increased with the number of hyperkalemia episodes within 12 months (Fig 2B). Total health care costs within 12 months in patients with 0, 1, 2, 3, and 4 or more hyperkalemia episodes were $9,426 (95% CI, $9,067-$9,785), $12,718 (95% CI, $12,389-$13,048), $17,361 (95% CI, $16,747-$17,975), $20,196 (95% CI, $19,331-$21,061), and $32,122 (95% CI, $30,982-$33,262), respectively (P < 0.001).
Table 2.
Total Health Care Costs and Resource Use Within and After 12 Months of Follow-up in Patients With Hyperkalemia and Normokalemic Controls
| Overall |
CKD |
HF |
Without CKD/HF |
|||||
|---|---|---|---|---|---|---|---|---|
| Hyperkalemia | Normokalemia | Hyperkalemia | Normokalemia | Hyperkalemia | Normokalemia | Hyperkalemia | Normokalemia | |
| Within 12 mo | ||||||||
| N | 27,534 | 233,098 | 16,133 | 15,287 | 9,674 | 27,628 | 7,049 | 187,012 |
| Annual total costs per patient, $ | 15,683a (15,428-15,938) | 2,566 (2,541-2,591) | 16,969a (16,621-17,316) | 4,439 (4,298-4,580) | 19,916a (19,420-20,412) | 5,183 (5,064-5,302) | 11,418a (11,011-11,825) | 2,166 (2,142-2,190) |
| Annual total costs per patient, $ | 7,617a [3,119-19,733] | 938 [345-2,359] | 8,407a [3,582-21,785] | 2,211 [1,106-4,239] | 11,147a [4,458-25,651] | 2,298 [1,082-4,712] | 5,196a [2,072-14,159] | 778 [298-1,952] |
| Patients required hospitalization | 12,531 (46%)a | 32,668 (14%) | 7,968 (49%)a | 2,661 (17%) | 5,198 (54%)a | 6,746 (24%) | 2,465 (35%)a | 24,239 (13%) |
| Patients required rehospitalization | 2,179 (8%)a | 2,526 (1%) | 1,566 (10%)a | 298 (2%) | 1,016 (11%)a | 713 (3%) | 296 (4%)a | 1,665 (1%) |
| Patients required emergency visit | 6,398 (23%)a | 7,459 (3%) | 3,948 (25%)a | 725 (5%) | 3,001 (31%)a | 2,120 (8%) | 1,221 (17%)a | 4,964 (3%) |
| No. of hospitalizations per patient | 1.7 ± 1.1a | 1.2 ± 0.6 | 1.7 ± 1.2a | 1.4 ± 0.8 | 1.7 ± 1.1a | 1.4 ± 0.7 | 1.5 ± 0.9a | 1.2 ± 0.6 |
| No. of emergency visits per patient | 1.3 ± 0.7a | 1.1 ± 0.3 | 1.3 ± 0.7a | 1.1 ± 0.4 | 1.3 ± 0.7a | 1.1 ± 0.4 | 1.2 ± 0.6a | 1.1 ± 0.3 |
| No. of outpatient visits per patient | 13.3 ± 15.7a | 7.3 ± 7.2 | 14.9 ± 18.0a | 9.7 ± 8.3 | 14.0 ± 16.5a | 9.3 ± 8.1 | 10.5 ± 9.2a | 7.0 ± 7.0 |
| Length of hospital stay per hospitalization, d | 23.0 ± 35.3a | 11.1 ± 25.7 | 23.4 ± 35.6a | 11.6 ± 18.5 | 23.9 ± 33.7a | 11.6 ± 32.1 | 21.1 ± 35.3a | 10.7 ± 21.9 |
| After 12 mo | ||||||||
| N | 22,791 | 232,091 | 14,193 | 15,159 | 7,335 | 27,092 | 5,583 | 186,435 |
| Annual total costs per patient, $ | 9,884a (9,682-10,085) | 1,947 (1,927-1,967) | 11,980a (11,702-12,257) | 3,228 (3,115-3,340) | 12,463a (12,046-12,880) | 3,165 (3,072-3,259) | 4,901a (4,630-5,172) | 1,619 (1,601-1,637) |
| Annual total costs per patient, $ | 4,335a [1,468-11,620] | 779 [269-2,079] | 5,839a [2,255-14,671] | 1,823 [753-3,632] | 6,105a [2,176-15,824] | 1,636 [588-3,458] | 1,913a [604-5,010] | 629 [229-1,685] |
| Patients required hospitalization | 11,390 (50%)a | 48,537 (21%) | 8,050 (56.7%)a | 3,600 (24%) | 4,250 (58%)a | 7,121 (26%) | 1,758 (31%)a | 34,660 (18.6%) |
| Patients required rehospitalization | 2,708 (12%)a | 4,700 (2%) | 2,071 (14.6%)a | 414 (3%) | 1,098 (15%)a | 797 (3%) | 298 (5%)a | 3,027 (2%) |
| Patients required emergency visit | 6,371 (28%)a | 12,712 (5%) | 4,558 (32.1%)a | 1,115 (7%) | 2,723 (37%)a | 2,428 (9%) | 849 (15%)a | 8,025 (4%) |
| No. of hospitalizations per patient | 1.0 ± 0.9a | 0.6 ± 0.4 | 1.1 ± 1.0a | 0.6 ± 0.5 | 1.2 ± 1.0a | 0.6 ± 0.5 | 0.9 ± 0.8a | 0.6 ± 0.4 |
| No. of emergency visits per patient | 0.8 ± 0.6a | 0.5 ± 0.4 | 0.8 ± 0.6a | 0.5 ± 0.4 | 0.9 ± 0.7a | 0.5 ± 0.4 | 0.7 ± 0.6a | 0.5 ± 0.3 |
| No. of outpatient visits per patient | 12.5 ± 21.6a | 5.7 ± 5.7 | 15.4 ± 26.2a | 7.7 ± 6.8 | 13.3 ± 22.6a | 7.0 ± 6.6 | 7.4 ± 7.2a | 5.3 ± 5.5 |
| Length of hospital stay per hospitalization, d | 21.1 ± 35.0a | 10.9 ± 21.8 | 21.0 ± 31.8a | 11.7 ± 18.0 | 23.1 ± 38.2a | 11.1 ± 19.4 | 19.2 ± 32.8a | 10.6 ± 20.4 |
Note: Values expressed as mean (95% CI), median [25th-75th percentile], number (percent), or mean ± standard deviation.
Abbreviations: CKD, chronic kidney disease; HF, heart failure.
P < 0.001 versus normokalemic control by analysis of variance for continuous variables and χ2 test or Fisher exact test for categorical variables.
Figure 2.
Cumulative health care costs stratified by chronic kidney disease (CKD) stages and number of hyperkalemic episodes within 12 months after the first hyperkalemic episode: (A) stratification by CKD stages; (B) stratification by number of hyperkalemic episodes within 12 months.
Health Care Resource Use
The proportion of patients with incident hospitalizations per patient was more than 3 times higher in patients with hyperkalemia than controls at 46% versus 14% within 12 months (P < 0.001); after 12 months, the proportion was 2.4 times higher at 50% versus 21% (P < 0.001). Similarly, the proportion of patients with rehospitalization and emergency visits was higher in patients with hyperkalemia than controls (Table 2). Proportions of patients who were prescribed drug treatments for kidney disease (eg, ESAs, phosphate binders, active vitamin D, uremic toxin absorbents, sodium bicarbonate, or potassium binders) increased in advanced CKD stages and were significantly higher in patients with hyperkalemia than controls (Table S3). For example, drug costs per year for ESA in patients with hyperkalemia and controls per patients in each subgroup were $928 versus $686 in stage 3a, $759 versus $785 in stage 3b, $942 versus $888 in stage 4, and $1,128 versus $701 in stage 5 CKD within 12 months, and they were $655 versus $747 in stage 3a, $667 versus $496 in stage 3b, $854 versus $832 in stage 4, and $898 versus $899 in stage 5 CKD after 12 months.
Higher health care costs were incurred from hospitalization for kidney replacement therapy (KRT). The proportion of patients who required hospitalization for KRT was higher in patients with hyperkalemia than controls in all CKD stages. When focused on patients with CKD stage 4 to 5, the cumulative health care cost per patient in patients with hyperkalemia and patients with normokalemia within 12 months were $18,593 and $4,911, for which KRT hospitalization cost accounted for $5,053 and $706, respectively. Therefore, the cumulative health care cost per patient independent of KRT hospitalization cost was still higher in patients with hyperkalemia ($13,540) compared with patients with normokalemia ($4,205) in CKD stages 4 to 5 patients (Fig S3).
Cost and Resource Use Differences in the Propensity Score–Matched Cohort and Factors Associated With Health Care Cost
Table 3 summarizes health care costs and resource use among propensity score–matched patients with hyperkalemia and controls. Patient characteristics of the propensity score–matched cohort are described in Table S4; these were well balanced between the 2 groups. Total health care costs were higher for patients with hyperkalemia than controls, with mean differences of $8,611 (95% CI, $8,046-$9,175) within 12 months and $5,150 (95% CI, $4,733-$5,566) after 12 months. Mean lengths of hospitalizations were longer among patients with hyperkalemia by 10.3 (95% CI, 8.1-12.5) days within 12 months and 7.4 (95% CI, 5.9-8.9) days after 12 months. Similarly, mean differences in numbers of hospitalizations and emergency visits per patient per year were 0.33 (95% CI, 0.29-0.36) and 0.20 (95% CI, 0.13-0.28) within 12 months and 0.36 (95% CI, 0.33-0.39) and 0.17 (95% CI, 0.12-0.23) after 12 months, respectively.
Table 3.
Health Care Costs and Resource Use in Propensity Score–Matched Patients With Hyperkalemia and Normokalemia Controls
| Within 12 mo |
After 12 mo |
|||||
|---|---|---|---|---|---|---|
| Hyperkalemia (N = 5,859) | Normokalemia (N = 5,859) | Difference (95% CI) | Hyperkalemia (N = 5,518) | Normokalemia (N = 5,762) | Difference (95% CI) | |
| Health Care Costs | ||||||
| Annual total costs per patient, $ | 13,308 ± 19,978a | 4,698 ± 9,342 | 8,611 (8,046 to 9,175) | 8,785 ± 13,938a | 3,636 ± 7,920 | 5,150 (4,733 to 5,566) |
| Hospitalization cost per visit, $ | 10,972 ± 15,428a | 7,544 ± 8,592 | 3,428 (2,578 to 4,278) | 9,704 ± 13,111a | 7,459 ± 8,754 | 2,245 (1,677 to 2,814) |
| Outpatient visit cost per visit, $ | 305 ± 540 | 288 ± 570 | 16 (−4 to 37) | 347 ± 606b | 309 ± 884 | 37 (9 to 66) |
| Emergency department cost per visit, $ | 12,261 ± 13,950a | 8,502 ± 7,977 | 3,759 (2,179 to 5,339) | 11,544 ± 13,668a | 9,071 ± 9,557 | 2,472 (1,203 to 3,741) |
| Health Care Resource Use | ||||||
| No. of hospitalizations per patient | 1.67 ± 1.10a | 1.35 ± 0.69 | 0.33 (0.29 to 0.36) | 0.96 ± 0.98a | 0.60 ± 0.48 | 0.36 (0.33 to 0.39) |
| No. of emergency visits per patient | 1.31 ± 0.68b | 1.10 ± 0.32 | 0.20 (0.13 to 0.28) | 0.69 ± 0.57 | 0.51 ± 0.36 | 0.17 (0.12 to 0.23) |
| No. of outpatient visits per patient | 12.8 ± 12.1a | 9.9 ± 7.5 | 2.9 (2.6 to 3.3) | 11.0 ± 13.8a | 7.8 ± 6.6 | 3.2 (2.8 to 3.6) |
| Length of hospital stay per hospitalization, d | 22.3 ± 40.9a | 12.1 ± 16.1 | 10.3 (8.1 to 12.5) | 20.3 ± 34.8a | 13.0 ± 21.2 | 7.4 (5.9 to 8.9) |
Note: Values expressed as mean ± standard deviation unless otherwise noted.
P < 0.001 and
P < 0.05 versus normokalemic control by generalized estimating equations for hospitalization cost per visit, outpatient visit cost, and emergency department cost per visit and paired t test for other variables.
Table 4 shows factors associated with health care costs among patients with hyperkalemia. CKD, HF, and hospital admission at the first hyperkalemic episode were the 3 most important factors associated with health care costs within 12 months. In addition to these factors, the number of repeated hyperkalemic episodes was the factor with the most significant association with total health care costs after 12 months, whereas severity of hyperkalemia was not associated. Total health care costs in patients with CKD and those with HF increased by 70% and 21%, respectively. In the subgroup of patients who had 4 or more hyperkalemic episodes within 12 months, total health care costs increased by 79% compared with patients with 0 to 1 hyperkalemic episode (Table 4).
Table 4.
Factors Associated With Total Health Care Costs for Patients With Hyperkalemia Within and After 12 Months
| Explanatory Variables | Within 12 mo (n = 27,534) |
After 12 mo (n = 22,791) |
||||
|---|---|---|---|---|---|---|
| Estimated β | Cost Ratioa (95% CI) | P | Estimated β | Cost Ratioa (95% CI) | P | |
| Chronic kidney disease | 0.347 | 1.415 (1.379-1.452) | <0.001 | 0.533 | 1.704 (1.641-1.770) | <0.001 |
| Heart failure | 0.255 | 1.290 (1.255-1.326) | <0.001 | 0.188 | 1.207 (1.161-1.255) | <0.001 |
| Age group | ||||||
| ≥18-<45 y | Reference | Reference | Reference | Reference | ||
| ≥45-<65 y | −0.143 | 0.867 (0.810-0.928) | <0.001 | −0.254 | 0.776 (0.709-0.849) | <0.001 |
| ≥65-<75 y | −0.192 | 0.825 (0.771-0.883) | <0.001 | −0.259 | 0.772 (0.707-0.844) | <0.001 |
| ≥75 y | −0.247 | 0.781 (0.732-0.835) | <0.001 | −0.200 | 0.819 (0.751-0.894) | <0.001 |
| Serum potassium level | ||||||
| ≥5.1-<5.5 mmol/L | Reference | Reference | Reference | Reference | ||
| ≥5.5-<6.0 mmol/L | 0.037 | 1.037 (1.006-1.069) | 0.019 | 0.038 | 1.039 (0.995-1.084) | 0.084 |
| ≥6.0 mmol/L | −0.005 | 0.995 (0.951-1.042) | 0.832 | 0.016 | 1.017 (0.947-1.091) | 0.649 |
| Charlson Comorbidity Index score | 0.054 | 1.056 (1.044-1.067) | <0.001 | 0.112 | 1.119 (1.102-1.136) | <0.001 |
| Admitted to hospital at first hyperkalemic episodes | 0.887 | 2.428 (2.367-2.491) | <0.001 | 0.238 | 1.269 (1.222-1.317) | <0.001 |
| History of hospitalization for ≥3 consecutive d | 0.142 | 1.153 (1.121-1.185) | <0.001 | 0.119 | 1.126 (1.084-1.170) | <0.001 |
| Female sex | −0.014 | 0.986 (0.962-1.011) | 0.274 | −0.042 | 0.959 (0.926-0.993) | 0.018 |
| Use of RAASi | −0.165 | 0.848 (0.826-0.871) | <0.001 | −0.011 | 0.989 (0.953-1.027) | 0.566 |
| Use of any potassium-lowering agentsb | 0.146 | 1.157 (1.124-1.191) | <0.001 | 0.181 | 1.199 (1.150-1.249) | <0.001 |
| No. of repeated hyperkalemic episodes within 12 mo after first hyperkalemic episode | ||||||
| 0-1 times | Reference | Reference | Reference | Reference | ||
| 2-3 times | NA | NA | NA | 0.155 | 1.168 (1.122-1.216) | <0.001 |
| ≥4 times | NA | NA | NA | 0.581 | 1.787 (1.691-1.889) | <0.001 |
Abbreviation: RAASi, renin-angiotensin-aldosterone system inhibitor.
Cost ratio indicates the effect of explanatory variables on total health care costs, which were calculated by exponential function, exp(estimated β).
Potassium-lowering agents included thiazide diuretics, loop diuretics, potassium binders, and sodium bicarbonate.
Discussion
In this study, we evaluated the long-term clinical and economic burden of hyperkalemia based on a large hospital claims database. We found that health care costs and resource use were substantially increased in patients with hyperkalemia within 12 months and this trend continued after 12 months, and the higher health care cost and resource use in patients with hyperkalemia remained after adjustment of patient characteristics by propensity score matching. The proportion of patients who were prescribed drug and nondrug treatments for kidney diseases increased with the CKD stages but was remarkably higher among patients with hyperkalemia. As a result, expenditures for several drug classes such as ESAs and sodium bicarbonate are higher among patients with hyperkalemia. Among these treatments, the highest costs were incurred from hospitalization for KRT, and it increased after 12 months. CKD, HF, and the number of repeat hyperkalemic episodes within 12 months were the 3 most important factors associated with higher health care costs after 12 months, whereas severity of hyperkalemia was not associated with higher health care costs.
Several studies have reported the economic burden of hyperkalemia for relatively short terms; for example, a Danish registry study reported increased costs over 6 months after hyperkalemic episodes.14 In this study, the hyperkalemia-associated cost was €5,077 ($5,575) in patients with CKD and the cost was higher in patients with HF at €6,018 ($6,609). A US study reported increased total health care costs within 30 days and 1 year after hyperkalemia and reported $4,128 higher 30-day costs and $15,983 higher 1-year costs compared with patients without hyperkalemia.15 The extent of increased costs might be dependent on the health care systems of individual countries. However, we found consistently higher health care costs and resource use among patients with hyperkalemia, and this can be largely attributed to increased hospitalization and outpatient visit costs.
Health care costs substantially increased among patients with hyperkalemia with CKD or HF, probably because specialized interventions and medications are required to treat CKD or HF. Interestingly, health care costs were substantially higher in patients with hyperkalemia than controls even after adjusting for patient background factors using propensity score matching, suggesting that the hyperkalemic condition per se is associated with higher health care costs. The cost difference was derived from the increased hospitalization and emergency visit costs, and these included increased medications, procedures, examinations, and surgery costs. Hospitalization and emergency visits can cause significant cost burdens for patients. Despite variations in health care systems, several studies have reported consistent findings regarding longer hospital stays and higher incidence of hospitalization and emergency visits.15,22 Studies are increasingly concluding that 30-day readmission, an indicator of quality of care, is an important burden for patients and the health care economy.23 Patients with end-stage renal disease bore the burden of high readmission rates, with 35% experiencing readmission within 30 days of discharge.24,25 We found a substantial increase in readmission rates in patients with hyperkalemia with advanced CKD, suggesting that hyperkalemia can be a risk factor for hospital readmission. The identified factors associated with higher health care cost suggest the importance of preventing recurrence of hyperkalemia regardless of the severity of first episodes. These results may also provide a guide for identifying patients likely to incur higher long-term health care costs and resource use, including those who have high-risk comorbid conditions such as CKD and/or HF or have a history of hospitalizations.
It is important to investigate the cost-effectiveness of maintaining normal serum potassium levels after hyperkalemia episodes. A recent study assessed the cost-effectiveness of sustained serum potassium level control and ongoing RAAS inhibitor therapy using a patient-level simulation model in patients with CKD.26 In this study, sustained serum potassium level control and ongoing RAAS inhibitor therapy resulted in longer life expectancy (by 2.36 years), delayed onset of end-stage renal disease (by 5.4 years), quality-adjusted life-year gains (1.04 year), and cost savings of £3,135 ($3,871) compared with the absence of RAAS inhibitor use to prevent hyperkalemia. Evidence of the cost-effectiveness of long-term serum potassium level management has become increasingly important, particularly with the recent introduction of newer potassium-binding agents such as patiromer and sodium zirconium cyclosilicate in clinical practice with improved tolerability for continuous use.27 We found that approximately half the patients with hyperkalemia with stage 5 CKD had KRT mostly because of dialysis introductions during long-term follow-ups. whereas only 10% of patients with stage 5 CKD in control required KRT. Considering that the cost associated with KRT was the highest among the treatments for kidney disease studied, these results suggest the importance of dialysis introductions as a contributing factor for the long-term clinical and economic burdens of hyperkalemic patients. Therefore, it is also of interest to study whether continuous hyperkalemia management can delay the introduction of KRT and reduce health care costs.
Several limitations of this study should be noted. First, we used hospital claims data that were not collected specifically for research purposes. Although the data allowed the analysis of a large patient population in a broad range of clinical settings, inherent biases and unmeasured confounders might exist in the data. Diagnostic and procedural codes were recorded in routine clinical practice, so the accuracy of the data might have varied by health care facility. However, patient records were collected systematically and electronically as part of routine clinical practice, which helped in avoiding recall bias in collecting clinical information. Moreover, the hospital claims data contained nearly 100% of patients’ prescription information and activity health care costs. Hence, the data allowed us to capture sufficient information to assess patients’ economic burden. Data were collected from 374 hospitals across Japan, which aided in the generalizability of the findings.
Second, we analyzed health care costs by aggregating the activity-based costs that were actually incurred at health care facilities. However, the Japanese health insurance system uses the diagnostic procedure combination per-diem system, in which provider reimbursement is calculated using flat-rate per-diem fees based on the diagnosis group.28 Therefore, the actual reimbursed costs may have been different when this system was applied to the results. However, findings from our study can provide evidence of increased health care costs with fair comparisons based on the accumulation of activity-based costs.
Finally, because this was an observational study, the associations found in this study cannot be directly considered as causal relationships.
In conclusion, we report the long-term clinical and economic burden on patients with hyperkalemia under continuous medical care. We found significantly higher inpatient and outpatient costs that lead to substantially increased total health care costs in patients with hyperkalemia within and after 12 months. Increased hospitalizations and emergency visits contributed substantially to these increased health care costs. We identified several contributing factors—including hospital admission at the time of first hyperkalemic episodes, CKD, HF, and the number of repeated hyperkalemic episodes—to understand the high-cost patient profiles. Our results suggest that hyperkalemia continues to be associated with a significant long-term clinical and economic burden and stress the importance of continuous management of serum potassium levels as part of the ongoing medical care for high-risk patients with hyperkalemia to reduce the economic burden on patients and the health care system.
Article Information
Authors’ Full Names and Academic Degrees
Eiichiro Kanda, MD, PhD, MPH, Naoki Kashihara, MD, PhD, Shun Kohsaka, MD, Suguru Okami, PhD, and Toshitaka Yajima, MD, PhD.
Authors’ Contributions
Conception and design: all authors; analysis and interpretation of data: SO, TK, SK, and EK. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated or resolved.
Support
This study and the corresponding analyses were supported and funded by AstraZeneca K.K., Japan. The authors from the funding source participated in the organization of study design, interpretation of results, contribution to manuscript drafts and revisions, and the decision to approve publication of the finished manuscript.
Financial Disclosure
Dr Kohsaka reports investigator-initiated grant funding from Bayer and Daiichi Sankyo and personal fees from AstraZeneca, Bayer, Bristol-Myers Squibb, and Pfizer. Drs Okami and Yajima are employed by AstraZeneca. The remaining authors declare that they have no relevant financial interests.
Acknowledgements
The authors thank Masafumi Okada, ZhenZhen Fang, Yiyun Lin, and all project members of IQVIA Solutions, K.K. for providing technical and editorial support for this study.
Peer Review
Received February 3, 2020. Evaluated by 1 external peer reviewer, with direct editorial input from the Statistical Editor, an Associate Editor, and the Editor-in-Chief. Accepted in revised form September 27, 2020.
Footnotes
Complete author and article information provided before references.
Figure S1: Flow diagram of patient inclusion in the study
Figure S2: Cumulative health care costs within 12 months in cohorts with or without CKD or HF
Figure S3: Cumulative health care cost per patient within 12 months in patients with CKD stage 4-5.
Item S1: STROBE checklist
Table S1: Definitions of high-risk subgroups
Table S2: List of comorbid conditions
Table S3: Drug and nondrug treatments for renal disease stratified by CKD stages
Table S4: Patient characteristics of propensity score–matched cohort of hyperkalemia and normokalemic controls
Supplementary Material
Figures S1-S3; Tables S1-S4.
References
- 1.Gumz M.L., Rabinowitz L., Wingo C.S. An integrated view of potassium homeostasis. N Engl J Med. 2015;373(1):60–72. doi: 10.1056/NEJMra1313341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palmer B.F. Regulation of potassium homeostasis. Clin J Am Soc Nephrol. 2015;10(6):1050–1060. doi: 10.2215/CJN.08580813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaitman M., Dixit D., Bridgeman M.B. Potassium-binding agents for the clinical management of hyperkalemia. P.T. 2016;41(1):43–50. [PMC free article] [PubMed] [Google Scholar]
- 4.Kovesdy C.P. Management of hyperkalemia: an update for the internist. Am J Med. 2015;128(12):1281–1287. doi: 10.1016/j.amjmed.2015.05.040. [DOI] [PubMed] [Google Scholar]
- 5.Khanagavi J., Gupta T., Aronow W.S. Hyperkalemia among hospitalized patients and association between duration of hyperkalemia and outcomes. Arch Med Sci. 2014;10(2):251–257. doi: 10.5114/aoms.2014.42577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palmer B.F. Managing hyperkalemia caused by inhibitors of the renin–angiotensin–aldosterone system. N Engl J Med. 2004;351(6):585–592. doi: 10.1056/NEJMra035279. [DOI] [PubMed] [Google Scholar]
- 7.Kashihara N., Kohsaka S., Kanda E. Hyperkalemia in real-world patients under continuous medical care in Japan. Kidney Int Rep. 2019;4(9):1248–1260. doi: 10.1016/j.ekir.2019.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Evans K.J., Greenberg A. Hyperkalemia: a review. J Intensive Care Med. 2005;20(5):272–290. doi: 10.1177/0885066605278969. [DOI] [PubMed] [Google Scholar]
- 9.Tromp J., van der Meer P. Hyperkalemia: aetiology, epidemiology, and clinical significance. Eur Heart J Suppl. 2019;21(suppl A):A6–A11. doi: 10.1093/eurheartj/suy028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luo J., Brunelli S.M., Jensen D.E. Association between serum potassium and outcomes in patients with reduced kidney function. Clin J Am Soc Nephrol. 2016;11(1):90–100. doi: 10.2215/CJN.01730215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collins A.J., Pitt B., Reaven N. Association of serum potassium with all-cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am J Nephrol. 2017;46(3):213–221. doi: 10.1159/000479802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linde C., Qin L., Bakhai A. Serum potassium and clinical outcomes in heart failure patients: results of risk calculations in 21334 patients in the UK. ESC Heart Fail. 2019;6(2):280–290. doi: 10.1002/ehf2.12402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Furuland H., McEwan P., Evans M. Serum potassium as a predictor of adverse clinical outcomes in patients with chronic kidney disease: new risk equations using the UK clinical practice research datalink. BMC Nephrol. 2018;19(1):211. doi: 10.1186/s12882-018-1007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim K., Thomsen R.W., Nicolaisen S.A. Healthcare resource utilization and cost associated with elevated potassium levels: a Danish population-based cohort study. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-026465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Betts K.A., Wooley J.M., Mu F. The cost of hyperkalemia in the United States. Kidney Int Rep. 2018;3:385–393. doi: 10.1016/j.ekir.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fitch K., Woolley M., Engel T. The clinical and economic burden of hyperkalemia on Medicare and commercial payers. Am Health Drug Benefits. 2017;10(4):202–210. [PMC free article] [PubMed] [Google Scholar]
- 17.Betts K.A., Woolley J.M., Mu F. The prevalence of hyperkalemia in the United States. Curr Med Res Opin. 2018;34(6):971–978. doi: 10.1080/03007995.2018.1433141. [DOI] [PubMed] [Google Scholar]
- 18.Kovesdy C.P. Management of hyperkalemia in chronic kidney disease. Nat Rev Nephrol. 2014;10(11):653–662. doi: 10.1038/nrneph.2014.168. [DOI] [PubMed] [Google Scholar]
- 19.The Organisation for Economic Co-operation and Development (OECD) Purchasing power parities (indicator). 2019. https://doi.org/10.1787/1290ee5a-en Accessed August 28, 2019.
- 20.Barber J., Thompson S. Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy. 2004;9:197–204. doi: 10.1258/1355819042250249. [DOI] [PubMed] [Google Scholar]
- 21.Dodd S., Bassi A., Bodger K., Williamson P. A comparison of multivariate regression models to analyse cost data. J Eval Clin Pract. 2006;12:76–86. doi: 10.1111/j.1365-2753.2006.00610.x. [DOI] [PubMed] [Google Scholar]
- 22.Chazard E., Dumesnil C., Beuscart R. How much does hyperkalemia lengthen inpatient stays? About methodological issues in analyzing time-dependent events. Stud Health Technol Inform. 2015;210:835–839. [PubMed] [Google Scholar]
- 23.Kwok C.S., Hulme W., Olier I. Review of early hospitalization after percutaneous coronary intervention. Int J Cardiol. 2017;227:370–377. doi: 10.1016/j.ijcard.2016.11.050. [DOI] [PubMed] [Google Scholar]
- 24.US Renal Data System. Chapter 4: hospitalization. In: USRDS 2017 Annual Data Report: epidemiology of kidney disease in the United States. Accessed August 28, 2019. https://www.usrds.org/2017/download/v2_c04_Hospitalization_17.pdf
- 25.Lin E., Bhattacharya J., Chertow G.M. Prior hospitalization burden and the relatedness of 30-day readmissions in patients receiving hemodialysis. J Am Soc Nephrol. 2019;30:323–335. doi: 10.1681/ASN.2018080858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evans M., Palaka E., Furuland H. The value of maintaining normokalemia and enabling RAASi therapy in chronic kidney disease. BMC Nephrol. 2019;20:31. doi: 10.1186/s12882-019-1228-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosano G.M.C., Spoletini I., Agewall S. Pharmacology of new treatments for hyperkalemia: patiromer and sodium zirconium cyclosiliate. Eur Heart J Suppl. 2019;21(suppl A):A28–A33. doi: 10.1093/eurheartj/suy035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ishii M. DRG/PPS and DPC/PDPS as prospective payment system. JMAJ. 2012;55(4):279–291. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figures S1-S3; Tables S1-S4.