Abstract
Background
Aspirin-exacerbated respiratory disease (AERD) is an aggressive inflammatory disorder of the upper and lower respiratory tract. Corticosteroids, leukotriene modifiers, endoscopic sinus surgery (ESS), aspirin (ASA) desensitization, and biological immunomodulators are currently used to treat the disorder.
Objective
The objective of this study was to determine the psychosocial impact of ESS and ASA desensitization on AERD patients.
Methods
All AERD patients who underwent complete ESS were divided into two cohorts based on ASA desensitization status. The psychosocial metrics of the SNOT-22 were collected and analyzed at the following time points: pre-operative, 1-month, 3-month, 6-month, and 12-month after ESS.
Results
One hundred and eighty-four AERD patients underwent ESS from November 2009 to November 2018. From this group, 130 patients underwent ASA desensitization (AD cohort) and 54 patients remained non-desensitized (ND cohort). AD patients showed a significantly greater reduction in total SNOT-22 scores over the study period compared to ND patients (p = 0.0446). Analysis of SNOT-22 psychosocial metrics showed a significantly greater improvement in patient productivity in the AD cohort when compared to the ND cohort (p = 0.0214). Further, a sub-group analysis accounting for subject attrition showed a significantly greater improvement in both productivity and concentration in AD patients when compared to the ND cohort (productivity: p = 0.0068; concentration: p = 0.0428).
Conclusions
ESS followed by ASA desensitization decreases the overall psychosocial burden in AERD patients with a significant improvement in perceived productivity and concentration. This has significant implications given the psychosocial impact of chronic diseases.
Keywords: Psychosocial domain, AERD, Aspirin desensitization, Sinus surgery
Introduction
Aspirin-exacerbated respiratory disease (AERD) is an inflammatory disorder of the upper and lower respiratory tract, represented by the triad of adult-onset asthma, chronic rhinosinusitis with nasal polyposis (CRSwNP), and respiratory sensitivity to aspirin (ASA) and other cyclooxygenase-1 (COX-1) inhibitors.1, 2, 3 Patients with AERD are intolerant to COX-1 inhibitors due to abnormal shunting of arachidonic acid metabolism toward the production of pro-inflammatory leukotrienes, resulting in activation of mast cells, increased eosinophilic inflammation, and amplification of the type 2 adaptive immune response.4 The disorder affects 0.6%–2.5% of the general population.2,5 The prevalence of ASA sensitivity is found in 16% of CRS cases, 28.3% in CRSsNP cases, and 38.5% in CRSwNP and asthma cases.6 Current treatment options for AERD include medical therapy using anti-leukotrienes, monoclonal antibodies, corticosteroids, aspirin desensitization, and endoscopic sinus surgery (ESS).1 Previously, ASA desensitization has been shown to improve smell and sinonasal complaints, maintain disease control, and reduce asthma exacerbations, corticosteroid use, number of revision surgeries, and number of sinus infections in patients with AERD.3,7,8 Furthermore, sinus surgery followed by desensitization has been shown to be effective at controlling disease burden.9, 10, 11
It is well known that chronic rhinosinusitis (CRS) results in significant functional and emotional impairment in patients.12 Previous studies have found that AERD patients have objectively worse disease burden, poorer quality of life, and higher financial costs compared to their CRS counterparts.5,13, 14, 15, 16 While ASA desensitization and ESS have demonstrated improvement in disease burden and symptoms, little is known about the psychosocial impact of ESS and ASA desensitization on AERD patients. In this study, we evaluate the impact of desensitization on the psychosocial burden of AERD patients who have recently undergone ESS using a validated sinonasal outcome questionnaire administered longitudinally, at multiple time points.
Materials and methods
This study was approved by the Institutional Review Board at the University of Pennsylvania. A retrospective review was performed of all patients with aspirin-exacerbated respiratory disease (AERD) who underwent complete ESS at a tertiary academic medical center with a dedicated AERD center. The group was divided into two cohorts based on aspirin (ASA) desensitization status. Inclusion criteria consisted of (1) oral aspirin challenge with worsening of airway symptoms; (2) diagnosis of asthma; (3) chronic rhinosinusitis refractory to medical therapy; (4) pre-operative endoscopic evidence of chronic rhinosinusitis with nasal polyposis, and (5) complete ESS. Exclusion criteria for the study consisted of: age under 18 years, immunodeficiency, pregnancy, cystic fibrosis, or negative aspirin challenge.
All patients underwent complete ESS, which is defined as removal of polypoid disease and bilateral maxillary antrostomy, sphenoethmoidectomy, and frontal sinusotomy. Due to disease severity, a number of patients had middle turbinate resection and/or a Draf III performed. All patients were given a similar postoperative corticosteroid taper based on endoscopic exam and long-term topical corticosteroid irrigations. In the AD cohort, ASA desensitization was conducted approximately 6 weeks after surgery, once systemic steroids were tapered off completely. Patients with a questionable history of AERD underwent ASA challenge pre-operatively. Otherwise, patients had ASA challenge postoperatively as part of our desensitization protocol. All ASA desensitization was performed in an outpatient surgicenter setting under continuous monitoring using the modified intranasal ketorolac and aspirin challenge/desensitization protocol.17 ASA maintenance therapy was based on the following protocol: initial dosing of 650 mg twice daily with attempted titration after 3–6 months down to a minimum of 325 mg daily, depending on patient response and tolerance. About 6 months post-ASA desensitization, patients were typically on a stable maintenance dose of 325 mg–1300 mg of aspirin daily.
Sinonasal outcomes were assessed using the 22-item Sino-Nasal Outcome Test (SNOT-22), which is scored from a 0 (no problem) to a 5 (problem as bad as it can be) with a total range from 0 to 110. The SNOT-22 questionnaire assesses rhinologic, extra-nasal rhinologic, ear/facial, sleep, and psychosocial metrics. SNOT-22 scores were collected pre-operatively and post-operatively at 1 month (4–6 weeks), 3 months (2–4 months), 6 months (5–8 months), and 12 months (9–13 months) after surgery, with attention focused on outcomes within the psychosocial domain. In this domain, patients scored (Q1) “reduced productivity”, (Q2) “reduced concentration”, (Q3) “frustrated”, (Q4) “sad”, and (Q5) “embarrassed” from a 0 to a 5 to produce a psychosocial SNOT-22 sub-score from 0 to 25.
The primary goal of these analyses was to evaluate the effects of ASA desensitization after ESS on total SNOT-22 and psychosocial domain scores over time. Continuous variables were summarized using means and standard deviations. Time was measured as a categorical variable since the intervals at which SNOT-22 scores were collected were non-linear. Analyses testing the effects of aspirin desensitization on SNOT-22 and psychosocial scores over time were performed using a repeated measure mixed model ANOVA using subject as a random effect. Significant interactions were further examined using a post-hoc multiple comparisons test using Student's T-tests. Statistical analyses were performed using JMP Software (SAS Institute, Cary, NC).
Results
One hundred and eighty-four patients with aspirin challenge-proven AERD from November 2009 to November 2018 met inclusion criteria for this study. Any patients who did not undergo ESS or receive ASA desensitization within 4 months after surgery were excluded from this study. Patients who underwent ESS but received ASA desensitization outside the study period (greater than 12 months after surgery) were placed in the non-desensitized group. All 184 AERD patients successfully underwent ESS. From this group, 130 patients underwent ASA desensitization (AD cohort) while 54 patients were not desensitized (ND cohort), and both groups were followed for up to 12 months after surgery. Of these patients, 24 AD patients and 5 ND patients had SNOT-22 available at all time points (“survivors”).
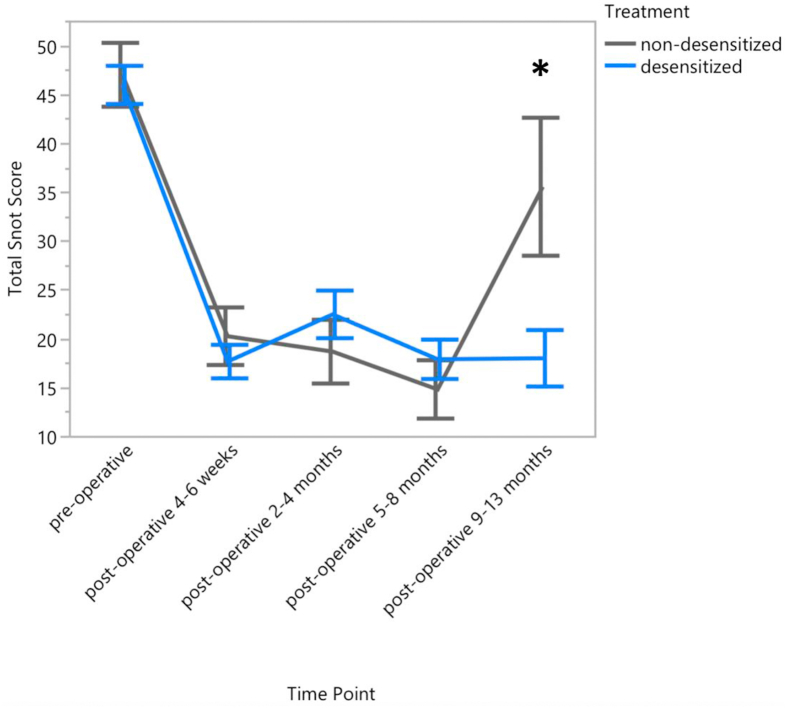
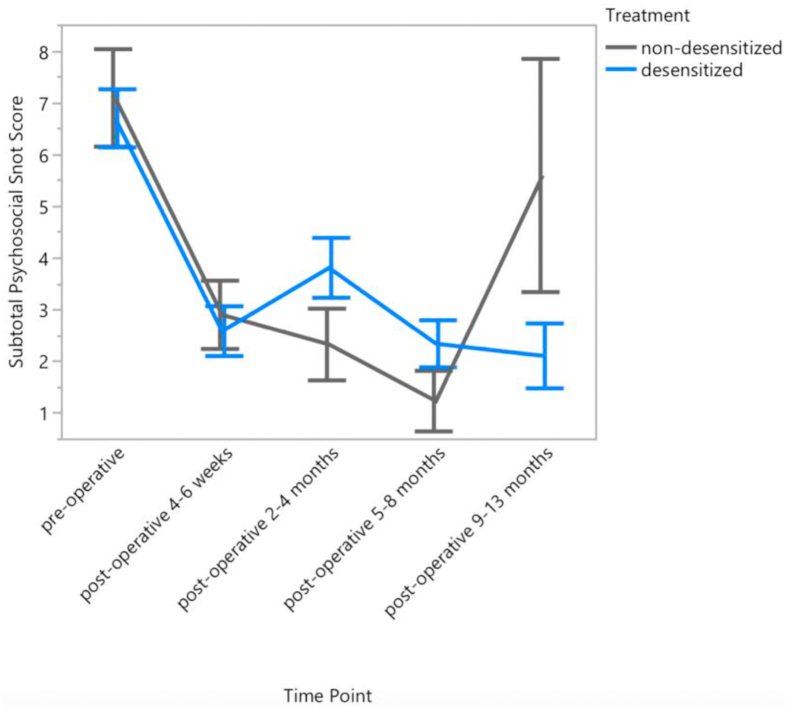
Subject demographics and baseline characteristics are shown in Table 1. Primary outcome measures were assessed using a validated, 22-item sinonasal outcome test (SNOT-22). Pre-operatively, the total mean (±SD) SNOT-22 score was 46.2 ± 21.1 (AD) and 46.2 ± 22.7 (ND). 1-month postoperative SNOT-22 scores showed a significant reduction in both groups, to 17.9 ± 17.0 (AD) and 20.4 ± 19.6 (ND) (AD: p < 0.0001; ND: p < 0.0001) with total scores of 22.4 ± 21.5, 17.9 ± 17.2, and 17.7 ± 19.1 (AD) and 18.7 ± 18.7, 14.9 ± 13.7, and 35.6 ± 22.3 (ND) at 3, 6, and 12 months post-surgery, respectively (Fig. 1). At 3 months postoperatively, the AD group showed a transient increase in their total SNOT-22 scores when compared to the ND group, however this was not significantly different (p = 0.8279) (Fig. 1, Fig. 2). This transient increase is likely secondary to worsening symptoms following desensitization. A similar trend was observed in the psychosocial SNOT-22 domain (Table 2, Fig. 2).
Table 1.
Demographic characteristics of the study sample (Mean ± SD).
| Group | n | Age (years) | Male (%) | BMI (kg/m2) |
|---|---|---|---|---|
| Aspirin desensitized | 130 | 48.1 ± 12.9 | 40.0 | 28.4 ± 5.6 |
| Not desensitized | 54 | 49.9 ± 11.8 | 55.6 | 28.3 ± 6.7 |
| All | 184 | 48.6 ± 12.6 | 44.6 | 28.4 ± 5.8 |
BMI = body mass index, AD = aspirin desensitized, ND = not desensitized.
Fig. 1.
Total SNOT-22 scores, displayed as an average ± 1 standard error. Asterisks indicate statistical significance at the 0.05 level.
Fig. 2.
Psychosocial SNOT-22 scores, displayed as an average ± 1 standard error.
Table 2.
SNOT-22 and psychosocial domain scores (Mean ± SD).
| Variable | Pre-ESS | 1 month post-ESS | 3 months post-ESS | 6 months post-ESS | 12 months post-ESS |
|---|---|---|---|---|---|
| Aspirin desensitized | |||||
| SNOT-22 total | 46.2 ± 21.1 | 17.9 ± 17.0 | 22.4 ± 21.5 | 17.9 ± 17.2 | 17.7 ± 19.1 |
| Psychosocial domain total | 6.85 ± 6.12 | 2.81 ± 4.83 | 3.83 ± 5.13 | 2.46 ± 3.95 | 2.09 ± 4.21 |
| Q1. Reduced productivity | 1.75 ± 1.55 | 0.82 ± 1.34 | 1.06 ± 1.34 | 0.68 ± 1.23 | 0.56 ± 1.05 |
| Q2. Reduced concentration | 1.73 ± 1.57 | 0.78 ± 1.29 | 1.03 ± 1.33 | 0.53 ± 1.03 | 0.53 ± 1.05 |
| Q3. Frustrated | 1.72 ± 1.57 | 0.64 ± 1.22 | 0.83 ± 1.37 | 0.66 ± 1.09 | 0.51 ± 1.10 |
| Q4. Sad | 0.83 ± 1.31 | 0.35 ± 0.96 | 0.54 ± 1.09 | 0.26 ± 0.70 | 0.26 ± 0.79 |
| Q5. Embarrassed | 0.83 ± 1.29 | 0.22 ± 0.75 | 0.38 ± 0.94 | 0.32 ± 0.85 | 0.23 ± 0.78 |
| Not desensitized | |||||
| SNOT-22 total | 46.2 ± 22.7 | 20.4 ± 19.6 | 18.7 ± 18.7 | 14.9 ± 13.7 | 35.6 ± 22.3 |
| Psychosocial domain total | 6.78 ± 6.58 | 2.90 ± 4.39 | 2.33 ± 3.99 | 1.24 ± 2.68 | 5.60 ± 7.12 |
| Q1. Reduced productivity | 1.63 ± 1.69 | 0.86 ± 1.32 | 0.64 ± 1.17 | 0.43 ± 0.81 | 1.70 ± 1.83 |
| Q2. Reduced concentration | 1.73 ± 1.59 | 0.76 ± 1.23 | 0.70 ± 1.21 | 0.29 ± 0.72 | 1.50 ± 1.65 |
| Q3. Frustrated | 1.92 ± 1.81 | 0.76 ± 1.25 | 0.64 ± 1.14 | 0.33 ± 0.91 | 1.40 ± 1.96 |
| Q4. Sad | 0.82 ± 1.44 | 0.24 ± 0.58 | 0.21 ± 0.74 | 0.05 ± 0.22 | 0.50 ± 1.58 |
| Q5. Embarrassed | 0.67 ± 1.26 | 0.29 ± 0.67 | 0.15 ± 0.62 | 0.14 ± 0.65 | 0.50 ± 1.08 |
ESS = endoscopic sinus surgery, SNOT-22 = 22-item Sino-Nasal Outcomes Test.
Post-operative 4–6 weeks, 2–4 months, 5–8 months, and 9–13 months refer to the ranges associated with the 1-month, 3-month, 6-month, and 12-month time points, respectively.
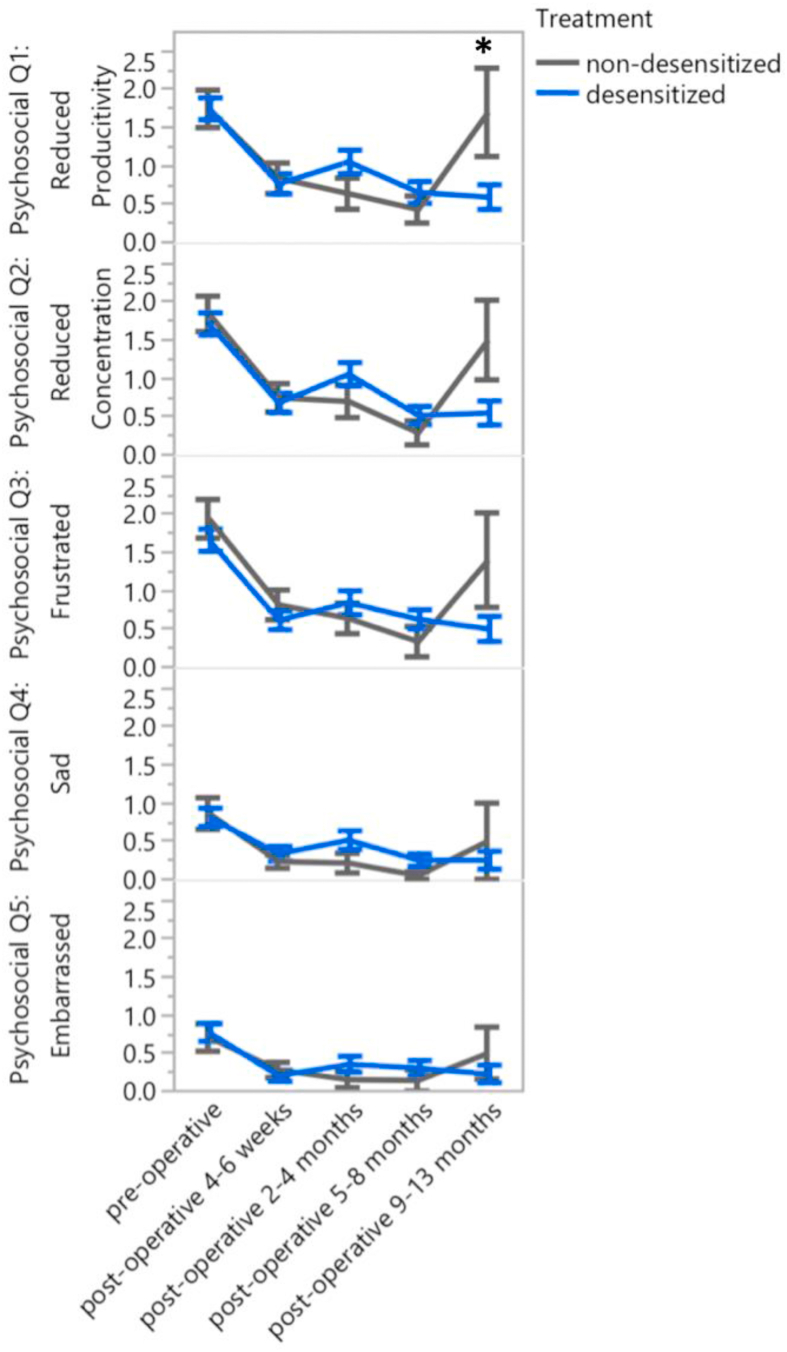
Compared to the ND patients, AD patients showed a significant reduction in total SNOT-22 scores over the study period (p = 0.0446). At baseline, total SNOT-22 scores did not differ between groups (p = 0.9092) but were significantly different at 12 months (p = 0.0036). Within the psychosocial domain, AD showed a marked improvement in patient productivity compared to the ND group, illustrated by a significant difference in (Q1) “reduced productivity” scores (p = 0.0214) over the study period (baseline: p = 0.6960; 12 months: p = 0.0041). Changes in individual psychosocial questions over the study period are illustrated in Fig. 3.
Fig. 3.
Psychosocial SNOT-22 scores by individual questions, displayed as an average ± 1 standard error. Asterisks indicate statistical significance at the 0.05 level.
Due to subject attrition, analyses were also performed on those who had SNOT-22 data available at all time points (“survivors”). Compared to the ND group, AD patients showed a significant reduction in total SNOT-22 scores (p = 0.0298) over the study period (baseline: p = 0.4602; 12 months: p = 0.0164). Overall psychosocial domain scores showed a trending reduction (p = 0.0547) in AD patients compared to ND patients. Within the psychosocial domain, AD patients showed a significant improvement in both patient (Q1) “reduced productivity” (p = 0.0068) and (Q2) “reduced concentration” (p = 0.0428) compared to ND patients. Q1 and Q2 scores did not significantly differ at baseline between groups (Q1: p = 0.7823; Q2: p = 0.5431) but were significantly different between groups at 12 months (Q1: p = 0.0257; Q2: p = 0.0477).
Discussion
Our study highlights a significant improvement in productivity and concentration in AERD patients after ESS and ASA desensitization. The disease burden of AERD has been well-studied, from its physiologic effects to its impact on quality of life.6,15,16,18 For instance, a cross-sectional study surveyed AERD patients nationwide and found that chronic nasal symptoms followed by decreased sense of smell had the greatest impact on quality of life.15 It has been established that loss of smell results in poorer quality of life, physiologic pain, and mental health issues.19 It is well known that ASA desensitization and maintenance therapy are well tolerated and improve symptoms scores as well as need for systemic corticosteroid use and asthma exacerbations.3,5,7,8,20, 21, 22 We have previously shown that complete ESS with subsequent ASA desensitization has improved sinonasal quality of life scores,10 which is in line with current best-practice recommendations for recalcitrant AERD.9,23 This current study focuses not on the physical impact of AERD, but on its psychosocial and emotional aspects. There is limited research on the effects of AERD on psychologic well-being. A recent study by Feldman et al found that while AERD patients had clinically worse asthma, there were lower levels of depression, better asthma-related quality of life, and improve subjective perception of asthma compared to the asthma-only cohort.24 A retrospective case series by Cho et al evaluated sinonasal outcomes in AERD patients undergoing ESS followed by AD and found a significant reduction in SNOT-22 scores immediately post-op at 1 and 4 weeks and remained low through the 30-month post-desensitization period.9 Sub-analysis of nasal blockage and hyposmia components of the SNOT-22 showed significant improvement after ESS. A described limitation of the study was the lack of a comparison cohort that did not undergo desensitization after ESS. Our study included a cohort of AERD patients who only underwent complete ESS (ND). Consistent with the aforementioned published studies, our AD and ND cohorts both exhibited a significant reduction in SNOT-22 scores at 1-month postop/pre-ASA desensitization and scores remained reduced in both groups through the study period. The addition of ASA desensitization results in a significant improvement in SNOT-22 at the 12-month time point when compared to non-desensitization (Table 2). ASA desensitization results in a transient increase in SNOT-22 scores in the AD group at the 3-month time point, which corresponds to 2 months of aspirin maintenance therapy. This finding could reflect a transient increase in inflammation and sinonasal symptoms during the early desensitization period. Interestingly, independent analysis of the psychosocial sub-scores of the SNOT-22 showed a relative reduction in psychosocial domain scores with a significant improvement in patient productivity (Q1) in AD cohort compared to ND cohort at the 12-month postoperative time point. Within group comparison of the AD cohort demonstrated significant improvement of Q1 at all time points when compared to baseline. When controlled for subject attrition, the same significant improvements were observed not just in patient productivity but also in concentration (Q2) between cohorts and within the AD group. Our study is unique in that it emphasizes the psychosocial benefit of combined ESS and AD in AERD patients. Chronic rhinosinusitis, among other chronic conditions such as asthma, diabetes, and arthritis, is associated with depression, anxiety, and productivity loss.25, 26, 27, 28 AERD patients are most likely to have more recalcitrant forms of CRS and asthma.21,29 While the severity and progression of AERD can vary between patients, it is clear that a multimodality approach, consisting of surgery and ASA desensitization, optimizes not just physiological outcomes but also improves the psychosocial burden of the disease.
Our study has the inherent limitations of a retrospective review, however our use of a validated quality of life questionnaire supports the benefit of ASA desensitization following ESS in AERD patients. Due to our intent to analyze, patients also had varying lengths of follow-up. In addition, the time points used in our study were presented as a range due to longer post-operative follow-up intervals, preference for local follow-up, and survey bias. However, independent analysis of a sub-group of patients who were present for the entirety of the study showed similar findings between both cohorts.
Conclusion
AERD patients appear to benefit psychologically from a multidisciplinary approach for control of disease burden. In our analysis, complete endoscopic sinus surgery followed by aspirin desensitization resulted in a significant improvement in patient productivity and concentration. Future studies will aim to evaluate the psychosocial burden of AERD as it compares to other chronic conditions.
Statement of ethics
Subjects have given their written informed consent. The study protocol was approved by the University of Pennsylvania Institutional Review Board and was conducted in accordance with the World Medical Association Declaration of Helsinki.
Author contributions
Tran Locke, conception and design, analysis and interpretation of data, original draft and manuscript revision, responsibility for content of manuscript; Auddie Sweis, conception and design, analysis and interpretation of data, manuscript revision, responsibility for content of manuscript; Theodore Lin, acquisition of data, analysis and interpretation of data, original draft, responsibility for content of manuscript; Brian Sweis, analysis and interpretation of data, drafting and revision of figures; Patrick Gleeson, acquisition of data, manuscript revision, responsibility for content of manuscript; Nithin Adappa, conception and design, manuscript revision, final approval, responsibility for content of manuscript; Michael Kohanski, manuscript revision, final approval, responsibility for content of manuscript; James Palmer, conception and design, manuscript revision, final approval, responsibility for content of manuscript; John Bosso, conception and design, supervision, manuscript revision, final approval, responsibility for content of manuscript.
Declaration of competing interest
The authors have no relevant conflicts of interest to declare. The authors alone are responsible for the content and writing of this article.
Edited by Yu-Xin Fang
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Walgama E.S., Hwang P.H. Aspirin-exacerbated respiratory disease. Otolaryngol Clin North Am. 2017;50:83–94. doi: 10.1016/j.otc.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Rajan J.P., Wineinger N.E., Stevenson D.D., White A.A. Prevalence of aspirin-exacerbated respiratory disease among asthmatic patients: a meta-analysis of the literature. J Allergy Clin Immunol. 2015;135:676–681. doi: 10.1016/j.jaci.2014.08.020. e1. [DOI] [PubMed] [Google Scholar]
- 3.Stevenson D.D., Hankammer M.A., Mathison D.A., Christiansen S.C., Simon R.A. Aspirin desensitization treatment of aspirin-sensitive patients with rhinosinusitis-asthma: long-term outcomes. J Allergy Clin Immunol. 1996;98:751–758. doi: 10.1016/s0091-6749(96)70123-9. [DOI] [PubMed] [Google Scholar]
- 4.Pan D., Buchheit K.M., Samuchiwal S.K. COX-1 mediates IL-33-induced extracellular signal-regulated kinase activation in mast cells: implications for aspirin sensitivity. J Allergy Clin Immunol. 2019;143:1047–1057. doi: 10.1016/j.jaci.2018.06.033. e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chu D.K., Lee D.J., Lee K.M., Schünemann H.J., Szczeklik W., Lee J.M. Benefits and harms of aspirin desensitization for aspirin-exacerbated respiratory disease: a systematic review and meta-analysis. Int Forum Allergy Rhinol. 2019;9:1409–1419. doi: 10.1002/alr.22428. [DOI] [PubMed] [Google Scholar]
- 6.Batra P.S., Tong L., Citardi M.J. Analysis of comorbidities and objective parameters in refractory chronic rhinosinusitis. Laryngoscope. 2013;123(Suppl 7):S1–S11. doi: 10.1002/lary.24418. [DOI] [PubMed] [Google Scholar]
- 7.Berges-Gimeno M.P., Simon R.A., Stevenson D.D. Long-term treatment with aspirin desensitization in asthmatic patients with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2003;111:180–186. doi: 10.1067/mai.2003.7. [DOI] [PubMed] [Google Scholar]
- 8.Tajudeen B.A., Schwartz J.S., Bosso J.V. The role of aspirin desensitization in the management of aspirin-exacerbated respiratory disease. Curr Opin Otolaryngol Head Neck Surg. 2017;25:30–34. doi: 10.1097/MOO.0000000000000331. [DOI] [PubMed] [Google Scholar]
- 9.Cho K.S., Soudry E., Psaltis A.J. Long-term sinonasal outcomes of aspirin desensitization in aspirin exacerbated respiratory disease. Otolaryngol Head Neck Surg. 2014;151:575–581. doi: 10.1177/0194599814545750. [DOI] [PubMed] [Google Scholar]
- 10.Adappa N.D., Ranasinghe V.J., Trope M. Outcomes after complete endoscopic sinus surgery and aspirin desensitization in aspirin-exacerbated respiratory disease. Int Forum Allergy Rhinol. 2018;8:49–53. doi: 10.1002/alr.22036. [DOI] [PubMed] [Google Scholar]
- 11.McMains K.C., Kountakis S.E. Medical and surgical considerations in patients with Samter's triad. Am J Rhinol. 2006;20:573–576. doi: 10.2500/ajr.2006.20.2913. [DOI] [PubMed] [Google Scholar]
- 12.Senior B.A., Glaze C., Benninger M.S. Use of the rhinosinusitis disability index (RSDI) in rhinologic disease. Am J Rhinol. 2001;15:15–20. doi: 10.2500/105065801781329428. [DOI] [PubMed] [Google Scholar]
- 13.Staikūniene J., Vaitkus S., Japertiene L.M., Ryskiene S. Association of chronic rhinosinusitis with nasal polyps and asthma: clinical and radiological features, allergy and inflammation markers. Medicina (Kaunas) 2008;44:257–265. [PubMed] [Google Scholar]
- 14.Smith T.L., Mendolia-Loffredo S., Loehrl T.A., Sparapani R., Laud P.W., Nattinger A.B. Predictive factors and outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2005;115:2199–2205. doi: 10.1097/01.mlg.0000182825.82910.80. [DOI] [PubMed] [Google Scholar]
- 15.Ta V., White A.A. Survey-defined patient experiences with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol Pract. 2015;3:711–718. doi: 10.1016/j.jaip.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 16.Chang J.E., White A., Simon R.A., Stevenson D.D. Aspirin-exacerbated respiratory disease: burden of disease. Allergy Asthma Proc. 2012;33:117–121. doi: 10.2500/aap.2012.33.3541. [DOI] [PubMed] [Google Scholar]
- 17.Lee R.U., White A.A., Ding D. Use of intranasal ketorolac and modified oral aspirin challenge for desensitization of aspirin-exacerbated respiratory disease. Ann Allergy Asthma Immunol. 2010;105:130–135. doi: 10.1016/j.anai.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 18.Stevens W.W., Peters A.T., Hirsch A.G. Clinical characteristics of patients with chronic rhinosinusitis with nasal polyps, asthma, and aspirin-exacerbated respiratory disease. J Allergy Clin Immunol Pract. 2017;5:1061–1070. doi: 10.1016/j.jaip.2016.12.027. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neuland C., Bitter T., Marschner H., Gudziol H., Guntinas-Lichius O. Health-related and specific olfaction-related quality of life in patients with chronic functional anosmia or severe hyposmia. Laryngoscope. 2011;121:867–872. doi: 10.1002/lary.21387. [DOI] [PubMed] [Google Scholar]
- 20.Esmaeilzadeh H., Nabavi M., Aryan Z. Aspirin desensitization for patients with aspirin-exacerbated respiratory disease: a randomized double-blind placebo-controlled trial. Clin Immunol. 2015;160:349–357. doi: 10.1016/j.clim.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 21.White A.A., Stevenson D.D. Aspirin-exacerbated respiratory disease. N Engl J Med. 2018;379:1060–1070. doi: 10.1056/NEJMra1712125. [DOI] [PubMed] [Google Scholar]
- 22.Świerczyńska-Krępa M., Sanak M., Bochenek G. Aspirin desensitization in patients with aspirin-induced and aspirin-tolerant asthma: a double-blind study. J Allergy Clin Immunol. 2014;134:883–890. doi: 10.1016/j.jaci.2014.02.041. [DOI] [PubMed] [Google Scholar]
- 23.Levy J.M., Rudmik L., Peters A.T., Wise S.K., Rotenberg B.W., Smith T.L. Contemporary management of chronic rhinosinusitis with nasal polyposis in aspirin-exacerbated respiratory disease: an evidence-based review with recommendations. Int Forum Allergy Rhinol. 2016;6:1273–1283. doi: 10.1002/alr.21826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feldman J.M., Zeigler A.E., Nelson K. Depression symptoms and quality of life among individuals with aspirin-exacerbated respiratory disease. J Asthma. 2019;56:731–738. doi: 10.1080/02770903.2018.1490754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campbell A.P., Phillips K.M., Hoehle L.P. Depression symptoms and lost productivity in chronic rhinosinusitis. Ann Allergy Asthma Immunol. 2017;118:286–289. doi: 10.1016/j.anai.2016.12.012. [DOI] [PubMed] [Google Scholar]
- 26.Kim J.Y., Ko I., Kim M.S., Yu M.S., Cho B.J., Kim D.K. Association of chronic rhinosinusitis with depression and anxiety in a nationwide insurance population. JAMA Otolaryngol Head Neck Surg. 2019;145:313–319. doi: 10.1001/jamaoto.2018.4103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rudmik L., Smith T.L., Mace J.C., Schlosser R.J., Hwang P.H., Soler Z.M. Productivity costs decrease after endoscopic sinus surgery for refractory chronic rhinosinusitis. Laryngoscope. 2016;126:570–574. doi: 10.1002/lary.25656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moussavi S., Chatterji S., Verdes E., Tandon A., Patel V., Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 29.Divekar R., Patel N., Jin J. Symptom-based clustering in chronic rhinosinusitis relates to history of aspirin sensitivity and postsurgical outcomes. J Allergy Clin Immunol Pract. 2015;3:934–940. doi: 10.1016/j.jaip.2015.06.018. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]