Key Points
Question
What are the fitted filtration efficiencies (FFEs) of consumer-grade masks, improvised face coverings, and modified procedure masks commonly used during the coronavirus disease 2019 (COVID-19) pandemic?
Findings
In this comparative study of face covering FFEs, we observed that consumer-grade masks and improvised face coverings varied widely, ranging from 26.5% to 79.0% FFE. Modifications intended to enhance the fit of medical procedure masks improved FFE measurements from 38.5% (unmodified mask) to as much as 80.2%.
Meaning
Simple modifications can improve the fit and filtration efficiency of medical procedure masks; however, the practical effectiveness of consumer-grade masks available to the public is, in many cases, comparable with or better than their non-N95 respirator medical mask counterparts.
Abstract
Importance
During the coronavirus disease 2019 (COVID-19) pandemic, the general public has been advised to wear masks or improvised face coverings to limit transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). However, there has been considerable confusion and disagreement regarding the degree to which masks protect the wearer from airborne particles.
Objectives
To evaluate the fitted filtration efficiency (FFE) of various consumer-grade and improvised face masks, as well as several popular modifications of medical procedure masks that are intended to improve mask fit or comfort.
Design, Setting, and Participants
For this study conducted in a research laboratory between June and August 2020, 7 consumer-grade masks and 5 medical procedure mask modifications were fitted on an adult male volunteer, and FFE measurements were collected during a series of repeated movements of the torso, head, and facial muscles as outlined by the US Occupational Safety and Health Administration Quantitative Fit Testing Protocol. The consumer-grade masks tested included (1) a 2-layer nylon mask with ear loops that was tested with an optional aluminum nose bridge and filter insert in place, (2) a cotton bandana folded diagonally once (ie, “bandit” style) or in a (3) multilayer rectangle according to the instructions presented by the US Surgeon General, (4) a single-layer polyester/nylon mask with ties, (5) a polypropylene mask with fixed ear loops, (6) a single-layer polyester gaiter/neck cover balaclava bandana, and (7) a 3-layer cotton mask with ear loops. Medical procedure mask modifications included (1) tying the mask’s ear loops and tucking in the side pleats, (2) fastening ear loops behind the head with 3-dimensional–printed ear guards, (3) fastening ear loops behind the head with a claw-type hair clip, (4) enhancing the mask/face seal with rubber bands over the mask, and (5) enhancing the mask/face seal with a band of nylon hosiery over the fitted mask.
Main Outcomes and Measures
The primary study outcome was the measured FFE of common consumer-grade and improvised face masks, as well as several popular modifications of medical procedure masks.
Results
The mean (SD) FFE of consumer grade masks tested on 1 adult male with no beard ranged from 79.0% (4.3%) to 26.5% (10.5%), with the 2-layer nylon mask having the highest FFE. Unmodified medical procedure masks with ear loops had a mean (SD) FFE of 38.5% (11.2%). All modifications evaluated in this study increased procedure mask FFE (range [SD], 60.3% [11.1%] to 80.2% [3.1%]), with a nylon hosiery sleeve placed over the procedure mask producing the greatest improvement.
Conclusions and Relevance
While modifications to improve medical procedure mask fit can enhance the filtering capability and reduce inhalation of airborne particles, this study demonstrates that the FFEs of consumer-grade masks available to the public are, in many cases, nearly equivalent to or better than their non-N95 respirator medical mask counterparts.
This comparative study examines the fitted filtration efficiency of 7 consumer-grade face masks and 5 medical procedure mask modifications.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the cause of coronavirus disease 2019 (COVID-19), is a transmissible virus that infects the upper and lower respiratory tract,1 leading to a high viral titer in saliva and respiratory secretions.2 A key public health control strategy for mitigating SARS-CoV-2 transmission is use of masks or face coverings by the public.3 Masks that completely cover the nose and mouth are effective at reducing seasonal coronavirus and influenza transmission when worn by infected persons4,5 and noninfected persons who may come into contact with infected individuals.6,7 This is supported by emerging epidemiologic data that indicate that community-wide use of masks can effectively contribute to the prevention of SARS-CoV-2 transmission.8
As the adoption of face coverings during the COVID-19 pandemic becomes commonplace, there has been a rapid expansion in the public use of commercial, homemade, and improvised masks that vary considerably in design, material, and construction. Similarly, the press and social media outlets have reported on numerous innovative “hacks,” devices, and modifications (enhancements) that claim to improve the performance characteristics of conventional masks (typically surgical or procedure masks). Despite their widespread dissemination and use during the pandemic, there have been few evaluations of the efficiency of these face coverings or mask enhancements at filtering airborne particles. In this study, we used a recently described methodological approach9 based on the Occupational Safety and Health Administration (OSHA) Fit Test to determine the fitted filtration efficiency (FFE) of various consumer-grade and improvised face masks, as well as several popular modifications of medical procedure masks.
Methods
Testing Procedure
Fitted filtration efficiency tests were conducted between June and August 2020 in a custom-built exposure chamber (US Environmental Protection Agency Human Studies Facility in Chapel Hill, North Carolina) as recently described.9 The institutional review board at the University of North Carolina at Chapel Hill waived the need for study approval as well as individual consent needed for device testing. Briefly, a TSI 8026 Particle Generator was used to supplement the chamber with sodium chloride (NaCl) particles that had a count median diameter of 0.05 μm (range, 0.02-0.60 μm) as measured by a scanning mobility particle sizer. The test atmosphere was allowed to stabilize for 30 minutes before FFE testing. The chamber temperature and humidity during testing ranged from 73.4 °F to 85.1 °F and 10% to 50%, respectively. The test atmosphere used for this study reflects typical indoor conditions, with exposure to small particles that are slightly smaller than individual SARS-CoV-2 virions (reported to range between 0.06 μm and 0.14 μm10). A sampling port was installed in each mask using a TSI model 8025-N95 Fit Test Probe Kit to allow sampling behind the mask. All masks were fitted on a man (weight, 165.3 lb; height, 5 ft and 10.1 in; head size, 23.0 in) with no beard. A pair of TSI 3775 Condensation Particle Counters were run in single-particle analysis mode to continuously monitor ambient particles (0.02 μm-3 μm) in the chamber just outside the face mask and particles in the breathing space behind the face mask at a sampling rate of 1 second.
Fitted filtration efficiency measurements were collected during a series of repeated movements of the torso, head, and facial muscles as outlined by the OSHA Quantitative Fit Testing Protocol (Modified Ambient Aerosol CNC Quantitative Fit Testing Protocol For Filtering Facepiece Table A–2—RESPIRATORS). The FFE corresponds to the concentration of particles behind the mask expressed as a percentage of the particle concentration in the chamber air, and was measured for the duration of each test described in the OSHA protocol (bending at the waist, reading aloud, looking left and right, and looking up and down). The overall percentage of FFE is calculated as 100 × (1 − behind the mask particle concentration / ambient particle concentration), and the percentage of FFE and the standard deviation were calculated across the length of the test. The total testing time for each mask was approximately 3 minutes.
Products Tested
Two categories of products were tested for this study: consumer-grade face masks and medical procedure masks with and without enhancements. The following consumer-grade masks were tested (Figure 1): (1) a 2-layer nylon mask (54% recycled nylon, 43% nylon, 3% spandex) with ear loops (Easy Masks LLC) tested with an optional aluminum nose bridge and filter insert in place (Figure 1A), (2) a cotton bandana folded diagonally once “bandit” style (Figure 1B) or in a multilayer rectangle according to the instructions presented by the US Surgeon General (Figure 1C; https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-to-make-cloth-face-covering.html), (3) a single-layer polyester/nylon mask (80% polyester, 17% nylon, 3% spandex) with ties (Renfro Corporation) (Figure 1D), (4) a polypropylene mask with fixed ear loops (Red Devil Inc) (Figure 1E), (5) a single-layer gaiter/neck cover balaclava bandana (92% polyester and 8% spandex; MPUSA LLC) (Figure 1F), and (6) a 3-layer cotton mask (100% cotton) with ear loops (Hanesbrands Inc) (Figure 1G).
Figure 1. Consumer-Grade Masks and Improvised Face Coverings.
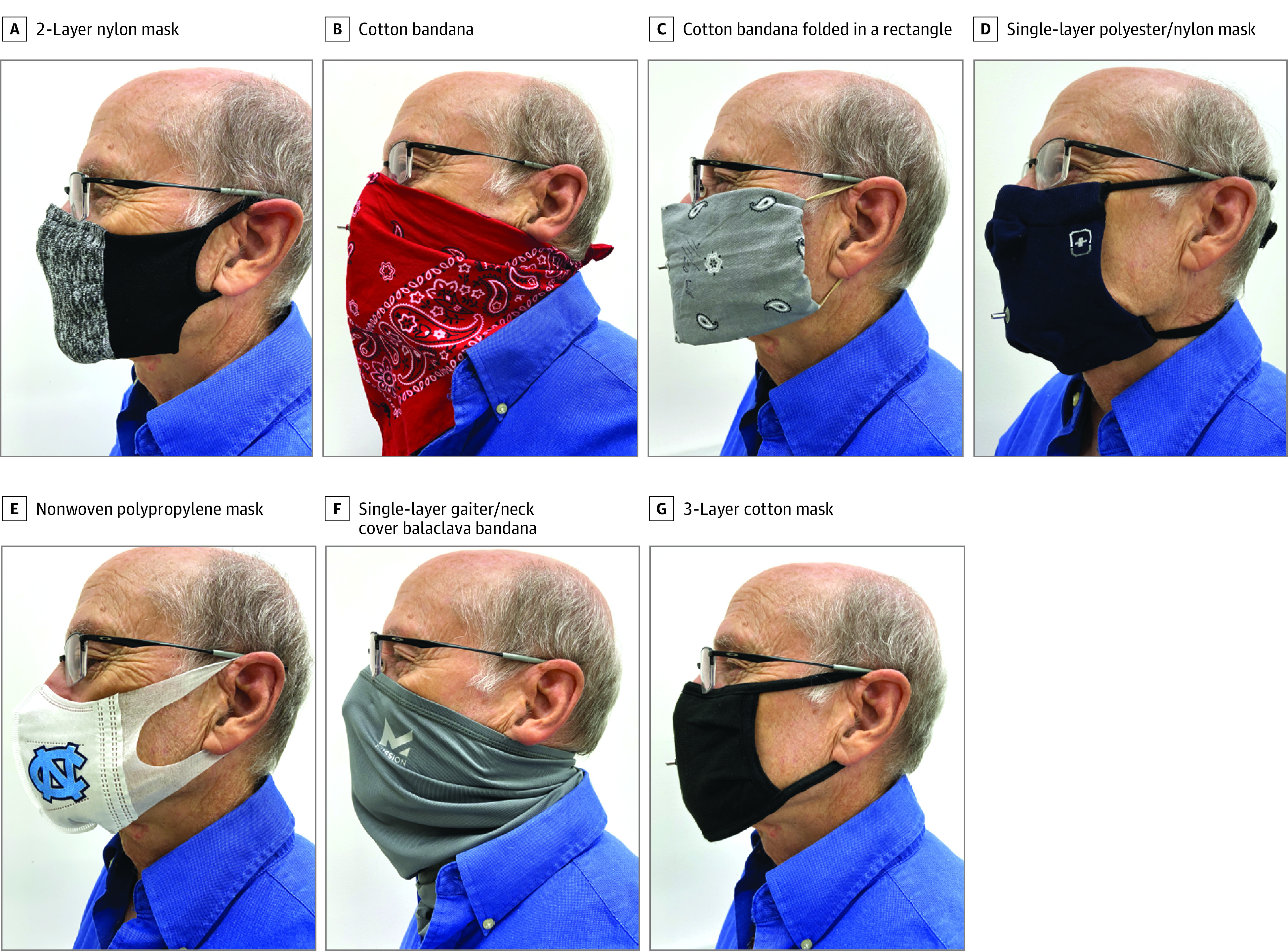
The face coverings tested in this study included a 2-layer nylon mask with ear loops (54% recycled nylon, 43% nylon, 3% spandex), tested with and without an optional aluminum nose bridge and filter insert in place (A), a cotton bandana folded diagonally once “bandit” style (B), a cotton bandana folded in a multilayer rectangle according to the instructions presented by the US Surgeon General (C), a single-layer polyester/nylon mask (80% polyester, 17% nylon, 3% spandex) with ties (D), a polypropylene mask with fixed ear loops (E), a single-layer gaiter/neck cover balaclava bandana (92% polyester and 8% spandex) (F), and a 3-layer cotton mask (100% cotton) with ear loops (G).
The baseline FFE of unmodified medical procedure masks with elastic ear loops (Cardinal Health Inc) was measured (n = 4) and compared with the FFE of the same type of mask with various modifications designed to enhance its function (Figure 2). The following modifications were tested: (1) enhancing the mask/face seal by tying the ear loops and tucking in the side pleats (Figure 2B; https://youtu.be/UANi8Cc71A0), (2) fastening ear loops behind the head with 3-dimensional–printed ear guards (Figure 2C; https://www.thingiverse.com/thing:4249113), (3) fastening ear loops behind the head with a 23-mm claw-type hair clip (Figure 2D), (4) enhancing the mask/face seal by placing a ring of 3 ganged rubber bands over the mask, with the center rubber band placed over the nose and chin of the participant and the left and right side bands looped over each ear (Figure 2E; “fix-the-mask” 3–rubber band method https://www.youtube.com/watch?v=CVjGCPfRwUo), and (5) enhancing the mask/face seal by sliding a 10-inch segment of nylon hosiery over the fitted mask (Figure 2F).11
Figure 2. Medical Procedure Mask and Modifications Designed to Enhance Mask Fit or Comfort for the Wearer.
A medical procedure mask with ear loops (A) was modified by tying the ear loops and tucking in the side pleats (B), attaching ear loops to a 3-dimensional–printed “ear guard” (C), fastening ear loops with a 23-mm claw-type hair clip placed behind the wearer’s head (D), placing a ring of 3 ganged rubber bands over the mask and around the wearer’s ears (E), and sliding a 10-inch segment of nylon hosiery over the fitted procedure mask (F).
Results
This study evaluated the FFE of 7 consumer-grade masks and five procedure mask modifications. The mean (SD) FFE of consumer-grade face masks tested in this study ranged from 79.0% (4.3%) to 26.5% (10.5%), with the washed, 2-layer nylon mask having the highest FFE and the 3-layer cotton mask having the lowest. The cotton bandana folded into a multilayer rectangle affixed to the ears with rubber bands, as described by the US Surgeon General, provided a mean (SD) FFE of 49.9% (5.8%). Folding the bandana bandit style produced a similar result (mean [SD] FFE, 49.0% [6.2%]). The tested mean (SD) FFE of the single-layer polyester gaiter/neck cover balaclava bandana was 37.8% (5.2%). The single-layer polyester/nylon mask, which is attached with tie strings, tested at a mean (SD) FFE of 39.3% (7.2%). The polypropylene mask with nonelastic (fixed) ear loops tested at a mean (SD) FFE of 28.6% (13.9%).
As expected based on data from our previous work,9 a National Institute for Occupational Safety and Health–approved 3M 9210 N95 respirator used as a reference control provided very high mean FFE (98.4% [0.5%]; n = 1) (Table). The medical procedure masks with elastic ear loops tested in this study had a mean (SD) FFE of 38.5% (11.2%) (Figure 3A), which was lower than that of medical surgical masks with tie strings (71.5% [5.5%]; n = 4). Tying the ear loops and tucking in the corners of the procedure mask to minimize gaps in the sides of the mask increased the mean (SD) FFE to 60.3% (11.1%) (Figure 3B). The “fix-the-mask” 3–rubber band modification and the nylon hosiery sleeve modifications, which were also intended to reduce gaps between the mask and the wearer’s face, improved mean (SD) FFE to 78.2% (3.3%) and 80.2% (3.1%), respectively.
Table. Face Mask FFE Against Submicron Particle Penetration.
| Consumer-grade face masks | Condition | % FFE (SD)a |
|---|---|---|
| 2-Layer nylon mask with ear loops | ||
| Without aluminum nose bridge | New | 44.7 (6.4) |
| With aluminum nose bridge | New | 56.3 (6.5) |
| With aluminum nose bridge and 1 insert | New | 74.4 (4.8) |
| With aluminum nose bridge, washed (no insert) | Washed 1 time | 79.0 (4.3) |
| Cotton bandana | ||
| Folded surgeon general style | New | 49.9 (5.8) |
| Folded “bandit” style | New | 49.0 (6.2) |
| Single-layer polyester gaiter/neck cover (balaclava bandana) | New | 37.8 (5.2) |
| Single-layer polyester/nylon mask with ties | New | 39.3 (7.2) |
| Polypropylene mask with fixed ear loops | New | 28.6 (13.9) |
| 3-Layer cotton mask with ear loops | New | 26.5 (10.5) |
| Medical face masks and modifications | ||
| 3M 9210 NIOSH–approved N95 respirator | New | 98.4 (0.5) |
| Surgical mask with ties | New | 71.5 (5.5) |
| Procedure mask with ear loops | New | 38.5 (11.2) |
| Procedure mask with ear loops | ||
| Loops tied and corners tucked in | New | 60.3 (11.1) |
| Ear guard | New | 61.7 (6.5) |
| 23-mm Claw hair clip | New | 64.8 (5.1) |
| Fix-the-mask (3 rubber bands) | New | 78.2 (3.3) |
| Nylon hosiery sleeve | New | 80.2 (3.1) |
Abbreviations: FFE, fitted filtration efficiency; NIOSH, National Institute for Occupational Safety and Health.
The percentage of FFE corresponds to 100 × (1 − behind the mask particle concentration / ambient particle concentration). Overall FFE percentage and SD were calculated across the length of the test.
Figure 3. Evaluation of Fitted Filtration Efficiency (FFE) Using the US Occupational Safety and Health Administration Modified Ambient Aerosol CNC Quantitative Fit Testing Protocol for Filtering Facepiece.
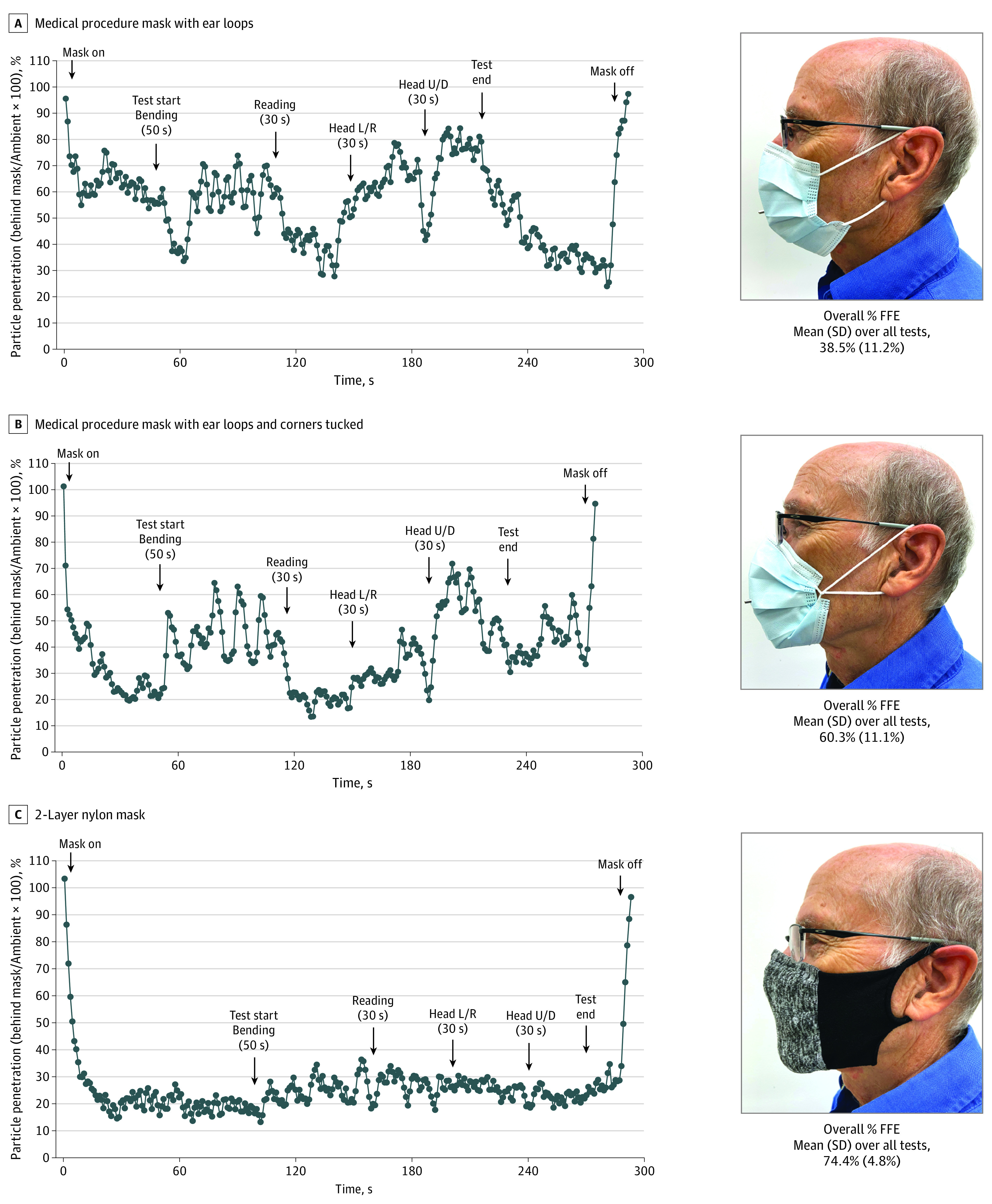
The overall FFE for a medical procedure mask with ear loops (A), medical procedure mask with the ear loops tied and mask corners tucked against the wearer’s face (B), and 2-layer nylon mask with an aluminum nose bridge and 1 filter insert (C) was 38.5%, 60.3%, and 74.4%, respectively. Particle penetration (y-axes) is defined as particle concentration behind the mask expressed as a percentage of the ambient particle concentration and is calculated during repeated-movement tests (bending at the waist, reading aloud, looking left and right, and looking up and down). The overall percentage of FFE is defined as 100 × (1 − behind the mask particle concentration / ambient particle concentration). Overall FFE percentage and SD were calculated across the length of the test. L/R indicates left/right; U/D, up/down.
Modifications to improve the seal of the mask against the face by increasing the tension of the ear loops also improved FFE. Attaching the ear loops to the ear guards device using the center hooks (tightest option) increased procedure mask mean (SD) FFE to 61.7% (6.5%). Similarly, joining the ear loops behind the wearer’s head using a claw-style hair clip increased the procedure mask mean (SD) FFE to 64.8% (5.1%). None of the modifications tested enhanced procedure mask FFE to the level of an N95 respirator.
Discussion
In this study, consumer-grade masks and medical procedure mask modifications were tested as personal protective equipment (protection for the wearer) against a test aerosol of 0.05-μm NaCl particles. Although the FFE of consumer-grade masks and face coverings was variable, the FFE of some consumer-grade products exceeded that of medical-grade procedure masks. For example, the 2-layer nylon mask with ear loops was tested under various conditions, including with and without an aluminum nose bridge, with and without a commercially available insert, and after 1 wash cycle in a standard household washing machine (air-dried on a drying rack). The unwashed nylon mask without a nose bridge or insert had an FFE of 44.7%. The addition of a nose bridge reduced visible gaps around the nose and increased FFE to 56.3%. Adding a filter insert to the mask with the nose bridge in place resulted in a further increase in FFE to 74.4% (Figure 3C). Interestingly, the FFE of the nylon mask (with the nose bridge but without the filter insert) improved slightly to 79.0% after washing. It is unclear why washing alone improved the FFE from 56.3% to 79.0%. It may be that the washing/drying process unraveled some of the fibers to increase the overall filtration surface, and thus filtration efficiency, of the medium, or perhaps it modified the mask shape or size in a way that improved fit, or both. The washing/drying test was not repeated with additional nylon masks. Further investigation to assess the association of single and multiple washing with mask integrity and material disposition would be necessary to validate any improvement in FFE.
The cotton mask, which comprises 3 layers and has a thin, flexible metal nose bridge, had the lowest FFE in this study (26.5%). The relatively loose arrangement of the cotton layers, while providing improved breathability and comfort, may reduce filtration efficiency. Additionally, we evaluated the FFE of improvised face coverings, including a standard cotton bandana and a neck gaiter balaclava bandana. The cotton bandana, when folded either bandit style or according to the US Surgeon General’s instructions, achieved approximately 50% FFE, which is better than the ear loop procedure mask we tested. Neck gaiter balaclava bandanas have also emerged as a popular face covering, particularly among athletes and young adults. As tested in this study, the single-layer gaiter, which was made of 92% polyester and 8% spandex and fits tightly to the wearer’s nose and mouth, had an FFE of 37.8%. While this face covering appeared to fit the wearer well, with no visible gaps in the seal, it may be that the relatively low FFE can be attributed to the low filtering efficiency of a single thin layer of material with large porosity.
For medical procedure masks, modifications that enhanced the fit between the mask and the wearer’s face improved FFE. Simply tying the ear loops and tucking the corners of the mask against the wearer’s cheeks visibly improved mask fit and increased FFE from 38.5% to 60.3% (Figure 3, A and B). The most effective modification tested was the use of a nylon hosiery sleeve placed over the procedure mask. This modification, which held the mask tight to the wearer’s face, eliminated all visible gaps and increased FFE from 38.5% to 80.2%. However, donning the nylon sleeve over the procedure mask was cumbersome and limited the wearer’s ability to adjust the procedure mask. Generally, improvements in procedure mask FFE appeared to be associated with the integrity of the seal of the edges of the mask to the wearer’s face, demonstrating the importance of mask fit to maximizing filtration. While all of the modifications described in the Table enhanced protection against airborne particles for the wearer, not all were comfortable or practical for extended use. For example, the 3–rubber band “fix-the-mask” modification created considerable pressure on the wearer’s ears (visible in Figure 2E), making it uncomfortable after only minutes of wear and raising questions about its adoption by the general public. While the modifications shown in this article can improve mask fit and provide increased filtration of airborne particles, it is important to choose a modification in which discomfort is not a deterrent from wearing the mask for prolonged periods.
Limitations
The data presented in this article provide information on the use of masks and face coverings as personal protective equipment, which is defined in this study as protection for the wearer against exposure to an aerosol composed of small (0.05-μm) particles. However, we acknowledge that there are limitations to these findings. First, all FFE tests were performed on a single individual to ensure consistency and allow for a controlled comparison between test products. Interperson heterogeneity in facial geometries may result in variability of mask fit and differences in FFE. Second, the size of the NaCl particles used in this study (0.05 μm) may not reflect the most penetrating particle size for all of the mask materials tested. The most penetrating particle size for nonelectret filter media (filters that collect particles by aerodynamic rather than electrostatic mechanisms) can range from 0.2 μm to 0.5 μm.12 As a result, the reported FFE values at 0.05 μm may slightly overestimate the FFE of particles in the most penetrating size range. However, based on the mechanisms of particle deposition that govern filtration (ie, diffusion, impaction, interception, and sedimentation), it is clear that protection against aerosols of 0.05-μm particles would also confer similar or better protection against much larger aerosols or droplets,13 which are currently believed to be the predominant source for COVID-19 transmission.
Conclusions
Masks serve a dual purpose to protect the wearer and others. These analyses were designed to quantify the protection that masks offer to the wearer when exposed to others who may be infected. The exact FFE required to prevent respiratory virus transmission is not precisely known. However, evidence from previous studies suggests that even face masks with an FFE less than 95% (eg, surgical masks) are effective in preventing the acquisition of epidemic coronaviruses (SARS-CoV-1, SARS-CoV-2) by health care clinicians, except possibly during aerosol-generating procedures.6,7,8 For prevention of an associated coronavirus, SARS-CoV-1, N95 respirators had no increased prevention benefit over surgical masks.7 In this article, we reported that simple modifications to improve medical mask fit can substantially improve filtration efficiency. However, when FFE is considered (combined fit and material filtration), we demonstrated the practical effectiveness of consumer-grade masks to be, in many cases, nearly equivalent to or better than their nonrespirator medical mask counterparts.
References
- 1.Hou YJ, Okuda K, Edwards CE, et al. SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell. 2020;182(2):429-446.e14. doi: 10.1016/j.cell.2020.05.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.To KK-W, Tsang OT-Y, Leung W-S, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20(5):565-574. doi: 10.1016/S1473-3099(20)30196-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention . Considerations for wearing cloth face coverings; help slow the spread of COVID-19. Accessed July 23, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html
- 4.Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9(3):e1003205. doi: 10.1371/journal.ppat.1003205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leung NHL, Chu DKW, Shiu EYC, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26(5):676-680. doi: 10.1038/s41591-020-0843-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors . Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973-1987. doi: 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Offeddu V, Yung CF, Low MSF, Tam CC. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta-analysis. Clin Infect Dis. 2017;65(11):1934-1942. doi: 10.1093/cid/cix681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng VC, Wong SC, Chuang VW, et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect. 2020;81(1):107-114. doi: 10.1016/j.jinf.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sickbert-Bennett EE, Samet JM, Clapp PW, et al. Filtration efficiency of hospital face mask alternatives available for use during the COVID-19 pandemic. JAMA Intern Med. 2020. doi: 10.1001/jamainternmed.2020.4221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu N, Zhang D, Wang W, et al. ; China Novel Coronavirus Investigating and Research Team . A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-733. doi: 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mueller AV, Eden MJ, Oakes JM, Bellini C, Fernandez LA. Quantitative method for comparative assessment of particle removal efficiency of fabric masks as alternatives to standard surgical masks for PPE. Matter. 2020;3(3):950-962. doi: 10.1016/j.matt.2020.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee K, Liu B. On the minimum efficiency and the most penetrating particle size for fibrous filters. J Air Pollution Control Association. 1980;30(4):377-381. doi: 10.1080/00022470.1980.10464592 [DOI] [Google Scholar]
- 13.Hinds WC. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles. John Wiley & Sons; 1999. [Google Scholar]



