Abstract
Background: The clinical use of zirconia implants has been shown to increase steadily due to their biological, aesthetic, and physical properties; therefore, this bibliometric study aimed to review the clinical research and co-authors in the field of zirconia dental implant rehabilitation. Methods: We searched Scopus and Web of Science databases using a comprehensive search strategy to 5 October 2020, and independently paired reviewers who screened studies, and collected data with inclusion criteria restricted to clinical research only (either prospective or retrospective). Data on article title, co-authors, number of citations received, journal details, publication year, country and institution involved, funding, study design, marginal bone loss, survival rate, failure, follow-up, and the author’s bibliometric data were collected and evaluated. Results: A total of 29 clinical studies were published between 2008 and 2020 as 41.4% were prospective cohort studies and 48.3% originated from Germany. Most of the included studies had been published in Clinical Oral Implant Research (n = 12), and the most productive institution was the Medical Center of University of Freiburg. The author with the largest number of clinical studies on zirconia implants was Kohal R.J. (n = 10), followed by Spies B.C. (n = 8). Conclusions: This study revealed that zirconia implants have been more prominent in the last ten years, which is a valuable option for oral rehabilitation with marginal bone loss and survival rate comparable to titanium dental implants.
Keywords: zirconia implant, bibliometrics, citations, scientometric
1. Introduction
The clinical application of dental implant rehabilitation represents consolidated effectiveness in the literature due to long-term predictability and high-level satisfactory functioning and aesthetics [1,2,3,4]. Titanium alloys are the most widely used biomaterials for dental implant fixtures due to their physical, chemical, and thermal properties, which produce the osseointegrating ability of the fixture placed to replace the natural teeth [2,5,6,7,8,9,10,11,12].
Recently, the use of zirconia as an implant material has become more prevalent due to its high aesthetic characteristics, particularly in the rehabilitation of the compromised anterior jaw area, where there is fine soft-tissue biotype and the metal sensibility of the patients [13,14,15].
In fact, the literature reports that the titanium ion dissolution related to the implant corrosion could alter the natural oral microbiome and the homeostatic functional balance of the oral tissues [16,17,18,19,20].
On the contrary, it has been shown in vitro that the zirconia surface can lead to a significant decrease in periodontal pathogen adhesion compared to the titanium surface [21], alongside similar bone–implant contact compared to the titanium fixture with an almost overlapping range [22].
Additionally, Scarano et al. reported in a rabbit study that zirconia implants had about 68.4% bone–implant contact with evidence of contact osteogenesis without fibrous tissue interposition [23].
Zirconia material is distinguished by its clear ivory appearance, which is very similar to the natural color of the teeth and is characterized by an intrinsic strength and physical resistance to the loading [24,25,26]; as a result, it has been introduced as a restorative material for dental crowns, bars, abutments, and specially designed drills and burs [26,27,28,29,30,31,32,33,34]. Therefore, zirconia has recently gained further attention in the scientific community by growing research activities to confirm the clinical effectiveness of zirconia as a dental implant material.
Although citations are not an infallible metric to determine whether research is beneficial to researchers and clinicians, citations and citation analysis can quantify an article’s influence, author, subject of debate, country, journal, or a specialty [35,36]. Based on citation analysis, the bibliometric analysis aims to provide information about the trend in a research field and demonstrates its growth and development [37]; the number of citations received, researcher H-index, and journal impact factor are the most common bibliometric evaluation variables and considered as a scientific productivity score for the scientometric evaluation [38].
With the significant increase in the published articles on dental implants, recognizing trends and advances in a research field is critical and relevant to the needs of dental practitioners and researchers [39,40]. In this sense, bibliometric analysis is a useful tool for this purpose [41,42].
As far as we know, the trends and advances in zirconia dental implants have not been studied before; hence this study aimed to evaluate the bibliometric output of clinical research and co-authors in the field of zirconia dental implant rehabilitations.
2. Materials and Methods
We reported this bibliometric study in compliance with the Standards for Reporting Qualitative Research (SRQR) [43] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [44].
2.1. Search Strategy
An online literature search was conducted in Elsevier’s Scopus and Clarivate Analytics’ Web of Science (WoS) until 5 October 2020. We used the medical terms (MeSH) feature in the Cochrane Library to obtain the available synonyms for our search terms to create a detailed search strategy (Table 1).
Table 1.
Search strategy used for each database.
| Scopus | TITLE-ABS-KEY (“Zirconia” OR “Zirconium” OR “Zircon*”) AND TITLE-ABS-KEY (“Dental implant” OR “Dental implants” OR “Oral implant” OR “Oral implants” OR “Implant dentistry” OR “Dental implantology” OR “Dental Implantation” OR “Osseointegrated” OR “Osseointegrated Dental Implantation”) AND TITLE-ABS-KEY (“Intervention Study” OR “Clinical Trial” OR “Controlled Clinical Trial” OR “Randomized Controlled Trials OR “Non-Randomized Clinical Trial” OR “Nonrandomized Clinical Trial” OR “Quasi-Experimental” OR “Observational Study” OR “Prospective Study” OR “Prospective” OR “Retrospective Study” OR “Retrospective” OR “Comparative Study” OR “Multicenter Studies” OR “Epidemiologic Study” OR “Epidemiological Studies” OR “Cohort Study” OR “Case Studies” OR “Follow-Up Study” OR “Case-Control Study” OR “Case Report” OR “Case Series” OR “Pilot Study”) |
| Web of Science | TS = (“Zirconia” OR “Zirconium” OR “Zircon*”) AND TS = (“Dental implant” OR “Dental implants” OR “Oral implant” OR “Oral implants” OR “Implant dentistry” OR “Dental implantology” OR “Dental Implantation” OR “Osseointegrated” OR “Osseointegrated Dental Implantation”) AND TS = (“Intervention Study” OR “Clinical Trial” OR “Controlled Clinical Trial OR “Randomized Controlled Trials” OR “Non-Randomized Clinical Trial” OR “Nonrandomized Clinical Trial” OR “Quasi-Experimental” OR “Observational Study” OR “Prospective Study” OR “Prospective” OR “Retrospective Study” OR “Retrospective” OR “Comparative Study” OR “Multicenter Studies” OR “Epidemiologic Study” OR “Epidemiological Studies” OR “Cohort Study” OR “Case Studies” OR “Follow-Up Study” OR “Case-Control Study” OR “Case Report” OR “Case Series” OR “Pilot Study”) Timespan: All years. Databases: WOS, ARCI, BCI, KJD, MEDLINE, RSCI, SCIELO, ZOOREC. Search language = Auto. |
2.2. Data Extraction and Bibliometric Parameters
We used a specially built Excel file (Microsoft, Redmond, WA, USA) to collect the findings of the literature search. The file contained the following information: abstracts, year of publication, indexed keywords, journal name, citations as well as all co-author bibliometric data (H-index, number of papers related to zirconia implant, the total number of papers, citation of paper regarding zirconia implant, and citation of paper regarding zirconia implant). Authors with the highest quantity of clinical studies regarding zirconia dental implants were evaluated and measured the average, the standard deviation, minimum and maximum of topic paper, total papers, topic citations, overall citations, and H-index. Moreover, we evaluated the scientific trend of the included study according to the year of publication and journal details (full title, the impact factor (IF), and rank) based on the Clarivate Analytics report for 2019 with selected categories: “Dentistry, Oral Surgery & Medicine”, study design, number of citations received, marginal bone loss, survival rate, failure, and study follow-up.
2.3. Study Selection
We screened the literature search results in two steps, where the first phase was the screening of the title and abstract by paired reviewers separately. Then, the second phase was a full-text assessment by two expert reviewers (L.F and A.S). The reference list of the studies included in the full-text screening was hand-screened for potential additional studies. In this bibliometric study, inclusion criteria were only clinical studies (either prospective or retrospective) without time restrictions. Exclusion criteria were animal studies, in vitro studies, literature reviews, systematic reviews, short communications, personal opinion, letters, book chapters, and non-English studies.
2.4. Data Analysis
We used VOSviewer software (version 1.6.8; Leiden University, Leiden, The Netherlands) to visualize a term map analyzing keywords from the data obtained. “Create Map” function was used to analyze the data by using the “Citation” type and setting the unit of analysis as a “number of citations.” In the keyword map, the node’s size reflects the number of received citations, as the larger size indicates the author with the highest citations. Furthermore, keywords that often appeared together were classified as the same color in network visualization mode [45,46].
3. Results
3.1. Study Selection
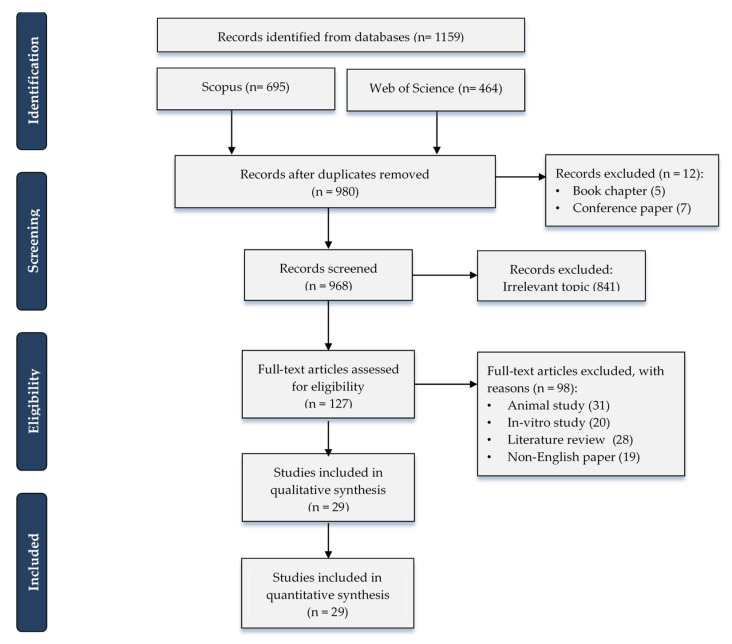
A total of 1159 references were collected from electronic databases in which (n = 185) were omitted due to duplication. By title and abstract, 968 articles were screened and 841 excluded as irrelevant topics. By the full-text screening of 127 papers, 29 studies were included in this bibliometric study [47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75] excluding the remaining 98 articles because they did not meet our inclusion criteria (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart demonstrates the process of literature search and study selection.
3.2. Study Characteristics
The included studies showed wide variability in the study design, presence/absence of a control group, experimental site, type of prosthetic rehabilitation, prosthetic connection (one-piece or two-piece), follow-up period, and different methods for evaluating the effectiveness of research. Although these differences exist, most studies reported favorable outcomes for the use of zirconia implants in oral rehabilitation. The main characteristics of the included studies are summarized in Table 2.
Table 2.
Main characteristics of the clinical research included (Zir: Zirconia implant group, Tit: Titanium implant group, IF: impact factor, RCT: Randomized controlled trial).
| Authors (Year) [Ref] |
Journal | Cited By | Study Design | Patients (Implants) | Test | Control | Marginal Bone Loss (Mean ± SD) |
Survival Rate | Failure | Follow Up | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Full Title | Rank | IF | ||||||||||
| Pirker et al. (2008) [68] |
International Journal of Oral and Maxillofacial Surgery | 33 | 2.068 | 50 | Case report | 1 (1 Implant) | Microretention and sandblasted root-analogue zirconia implant | - | - | 100% | - | 2 years |
| Pirker et al. (2009) [69] |
International Journal of Oral and Maxillofacial Surgery | 33 | 2.068 | 58 | Prospective Case Series | 18 (18 Implants) | Microretention and sandblasted root-analogue zirconia implants | Sandblasted root-analogue zirconia implants | 0.5 ± 0.7 mm | Test: 92% Control: 0% |
Test: 1 implant Control: All implants (6) |
2 years |
| Cannizzaro et al. (2010) [54] |
European Journal of Implantology | - | - | 69 | Multicenter RCT | 40 (40 Implants) | Immediate occlusal loading zirconia Implants | Immediate non-occlusal loading zirconia Implants | Test: 0.90 ± 0.48 mm Control: 0.72 ± 0.59 mm |
88.50% | 5 implants (12.5%): Test: 3 Implants Control: 2 Implants |
1 year |
| Borgonovo et al. (2011) [51] |
Minerva Stomatologica | - | - | 21 | Prospective Case Series | 16 (26 Implants) | One-piece yttrium stabilized zirconia implants | - | - | 96.16% | 1 Implant osseointegration failure | 2 years |
| Payer et al. (2012) [66] |
Clinical Oral Implants Research | 8 | 3.723 | 61 | Prospective Case Series | 20 (20 Implants) | One-piece zirconia implants | - | 1.29 ± 0.73 mm | 95% | 1 Implant osseointegration failure | 2 years |
| Akça et al. (2013) [47] |
International Journal of Oral and Maxillofacial Implants | 24 | 2.32 | 8 | Prospective Case Series | 23 (52 Implants) | - | - | 0.32 ± 0.24 mm | 100% | No failure | 2 years |
| Borgonovo et al. (2013) [52] |
Minerva Stomatologica | - | - | 10 | Prospective Case Series | 6 (14 Implants) | One-piece yttrium stabilized zirconia implants | - | 0.67 ± 0.51 mm | 100% | No failure | 4 years |
| Kohal et al. (2013) [59] |
Journal of Clinical Periodontology | 2 | 5.241 | 47 | Prospective Case Series | 28 (56 Implants) | One-piece yttria-stabilized tetragonal zirconia implants | - | 1.95 ± 0.65 | 98.20% | 1 Implant osseointegration failure | 1 year |
| Osman et al. (2013) [63] |
International Journal of Prosthodontics | 61 | 1.49 | 6 | Pilot study | 4 (28 Implants) | One-piece zirconia implants for ball abutment | - | - | 85.70% | 4 Implants | 1 year |
| Osman et al. (2014) [64] |
Clinical Oral Implants Research | 8 | 3.723 | 34 | RCT | 19 (129 Implants) | One-piece zirconia implants for ball-abutment | One-piece titanium implants for ball-abutment | Zir: 0.42 ± 0.40 Tit: 0.18 ± 0.47 |
Zir: 90.9%Tit: 95.8% | Zir: 21Implants (3 fractured) Tit: 10Implants |
1 year |
| Becker et al. (2015) [50] |
Clinical Oral Implants Research | 8 | 3.723 | 15 | Prospective Cohort Study | 52 (52 Implants) | Two-piece zirconia implants | - | - | 95.80% | 2 Implants | 2 years |
| Cionca et al. (2015) [55] |
Clinical Oral Implants Research | 8 | 3.723 | 43 | Prospective Case Series | 32 (49 Implants) | Two-piece zirconia implants | - | - | 87% | 6 Implants | 1 year |
| Jung et al. (2015) [56] |
Clinical Oral Implants Research | 8 | 3.723 | 27 | Prospective Cohort Study | 60 (71 Implants) | Immediate one-piece zirconia implants | - | 0.78 ± 0.79 mm | 98.30% | 1 implant osseointegration failure | 1 year |
| Payer et al. (2015) [67] |
Clinical Oral Implants Research | 8 | 3.723 | 41 | RCT | 22 (31 Implants) | Two-piece zirconia implants | Two-piece titanium implants | Zir: 1.48 ± 1.05 Tit: 1.43 ± 0.67 |
Zir: 93.3% Tit: 100% |
Zir: 1 Implant Tit: No failure |
2 years |
| Siddiqi et al. (2015) [70] |
Clinical Implant Dentistry and Related Research | 9 | 3.396 | 17 | RCT | 22 (150 Implants) | One-piece zirconia implants for ball-abutment | Titanium implants for one-piece ball-abutment | Zir: 2.23 ± 0.69 Tit: 1.59 ± 0.33 |
Zir: 67.6% Tit: 66.7% |
Zir: 16 Implants Tit: 7 Implants |
1 year |
| Spies et al. (2015) [73] |
Journal of Dental Research | 3 | 4.914 | 22 | Prospective Cohort Study | 40 (53 Implants) | One-piece alumina-toughened zirconia implant | - | 0.79 ± 0.47 mm | 94.2% | 3 Implants osseointegration failure | 3 years |
| Patankar et al. (2016) [65] |
Journal of Maxillofacial and Oral Surgery | - | - | 3 | Case report | 1 (1 Implant) | Microretention and sandblasted root-analogue zirconia implant | - | - | 100% | - | 1.5 year |
| Spies et al. (2016) [74] |
Clinical Oral Implants Research | 8 | 3.723 | 13 | Prospective Cohort Study | 27 (27 Implants) | Immediate one-piece alumina-toughened zirconia implant | - | 0.77 ± 0.31 mm | 88.90% | 3 Implants osseointegration failure | 1 year |
| Kniha et al. (2017) [58] |
International Journal of Oral and Maxillofacial Surgery | 33 | 2.068 | 9 | Prospective Cohort Study | 81 (105 Implants) | Zirconia implants | - | 0.66 ± 0.33 mm | 100% | No failure | 3 years |
| Kniha et al. (2017) [57] |
International Journal of Oral and Maxillofacial Surgery | 33 | 2.068 | 9 | Prospective Cohort Study | 78 (82 Implants) | Immediate loading one-piece zirconia implants | Delayed one-piece zirconia implants | Immediate: 0.76 ± 1.13 mm Delayed: 0.83 ± 0.65 mm |
Immediate: 100% Delayed: 100% |
No failure | 1 year |
| Spies et al. (2017) [71] |
Journal of Dentistry | 10 | 3.242 | 6 | Prospective Case Series | 60 (71 Implants) | One-piece zirconia oral implants | - | - | 100% | No failure | 3 years |
| Spies et al. (2017) [75] |
Clinical Oral Implants Research | 8 | 3.723 | 11 | Prospective Case Series | 13 (26 Implants) | One-piece zirconia implants | - | - | 100% | No failure | 5 years |
| Balmer et al. (2018) [49] |
Clinical Oral Implants Research | 8 | 3.723 | 11 | Prospective Multicenter Cohort Study | 60 (71 Implants) | One-piece immediate loading zirconia implants | - | 0.70 ± 0.72 mm | 98.50% | 1 Implant osseointegration failure | 3 years |
| Bormann et al. (2018) [53] |
BMC Oral Health | 38 | 1.911 | 7 | Prospective Multicenter Cohort Study | 44 (44 Implants) | Zirconia implants | - | 0.97 ± 0.88 mm | 97.50% | 1 Implant | 3 years |
| Kohal et al. (2018) [60] |
Journal of Clinical Periodontology | 2 | 5.241 | 5 | Prospective Cohort Study | 65 (65 Implants) | Immediate loading one-piece zirconia implants | - | 1.45 ± 1.96 mm | 90.80% | 6 Implants | 3 years |
| Lorenz et al. (2019) [62] |
Clinical Implant Dentistry and Related Research | 9 | 3.396 | 4 | Prospective Cohort Study | 28 (83 Implants) | Zirconia implants | Natural teeth | 1.2 ± 0.76 mm | 100% | No failure one peri-implantitis resistant to therapies | 7.8 years |
| Spies et al. (2019) [72] |
Clinical Oral Implants Research | 8 | 3.723 | 5 | Prospective Multicenter Cohort Study | 45 (45 Implants) | Zirconia implants | - | - | 97.5 ± 2.47%. | Chipping (n = 19) occlusal roughness (n = 35) | 5 years |
| Balmer et al. (2020) [48] |
Clinical Oral Implants Research | 8 | 3.723 | 4 | Prospective Multicenter Cohort Study | 60 (71 Implants) | Single crown one-piece zirconia implant | Multiple prostheses one-piece zirconia implant | 0.7 ± 0.6 mm | 98.4% | 1 Implant | 5 years |
| Koller et al. (2020) [61] |
Clinical Oral Implants Research | 8 | 3.723 | 0 | Pilot RCT | 22 (31 Implants) | Two-piece zirconia implants | Two-piece titanium implants | Zir: 1.38 ± 0.81 Tit: 1.17 ± 0.73 mm |
Zir: 87.5%Tit: 93.3% | Zir: 2 Implants Tit: 1 Implant |
6.67 years |
A total of 21 studies evaluated monolithic or one-piece zirconia implants [47,48,49,51,52,53,54,56,57,58,60,62,64,66,70,71,72,73,74,76], two of which had titanium implants as their control and showed no significant difference in survival rate and marginal bone loss between groups (p > 0.05) [64,70]. Two studies evaluated the immediate loading of zirconia implants [53,64]: one study compared it to the non-occlusal loading procedure [64], while the other study compared it with the standard loading protocol [57]. Furthermore, 26 papers assessed the cylindrical microgeometry of zirconia implants [47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,67,70,71,72,73,74,75], while three studies evaluated the root-analog zirconia implants obtained by a three-dimensional scan [66,68,69]. However, Akça et al. and Pirker et al. reported the lowest marginal bone loss after two years (0.31 ± 0.24 and 0.5 ± 0.7 mm, respectively), in which Akça et al. used specially designed titanium–zirconia alloy implants [47], and Pirker et al. used specially designed root-analog zirconia implants with a micro-retention surface in a fresh extraction socket [69].
3.3. Growth of Publications
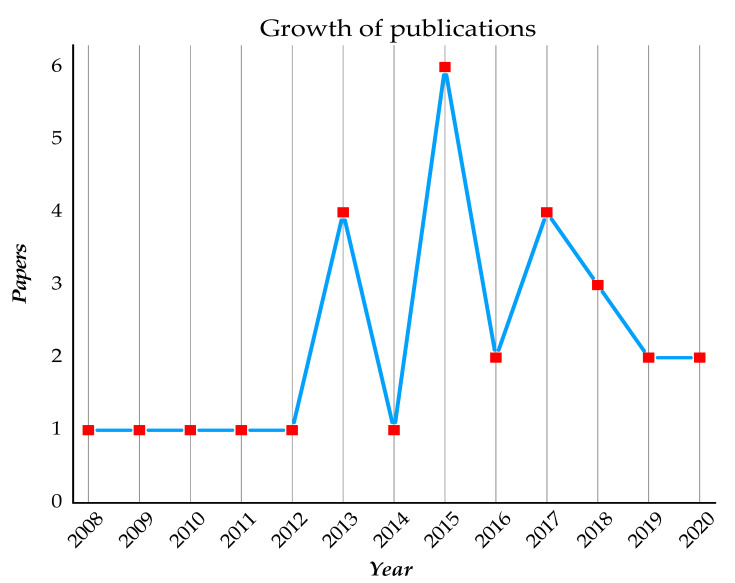
In total, 29 clinical studies were published between 2008 and 2020, in which 19 papers (65.5%) were published in the last five years and ten papers published before 2015. The highest number of published studies was in 2015 (n = 6, 20.6%) followed by 2013 and 2017 (n = 4, 13.7% for each) (Figure 2).
Figure 2.
Publication trend of the clinical studies on the zirconia implants.
3.4. Journal of Publication
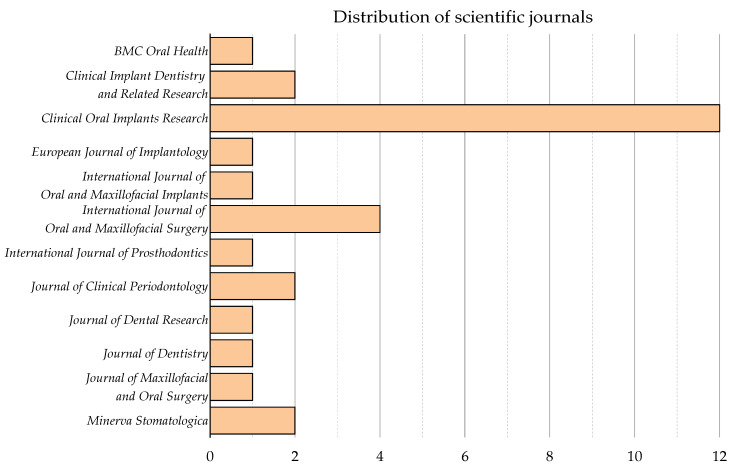
The clinical studies on the use of zirconia dental implants for oral rehabilitation were published across ten peer-reviewed journals. The journal with the largest number of publications was “Clinical Oral Implants Research” (n = 12, 41%), followed by “International Journal of Oral and Maxillofacial Surgery” (n = 4, 13.7%) (Figure 3).
Figure 3.
Contribution journals in clinical research on zirconia implants.
The majority of publications were published in Q1 journals (n = 25, 86%), while the journal with the highest impact factor was “Journal of Clinical Periodontology” (IF = 5.241), which had two articles.
3.5. Study Design and Level of Evidence
All included studies were prospective, while the most common study design of clinical research on zirconia implants was cohort study (n = 12, 41.4%), followed by case series (n = 9, 31%), and RCT (n = 5, 17%). According to the hierarchy of evidence levels (Is) [77,78], the available evidence supporting the use of zirconia implants is 17% level II, 41.4% EL IV, and the remaining EL VI.
3.6. Contribution of Countries and Institutions
The majority of the studies originated from institutions in Germany (n = 14, 48.3%), followed by Switzerland, (n = 6, 20.7%), and Austria (n = 5, 17%), where the most productive institution was the Medical Center of University of Freiburg (n = 8, 27.6%), followed by the Center of Dental Medicine, University of Zürich (n = 5, 17%). While many of the included studies were funded, the most funding support for included research was provided by VITA Zahnfabrik—H. Rauter GmbH & Co. KG, Bad Säckingen, Germany (n = 5, 17%) (Table 3).
Table 3.
Contribution of countries and institutions to clinical studies on zirconia implants.
| Country | Institution | Study [Ref] | Funding |
|---|---|---|---|
| Germany | Universitätsklinikum Düsseldorf, Düsseldorf | Becker et al., 2015 [50] | ZV3 Zircon Vision GmbH, Wolfratshausen, Germany |
| University Hospital Aachen, Aachen | Kniha et al., 2017 [57] | No Funding | |
| Friedrich-Alexander-University Erlangen-Nürnberg | Kniha et al., 2017 [58] | ||
| Johann-Wolfgang Goethe University, Frankfurt/Main | Lorenz et al., 2019 [62] | ||
| Hannover Medical School, Hannover | Bormann et al., 2018 [53] | Institut Straumann AG, Basel, Switzerland | |
| School of Dentistry, Albert-Ludwigs University, Freiburg | Kohal et al., 2013 [59] | Nobel Biocare AB, Göteborg, Sweden | |
| Medical Center of University of Freiburg, Freiburg | Kohal et al., 2018 [60] | ||
| Spies et al., 2015 [73] | Metoxit AG (Thayngen, Switzerland) | ||
| Spies et al., 2016 [74] | |||
| Spies et al., 2017 [75] | Ivoclar Vivadent | ||
| Germany and Switzerland | Medical Center of University of Freiburg, Freiburg and Center of Dental Medicine, University of Zürich, Zürich | Spies et al., 2017 [71] | VITA Zahnfabrik—H. Rauter GmbH & Co. KG, Bad Säckingen, Germany |
| Balmer et al., 2018 [49] | |||
| Spies et al., 2019 [72] | |||
| Balmer et al., 2020 [48] | |||
| Switzerland | School of Dental Medicine, University of Geneva, Geneva | Cionca et al., 2015 [55] | Dentalpoint AG, Zürich, Switzerland |
| Center of Dental Medicine, University of Zürich, Zürich | Jung et al., 2015 [56] | VITA Zahnfabrik—H. Rauter GmbH & Co. KG, Bad Säckingen, Germany | |
| Austria | Alfred Kocher, Medical University Vienna, Vienna | Pirker et al., 2008 [68] | No Funding |
| Pirker et al., 2009 [69] | |||
| School of Dentistry, Medical University Graz, Graz | Payer et al., 2012 [66] | Bredent medical GmbH, Senden, Germany | |
| Payer et al., 2015 [67] | Ziterion GmbH, Uffenheim, Germany | ||
| Koller et al., 2020 [61] | |||
| Italy | Private practice | Cannizzaro et al., 2010 [54] | Partially supported by Z-systems |
| School of Dentistry, University of Milan, Milan | Borgonovo et al., 2011 [51] | Not reported | |
| Borgonovo et al., 2013 [52] | |||
| New Zealand | Oral Implantology Research Group, Sir John Walsh Research Institute, School of Dentistry, University of Otago | Osman et al., 2013 [63] | Oral Implantology Research Group, Sir John Walsh Research Institute, School of Dentistry, University of Otago and Southern Implants |
| Osman et al., 2014 [64] | |||
| Siddiqi et al., 2015 [70] | |||
| India | BV Dental College and Hospital, Pune | Patankar et al., 2016 [65] | No Funding |
| Turkey | Faculty of Dentistry, Hacettepe University | Akça et al., 2013 [47] | No Funding |
3.7. Bibliometric Assessment
A total of 29 articles with total citations[Scopus] ranged from 0 to 176 (mean 57.28 ± 42.18), while the number of citations[Scopus] received by each paper ranged from 0 to 69 (mean 21.3 ± 20). The top-cited study was the RCT of Cannizzaro et al. (2010) (n[Scopus] = 69) [54], followed by the prospective case series of Payer et al. (2012) (n[Scopus] = 61) [66], and Pirker et al. (2009) (n[Scopus] = 58) [69].
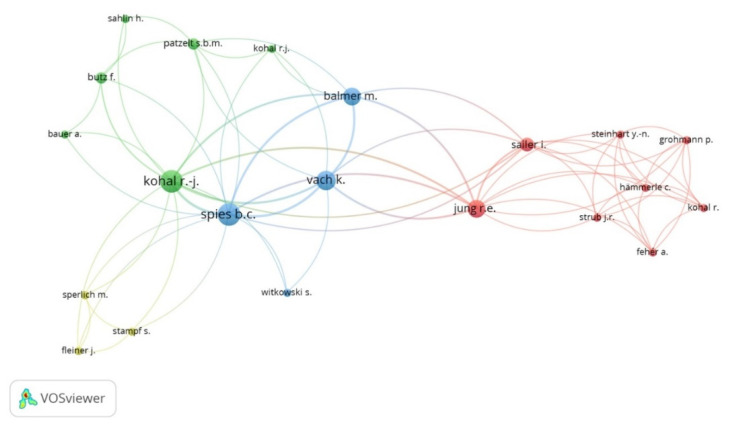
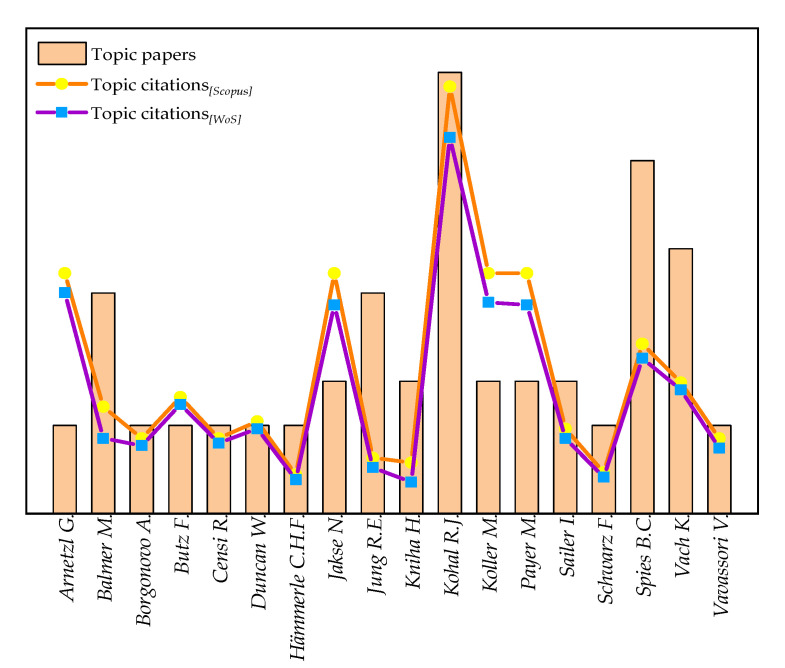
However, the author with the highest number of clinical research on zirconia implants was Kohal R.J. (n = 10), followed by Spies B.C. (n = 8) and Vach K. (n = 6), while the top-cited author of clinical studies on zirconia implants was Kohal R.J. (n[WoS] = 155), followed by Arnetzl G. (n[WoS] = 91), Koller M. (n[WoS] = 87), Payer M., and Jakse N. (n[WoS] = 86 for each) (Figure 4 and Figure 5).
Figure 4.
Network analysis of the authors with the largest number of clinical studies on zirconia implants.
Figure 5.
Bibliometric variables for authors with the highest number of topic papers.
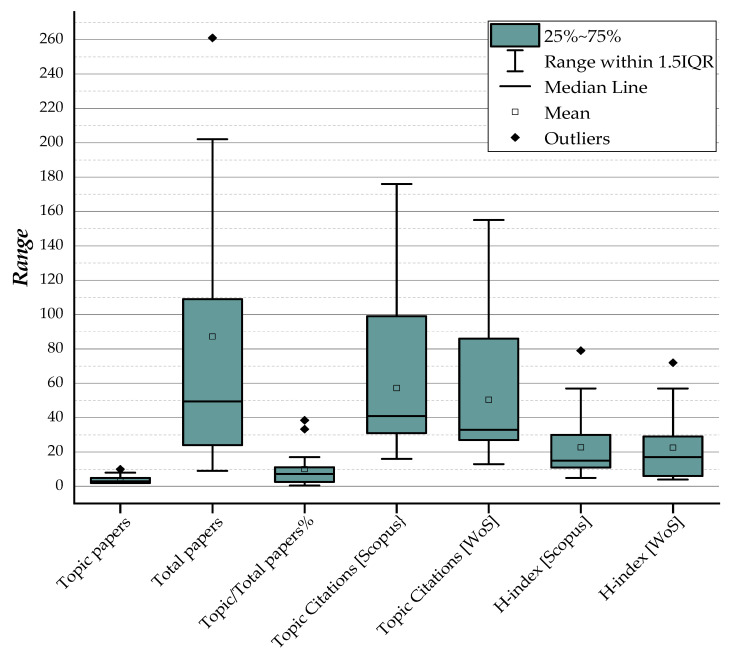
The authors’ H-indexScopus ranged from one to 79 (mean 22.67 ± 19.96), and the author with the most bibliometric characteristics was Hämmerle C.H.F., who had 364 publications (two of which were clinical studies on zirconia implants) with 8311 total citations and H-indexScopus = 79 (Table 4 and Figure 6).
Table 4.
General bibliometric variables for authors with the largest number of topic papers.
| Author | Topic Papers | Total Papers | Topic/Total Papers % | Topic Citations [Scopus] | Topic Citations [WoS] | Total Citations [Scopus] |
Total Citation [WoS] | Topic/Total Citations % [Scopus-WoS] | H-index [Scopus] | H-index [WoS] |
|---|---|---|---|---|---|---|---|---|---|---|
| Kohal R.J. | 10 | 109 | 9.17% | 176 | 155 | 3053 | 2975 | [5.76–5.21%] | 30 | 29 |
| Spies B.C. | 8 | 47 | 17.02% | 70 | 64 | 452 | 448 | [15.49–14.29%] | 14 | 14 |
| Vach K. | 6 | 73 | 8.22% | 54 | 51 | 661 | 820 | [8.17–6.21%] | 15 | 16 |
| Balmer M. | 5 | 13 | 38.46% | 44 | 31 | 256 | 130 | [17.19–23.84%] | 7 | 5 |
| Jung R.E. | 5 | 202 | 2.48% | 23 | 19 | 8359 | 9126 | [0.28–0.21%] | 47 | 57 |
| Jakse N. | 3 | 70 | 4.29% | 99 | 86 | 1114 | 981 | [8.89–8.77%] | 18 | 18 |
| Kniha H. | 3 | 28 | 10.71% | 21 | 13 | 664 | 726 | [3.16–1.779%] | 11 | 13 |
| Koller M. | 3 | 9 | 33.33% | 99 | 87 | 166 | 312 | [59.64–27.88%] | 5 | 5 |
| Payer M. | 3 | 48 | 6.25% | 99 | 86 | 770 | 1484 | [12.86–5.79%] | 15 | 23 |
| Sailer I. | 3 | 113 | 2.65% | 35 | 31 | 6027 | 5713 | [0.58–0.54%] | 34 | 33 |
| Arnetzl G. | 2 | 40 | 5.00% | 99 | 91 | 437 | 183 | [22.65–49.72%] | 11 | 6 |
| Butz F. | 2 | 24 | 8.33% | 48 | 45 | 1248 | 1441 | [3.85–3.12%] | 18 | 19 |
| Censi R. | 2 | 18 | 11.11% | 31 | 29 | 169 | 95 | [18.34–30.52%] | 8 | 4 |
| Duncan W. | 2 | 87 | 2.30% | 38 | 35 | 2163 | 1356 | [1.76–2.58%] | 20 | 19 |
| Hämmerle C.H.F. | 2 | 364 | 0.55% | 16 | 14 | 18,311 | 16,032 | [0.09–0.08%] | 79 | 72 |
| Schwarz F. | 2 | 261 | 0.77% | 17 | 15 | 9093 | 9169 | [0.19–0.16%] | 57 | 57 |
| Vavassori V. | 2 | 12 | 16.67% | 31 | 27 | 136 | 96 | [22.79–28.12%] | 7 | 5 |
| Borgonovo A. | 2 | 51 | 3.92% | 31 | 28 | 535 | 449 | [5.79–6.23%] | 12 | 11 |
|
Summary
(Mean ± SD) |
3.61 ± 2.33 | 87.17 ± 96.37 | 10.07 ± 0.11% | 57.28 ± 42.18 | 50.39 ± 37.68 | 2978.56 ± 4750.05 | 2863.11 ± 4386.90 | - | 22.67 ± 19.96 | 22.56 ± 20.14 |
Figure 6.
Box plots summarize the bibliometric variables of the authors with the largest number of studies.
4. Discussion
The present study carried out a bibliometric evaluation of clinical research on zirconia implant rehabilitation, highlighting the significant heterogeneity of the included studies, which revealed considerable variations in methodology, technical approaches, follow-up, and control group involvement. Our findings indicate that there is a trend for zirconia implants in oral rehabilitation as there has been an increase in about 180% of the studies published in the last five years.
The included studies reported a survival rate for zirconia implants ranging from 87% to 100% with follow-up periods from one to 7.8 years, while the least survival rate reported in RCT by Siddiqi et al. was 67.6% after one-year follow-up (i.e., 16 zirconia implants failed out of 68) [70]. This RCT aimed to study the effectiveness of zirconia vs. titanium implants restored with one-piece ball-abutment in mandibular and maxillary overdentures, while this high decrease in the survival rate was for both groups (i.e., 67.6% for zirconia implants and 66.7% for titanium implants); the outcomes of maxillary rehabilitation were worse than the mandible, while no mechanical fractures of the fixtures were reported [70].
Although one-piece and two-piece zirconia implants have been evaluated, the lower marginal bone loss and higher survival rates were observed in studies of one-piece zirconia implant rehabilitation on a single tooth or three element prosthetic rehabilitation [59,61]. However, the studies did not report any differences in the marginal bone loss and survival rate between the single crown and the fixed multiple zirconia implant recovery, while the prosthetic connection appears to have no apparent effect on these parameters [48]. Additionally, Lorenz et al. showed no significant difference in marginal bone loss with a total of 83 zirconia implants compared to natural teeth after 7.8 years of function [47], and the marginal bone loss was similar in the other studies, which was less than 1 mm in the first year and stabilized in subsequent functional loading [47,48,49,52,56,57,58,64,69,73,74]. Moreover, the prospective study by Kniha et al. contained the largest sample size of the included studies involving 81 patients with 105 implants for fixed rehabilitation, who reported a significant decrease of 0.66 ± 0.30 mm with a survival rate of 100% after three years [58].
However, the most common complication (70%) was the failure of implant osseointegration as 17 studies reported a loss of at least one implant in the first six months [48,49,50,51,53,54,55,56,59,60,61,63,64,66,67,69,70,72,73,74].
As previously reported for titanium dental implant threads, microgeometry appears to have a significant effect on the osseointegration of zirconia implants [79,80], whereas a more retentive surface resulted in an increased survival rate compared to a sandblasted surface only [68,69].
Although all clinical research included in this analysis was screened and selected from the Scopus and Web of Science databases, which may avoid restriction in each database [39,81], our investigation has further limitations. First, the year of publication, which is a reliable indicator of the number of citations received, as older papers receive more citations than recent publications because there is more time to cite them, regardless of their impact [82,83]. Second, open access policies have a significant influence on the citations received in the evaluated papers [84,85,86], as a result, we found large heterogeneity in Topic/Total Citations% and co-authors’ H-index.
5. Conclusions
This was the first study highlighting bibliometric output of clinical research and co-authors in the field of zirconia dental implants and shows a strong interest in the development of research into the clinical application of zirconia dental implants, as evidenced by the increase in the number of scientific papers published in the last ten years.
Author Contributions
Conceptualization, F.L. and A.S.; Methodology, F.L. and A.G.A.K.; Software, F.L.; Validation, F.L. and A.S.; Formal analysis, F.L. and A.G.A.K.; Investigation, A.S., F.L. and B.R.; Data curation, F.L., A.G.A.K. and A.S.; Writing—original draft preparation, F.L. and A.S.; Writing—review and editing, F.L., A.G.A.K. and S.N.; Visualization, A.S., B.R. and I.F.; Supervision, A.S. and I.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
Authors declare no conflicts of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Albrektsson T., Wennerberg A. On osseointegration in relation to implant surfaces. Clin. Implant Dent. Relat. Res. 2019;21(Suppl. 1):4–7. doi: 10.1111/cid.12742. [DOI] [PubMed] [Google Scholar]
- 2.Buser D., Janner S.F.M., Wittneben J.-G., Brägger U., Ramseier C.A., Salvi G.E. 10-Year Survival and Success Rates of 511 Titanium Implants with a Sandblasted and Acid-Etched Surface: A Retrospective Study in 303 Partially Edentulous Patients. Clin. Implant Dent. Relat. Res. 2012;14:839–851. doi: 10.1111/j.1708-8208.2012.00456.x. [DOI] [PubMed] [Google Scholar]
- 3.Degidi M., Piattelli A. A 7-year Follow-up of 93 Immediately Loaded Titanium Dental Implants. J. Oral Implantol. 2005;31:25–31. doi: 10.1563/0-730.1. [DOI] [PubMed] [Google Scholar]
- 4.Scarano A., Inchingolo F., Murmura G., Traini T., Piattelli A., Lorusso F. Three-Dimensional Architecture and Mechanical Properties of Bovine Bone Mixed with Autologous Platelet Liquid, Blood, or Physiological Water: An In Vitro Study. Int. J. Mol. Sci. 2018;19 doi: 10.3390/ijms19041230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barros R.R.M., Degidi M., Novaes A.B., Piattelli A., Shibli J.A., Iezzi G. Osteocyte Density in the Peri-Implant Bone of Immediately Loaded and Submerged Dental Implants. J. Periodontol. 2009;80:499–504. doi: 10.1902/jop.2009.080484. [DOI] [PubMed] [Google Scholar]
- 6.Gehrke S., Mazón P., Del Fabbro M., Tumedei M., Aramburú Júnior J., Pérez-Díaz L., De Aza P. Histological and Histomorphometric Analyses of Two Bovine Bone Blocks Implanted in Rabbit Calvaria. Symmetry. 2019;11:641. doi: 10.3390/sym11050641. [DOI] [Google Scholar]
- 7.Scarano A., Carinci F., Lorusso F., Festa F., Bevilacqua L., Santos de Oliveira P., Maglione M. Ultrasonic vs Drill Implant Site Preparation: Post-Operative Pain Measurement Through VAS, Swelling and Crestal Bone Remodeling: A Randomized Clinical Study. Mater. Basel. 2018;11:2516. doi: 10.3390/ma11122516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scarano A., Crincoli V., Di Benedetto A., Cozzolino V., Lorusso F., Podaliri Vulpiani M., Grano M., Kalemaj Z., Mori G., Grassi F.R. Bone Regeneration Induced by Bone Porcine Block with Bone Marrow Stromal Stem Cells in a Minipig Model of Mandibular “Critical Size” Defect. Stem. Cells Int. 2017;2017:9082869. doi: 10.1155/2017/9082869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scarano A., De Oliveira P.S., Traini T., Lorusso F. Sinus Membrane Elevation with Heterologous Cortical Lamina: A Randomized Study of a New Surgical Technique for Maxillary Sinus Floor Augmentation without Bone Graft. Mater. Basel. 2018;11:1457. doi: 10.3390/ma11081457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Piattelli A., Scarano A., Piattelli M. Detection of alkaline and acid phosphatases around titanium implants: A light microscopical and histochemical study in rabbits. Biomaterials. 1995;16:1333–1338. doi: 10.1016/0142-9612(95)91049-5. [DOI] [PubMed] [Google Scholar]
- 11.Comuzzi L., Tumedei M., Piattelli A., Iezzi G. Short vs. Standard Length Cone Morse Connection Implants: An In Vitro Pilot Study in Low Density Polyurethane Foam. Symmetry. 2019;11:1349. doi: 10.3390/sym11111349. [DOI] [Google Scholar]
- 12.Tumedei M., Savadori P., Del Fabbro M. Synthetic Blocks for Bone Regeneration: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2019;20:4221. doi: 10.3390/ijms20174221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Afrashtehfar K.I., Del Fabbro M. Clinical performance of zirconia implants: A meta-review. J. Prosthet. Dent. 2020;123:419–426. doi: 10.1016/j.prosdent.2019.05.017. [DOI] [PubMed] [Google Scholar]
- 14.Hanawa T. Zirconia versus titanium in dentistry: A review. Dent. Mater. J. 2020;39:24–36. doi: 10.4012/dmj.2019-172. [DOI] [PubMed] [Google Scholar]
- 15.Hashim D., Cionca N., Courvoisier D.S., Mombelli A. A systematic review of the clinical survival of zirconia implants. Clin. Oral Investig. 2016;20:1403–1417. doi: 10.1007/s00784-016-1853-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cantore S., Mirgaldi R., Ballini A., Coscia M.F., Scacco S., Papa F., Inchingolo F., Dipalma G., De Vito D. Cytokine gene polymorphisms associate with microbiogical agents in periodontal disease: Our experience. Int. J. Med. Sci. 2014;11:674–679. doi: 10.7150/ijms.6962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noronha Oliveira M., Schunemann W.V.H., Mathew M.T., Henriques B., Magini R.S., Teughels W., Souza J.C.M. Can degradation products released from dental implants affect peri-implant tissues? J. Periodontal Res. 2017;53:1–11. doi: 10.1111/jre.12479. [DOI] [PubMed] [Google Scholar]
- 18.Noumbissi S., Scarano A., Gupta S. A Literature Review Study on Atomic Ions Dissolution of Titanium and Its Alloys in Implant Dentistry. Mater. Basel. 2019;12:368. doi: 10.3390/ma12030368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ottria L., Lauritano D., Andreasi Bassi M., Palmieri A., Candotto V., Tagliabue A., Tettamanti L. Mechanical, chemical and biological aspects of titanium and titanium alloys in implant dentistry. J. Biol. Regul. Homeost. Agents. 2018;32(Suppl. 1):81–90. [PubMed] [Google Scholar]
- 20.Rodrigues D.C., Valderrama P., Wilson T.G., Palmer K., Thomas A., Sridhar S., Adapalli A., Burbano M., Wadhwani C. Titanium Corrosion Mechanisms in the Oral Environment: A Retrieval Study. Mater. Basel. 2013;6:5258–5274. doi: 10.3390/ma6115258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scarano A., Piattelli M., Caputi S., Favero G.A., Piattelli A. Bacterial Adhesion on Commercially Pure Titanium and Zirconium Oxide Disks: An In Vivo Human Study. J. Periodontol. 2004;75:292–296. doi: 10.1902/jop.2004.75.2.292. [DOI] [PubMed] [Google Scholar]
- 22.Mihatovic I., Golubovic V., Becker J., Schwarz F. Bone tissue response to experimental zirconia implants. Clin. Oral Investig. 2016;21:523–532. doi: 10.1007/s00784-016-1904-2. [DOI] [PubMed] [Google Scholar]
- 23.Scarano A., Di Carlo F., Quaranta M., Piattelli A. Bone Response to Zirconia Ceramic Implants: An Experimental Study in Rabbits. J. Oral Implantol. 2003;29:8–12. doi: 10.1563/1548-1336(2003)029<0008:BRTZCI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Agustín-Panadero R., Serra-Pastor B., Roig-Vanaclocha A., Fons-Font A., Solá-Ruiz M.F. Fracture resistance and the mode of failure produced in metal-free crowns cemented onto zirconia abutments in dental implants. PLoS ONE. 2019;14:e0220551. doi: 10.1371/journal.pone.0220551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bethke A., Pieralli S., Kohal R.-J., Burkhardt F., von Stein-Lausnitz M., Vach K., Spies B.C. Fracture Resistance of Zirconia Oral Implants In Vitro: A Systematic Review and Meta-Analysis. Mater. Basel. 2020;13:562. doi: 10.3390/ma13030562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sailer I., Asgeirsson A.G., Thoma D.S., Fehmer V., Aspelund T., Özcan M., Pjetursson B.E. Fracture strength of zirconia implant abutments on narrow diameter implants with internal and external implant abutment connections: A study on the titanium resin base concept. Clin. Oral Implant. Res. 2018;29:411–423. doi: 10.1111/clr.13139. [DOI] [PubMed] [Google Scholar]
- 27.Cao Y., Yu C., Wu Y., Li L., Li C. Long-Term Survival and Peri-Implant Health of Titanium Implants with Zirconia Abutments: A Systematic Review and Meta-Analysis. J. Prosthodont. 2019;28:883–892. doi: 10.1111/jopr.13097. [DOI] [PubMed] [Google Scholar]
- 28.Fanali S., Tumedei M., Pignatelli P., Inchingolo F., Pennacchietti P., Pace G., Piattelli A. Implant primary stability with an osteocondensation drilling protocol in different density polyurethane blocks. Comput. Methods Biomech. Biomed. Eng. 2020:1–7. doi: 10.1080/10255842.2020.1806251. [DOI] [PubMed] [Google Scholar]
- 29.Fujiwara S., Kato S., Bengazi F., Urbizo Velez J., Tumedei M., Kotsu M., Botticelli D. Healing at implants installed in osteotomies prepared either with a piezoelectric device or drills: An experimental study in dogs. Oral Maxillofac. Surg. 2020 doi: 10.1007/s10006-020-00895-y. [DOI] [PubMed] [Google Scholar]
- 30.Kermanshah H., Geramy A., Ebrahimi S.F., Bitaraf T. IPS-Empress II inlay-retained fixed partial denture reinforced with zirconia bar: Three-dimensional finite element andin-vitrostudies. Acta Odontol. Scand. 2012;70:569–576. doi: 10.3109/00016357.2011.640283. [DOI] [PubMed] [Google Scholar]
- 31.Kotsu M., Urbizo Velez J., Bengazi F., Tumedei M., Fujiwara S., Kato S., Botticelli D. Healing at implants installed from ~ 70- to <10-Ncm insertion torques: An experimental study in dogs. Oral Maxillofac. Surg. :2020. doi: 10.1007/s10006-020-00890-3. [DOI] [PubMed] [Google Scholar]
- 32.Scarano A., Di Carlo F., Piattelli A. Effect of sterilization and cleansing on implantology drills: Zirconia vs steel. Ital. Oral Surg. 2008;3:61–72. [Google Scholar]
- 33.Scarano A., Valbonetti L., Marchetti M., Lorusso F., Ceccarelli M. Soft Tissue Augmentation of the Face with Autologous Platelet-Derived Growth Factors and Tricalcium Phosphate. Microtomography Evaluation of Mice. J Craniofac. Surg. 2016;27:1212–1214. doi: 10.1097/SCS.0000000000002712. [DOI] [PubMed] [Google Scholar]
- 34.Scarano A., Piattelli A., Quaranta A., Lorusso F. Bone Response to Two Dental Implants with Different Sandblasted/Acid-Etched Implant Surfaces: A Histological and Histomorphometrical Study in Rabbits. BioMed Res. Int. 2017;2017:8724951. doi: 10.1155/2017/8724951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ibrahim G.M., Carter Snead O., Rutka J.T., Lozano A.M. The most cited works in epilepsy: Trends in the “Citation Classics”. Epilepsia. 2012;53:765–770. doi: 10.1111/j.1528-1167.2012.03455.x. [DOI] [PubMed] [Google Scholar]
- 36.Parker J.N., Lortie C., Allesina S. Characterizing a scientific elite: The social characteristics of the most highly cited scientists in environmental science and ecology. Scientometrics. 2010;85:129–143. doi: 10.1007/s11192-010-0234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Park K.M., Park B.S., Park S., Yoon D.Y., Bae J.S. Top-100 cited articles on headache disorders: A bibliometric analysis. Clin. Neurol. Neurosurg. 2017;157:40–45. doi: 10.1016/j.clineuro.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 38.Lorusso F., Inchingolo F., Scarano A. Scientific Production in Dentistry: The National Panorama through a Bibliometric Study of Italian Academies. BioMed Res. Int. 2020;2020:3468303. doi: 10.1155/2020/3468303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jayaratne Y.S.N., Zwahlen R.A. The evolution of dental journals from 2003 to 2012: A bibliometric analysis. PLoS ONE. 2015;10:e0119503. doi: 10.1371/journal.pone.0119503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pommer B., Valkova V., Ubaidha Maheen C., Fürhauser L., Rausch-Fan X., Seeman R. Scientific Interests of 21st Century Clinical Oral Implant Research: Topical Trend Analysis. Clin. Implant Dent. Relat. Res. 2015;18:850–856. doi: 10.1111/cid.12371. [DOI] [PubMed] [Google Scholar]
- 41.Gutiérrez-Vela M.M., Díaz-Haro A., Berbel-Salvador S., Lucero-Sánchez A., Robinson-García N., Cutando-Soriano A. Bibliometric analysis of research on regenerative periodontal surgery during the last 30 years. J. Clin. Exp. Dent. 2012;4:e112–e118. doi: 10.4317/jced.50646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tetè S., Zizzari V.L., De Carlo A., Lorusso F., Di Nicola M., Piattelli A., Gherlone E., Polimeni A. Characterizing scientific production of Italian Oral Surgery professionals through evaluation of bibliometric indices. Ann. Di Stomatol. 2014;5:23. doi: 10.11138/ads/2014.5.1.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Brien B.C., Harris I.B., Beckman T.J., Reed D.A., Cook D.A. Standards for Reporting Qualitative Research. Acad. Med. 2014;89:1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 44.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van Eck N.J., Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523–538. doi: 10.1007/s11192-009-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Van Eck N.J., Waltman L. VOSviewer manual. Leiden Univeristeit Leiden. 2013;1:1–53. [Google Scholar]
- 47.Akça K., Cavusoglu Y., Uysal S., Cehreli M.C. A Prospective, Open-Ended, Single-Cohort Clinical Trial on Early Loaded Titanium-Zirconia Alloy Implants in Partially Edentulous Patients: Up-to-24-Month Results. Int. J. Oral Maxillofac. Implant. 2013;28:573–578. doi: 10.11607/jomi.3088. [DOI] [PubMed] [Google Scholar]
- 48.Balmer M., Spies B.C., Kohal R.J., Hämmerle C.H.F., Vach K., Jung R.E. Zirconia implants restored with single crowns or fixed dental prostheses: 5-year results of a prospective cohort investigation. Clin. Oral Implant. Res. 2020;31:452–462. doi: 10.1111/clr.13581. [DOI] [PubMed] [Google Scholar]
- 49.Balmer M., Spies B.C., Vach K., Kohal R.-J., Hämmerle C.H.F., Jung R.E. Three-year analysis of zirconia implants used for single-tooth replacement and three-unit fixed dental prostheses: A prospective multicenter study. Clin. Oral Implant. Res. 2018;29:290–299. doi: 10.1111/clr.13115. [DOI] [PubMed] [Google Scholar]
- 50.Becker J., John G., Becker K., Mainusch S., Diedrichs G., Schwarz F. Clinical performance of two-piece zirconia implants in the posterior mandible and maxilla: A prospective cohort study over 2 years. Clin. Oral Implant. Res. 2015;28:29–35. doi: 10.1111/clr.12610. [DOI] [PubMed] [Google Scholar]
- 51.Borgonovo A., Censi R., Dolci M., Vavassori V., Bianchi A., Maiorana C. Use of endosseous one-piece yttrium-stabilized zirconia dental implants in premolar region: A two-year clinical preliminary report. Minerva. Stomatol. 2011;60:229–241. [PubMed] [Google Scholar]
- 52.Borgonovo A., Vavassori V., Censi R., Calvo J., Re D. Behavior of endosseous one-piece yttrium stabilized zirconia dental implants placed in posterior areas. Minerva. Stomatol. 2013;62:247–257. [PubMed] [Google Scholar]
- 53.Bormann K.-H., Gellrich N.-C., Kniha H., Schild S., Weingart D., Gahlert M. A prospective clinical study to evaluate the performance of zirconium dioxide dental implants in single-tooth edentulous area: 3-year follow-up. BMC Oral Health. 2018;18:181. doi: 10.1186/s12903-018-0636-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cannizzaro G., Torchio C., Felice P., Leone M., Esposito M. Immediate occlusal versus non-occlusal loading of single zirconia implants. A multicentre pragmatic randomised clinical trial. Eur. J. Oral Implant. 2010;3:111–120. [PubMed] [Google Scholar]
- 55.Cionca N., Müller N., Mombelli A. Two-piece zirconia implants supporting all-ceramic crowns: A prospective clinical study. Clin. Oral Implant. Res. 2015;26:413–418. doi: 10.1111/clr.12370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jung R.E., Grohmann P., Sailer I., Steinhart Y.-N., Fehér A., Hämmerle C., Strub J.R., Kohal R. Evaluation of a one-piece ceramic implant used for single-tooth replacement and three-unit fixed partial dentures: A prospective cohort clinical trial. Clin. Oral Implant. Res. 2015;27:751–761. doi: 10.1111/clr.12670. [DOI] [PubMed] [Google Scholar]
- 57.Kniha K., Kniha H., Möhlhenrich S.C., Milz S., Hölzle F., Modabber A. Papilla and alveolar crest levels in immediate versus delayed single-tooth zirconia implants. Int. J. Oral Maxillofac. Surg. 2017;46:1039–1044. doi: 10.1016/j.ijom.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 58.Kniha K., Schlegel K.A., Kniha H., Modabber A., Hölzle F., Kniha K. Evaluation of peri-implant bone levels and soft tissue dimensions around zirconia implants—A three-year follow-up study. Int. J. Oral Maxillofac. Surg. 2017;47:492–498. doi: 10.1016/j.ijom.2017.10.013. [DOI] [PubMed] [Google Scholar]
- 59.Kohal R.-J., Patzelt S.B.M., Butz F., Sahlin H. One-piece zirconia oral implants: One-year results from a prospective case series. 2. Three-unit fixed dental prosthesis (FDP) reconstruction. J. Clin. Periodontol. 2013;40:553–562. doi: 10.1111/jcpe.12093. [DOI] [PubMed] [Google Scholar]
- 60.Kohal R.-J., Spies B.C., Bauer A., Butz F. One-piece zirconia oral implants for single-tooth replacement: Three-year results from a long-term prospective cohort study. J. Clin. Periodontol. 2018;45:114–124. doi: 10.1111/jcpe.12815. [DOI] [PubMed] [Google Scholar]
- 61.Koller M., Steyer E., Theisen K., Stagnell S., Jakse N., Payer M. Two-piece zirconia versus titanium implants after 80 months: Clinical outcomes from a prospective randomized pilot trial. Clin. Oral Implant. Res. 2020;31:388–396. doi: 10.1111/clr.13576. [DOI] [PubMed] [Google Scholar]
- 62.Lorenz J., Giulini N., Hölscher W., Schwiertz A., Schwarz F., Sader R. Prospective controlled clinical study investigating long-term clinical parameters, patient satisfaction, and microbial contamination of zirconia implants. Clin. Implant Dent. Relat. Res. 2019;21:263–271. doi: 10.1111/cid.12720. [DOI] [PubMed] [Google Scholar]
- 63.Osman R.B., Payne A., Duncan W., Ma S. Zirconia implants supporting overdentures: A pilot study with novel prosthodontic designs. Int. J. Prosthodont. 2013;26:277–281. doi: 10.11607/ijp.2903. [DOI] [PubMed] [Google Scholar]
- 64.Osman R.B., Swain M.V., Atieh M., Ma S., Duncan W. Ceramic implants (Y-TZP): Are they a viable alternative to titanium implants for the support of overdentures? A randomized clinical trial. Clin. Oral Implant. Res. 2014;25:1366–1377. doi: 10.1111/clr.12272. [DOI] [PubMed] [Google Scholar]
- 65.Patankar A., Kshirsagar R., Patankar S., Pawar S. Immediate, non submerged root analog zirconia implant in single rooted tooth replacement: Case report with 2 years follow up. J. Maxillofac. Oral Surg. 2016;15:270–273. doi: 10.1007/s12663-015-0786-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Payer M., Arnetzl V., Kirmeier R., Koller M., Arnetzl G., Jakse N. Immediate provisional restoration of single-piece zirconia implants: A prospective case series-results after 24 months of clinical function. Clin. Oral Implant. Res. 2012;24:569–575. doi: 10.1111/j.1600-0501.2012.02425.x. [DOI] [PubMed] [Google Scholar]
- 67.Payer M., Heschl A., Koller M., Arnetzl G., Lorenzoni M., Jakse N. All-ceramic restoration of zirconia two-piece implants—A randomized controlled clinical trial. Clin. Oral Implant. Res. 2015;26:371–376. doi: 10.1111/clr.12342. [DOI] [PubMed] [Google Scholar]
- 68.Pirker W., Kocher A. Immediate, non-submerged, root-analogue zirconia implant in single tooth replacement. Int. J. Oral Maxillofac. Surg. 2008;37:293–295. doi: 10.1016/j.ijom.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 69.Pirker W., Kocher A. Immediate, non-submerged, root-analogue zirconia implants placed into single-rooted extraction sockets: 2-year follow-up of a clinical study. Int. J. Oral Maxillofac. Surg. 2009;38:1127–1132. doi: 10.1016/j.ijom.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 70.Siddiqi A., Kieser J.A., De Silva R.K., Thomson W.M., Duncan W.J. Soft and Hard Tissue Response to Zirconia versus Titanium One-Piece Implants Placed in Alveolar and Palatal Sites: A Randomized Control Trial. Clin. Implant Dent. Relat. Res. 2015;17:483–496. doi: 10.1111/cid.12159. [DOI] [PubMed] [Google Scholar]
- 71.Spies B.C., Balmer M., Jung R.E., Sailer I., Vach K., Kohal R.-J. All-ceramic, bi-layered crowns supported by zirconia implants: Three-year results of a prospective multicenter study. J. Dent. 2017;67:58–65. doi: 10.1016/j.jdent.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 72.Spies B.C., Balmer M., Jung R.E., Sailer I., Vach K., Kohal R.J. All-ceramic single crowns supported by zirconia implants: 5-year results of a prospective multicenter study. Clin. Oral Implant. Res. 2019;30:466–475. doi: 10.1111/clr.13433. [DOI] [PubMed] [Google Scholar]
- 73.Spies B.C., Balmer M., Patzelt S.B.M., Vach K., Kohal R.J. Clinical and Patient-reported Outcomes of a Zirconia Oral Implant: Three year Results of a Prospective Cohort Investigation. J. Dent. Res. 2015;94:1385–1391. doi: 10.1177/0022034515598962. [DOI] [PubMed] [Google Scholar]
- 74.Spies B.C., Sperlich M., Fleiner J., Stampf S., Kohal R.-J. Alumina reinforced zirconia implants: 1-year results from a prospective cohort investigation. Clin. Oral Implant. Res. 2016;27:481–490. doi: 10.1111/clr.12560. [DOI] [PubMed] [Google Scholar]
- 75.Spies B.C., Witkowski S., Vach K., Kohal R.J. Clinical and patient-reported outcomes of zirconia-based implant fixed dental prostheses: Results of a prospective case series 5 years after implant placement. Clin. Oral Implant. Res. 2017;29:91–99. doi: 10.1111/clr.13072. [DOI] [PubMed] [Google Scholar]
- 76.Borgonovo A.-E., Fabbri A., Vavassori V., Censi R., Maiorana C. Multiple teeth replacement with endosseous one-piece yttrium-stabilized zirconia dental implants. Med. Oral Patol. Oral Cir. Bucal. 2012;17:e981–e987. doi: 10.4317/medoral.18194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Greenhalgh T. How to read a paper: Getting your bearings (deciding what the paper is about) BMJ. 1997;315:243–246. doi: 10.1136/bmj.315.7102.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Guyatt G.H., Sackett D.L., Sinclair J.C., Hayward R., Cook D.J., Cook R.J., Bass E., Gerstein H., Haynes B., Holbrook A. Users’ guides to the medical literature: IX. A method for grading health care recommendations. JAMA. 1995;274:1800–1804. doi: 10.1001/jama.1995.03530220066035. [DOI] [PubMed] [Google Scholar]
- 79.Scarano A., Crocetta E., Quaranta A., Lorusso F. Influence of the thermal treatment to address a better osseointegration of Ti6Al4V dental implants: Histological and histomorphometrical study in a rabbit model. BioMed Res. Int. 2018 doi: 10.1155/2018/2349698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Scarano A., Degidi M., Perrotti V., Degidi D., Piattelli A., Iezzi G. Experimental Evaluation in Rabbits of the Effects of Thread Concavities in Bone Formation with Different Titanium Implant Surfaces. Clin. Implant Dent. Relat. Res. 2013;16:572–581. doi: 10.1111/cid.12033. [DOI] [PubMed] [Google Scholar]
- 81.Van Eck N.J., Waltman L. Accuracy of citation data in Web of Science and Scopus. arXiv. 20191906.07011 [Google Scholar]
- 82.Feijoo J.F., Limeres J., Fernández-Varela M., Ramos I., Diz P. The 100 most cited articles in dentistry. Clin. Oral Investig. 2014;18:699–706. doi: 10.1007/s00784-013-1017-0. [DOI] [PubMed] [Google Scholar]
- 83.Ugolini D., Neri M., Cesario A., Bonassi S., Milazzo D., Bennati L., Lapenna L.M., Pasqualetti P. Scientific production in cancer rehabilitation grows higher: A bibliometric analysis. Supportive Care Cancer. 2012;20:1629–1638. doi: 10.1007/s00520-011-1253-2. [DOI] [PubMed] [Google Scholar]
- 84.Davis P.M. Open access, readership, citations: A randomized controlled trial of scientific journal publishing. FASEB J. 2011;25:2129–2134. doi: 10.1096/fj.11-183988. [DOI] [PubMed] [Google Scholar]
- 85.Gargouri Y., Hajjem C., Larivière V., Gingras Y., Carr L., Brody T., Harnad S. Self-selected or mandated, open access increases citation impact for higher quality research. PLoS ONE. 2010;5:e13636. doi: 10.1371/journal.pone.0013636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hua F., Shen C., Walsh T., Glenny A.-M., Worthington H. Open Access: Concepts, findings, and recommendations for stakeholders in dentistry. J. Dent. 2017;64:13–22. doi: 10.1016/j.jdent.2017.06.012. [DOI] [PubMed] [Google Scholar]