EUS-guided radiofrequency ablation (RFA) is an endoscopic procedure and emerging therapeutic option for the treatment of pancreatic tumors.1, 2, 3 It has been described in recent years for local therapy of pancreatic adenocarcinoma and neuroendocrine tumors in patients for whom operative management is deemed unsuitable.1,4,5 Hyperthermic ablation using radiofrequency waves at 500 kHz is used to induce irreversible cellular injury and necrosis of the target lesion.6,7 Precise delivery of thermal energy is critical to spare the normal surrounding pancreatic tissue from injury. There is a modest but growing body of literature regarding the use of this technique in pancreatic neuroendocrine tumors,3,7,8 and our case demonstrates the feasibility of achieving immediate and durable response.
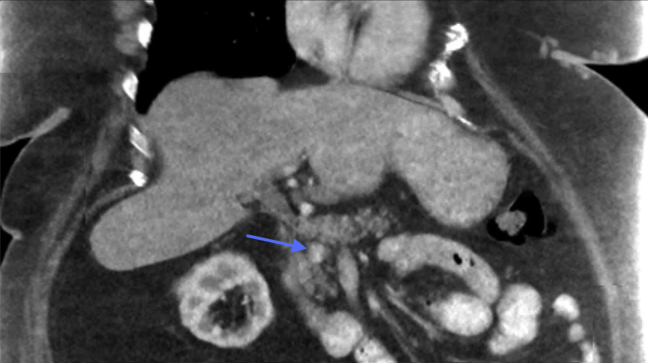
A 66-year-old woman with morbid obesity and type 2 diabetes was referred for management of a pancreatic insulinoma after multiple episodes of hypoglycemia. Biochemical markers were diagnostic of an insulinoma, with a fasting C-peptide level of 4 (reference: 0.8-3.5) and serum insulin of 27 mIU/L (reference: <25 mIU/L) in the setting of a fasting glucose level of 44 mg/dL (reference: 65-95 mg/dL). CT imaging revealed an early arterial phase-enhancing lesion measuring 1.8 × 0.9 × 1.3 cm in the pancreatic head (Fig. 1). After a multidisciplinary discussion, the patient was deemed a high-risk surgical candidate because of her comorbidities, and it was therefore decided to offer EUS-guided RFA of the tumor.
Figure 1.
CT image of arterial enhancing lesion in the pancreatic head.
The patient was admitted to the hospital for glucose monitoring before the procedure. Outpatient diazoxide, which was used to maintain her blood glucose, was discontinued before the procedure (T½ 24-36 hours). Informed consent was obtained, and the following day the patient underwent diagnostic and therapeutic EUS. From the duodenal bulb, a well-defined, hypoechoic, bilobed tumor was noted in the head of the pancreas. Fine-needle biopsy using a 22-gauge fine-needle biopsy needle was performed, and a visible core tissue was submitted for pathology review.
The needle was exchanged for the EUS-RFA electrode system (STARmed; Koyang, South Korea). We used a 19-gauge RFA needle with a 7-mm radiopaque exposed electrode tip attached to a radiofrequency generator with an internal cooling system. The RFA system has a 7F diameter; it requires a working channel of at least 2.4 mm and is compatible with a therapeutic linear echoendoscope. Under ultrasound guidance, the tumor was again punctured. Energy was applied at 20 W for 15 seconds. Special care was taken to ensure the hyperechoic treatment effect did not extend beyond the tumor margin. RFA applications were repeated until the entire tumor area showed hyperechoic bubbles suggestive of thermal injury (Figs. 2 and 3).
Figure 2.
Pretreatment EUS image of radiofrequency ablation needle inserted into tumor.
Figure 3.
Posttreatment EUS image showing compete tumor ablation.
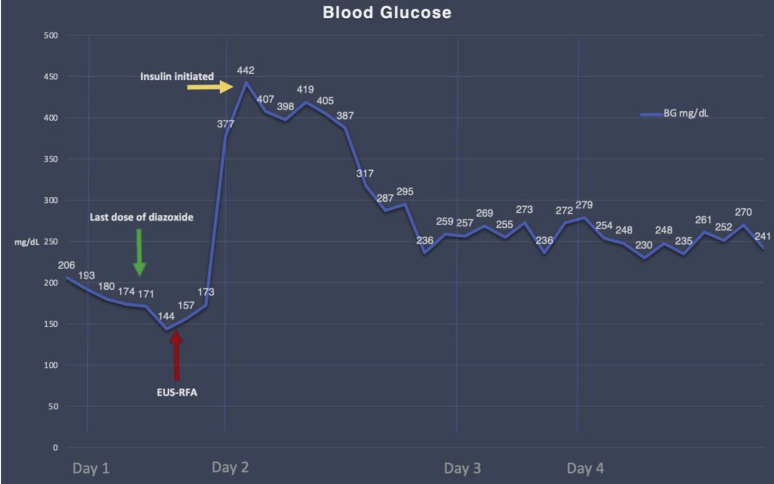
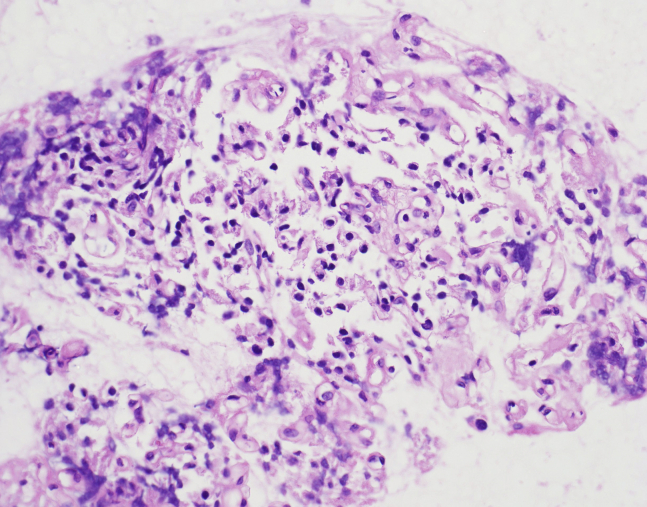
After the procedure, the patient was pain free and was observed for 72 hours. Within 12 hours of the ablation, there was a dramatic increase in random and fasting glucose values, which required initiation of insulin therapy (Fig. 4). Eight months after the procedure the patient remains well and without further symptoms; as a result, coordinating follow-up imaging has been a challenge. Pathology review confirmed a low-grade neuroendocrine tumor with a Ki-67 of less than 1% (Figs. 5 and 6).
Figure 4.
Blood glucose trends before and after radiofrequency ablation treatment.
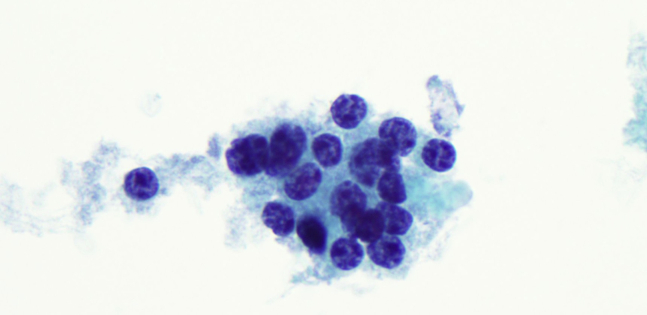
Figure 5.
Fine-needle biopsy cell block with loosely cohesive clusters of small cells with bland and uniform nuclei.
Figure 6.
Cells demonstrating round nuclei, with visibly course, stippled, and evenly distributed chromatin pattern and relatively scant cytoplasm. High magnification.
This case supports that EUS-guided RFA can be a safe and effective local therapy for functional pancreatic insulinoma.9,10 Video 1 (available online at www.VideoGIE.org) provides additional guidance for physicians who are pursuing this alternative treatment for patients for whom surgical management is not feasible. This also demonstrates the necessity of postprocedural blood glucose monitoring and anticipation of profound changes in blood glucose. Although very long-term efficacy studies of pancreatic neuroendocrine tumors are lacking, this is a promising endoscopic therapy.
Disclosure
Dr Brown received a training grant sponsored by Boston Scientific. Dr Gonda is a consultant for Cook Medical and Interpace Diagnostics and received grant support from Boston Scientific. All other authors disclosed no financial relationships.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Brown at nb2931@cumc.columbia.edu.
Supplementary data
Immediate and durable therapeutic response after EUS-guided radiofrequency ablation of a symptomatic pancreatic insulinoma.
References
- 1.Kim H.J., Seo D.W., Hassanuddin A. EUS-guided radiofrequency ablation of the porcine pancreas. Gastrointest Endosc. 2012;76:1039–1043. doi: 10.1016/j.gie.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Armellini E., Crinò S., Ballare M. Endoscopic ultrasound-guided radiofrequency ablation of a pancreatic neuroendocrine tumor. Endoscopy. 2015;47:E600–E601. doi: 10.1055/s-0034-1393677. [DOI] [PubMed] [Google Scholar]
- 3.Ligresti D., Amata M., Luca B. EUS-guided radiofrequency ablation of small pancreatic adenocarcinoma: a new therapeutic option for patients unfit for surgery. Gastrointest Endosc. 2019;4:29–31. doi: 10.1016/j.vgie.2018.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Signoretti M., Valente R., Repici A. Endoscopy-guided ablation of pancreatic lesions: technical possibilities and clinical outlook. World J Gastrointest Endosc. 2017;9:41–54. doi: 10.4253/wjge.v9.i2.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waung J.A., Todd J.F., Keane M.G. Successful management of a sporadic pancreatic insulinoma by endoscopic ultrasound-guided radiofrequency ablation. Endoscopy. 2016;48:E144–E145. doi: 10.1055/s-0042-104650. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed M., Brace C., Lee F. Principles of and advances in percutaneous ablation. Radiology. 2011;258:351–369. doi: 10.1148/radiol.10081634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ASGE Technology Committee. Navaneethan U., Thosani N. Radiofrequency ablation devices. VideoGIE. 2017;2:252–259. doi: 10.1016/j.vgie.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lakhtakia S., Ramchandani M., Galasso D. EUS-guided radiofrequency ablation for management of pancreatic insulinoma by using a novel needle electrode (with videos) Gastrointest Endosc. 2015;83:234–239. doi: 10.1016/j.gie.2015.08.085. [DOI] [PubMed] [Google Scholar]
- 9.Barthet M., Giovannini M., Lesavre N. Endoscopic ultrasound-guided radiofrequency ablation for pancreatic neuroendocrine tumors and pancreatic cystic neoplasms: a prospective multicenter study. Endoscopy. 2019;51:836–842. doi: 10.1055/a-0824-7067. [DOI] [PubMed] [Google Scholar]
- 10.Crinò S.F., D’Onofrio M., Bernardoni L. EUS-guided radiofrequency ablation (EUS-RFA) of solid pancreatic neoplasm using an 18-gauge needle electrode: feasibility, safety, and technical success. J Gastrointest Liver Dis. 2018;27:67–72. doi: 10.15403/jgld.2014.1121.271.eus. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Immediate and durable therapeutic response after EUS-guided radiofrequency ablation of a symptomatic pancreatic insulinoma.