Abstract
Background
We performed an updated systematic review and meta-analysis which enrolled 25 prospective randomized controlled trials (RCTs) to compare the outcomes between total hip arthroplasty (THA) and hemiarthroplasty (HA) in patients with femoral neck fractures (FNFs).
Methods
We searched English databases which included PubMed, Embase (vis OvidSP), The Cochrane Library, and Web of Science, and Chinese databases Chinese National Knowledge Infrastructure (CNKI), VIP, Wang Fang, and China Biology Medicine Disc (CBM) in July 2020. The quality of each study was assessed according to the Cochrane Collaboration’s Risk of Bias. Risk ratios (RRs) and weighted mean differences (WMDs) with 95% confidence intervals (95% CIs) were pooled with random-effects models. Data regarding baseline characteristics, hospital and surgery outcomes, clinical outcomes, patients’ quality of life, common complications, prothesis-related complications, mortality, and costs were reported.
Results
A total of 25 RCTs involving 3223 patients (1568 THA and 1655 HA) were included. THA had longer hospital length (WMD = 0.721, P < 0.0001) and surgery time (WMD = 20.044, P < 0.0001), and more blood loss compared with HA (WMD = 69.109, P < 0.0001). THA showed better ratings in the Harris Hip Score during follow-up periods between 1 and 5 years while no differences within 6 months and after 9 years. THA was associated with higher quality-of-life EuroQol-5 Dimension (EQ-5D) scores after 2 years of surgery but no difference within 1 year. There was no difference in common complications. THA had significant higher rate of dislocation (WMD = 1.897, P = 0.002) and lower acetabular erosion (WMD = 0.030, P = 0.001). For mortality, there was no difference during all the follow-up periods except for slightly higher 2-year mortality after surgery.
Conclusion
This meta-analysis demonstrates that THA has better medium-term functional results and quality of life and lower acetabular erosion rate, while HA shows better in reducing hospital stay, surgery time, and blood loss and also has lower dislocation rate.
Keywords: Total hip arthroplasty, Hemiarthroplasty, Femoral neck fractures, Randomized controlled trials
Background
Femoral neck fractures (FNFs) will bring baneful influences to patients due to its high morbidity, disability rate, economic burden, and mortality, and the rate is rapidly growing because of the increasing number of the elderly [23]. Arthroplasty is commonly recommended for displaced femoral neck fractures (67% of all types FNFs) in the elderly (age > 65 years) and can be categorized as total hip arthroplasty (THA) and hemiarthroplasty (HA) [34]. Whether THA or HA is more applicable in FNF remains controversial [21]. Both pros and cons of the treatments were widely reported in previous studies and synthesized reviews but did not reach a common conclusion [6, 11, 13, 15, 17, 24, 26, 33, 49–52]. The ongoing discussion requires highly reliable answers. However, previous meta-analysis and reviews have several limitations. First, they did not fully mention the details of surgical approach, prosthetic choice, surgeon experience, and the type of both femoral and acetabular fixation, all of which we consider may cause chaos in conclusion. Second, serious inclusion criteria in some studies may lead to limited data to analyze. Third, subgroup analysis was limited, and long-term results were not considered. The latest meta-analysis included trials reported between 2006 and 2017 and may be outdated [33]. Randomized controlled trials (RCTs) with high quality have been published recently and not been included, and we carefully selected Chinese articles reported with enough follow-up duration and reported outcomes in our analysis [3, 8, 18, 25, 27, 31, 38, 44].
We conducted an updated meta-analysis only including RCTs to provide the most reliable evidence.
Methods
The review followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (www.prisma-statement.org).
Searches and selection criteria
We searched English databases which included PubMed, Medline, Embase, The Cochrane Library, and Web of Science and Chinese databases CNKI, VIP, WAN FANG, and CBM (all inception to July 2020) without language or date restriction as well as retrieving articles identified in other reviews by manual search. And the search strategy is provided in Supplementary files. Inclusion criteria were RCTs comparing THA with HA for FNFs and at least reporting one of the predetermined outcomes. To make our conclusion generalizable, we set no restrictions for follow-up time, patients’ age, study size, or pre-surgery status.
Outcome measures
We included the following outcomes:
Hospital and surgery outcomes: hospital stays, surgery duration, blood loss;
Clinical outcomes: Harris Hip Scores (HHS) within 6 months and up to 13 years;
Patients’ quality of life: EQ-5D scores within 6 months and at 1 to 2 years;
Common complications: pulmonary embolism, deep vein thrombosis, pneumonia, urinary tract infection, pressure ulcer, wound disease, surgical-site infection, and cardiovascular disease.
Prothesis-related complications: revision, fracture, dislocation, loosening or subsidence, heterotopic ossification, and acetabular erosion;
Mortality: mortality in hospital, within 6 months, at 1 to 2 years and up to 13 years;
Cost;
Data extraction and study quality assessment
Two reviewers (T-XM, WD) independently screened the titles and abstracts for eligibility. We develop a data extraction form and collected data from including articles after full-text reading and cross-checking procedures. Any discrepancies were evaluated by a third reviewer(C-JL). For study quality assessment, the Cochrane Collaboration’s Risk of Bias was used. For missing data like standard deviation, we calculated them with formulas according to the Cochrane handbook for systematic reviews of interventions or articles’ figure data.
Statistical methods
For statistical analysis, the review used forest plots to present the synthesized results. For continuous and binary variables, the weighted mean differences (WMD) and risk ratios (RR) were reported respectively with 95% confident interval (CI). Survivorship was analyzed through the Kaplan–Meier survivor curve. Heterogeneity was assessed by both Q2 and I2 tests, and P value < 0.1 or I2 > 50% indicates statistical heterogeneity. Galbraith tests and sensitivity analysis were used to identify the possible heterogeneity origins. If necessary, subgroups will be used to dismiss heterogeneity. The random effects model was conducted in any condition. We used sensitivity analysis by sequential omission of individual studies to validate the credibility of pooled data. For publication bias, the symmetry of funnel plots was visually evaluated, and Egger’s tests were also applied. For statistical analyses, the Review Manager (Version 5.0.2) and STATA (Version 13.0) software programs. All P values were two-sided.
Results
Search results
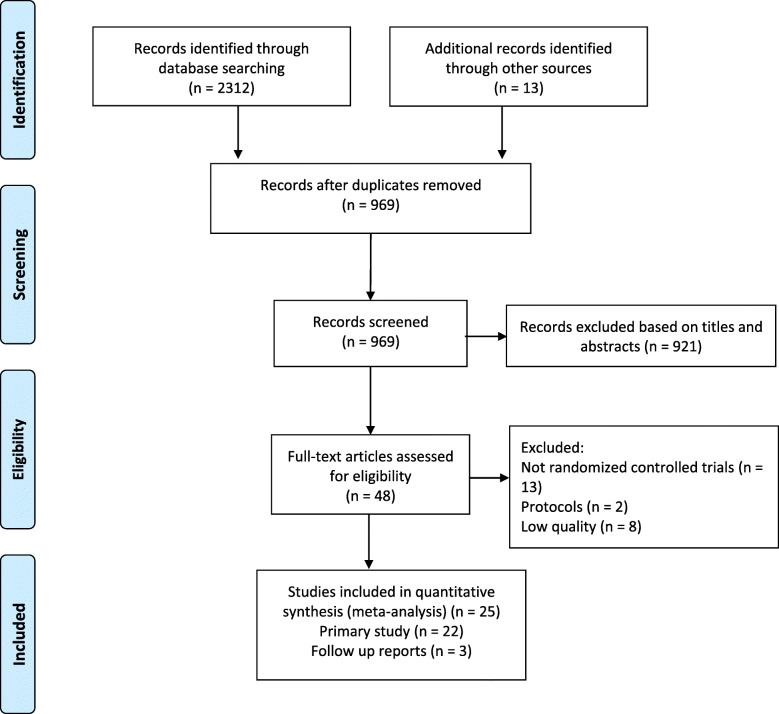
Our review yielded 2325 reports and excluded 1356 after duplicates. Of these literatures, 48 were included after selecting the title and abstracts. After full text screening, 23 were excluded, and the details were described in the flow chart (Fig. 1). For clinical outcomes, we included 25 reports based on 19 trials and extracted non-repeating data at different follow-up stages ([1–4, 7, 8, 10, 12, 16, 18, 22, 25]; H. H [27].; W [29].; William [30, 31, 36–38, 40, 42–44, 46, 47]).
Fig. 1.
PRISMA flowchart of the selection process
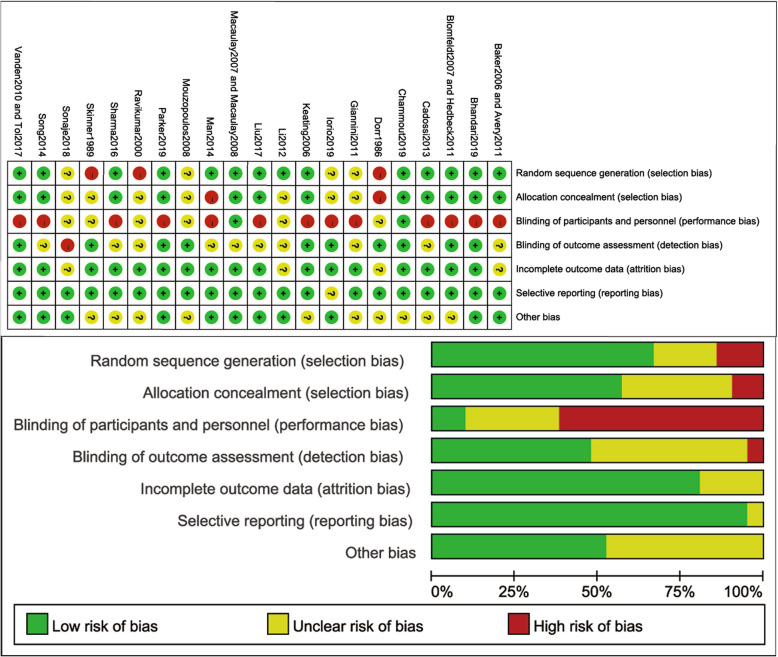
Methodological quality assessment
In this study, selection, attrition, and reporting bias can be considered low risk. Detection bias was moderate risk as well as performance bias. Therefore, the methodological assessment of this work can be judged as very good quality. Two reviewers independently assessed the risk of bias of included studies according to the Cochrane Collaboration’s Risk of Bias, and the results are shown in Fig. 2.
Fig. 2.
Risk of bias of included studies according to the Cochrane Collaboration’s Risk of Bias
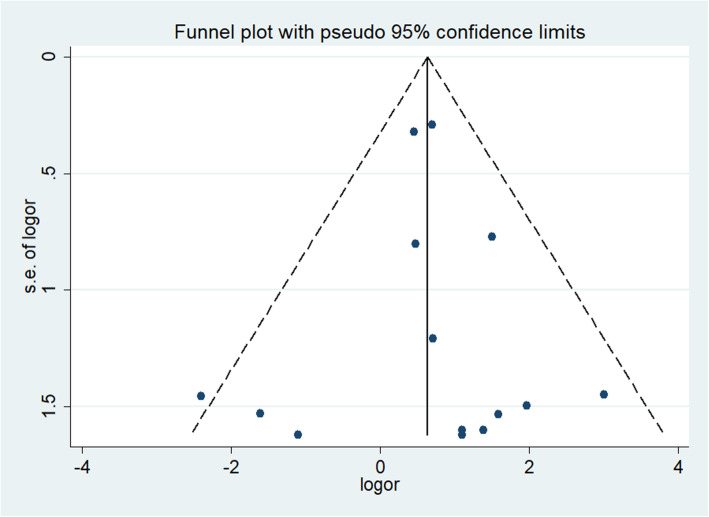
Risk of publication bias
Funnel plots of the outcome enrolled the most studies (dislocation) to detect publication bias. The symmetrical distribution and Egger’s test (P = 0.708) show low publication bias (Fig. 3).
Fig. 3.
Funnel plot based on dislocation rate
Study characteristics
We finally included 25 RCTs involving 3223 patients (THA 1568, HA 1655). Five of them ([1, 16]; W [29, 40].) were follow-up reports of previous trials. Table 1 summarizes the trials’ details.
Table 1.
Characteristics of the included studies
| Study | Country | Period | Surgical approach | Surgeon | Patients number | Age | Woman | ASA | Median time to surgery, h | Mobility | Mental status | THA | HA | Follow-up | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| THA | HA | THA mean (SD) | HA mean (SD) | THA n (%) | HA n (%) | THA | HA | THA | HA | ||||||||||
| Baker et al. [2] and Avery et al. [1] | England | N/A | Transgluteal lateral | Similar training levels | 40 | 41 | 74.2 (5.8) | 75.8 (5) | 32 (80%) | 32 (78%) | 2 (0.5) | 2 (0.5) | 42 | 46.8 | Walk > 0.8 km; live independently | MMSE9.83/9.98 | Zimmer; femoral: cemented; head 28 mm cobalt chrome; acetabular: Polyethylene cemented | Zimmer; cemented; unipolar | 3 years for Baker et al. [2]; 9 years for Avery et al. [1] |
| Bhandari et al. [3] | Multiple centers | 2009–2017 | Not standardize | 523 surgeons with expertise in THA/HA | 718 | 723 | 79.1 (8.3) | 78.6 (8.6) | 510 (71%) | 499 (69.1%) | 22/280/305/50 | 20/275/326/51 | 54.9(79) | 52.5(80.3) | 1072 (walk dependently)/369 (with assistance) | No dementia | Mixed | Mixed | 2 years |
| Blomfeldt et al. [4] and Hedbeck et al. [16] | Sweden | N/A | Anterolateral | 9 surgeons experienced in THA/HA | 60 | 60 | 80.5 (4.9) | 80.7 (4.8) | 47 (78%) | 54 (90%) | N/A | N/A | N/A | N/A | 111 no aids or one aid (92.5%) | SPMSQ > 9 | Johnson; femoral: cemented; head 28 mm exter modular stem; acetabular: OGEE, DePuy | Stryker cemented; bipolar | 12 months for Blomfeldt et al. [4]; 48 months for Hedbeck et al. [16] |
| Cadossi et al. [6] | Italy | 2008–2010 | Straight lateral | 2 experienced surgeons (SG, CF) | 42 | 41 | 82.3 (6.3) | 84.2 (6.3) | 34 (81%) | 28 (68%) | 2/15/16/9 | 1/10/22/8 | 2.9 (1.75) | 3.6 (1.5) | Independently walk | No senile dementia |
Unknown Femoral: uncemented; head: large metal; acetabular: 2.7-mm thick hydrophilic polycarbonate urethane (PCU) |
Mixed; bipolar | 30.1 months |
| Chammout et al. [8] | Sweden | 2009–2016 | Direct lateral | Consultant surgeon or registrar with assistance of consultant | 56 | 62 | 85 (4) | 86 (4) | 45 (75%) | 45 (75%) | ASA1/2:30; ASA3,4:30 | ASA1/2:20; ASA3,4:40 | < 36 h | < 36 h | No aids or one aid: THA30 (50%)/HA29 (48%) | SPMSQ:8-10 |
Schering-Plough Femoral: cemented; (vacuum-mixed low-viscosity cement with gentamicin);head 32-mm cobalt-chromium; acetabular: cemented highly cross-linked polyethylene |
Cemented; unipolar | 2 years |
| Dorr et al. [10] | America | 1980–1982 | Posterior | N/A | 39 | 50 | 69 (9) | 69 (12) | 23 (60%) | 35 (70%) | N/A | N/A | N/A | N/A | Ambulate | Mental status1/2: 70/19 |
Unknown Femoral: cemented; head: 28-mm; acetabular: unknown |
Mixed; bipolar | 2 years |
| Giannini et al. [12] | Italy | N/A | N/A | N/A | 30 | 30 | 80.7 (6) | 82.2 (6) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
Unknown Femoral: uncemented; head: large metal; acetabular: pliable, 3-mm-thick polycarbonate-urethane (PCU) |
Mixed; bipolar | 1 year |
| Iorio et al. [18] | Italy | 2015–2017 | Direct lateral | N/A | 30 | 30 | 82 (4) | 83 (3) | 18 (60%) | 17 (56.7%) | 0/3/23/4 | 0/4/21/5 | 59 (13) | 51 (15) | Walk unaided | MMSE < 18 |
Groupe Lépine Femoral: Uncemented; head: dual mobility cup Quattro; acetabular: N/A |
Uncemented; bipolar | 2 years |
| Keating et al. [22] | England | 1996–2000 | Decided by surgeon | Senior surgeon | 69 | 111 | 75.2 (6) | 75.4 (7) | 52 (75%) | 92 (83%) | N/A | N/A | < 48 h | < 48 h | Independent | MMSE > 6 |
Unknown Femoral: cemented; head: N/A; acetabular: N/A |
Cemented; bipolar | 2 years |
| Li et al. [25] | China | 2010–2012 | Anterolateral | N/A | 40 | 40 | 76.5 (6.5) | 75.8 (6.2) | 17 (42.5%) | 19 (47.5%) | N/A | N/A | N/A | N/A | N/A | Eliminate cognitive impairment |
Unknown Femoral: mixed; head: N/A; acetabular: N/A |
Mixed; N/A | 2 years |
| Liu et al. [27] | China | 2010–2012 | Posterior | N/A | 54 | 54 | 74.19(6.4) | 75.31 (6.2) | 24 (44.44%) | 26 (48.1%) | N/A | N/A | N/A | N/A | N/A | Excluded dementia patients | N/A | N/A | 1 year |
| Macaulay et al. [30] and Macaulay et al. [29] | America | N/A | Posterolateral and direct lateral (Modified Hardinge) | 14 surgeons, 5 reconstruction specialists | 17 | 23 | 82 (7) | 77 (9) | 7 (41%) | 14 (61%) | N/A | N/A | N/A | N/A | Independently walk | Excluded MMSE < 23 | Mixed | Mixed | 1 year for Macaulay et al. [30]; 2 years for Macaulay et al. [29] |
| Man et al. [31] | China | 2010–2012 | Moore approach | N/A | 37 | 37 | N/A | N/A | 28 (37.84%) | 28 (37.84%) | N/A | N/A | N/A | N/A | N/A | No cognitive impairment | Cemented; N/A | Mixed; bipolar | 3 years |
| Mouzopoulos et al. [36] | Greece | 1999–2002 | N/A | N/A | 37 | 34 | 73.07(4.9) | 74.24 (3.77) | 28 (75.68%) | 24 (70.59%) | 2.03 (1.97) | 2.21 (1.9) | 45.2 (7.3) | 45.8 (2.4) | Independently walk 37/34 | SPMSQ 7.9 (2.6)/7.5 (3.1) | N/A | N/A | 4 years |
| Parker et al. [28] | England | 2012–2018 | Anterolateral | See in a. | 52 | 53 | 77.1 (5.5) | 77.1 (7.25) | 40 (76.9%) | 45 (84.9%) | 2.2 | 2.0 | N/A | N/A | Mean mobility grade 1.6/1.4 (9 grades) | MMSE 8.7/8.9 | |||
| Skinner et al. [37] and Ravikumar et al. [40, 41] | England | 1984–1986 | Posterolateral | See in b. | 89 | 91 | 81.03 | 82.06 | N/A | N/A | N/A | N/A | Within 24 h | Within 24 h | N/A | Included patients with dementia |
Unknown Femoral: cemented (Howse II prosthesis); head 32 mm head; acetabular: semi-captive cup |
Bipolar; uncemented (Austin Moore) | 2 years for Skinner et al. [37]; 13 years for Ravikumar et al. [40, 41] |
| Sharma et al. [42] | India | 2010–2014 | Modified Gibson | Two senior arthroplasty surgeons | 40 | 40 | 78 (3.5) | 73 (1.25) | 26 (65%) | 29 (72.5%) | N/A | N/A | 72 h | 72 h | N/A | N/A | N/A | N/A | 1 year |
| Sonaje et al. [43] | India | 2011–2012 | N/A | N/A | 21 | 21 | 66.4 (3.5) | 65.3 (3) | 13 (65%) | 14 (70%) | N/A | N/A | N/A | N/A | N/A | No psychiatric and neurological disorder | N/A | N/A; bipolar | 2 years |
| Song et al. [44] | China | 2003–2012 | N/A | N/A | 31 | 31 | 64.5 (5.8) | 65.1 (5.9) | 12 (38.71%) | 10 (32.26%) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A; bipolar | 1 year |
| Van den et al. [47] and Tol et al. [46] | Netherlands | 1995–2002 | Anterolateral; straight lateral; posterolateral | Experienced surgeon or residents with assistant | 115 | 137 | 82.1 (6.3) | 80.3 (6.2) | 90 (78%) | 115 (84%) | 11/48/44/10 | 19/77/33/5 | 1(2.25) | 1(2.5) | Walk without aids:149 | N/A |
Sulzer AG/Protek AG Femoral: cemented (A Weber Rotations prosthesis, Müller Geradschaft prothesis); head 32 mm diameter modular head; acetabular: semi-captive cup |
Cemented; Bipolar; |
5 years for Van den2010 and 12 years for Tol2017 |
aAll but eight operations were directly undertaken or supervised by the lead trialist. Two hemiarthroplasties and two THR’s were undertaken by orthopedic consultants and three hemiarthroplasties and one THR by trainee or staff grade surgeons
bMostly by registers, occasionally by consultants or senior house officers
cSPMSQ Short Portable Mental Status Questionnaire
Outcome of interests
The overall results are presented in Table 2.
Table 2.
The results of meta-analysis
| Variables | N (study) | N (THA) | N (HA) | Pooled data | Heterogeneity | ||
|---|---|---|---|---|---|---|---|
| WMD/RR(95%CI) | P | I2(%) | Ph | ||||
| Hospital and Surgery | |||||||
| Hospital length | 9 | 418 | 443 | 2.360 (0.215, 4.506) | 0.031 | 96.0% | < 0.0001 |
| Hospital length (deleted Li et al. [25], Liu et al. [27]) | 7 | 324 | 349 | 0.721 (0.362, 1.080) | < 0.0001 | 0% | 0.428 |
| Surgery time | 15 | 1292 | 1341 | 20.044 (14.257, 25.830) | < 0.0001 | 95.7% | < 0.0001 |
| Blood loss | 9 | 1063 | 1038 | 69.106 (39.083, 99.129) | < 0.0001 | 96.4% | < 0.0001 |
| Blood loss (deleted developing countries’ studies) | 4 | 881 | 856 | 76.027 (51.951, 100.104) | < 0.0001 | 17.6% | 0.303 |
| Clinical outcomes | |||||||
| By follow-up | |||||||
| HHS(< 6 months) | 5 | 208 | 208 | 1.641 (− 0.449, 3.731) | 0.124 | 0% | 0.784 |
| HHS (at 1 year) | 6 | 317 | 333 | 3.593 (1.278, 5.907) | 0.002 | 12.5% | 0.335 |
| HHS (at 2 years) | 5 | 174 | 168 | 3.691 (0.571, 6.812) | 0.020 | 38.8% | 0.162 |
| HHS (3 to 5 years) | 5 | 233 | 251 | 6.027 (0.434, 11.621) | 0.035 | 90.1% | < 0.0001 |
| HHS (at 9 years) | 2 | 57 | 71 | 5.848 (− 4.603, 16.299) | 0.273 | 74.1% | 0.050 |
| Pain (HHS subscore) | 3 | 148 | 148 | 0.065 (− 0.385, 0.515) | 0.777 | 85.5% | < 0.0001 |
| Pain (HHS subscore, < 6 months) | 2 | 97 | 97 | − 0.042 (− 0.686, 0.602) | 0.897 | 79.5% | 0.027 |
| Pain (HHS subscore, at 1 year) | 3 | 128 | 128 | 0.405(− 0.575, 1.385) | 0.418 | 92.7% | 0.000 |
| Pain (HHS subscore, at 2 years) | 2 | 57 | 57 | − 0.020 (− 0.902, 0.862) | 0.964 | 78.6% | 0.031 |
| EQ-5D(<6 months) | 3 | 183 | 214 | 0.031 (− 0.031, 0.093) | 0.324 | 2.1% | 0.360 |
| EQ-5D(at 1 year) | 3 | 181 | 177 | 0.033 (− 0.036, 0.102) | 0.351 | 0.0% | 0.951 |
| EQ-5D(at 2 years) | 3 | 173 | 165 | 0.107 (0.049, 0.164) | < 0.0001 | 0.0% | 0.525 |
| Pain (binary) | 3 | 827 | 783 | 0.244 (0.050, 1.183) | 0.080 | 91.0% | < 0.0001 |
| Common complications | |||||||
| Pulmonary embolism | 4 | 187 | 235 | 0.597 (0.158, 2.257) | 0.447 | 0% | 0.517 |
| Deep vein thrombosis | 8 | 397 | 439 | 1.004 (0.386, 2.614) | 0.994 | 13.3% | 0.326 |
| Pneumonia | 7 | 308 | 315 | 0.932 (0.431, 2.014) | 0.858 | 0% | 0.733 |
| Pressure injury | 4 | 183 | 185 | 1.233 (0.301, 5.056) | 0.771 | 0% | 0.516 |
| Wound disease | 10 | 1170 | 1227 | 0.857 (0.488, 1.505) | 0.591 | 0% | 0.933 |
| Surgical site infection | 5 | 967 | 974 | 0.963 (0.422, 2.200) | 0.929 | 17.3% | 0.305 |
| Cardiovascular disease | 6 | 286 | 335 | 1.474 (0.672, 3.233) | 0.333 | 0% | 0.669 |
| Implant-related complications | |||||||
| Revision | 13 | 1397 | 1480 | 0.736 (0.419, 1.292) | 0.286 | 47.2% | 0.030 |
| Revision (Deleted Ravikumar et al. [40, 41]) | 12 | 1308 | 1389 | 0.882 (0.513, 1.517) | 0.651 | 30.3% | 0.150 |
| Fracture | 7 | 1065 | 1094 | 1.064 (0.707, 1.600) | 0.767 | 0% | 0.853 |
| Dislocation | 16 | 1473 | 1562 | 1.897 (1.273, 2.827) | 0.002 | 4% | 0.407 |
| Heterotopic Ossification | 3 | 853 | 880 | 1.272 (0.844, 1.918) | 0.251 | 0% | 0.647 |
| Loosening or Subsidence | 2 | 833 | 860 | 0.640 (0.170, 2.409) | 0.509 | 25.5% | 0.247 |
| Acetabular Erosion | 2 | 215 | 238 | 0.030 (0.004, 0.219) | 0.001 | 0% | 0.769 |
| Mortality | |||||||
| By follow-up | |||||||
| Mortality (in hospital) | 8 | 414 | 456 | 1.484 (0.616, 3.579) | 0.379 | 0% | 0.434 |
| Mortality (< 6 months) | 2 | 69 | 76 | 0.679 (0.094, 4.892) | 0.767 | 37.5% | 0.206 |
| Mortality (at 1 year) | 7 | 372 | 394 | 1.011 (0.684, 1.493) | 0.958 | 0% | 0.705 |
| Mortality (at 2 years) | 8 | 1197 | 1294 | 1.224(1.055,1.421) | 0.008 | 12.3% | 0.334 |
| Mortality(3 to 5 years) | 2 | 249 | 270 | 1.138(0.869,1.490) | 0.346 | 12.8% | 0.284 |
| Mortality(9 to 13 years) | 3 | 435 | 473 | 1.021(0.881,1.183) | 0.786 | 0% | 0.489 |
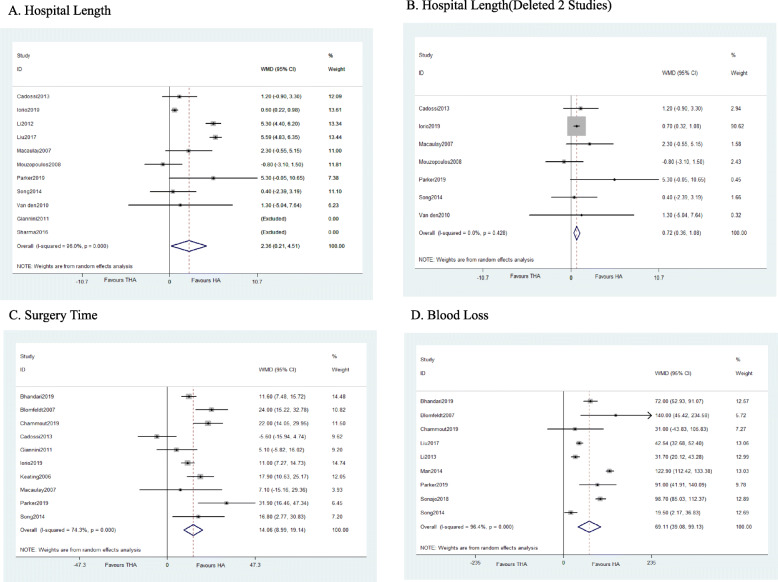
Hospital and surgery outcomes
Compared to HA, THA has longer surgery time (WMD = 20.044, P < 0.0001), more blood loss (WMD = 69.106, P < 0.0001), and longer hospital length (WMD = 2.360, P = 0.031). Fifteen studies reported surgery time (THA 1292, HA 1341) while nine studies reported hospital length (THA 418, HA 443) with high heterogeneity (I2 = 96%). We further did the Galbraith test and found the main source of the heterogeneity ([25]; H. H [27].). We excluded them, and the results are stable with no heterogeneity (I2 = 0%). For blood loss, nine studies were included (THA 1063, HA 1038), and the results are stable after removing developing countries’ studies (Fig. 4).
Fig. 4.
Forest plot of meta-analysis: Hospital and surgery outcomes
Clinical outcomes
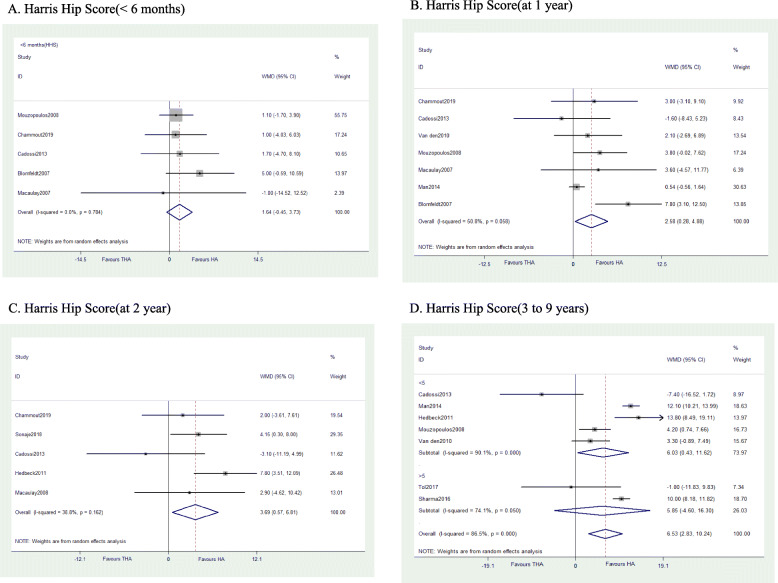
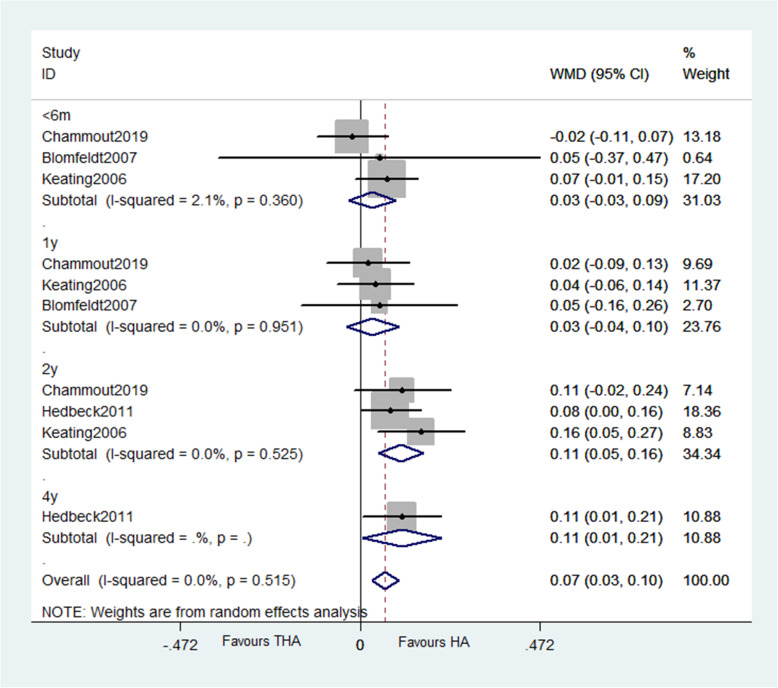
The results evidenced THA has similar HHS score with HA within 6 months (WMD = 1.641, P = 0.124) or after 9 years (WMD = 5.848, P = 0.273) but higher scores at 1 year (WMD = 3.593, P = 0.002), 2 years (WMD = 3.691, P = 0.020), and 3 to 5 years (WMD = 6.027, P = 0.035) (Fig. 5). Three studies reported pain score based on HHS subscore, and other three studies reported pain as binary variables; the results of both show no difference between groups at any follow-up points. For patients’ quality of life, pooled data revealed no significant difference of EQ-5D scores up to 1 year after surgery. But the results favor THA 2 years later (WMD = 0.107, P < 0.0001) (Fig. 6).
Fig. 5.
Forest plot of meta-analysis: Harris Hip Score
Fig. 6.
Forest plot of meta-analysis: EQ–5D
Patients’ quality of life
The results showed that EQ-5D scores within 6 months (WMD = 0.031, P = 0.324) and at the first year after surgery (WMD = 0.033, P = 0.351) are similar between groups while favor THA 2 years later (WMD = 0.107, < 0.0001).
Common complications
The pooling data elicited no statistical difference across groups in terms of the events of pulmonary embolism, deep vein thrombosis, pneumonia, pressure injury, wound disease, surgical-site infection, and cardiovascular disease.
Prothesis-related complications
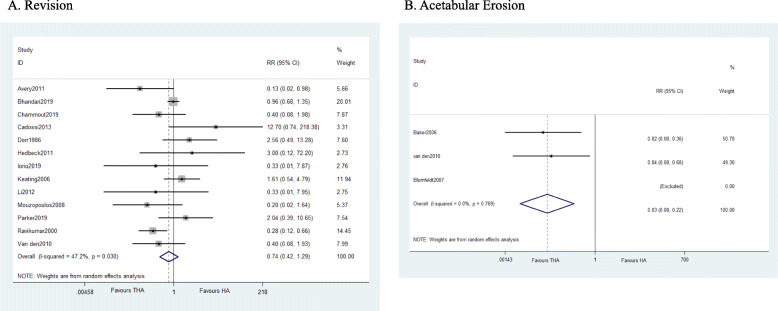
A total of 13 studies suggested that revision rate is similar in both groups with a moderate heterogeneity (I2 = 47.2%), the Galbraith test detected the main source, and the results are stable after deleting the study [40] (I2 = 30.3%). The study reported a result of 13 years follow-up thus generate the heterogeneity. Sixteen studies evidenced that THA has higher dislocations rate than HA with significant difference (WMD = 1.897, P = 0.002). Compared with THA, HA has a higher rate of acetabular erosion (WMD = 0.030, 95% CI 0.004 to 0.219, P = 0.001) (Fig. 7). As for fracture, loosening or subsidence, and heterotopic ossification, the results detected no statistical difference between groups.
Fig. 7.
Forest plot of meta-analysis: Prosthesis-related complications
Mortality
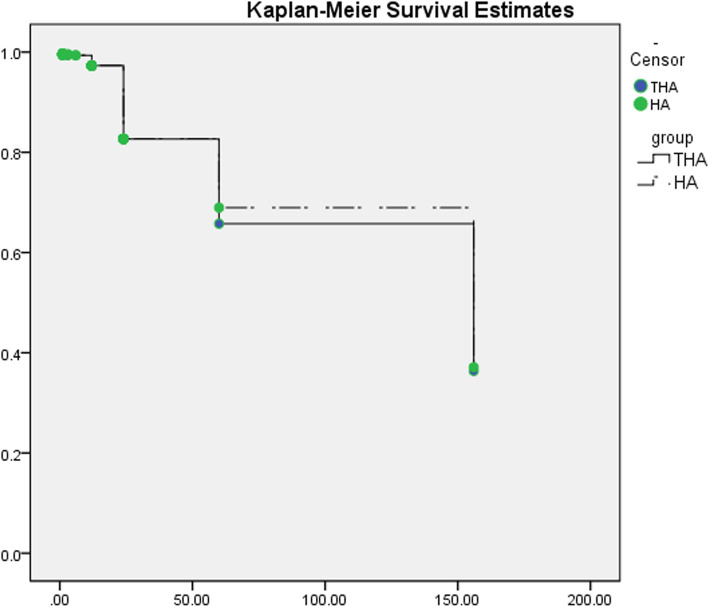
The Kaplan–Meier curve was applied, and we detected the similarity of survivorship (HR 1.029; 95% CI 0.905 to 1.169; P = 0.665; Fig. 8). Subgroup analysis of 2 years follow-up revealed reduced mortality in HA group (WMD = 1.224, P = 0.008)
Fig. 8.
Survival curve
Discussion
Hospital and surgery outcomes
For surgery time, almost all previous synthesized outcomes are in consistence with our results [24, 28, 33, 48, 49]. And we consider the main reasons are that HA requires less operative installation steps including cup preparation and implantation. For hospital length, we found that THA has longer in-hospital duration in our study. The common reasons for delayed discharges are usually post-surgery complications, since we did not find out the difference in common complications, and we consider that the early ambulation ability for patients who undergone HA may cause the difference. We also found reduced blood loss in HA group and less surgical procedures; tissue damage may clarify the results.
All three indicators are in favor of HA group, and the results are hardly to change even with more evidence. However, the results may lack clinical values when it comes to decision-making.
Clinical outcomes
Many studies have proved better outcomes in THA group in terms of HHS but did not provide long-term results or subgroup analysis due to limited trials ([24]; Y [28, 33, 49].). We made subgroups based on follow-up periods and initially found that THA group has higher total HHS in medium term (1–5 years) but no difference in short (< 6 months) or long terms (> 9 years).
For pain scores, we detect no difference between two groups, and the PCU-THA used in one trial is the main source of heterogeneity [6]. Liu (Y [28].) and Wang [20] found that patients in THA group experienced significantly less pain, but they only include limited trials in the pooled results.
Patients’ quality of life
For EQ-5D scores, our conclusion agreed with other studies that THA has better overall patients’ quality of life ([24]; Y [28, 48, 49].). We did the subgroup analysis and found that the difference became obvious 2 years after the surgery.
Common complications
Our result found no difference in terms of common complications, and we believed further studies can hardly change it. Our results are against Liu et al.’s study (Y [28].). In his study, he limited patients’ age to over 75 years old, and we believe the complications may largely be attributed to the patients’ own condition rather than implants type.
Prothesis-related complications
The results show that revision rate is similar with moderate heterogeneity (I2 = 47%). After sensitivity analysis, Ravikumar and Marsh’s [41] study was considered as the source because they reported 13-year follow-up results (24% in HA; 6.75% in THA). In meta-analysis that only include RCTs, Metcalfe et al. [32], Liu et al. (Y [28].), and Migliorini et al. [33] are in favor of our results but Migliorini et al. found a higher revision rate in THA within 5 years while in HA after 5 years. Lewis et al. [24] found that THA was superior to HA, but the non-RCTs in his study may influence the evidence grades.
However, data from registries are in contrast to the results from randomized trials because RCTs always have certain selections of enrolled patients. According to national registry studies, dislocation, infection, and periprosthetic fracture are the main reasons for revision [35, 45]. Anterolateral approach, cemented stem, bipolar head, and 36-mm cups are useful methods to reduce revisions and should be considered by the surgeons for the best outcomes for patients [14, 32, 35, 45]. Dislocations are always a concern by clinical doctors because they are the main reason for revision. We found that THA has a higher rate of dislocation compared with HA. The types of head (bipolar vs. unipolar), cups (dual-mobility vs. single cup), age of patients, pre-injury ambulation status, and surgical approaches may cause influence on the dislocation rate. Our conclusion is in line with other reviews and registry reports ([19, 24]; Y [28, 33].; ). Acetabular erosion is a theoretical indication to perform a revision in a painful HA. The pooled data shows higher acetabular erosion rate in HA group. And we found no dissent from other authors. Osteoarthritis also represents an important pillar for the decision on therapy.
Usually, surgeons are conservative about THA due to the elevated risk of dislocation, with the associated risk of subsequent revisions and the death risk in the end. However, our results found that the revision rate is similar between two groups. The possible reason is that THA has higher dislocations rates while HA has higher acetabular erosion rates and thus equals the revision rate between the two groups. The long-term results favor the THA, and surgeons could choose propriate implants and approaches to reduce dislocation rates.
Mortality
We found that the mortality rate was similar in groups, and comparable results were found by other meta-analysis [24, 33, 48, 49]. However, we found that THA has a slightly higher mortality rate 2 years after surgery, and it proves the detective ability of our study. We hypothesize that the early revision caused by dislocations will lead to more deaths in THA group while will be offset by acetabular erosion later. But the result should be interpreted carefully with more studies.
Cost
Three studies mentioned the cost of both techniques. Burgers et al. [5] found that main cost were rehabilitation fares and nursing home care payments in the first year after surgery. Keating et al. [22] found that the cost between groups was not significant, but highlight the high costs of the readmissions in patients who underwent HA. Ravi et al. [39] found that THA reduced health care costs about the index admission 1 year after surgery, relative to HA. Dangelmajer et al. [9] found that patient’s age and medical care payer status were all associated with odds of receiving THA, and patients with private insurance had higher odds of receiving THA. Reducing costs after hip fracture surgery should focus on improving the duration and efficiency of the rehabilitation phase. The economic evidence showed that THA should be more considered because it can cut the cost of readmission and rehabilitation.
Limitations
There are some limitations also needed to be noticed. First, lack of information (implant types, operative approach, etc.), uncontrollability of confounders (medical resources, surgeon experience, etc.), and other factors might affect the credibility of the pooled data despite that we selected the most reliable types of trials. Secondly, we did not set strict inclusion criteria since they have already been considered in the process of RCTs, and the low heterogeneity of these results also proves it. Thirdly, despite that our results suggested the difference between short-term and long-term results in functional outcomes and patients’ quality of life, the long-term reports are still limited.
Therefore, the multicentered and large population-based designs of future research should be considered, and more long-term follow-up surveys should be focused and reported.
Conclusion
Based on the results, we thought HA could be recommended for patients who have cognitive impairment, comorbidities, reduced performance status, and low function demands. And THA should be recommended for patients who are active, healthy, with long life expectancy and young biological age, and have higher demands for functions and quality of life.
Supplementary Information
Additional file 1: Supplementary file 1. Search Strategy
Acknowledgements
Not applicable
Abbreviations
- RCTs
Randomized controlled trials
- THA
Total hip arthroplasty
- HA
Hemiarthroplasty
- FNFs
Femoral neck fractures
- CNKI
Chinese National Knowledge Infrastructure
- CBM
China Biology Medicine Disc
- RRs
Risk ratios
- WMDs
Weighted mean differences
- CIs
Confidence intervals
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- EQ-5D
EuroQol Five Dimensions Questionnaire
- HHS
Harris Hip Scores
Authors’ contributions
TXM conceived the methods of the study; performed the database search, the article selection, and data extraction processes; performed the statistical analysis; and drafted the manuscript. WD conceived the methods of the study; performed the database search, the article selection, and data extraction processes; and drafted the manuscript. CJL conceived the methods of the study, helped with the data extraction process, and drafted the manuscript. LY, LPF, NN, and ZZZ helped to draft the manuscript. All authors read and approved the manuscript.
Funding
Supported by the Sichuan Science and Technology Program (No.2019YJ0031)
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This meta-analysis and all the included studies meet all the ethical standards described in the declaration of Helsinki. No ethical committee approval was required for this study.
Consent for publication
Not applicable
Competing interests
The authors declared no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xiumei Tang, Email: tangxiumei1997@outlook.com.
Duan Wang, Email: 476825891@qq.com.
Ying Liu, Email: liusaisaio@163.com.
Jiali Chen, Email: cjl85614115@163.com.
Zongke Zhou, Email: zhouzongke@scu.edu.cn.
Peifang Li, Email: 18382076258@163.com.
Ning Ning, Email: ningning6405@163.com.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-020-02122-6.
References
- 1.Avery PP, Baker RP, Walton MJ, Rooker JC, Squires B, Gargan MF, Bannister GC. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. J Bone Joint Surg. 2011;93-B:1045–1048. doi: 10.1302/0301-620X.93B8. [DOI] [PubMed] [Google Scholar]
- 2.Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88(12):2583–2589. doi: 10.2106/jbjs.E.01373. [DOI] [PubMed] [Google Scholar]
- 3.Bhandari M, Einhorn TA, Guyatt G, Schemitsch EH, Zura RD, Sprague S, et al. Total hip arthroplasty or hemiarthroplasty for hip fracture. N Engl J Med. 2019;381(23):2199–2208. doi: 10.1056/NEJMoa1906190. [DOI] [PubMed] [Google Scholar]
- 4.Blomfeldt R, Törnkvist H, Eriksson K, Söderqvist A, Ponzer S, Tidermark J. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br. 2007;89(2):160–165. doi: 10.1302/0301-620x.89b2.18576. [DOI] [PubMed] [Google Scholar]
- 5.Burgers PT, Hoogendoorn M, Van Woensel EA, Poolman RW, Bhandari M, Patka P, Van Lieshout EM. Total medical costs of treating femoral neck fracture patients with hemi- or total hip arthroplasty: a cost analysis of a multicenter prospective study. Osteoporos Int. 2016;27(6):1999–2008. doi: 10.1007/s00198-016-3484-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burgers PT, Van Geene AR, Van den Bekerom MP, Van Lieshout EM, Blom B, Aleem IS, et al. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis and systematic review of randomized trials. Int Orthop. 2012;36(8):1549–1560. doi: 10.1007/s00264-012-1569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cadossi M, Chiarello E, Savarino L, Tedesco G, Baldini N, Faldini C, Giannini S. A comparison of hemiarthroplasty with a novel polycarbonate-urethane acetabular component for displaced intracapsular fractures of the femoral neck: a randomised controlled trial in elderly patients. Bone Joint J. 2013;95B(5):609–615. doi: 10.1302/0301-620x.95b5.31083. [DOI] [PubMed] [Google Scholar]
- 8.Chammout G, Kelly-Pettersson P, Hedbeck CJ, Stark A, Mukka S, Sköldenberg O. HOPE-Trial: hemiarthroplasty compared with total hip arthroplasty for displaced femoral neck fractures in octogenarians: a randomized controlled trial. JB JS Open Access. 2019;4(2):e0059. doi: 10.2106/jbjs.Oa.18.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dangelmajer S, Yang A, Githens M, Harris AHS, Bishop JA. Disparities in total hip arthroplasty versus hemiarthroplasty in the management of geriatric femoral neck fractures. Geriatr Orthop Surg Rehabil. 2017;8(3):155–160. doi: 10.1177/2151458517720991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dorr LD, Glousman R, Hoy AL, Vanis R, Chandler R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J Arthroplasty. 1986;1(1):21–28. doi: 10.1016/s0883-5403(86)80006-7. [DOI] [PubMed] [Google Scholar]
- 11.Gao H, Liu Z, Xing D, Gong M. Which is the best alternative for displaced femoral neck fractures in the elderly?: a meta-analysis. Clin Orthop Relat Res. 2012;470(6):1782–1791. doi: 10.1007/s11999-012-2250-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giannini S, Chiarello E, Cadossi M, Luciani D, Tedesco G. Prosthetic surgery in fragility osteopathy. Aging Clin Exp Res. 2011;23:40–42. [PubMed] [Google Scholar]
- 13.Goh SK, Samuel M, Su DH, Chan ES, Yeo SJ. Meta-analysis comparing total hip arthroplasty with hemiarthroplasty in the treatment of displaced neck of femur fracture. J Arthroplasty. 2009;24(3):400–406. doi: 10.1016/j.arth.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 14.Hansson S, Nemes S, Karrholm J, Rogmark C. Reduced risk of reoperation after treatment of femoral neck fractures with total hip arthroplasty. Acta Orthop. 2017;88(5):500–504. doi: 10.1080/17453674.2017.1348095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.He JH, Zhou CP, Zhou ZK, Shen B, Yang J, Kang PD, Pei FX. Meta-analysis comparing total hip arthroplasty with hemiarthroplasty in the treatment of displaced femoral neck fractures in patients over 70 years old. Chin J Traumatol. 2012;15(4):195–200. [PubMed] [Google Scholar]
- 16.Hedbeck CJ, Enocson A, Lapidus G, Blomfeldt R, Törnkvist H, Ponzer S, Tidermark J. Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Joint Surg Am. 2011;93(5):445–450. doi: 10.2106/jbjs.J.00474. [DOI] [PubMed] [Google Scholar]
- 17.Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. Bmj. 2010;340:c2332. doi: 10.1136/bmj.c2332. [DOI] [PubMed] [Google Scholar]
- 18.Iorio R, Iannotti F, Mazza D, Speranza A, Massafra C, Guzzini M, et al. Is dual cup mobility better than hemiarthroplasty in patients with dementia and femoral neck fracture? A randomized controlled trial. Sicot j. 2019;5:38. doi: 10.1051/sicotj/2019035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jameson SS, Lees D, James P, Johnson A, Nachtsheim C, McVie JL, et al. Cemented hemiarthroplasty or hip replacement for intracapsular neck of femur fracture? A comparison of 7732 matched patients using national data. Injury. 2013;44(12):1940–1944. doi: 10.1016/j.injury.2013.03.021. [DOI] [PubMed] [Google Scholar]
- 20.Johnson JP, Kleiner J, Goodman AD, Gil JA, Daniels AH, Hayda RA. Treatment of femoral neck fractures in patients 45-64 years of age. Injury. 2019;50(3):708–712. doi: 10.1016/j.injury.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 21.Kannan A, Kancherla R, McMahon S, Hawdon G, Soral A, Malhotra R. Arthroplasty options in femoral-neck fracture: answers from the national registries. Int Orthop. 2012;36(1):1–8. doi: 10.1007/s00264-011-1354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keating JF, Grant A, Masson N, Scott NW, Forbes JF, Scottish Orthopaedic Trials N. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty - treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88A(2):249–260. doi: 10.2106/jbjs.E.00215. [DOI] [PubMed] [Google Scholar]
- 23.Kim BS, Lim JY, Ha YC. Recent epidemiology of hip fractures in South Korea. Hip Pelvis. 2020;32(3):119–124. doi: 10.5371/hp.2020.32.3.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis, D. P., Wæver, D., Thorninger, R., & Donnelly, W. J. (2019). Hemiarthroplasty vs total hip arthroplasty for the management of displaced neck of femur fractures: a systematic review and meta-analysis. J Arthroplasty, 34(8), 1837-1843.e1832. doi:10.1016/j.arth.2019.03.070. [DOI] [PubMed]
- 25.Li K, Song B. Comparison Clin effect Between Artificial femoral head replacement and total hip arhtroplasty on the fracture of neck of femur of elderly. J Clin Med Pract. 2013;17(03):45–48. [Google Scholar]
- 26.Liao L, Zhao J, Su W, Ding X, Chen L, Luo S. A meta-analysis of total hip arthroplasty and hemiarthroplasty outcomes for displaced femoral neck fractures. Arch Orthop Trauma Surg. 2012;132(7):1021–1029. doi: 10.1007/s00402-012-1485-8. [DOI] [PubMed] [Google Scholar]
- 27.Liu HH, Guan YJ, Wang QX, Liang XL. A comparision of the efficacy and quality of life between hemiarthroplasty and total hip replacement in the treatment of femoral neck fracture in the elderly. Chin J Gerontol. 2017;37(06):1457–1458. [Google Scholar]
- 28.Liu Y, Chen X, Zhang P, Jiang B. Comparing total hip arthroplasty and hemiarthroplasty for the treatment of displaced femoral neck fracture in the active elderly over 75 years old: a systematic review and meta-analysis of randomized control trials. J Orthop Surg Res. 2020;15(1):215. doi: 10.1186/s13018-020-01725-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Macaulay W, Nellans KW, Garvin KL, Iorio R, Healy WL, Rosenwasser MP, other members of the, D. C Prospective randomized clinical trial comparing hemiarthroplasty to total hip arthroplasty in the treatment of displaced femoral neck fractures: winner of the Dorr Award. J Arthroplasty. 2008;23(6 Suppl 1):2–8. doi: 10.1016/j.arth.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 30.Macaulay W, Nellans KW, Iorio R, Garvin KL, Healy WL, Rosenwasser MP. Total hip arthroplasty is less painful at 12 months compared with hemiarthroplasty in treatment of displaced femoral neck fracture. HSS J. 2007;4(1):48–54. doi: 10.1007/s11420-007-9061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Man D. Effect comparison between total hip replacement and bipolar femoral head replacement in treatment of elderly patients with femoral neck fracture. J Clin Med Pract. 2014;18(7):41–43. doi: 10.7619/jcmp.201407012. [DOI] [Google Scholar]
- 32.Metcalfe D, Judge A, Perry DC, Gabbe B, Zogg CK, Costa ML. Total hip arthroplasty versus hemiarthroplasty for independently mobile older adults with intracapsular hip fractures. BMC Musculoskelet Disord. 2019;20(1):226. doi: 10.1186/s12891-019-2590-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Migliorini F, Trivellas A, Driessen A, Quack V, El Mansy Y, Schenker H, et al. Hemiarthroplasty versus total arthroplasty for displaced femoral neck fractures in the elderly: meta-analysis of randomized clinical trials. Arch Orthop Trauma Surg. 2020. 10.1007/s00402-020-03409-3. [DOI] [PubMed]
- 34.Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthop Surg. 2008;16(10):596–607. doi: 10.5435/00124635-200810000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Moerman S, Mathijssen NMC, Tuinebreijer WE, Vochteloo AJH, Nelissen R. Hemiarthroplasty and total hip arthroplasty in 30,830 patients with hip fractures: data from the Dutch Arthroplasty Register on revision and risk factors for revision. Acta Orthop. 2018;89(5):509–514. doi: 10.1080/17453674.2018.1499069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mouzopoulos G, Stamatakos M, Arabatzi H, Vasiliadis G, Batanis G, Tsembeli A, et al. The four-year functional result after a displaced subcapital hip fracture treated with three different surgical options. Int Orthop. 2008;32(3):367–373. doi: 10.1007/s00264-007-0321-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Skinner P, Ellery DRJ, Beaumont A, Coumine R, Shafighian B. Displaced subcapital fractures of the femur: a prospective randomized comparison of internal fixation, hemiarthroplasty and total hip replacement. Injury. 1989;20(5):291–293. doi: 10.1016/0020-1383(89)90171-X. [DOI] [PubMed] [Google Scholar]
- 38.Parker MJ, Cawley S. Treatment of the displaced intracapsular fracture for the ‘fitter’ elderly patients: a randomised trial of total hip arthroplasty versus hemiarthroplasty for 105 patients. Injury. 2019;50(11):2009–2013. doi: 10.1016/j.injury.2019.09.018. [DOI] [PubMed] [Google Scholar]
- 39.Ravi B, Pincus D, Khan H, Wasserstein D, Jenkinson R, Kreder HJ. Comparing complications and costs of total hip arthroplasty and hemiarthroplasty for femoral neck fractures: a propensity score-matched, population-based study. J Bone Joint Surg Am. 2019;101(7):572–579. doi: 10.2106/JBJS.18.00539. [DOI] [PubMed] [Google Scholar]
- 40.Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur--13 year results of a prospective randomised study. Injury. 2000;31(10):793–797. doi: 10.1016/s0020-1383(00)00125-x. [DOI] [PubMed] [Google Scholar]
- 41.Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur--13 year results of a prospective randomised study. Injury. 2000;31(10):793–797. doi: 10.1016/S0020-1383(00)00125-X. [DOI] [PubMed] [Google Scholar]
- 42.Sharma V, Awasthi B, Kumar K, Kohli N, Katoch P. Outcome analysis of hemiarthroplasty vs. total hip replacement in displaced femoral neck fractures in the elderly. J Clin Diagn Res. 2016;10(5):RC11–RC13. doi: 10.7860/JCDR/2016/18638.7877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sonaje JC, Meena PK, Bansiwal RC, Bobade SS. Comparison of functional outcome of bipolar hip arthroplasty and total hip replacement in displaced femoral neck fractures in elderly in a developing country: a 2-year prospective study. Eur J Orthop Surg Traumatol. 2018;28(3):493–498. doi: 10.1007/s00590-017-2057-y. [DOI] [PubMed] [Google Scholar]
- 44.Song Q. Comparison of effect of total hip replacement and artificial head of femur replacement in patients with failed femoral neck fracture. Chin J Prim Med Pharm. 2014;21(12):1820–1822. [Google Scholar]
- 45.Stucinskas J, Grigaitis K, Smailys A, Robertsson O, Tarasevicius S. Bipolar hemiarthroplasty versus total hip arthroplasty in femoral neck fracture patients: results from Lithuanian Arthroplasty Register. Hip Int. 2020;1120700020907124. 10.1177/1120700020907124. [DOI] [PubMed]
- 46.Tol MC, van den Bekerom MP, Sierevelt IN, Hilverdink EF, Raaymakers EL, Goslings JC. Hemiarthroplasty or total hip arthroplasty for the treatment of a displaced intracapsular fracture in active elderly patients: 12-year follow-up of randomised trial. Bone Joint J. 2017;99-B(2):250–254. doi: 10.1302/0301-620X.99B2.BJJ-2016-0479.R1. [DOI] [PubMed] [Google Scholar]
- 47.van den Bekerom MPJ, Hilverdink EF, Sierevelt IN, Reuling EMBP, Schnater JM, Bonke H, et al. A comparison of hemiarthroplasty with total hip replacement for displaced intracapsular fracture of the femoral neck: a randomised controlled multicentre trial in patients aged 70 years and over. J Bone Joint Surg Bri. 2010;92B(10):1422–1428. doi: 10.1302/0301-620X.92B10.24899. [DOI] [PubMed] [Google Scholar]
- 48.Wang F, Zhang H, Zhang Z, Ma C, Feng X. Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis. BMC Musculoskelet Disord. 2015;16:229. doi: 10.1186/s12891-015-0696-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yoo JI, Cha YH, Kim JT, Park CH. Clinical outcomes of bipolar hemiarthroplasty versus total hip arthroplasty: assessing the potential impact of cement use and pre-injury activity levels in elderly patients with femoral neck fractures. Hip Pelvis. 2019;31(2):63–74. doi: 10.5371/hp.2019.31.2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yu L, Wang Y, Chen J. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures: meta-analysis of randomized trials. Clin Orthop Relat Res. 2012;470(8):2235–2243. doi: 10.1007/s11999-012-2293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhao Y, Fu D, Chen K, Li G, Cai Z, Shi Y, Yin X. Outcome of hemiarthroplasty and total hip replacement for active elderly patients with displaced femoral neck fractures: a meta-analysis of 8 randomized clinical trials. PLoS One. 2014;9(5):e98071. doi: 10.1371/journal.pone.0098071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zi-Sheng A, You-Shui G, Zhi-Zhen J, Ting Y, Chang-Qing Z. Hemiarthroplasty vs primary total hip arthroplasty for displaced fractures of the femoral neck in the elderly: a meta-analysis. J Arthroplasty. 2012;27(4):583–590. doi: 10.1016/j.arth.2011.07.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary file 1. Search Strategy
Data Availability Statement
The datasets used during the current study are available from the corresponding author on reasonable request.