Summary
The first COVID-19 patient in New York (NY) was reported on March 1, 2020. Since then NY has become one of the largest epicenters in the world where the disease has been overwhelming the healthcare system. Here I report how rapidly COVID-19 spread, and how the community responded during the first 30 days in NY. Gathering reliable information quickly was important in the evolving situation. Shortage of beds, personal protective equipment, ventilators, and staffing was observed. Reducing the number of infections and increasing the efficiency of medical resource allocation have been two major strategies taken in NY. It is important for Japan to accurately analyze the current situation, refer to answers in other parts of the world, and quickly establish strategy for clear goals that will lead to a "New Normal".
Keywords: COVID-19, New York, New Normal
Introduction
The global outbreak of novel coronavirus (SARS-CoV-2) was begun in Wuhan, China, in December 2019 (1). The first United States (U.S.) case was in Washington State (2), reported on January 20, 2020. The disease was named COVID-19 by World Health Organization on February 11 (3). In the U.S., the alertness was firstly raised on the West Coast. However, shortly thereafter, a rapid spread hit the East Coast hard, and New York City (NYC) has been one of the largest epicenters in the world where the disease has been overwhelming the healthcare system. As of April 15, total global deaths reached 137,193 and the deaths in New York State (NYS) counted 11,586, which is 43% of 26,708 U.S. deaths (4). Here I report how rapidly COVID-19 spread, and how the community responded during the first 30 days in New York (Figure 1). I also discuss which sources of information were useful, and what Japan should prepare.
Figure 1.
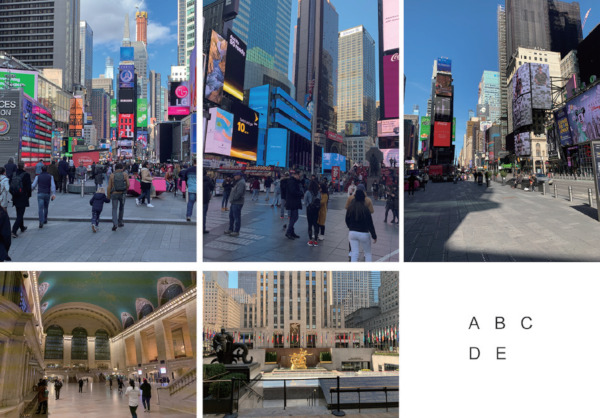
Pictures of Manhattan in the evolving situation. (A), Times Square, March 16, 2019; (B), Times Square, March 15, 2020; (C), Times Square, March 22, 2020; (D), Grand Central Terminal, March 17, 2020; (E), Rockefeller Plaza, March 22, 2020. Picture (A) was before COVID-19, pictures (B-E) were after COVID-19. All pictures were taken by the author.
March 2020 of New York
The first COVID-19 patient in NYS was reported on March 1, forty-one days after the disease reached the U.S.. This got widely known in the Japanese community in New York by an email from the Consulate General of Japan in New York issued at late night. That was the beginning. Three days later, on March 4, eleven people were reportedly test-positive and several schools related to the patients shut down. New Yorkers in the 5 Boroughs (Manhattan, Queens, Bronx, Brooklyn, and Staten Island, which constitute NYC) did not take the situation seriously because 10 out of 11 patients lived outside the City. At that time, NYC recommended i) staying home if feeling sick, ii) covering the sneezes and coughs with the sleeve, and iii) washing hands often, to prevent the spread of any virus. Mount Sinai Health System held the first town hall meeting on COVID-19 on March 4 in an auditorium of the hospital. This town hall was broadcasted via the web, but for those who could not leave their workplace, not for "social distancing". Other university hospitals in NYC banned domestic business travels of their employees.
NYS declared the State of Emergency on March 7 when test-positives tolled 11 (NYC) and 76 (NYS). Majorities of test-positives were the residents in Westchester County. New Rochelle, Westchester was designated as a containment area because there was the largest cluster of patients. The state authority seemed to try to track all contacts of patients at that time. On March 12, all Broadway theaters, Carnegie Hall, and Metropolitan Opera went dark with the State of Emergency of NYC. Museums including Metropolitan Museum closed, and all sports games after that day were canceled. This abruptly raised the alertness of people in the City. The numbers of cases were 96 (NYC) and 325 (NYS) on March 12, which were increased by more than 1.5-fold every day, and the number reached 269 (NYC) and 613 (NYS) on March 14. This rapid increase prompted me to start collecting COVID-19-related information. I supposed that Twitter (twitter.com) was the best tool because the spread should be exponential and very rapid in its nature and Twitter was a suitable channel for real-time information. Mayor of NYC Bill de Blasio tweeted on Sunday, March 15 - "We need to treat this like wartime - and we have a simple mission: protect the people most vulnerable and protect our health care system" (5). There were 329 (NYC) and 729 (NYS) patients, and the deaths were reported for the first time - 5 in NYS. NYS Governor Andrew Cuomo stated that there was an urgent need for more ICU beds. NYS urgently expanded the testing capacity of SARS-CoV-2 nucleic acid for COVID-19. The wartime began in NYS only after two weeks from the first case.
In the week of March 16, several key measures were announced in a flash. All public schools were shut down on Monday. Bars and eating-in at all restaurants were prohibited from Monday night, earlier than originally announced. Icahn School of Medicine at Mount Sinai announced that all non-essential researches should be ramping down by Friday. By the end of this week, Cuomo stated "potential staffing shortages (6)", and "critical need for Personal Protective Equipment (PPE) including gloves, gowns and masks - as well as ventilators (7)". The numbers of test-positives in NYC and NYS were 1,871 and 2,914 on March 18, and increased to 5,683 and 8,516 on Friday, March 20, respectively. On March 20 Cuomo announced the "New York State on PAUSE" executive order (Table 1) (8), a 10-point policy including "All non-essential businesses statewide will be closed by March 22", and "When in public individuals must practice social distancing of at least six feet from others", which has been considered as the beginning of so-called "lockdown" of NYS and NYC - currently ongoing.
Table 1. New York State on PAUSE (8) .
| The 10-point NYS on PAUSE plan is as follows: |
| 1 Effective at 8PM on Sunday, March 22, all non-essential businesses statewide will be closed; |
| 2 Non-essential gatherings of individuals of any size for any reason (e.g. parties, celebrations or other social events) are canceled or postponed at this time; |
| 3 Any concentration of individuals outside their home must be limited to workers providing essential services and social distancing should be practiced; |
| 4 When in public individuals must practice social distancing of at least six feet from others; |
| 5 Businesses and entities that provide other essential services must implement rules that help facilitate social distancing of at least six feet; |
| 6 Individuals should limit outdoor recreational activities to non-contact and avoid activities where they come in close contact with other people; |
| 7 Individuals should limit use of public transportation to when absolutely necessary and should limit potential exposure by spacing out at least six feet from other riders; |
| 8 Sick individuals should not leave their home unless to receive medical care and only after a telehealth visit to determine if leaving the home is in the best interest of their health; |
| 9 Young people should also practice social distancing and avoid contact with vulnerable populations; |
| 10 Use precautionary sanitizer practices such as using isopropyl alcohol wipes. |
The last 10 days of March saw a mix of number of rumors and official annoucements fly. On March 21, NYS announced the purchase of 1 million N95 masks for NYC, 500,000 for Long Island, and an additional 6,000 ventilators statewide, and at the same time, Twitter showed that some hospitals were running out of PPE/ventilators and healthcare providers were scared. In addition, on Monday, March 23, it was reported that one emergency department in NYC was experiencing 1-2 tracheal intubations per hour, and several sources reported that the ICU beds in NYC were almost full. For staffing shortages, along with the recruitment of retired healthcare providers, New York University and Department of Defense announced that they let their medical students graduate early to help the COVID-19 frontline. Key statistics of NYS were released on March 27. To prepare for the "apex" or the maximum load in about 21 days, 140,000 COVID-19 beds and 40,000 ICU beds were needed, but only 53,000 and 3,000 were available at the moment, while needed 20 million N95 masks and 30,000 ventilators, but only about 1.5 million and several thousand respectively. These statistics provided a straightforward road map to save and maintain the local healthcare system and eventually the lives of New Yorkers. With the clear numbers, people recognized the vital items and numbers under the shortage and were facilitated to unite each other to fight against the COVID-19 pandemic which was still going up the mountain to the apex. Clear goal setting by the leader with strong leadership was critical to the emergency situation.
What happened and what was done
In NYC, the situation progressed from the work-from-home order for non-essential workers to the shortage of ICU beds in a very short period of time, less than a week. During this time, four bad things progressed in NYC hospitals. The first was the shortage of PPE (N95 masks, surgical masks, medical gowns, etc.), which was supplemented by massive donations from various organizations and global companies. Extended use or even reprocessing of N95 masks was done under a policy of each hospital. Second, there has been a definite shortage of ventilators, which has been replenished by global sourcings and the establishment of new production lines. Ventilators for large animals were converted to human use. Some anesthetic machines were also utilized as ventilators. Even using one ventilator for two patients has been considered. Third, there has been a shortage of beds, mainly ICU beds. This has been supplied by both increasing the capacity and reducing the demand. The bed capacity was increased, by building eight temporary hospitals in the New York metropolitan area through a close collaboration between the NYS and the Federal Emergency Management Agency, by converting hotel rooms to beds, by constructing medical tents in such as Central Park, and by doubling the number of ICU beds of each hospital. Reducing the load to hospitals was achieved by ordering people with mild to moderate symptoms to stay home until they got severe. The fourth and last was the shortage of medical personnel. This was responded to by bringing in retired healthcare providers, recruiting healthcare providers from other States, expediting medical school graduations, and even sending research trainees and medical students to the field as auxiliary personnel. Even when a healthcare provider comes into close contact with COVID-19 patients, it has been often the policy to continue working as long as he or she is asymptomatic.
The NYS public health administration has responded to the COVID-19 outbreak in two major ways. Firstly, policies have taken place to reduce the spread of COVID-19, as summarized in "New York State on PAUSE (8)," intended to reduce interpersonal contacts, focusing on "social distancing." Secondly, policies to expand and replenish the health care system in response to the rapid growth in the number of patients. The policy covered facilities, beds, staffing, ventilators, PPE, COVID-19 testings, and new treatments. NYS announced that its Central Coordinating Team would manage those issues of the healthcare system of the state (9), seeking help from the federal government.
Living in an evolving situation
In an evolving situation, gathering reliable information quickly is important. At the same time as the press conference by Governor Cuomo, public information was tweeted from him, allowing us to quickly and accurately learn about upcoming policies and when they would come into effect. The press conferences were also sent out live on Twitter, allowing us to learn the number of patients, ICU admissions, tracheal intubation, deaths, and hospital discharges that day. It was emphasized by Cuomo that these statistics were important for health care policymaking in the evolving situations, and he gave a relatively logical explanation of how he reasoned from those statistics to make decisions. Moreover, Cuomo gave New Yorkers strong messages to encourage them in the difficult situation. I believe that this consistency has fostered an atmosphere of unity, where people cooperate with each other and appreciate the healthcare providers.
I personally gathered information to find out two things - i) the spread of COVID-19 and ii) whether the health care infrastructure was likely to collapse. For these purposes, I started to follow City of New York (@nycgov), Mayor Bill de Blasio (@NYCMayor) and Andrew Cuomo (@NYGovCuomo) because the statistics they published were also useful for my analysis of the ongoing situation. As they retweeted other useful public sources, I added those accounts to my asset. Tweets from non-medical people living in NYC area were also very helpful. They provided the atmosphere of every part of the city, and even provided the information, from a friend healthcare provider, that what was going on in the emergency department. Of course, this kind of hearsay is often inaccurate, so I checked the bio of the account and treated the information as a clue to be aware of similar observations. Importantly, at the very beginning of the surge, healthcare providers did not post much on Twitter or Facebook because they were under institutional social media policy and did not have time to post.
For the future of New York and Tokyo
The number of patients in Tokyo is still certainly on the rise, although it is difficult to predict whether Tokyo and other parts of Japan will experience medical resource depletion at a similar speed to what happened in NYC. The measures taken in NYC, such as reducing the number of infections and increasing the efficiency of medical resource allocation, are certainly necessary in Japan. Beds, PPE, ventilators, and staffing may be in short supply, thus there is a need for adequate preparation by government and administrative leadership. As of April 15, NYS appears to have reached the apex, and will someday enter a phase of cautious PAUSE mitigation. Governor Cuomo insisted that NYS on PAUSE would continue for another month or so, during which time he would work with neighboring states to i) control the spread of infection, ii) strengthen hospital functions, iii) establish a testing and tracking system, and iv) consider a "New Normal".
Fortunately, we have some answers on how to fight COVID-19 all over the world. Under strong leadership, it is important for Japan to accurately analyze the current situation, refer to those answers, and quickly establish strategy for clear goals that will lead to a "New Normal".
References
- 1. World Health Organization. Pneumonia of unknown cause - China. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ (accessed April 15, 2020).
- 2. Holshue ML, DeBolt C, Lindquist S, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020; 382:929-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. Novel Coronavirus (2019- nCoV) Situation Report - 22. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200211-sitrep-22-ncov.pdf?sfvrsn=fb6d49b1_2 (accessed April 15, 2020).
- 4. Johns Hopkins Coronavirus Resource Center. COVID-19 Case Tracker. https://coronavirus.jhu.edu/ (accessed April 15, 2020).
- 5. de Blasio B. Twitter, March 15, 2020. https://twitter.com/NYCMayor/status/1239331781041623040?s=20 (accessed April 15, 2020).
- 6. Cuomo A. Twitter, March 17, 2020. https://twitter.com/NYGovCuomo/status/1239999843508068352?s=20 (accessed April 15, 2020).
- 7. Cuomo A. Twitter, March 17, 2020. https://twitter.com/NYGovCuomo/status/1241106110658088962?s=20 (accessed April 15, 2020).
- 8. New York State. New York State on PAUSE. https://coronavirus.health.ny.gov/new-york-state-pause (accessd April 15, 2020) .
- 9. New York State. Amid Ongoing COVID-19 Pandemic, Governor Cuomo Announces New Hospital Network Central Coordinating Team. https://www.governor.ny.gov/news/amid-ongoing-covid-19-pandemic-governor-cuomo-announces-new-hospital-network-central (accessd April 15, 2020) .


