Summary
During the past 70 years, there has been a continued incremental worsening of antimicrobial resistance (AMR) by a combination of abusing antimicrobials in humans and animals as well as insufficient research and investment for new antimicrobial agents. The current trend of worsening AMR is likely to result in increased mortality and morbidity, longer stays in hospitals and accelerated health care costs. It is estimated that the global mortality attributed by AMR could reach 10 million per year by 2050, which is a massive increase from the current estimated mortality of 700, 000 per year. The year 2014 was the turning point of more than a half century of AMR history, transforming it from technical issue to a political agenda. Major progress includes adoption of the Global Action Plan on AMR at the WHO World Health Assembly in May 2015, followed by completion of a National Action Plan in most parts of the world, enactment of the Global Antimicrobial Surveillance System (GLASS) in October 2015, launch of the World Antibiotic Awareness Week in November 2015, and G20 Leaderscommitment to create the AMR Global Collaboration Hub in July 2017. Moreover, a comprehensive program against AMR has been implemented in some countries, such as UK, USA, and Germany. The strategic approach through coordination led by WHO with relevant international agencies and other entities was one of the key enabling factors for sustained political commitment on AMR.
Keywords: Antimicrobials, antibiotic resistance, drug resistance
Introduction
Antimicrobials are often regarded as one of the greatest inventions of human history. Since Dr. Alexander Fleming first discovered penicillin in 1928, it became one of the indispensable elements of modern medicine, not only treating infectious disease, but also for a wide range of medical interventions such as joint replacement, caesarian section and chemo-therapy for cancer. However, one of the first notable warnings of antimicrobial resistance (AMR) - formally referred as antibiotic resistance or drug resistance - was made in 1945 by Dr. Alexander Fleming, in his speech at the Nobel Lecture, he predicted that "The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non lethal quantities of the drug make them resistant" (1). During the past 70 years, there has been a continued incremental worsening of AMR by a combination of abusing antimicrobials in humans and animals as well as insufficient research and investment for new antimicrobial agents (2-4). It is worth noting that different from other political agendas such as health emergencies that had specific outbreaks to induce political attention, the disease burden of AMR worsens only in an incremental manner (5). By 2014, the threat of AMR became gradually obvious among the science and medical community due to increased prevalence of sporadic drug resistant infection outbreaks in health care settings even among high income countries, as well as worsening of drug resistance among three major infectious diseases - HIV/AIDS, tuberculosis and malaria - in low- and middle-income countries (6). Besides, although some of the infectious diseases are among the leading causes of disease burden in recent studies, such as lower respiratory infections, diarrheal diseases and neonatal encephalopathy, where a substantial portion of them are caused by AMR, AMR itself is not categorized as a disease in these studies and hence its direct burden is not measurable (7). The same is true for risk assessment. While some of the infection related risks, such as unsafe sex, unsafe water, insufficient handwashing, and unsafe sanitation are identified as a factor to be calculated, AMR is not included as a risk factor (8). AMR is invisible both in terms of disease burden analysis and risk analysis.
The global political strategies of AMR control
It was since 2014 when AMR got due attention from the political circle, which enables the agenda to make remarkable progress in terms of policy formulation, resource mobilization and effective implementation (9). This recent progress encompasses a wide variety of programs and initiatives, including adoption of the Global Action Plan on AMR at the WHO World Health Assembly in May 2015 (10), followed by completion of the National Action Plan in most parts of the world (11), enactment of the Global Antimicrobial Surveillance System (GLASS) in October 2015 (12), launch of the World Antibiotic Awareness Week in November 2015, and G20 Leaders' commitment to create the AMR Global Collaboration Hub in July 2017 (13). To catalyze and facilitate the required action with adequate financing and legal framework, the political process played a pivotal role (14).
In spite of its elusive nature, since 2014, AMR has emerged as one of the most prominent political agendas with the highest attention, discussed at G7 and G20 Summits as well as UN General Assembly High Level Meeting (13,15-17). This recent transformation of the agenda was phenomenal after more than half century of AMR history. While AMR has been technically discussed among science and health communities for more than half century with several problem-solving approaches proposed and tried, we could not deliver tangible results until recently.
AMR Global Action Plan
AMR Global Action Plan was adopted at the WHO World Health Assembly in 2015 and member states agreed to plan and finalize a national action plan in each country in the following 2 years (11).
This Global Action Plan contains five objectives (18): i) raising awareness; ii) surveillance; iii) reduce the incidence of infections; iv) optimal use of and access to medicine; and v) research & development of new antimicrobials and diagnostics.
While objective iii (reduce the incidence of infections) is not AMR specific because it would be achieved through immunization and infection prevention and control (IPC) programs, the other four objectives are AMR specific. It is notable that the planning of National Action Plans and programs for these four AMR specific goals has been implemented in the succeeding periods from 2015 to 2017 as shown in Figure 1.
Figure 1.
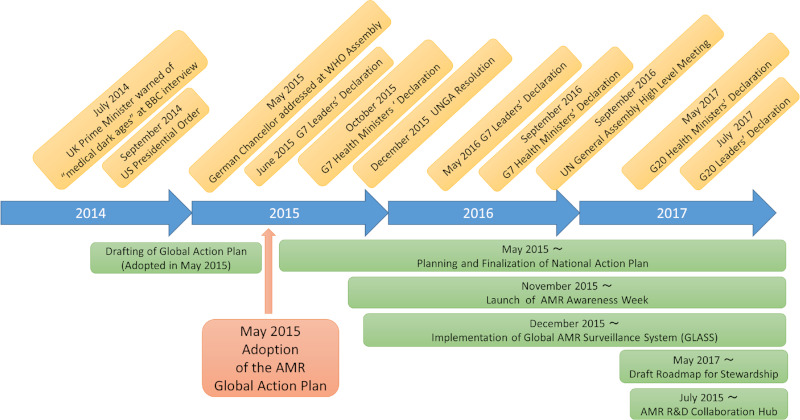
Key political milestones and technical implementations from 2014 to 2017.
The major actions include: i) National Action Plans have been planned and finalized in the following 2 years after the adoption of the Global Action Plan in May 2015 for around 130 countries, which covers more than 95% of the global population (13); ii) AMR Awareness Week was launched in November 2015, the first time in AMR history as a major public communication programs and continues since then; iii) AMR Global Surveillance System (GLASS) was launched in December 2015 to monitor the prevalence of AMR among major pathogens in clinical settings, where more than 40 countries across all continents have joined so far (12,19); iv) Roadmap on Global Framework for Development & Stewardship to Combat AMR was drafted in May 2017 for further elaboration (20); and v) AMR Research and Development Collaboration Hub was established in July 2017 (13).
During this implementation period from 2015 to 2017, there had been a constant issuance of political declaration by G7, G20 and UN General Assembly. All these political declarations reiterated its firm support for the Global Action Plan and committed to implementation of its objectives. This unprecedented level of rapid implementation of the technical outputs during this period could not be explained without this constant and repeated political declaration from the highest level (14).
The challenge of AMR control
Although development and spread of AMR is a natural phenomenon that occurs irrespective of human activities, massive and irrational use of antimicrobials are the major attributing factor for the current rapid spread of AMR (21). The use of antimicrobials is not well regulated in low- and middle-income countries, being accessible without prescription and not dispensed by qualified health professionals. Rampant contamination of substandard and falsified medicine into the supply chain of antimicrobials also contributes to spread of AMR among low- and middle-income countries (7).
In addition to its use for humans in clinical settings, far greater amounts of antimicrobials are currently consumed by the animal husbandry sector, including aqua culture. This massive usage is not only for treatment or prophylaxis of food animals, but also growth promotion purposes as well (22,23).
This under-regulated massive use of anti-microbials both in human and animal sector contributes to the spread of AMR on the global scale, combined with lack of adequate investment on research and development for new medicines. It poses a risk of returning ourselves to an era akin to before Fleming.
The current trend of worsening AMR is likely to result in increased mortality and morbidity, longer stays in hospitals and accelerated health care costs. According to a study initiated by UK Prime Minister David Cameron, the global mortality attributed to AMR could reach 10 million per year by 2050, which is a massive increase from the current estimated mortality of 700, 000 per year (7). This would impact not only health but also political and socio-economic stability of the globe (24).
The strategy of AMR control: from technical issue to a political agenda
The year 2014 was the turning point of more than half century of AMR history, transforming it from technical issue to a political agenda. Prime Minister of UK David Cameron, President of the United States Barack Obama and German Chancellor Angela Merkel played a key role (25,26).
On July 2, 2014, Prime Minister Cameron appeared on a BBC interview for the first time on this issue. In this broadcast, he said the world could soon be "cast back into the dark ages of medicine" and "if we fail to act, we are looking at an almost unthinkable scenario where antibiotics no longer work, and we are cast back into the dark ages of medicine where treatable infections and injuries will kill once again". Prime Minister Cameron also revealed in this broadcast that he discussed the issue in June 2014 with US President Barak Obama and German Chancellor Angela Markel in Brussels, saying that "it's good that Britain is taking the lead on this issue to solve what could otherwise be a really serious global health problem".
It was successfully relayed to US President Barak Obama. President Obama issued an executive order on September 18, 2014 on Combating Antibiotic- Resistant Bacteria (25). This executive order states that "the rise of antibiotic-resistant bacteria represents a serious threat to public health and the economy" and "combating antibiotic-resistant bacteria is a national security priority". Based on this recognition, it contains a comprehensive program against AMR, that encompasses establishment of an oversight and coordination mechanism within the government led by the National Security Council, launch of the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria, improved antibiotic stewardship, strengthening national surveillance efforts for resistant bacteria, preventing and responding to infections and outbreaks with antibiotic-resistant organisms, promoting new and next generation antibiotics and diagnostics, and international cooperation.
The introduction of the AMR agenda by two political leaders - Prime Minister David Cameron and President Barack Obama - in 2014 was perceived as somewhat abrupt as is often the case with the initial stage of any agenda. There was a need for adequate political follow up to keep the momentum. As a strategy to broaden the commitment, it would be desirable for this follow up to be made by different leaders or entities. After the introduction of the agenda into the political arena by UK and US, this follow up role was made by Germany, as the president of G7 in 2015. This German G7 Summit meeting in June 7-8, 2015 was the first time in history for a group of heads of state and heads of government to make a declaration on AMR (15,16) (Previously, it was described as "antibiotic resistance", but starting from this political document, the wording became "antimicrobial resistance (AMR)" to broaden the concept, which became the standard wording thereafter).
This political document states that "Antimicrobials play a crucial role for the current and future success of human and veterinary medicine. We fully support the recently adopted WHO Global Action Plan on Antimicrobial Resistance. We will develop or review and effectively implement our national action plans and support other countries as they develop their own national action plans. We are strongly committed to the One Health approach, encompassing all areas - human and animal health as well as agriculture and the environment. We will foster the prudent use of antibiotics and will engage in stimulating basic research, research on epidemiology, infection prevention and control, and the development of new antibiotics, alternative therapies, vaccines and rapid point-of-care diagnostics. We commit to the annex (Joint Efforts to Combat Antimicrobial Resistance) as we develop or review and share our national action plans".
In conclusion, the level, frequency and density of the politicization on AMR during the period from 2014 to 2017 was unprecedented as a health agenda. This has been the key element in facilitating the recent technical outputs. AMR has successfully maintained political momentum because it is not considered as a mere health issue, it is also a matter of national security, economic growth, social stability, food security and a key determinant for the attainment of Sustainable Development Goals (SDGs). This strategic broadening of the scope of the agenda, through coordination led by WHO with relevant international agencies and other entities was one of the key enabling factors for sustained political commitment on AMR. As observed for AMR, politicization, though not an end in itself, is an effective tool for implementing the output, which could ultimately deliver the expected outcome, in terms of health improvement and mitigation of its socio-economic impact.
References
- 1. Fleming A. "Penicillin". Nobel Lecture, December 11, 1945. https://archive.org/details/B-001-026-408-ALL (accessed October 20, 2019).
- 2. Hardin G. The tragedy of the commons. Science. 1968; 162:1243-1248. [PubMed] [Google Scholar]
- 3. Mackie B. Lessons from Europe on reducing antibiotic use in livestock. BC Medical Journal. 2011; 53:487 [Google Scholar]
- 4. Spellberg B, Powers JH, Brass EP, Miller LG, Edwards JE Jr. Trends in antimicrobial drug development: implications for the future. Clin Infect Dis. 2004; 38:1279-1286. [DOI] [PubMed] [Google Scholar]
- 5. Roca I, Akova M, Baquero F, et al. The global threat of antimicrobial resistance: science for intervention. New Microbes New Infect. 2015; 6:22-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Laxminarayan R, Matsoso P, Pant S, Brower C, Røttingen JA, Klugman K, Davies S. Access to effective antimicrobials: a worldwide challenge. Lancet. 2016; 387:168-175. [DOI] [PubMed] [Google Scholar]
- 7. O'Neill J. (2016). Tackling drug-resistant infections globally: an overview of our work. https://www.biomerieuxconnection.com/wp-content/uploads/2018/04/Tackling-drug-resistant-infections-An-overview-of-our-work_LR_NOCROPS.pdf (accessed October 22, 2019).
- 8. Murray C, Murray CJ, Vos T, Lozano R, et al. (2010). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380:2197-2223 [DOI] [PubMed] [Google Scholar]
- 9. UN. (2015). Press release: high-level meeting on antimicrobial resistance. http://www.un.org/pga/71/2016/09/21/press-release-hl-meeting-on-antimicrobial-resistance/ (accessed October 22, 2019).
- 10. WHO. (2015 a). Global action plan on antimicrobial resistance. 26 May 2015. http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R7-en.pdf?ua=1 (accessed October 23, 2019).
- 11. WHO. At UN, global leaders commit to act on antimicrobial resistance. http://www.who.int/mediacentre/news/releases/2016/commitment-antimicrobial-resistance/en/ (accessed October 23, 2019).
- 12. WHO. Global antimicrobial resistance surveillance system (GLASS). https://www.who.int/glass/en/ (accessed October 24, 2019).
- 13. European Council Council of the European Union. G20 Leaders' Declaration: Shaping an interconnected world. Hamburg, 7/8 July 2017. https://www.consilium.europa.eu/en/press/press-releases/2017/07/08/g20-hamburg-communique/ (accessed October 26, 2019).
- 14. Inoue H, Ren M. Antimicrobial resistance: translating political commitment into national action. Bull World Health Org. 2017; 95:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. G7. Leaders' Declaration, G7 Summit, 7-8 June 2015. https://www.bundesregierung.de/Content/EN/_Anlagen/G7/2015-06-08-g7-abschluss-eng_en.pdf?__blob=publicationFile&v=3 (accessed October 28, 2019).
- 16. G7. Annex to the Leaders' Declaration, G7 Summit, 7- 8 June 2015. https://www.bundesregierung.de/Content/EN/_Anlagen/G7/2015-06-08-g7-abschluss-annex-eng_en.pdf?__blob=publicationFile&v=2 (accessed October 28, 2019).
- 17. G7. G7 Ise-Shima Leaders' Declaration, G7 Ise-Shima Summit, 26-27 May 2016. http://www.mofa.go.jp/files/000160266.pdf (accessed November 2, 2019).
- 18. WHO. Global Action Plan on Antimicrobial Resistance. http://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/ (accessed November 3, 2019).
- 19. WHO. Call for participation: Global Antimicrobial Resistance Surveillance System (GLASS). http://www.who.int/drugresistance/surveillance/glass-enrolment/en/ (accessed November 3, 2019).
- 20. WHO. Global framework for development & stewardship to combat antimicrobial resistance. Draft roadmap. http://www.who.int/phi/implementation/research/WHA_BackgroundPaper-AGlobalFrameworkDevelopmentStewardship-Version2.pdf?ua=1 (accessed November 3, 2019).
- 21. OIE. The OIE strategy on antimicrobial resistance and the prudent use of antimicrobials. November 2016. http://www.oie.int/fileadmin/Home/eng/Media_Center/docs/pdf/PortailAMR/EN_OIE-AMRstrategy.pdf (accessed November 4, 2019) .
- 22. FAO. Status Report on Antimicrobial Resistance. Thirty-ninth session. Rome, 6-13 June 2015. http://www.fao.org/3/a-mm736rev1e.pdf (accessed November 4, 2019).
- 23. FAO. The FAO action plan on antimicrobial resistance 2016-2020. http://www.fao.org/3/a-i5996e.pdf (accessed November 4, 2019).
- 24. World Bank. Final report - drug resistant infections: a threat to our economic future. http://documents.worldbank.org/curated/en/323311493396993758/pdf/114679-REVISED-v2-Drug-Resistant-Infections-Final-Report.pdf (accessed November 5, 2019).
- 25. The White House. Executive order -- combating antibiotic-resistant bacteria. https://obamawhitehouse.archives.gov/the-press-office/2014/09/18/executive-order-combating-antibiotic-resistant-bacteria (accessed November 5, 2019).
- 26. Hoffman SJ, Caleo GM, Daulaire N, Elbe S, Matsoso P, Mossialos E, Rizvi Z, Røttingen JA. Strategies for achieving global collective action on antimicrobial resistance. Bull World Health Org. 2015; 93:867-876. [DOI] [PMC free article] [PubMed] [Google Scholar]


