Summary
Hypercoagulation and anticoagulation treatment have become new challenges in coronavirus disease 2019 (COVID-19) patients during the COVID-19 pandemic. We herein suggest an algorithm for an anticoagulation treatment with unfractionated heparin in moderate to severe COVID-19 cases in Japan, and report a case of COVID-19 pneumonia with anticoagulation treatment. Although several promising drugs for COVID-19 are being tested in clinical trials, definitive treatments have not yet been established. In this report, we demaonstrate that anticoagulation treatment with unfractionated heparin has the possibility of becoming at least a supportive treatment for COVID-19 patients.
Keywords: COVID-19, hypercoagulation, anticoagulation treatment, unfractionated heparin
Introduction
With coronavirus disease 2019 (COVID-19) being a global threat (1), several case reports, including autopsy series, show that patients with COVID-19 experience pulmonary embolism (PE) (2-4). Although several promising drugs for COVID-19 are being tested in clinical trials, a definitive treatment has not yet been established (5). A previous study with 449 patients indicated that anticoagulation (AC) treatment using low molecular weight heparin (LMWH) and unfractionated heparin (UFH) was associated with decreased mortality in severe COVID-19 patients with coagulopathy (6). Although several facilities around the world have developed an AC algorithm for COVID-19 patients (7-9), there is no such algorithm nor case reports of COVID-19 patients with AC in Japan. In order to develop such an algorithm, it is necessary to consider which drugs have been approved in a given country. Based on an AC algorithm used in other countries (7-9), we herein suggest an AC therapy with UFH for moderate to severe COVID-19 patients in Japan (Figure 1), and report a case of a COVID-19 patient with pneumonia and AC.
Figure 1.
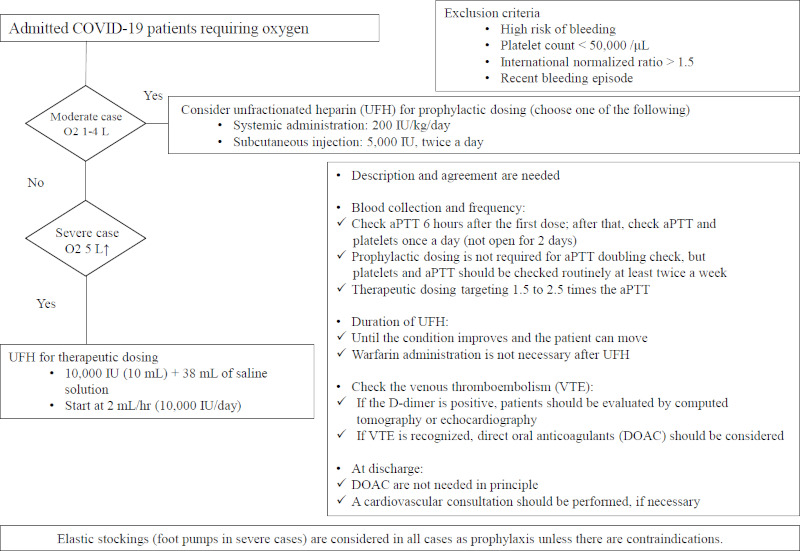
Algorithm for unfractionated heparin anticoagulation treatment in patients with moderate to severe COVID-19. This figure shows the algorithm for unfractionated heparin anticoagulation therapy in patients with moderate to severe COVID-19 that can be used safely in Japan.
Patient and Methods
A healthy 68-year-old male presented to the hospital with a 7-day history of fever, productive cough, and progressing dyspnea. The physical examination revealed a body temperature of 37.1℃, blood pressure of 124/76 mmHg, pulse of 94 beats per minute, respiratory rate of 24 breath per minute, and oxygen saturation of 91% in ambient air. In addition to lymphopenia (7.1%), laboratory testing revealed that the lactate dehydrogenase (440 U/L) and C-reactive protein (11.7 mg/dL) concentrations were elevated, while the d-dimer level was normal (< 0.5 μg/mL). A chest computed tomography (CT) scan showed bilateral multifocal peripheral ground-glass opacities; thus, the patient was diagnosed with COVID-19 by reverse transcription polymerase chain reaction. We administered hydroxychloroquine (200 mg BID), methylprednisolone (1 mg/kg/day), oxygen at 1 liter per minute (LPM), and systemic prophylactic dosing (10,000 IU/day) of UFH. As his oxygen requirement increased to 4 LPM by hospital day (HD) 5, and his d-dimer level increased to 10.9 μg/mL, UFH was initiated for therapeutic dosing (10,000 IU/ day with a target of 1.5 to 2.5 times the activated partial thromboplastin time [aPTT]). After the patient was started on UFH, his oxygen requirement and d-dimer level gradually decreased. As oxygen administration was halted when his d-dimer level decreased to 2.0 μg/ mL and he could move by himself on HD 11, UFH was terminated without any adverse events (the duration of UFH for therapeutic dosing was 7 days).
Discussion
We herein suggest an AC treatment using UFH in moderate to severe COVID-19 cases in Japan (Figure 1), while showing that intubation was avoided in a high-risk patient using AC. Although the pathogenesis of COVID-19 has not yet been elucidated, the clinical stage of the disease is thought to be divided into three phases: the viremia phase, the acute phase, and the recovery phase (10). AC may be especially recommended for patients in the viremia and acute phases (10) as the disease itself and inflammation as well as other factors may lead to excessive activation of coagulation in these phases (6,11).
In a study supporting AC therapy as an effective treatment for COVID-19, veno-venous extracorporeal membrane oxygenation (VV-ECMO) is reported as one of the treatments of severe COVID-19 which is thought to be possibility of comorbid PE has been pointed out (12). VV-ECMO may have been useful in AC. The one of the reasons for it are that the therapeutic effect of VV-ECMO is not direct treatment of respiratory failure, but UFH which is used to maintain the circuitry of VV-ECMO may treat for PE of severe COVID-19 (12). Previous autopsy case series have also reported embolism in the lung of a COVID-19 patient (4).
Although we suggest AC therapy with UFH as treatment for moderate to severe COVID-19 cases, several issues with AC therapy remain and should be addressed in the future. First, the practical application aof AC with UFH, including indications, dosage, and duration of AC, should be explored further. Although one algorithm recommends AC for all patients with COVID-19 (8), we suggest considering prophylactic dosing of UFH (systemic administration of 200 IU/kg/ day or subcutaneous injection at 5,000 IU, twice a day) for moderate COVID-19 patients requiring 1-4 liters of oxygen and therapeutic dosing (systemic administration of 200 IU/kg/day with a target of 1.5 to 2.5 times the aPTT) for severe COVID-19 patients requiring more than 5 liters of oxygen. The recommended duration of UFH is until the patient's condition improves and the patient can move. As AC treatment is currently controversial, clinicians should consider the risk of bleeding as well as post-discharge treatment. The Mount Sinai algorithm calls for treatment with direct oral anticoagulants (DOAC) for 2 weeks after the patient has been discharged (9). However, there is no indication for DOAC use for COVID-19 in Japan. Additionally, as DOAC is a new drug, interactions with COVID-19 therapies as well as the high costs must be considered. Despite these issues, we suggest an UFH AC treatment algorithm for moderate to severe COVID-19 cases that can be used safely in Japan (Figure 1).
Our study has several limitations. First, we report only one case of COVID-19 with AC. Second, adequate assessment of thrombosis using an enhanced CT scan and an ultrasound scan before treatment with AC was not carried out due to restrictions associated with infection prevention and control. Third, the therapeutic impact of AC on COVID-19 pneumonia cannot be confirmed by this report alone as there were many confounding factors, such as patient demographics and anti-COVID-19 therapies. However, given the hypercoagulability of COVID-19 patients and the clinical impact of AC observed in previous studies (6,10), at a minimum, AC may be used as supportive therapy for COVID-19 patients.
In conclusion, this is the first report of an AC treatment algorithm for patients with moderate to severe COVID-19, and the first successfully recovered case of COVID-19 with AC in Japan. Hypercoagulation and AC in COVID-19 patients is thought to be a new challenge (13). With the current large numbers of COVID-19 cases, further studies that explore the improvement of AC algorithms and evaluation of the therapeutic impact of AC using multivariate analysis are expected.
Acknowledgements
We thank all the clinical staff at our hospital for their dedication to clinical practice and patient care.
References
- 1. World Health Organization. Coronavirus disease (COVID-19) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed April 30, 2020).
- 2. Ullah W, Saeed R, Sarwar U, Patel R, Fischman DL. COVID-19 complicated by acute pulmonary embolism and right-sided heart failure. JACC Case Rep. 2020; doi:10.1016/j.jaccas.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rotzinger DC, Beigelman-Aubry C, von Garnier C, Qanadli SD. Pulmonary embolism in patients with COVID-19: Time to change the paradigm of computed tomography. Thromb Res. 2020; 190:58-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fox SE, Akmatbekov A, Harbert JL, Li G, Brown Q, Vander Heide RS. Pulmonary and cardiac pathology in Covid-19: The first autopsy series from New Orleans. medRxiv. 2020; https://doi.org/10.1101/2020.04.06.20050575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020; doi:10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 6. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020; 18:1094-1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Massachuset ts General Hospi tal. COVID-19 Anticoagulation Algorithm. https://www.massgeneral.org/assets/MGH/pdf/news/coronavirus/mass-general-covid-19-anticoagulation-algorithm.pdf (accessed April 30, 2020).
- 8. Brigham and Womens Hospital. COVID-19 Clinical Guidelines. Thrombotic Disease. https://covidprotocols.org/protocols/09-hematology (accessed April 30, 2020).
- 9. Mount Sinai. COVID-19 Anticoagulation Algorithm. https://emergencymedicinecases.com/wp-content/uploads/2020/04/COVID-19-Anticoagulation-Algorithm-version_final_1.1.pdf (accessed April 30, 2020).
- 10. Lin L, Lu L, Cao W, Li T. Hypothesis for potential pathogenesis of SARS-CoV-2 infection - a review of immune changes in patients with viral pneumonia. Emerg Microbes Infect. 2020; 9:727-732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel A, Mehra M, Schuepbach R, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020; 395:1417-1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Taniguchi H, Ogawa F, Honzawa H, Yamaguchi K, Niida S, Shinohara M, Takahashi K, Iwashita M, Abe T, Kubo S, Kudo M, Takeuuchi I. Veno-venous extracorporeal membrane oxygenation for severe pneumonia: COVID-19 case in Japan. Acute Med Surg. 2020; 7:e509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Violi F, Pastori D, Cangemi R, Pignatelli P, Loffredo L. Hypercoagulation and antithrombotic treatment in coronavirus 2019: a new challenge. Thromb Haemost. 2020; doi: 10.1055/s-0040-1710317. [DOI] [PMC free article] [PubMed] [Google Scholar]


