Abstract
PURPOSE:
We recently reported a 17.5 % objective RECIST 1.1 response rate in a phase II study of pembrolizumab in patients with advanced sarcoma (SARC028). The majority of responses occurred in undifferentiated pleomorphic sarcoma (UPS) and dedifferentiated liposarcoma (DDLPS). We sought to determine whether we can identify immune features that correlate with clinical outcomes from tumor tissues obtained pre- and on-treatment.
EXPERIMENTAL DESIGN:
Pretreatment (n=78) and 8-week on-treatment (n=68) tumor biopsies were stained for PD-L1 and multiplex immunofluorescence panels. The density of positive cells was quantified to determine associations with anti-PD-1 response.
RESULTS:
Patients that responded to pembrolizumab were more likely to have higher densities of activated T cells (CD8+ CD3+ PD-1+) and increased percentage of tumor associated macrophages (TAMs) expressing PD-L1 pre-treatment compared to non-responders. Pre-treatment tumors from responders also exhibited higher densities of effector memory cytotoxic T cells and regulatory T cells compared to non-responders. Additionally, higher density of cytotoxic tumor infiltrating T-cells at baseline correlated with a better progression-free survival (PFS).
CONCLUSIONS:
We show that quantitative assessments of CD8+ CD3+ PD-1+ T cells, % TAMs expressing PD-L1, and other T cell densities correlate with sarcoma response to pembrolizumab and improved PFS. Our findings support that multiple cell types present at the start of treatment may enhance tumor regression following anti-PD-1 therapy in specific advanced sarcomas. Efforts to confirm the activity of pembrolizumab in an expansion cohort of UPS/DDLPS patients are underway.
Keywords: bone sarcoma, immunotherapy, immune cell infiltrate, SARC028, soft tissue sarcoma
INTRODUCTION
Sarcomas are a heterogeneous and rare group of malignancies, constituting approximately 1% of all adult cancers (1). With over 50 recognized histologic subtypes, sarcomas are broadly classified into soft tissue sarcomas (STS) and bone sarcomas. Although primary treatment for localized sarcomas is surgical resection and may also include systemic and radiation therapies, approximately 50% of patients with large, high-grade sarcomas will develop distant metastases (2). Systemic therapy remains the standard for metastatic sarcoma (doxorubicin, ifosfamide, dacarbazine, gemcitabine/docetaxel, trabectidin, erurubin, pazopanib), however fewer than 20% of patients achieve objective responses and chemotherapy options are associated with substantial toxicities and limited durability. Median progression-free survival (PFS) with chemotherapy regimens is ~5 months (3) and median overall survival (OS) for patients with metastatic sarcoma is less than 2 years (4,5).
There is a clear need for novel therapies for patients with metastatic sarcoma. The burgeoning field of immuno-oncology has led to improvement in patient outcomes across a wide range of cancer types, with FDA approvals in melanoma, Merkel cell carcinoma, urologic malignancies, and non-small cell lung cancer, among others, in both the metastatic and adjuvant settings (5–7). The success of immune checkpoint inhibitors has led to considerable interest in evaluating immunotherapy for sarcomas (3,7–15).
The multicenter phase 2 trial SARC028 (NCT02301039) is one of the first clinical trials of immunotherapy with checkpoint inhibitors in patients with advanced STS and bone sarcomas (8). This investigator-initiated, open-label phase 2 trial of pembrolizumab (anti-PD-1) monotherapy in patients with advanced STS or bone sarcoma was completed at 12 academic medical centers in the USA. Although sarcomas are generally considered to be poorly-immunogenic tumors and are typically characterized by low mutational burden (16), patients with advanced sarcomas participating in SARC028 demonstrated highly variable and histologic subtype-dependent response rates to pembrolizumab.
A hallmark of this study was the rigorous translational approach in terms of required longitudinal blood and tumor sampling to better understand biomarkers predictive of clinical response. Here, we report tumor immunohistochemical and immunofluorescence characterization of the tumor immune microenvironment. Through this work, we sought to 1) characterize the tumor-associated immune response in patients with advanced STS and bone sarcoma at baseline, 2) elucidate changes induced upon treatment with pembrolizumab, and 3) identify predictors of response or resistance to immune checkpoint therapy.
MATERIALS AND METHODS
Study design and participants
Patients with STS age 18 years or older and bone sarcoma age 12 years or older with histological evidence of metastatic or surgically unresectable locally advanced sarcoma were eligible. Patients had one of several histological subtypes: leiomyosarcoma, poorly differentiated or dedifferentiated liposarcoma (DDLPS), undifferentiated pleomorphic sarcoma (UPS), synovial sarcoma, Ewing’s sarcoma, osteosarcoma, and dedifferentiated or mesenchymal chondrosarcoma. Eligible patients also had measurable disease by computed tomography (CT) or magnetic resonance imaging (MRI) according to Response Evaluation Criteria In Solid Tumors (RECIST) version 1.1 and at least one site of disease that was safely accessible for core needle biopsies before and during treatment. The protocol was approved by the institutional review boards at each site. All participants gave written informed consent on the basis of the Declaration of Helsinki principles.
Procedures
Patients received 200mg pembrolizumab every 3 weeks until disease progression or unacceptable toxicity. Disease was assessed using CT or MRI at baseline, after 8 weeks on therapy, and then every 12 weeks until disease progression. Response was determined using RECIST 1.1. Tumor biopsies before and during treatment were required and obtained before the first drug administration and after 8 weeks of therapy. Some patients had multiple biopsies available for analysis for a given time-point.
Immunohistochemistry (IHC) PD-L1 staining
Hematoxylin and eosin slides from all formalin-fixed paraffin-embedded (FFPE) tissue specimens were reviewed by specialized sarcoma pathology experts (ERP, RS, JRC, AJL) to identify the presence of malignant cells and to select the best representative tumor block from each patient. For IHC staining 4-μm-thick sections were cut and staining was done using an automated staining system (Leica Bond Max, Leica Biosystems, Nussloch GmbH) with antibody against PD-L1 using clone 22C3, (dilution 1:50; DAKO, Santa Clara, CA, Cat# M365329–2) with previously optimized IHC conditions and performed according to standard automated protocols (17). The antibody was detected with the Leica Bond Polymer Refine detection kit (Leica Biosystems, cat# DS9800), including diaminobenzidine reaction to detect the antibody labeling and hematoxylin counterstaining. Human tonsil FFPE tissues were also used with and without primary antibodies as positive and negative controls, respectively.
Scoring of IHC PD-L1 expression in malignant cells was performed by two pathologists (RS, ERP) under light microscopy, considering a partial or complete membranous staining at any intensity equal to or greater than 1% of tumor cells expressing antigen as the criteria for positive cases. Cases without agreement were resolved by consensus discussion with a third pathologist (AJL or WLW).
Multiplex Immunofluorescence
Multiplex immunofluorescence (mIF) was performed as previously described (18). Manual mIF staining was performed in 4-μm sequential histologic tumor sections obtained from representative FFPE tumor blocks by using the Opal 7-Color fIHC Kit (PerkinElmer, Waltham, MA). The stained slides were scanned by a Vectra multispectral microscope (PerkinElmer). The immunofluorescence (IF) markers used were grouped into two 5-antibody panels (Table 1). Panel 1 consisted of PD-L1 (clone E1L3N, dilution 1:100; Cell Signaling Technology, Beverly, MA), CD3 (T-cell lymphocytes; dilution 1:100; Dako), CD8 (cytotoxic T cells; clone C8/144B, dilution 1:20; Thermo Fisher Scientific, Waltham, MA), PD-1 (clone EPR4877–2, dilution 1:250; Abcam, Cambridge, MA), and CD68 (macrophages; clone PG-M1, dilution 1:450; Dako). Panel 2 consisted of CD3 (T-cell lymphocytes; dilution 1:100; Dako), CD8 (cytotoxic T cells; clone C8/144B, dilution 1:20; Thermo Fisher Scientific, Waltham, MA), granzyme B (cytotoxic lymphocytes; clone F1, ready to use; Leica Biosystems), FOXP3 (regulatory T cells; clone 206D, dilution 1:50; BioLegend, San Diego, CA), and CD45RO (memory T cells; clone UCHL1, ready to use; Leica Biosystems).
Table 1.
Definitions of immune cell phenotypes
| Immune cell type | Immune cell phenotype |
|---|---|
| Panel 1 | |
| T lymphocytes | (CD3+ CD8+) + (CD3+ PD-1+) + (CD3+ CD8+ PD-1+) + (CD3+) |
| Cytotoxic T cells | (CD3+ CD8+) + (CD3+ CD8+ PD-1+) |
| T cells antigen-experienced | (CD3+ PD-1+) + (CD3+ CD8+ PD-1+) |
| Cytotoxic T cells antigen experienced | CD3+ CD8+ PD-1+ |
| Macrophages | (CD68+ PD-L1-) + (CD68+ PD-L1+) |
| Panel 2 | |
| T lymphocytes | (CD3+ CD8) + (CD3+ CD8+ GranzymeB+) + (CD3+ CD8+ CD45RO+) + (CD3+ FOXP3+) + (CD3+ CD8+ FOXP3+) + (CD3+) |
| Cytotoxic T cells activated | CD3+ CD8+ GranzymeB+ |
| Effector memory cytotoxic T cells | CD3+ CD8+ CD45RO+ |
| Regulatory T cells | (CD3+ FOXP3+) - (CD3+ CD8+ FOXP3+) |
Visualization of primary antibody was accomplished by using tyramide signal amplification linked to a specific fluorochrome from the Opal 7-Color fIHC Kit for each primary antibody using our standard protocol as previously described. Human tonsil FFPE tissues were also used with and without primary antibodies as positive and negative (autofluorescence) controls, respectively. The mIF slides were scanned using a multispectral microscope (Vectra™ 3.0, PerkinElmer) under fluorescent illumination. From each slide, Vectra automatically captured the fluorescent spectra from 420 nm to 720 nm at 20-nm intervals with the same exposure time and then combined the captured images to create a single stack image that retained the particular spectral signature of all IF markers. After the specimens were scanned at low magnification (×10), the entire tissue were sampled with individual fields (334 × 250 μm each) with a phenochart 1.0.4 (PerkinElmer) viewer so that they could be scanned at high resolution (×40).
Each mIF image was analyzed using the InForm software (InForm™, PerkinElmer). The spectral signature for each fluorophore used was obtained using the spectral library according the uniplex IF staining plus the autofluorescence spectral background which can be subtracted from the analysis. These spectral signatures were then used to separate the different targets in the mIF images. A trained pathologist used this information to modify the InForm algorithm to identify different co-localization of the various cell populations using panel 1 and panel 2 labeling. Every cell phenotype was evaluated as cell density and the data was consolidated using SpotFire (PerkinElmer) and Excel 2013.
Statistical analysis
Descriptive statistics, such as mean, standard deviation, and median, were used to summarize the data. For cases with multiple biopsies evaluable at a given time-point, scores were averaged across evaluable biopsies. Differences in tumor-associated immune cell populations between baseline and on-treatment samples and between samples acquired from responder and nonresponder patients were compared using independent-samples median and Kruskal-Wallis tests using SPSS Statistics 24 (IBM SPSS, Chicago, IL, USA) and SAS 9.4. Survival analyses were performed by Kaplan-Meier method. For all analyses, p-value <0.05 was considered significant. Plots were generated using GraphPad Prism version 7 and SAS 9.4.
RESULTS
Eighty-six patients were enrolled to SARC 028 between March 13, 2015 and February 18, 2016 of whom 84 received pembrolizumab (42 in each of the STS and bone sarcoma cohorts) and 80 were evaluable for response (40 in each disease cohort) (Supplemental Table 1) (8). Overall, 7 (18%) of 40 patients with STS had an objective response with the best response seen in patients with UPS (40%, 4 of 10) and DDLPS (20%, 2 of 10).
Tumor biopsies were safely obtained from 78 (93%) of 84 patients before treatment and from 68 (81%) of 84 patients during treatment. Some patients had multiple biopsies available from a given time-point, however not all specimens were evaluable due to low or no viable tumor content. Only biopsies which passed quality control (QC) and which were acquired from patients evaluable for response (n=80) were included in this study for evaluation by IHC and mIF. In total, 66 tumor biopsies were obtained prior to first dose treatment, passed QC and were acquired from patients evaluable for response (Supplemental Table 2). Seventy-one tumor biopsies were obtained after 8 weeks on therapy, passed quality control and were acquired from patients evaluable for response.
PD-L1 expression by tumor cells
We first examined whether response to anti-PD1 therapy was associated with PD-L1 expression in the tumor microenvironment. As previously reported, few STS and bone sarcomas expressed PD-L1 at baseline in this cohort (8). PD-L1 expression was observed in only 2 (5%) of 40 tumors with evaluable biopsies (Figure 1a). Although both tumors expressing PD-L1 were UPS and responded to therapy, response to pembrolizumab was also seen in 5 patients with STS (2 UPS, 2 DDLPS, 1 SS) in the absence of tumor PD-L1 expression at baseline (Figure 1b).
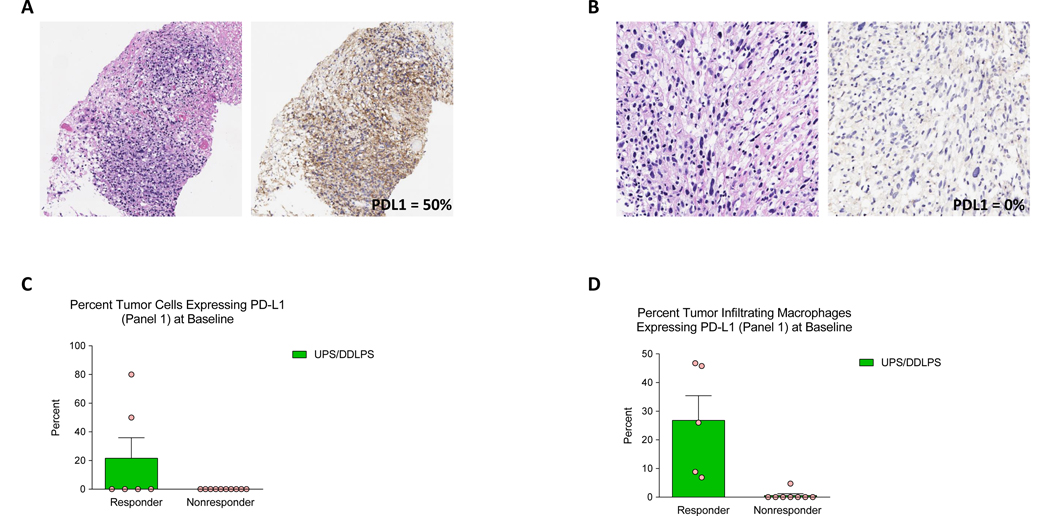
Figure 1.
Responders to pembrolizumab included patients with tumors (A) with PD-L1 expression and (B) without PD-L1 expression at baseline. Response to anti-PD1 therapy is associated with higher levels of PD-L1 expression by (C) tumor cells and (D) tumor infiltrating macrophages at baseline among patients with UPS and DDLPS (left panel A, B: H+E; right panel A, B: tumor PD-L1 expression). Baseline tumor samples available for immune profiling by IHC were obtained prior to anti-PD1 treatment (8 responder and 58 non-responder patients). Error bars represent SEM. * = p≤0.05, ** = p≤0.01, *** = p≤0.001, n.s. = not significant.
Baseline density of tumor-associated immune cells
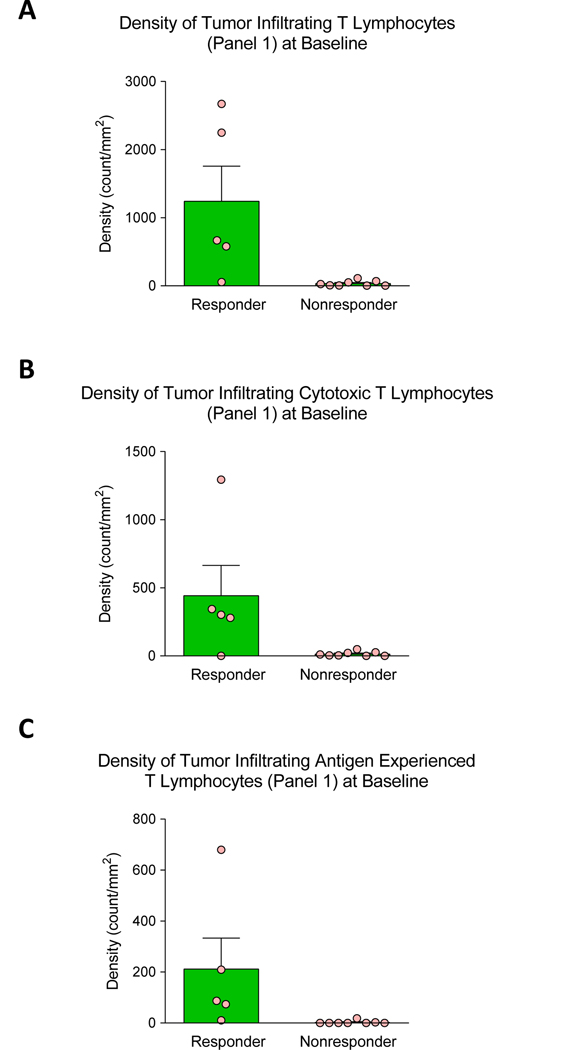
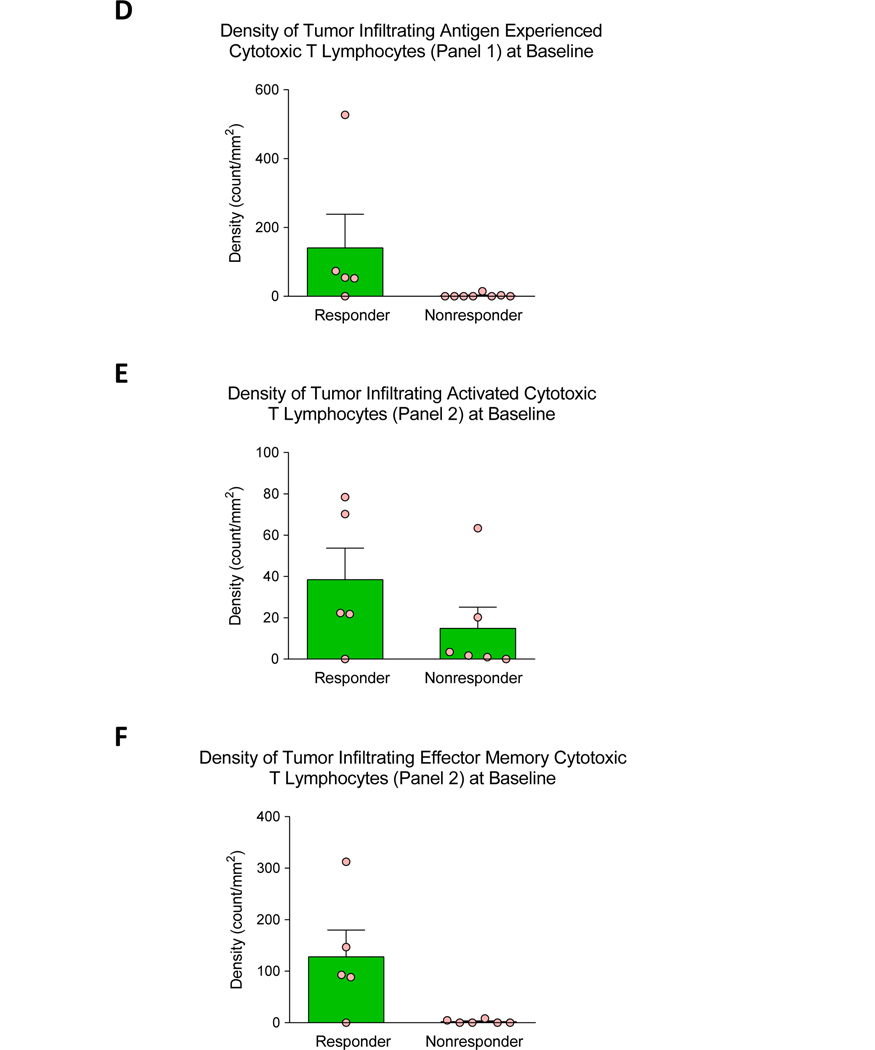
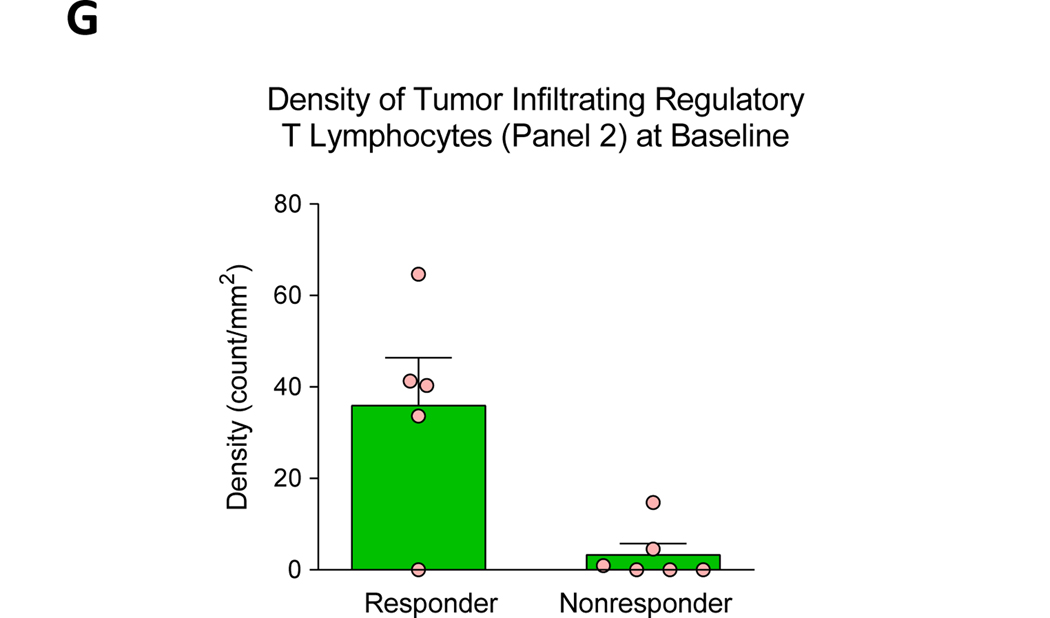
Patients who had an objective response to pembrolizumab by RECIST 1.1 had a significantly higher average percentage of tumor cells and tumor-associated macrophages (TAMs) expressing PD-L1 at baseline compared to non-responders (Table 2, Figure 1c–d, Supplemental Figure 1a–b). Responders also had greater density of nearly all tumor-associated immune cell phenotypes examined (Table 2, Figure 2, Supplemental Figure 1c–i). These results were also consistent when analyses were performed focusing on STS histologies only (Supplemental Table 3) or on the UPS/DDLPS cases alone (Supplemental Table 4).
Table 2.
Comparison of tumor PD-L1 expression and tumor-associated immune infiltrate between baseline tumor biopsies from responders and nonresponders (all histologies)
| Responders (n=8) | Nonresponders (n=58) | |||||||
|---|---|---|---|---|---|---|---|---|
| Immune cell phenotype | Mean | Median | Range | Mean | Median | Range | P valuea | P valueb |
| % tumor cells expressing PD-L1 | 21.7 | 0 | 0–80.0 | 0 | 0 | 0–0 | <0.001 | <0.001 |
| Panel 1 | ||||||||
| T lymphocytes* | 1254.3 | 668.3 | 104.6–2671.1 | 71.8 | 38.0 | 0–563.0 | 0.031 | 0.001 |
| Cytotoxic T cells* | 443.7 | 301.7 | 0–1293.6 | 23.3 | 10.6 | 0–131.2 | 0.195 | 0.012 |
| T cells antigen-experienced* | 216.6 | 87.0 | 32.8–680.0 | 13.4 | 0 | 0–123.0 | 0.065 | 0.002 |
| Cytotoxic T cells Antigen-experienced* | 141.3 | 54.5 | 0–526.8 | 6.8 | 0 | 0–61.7 | 0.212 | 0.012 |
| Macrophages* | 480.3 | 337.5 | 171.5–1035.1 | 250.8 | 166.8 | 12.0–2145.2 | 0.195 | 0.030 |
| % macrophages PD-L1+ | 30.6 | 44.8 | 6.9–46.7 | 0.9 | 0 | 0–37.2 | <0.001 | <0.001 |
| Panel 2 | ||||||||
| T lymphocytes* | 434.5 | 218.9 | 34.4–1228.0 | 740 | 35.5 | 0.2–671.9 | 0.355 | 0.023 |
| Cytotoxic T cells activated* | 365.4 | 46.3 | 0–1999.6 | 139.5 | 5.3 | 0–6215.5 | 0.226 | 0.095 |
| Effector memory cytotoxic T cells* | 184.2 | 120.1 | 0–464.1 | 14.7 | 2.0 | 0–298.5 | 0.226 | 0.006 |
| Regulatory T cells* | 121.1 | 40.8 | 0–546.4 | 3.8 | 0.6 | 0–36.6 | 0.226 | 0.004 |
| Cytotoxic T cells / regulatory T cells | 0.8 | 0.7 | 0–1.9 | 27.9 | 2.6 | 0–888.8 | 0.064 | 0.253 |
| % cytotoxic T cells activated | 8.6 | 10.2 | 0–16.0 | 21.3 | 19.3 | 0–79.1 | 0.372 | 0.250 |
| % effector memory cytotoxic T cells | 31.2 | 25.5 | 0–67.1 | 15.0 | 7.4 | 0–75.2 | 0.034 | 0.029 |
| % regulatory T cells | 9.9 | 8.4 | 0–20.2 | 7.5 | 2.1 | 0–100.1 | 0.034 | 0.063 |
Responders = complete response + partial response
Nonresponders = stable disease + progressive disease
number/mm2
Independent samples median test
Independent samples Kruskal-Wallis test
Figure 2.
Response to anti-PD1 therapy is associated with higher density of sarcoma-associated immune infiltrates at baseline among patients with UPS and DDLPS. Tumor biopsies obtained from patients who responded to pembrolizumab therapy had higher baseline density (cell count/mm2) of tumor infiltrating (A) T lymphocytes, (B) cytotoxic T lymphocytes, (C) antigen experience T lymphocytes, (D) antigen experienced cytotoxic T lymphocytes, (E) activated cytotoxic T lymphocytes, (F) effector memory cytotoxic T lymphocytes, and (G) regulatory T lymphocytes. Baseline tumor samples available for immune profiling by IHC were obtained prior to anti-PD1 treatment (8 responder and 58 non-responder patients). Error bars represent SEM. * = p≤0.05, ** = p≤0.01, *** = p≤0.001, n.s. = not significant.
Sarcoma-associated effector memory cytotoxic T cells and regulatory T cells increase upon anti-PD1 treatment while other tumor-associated immune cell populations remain largely unchanged
As anti-PD-1 generally targets tumor-resident T cells (19), we next examined whether anti-PD1 therapy was associated with changes in the tumor-associated immune infiltrate by comparing biopsies obtained prior to initiation of treatment and those early on-treatment (after 8 weeks of therapy, Table 3). Across all histologies, we found largely stable densities of most tumor-associated immune cell phenotypes comparing baseline and early on-treatment biopsies. However, both effector memory cytotoxic T cells (CD3+ CD8+ CD45RO+) and regulatory T cells [(CD3+ FOXP3+) - (CD3+ CD8+ FOXP3+)] increased in frequency upon PD-1 blockade when examined as a percentage of all tumor-associated T lymphocytes (median on-treatment vs baseline % effector memory cytotoxic T cells 21.5% versus 7.9%, p=0.054; median on-treatment versus baseline % regulatory T cells 8.3% versus 3.7%, p=0.022). These trends were consistent in analyses limited to either STS histologies (Supplemental Table 5) or bone histologies (Supplemental Table 6). Interestingly, however, within the UPS and DDLPS subtypes, effector memory cytotoxic T cell and regulatory T cell populations made up a large proportion of T lymphocytes at baseline while their proportion did not increase after 8 weeks of pembrolizumab treatment (Supplemental Table 7).
Table 3.
Comparison of tumor PD-L1 expression and tumor immune infiltrate between baseline biopsies and at 8 weeks on treatment (all histologies)
| Pre-treatment | 8 weeks on-treatment | |||||||
|---|---|---|---|---|---|---|---|---|
| Immune cell phenotype | Mean | Median | Range | Mean | Median | Range | P valuea | P valueb |
| % tumor cells expressing PD-L1 | 3.2 | 0 | 0–90.0 | 0.6 | 0 | 0–15.0 | 0.278 | 0.192 |
| Panel 1 | ||||||||
| T lymphocytes* | 180.5 | 47.9 | 0–2671.1 | 123.1 | 56.9 | 0–854 | 0.857 | 0.539 |
| Cytotoxic T cells* | 60.4 | 16.0 | 0–1293.6 | 40.7 | 20.9 | 0–289.8 | 0.857 | 0.436 |
| T cells antigen-experienced* | 31.3 | 0.9 | 0–680 | 12.9 | 0 | 0–499 | 0.207 | 0.021 |
| Cytotoxic T cells antigen-experienced* | 18.7 | 0 | 0–526.8 | 4.9 | 0 | 1–110.7 | 0.583 | 0.119 |
| Macrophages* | 279.8 | 193.7 | 12–2145.2 | 224.8 | 74.9 | 0–2544.7 | 0.007 | 0.002 |
| % macrophages PD-L1+ | 4.7 | 0 | 0–80.8 | 2.5 | 0 | 0–26.8 | 0.042 | 0.071 |
| Panel 2 | ||||||||
| T lymphocytes* | 102.0 | 36.3 | 0.2–1228.0 | 120.3 | 53.1 | 3.6–2202.2 | 0.472 | 0.201 |
| Cytotoxic T cells activated* | 152.9 | 6.5 | 0–6215.5 | 15.3 | 8.0 | 0–96.7 | 0.929 | 0.765 |
| Effector memory cytotoxic T cells* | 31.5 | 3.3 | 0–464.1 | 27.8 | 9.2 | 0–161.3 | 0.003 | 0.011 |
| Regulatory T cells* | 15.5 | 0.7 | 0–546.4 | 9.8 | 5.8 | 0–95.7 | 0.008 | 0.022 |
| Cytotoxic T cells / regulatory T cells | 24.0 | 2.1 | 0–888.8 | 10.9 | 1.9 | 0–193.3 | 0.928 | 0.619 |
| % cytotoxic T cells activated | 20.5 | 15.8 | 0–79.1 | 22.7 | 16.9 | 0–83.8 | 0.928 | 0.567 |
| % effector memory cytotoxic T cells | 17.9 | 7.9 | 0–75.2 | 22.9 | 21.5 | 0–62.1 | 0.054 | 0.018 |
| % regulatory T cells | 7.9 | 3.7 | 0–100.1 | 12.6 | 8.3 | 0–53.8 | 0.022 | 0.007 |
number/mm2
Independent samples median test
Independent samples Kruskal-Wallis test
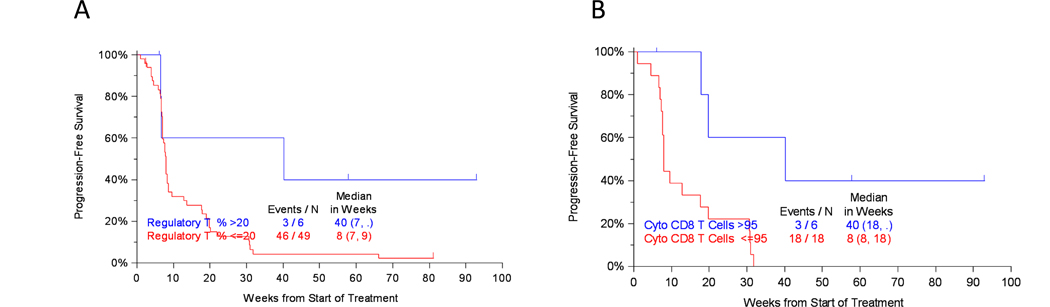
Tumor-associated immune infiltrate may be predictive of patient response to anti-PD-1 therapy and prognostic of survival
Finally, we sought to determine whether features of the tumor-associated immune infiltrate either at baseline or early on-treatment was prognostic of patient outcomes. We investigated whether there was an association between tumor-associated immune infiltrate either at baseline or early on-treatment (after 8 weeks pembrolizumab therapy) and either PFS or OS by the Kaplan-Meier method. We found that patients whose T-cell infiltrate contained a greater percentage of regulatory T cells at baseline had longer median PFS compared to those whose T-cell infiltrate contained a lower proportion of regulatory T cells at baseline (40 versus 8 weeks, p=0.044) (Figure 3a). Additionally, patients with higher density of cytotoxic T-cell infiltrate at baseline had longer median PFS compared to those with lower density of cytotoxic T-cell infiltrate at baseline (40 versus 8 weeks, p=0.016) (Figure 3b).
Figure 3.
Association between sarcoma-associated immune infiltrate and survival. Higher baseline (A) percentage of regulatory T cells and (B) cytotoxic T cells are associated with longer progression-free survival.
DISCUSSION
Among participants of the SARC028 study, pembrolizumab demonstrated encouraging activity in patients with specific subtypes of advanced STS. The greatest response to anti-PD1 therapy was observed in patients with UPS and DDLPS, with 40% and 20% of patients achieving objective response, respectively (8). We examined the tumor immune microenvironment to identify baseline features associated with response to pembrolizumab in patients with advanced STS and bone sarcomas and observed a correlation between higher PD-L1 expression at baseline by tumor-associated macrophages and higher baseline density of tumor-associated T-cell infiltrates with improved clinical outcomes (objective response rate, PFS). Additionally, although few sarcomas in this study expressed PD-L1 (2/40), those that did were tumors which responded to pembrolizumab.
Interestingly, the objective response rate to pembrolizumab observed in SARC028 remains the highest among studies evaluating immune checkpoint therapy in similar patient cohorts reported to date (3,13–15). Single institution studies of single agent anti-PD1 therapy have reported a variable mixed response to therapy. In 2016 for instance, two studies evaluated single-agent nivolumab (anti-PD-1) in advanced sarcomas. Ben-Ami et al reported no objective responses to therapy among 12 patients with advanced uterine leiomyosarcoma (13), while in a study of 28 patients with advanced STS and bone sarcomas Paoluzzi et al observed a partial response in 3 and stable disease in 9 patients, respectively (14). Subsequent to SARC028, 2 multicenter center phase 2 studies of anti-PD1 therapy in combination with a second agent were reported (3,15). Toulmonde et al performed a multicenter, phase 2 study to evaluate the efficacy and safety of pembrolizumab in combination with metronomic cyclophosphamide in patients with advanced STS but observed limited activity (1 partial response in a patient with solitary fibrous tumor) (15). D’Angelo et al reported results of a multicenter, open-label, non-comparative, randomized, phase 2 study (Alliance A091401) which evaluated the activity and safety of nivolumab alone or in combination with ipilimumab (anti-CTLA-4) in patients with locally advanced, unresectable, or metastatic STS and bone sarcoma (3). Interestingly, in contrast to the SARC028 cohort, single agent nivolumab in the Alliance study was associated with only a 5% objective response rate (2 of 38 patients). Although a higher response rate was seen among patients who received combination nivolumab (3mg/kg) and ipilimumab (1mg/kg) vs. nivolumab alone (16% vs 5%), there was also a higher rate of serious treatment-related adverse events (26% vs 19%).
Although sarcomas are generally not considered to be highly immunogenic tumors and typically have low mutational burden (but are often characterized by prominent copy number variations and chromosomal rearrangements) (16,20), the promising clinical results of SARC028 and other studies have led to a burgeoning field of investigation into sarcoma immune-oncology (4). A limited number of studies have now begun to examine the baseline sarcoma immune microenvironment to characterize these tumors at baseline (21–30). Such studies have, to date, been largely retrospective with some studies reporting worse patient outcomes associated with tumor PD-L1 expression (21,26), others reporting better patient outcomes associated tumor PD-L1 expression (24), and yet other studies reporting no association between patient survival and tumor PD-L1 expression (25). In 2017, Pollack et al reported their results of a study of sarcoma FFPE samples from 81 patients with metastatic sarcoma across multiple histologies in which they examined gene expression, PD-1 and PDL-1 expression by IHC, and T-cell receptor Vβ gene sequencing (23). They observed that UPS tumors had higher levels of PD-L1 and PD-1 expression on IHC as well as the highest T-cell infiltration based on T-cell receptor sequencing. These results suggest and support the observation in SARC028 that UPS may be associated with immunologic features that are more responsive to treatment with immune checkpoint inhibitors.
Currently, the heterogeneous objective response to immune checkpoint therapy seen across these studies and across histologies is poorly understood. As described above, published and ongoing studies have largely focused on describing the sarcoma-associated immune microenvironment at baseline and significant work remains to be done towards enhancing our understanding of the biology underlying the heterogeneous response to immune checkpoint blockade observed across sarcoma histologies and between patients with the same histology. Empirically some histologic subtypes such as UPS, alveolar soft part sarcoma, and angiosarcoma of the scalp appear to have particular sensitivity to immunotherapy and there is a limited but important body of published literature examining the tumor immune infiltrates in patients with these histologies who have responded to immunotherapy (31,32). Interestingly, in the current study, patients who achieved an objective response to pembrolizumab had a higher density of tumor-associated immune infiltrates at baseline, including most subtypes of T lymphocytes examined. Responders exhibited increased tumor-infiltrating Tregs [(CD3+ FOXP3+) – (CD3+ CD8+ FOXP3+)] compared to nonresponders, both with respect to absolute density of Tregs and Tregs as a percentage of tumor-infiltrating T cells. Although a high density of tumor-infiltrating FOXP3+ Tregs have been associated with poor outcomes in various solid tumors, others have reported the converse (33,34). Responders also exhibited higher tumor-associated numbers of macrophages (CD68+) and, in particular, PD-L1 expressing macrophages compared to nonresponders. Macrophages are known to be quite plastic and able to acquire distinct functional phenotypes depending on environmental cues. The mechanistic role of the TAMs across tumor types is incompletely understood and it is important to note that although CD68 was used as a marker for macrophages in this study, this does not distinguish between M1 and M2 phenotypes, typically and often too simplistically considered to be “anti-tumoral” and “pro-tumoral,” respectively (35,36). Additionally, whether TAMs are truly synonymous with M1 and M2 macrophages remains unclear.
These data suggest that a subpopulation of patients with soft tissue sarcoma may derive significant benefit from immunotherapy, although greater work is required to predict which patients should be selected for future immunotherapy trials. To date, various assays have been used across tumor types to assess pretreatment tumor tissue. These include IHC and associated scoring systems such as combined positive score (37), multiplex IHC/IF, tumor mutational burden, and gene expression profiling including Nanostring signatures (38,39). The predictive performance of each of these modalities to predict response to immunotherapy is yet to be established and will also depend on specific tumor type/histology. As the sarcoma community gains increased experience treating patients with immunotherapies, future work should include development and validation of an IHC-based signature that, alone or in combination with other tumor analytic approaches, can reliably predict tumor response to immunotherapy and impact patient outcomes as a valuable clinical decision-making tool in this highly heterogeneous but individually rare group of malignancies.
There is also growing interest in identifying novel treatment approaches and rational combination therapies that might enhance sarcoma immunogenicity and augment response to immunotherapies. For instance, there are numerous ongoing preclinical studies and active clinical trials to evaluate combining radiation therapy with immune checkpoint blockade (7). The abscopal effect, in which local irradiation results in a systemic immune response leading to regression of distant tumors outside the radiation field, has been reported in preclinical studies and uncommonly in clinical practice, and provides rationale for combining radiation therapy and immune checkpoint therapy (40–42). There has also been recent work describing increased tumor-associated immune cell infiltrate following radiation treatment of STS (22,41).
Limitations of this study include our small sample size and the small quantities of evaluable tumor specimens given that most of the samples were core needle biopsies from metastatic lesions, despite protocol-mandated tumor biopsies. Difficulties in the analysis included the presence of extensive necrotic tumor tissue in both the baseline and on-treatment tumor specimens. Five patients who responded to pembrolizumab did not have matched tumor biopsies (baseline, on-treatment) available for analysis, limiting our ability to observe changes in the sarcoma immune microenvironment in response to pembrolizumab that may have correlated with tumor response.
The introduction of immunotherapy has led to a revolution in the multimodality treatment of advanced, unresectable, and metastatic malignancies across cancer types. There is now considerable interest in evaluating immune checkpoint blockade for patients with STS and bone sarcomas. Although the 40% and 20% objective response rates to pembrolizumab in patients with advanced UPS and DDLPS, respectively, observed in the SARC028 multicenter phase II clinical trial are encouraging, our ability to anticipate and select patients who will benefit from immune checkpoint blockade and who may also develop immune related adverse events remains poor. Our study suggests that there are features of the sarcoma-associated immune microenvironment which may correlate with response to immune checkpoint therapy and that these may include greater TAM and tumor PD-L1 expression and greater density of tumor immune cell infiltrates at baseline. Future work to confirm the activity of pembrolizumab in the expansion cohort of patients with UPS and DDLPS is ongoing.
Supplementary Material
Translational Relevance.
SARC028 is one of the first clinical trials of immune checkpoint blockade (ICB) in soft tissue and bone sarcomas and in which 17.5% of patients with advanced sarcoma receiving pembrolizumab monotherapy demonstrated objective RECIST response. We performed the first study to comprehensively characterize the tumor-associated immune infiltrate in advanced sarcoma using multiplex immunofluorescence (mIF) in order to elucidate changes induced upon treatment with pembrolizumab, and identify predictors of response or resistance to ICB. Our findings suggest that multiple cell types present at the start of treatment may correlate with sarcoma response to pembrolizumab and improved outcomes. Efforts to confirm the activity of pembrolizumab and these correlative findings in an expansion cohort of patients are underway. Development and validation of a mIF-based signature will afford a valuable clinical decision-making tool to predict response to immunotherapy, advance patient care and improve outcomes in this highly heterogeneous and poorly understood group of malignancies.
Acknowledgements:
This study was funded by the Sarcoma Alliance for Research through Collaboration, Pittsburgh Cure Sarcoma, Merck, and The University of Texas MD Anderson Cancer Center (H. Tawbi). E. Keung was supported by National Institutes of Health (NIH) grant T32 CA009599. We thank the patients and their families, the investigators, and participating study teams.
Financial support:
This study was funded by the Sarcoma Alliance for Research through Collaboration, Pittsburgh Cure Sarcoma, Merck, and The University of Texas MD Anderson Cancer Center (H. Tawbi). E. Keung was supported by National Institutes of Health (NIH) grant T32 CA009599.
Abbreviations:
- CT
computed tomography
- DDLPS
dedifferentiated liposarcoma
- FFPE
formalin-fixed paraffin-embedded
- IHC
immunohistochemistry
- IF
immunofluorescence
- mIF
multiplex immunofluorescence
- MRI
magnetic resonance imaging
- OS
overall survival
- PFS
progression-free survival
- QC
quality control
- RECIST
Response Evaluation Criteria In Solid Tumors
- STS
soft tissue sarcoma
- TAMs
tumor-associated macrophages
- UPS
undifferentiated pleomorphic sarcoma
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 66:7–30. [DOI] [PubMed] [Google Scholar]
- 2.Brennan MF, Antonescu CR, Moraco N, Singer S. Lessons learned from the study of 10,000 patients with soft tissue sarcoma. Ann Surg. 2014;260:416–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D’Angelo SP, Mahoney MR, Van Tine BA, Atkins J, Milhem MM, Jahagirdar BN, et al. Nivolumab with or without ipilimumab treatment for metastatic sarcoma (Alliance A091401): two open-label, non-comparative, randomised, phase 2 trials. Lancet Oncol. Elsevier Ltd; 2018;19:416–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pollack SM, Ingham M, Spraker MB, Schwartz GK. Emerging targeted and immune-based therapies in sarcoma. J Clin Oncol. 2018;36:125–35. [DOI] [PubMed] [Google Scholar]
- 5.Nathenson MJ, Conley AP, Sausville E. Immunotherapy: A new (and old) approach to treatment of soft tissue and bone sarcomas. Oncologist. 2018;23:71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keung EZ, Ukponmwan EU, Cogdill AP, Wargo JA. The rationale and emerging use of neoadjuvant immune checkpoint blockade for solid malignancies. Ann Surg Oncol. 2018;25:1814–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wisdom AJ, Mowery YM, Riedel RF, Kirsch DG. Rationale and emerging strategies for immune checkpoint blockade in soft tissue sarcoma. Cancer. 2018;124:3819–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tawbi HA, Burgess M, Bolejack V, Van Tine BA, Schuetze SM, Hu J, et al. Pembrolizumab in advanced soft-tissue sarcoma and bone sarcoma (SARC028): a multicentre, two-cohort, single-arm, open-label, phase 2 trial. Lancet Oncol. 2017;18:1493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Groisberg R, Hong DS, Behrang A, Hess K, Janku F, Piha-Paul S, et al. Characteristics and outcomes of patients with advanced sarcoma enrolled in early phase immunotherapy trials. J Immunother cancer. 2017;5:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dallos M, Tap WD, D’Angelo SP. Current status of engineered T-cell therapy for synovial sarcoma. Immunotherapy. 2016;8:1073–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mitsis D, Francescutti V, Skitzki J. Current immunotherapies for sarcoma: Clinical trials and tationale. Sarcoma. 2016;2016:9757219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffman RM, Singh AS, Eilber FC. Potential of immunotherapy for sarcoma. Cancer. 2017;123:1488–9. [DOI] [PubMed] [Google Scholar]
- 13.Ben-Ami E, Barysauskas CM, Solomon S, Tahlil K, Malley R, Hohos M, et al. Immunotherapy with single agent nivolumab for advanced leiomyosarcoma of the uterus: Results of a phase 2 study. Cancer. 2017;123:3285–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paoluzzi L, Cacavio A, Ghesani M, Karambelkar A, Rapkiewicz A, Weber J, et al. Response to anti-PD1 therapy with nivolumab in metastatic sarcomas. Clin Sarcoma Res. 2016;6:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toulmonde M, Penel N, Adam J, Chevreau C, Blay JY, Le Cesne A, et al. Use of PD-1 targeting, macrophage infiltration, and IDO pathway activation in sarcomas a phase 2 clinical trial. JAMA Oncol. 2018;4:93–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cancer Genome Atlas Research Network. Comprehensive and integrated genomic characterization of adult soft tissue sarcomas. Cell. 2017;171:950–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parra ER, Villalobos P, Mino B, Rodriguez-Canales J. Comparison of different antibody clones for immunohistochemistry detection of programmed cell death ligand 1 (PD-L1) on non-small cell lung carcinoma. Appl Immunohistochem Mol Morphol. 2018;26:83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parra ER, Uraoka N, Jiang M, Cook P, Gibbons D, Forget M-A, et al. Validation of multiplex immunofluorescence panels using multispectral microscopy for immune-profiling of formalin-fixed and paraffin-embedded human tumor tissues. Sci Rep. 2017;7:13380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wei SC, Levine JH, Cogdill AP, Zhao Y, Anang N-AAS, Andrews MC, et al. Distinct cellular mechanisms underlie anti-CTLA-4 and anti-PD-1 checkpoint blockade. Cell. 2017;170:1120–1133.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawrence MS, Stojanov P, Polak P, Kryukov G V, Cibulskis K, Sivachenko A, et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 2013;499:214–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim C, Kim EK, Jung H, Chon HJ, Han JW, Shin K-H, et al. Prognostic implications of PD-L1 expression in patients with soft tissue sarcoma. BMC Cancer. 2016;16:434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keung EZ, Tsai J-W, Ali AM, Cormier JN, Bishop AJ, Guadagnolo BA, et al. Analysis of the immune infiltrate in undifferentiated pleomorphic sarcoma of the extremity and trunk in response to radiotherapy: Rationale for combination neoadjuvant immune checkpoint inhibition and radiotherapy. Oncoimmunology. 2018;7:e1385689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pollack SM, He Q, Yearley JH, Emerson R, Vignali M, Zhang Y, et al. T-cell infiltration and clonality correlate with programmed cell death protein 1 and programmed death-ligand 1 expression in patients with soft tissue sarcomas. Cancer. 2017;1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boxberg M, Steiger K, Lenze U, Rechl H, von Eisenhart-Rothe R, Wörtler K, et al. PD-L1 and PD-1 and characterization of tumor-infiltrating lymphocytes in high grade sarcomas of soft tissue - prognostic implications and rationale for immunotherapy. Oncoimmunology. 2018;7:e1389366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.D’Angelo SP, Shoushtari AN, Agaram NP, Kuk D, Qin L, Carvajal RD, et al. Prevalence of tumor-infiltrating lymphocytes and PD-L1 expression in the soft tissue sarcoma. Hum Pathol. 2015;46:357–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bertucci F, Finetti P, Perrot D, Leroux A, Collin F, Le Cesne A, et al. PDL1 expression is a poor-prognosis factor in soft-tissue sarcomas. Oncoimmunology. 2017;6:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nowicki TS, Akiyama R, Huang RR, Shintaku IP, Wang X, Tumeh PC, et al. Infiltration of CD8 T cells and expression of PD-1 and PD-L1 in synovial sarcoma. Cancer Immunol Res. 2017;5:118–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kostine M, Cleven AHG, Miranda NFCC De, Italiano A, Bovée JVMG. Analysis of PD-L1, T-cell infiltrate and HLA expression in chondrosarcoma indicates potential for response to immunotherapy specifically in the dedifferentiated subtype. Mod Pathol. 2016;29:1028–37. [DOI] [PubMed] [Google Scholar]
- 29.Schilham MW, Marie A, Jansen C. Increased PD‑L1 and T‑cell infiltration in the presence of HLA class I expression in metastatic high‑grade osteosarcoma: a rationale for T‑cell‑based immunotherapy. Cancer Immunol Immunother. 2017;66:119–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Budczies J, Mechtersheimer G, Denkert C, Klauschen F, Mughal SS, Chudasama P, et al. PD-L1 (CD274) copy number gain, expression, and immune cell infiltration as candidate predictors for response to immune checkpoint inhibitors in soft-tissue sarcoma. Oncoimmunology. 2017;6:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Florou V, Rosenberg AE, Wieder E, Komanduri K V, Kolonias D, Uduman M, et al. Angiosarcoma patients treated with immune checkpoint inhibitors: a case series of seven patients from a single institution. J Immunother cancer. 2019;7:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wilky BA, Trucco MM, Subhawong TK, Florou V, Park W, Kwon D, et al. Axitinib plus pembrolizumab in patients with advanced sarcomas including alveolar soft-part sarcoma: a single-centre, single-arm, phase 2 trial. Lancet Oncol. 2019;20:837–48. [DOI] [PubMed] [Google Scholar]
- 33.Salama P, Phillips M, Grieu F, Morris M, Zeps N, Joseph D, et al. Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J Clin Oncol. 2009;27:186–92. [DOI] [PubMed] [Google Scholar]
- 34.Badoual C, Hans S, Rodriguez J, Peyrard S, Klein C, Agueznay NEH, et al. Prognostic value of tumor-infiltrating CD4+ T-cell subpopulations in head and neck cancers. Clin Cancer Res. 2006;12:465–72. [DOI] [PubMed] [Google Scholar]
- 35.Petty AJ, Yang Y. Tumor-associated macrophages: implications in cancer immunotherapy. Immunotherapy. 2017;9:289–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bercovici N, Guérin M V, Trautmann A, Donnadieu E. The remarkable plasticity of macrophages: A chance to fight cancer. Front Immunol. 2019;10:1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kulangara K, Zhang N, Corigliano E, Guerrero L, Waldroup S, Jaiswal D, et al. Clinical utility of the combined positive score for programmed death ligand-1 expression and the approval of pembrolizumab for treatment of gastric cancer. Arch Pathol Lab Med. 2019;143:330–7. [DOI] [PubMed] [Google Scholar]
- 38.Lu S, Stein JE, Rimm DL, Wang DW, Bell JM, Johnson DB, et al. Comparison of biomarker modalities for predicting response to PD-1/PD-L1 checkpoint blockade: A systematic review and meta-analysis. JAMA Oncol. 2019;5:1195–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Petitprez F, de Reynies A, Keung EZ, Chen T, Sun C, Calderaro J, et al. B cells are associated with sarcoma survival and immunotherapy response. Nature. 2019;In press. [DOI] [PubMed] [Google Scholar]
- 40.Sharma A, Bode B, Wenger RH, Lehmann K, Sartori AA, Moch H, et al. γ−Radiation promotes immunological recognition of cancer cells through increased expression of cancer-testis antigens in vitro and in vivo. PLoS One. 2011;6:e28217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharma A, Bode B, Studer G, Moch H, Okoniewski M, Knuth A, et al. Radiotherapy of human sarcoma promotes an intratumoral immune effector signature. Clin Cancer Res. 2013;19:4843–53. [DOI] [PubMed] [Google Scholar]
- 42.Demaria S, Golden EB, Formenti SC. Role of local radiation therapy in cancer immunotherapy. JAMA Oncol. 2015;1:1325–1332. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.