Summary
Since the initial report of coronavirus disease (COVID-19) from the City of Wuhan, China in December 2019, there have been multiple cases globally. Reported here are 11 cases of COVID-19 at this hospital; all of the patients in question presented with relative bradycardia. The severity of the disease was classified into four grades. Of the patients studied, 3 with mild COVID-19 and 3 with moderate COVID-19 improved spontaneously. Lopinavir/ ritonavir was administered to 3 patients with severe COVID-19 and 2 with critical COVID-19. Both patients with critical COVID-19 required mechanical ventilation and extracorporeal membrane oxygenation. Both patients with critical COVID-19 had a higher fever that persisted for longer than patients with milder COVID-19. The respiratory status of patients with critical COVID-19 worsened rapidly 7 days after the onset of symptoms. Relative bradycardia may be useful in distinguishing between COVID-19 and bacterial community-acquired pneumonia. In patients who have had a fever for > 7 days, the condition might worsen suddenly.
Keywords: COVID-19, SARS-CoV-2, pneumonia
Introduction
Since the initial reports of coronavirus disease (COVID-19) infection from the City of Wuhan, China in December 2019, there have been multiple cases globally. As of May 1, 2020, there were 3,175,207 confirmed cases worldwide. Japan has reported 14,545 cases, and the number continues to increase.
The mortality rate of COVID-19 is reported to be 2.3% (1). The number of severe cases will increase as the number of patients who contract the disease increases. At present, most case reports are from China, and there is a lack of detailed reports from Japan. A better understanding of the clinical profile will help improve the treatment and prevention of COVID-19.
The aim of this report was to describe the clinical characteristics of 11 patients with COVID-19 at this hospital.
Patients and Methods
This study was approved by the ethics committee of the National Center for Global Health and Medicine (NCGM) (approval no. NCGM-G-003472-02) and conducted in accordance with the Declaration of Helsinki. Patient information was anonymized and de-identified prior to analysis. Because of the retrospective nature of the study, the requirement for patient consent was waived.
A retrospective cohort study of patients with COVID-19 was conducted between January 2020 and February 2020 at the NCGM, Tokyo, Japan. This center has approximately 780 hospital beds. All patients were admitted through the NCGM referral center for infectious disease from January 26, 2020 to February 13, 2020.
The following information was collected from the patient charts: i) characteristics and comorbidities; ii) symptoms, body temperature, heart rate, oxygen demand, treatment, and use of a respirator and extracorporeal membrane oxygenation (ECMO); and iii) 30-day mortality.
The severity of COVID-19 was classified into 4 grades. Upper respiratory symptoms without pneumonia were graded as mild. Pneumonia requiring no supplemental oxygen was graded as moderate, whereas the requirement for supplemental oxygen was graded as severe. The requirement for intensive care, including mechanical ventilation, was graded as critical. A body temperature > 37.5°C was defined as a "fever". "Abatement of a fever" was defined as the absence of a fever for > 48 h. The "duration of fever" was calculated as the day when the body temperature first reached ≥ 37.5°C to the day when the body temperature finally dropped to ≤ 37.5°C. "Relative bradycardia" was determined based on the definition of Cunha et al. (2). Given the difference between axillary temperature and oral temperature, body temperature was calculated by adding 0.3°C (0.5°F) to the axillary temperature (3). The values of continuous variables are expressed as the median and range.
Results and Discussion
A total of 11 patients with COVID-19 were examined in this study. Median (range) age was 54 years (28-83), and 4 patients (36.4%) were female. One patient (9.1%) had diabetes mellitus, 1 (9.1%) had prostate cancer, 1 (9.1%) had bradycardia, 1 (9.1%) had Alzheimer's dementia, and no patients had pulmonary disease (Table 1).
Table 1. Characteristics of patients with COVID-19.
| Items | Mild, n = 3 | Moderate, n = 3 | Severe, n = 3 | Critical, n = 2 |
|---|---|---|---|---|
| Age (range) | 64 (28-70) | 52 (41-54) | 50 (33-83) | 78.5 (74-83) |
| Female (%) | 2 (66.7) | 0 (0) | 2 (66.7) | 0 (0) |
| BMI (range) | 27.2 (23.0-28.5) | 23.5 (21.8-24.7) | 25.5 (23.3-25.7) | 25.2 (24.8-25.6) |
| Comorbidity | ||||
| Pulmonary disease (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Neurologic disease (%) | 1 (33.3) | 0 (0) | 0 (0) | 0 (0) |
| Cardiovascular disease (%) | 0 (0) | 0 (0) | 0 (0) | 1 (50.0) |
| Malignancy (%) | 1 (33.3) | 0 (0) | 0 (0) | 0 (0) |
| Diabetes (%) | 0 (0) | 0 (0) | 0 (0) | 1 (50.0) |
The most common symptom among all of the patients was a fever (9 patients, 81.8%), followed by a sore throat (4 patients, 36.4%), cough (4 patients, 36.4%), and dyspnea (4 patients, 36.4%). The median duration of fever (range) was 6 days (0-31), and the 30- day mortality was 1 (9.1%) (Table 2). The relationship between body temperature and pulse is shown in Figure 1. Relative bradycardia was confirmed in almost all of the patients.
Table 2. Symptoms, treatment, and outcomes for patients with COVID-19.
| Items | Mild, n = 3 | Moderate, n = 3 | Severe, n = 3 | Critical, n = 2 | Total, n = 11 |
|---|---|---|---|---|---|
| Symptom | |||||
| Fever (%) | 2 (66.7) | 3 (100) | 2 (66.7) | 2 (100) | 9 (81,8) |
| Sore throat (%) | 0 (0) | 2 (66.7) | 2 (66.7) | 0 (0) | 4 (36.4) |
| Cough (%) | 0 (0) | 1 (33.3) | 2 (66.7) | 1 (50) | 4 (36.4) |
| Dyspnea (%) | 0 (0) | 1 (33.3) | 1 (33.3) | 2 (100) | 4 (36.4) |
| Runny nose (%) | 1 (33.3) | 1 (33.3) | 0 (0) | 1 (50) | 3 (27.3) |
| Phlegm (%) | 0 (0) | 0 (0) | 2 (66.7) | 1 (50) | 3 (27.3) |
| Nausea (%) | 0 (0) | 1 (33.3) | 1 (33.3) | 1 (50) | 3 (27.3) |
| Malaise (%) | 0 (0) | 1 (33.3) | 1 (33.3) | 1 (50) | 3 (27.3) |
| Headache (%) | 0 (0) | 0 (0) | 1 (33.3) | 0 (0) | 1 (9.1) |
| Chills (%) | 0 (0) | 0 (0) | 1 (33.3) | 0 (0) | 1 (9.1) |
| Diarrhea (%) | 0 (0) | 0 (0) | 1 (33.3) | 0 (0) | 1 (9.1) |
| Abdominal bloating (%) | 0 (0) | 0 (0) | 1 (33.3) | 0 (0) | 1 (9.1) |
| Treatment | |||||
| Oxygen (%) | 0 (0) | 0 (0) | 3 (100) | 2 (100) | 5 (45.5) |
| LPV/r (%) | 0 (0) | 0 (0) | 3 (100) | 2 (100) | 5 (45.5) |
| Mechanical ventilation (%) | 0 (0) | 0 (0) | 0 (0) | 2 (100) | 2 (18.2) |
| ECMO (%) | 0 (0) | 0 (0) | 0 (0) | 2 (100) | 2 (18.2) |
| Steroid (%) | 0 (0) | 0 (0) | 1 (33.3) | 2 (100) | 3 (27.3) |
| Interferon α2a (%) | 0 (0) | 0 (0) | 0 (0) | 1 (50) | 1 (9.1) |
| Duration of fever (range) | 2 (0-5) | 6 (1-12) | 6 (6-19) | 23.5 (16-31) | 6 (0-31) |
| 30-day mortality | 0 (0) | 0 (0) | 0 (0) | 1 (50) | 1 (9.1) |
LPV/r, lopinavir/ritonavir; ECMO, extracorporeal membrane oxygenation.
Figure 1.
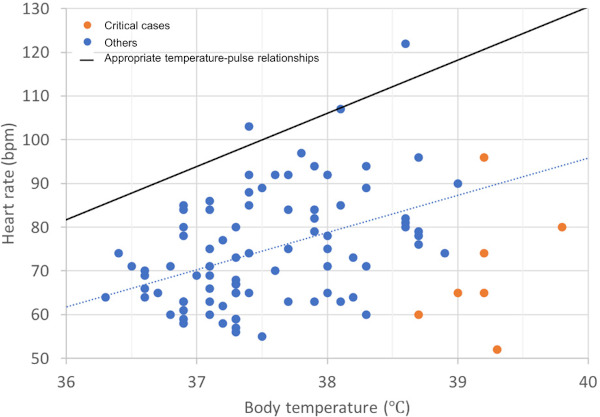
Scatter plot of heart rate and body temperature for all patients. All of the patients with COVID-19 displayed relative bradycardia. Patients with critical COVID-19 tended to have a higher fever than those with less severe COVID-19.
Patients were categorized into 4 groups: i) 3 with mild COVID-19; ii) 3 with moderate COVID-19; iii) 3 with severe COVID-19, and iv) 2 with critical COVID-19. All 5 of the patients with severe or critical COVID-19 received lopinavir/ritonavir (LPV/r). The 2 patients with critical COVID-19 both required mechanical ventilation as well as ECMO. Patients with critical COVID-19 tended to have a fever for a longer period than patients with less severe COVID-19 (23.5 days [16-31] vs. 6 days [0-19]). Patients with critical COVID-19 presented with a higher body temperature than patients with mild-severe COVID-19 (39.0°C [38.4-39.8°C] vs. 37.1°C [36.0-38.7°C]). Progress charts for patients with critical COVID-19 are shown in Figure 2. In both cases, respiratory status deteriorated rapidly on days 9-10, and the patient had to be intubated.
Figure 2.
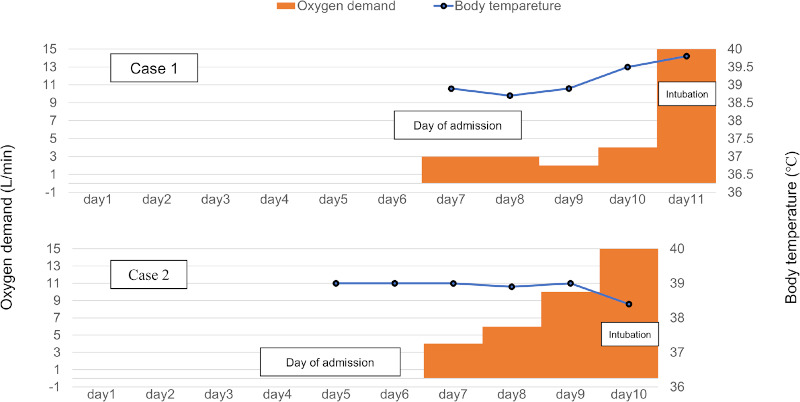
Progress charts for patients with critical COVID-19. Shown here are progress charts for 2 patients with critical COVID-19. They had a high fever for over 7 days and their respiratory status rapidly deteriorated.
Based on an analysis of 11 patients with COVID-19, an important finding is that almost all of the patients exhibited relative bradycardia. According to Cunha et al., relative bradycardia is a finding reported in intracellular parasite infections, such as typhoid fever and mycoplasma pneumonia, and viral diseases, such as dengue fever. Since COVID-19 is also a viral disease caused by the severe acute respiratory syndrome coronavirus 2, detection of relative bradycardia is not surprising (2). Relative bradycardia may be useful in distinguishing COVID-19 from bacterial community-acquired pneumonia.
COVID-19 has a wide range of clinical presentation, from asymptomatic or mildly symptomatic patients to those requiring intensive care (4,5). The current study classified the severity of the disease into 4 grades. COVID-19 needed to be classified into 4 grades of severity and different treatment plans needed to be devised for each. In patients with mild to severe COVID-19, fever resolved within 7 days, whereas in patients with critical COVID-19, respiratory status deteriorated rapidly after day 7, and a ventilator was needed. Patients with critical COVID-19 had a markedly higher body temperature than patients with less severe COVID-19 (Figure 2). This finding is consistent with a previous study reporting that the period from onset to development of acute respiratory distress syndrome takes approximately 8 days (6). According to a study by Pan et al., computed tomography (CT) scans revealed the most deterioration on day 10 after the onset of COVID-19 (6). Risk factors for mortality include being elderly, a decreased lymphocyte count, X-ray findings of diffuse patchy/interstitial lung opacities, and comorbidities, such as heart disease, diabetes mellitus, chronic lung disease, hypertension, or malignancy, high SOFA score, and high d-dimer (6-8). The condition of patients with risk factors for mortality and a fever for > 7 days may worsen suddenly. Therefore, strict monitoring and a prompt transition to supportive care, such as mechanical ventilation or ECMO, are required.
The current study had several limitations. First, it only included 11 patients for the sake of time. Nonetheless, the number of patients with COVID-19 is increasing daily, and additional cases will need to be studied in the future. Second, this was a retrospective study, and treatment strategies varied. All of the patients with severe or critical COVID-19 received LPV/r, but some patients also received steroids and interferon alpha. These differences may have affected the severity of the disease. A prospective study needs to be conducted in the future.
In conclusion, relative bradycardia may be useful in distinguishing COVID-19 from bacterial community-acquired pneumonia. COVID-19 can be classified into 4 grades of severity. The condition of patients presenting with a fever for > 7 days may worsen suddenly.
Acknowledgements
The authors wish to thank the staff at the National Center for Global Health and Medicine, and especially those involved in providing care to patients.
References
- 1. Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020; 41:145-151. (in Chinese). [DOI] [PubMed] [Google Scholar]
- 2. Cunha BA. The diagnostic significance of relative bradycardia in infectious disease. Clin Microbiol Infect. 2000; 6:633-634. [DOI] [PubMed] [Google Scholar]
- 3. Singh V, Sharma A, Khandelwal R, Kothari K. Variation of axillary temperature and its correlation with oral temperature. J Assoc Physicians India. 2000; 48:898-900. [PubMed] [Google Scholar]
- 4. Hu Z, Song C, Xu C, Jin G, Chen Y, Xu X, Ma H, Chen W, Lin Y, Zheng Y, Wang J, Hu Z, Yi Y, Shen H. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020; 63:706-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guo G, Ye L, Pan K, Chen Y, Xing D, Yan K, Chen Z, Ding N, Li W, Huang H, Zhang L, Li X, Xue X. New insights of emerging SARS-CoV-2: epidemiology, etiology, clinical features, clinical treatment, and prevention. Front Cell Dev Biol. 2020; 8:1-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323:1061-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020; 295:715-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395:1054-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]


