Summary
Lagos State, Nigeria, Africa's largest city with an estimaed 21 million population, continues to face challenges in its attempts to reduce maternal mortality (555 deaths per 100,000 live births) and deaths of children under five (59 per 1,000 live births). These deaths are more common among women and children living in poverty, many of whom rarely utilize health services. This paper describes the trend in the use of maternal, neonatal and child health (MNCH) services in the State in the past decade and shows barriers to the use of the services. Significant improvement in the coverage of the services were not observed. We identified the following five types of barriers to the use of MNCH services: i) financial barriers, ii) physical barriers, iii) cognitive barriers, iv) organizational barriers, and v) psychological and socio-cultural barriers. To address these interrelated barriers, the Lagos State Ministry of Health should prioritize regular outreach health services including health promotion, and realize the current initiative for massive recruitment of health personnel and appropriate deployment of them.
Keywords: health seeking behaviour, barriers to health services, qualitative study, Nigeria
Introduction
Despite the currently reported global decreases in maternal deaths (1) and deaths of children under five (2), certain regions of the world are still struggling to reduce their local rates of maternal and early childhood death. Developing countries account for 99% of global maternal deaths (1) and under-five deaths (2). Sub- Saharan Africa alone accounts for 62% of global maternal deaths (1) and 50% of global under-five deaths (2). At the country level, India and Nigeria together were estimated to account for one-third of all maternal (1) and under-five deaths worldwide in 2013 (2).
In Lagos State, Nigeria, Africa's largest city with an estimaed 21 million population, the maternal mortality ratio (MMR) remained high at 555 per 100,000 live births according to the latest data available as of 2020 (3). Change in the MMR in the State in the past decade is not known yet. At the national level, the MMR in 2018 was almost the same as in 2008 as the MMR confidence intervals (CIs) overlap for the 2008 and 2018 surveys (4,5). The under-five mortality rates (U5MRs) in the State in 2011 and 2018 were 65 (6) (no CI available) and 59 (CI: 46-73) (5) per 1,000 live births, respectively. Significant improvement in the U5MR in the State was not observed during the period, either. These figures widely range across the Local Gernment Areas (LGAs) within the State (3). A recent cross-sectional study conducted in slum areas in the State shows high MMR at 1,050 per 100,000 live births and U5MR at 103 (7).
This paper aims i) to describe trend in utilization of maternal, neonatal and child health services in Lagos State in the past decade, ii) to show barriers to utilization of the services identified in our previous study, and iii) to discuss policy implications.
Trend in the utilization of maternal, neonatal and child health services in Lagos State
Table 1 shows trend in the utilization of maternal, newborn and child health (MNCH) services in Lagos State. The proportion of deliveries in health facilities in the State has been relatively high at 79% between 2011 and 2017 (6,8). Percentages of women and births with a postnatal check in the first two days after birth decreased and increased between 2013 (9) and 2018 (5), respectively. Yet, as CIs are not available for the indicators, it is unclear that the changes are statistically significant. The same applies to immunization coverage although it increased by 8.5% during the same period. It should be noted that there are large inequities in regard to the coverage of MNCH services across wealth quintiles. This is likely one reason why more maternal and under-five deaths in the State occur among women and children living in poor conditions, as has also been observed globally (10). The majority of these deaths are preventable through services available at the primary healthcare level. Given that the public primary health centres (PHCs) provide free or relatively inexpensive health services, it would be beneficial for the poor to utilize the MNCH services available at the PHCs.
Table 1. Trend in the utilization of maternal, newborn and child health services in Lagos State.
| Type of services | 2011 (%) (Ref. 6) | 2013 (%) (Ref. 9) | 2017 (%) (Ref. 8) | 2018 (%) (Ref. 5) |
|---|---|---|---|---|
| Delivery in health facility | 79.3 | 79.5 | ||
| Poorest | 68.1 | |||
| Poor | 69.7 | |||
| Middle | 80.2 | |||
| Rich | 86.7 | |||
| Richest | 93.1 | |||
| Postnatal checkup for mothers | 83.9 | 72.8 | ||
| Postnatal checkup for newborns | 57.9 | 79.8 | 66.8 | |
| Poorest | 65.8 | |||
| Poor | 71.1 | |||
| Middle | 80.7 | |||
| Rich | 90.6 | |||
| Richest | 89.5 | |||
| Immunization | 53.9 | 63.2 | 62.4 | |
| Poorest | 49.8 | |||
| Poor | 57.0 | |||
| Middle | 58.2 | |||
| Rich | 80.4 | |||
| Richest | 83.0 |
In view of the current low rates of MNCH access, it is worth identifying barriers to the utilization of the services among the poor. A quantitative study is not typically designed to provide insights into the underlying causes of non-use of services. Qualitative data are helpful to interpret the underlying causes of the limited use of MNCH services in the State.
Barriers to utilization of MNCH services in Lagos State
We conducted a qualitative study in four deliberately selected slum settlements in Lagos State in December 2014. Data was collected through 24 semi-structured interviews (12 males and 12 females) and seven focus group discussions (15 males and 20 females). The qualitative data obtained were coded and categorized. We identified the following five types of barriers to the use of MNCH services: i) financial barriers, ii) physical barriers, iii) cognitive barriers, iv) organizational barriers, and v) psychological and socio-cultural barriers. To understand the underlying barriers, the authors mapped out them by confirming the linkages between them (Figure 1), which could contribute to the lower use of services.
Figure 1.
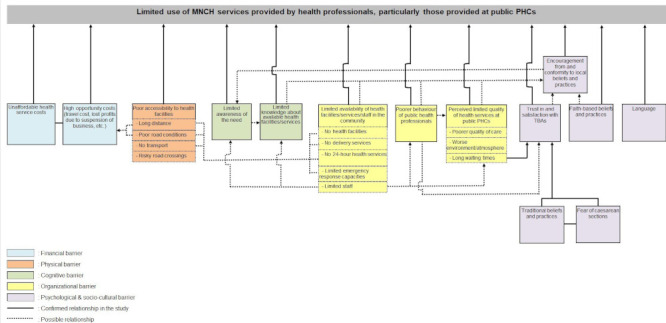
Barrires to use of MNCH services and interactions amongst the barriers.
Financial barriers
Starting from the left of Figure 1, "Unaffordable health service costs" is related to "High opportunity costs" such as travel cost and lost profits due to suspension of business.
Physical barriers
Regarding "Poor accessibility to health facilities", due to the limited number of pedestrian bridges over major roads in the study area, some people choose not to visit a public PHC on the other side of a major road due to the "risky road crossing".
Cognitive barriers
When women and caregivers are not aware of the need for MNCH services (Limited awareness of the need), they may not notice the availability of health facilities and services in their community (Limited knowledge about health facilities/services available).
Organizational barriers
"Limited availability of health facilities/services/staff in the community" is an obvious barrier to the use of MNCH services. Even when services are available at health facilities, however, the issue of "Limited staff" may prevent facilities from attending to their many clients in a friendly and attentive manner (Poorer behaviour of public health professionals) and also leads to "Long waiting times". "Limited staff" at public PHCs also prevents staff from taking the time to conduct regular outreach health activities. Therefore, the issue of "Limited staff" could be an underlying cause of "Limited awareness of the need" and "Limited knowledge about available health facilities/services". In Lagos State, health professionals are in short supply and unevenly distributed. It is estimated that the majority of doctors and nurses/midwives in public and private health facilities in the State work for higher level health facilities (i.e. secondary and tertiary hospitals) (3). The scarcity of community health extension workers (CHEWs) is an additional critical issue. CHEWs are crucial in increasing the use of and demand for health services.
"Poorer behaviour of public health professionals" could downgrade the perceived value of public PHCs (Perceived limited quality of health services at public PHCs), which could discourage people from using the PHCs again. Our data also showed that "Long waiting times" contribute to the preference for traditional birth attendants (TBAs) (Trust in and satisfaction with TBAs), which could also be partially attributable to "Poorer behaviour of public health professionals".
Respondents tended to perceive the limited types of medical equipment and numbers of drugs as an indicator of "Poorer quality of care", regardless of whether a public PHC actually needs a wide variety of equipment and drugs to be effective. They also had the impression that a public PHC has a "Worse environment and atmosphere".
Psychological and socio-cultural barriers
"Traditional beliefs and practices" and "Fear of caesarean sections" are interrelated and seem to be the underlying causes of "Trust in and satisfaction with TBAs".
Since traditional practitioners including TBAs are acquainted with herbal medicines and rituals (Traditional beliefs and practices) in accordance with the needs of the local community, they are recognized as individuals who have an important role to play in ensuring desirable health outcomes (11).
"Fear of caesarean sections" is a specific barrier to the use of facility delivery services. In Nigerian culture, the inability to achieve vaginal delivery is regarded as the failure of a woman's reproductive functions (12).
In Nigeria, faith-based clinics are patronized by many women for maternal health services (Faith-based beliefs and practices) for various reasons such as the desire for spiritual protection against satanic attacks during delivery, lower financial burdens and the harsh attitudes of health professionals (13).
"Encouragement from and conformity to local beliefs and practices" could be attributable to "Limited knowledge about available health facilities/services", all types of organizational barriers, "Trust in and satisfaction with TBAs" and "Faith-based beliefs and practices", as these factors likely shape the opinions of community members on health services provided by health professionals and/or public PHCs. Furthermore, "Encouragement from and conformity to local beliefs and practices" is likely to contribute to "Limited awareness of the need", as people who should seek care may not perceive the need if their neighbours are not aware of the need.
For those who immigrate from outside Lagos State and have difficulty in communicating in Yoruba or English, "Language" is one of the barriers to accessing MNCH services.
Policy discussion
Our analyses pointed to several intervention options that we recommend to the State Ministry of Health.
To address the issus of financial, cognitive and physical barriers, regular outreach health services along with health education and promotion could be an option to enable the poor to receive MNCH services, to be enlightened and to minimize their expenditures in seeking care.
Regarding the issue of "Limited availability of health facilities/services/staff in health facilities", in 2013, Lagos State launched an initiative to establish Comprehensive PHCs in all 57 administrative areas that provide 24-hour health services including those for MNCH (14). The issue of "limited emergency response capacities" is likely to be alleviated once all the Comprehensive PHCs in the State have been renovated. But, only 14 Comprehensive PHCs have been established by 2018 (15). The earlier full-scale State-wide establishment of PHCs is expected. The state government has recently commenced mass recruitment of health personnel (16). We hope that the newly recruited health personnel will be deployed mainly to public PHCs in proportion to the population size to redress the current problematic distribution (17). The State Ministry of Health also recognizes the issue of "Poorer behaviour of public health professionals" and recently provided health workers with training on etiquette (18). To reduce the biased "limited quality of health services at public PHCs", communities need to be informed about the particular kinds of health services that a public PHC is intended to provide. Ward Health Committees (WHCs) (in Lagos State, a Ward Health System has been promoted based on Health Sector Reforms established in 2008, and WHCs have been set up since then) could play leading roles in the education process.
Worldwide, there is disagreement about whether training programmes for TBAs are effective in improving MNCH outcomes (19). Given that TBAs are in great demand in Lagos State, establishing cooperative ties between TBAs and the formal health system would be a better choice, than attempts to discourage the public from using TBAs or demands for substantial improvements in TBAs' midwifery knowledge and skills. Some PHCs in the State have regular meetings with TBAs practising in their catchment areas to share information. Such regular interactions could strengthen the cooperative ties between the health system and TBAs and improve referral rates. In Lagos State, "Traditional practices" such as herbal remedies are likely widely used as seen in other Nigerian states (20). Yet, some herbal medications may cause teratogenic effects to the fetus (21). Assessments of the safety and efficacy of the herbal remedies are needed. Additionally, efforts should be geared towards ensuring that laws are in place in Lagos State that will guide the practice of traditional medicine. To avoid preventable maternal deaths, medically unsuitable "Traditional beliefs" such as the meaning of non-vaginal delivery should be changed through health education. Faith-based clinics are not often properly staffed or well-equipped although they are well patronized. As in the case of TBAs, enhancing collaboration between the health system and "Faith-based" clinics would be an option to improve referral rates. As "Encouragement from and conformity to local beliefs and practices" could be related to various cognitive and psycological and socio-cultural barriers, an approach to health education and promotion that is inclusive of all community members is necessary for MNCH programmes to be successful. To overcome the "Language" barrier, the Lagos State Ministry of Health provides health information in several languages through radio programmes, leaflets and posters, and this should be continued.
Among the intervention options, i) regular outreach health services along with health education and promotion, and ii) realization of the current initiative for massive recruitment of health personnel and appropritae deployment of them should be the top priorities. Because "Traditional beliefs and practices" and "Limited staff" seem to be the underlying causes of multiple barriers.
Acknowledgements
We express our gratitude to Dr. Hidechika Akashi, Dr. Hironori Okabayashi, Mr. Hideaki Masuda, and Mr. Kazuki Miyazaki, from the National Center for Global Health and Medicine (NCGM), Japan, for their intellectual input. We are also grateful to the Japan International Cooperation Agency (JICA) for its financial support for this study conducted as a part of the JICA Project for Strengthening Pro-poor Community Health Services in Lagos State. This work was partly supported by the Grant for NCGM, Japan (28-1).
References
- 1. World Health Organization, United Nations Children's Fund, United Nations Population Fund, World Bank, United Nations Population Division. Trends in maternal mortality: 1990 to 2013. https://apps.who.int/iris/bitstream/handle/10665/112682/9789241507226_eng.pdf;jsessionid=1516E7FC4869746A53303B553714D992?sequence=2 (accessed April 6, 2020).
- 2. United Nations Children's fund, World Health Organization, World Bank, United Nations Population Division. Levels & Trends in Child Mortality Report 2014. https://www.unicef.org/media/files/Levels_and_Trends_in_Child_Mortality_2014.pdf (accessed April 6, 2020).
- 3. Lagos State of Ministry of Health, United Nations Children's Fund. Reducing health disparities in Lagos State: an investment case. Lagos, Nigeria 2012; p.14. [Google Scholar]
- 4. National Population Commission Nigeria, IFC Macro. Nigeria Demographic and Health Survey 2008. https://dhsprogram.com/pubs/pdf/FR222/FR222.pdf (accessed April 6, 2020).
- 5. National Population Commission Nigeria, IFC International. Nigeria Demographic and Health Survey 2018. https://www.dhsprogram.com/pubs/pdf/FR359/FR359.pdf (accessed April 6, 2020).
- 6. National Bureau of Statistics, United Nations Children's fund, United Nations Population Fund. Nigeria Multiple Indicator Cluster Survey 2011. https://www.unicef.org/nigeria/media/1376/file/Nigeria-multiple-indicator-cluster-survey-2011_0.pdf.pdf (accessed April 6, 2020).
- 7. Anastasi E, Ekanem E, Hill O, Adebayo Oluwakemi A, Abayomi O, Bernasconi A. Unmasking inequalities: Sub-national maternal and child mortality data from two urban slums in Lagos, Nigeria tells the story. PloS One. 2017; 12:e0177190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Bureau of Statistics, United Nations Children's fund. Multiple Indicator Cluster Survey 2016-17, Survey Findings Report. https://www.unicef.org/nigeria/media/1406/file/Nigeria-MICS-2016-17.pdf.pdf (accessed April 6, 2020).
- 9. National Population Commission Nigeria, International I. Nigeria Demographic and Health Survey 2013. Abuja, Nigeria, and Rockville, Maryland, USA. 2014. [Google Scholar]
- 10. World Health Organization. Children: reducing mortality. http://www.who.int/mediacentre/factsheets/fs178/en/ (accessed April 25, 2017).
- 11. Adetunji JA. Preserving the pot and water: a traditional concept of reproductive health in a Yoruba community, Nigeria. Soc Sci Med. 1996; 43:1561-1567. [DOI] [PubMed] [Google Scholar]
- 12. Aziken M, Omo-Aghoja L, Okonofua F. Perceptions and attitudes of pregnant women towards caesarean section in urban Nigeria. Acta Obstet Gynecol Scand. 2007; 86:42-47. [DOI] [PubMed] [Google Scholar]
- 13. Udoma EJ, Ekanem AD, Abasiattai AM, Bassey EA. Reasons for preference of delivery in spiritual church-based clinics by women of south-south Nigeria. Niger J Clin Pract. 2008; 11:100-103. [PubMed] [Google Scholar]
- 14. Ogunbiyi T. Lagos Flagship Primary Health Centres Initiative. https://www.pmnewsnigeria.com/2013/07/23/lagos-flagship-primary-health-centres-initiative/ (accessed August 23, 2019).
- 15. Awojobi NO, Tinubu AR. Governor Akinwumi Ambode: A catalyst for good governance in Lagos State, A rapid assessment. Hamburg, Germany: National Youth Council of Nigeria Lagos State Chapter. 2018. [Google Scholar]
- 16. Lagos State Ministry of Health. Lagos embarks on massive recruitment for health sector. https://lagosstate.gov.ng/blog/2020/01/23/lagos-embarks-on-massive-recruitment-for-health-sector-2/ (accesssed March 3, 2020) .
- 17. Matsuoka S, Koga S, Suzui E, Tsukada Y, Ohashi K, Johnson T. Impact assessment of a maternal health project in a megacity, Nigeria: toward a future with more demand for maternal health services. Int J Health Plann Manage. 2017; 32:465-480. [DOI] [PubMed] [Google Scholar]
- 18. Lagos State of Ministry of Health. Lagos trains health workers on attitudinal change. https://health.lagosstate.gov.ng/2019/06/11/lagos-trains-health-workers-on-attitudinal-change/ (accesssed March 3, 2020) .
- 19. Koblinsky MA, Campbell O, Heichelheim J. Organizing delivery care: what works for safe motherhood? Bull World Health Organ. 1999; 77:399-406. [PMC free article] [PubMed] [Google Scholar]
- 20. Fakeye TO, Adisa R, Musa IE. Attitude and use of herbal medicines among pregnant women in Nigeria. BMC Complement Altern Med. 2009; 9:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ernst E. Herbal medicinal products during pregnancy: are they safe? BJOG. 2002; 109:227-235. [DOI] [PubMed] [Google Scholar]


