Summary
Insomnia is a symptom of physical or mental disorder and refers to decreased sleep time and potentially low quality. There is evidence showing that acupuncture could enhance management of insomnia, and Sanyinjiao (SP 6) is one of the promising acupoints. This review aimed to evaluate the effectiveness of stimulating single acupoint SP 6 in managing insomnia. The study was registered under PROSPERO CRD42019140855. English and Chinese databases were searched for randomized controlled trials on single acupoint SP 6 stimulation in management of insomnia. Quality of methodology was assessed by two authors independently using the Cochrane Risk of Bias Tool, and reporting quality was assessed by the STRICTA checklist. The primary outcome was the Pittsburgh Sleep Quality Index (PSQI), and secondary outcomes were improvement in clinical effect and sleep duration assessed by polysomnogram (PSG). The extracted data were pooled and meta-analyzed with RevMan 5.3 software. Four trials involving 288 participants were included in this review. The findings showed that SP 6 stimulation could improve sleep quality (MD -0.30, 95% CI [-0.52, -0.08]), lengthen deep sleep duration (MD 80.46, 95% CI [56.47, 104.45]), rapid eye movement (REM) duration (MD 91.53, 95% CI [68.41, 114.65]), and increase improvement in clinical effect. Quality of reporting and methodology was limited in all included trials. Some limited evidence showed that single acupoint stimulation of SP 6 could improve sleep quality, lengthen deep sleep and REM duration of patients with insomnia. However, the findings in this review should be interpreted with caution due to methodological limitations.
Keywords: acupuncture, single point, Sanyinjiao, SP 6, insomnia, meta-analysis
Introduction
Good quality sleep is the foundation of healthy life as a normal person spends more than 30% of their whole life time in bed (1). More than 27% of people worldwide have problems with sleeping (2), among which 6%- 10% meet the diagnostic criteria for primary insomnia (3). Insomnia is a condition of unsatisfactory sleep, in terms of sleep onset, and early waking. Insomnia is also a subjective condition, which can cause psychological discomfort including stress or mood disturbances because of low quality sleep and lack of sleeping time. Patients with insomnia may complain about difficulty falling asleep and/or early waking (4). Meanwhile, insomnia can be secondary to other diseases including anxiety and depression and is linked to increased incidence of cardiovascular diseases (5,6). A study reported that there are relationships between insomnia and paranoia, which has received sustained attention (7). In the United Kingdom (UK), the prevalence of primary insomnia is increasing (between 3.1% and 5.8%) and it is 1.5-2 times higher in women than in men (8). In addition to the above, insomnia is mostly considered a long-term dysfunction. A large UK study reported that approximate 75% of insomnia patients had symptoms lasting at least one year (9), and a three-year longitudinal study suggested that about 46% reported insomnia lasting three years (10).
Hypnotics have been reported to have good efficacy for managing insomnia, but there is still lack of evidence to prove hypnotics are the best choice to manage insomnia because of the significant adverse effects including daytime sedation, poor motor coordination, related concerns about driving accidents and injuries from falls, addictiveness and the effect on cognitive function (11-13). Some other adverse effects have also been reported: a fourteen-year follow-up study conducted in Taiwan showed that hypnotics increased the risks of oral and breast cancer in insomniacs with a hazard ratio of 1.49 times compared with insomnia patients who did not use hypnotics (14). A study performed in Korea showed that there were some associations between hypnotics and mortality (15). On the other hand, tolerance to hypnotics is another cause reducing their effectiveness for managing insomnia (16).
Traditional Chinese Medicine (TCM), especially acupuncture, has been widely accepted in many regions for some specific diseases. Sleep disorders are one of the preponderant illnesses for acupuncture therapy (17). Research evidence from a systematic review including 5,533 participants with all types of insomnia suggested that acupuncture reduced Pittsburgh Sleep Quality Index (PSQI) scores and appeared to be safe in comparison to Western medications (18). After a one-year follow-up with a 40-year-old insomnia patient, Zhang et al. reported that acupuncture improved sleep quality and accompaning symptoms (morning headache, fatigue, and mood worsening) by polysomnographic readings and therefore it may be considered to be used as primary and independent treatment for chronic insomnia (19). A Bayesian network meta-analysis of 42 studies involving 3,304 participants confirmed that scalp acupuncture might be the most effective intervention for primary insomnia compared with Western medicine, electro-acupuncture, warm acupuncture, and conventional acupuncture measured by PSQI score (20). In TCM theory, the cause of insomnia is an imbalance of Yang [阳] and Yin [阴], therefore the treatment of insomnia is to regulate the balance of Yang and Yin. Lower and inner parts of the body indicate Yin in TCM, and the sixth point of the Spleen meridian, Shanyinjiao (SP 6), is an acupoint where three Yin meridians (spleen, liver and kidney meridians, which run from the foot to the head) and converge near the inner ankle, so stimulation of SP 6 could activate the three Yin meridians and used as an optimal point for balancing Yin in the whole body. SP 6 is known to have an association with sleep because of its location and efficacy on coordinating Yang and Yin in the body. It records that SP 6 could calm the heart and tranquilize the mind from Classic Acupuncture and Moxibustion (known as Zhenjiu Jiayi Jing in Chinese). In clinical practice for insomnia, SP 6 is the second most commonly used acupoint after Shenmen (HT 7), at a frequency around 67% (21). Animal-based research showed that SP 6 stimulation improves the condition of sleep disorders maybe through increasing the content of 5-hydroxytryptamine (5-HT) in the hippocampus (22) or regulating energy metabolism in the paraventricular nucleus of the hypothalamus (23).
It will take a lot of work to make an easy-to-administer protocol on acupoint selection for managing insomnia because of the issue around blinding and lack of standardization in point selection, but we aim to offer a list of possible acupoints for managing insomnia by analyzing the effect of single acupoints individually. In our previous research, we showed that Shenmen (HT 7) could be a possible option for managing insomnia effectively (24). In this systematic review, the effectiveness of stimulating SP 6 for managing insomnia will be evaluated as a standardizable single point.
Materials and Methods
This study was reported following the Preferred Reporting Item for Systematic Review and Meta-Analysis (PRISMA) (25), and has been registered under PROSPERO (registration number CRD42019140855) (26).
Data sources and search items
Databases include PubMed, ScienceDirect, Web of Science, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang and Chinese Science and Technology Journal Database (VIP). Databases were searched from their inceptions to April 2019. The search strategy was developed following the guidelines of Cochrane Review Handbook. The search items are shown in Supplement Table S1 (https://www.globalhealthmedicine.com/site/supplementaldata.html?ID=5).
Inclusion criteria
Types of studies: Randomized controlled trials (RCTs) which evaluated the effectiveness of single acupoint Sanyinjiao (SP 6) for managing insomnia were included in this review, regardless of blinding, and publication region.
Types of participants: Participants diagnosed with clinical insomnia were included in this review, irrespective of age, gender, cause of insomnia, or the duration of insomnia.
Types of interventions: The interventions of treatment group were any stimulation at SP 6, including acupuncture, acupressure, moxibustion, catgut-embedding, acupoint application, acupoint injection, or other relevant stimulations. The comparisons included no treatment, hypnotics, sham, pseudo points (points nearby acupoints) stimulation, Chinese herbs, or other possible treatments.
Types of outcome measures: The primary outcome was Pittsburgh Sleep Quality Index (PSQI, score from 0 to 21, and lower scores indicate improvement in sleep), which includes seven items: global scores, quality of sleep, sleep latency, sleep duration, sleep efficiency, sleep disturbance, and daytime function. Higher PSQI scores indicated worse sleep.
The secondary outcomes were improvement in clinical effect and sleep duration monitoring by polysomnogram (PSG). PSG included four items: latency to persistent sleep, light sleep duration, deep sleep duration, and rapid eye movement (REM) duration. The higher scores of the first two items indicated worse sleep, while higher scores of the last two items indicated better sleep. All the outcomes were analyzed by using the values after treatment and at the follow-up points (if possible).
Data extraction
Data of study characteristics extracted from the included trials included study ID, sample size, age of participants, stimulation on SP 6, duration of stimulation, stimulating side of SP 6, interventions of control groups, outcomes, and their follow-ups.
Risk of bias and reporting quality of included trials
Two authors (ZJW, YZ) assessed risk of bias, reporting and methodology quality according to Cochrane Review Handbook by using Review Manager 5.3 software (The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) independently. Seven items were judged as low, high or unclear risk of bias. Different opinions were discussed by the two authors, and the third author (XYH) made the decision if discussions did not reach a consensus.
Reporting quality of the included trials was assessed by STRICTA checklist (27). Full, partial and no reporting were judged for each item. High reporting quality was defined as more than 70% of items being fully reported, whereas 50-70% indicated medium quality, 30-50% indicated low quality, and ≤ 30% indicated very low quality (27).
Data synthesis and analysis
Data was synthesized and analyzed using Review Manager 5.3 software. For dichotomous data we calculated the risk ratio (RR) with 95% confidence interval (CI) using the Mantel-Haenszel (M-H) method. For continuous data we calculated the mean difference (MD). The choice of effect model depended on the heterogeneity test: if I2 ≥ 50% and the p value of the Chi2 was less than 0.1, we chose the random-effects model because of high heterogeneity, otherwise we chose the fixed-effects model. The reasons for heterogeneity may be different types of stimulations in every trial and duration of stimulation, which would be sensitivity analyses if enough trials were included. Subgroup analysis would be conducted if possible according to different ages of participants, and data from each subgroup would be evaluated independently. If there were less than three trials in an analysis group that meta-analysis would be impossible, in which case a narrative description would be performed.
Results
An initial search identified 1,081 potential studies, and 586 were excluded by removing duplicates. The remaining 495 studies were scanned by title and abstract, with 487 studies excluded because of not meeting the inclusion criteria. The remaining eight trials were screened with full texts and four trials were finally included in this study (Figure 1).
Figure 1.
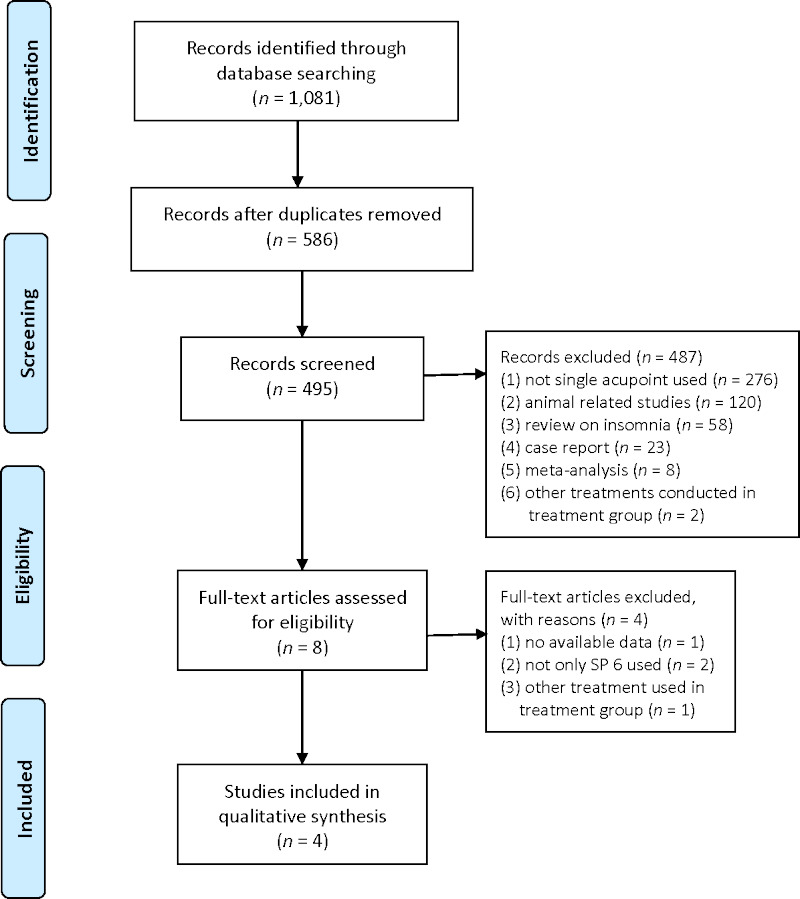
Flow diagram.
Study characteristics
Four trials (28-31) with 288 participants were involved in this study. All the included trials were conducted and published in mainland China. The condition in three of them was primary insomnia (28-30), one was insomnia after surgery (31). The outcome in all four trials included PSQI, two (29,30) reported improvement in clinical effect of sleeping disorders as an outcome, and one (31) reported PSG. Three trials (29-31) had a four-week follow-up. The detailed study characteristics are shown in Table 1.
Table 1. Study characteristics of the included trials.
| Study (Ref.) | Conditions | Sample size (T/C) |
Age (T/C) (year) | Stimulation | Duration | Side of point | Outcomes | Follow-ups |
|---|---|---|---|---|---|---|---|---|
| Geng 2017 (28) | Primary insomnia | 50/45 | 41.8/43.8 | warm-acupuncture | 50 min for 25 days | both sides | PSQI | NR |
| Zhao 2017 (29) | Primary insomnia | 34/32 | 51.67 ± 8.7/ 50.96 ± 8.46 | acupuncture | 30 min for 25 days | both sides | PSQI, improvement in clinical effect | 4-week |
| Shi 2017 (30) | Primary insomnia | 33/34 | 48.64 ± 8.31/ 50.26 ± 6.43 | acupuncture | 30 min for 25 days | NR | PSQI, improvement in clinical effect | 4-week |
| Li 2018 (31) | Insomnia after surgery | 30/30 | 20-70 | acupoint herbal plaster | 20 min for 7 days | both sides | PSQI, PSG | 4-week |
C: control group; NR: not reported; PSG: polysomnogram; PSQI: Pittsburgh Sleep Quality Index; sham: replace the herbal content with saline in the plaster; T: treatment group.
The stimulation on SP 6 in one trial (28) was warm-acupuncture (put a burning moxa stick on the needle handle), two (29,30) were acupuncture, and one (30) was acupoint herbal plaster. Three trials (29-31) reported that SP6 was stimulated on both sides.
Quality of reporting
The reporting quality of the four trials was low. According to the STRICTA checklist, two included trials (29,30) were judged low quality because the percentage of full reporting was 48.6% and 45.9% respectively, and the other two trials (28,31) were very low quality with 29.7% of the items being fully reported (Table 2).
Table 2. Reporting quality evaluation by STRICTA checklist.
| Section/Topic | No. | Item | Assessment (Ref.) |
|||
|---|---|---|---|---|---|---|
| Geng 2017 (28) |
Zhao 2017 (29) |
Shi 2017 (30) |
Li 2018 (31) |
|||
| Title and abstract | ||||||
| 1a | Identification as a randomized trial in the title | N | N | N | N | |
| 1b | Structured summary of trial design, methods, results, and conclusions (for specific guidance see CONSORT for abstracts) | Y | Y | Y | Y | |
| Introduction | ||||||
| Background and objectives | 2a | Scientific background and explanation of rationale | Y | Y | Y | Y |
| 2b | Specific objectives or hypotheses | Y | Y | Y | Y | |
| Methods | ||||||
| Trial design | 3a | Description of trial design (such as parallel, factorial) including allocation ratio | N | Y | Y | N |
| 3b | Important changes in methods after trial commencement (such as eligibility criteria), with reasons | N | N | N | N | |
| Participants | 4a | Eligibility criteria for participants | Y | Y | Y | Y |
| 4b | Settings and locations where the data were collected | Y | Y | Y | Y | |
| Acupuncture rationale | 5a | Style of acupuncture (e.g. Traditional Chinese Medicine, Japanese, Korean, Western medical, Five Element, ear acupuncture, etc.) | Y | Y | Y | Y |
| 5b | Reasoning for treatment provided, based on historical context, literature sources, and/or consensus methods, with references where appropriate | P | Y | P | P | |
| 5c | Extent to which treatment was varied | Y | Y | Y | Y | |
| Details of needling | 6a | Number of needle insertions per subject per session (mean and range where relevant) | P | P | P | P |
| 6b | Names (or location if no standard name) of points used (uni/bilateral) | Y | Y | Y | Y | |
| 6c | Depth of insertion, based on a specified unit of measurement, or on a particular tissue level | P | P | P | P | |
| 6d | Response sought (e.g. de qi or muscle twitch response) | Y | Y | Y | Y | |
| 6e | Needle stimulation (e.g. manual, electrical) | Y | Y | Y | Y | |
| 6f | Needle retention time | Y | Y | Y | Y | |
| 6g | Needle type (diameter, length, and manufacturer or material) | Y | Y | Y | Y | |
| Treatment regimen | 7a | Number of treatment sessions | Y | Y | Y | Y |
| 7b | Frequency and duration of treatment sessions | Y | Y | Y | Y | |
| Other components of treatment | 8a | Details of other interventions administered to the acupuncture group (e.g. moxibustion, cupping, herbs, exercises, lifestyle advice) | Y | Y | Y | Y |
| 8b | Setting and context of treatment, including instructions to practitioners, and information and explanations to patients | N | N | N | N | |
| Practitioner background | 9 | Description of participating acupuncturists (qualification or professional affiliation, years in acupuncture practice, other relevant experience) | N | N | N | N |
| Control or comparator | 10a | Rationale for the control or comparator in the context of the research question, with sources that justify this choice | P | P | P | P |
| 10b | Precise description of the control or comparator. If sham acupuncture or any other type of acupuncture-like control is used, provide details as for items 5 to 8 above | P | P | P | P | |
| Outcomes | 11a | Completely defined pre-specified primary and secondary outcome measures, including how and when they were assessed | P | P | P | P |
| 11b | Any changes to trial outcomes after the trial commenced, with reasons | N | Y | Y | N | |
| Sample size | 12a | How sample size was determined | N | N | N | N |
| 12b | When applicable, explanation of any interim analyses and stopping guidelines | N | N | N | N | |
| Randomization | ||||||
| Sequence generation | 13a | Method used to generate the random allocation sequence | N | Y | N | N |
| 13b | Type of randomization; details of any restriction (such as blocking and block size) | N | P | P | N | |
| Allocation concealment mechanism | 14 | Mechanism used to implement the random allocation sequence (such as sequentially numbered containers), describing any steps taken to conceal the sequence until interventions were assigned | N | Y | N | N |
| Implementation | 15 | Who generated the random allocation sequence, who enrolled participants, and who assigned participants to interventions | N | N | N | N |
| Blinding | 16a | If done, who was blinded after assignment to interventions (for example, participants, care providers, those assessing outcomes) and how | N | N | N | N |
| 16b | If relevant, description of the similarity of interventions | N | Y | Y | N | |
| Statistical methods | 17a | Statistical methods used to compare groups for primary and secondary outcomes | Y | Y | Y | Y |
| 17b | Methods for additional analyses, such as subgroup analyses and adjusted analyses | N | N | N | N | |
| Results | ||||||
| Participant flow (a diagram is strongly recommended) | 18a | For each group, the numbers of participants who were randomly assigned, received intended treatment, and were analyzed for the primary outcome | N | P | P | N |
| 18b | For each group, losses and exclusions after randomization, together with reasons | Y | Y | Y | Y | |
| Recruitment | 19a | Dates defining the periods of recruitment and follow-up | N | Y | Y | Y |
| 19b | Why the trial ended or was stopped | N | N | N | N | |
| Baseline data | 20 | A table showing baseline demographic and clinical characteristics for each group | N | Y | Y | N |
| Numbers analyzed | 21 | For each group, number of participants (denominator) included in each analysis and whether the analysis was by original assigned groups | Y | Y | Y | Y |
| Outcomes and estimation | 22a | For each primary and secondary outcome, results for each group, and the estimated effect size and its precision (such as 95% confidence interval) | Y | Y | Y | Y |
| 22b | For binary outcomes, presentation of both absolute and relative effect sizes is recommended | N | N | N | N | |
| Ancillary analyses | 23 | Results of any other analyses performed, including subgroup analyses and adjusted analyses, distinguishing pre-specified from exploratory | N | N | N | N |
| Harms | 24 | All important harms or unintended effects in each group (for specific guidance see CONSORT for harms) | N | P | P | N |
| Discussion | ||||||
| Limitations | 25 | Trial limitations, addressing sources of potential bias, imprecision, and, if relevant, multiplicity of analyses | N | P | P | N |
| Generalizability | 26 | Generalizability (external validity, applicability) of the trial findings | Y | Y | Y | Y |
| Interpretation | 27 | Interpretation consistent with results, balancing benefits and harms, and considering other relevant evidence | P | P | P | P |
| Other information | ||||||
| Registration | 28 | Registration number and name of trial registry | N | N | N | N |
| Protocol | 29 | Where the full trial protocol can be accessed, if available | N | N | N | N |
| Funding | 30 | Sources of funding and other support (such as supply of drugs), role of funders | Y | Y | Y | N |
| RATING OVERALL CONFIDENCE IN THE RESULITS OF THE TRIALS | VL | L | L | VL | ||
N: no reporting; P: partly reporting; Y: fully reporting. Evaluation criteria depended on the percentage of fully reporting items: ≤ 30%: Very Low quality (VL); 30-50%: Low quality (L); 50-70%: Medium quality (M); > 70%: High quality (H).
Risk of bias
Quality of methodology was limited in the four trials (Figure 2). Regarding randomization, one trial (29) reported using random number cards for random sequence generation, so low risk was judged, one (28) failed randomization by grouping participants according to the treatment plans, so high risk was judged, the other two (30,31) reported randomization without methods, so unclear risk was judged. Two included trials (29,30) reported using sealed envelopes, which were judged low risk. One trial (30) reported blinding of outcomes assessment. Two (29,30) did not fully report outcome data, so high risk of bias was judged. Two trials (29,30) reported similarity of baseline characteristics, detailed information of criteria, ethical approval, and funding, so low risk of other bias was judged.
Figure 2.
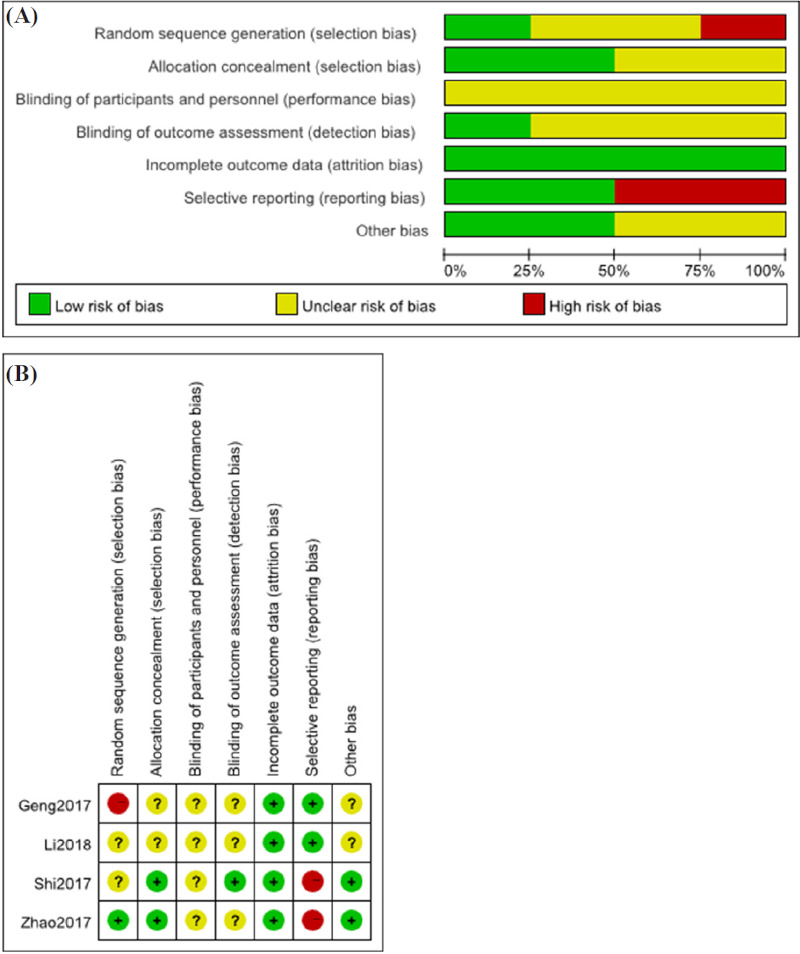
Risk of bias. (A) risk of bias graph; (B) risk of bias summary.
Effect estimation
Pittsburgh Sleep Quality Index (PSQI): All included trials reported PSQI as an outcome, but two trials (29,30) did not report the exact values of PSQI after treatment, so only two trials (28,31) were evaluated, which showed that stimulations on SP 6 were more effective than moxa on Shenmen acupoint intervention or sham group in global score of PSQI (MD -2.77, 95% CI [-3.84, -1.71], I2 = 97%, p < 0.00001). One trial (28) reported six aspects of PSQI separately showing that warm-acupuncture on SP 6 was more effective than moxa on Shenmen acupoint in improving quality of sleep (MD -0.30, 95% CI [-0.52, -0.08]), while there was no difference in sleep latency (MD -0.25, 95% CI [-0.59, 0.09]), sleep duration (MD -0.26, 95% CI [-0.82, 0.30]), sleep efficiency (MD -0.03, 95% CI [-0.53, 0.47]), sleep disturbance (MD -0.16, 95% CI [-0.42, 0.10]), or daytime function (MD -0.12, 95% CI [-0.29, 0.05]).
Improvement in clinical effect: Two included trials (29,30) suggested that acupuncture on SP 6 improved clinical effects in comparison with pseudo acupoint/ multi-acupoints stimulations (RR 0.76, 95% CI [0.60, 0.98]), but could improve clinical effects in comparison with pseudo acupoint (RR 1.52, 95% CI [0.93, 2.50]).
Sleep duration: One trial (31) assessed PSG by observing participants in sleep for 20 minutes every day, with 15 seconds as a measurement unit. It showed that acupoint herbal plaster on SP 6 improved sleep duration as measured by PSG when compared with a sham group, with shorter latency to persistent sleep (MD -32.35 seconds, 95% CI [-43.78, -20.92]), shorter light sleep duration in seconds (MD -29.70, 95% CI [-52.31, -7.09]), longer deep sleep duration in seconds (MD 80.46, 95% CI [56.47, 104.45]), and longer REM duration in seconds (MD 91.53, 95% CI [68.41, 114.65]).
Adverse events: Only one included trial (29) reported adverse events, showing that there was no adverse event in both acupuncture on SP 6 group or pseudo acupoint stimulation group during the whole 25-days of research.
Discussion
This is a systematic review focusing on single acupoint SP 6 stimulation for managing insomnia. It provides preliminary evidence of the effectiveness of single acupoint SP 6 for managing insomnia, although there were limitations to take into consideration.
Summary of main results
After combining the included four trials, the results showed that stimulation of SP 6 resulted in a better PSQI global score and sleep quality score. Meanwhile it may improve clinical effect and higher PSG scores than control interventions including moxa, multi-acupoints acupuncture, pseudo acupoint and sham. When it comes to the scores of sleep latency, sleep duration, sleep efficiency, sleep disturbance, and daytime function, there were no differences between stimulation of SP 6 and moxa on Shenmen acupoint.
In view of the results, stimulations on single acupoint SP 6 may improve sleep quality and lengthen deep sleep duration and REM duration of patients with primary insomnia and insomnia after surgery. The high heterogeneity may be because of the small number of trials and participants, different hospital settings, different ages of patients, different control interventions, lack of blinding, or difference characteristics of patients including education level and employment status. Hence more rigorous trials with high quality methodology and reporting should be performed in future clinical research.
The potential mechanism of acupoint stimulation for managing insomnia
Many acupoints could be used for managing insomnia, and the Evidence-Based Guideline in TCM for insomnia recommends SP6 as a main acupoint (32). Some potential mechanisms of stimulating acupoints for insomnia have been reported. Gamma-amino butyric acid (GABA), a main transmitter in the brain, has an inhibitory effect on neuroexcitability in the central nervous system (CNS). Lower GABA in the brain leads to many mental disorders including insomnia, and acupoint stimulation could increase GABA, which shows a similar effect with benzodiazepine (33). Acupoints stimulation also has an effect on controlling autonomic nervous system function such as regulating blood pressure and heart rate, which are disregulated in patients with insomnia (34-36).
Strength and limitations
Some limitations existed in this study. First, only English and Chinese databases were searched because of language barriers. So it may have missed some high quality trials published in other languages (such as Japanese and Korean). Second, only two placebo-controlled trials (one used pseudo acupoint acupuncture and one was sham) were included in this review, which led to limited evidence from placebo-controlled trials. Third, the reporting and methodological quality of the included trials was low therefore the findings of this review should be interpreted with caution. Insomnia is reported as a long-term disorder mostly, while only four-week follow-ups were conducted in the included trials, so it is hard to conclude whether single acupoint stimulation on SP 6 had an effect on long-term insomnia. Finally, because of the small numbers of included trials, subgroup analysis and meta-analysis could not be conducted in this study, which may have a significant influence on the effectiveness of SP 6 for managing insomnia.
Implications for practice
This systematic review suggests that there is a lack of high-quality evidence to support single acupoint SP 6 stimulation for managing insomnia. Though there are limitations, SP 6 stimulation including acupuncture, warm-acupuncture, and acupoint paste may be recommended for insomnia, especially for primary insomnia. The recommended regimen durations may be from 20 min to 50 min lasting from 7 days to 25 days. The long-term effect of acupuncture is unknown and its potential adverse effects are not entirely clear.
Priorities for future research
Existing randomized controlled trials of SP 6 for managing insomnia are of small size and low methodological quality. Further high-quality trials of larger size are needed to assess the effectiveness of SP 6 for managing insomnia. Since insomnia is a highly heterogeneous condition with different etiologies and severity and acupoint stimulation is also a highly heterogeneous intervention, different stimulation at SP 6 is likely to have different effects on different subgroups of patients. Therefore, further clinical trials could focus on treating a particular subgroup using a particular stimulation at SP 6. Potential self-management approaches include stimulating SP 6 with acupressure, moxibustion, or other easy-to-do methods, which may be safe and easily accessible for insomniacs to perform at home at low cost. Further research is warranted to explore these potentials.
Conclusion
Some limited evidence shows that single acupoint stimulation of SP 6 could improve sleep quality, lengthen deep sleep and REM duration of patients with insomnia. However, the findings in this study should be interpreted with caution due to limitations in methodology. Better quality clinical trials are needed with precise methodology for single acupoint stimulation for managing all types of insomnia with pragmatic designs.
Funding
ZJW and LXZ are supported by the Guangdong Famous TCM Workshop of Zhuanglixing. XYH is supported by the NIHR School for Primary Care Research. MLW is a NIHR Academic Clinical Lecturer, under grant CL-2016-26-005. The views expressed are those of the author(s) and not necessarily those of the NIHR or Zhuang's group.
References
- 1. Ren G, Zhong Y, Ke G, Liu X, Li H, Li X, Zheng Q, Yang M. The mechanism of compound Anshen essential oil in the treatment of insomnia was examined by network pharmacology. Evid Based Complement Alternat Med. 2019; 2019:9242403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007; 30:274-280. [PubMed] [Google Scholar]
- 3. Walsh JK. Clinical and socioeconomic correlates of insomnia. J Clin Psychiatry. 2004; 65 Suppl 8:13-19. [PubMed] [Google Scholar]
- 4. K Pavlova M, Latreille V. Sleep disorders. Am J Med. 2019; 132:292-299. [DOI] [PubMed] [Google Scholar]
- 5. Joober R, Cole K, Tabbane K, Boivin DB. An algorithmic approach to the management of insomnia in patients with schizophrenia. Ann Clin Psychiatry. 2017; 29:133-144. [PubMed] [Google Scholar]
- 6. Fernandez-Mendoza J. The insomnia with short sleep duration phenotype: an update on it is importance for health and prevention. Curr Opin Psychiatry. 2017; 30:56-63. [DOI] [PubMed] [Google Scholar]
- 7. Reeve S, Sheaves B, Freeman D. The role of sleep dysfunction in the occurrence of delusions and hallucinations: a systematic review. Clin Psychol Rev. 2015; 42:96-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Calem M, Bisla J, Begum A, Dewey M, Bebbington PE, Brugha T, Cooper C, Jenkins R, Lindesay J, McManus S, Meltzer H, Spiers N, Weich S, Stewart R. Increased prevalence of insomnia and changes in hypnotics use in England over 15 years: analysis of the 1993, 2000, and 2007 National Psychiatric Morbidity Surveys. Sleep. 2012; 35:377-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moreno RA, Hanna MM, Tavares SM, Wang YP. A double-blind comparison of the effect of the antipsychotics haloperidol and olanzapine on sleep in mania. Braz J Med Biol Res. 2007; 40:357-366. [DOI] [PubMed] [Google Scholar]
- 10. Morin CM, Belanger L, LeBlanc M, Ivers H, Savard J, Espie CA, Mérette C, Baillargeon L, Grégoire JP. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. 2009; 169:447-453. [DOI] [PubMed] [Google Scholar]
- 11. Consensus Experts Group on Definition, Diagnosis and Drug Treatment of Insomnia. Expert consensus on definition, diagnosis and drug treatment of insomnia (draft). Chinese Journal of Neurology. 2006; 2:141-143. (in Chinese). [Google Scholar]
- 12. Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ. 2000; 162:225-233. [PMC free article] [PubMed] [Google Scholar]
- 13. Buysse DJ. Insomnia. JAMA. 2013; 309:706-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fang HF, Lee TY, Hui KC, Yim HCH, Chi MJ, Chung MH. Association between sedative-hypnotics and subsequent cancer in patients with and without insomnia: a 14-year follow-up study in Taiwan. J Cancer. 2019; 10:2288-2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Choi JW, Lee J, Jung SJ, Shin A, Lee YJ. Use of sedative-hypnotics and mortality: a population-based retrospective cohort study. J Clin Sleep Med. 2018; 14:1669-1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005; 18:249-255. [DOI] [PubMed] [Google Scholar]
- 17. Li L, Hu H. The research progress in Chinese medicine treatments for insomnia. World Latest Medicine Information. 2019; 19:74-75. (in Chinese). [Google Scholar]
- 18. Cao HJ, Yu ML, Wang LQ, Fei YT, Xu H, Liu JP. Acupuncture for primary insomnia: an undated systematic review of randomized controlled trials. J Altern Complement Med. 2019; 25:451-474. [DOI] [PubMed] [Google Scholar]
- 19. Zhang W, Huang Z, Jin Y. Acupuncture as a primary and independent treatment for a patient with chronic insomnia: one-year follow-up case report. Medicine (Baltimore). 2017; 96:e9471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xu H, Shi Y, Xiao Y, Liu P, Wu S, Pang P, Deng L, Chen X. Efficacy comparison of different acupuncture treatments for primary insomnia: a Bayesian analysis. Evid Based Complement Alternat Med. 2019; 2019:8961748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu Y, Ren Y, Zhao L, Yu L, Chen J, Yang M, Liang F. Analysis on characteristics of meridians and acupoints about acupuncture in treatment of insomnia based on data mining. China Journal of Traditional Chinese Medicine and Pharmacy. 2015; 30: 2734-2737. (in Chinese). [Google Scholar]
- 22. Cao H, Feng M, Hou S, Teng J. Effects and mechanism study of electro-needling SP6 on sleep phase in rats with perimenopausal insomnia. Journal of Clinical Acupuncture and Moxibustion. 2019; 35:80-83. (in Chinese). [Google Scholar]
- 23. Zhu YH, Yang CH, He LX, Qiao L, Cheng CS. Effect of electroacupuncture at 'Shenmen' (HT7) and 'Sanyingjiao' (SP6) on energy metabolism in paraventricular nucleus of hypothalamus of insomnia rats. Zhen Ci Yan Jiu. 2019; 44:170-175. (in Chinese). [DOI] [PubMed] [Google Scholar]
- 24. Wang Z, Hu X, Su J, Gao X, Xu N, Xing Y, Zhuang L. The efficacy and safety stimulating a single acu-point shenmen (HT 7) for managing insomnia: a systematic review of randomized controlled trials. European Journal of Integrative Medicine. 2017; 15:17-22. [Google Scholar]
- 25. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and analyses: the PRISMA statement. PLoS Med. 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang Z. The efficacy and safety of stimulating on single acupoint Sanyinjiao (SP 6) for managing insomnia: a systematic review of randomized controlled trials. PROSPERO. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019140855. (accessed February 20, 2020). [DOI] [PMC free article] [PubMed]
- 27. Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004; 328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Geng X, Li W, Li X, Luo B. Clinical observation on the treatment of 50 cases of phlegm-dampness type insomnia with salt-partitioned moxibustion at shenque acupoint combined with warm needling method at sanyinjiao acupoint. Journal of Navy Medicine. 2017; 38:429-431, 458. (in Chinese). [Google Scholar]
- 29. Zhao J. Effect of acupuncture sanyinjiao (SP 6) on PSQI and PSG in patients with primary insomnia. Changchun University of Chinese Medicine. 2017. http://gb.oversea.cnki.net/KCMS/detail/detail.aspx?filename=1018006766.nh&dbcode=CMFD&dbname=CMFDREF (accessed January 10, 2020). (in Chinese). .
- 30. Shi L. The effect of sancai acupoint and sanyinjiao on ET and PSQI in patients with primary insomnia. Changchun University of Chinese Medicine. 2017. http://www.wanfangdata.com.cn/details/detail.do?_type=degree&id=Y3331448 (accessed January 10, 2020). (in Chinese). .
- 31. Li Y. Acupoint application on SP6 for insomnia after gynecologic operations. China Higher Medical Education. 2018; 10: 132, 139. (in Chinese). [Google Scholar]
- 32. TCM clinical guidelines of insomnia research group from Chinese Academy of Chinese Medical Sciences. TCM clinical guidelines of insomnia (WHO/WPO). World Journal of Sleep Medicine. 2016; 3:8-25. (in Chinese). [Google Scholar]
- 33. Shergis JL, Ni X, Jackson ML, Zhang AL, Guo X, Li Y, Lu C, Xue CC. A systematic review of acupuncture for sleep quality in people with insomnia. Complement Ther Med. 2016; 26:11-20. [DOI] [PubMed] [Google Scholar]
- 34. Li QQ, Shi GX, Xu Q, Wang J, Liu CZ, Wang LP. Acupuncture effect and central autonomic regulation. Evid Based Complement Alternat Med. 2013; 2013:267959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bonnet MH, Arand DL. Heart rate variability in insomniacs and matched normal sleepers. Psychosom Med. 1998; 60:610-615. [DOI] [PubMed] [Google Scholar]
- 36. Vgontzas AN, Bixler EO, Lin HM, Prolo P, Mastorakos G, Vela-Bueno A, Kales A, Chrousos GP. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications. J Clin Endocrinol Metab. 2001; 86:3787-3794. [DOI] [PubMed] [Google Scholar]


