Abstract
Purpose:
To evaluate the effect of residual amblyopia on functional vision and eye-related quality of life (ER-QOL) in children and their families using the Pediatric Eye Questionnaire (PedEyeQ).
Design:
Prospective cross-sectional study
Methods:
Seventeen children with residual amblyopia (no current treatment except glasses), 48 visually normal controls without glasses and 19 controls wearing glasses (aged 8–11 years) completed the Child 5–11 year PedEyeQ. One parent for each child completed the Proxy 5–11 PedEyeQ, Parent PedEyeQ. Rasch-calibrated domain scores were calculated for each questionnaire domain and compared between amblyopic children and controls.
Results:
PedEyeQ scores were significantly lower (worse) for children with residual amblyopia than for controls without glasses across all domains; Child PedEyeQ greatest mean difference 18 points worse on functional vision domain (95% CI −29 to −7; P<.001); Proxy PedEyeQ greatest mean difference 31 points worse on functional vision domain (95% CI −39 to −24; P<.001); Parent PedEyeQ greatest mean difference 34 points worse on the worry about the child’s eye condition domain (95% CI −46 to −22; P<.001). Compared with controls wearing glasses, PedEyeQ scores were lower for residual amblyopia on the Child frustration / worry domain (P=.03), on four of five Proxy domains (P≤ .05) and on three of four Parent domains (P≤ .05).
Conclusions:
Residual amblyopia affects functional vision and ER-QOL in children. Parents of amblyopic children also experience lower quality of life. These data help broaden our understanding of the everyday-life impact of childhood residual amblyopia.
INTRODUCTION
Amblyopia is the most common cause of reduced monocular visual acuity (VA) in children, affecting between 0.8% and 5% of children in the USA,1–3 and is associated with dysfunctions of accommodation, fixation, binocularity, vergence, reading speed, contrast sensitivity and fine motor skills.4–14 Despite these well-documented effects of amblyopia on vision-related functioning, the everyday-life impact of amblyopia on a child and their family is poorly characterized. Most previous studies assess the impact of amblyopia treatment,15 but few have used eye-related or vision-specific instruments to evaluate the effects of amblyopia itself on children and their families. The aim of the present study was to assess the impact of residual amblyopia on eye-related quality of life (ER-QOL) and functional vision, comparing scores with visually normal children with and without glasses. We used the recently-developed, Pediatric Eye Questionnaire (PedEyeQ), developed to assess functional vision and eye-related quality of life (ER-QOL) in children with any eye condition, and also to assess the quality of life of parents of affected children.16, 17 In addition we evaluated the impact of residual amblyopia on general health-related quality of life (HRQOL) using the Pediatric Quality of Life Inventory (PedsQL).
METHODS
Institutional Review Board approval for this prospective cross-sectional study was obtained from Institutional Review Boards at the Mayo Clinic, Rochester, Minnesota and the University of Texas Southwestern Medical Center, Dallas, Texas. All procedures and data collection were conducted in a manner compliant with the Health Insurance Portability and Accountability Act and all research procedures adhered to the tenets of the Declaration of Helsinki. Written informed consent and assent was obtained according to local IRB requirements. Consecutive eligible children with residual amblyopia were prospectively enrolled from pediatric ophthalmology outpatient clinics at a tertiary medical center (Mayo Clinic, MN), and in research clinics (Retina Foundation of the Southwest, TX) between December 2017 and October 2019. Subjects were identified in outpatient or research clinics, referred by friends or colleagues, or identified through a recruitment flyer. The few patients who declined participation did so primarily due to lack of time to complete the questionnaires. For all included subjects visual acuity was assessed in each eye using age-appropriate clinical tests (testing method not standardized).
Children with residual amblyopia
Seventeen children aged 8 to 11 years, with a current diagnosis of residual, unilateral amblyopia (strabismic, anisometropic or combined mechanism) were prospectively enrolled. Residual amblyopia met the following criteria: 1) inter-ocular visual acuity difference of two or more logMAR lines (letter optotype values converted to logMAR); 2) amblyopic-eye visual acuity below 20/25;18 3) a history of treatment with patching (n=16), atropine (n=5), binocular treatment (n=7), vision therapy (n=1), optical penalization (n=1), or a combination of treatments (n=10); 4) no treatment other than glasses for at least the past month (all other treatments having been discontinued). Any manifest strabismus was required to be <10 prism diopters by simultaneous prism cover test in refractive correction at distance and near (present in 5 [29%] of 17). Significant coexistent eye disease was excluded (Table 1).
Table 1.
Demographics of 8–11 year old children with residual amblyopia, being currently treated with glasses alone (N=17), visually normal controls without glasses (N=48), and visually normal controls wearing glasses (N=19), along with one parent for each child.
| Residual amblyopia (n=17) N (%) |
Visually normal controls without
glasses (n=48) N (%) |
Visually normal controls wearing
glasses (n=19) N (%) |
|
|---|---|---|---|
| Sex of child | |||
| Female | 9 (53) | 26 (54) | 9 (47) |
| Median age | 10 | 9 | 10 |
| Race/ethnicity | |||
| White | 13 (76) | 31 (65) | 11 (58) |
| Hispanic/Latino | 1 (6) | 2 (4) | 2 (11) |
| Black/African American | 2 (12) | 2 (4) | 0 (0) |
| Other | 1 (6) | 10 (21) | 5 (26) |
| More than one | 0 (0) | 2 (4) | 1 (0) |
| Not reported | 0 (0) | 1 (2) | 0 (0) |
| Visual acuity (logMAR): median (range) | |||
| Amblyopic Eye | 0.4 (0.2 to 1.2) | NA | NA |
| Fellow eye | 0.0 (−0.2 to 0.5) | NA | NA |
| Right Eye | NA | 0 (−0.2 to 0.1) | 0 (−0.1 to 0.1) |
| Refractive error spherical equivalent: median (range) | |||
| Amblyopic Eye | +4.50D (+0.88D to +9.00D) | NA | NA |
| Fellow eye | +1.63D (−1.50D to +7.88D) | NA | NA |
| Right Eye | NA | NA | +0.88D (−2.88D to +7.00D) |
| Cause of residual amblyopia | |||
| Anisometropic | 7 (41) | NA | NA |
| Strabismic | 1 (6) | NA | NA |
| Combined mechanism | 9 (53) | NA | NA |
Visually normal controls
Forty-eight 8- to 11 year-old children, with no glasses or other refractive correction, normal visual acuity for age,18 and no eye condition or history of an eye condition (including strabismus) were enrolled as the primary control group. Thirty-four of these control subjects were reported in previous studies.19–21
Glasses controls
We defined a second control group of 19 children with normal visual acuity for age but who were wearing glasses for refractive error. Since most children with residual amblyopia wear glasses we thought it would be helpful to know whether the impact of residual amblyopia is different from the impact of glasses wear itself. All glasses controls had no eye disease other than refractive error, no previous eye treatment other than glasses, and no history of other eye problems. Fifteen of these glasses controls were reported in a previous study.20
Questionnaires
All children completed the Child PedEyeQ and the Child PedsQL and one parent or legal guardian for each child completed the Proxy PedEyeQ, Parent PedEyeQ, Proxy PedsQL and the PedsQL Family Impact module. The majority of children/parents completing questionnaires did so electronically on an iPad; others completing on paper.
Pediatric Eye Questionnaire (PedEyeQ)
The PedEyeQ16, 17 comprises Child, Proxy and Parent components, each with distinct, separately-scored domains, using a 3-point frequency scale for responses (“Never,” “Sometimes,” “All of the time”). The Child 5–11 PedEyeQ (used in the present study) consists of Functional vision, Bothered by eyes/vision, Social, and Frustration/worry domains.16 The Proxy 5–11 PedEyeQ, consists of 5 domains: Functional vision, Bothered by eyes/vision, Social, Frustration/worry, Eye-care,16 and the Parent PedEyeQ assesses the effect of the child’s eye condition on the parent and family in 4 domains: Impact on parent/family, Worry about child’s eye condition, Worry about child’s self-perception and interactions, and Worry about child’s visual function.16 (Full questionnaires in English and Spanish, with Rasch-scoring look-up tables, are freely available at https://public.jaeb.org/pedig/view/Other_Forms).
Pediatric quality of life inventory (PedsQL)
The PedsQL is a general health-related quality of life (HRQOL) questionnaire. For the present study we used the Child module (8–12 year-old version), each with 23 items in 4 domains: physical, emotional, social, and school functioning), the Proxy module (parallel to Child) and the Family Impact PedsQL module (8 domains).22, 23 PedsQL questionnaires use 5 response options with the exception of the Child 5–7 which uses 3 options and the respondent is instructed to respond based on their experience over the past month (http://www.pedsql.org/about_pedsql.html, full questionnaires available by purchase only).
Analysis
Rasch-calibrated PedEyeQ domain scores were calculated for each participant, using previously-published Rasch look-up tables (freely available at: https://public.jaeb.org/pedig/view/Other_Forms), and converted to 0 (worst) to 100 for interpretation. All visual acuity data were converted to logMAR for analysis, calculating a logMAR letter score (Snellen equivalent reported for ease of interpretation). Median and range of visual acuity and refractive error were calculated for amblyopic and fellow eyes for children with residual amblyopia and right eyes for normal controls and glasses controls.
The primary analysis was a comparison of median PedEyeQ domain scores and PedsQL domain scores between children with residual amblyopia and visually normal controls not wearing glasses. In secondary analyses, we compared PedEyeQ domain scores and PedsQL domain scores in children with residual amblyopia and visually normal controls wearing glasses. Pairwise Wilcoxon tests were used for all analyses. Mean differences with a 95% confidence interval around the mean difference were also calculated.
RESULTS
Patients
Demographics and clinical characteristics for all enrolled children and parents are shown in Table 1. Median amblyopic-eye visual acuity was 20/50 (range 20/32 to 20/320) (Table 1). No children had developmental delay.
Residual amblyopia versus visually normal controls (not wearing glasses)
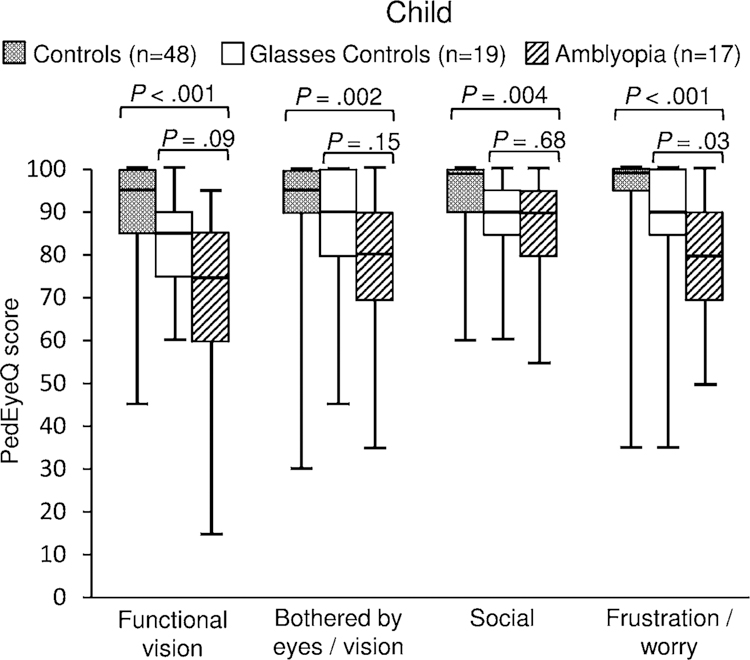
Child PedEyeQ
Children with residual amblyopia had lower (worse) scores than visually normal controls not wearing glasses, on each of the four Child PedEyeQ domains (P≤.004 for each; Figure 1; Table 2). The greatest difference was on the functional vision domain (median 75 vs 95; mean difference −18; 95% CI −29 to −7; P<.001; Figure 1; Table 2).
Figure 1.
Child Pediatric Eye Disease Questionnaire (PedEyeQ) domain scores for children with residual amblyopia compared with visually normal controls not wearing glasses and compared with visually normal controls wearing glasses. Amblyopic children had lower scores than controls not wearing glasses on all 4 domains, and lower scores than controls wearing glasses on the frustration / worry domain.
Table 2.
PedEyeQ domain scores for children with residual amblyopia (N=17), visually normal controls without glasses (N=48), and visually normal controls wearing glasses (N=19).
| PedEyeQ domains | Median (range) PedEyeQ scores | P value for difference Amblyopia vs Normal | Mean difference (95% CI) Amblyopia - Normal | P value for difference Amblyopia vs Glasses | Mean difference (95% CI) Amblyopia - Glasses | ||
|---|---|---|---|---|---|---|---|
| Residual Amblyopia N=17 | Normal controls without glasses N=48 | Glasses controls N=19 | |||||
| Child PedEyeQ domains | |||||||
| Functional Vision | 75 (15–95) | 95 (45–100) | 85 (60–100) | < .001 | −18 (−29 to −7) | .09 | −12 (−23 to 0) |
| Bothered by eyes/vision | 80 (35–100) | 95 (30–100) | 90 (45–100) | .002 | −13 (−23 to −3) | .15 | −6 (−18 to 5) |
| Social | 90 (55–100) | 100 (60–100) | 90 (60–100) | .004 | −7 (−13 to −2) | .68 | −1 (−9 to 7) |
| Frustration/worry | 80 (50–100) | 100 (35–100) | 90 (35–100) | < .001 | −16 (−23 to −8) | .03 | −9 (−18 to 1) |
| Proxy PedEyeQ domains | |||||||
| Functional Vision | 65 (35–95) | 100 (80–100) | 90 (40–100) | < .001 | −31 (−39 to −24) | .008 | −15 (−26 to −3) |
| Bothered by eyes/vision | 75 (45–100) | 100 (80–100) | 95 (55–100) | < .001 | −22 (−30 to −13) | .006 | −13 (−23 to −2) |
| Social | 88 (44–100) | 100 (94–100) | 94 (56–100) | < .001 | −23 (−34 to −12) | .049 | −14 (−26 to −2) |
| Frustration/worry | 70 (40–100) | 100 (80–100) | 100 (40–100) | < .001 | −25 (−37 to −13) | .050 | −14 (−29 to 1) |
| Eye-care | 67 (42–100) | 100 (67–100) | 100 (50–100) | < .001 | −28 (−40 to −16) | .06 | −16 (−30 to −2) |
| Parent PedEyeQ domains | |||||||
| Impact on parent/family | 90 (60–100) | 100 (85–100) | 100 (60–100) | < .001 | −16 (−23 to −9) | .02 | −9 (−17 to −1) |
| Worry about child’s condition | 60 (0–100) | 100 (40–100) | 80 (35–100) | < .001 | −34 (−46 to −22) | .01 | −17 (−31 to −3) |
| Worry about child’s self-perception/interactions | 71 (21–100) | 100 (64–100) | 93 (7–100) | < .001 | −27 (−38 to −16) | .07 | −11 (−26 to 4) |
| Worry about child’s visual function | 62 (6–100) | 100 (50–100) | 87 (12–100) | < .001 | −30 (−42 to −18) | .050 | −13 (−28 to 2) |
Bold values indicate significant difference between groups
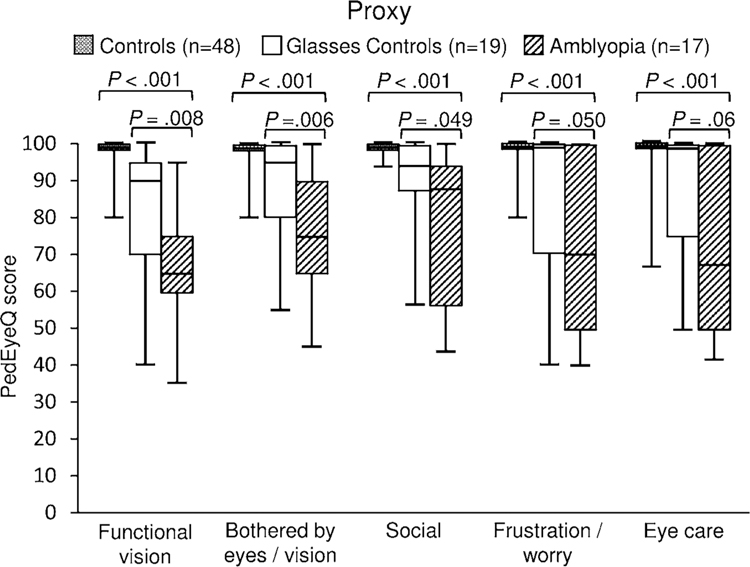
Proxy PedEyeQ
Using the Proxy PedEyeQ, amblyopic children again had lower scores across the five domains than visually normal controls not wearing glasses (P<.001 for each; Figure 2; Table 2). The greatest difference was on the functional vision domain (median 65 vs 100; mean difference −31; 95% CI −39 to −24; P<.001; Figure 2; Table 2).
Figure 2.
Proxy Pediatric Eye Disease Questionnaire (PedEyeQ) domain scores for children with residual amblyopia compared with children with visually normal controls not wearing glasses and compared with visually normal controls wearing glasses. As reported by the parent, amblyopic children had lower scores than controls not wearing glasses on all 5 domains, and lower scores than controls wearing glasses on 4 of the 5 domains (functional vision, bothered by eyes/vision, frustration/worry, and eye care).
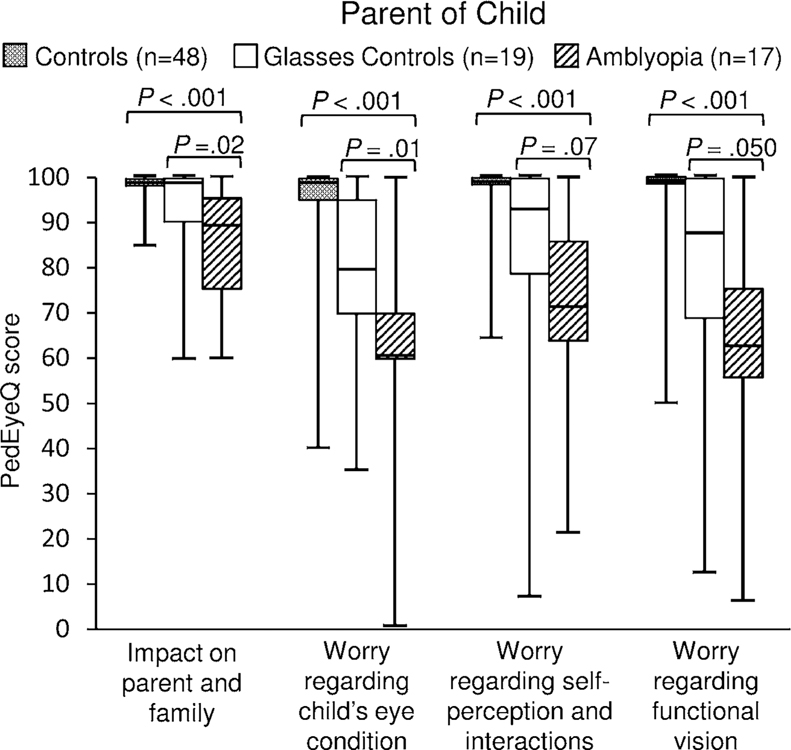
Parent PedEyeQ
Parent PedEyeQ scores were lower on each domain for parents of children with residual amblyopia than for parents of visually normal children (P<.001 for each; Figure 3; Table 2). The greatest difference was on the worry about child’s eye condition domain (median 60 vs 100; mean difference −34; 95% CI −46 to −22; P<.001; Figure 3; Table 2).
Figure 3.
Parent Pediatric Eye Disease Questionnaire (PedEyeQ) domain scores for parents of children with residual amblyopia compared with parents of visually normal controls not wearing glasses and compared with visually normal controls wearing glasses. Parents of amblyopic children had lower scores than parents of visually normal controls not wearing glasses on each of the 4 domains, and lower scores than parents of visually normal controls wearing glasses on 3 of the 4 domains (impact on the parent/family, worry about child’s eye condition, and worry about the child’s self-perception/interactions).
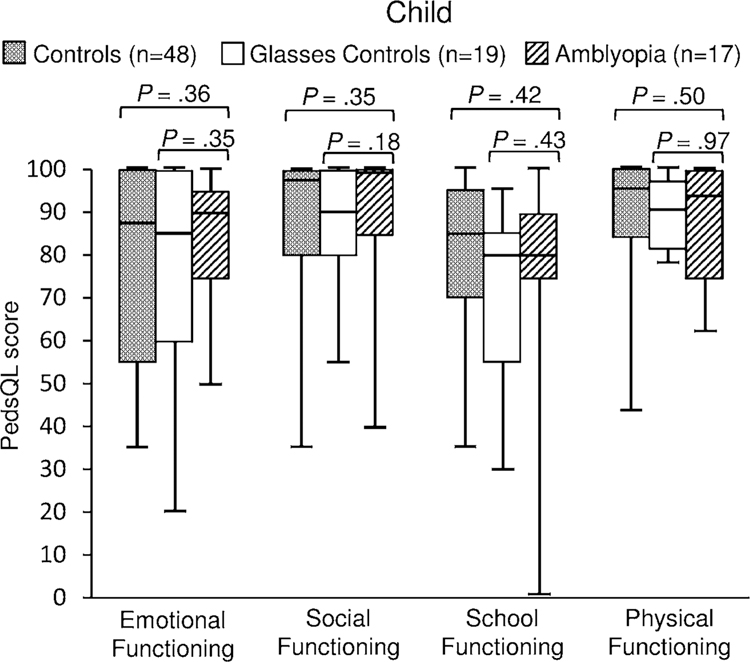
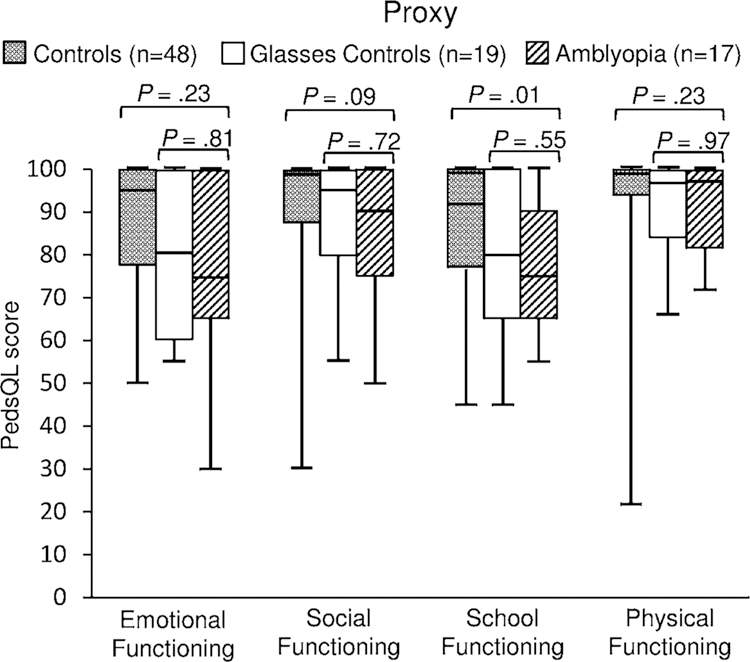
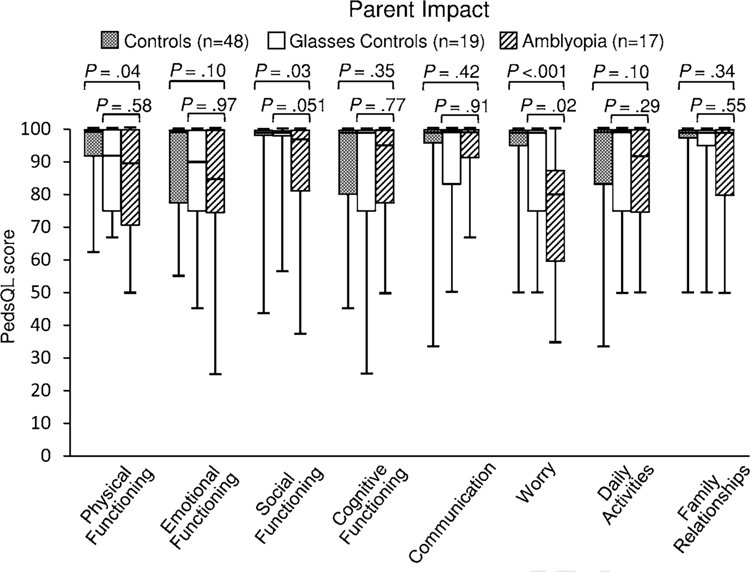
PedsQL
Child 8–12 years PedsQL scores were similar between children with residual amblyopia and visually normal controls not wearing glasses (P≥.35 for each; Figure 4; eTable). By proxy report, scores were lower for amblyopic children on the school functioning domain (median 75 vs 93; mean difference −10; 95% CI −19 to −1; P=.01; Figure 5; eTable) but similar on other Proxy PedsQL domain scores (P ≥.09 for each; Figure 5; eTable). Using the PedsQL Family Impact Module, scores were lower for 3 of the 8 domains: physical functioning (median 90 vs 100; mean difference −9; 95% CI −16 to −1; P=0.04), social functioning (median 97 vs 100; mean difference −6; −15 to 2; P=.03), and worry (median 80 vs 100; mean difference −19; 95% CI −30 to −8; P<.001) (Figure 6; eTable).
Figure 4.
Child Pediatric Quality of Life Inventory (PedsQL) domain scores for children with residual amblyopia compared with visually normal controls not wearing glasses and compared with visually normal controls wearing glasses. Scores were similar across domains between amblyopic children and controls not wearing glasses, and amblyopic children and controls wearing glasses.
Figure 5.
Proxy Pediatric Quality of Life Inventory (PedsQL) domain scores for children with residual amblyopia compared with visually normal controls not wearing glasses and compared with visually normal controls wearing glasses. As reported by the parent, amblyopic children had lower scores than controls not wearing glasses on the School functioning domain. There were no differences between amblyopic children and controls wearing glasses.
Figure 6.
Pediatric Quality of Life Inventory (PedsQL) Family Impact Module scores for parents of children with residual amblyopia compared with parents of visually normal controls not wearing glasses and parents of visually normal controls wearing glasses. Scores were lower for parents of amblyopic children than for parents of visually normal controls not wearing glasses on 3 of the 8 domains (Physical functioning, Social functioning, Worry) and lower for parents of amblyopic children than controls wearing glasses on the Worry domain.
Residual amblyopia versus controls wearing glasses
Child PedEyeQ
Compared with controls wearing glasses, children with residual amblyopia had significantly lower scores on the Child PedEyeQ frustration / worry domain (80 vs 90; mean difference −9; 95% CI −18 to 1; P=.03; Figure 1, Table 2). Scores were similar between children with residual amblyopia and glasses controls on the other three Child PedEyeQ domains (Figure 1, Table 2).
Proxy PedEyeQ
Using the Proxy PedEyeQ, children with residual amblyopia scored significantly lower than controls wearing glasses on 4 of the 5 domains: functional vision (65 vs 90; mean difference −15; 95% CI −26 to −3; P=.008), bothered by eyes and by vision (75 vs 95; mean difference −13; 95% CI −23 to −2; P=.006), social (88 vs 94; mean difference −14; 95% CI −26 to −2, P=.049), and frustration/worry (70 vs 100; mean difference −14; 95% CI −29 to 1, P=.050) (Figure 2, Table 2).
Parent PedEyeQ
Parent PedEyeQ scores were lower for parents of children with residual amblyopia than for parents of controls wearing glasses on three of the four domains: impact on parent/family (90 vs100; mean difference −9; 95% CI −17 to −1, P=.02), worry about child’s eye condition (60 vs 80; mean difference −17; 95% CI −31 to −3, P=.01), and worry about functional vision (62 vs 87; mean difference −13; 95%CI −28 to −2, P=.050) (Figure 3, Table 2).
PedsQL
All domains of the Child and Proxy PedsQL were similar between children with residual amblyopia and controls wearing glasses (P≥18 for each; Figures 4 and 5, eTable). Using the PedsQL Family Impact Module, scores were lower only on the worry domain (median 80 vs 87; mean difference −14; 95% CI −27 to −2; P=.02; Figure 6, eTable).
DISCUSSION
Children with residual amblyopia have reduced functional vision and ER-QOL across domains compared with visually normal controls, by both child self-report (using the Child PedEyeQ) and by proxy report (using the Proxy PedEyeQ). Parents of children with residual amblyopia also report reduced quality of life compared with parents of visually normal children (using the Parent PedEyeQ). Assessing general HRQOL using the child and proxy PedsQL, there was minimal impact of amblyopia. Nevertheless, parents of amblyopic children reported significant impact using the PedsQL Family Impact Module.
Most previous studies assessing quality of life in children with amblyopia by child self-report are designed to assess the impact of specific amblyopia treatments. Nevertheless, Webber et al24 found lower social acceptance in children with residual / recovered amblyopia assessed using the Self Perception Profile for Children and Birch et al25 found reduced scholastic, social and athletic competence in children with residual amblyopia. Sabri et al26 found worse scores on the Psychological Impact Questionnaire for older teenagers (16–18 years old) with residual amblyopia when compared with normal controls. In the present study we directly measured child-reported ER-QOL using the Child component of the PedEyeQ, and found scores were significantly lower across bothered by eyes/vision, social, and frustration/worry domains when compared with visually normal controls, confirming that children with residual amblyopia experience a range of quality of life concerns in their everyday life.
Regarding Proxy report, there are few previous data on the impact of amblyopia. Bogdănici et al,27 assessed quality of life in children with amblyopia (prior to treatment) by proxy evaluation and reported that the majority had poor school results, but did not report other concerns. We also found significantly lower school functioning scores in 8–11 year olds with residual amblyopia, compared with normal controls not wearing glasses using the proxy PedsQL (eTable). In addition, the Proxy PedEyeQ functional vision domain includes questions regarding schoolwork, and these domain scores were lower for children with residual amblyopia, compared with normal controls not wearing glasses (Table 2, Figures 1 and 2). Proxy evaluation of a child’s quality of life remains an important avenue of assessment, especially in young children where self-report may be limited. The PedEyeQ provides a means of assessing ER-QOL from both child and parent/caregiver perspectives. Data from the present study confirm that the PedEyeQ is sensitive to concerns of children with residual amblyopia when made by proxy report.
Considering functional vision, as distinct from ER-QOL, we found reduced functional vision in children with residual amblyopia, by both child self-report and by proxy report. Concerns included problems with schoolwork, learning and concentrating, general difficulties seeing, and running into things (full questionnaires available at: https://public.jaeb.org/pedig/view/Other_Forms). Impaired functional vision in amblyopia has been reported by others: Sabri et al26 administered the Visual Function-14 questionnaire and found worse scores in 16–18 year olds with amblyopia when compared with normal controls. In addition, in skill-based assessments, amblyopia has been associated with poor reading speed,11 reduced scholastic and athletic competence,25 and reduced physical competence.28 Data from the present study suggest that the new PedEyeQ provides insight regarding the type of functional vision deficits experienced by children with residual amblyopia.
Since glasses wear is almost universally a part of amblyopia treatment, and we had previously found that glasses wear for refractive error reduces functional vision and ER-QOL,20 we performed secondary analyses to evaluate the impact of residual amblyopia, above and beyond the impact of glasses wear itself. Given our previous findings regarding the impact of glasses wear,20 we anticipated that differences between children with residual amblyopia and normal controls wearing glasses might be less pronounced than when comparing with controls without glasses. The findings of the present study suggest that there is an impact of amblyopia that exceeds the impact of glasses wear alone. In other studies, Koklanis et al29 aimed to identify the effects of amblyopia itself as distinct from the effects of treatment, but concluded that there is little impact of amblyopia until treatment is commenced.29 Choong et al30 compared psychosocial well-being (proxy-rated) and parental stress before any amblyopia treatment and then again while wearing glasses, and also occlusion, and did not find any differences. Guimarães et al31 evaluated HRQOL, stress, anxiety and depression using generic instruments in children with refractive amblyopia treated with glasses alone, or with glasses plus occlusion and found no differences at least one year following cessation of occlusion. The absence of differences in previous studies may be attributable in part to the use of generic instruments that were insensitive to amblyopia-specific concerns and it would be of value to further evaluate the impact of amblyopia itself versus the impact of specific amblyopia treatments using the PedEyeQ.
In addition to evaluating functional vision and ER-QOL, we also assessed general HRQOL using the generic PedsQL instrument. By child and proxy report we found few differences between children with residual amblyopia and controls (only difference was school functioning domain on proxy report). These findings are consistent with those of Wen et al32 who found no differences between children with amblyopia (n=71) and those without amblyopia (n=3247) using the proxy PedsQL. Although we found few differences between amblyopic children and controls using the PedsQL, we did find differences between amblyopic children and controls using the PedEyeQ, suggesting that the PedEyeQ is more sensitive to the specific concerns of children with residual amblyopia than the PedsQL. There were numerically small but statistically significant differences in median values on some PedsQL scales, reflecting different distributions within each population, but these may not reflect meaningful differences.
This study is not without limitations. By requiring at least one month with no treatment other than glasses, we aimed to isolate the effect of residual amblyopia per se on functional vision and ER-QOL, as distinct from the effects of amblyopia treatments. However it is unknown whether the memory of previous treatments affected responses, despite being instructed to consider experience over the past month only. Ideally, the impact of residual amblyopia itself would be evaluated prior to the commencement of any treatment, but this may be practically difficult to achieve, and evaluation of residual amblyopia provides a reasonable surrogate. An additional limitation is that when administering any questionnaire it is possible that the respondent is alerted to a concern that they may not otherwise have articulated. Nevertheless, in designing the PedEyeQ, items were generated based on semi-structured interviews with children and their parents and worded to minimize leading the respondent. We had relatively small numbers which precluded analyses of the potential impact of severity of residual amblyopia on functional vision and ER-QOL, or of the broader relationship with normal and varying degrees of subnormal visual acuity, but we plan to evaluate this in future studies. We also had insufficient numbers to analyze the effect of small-angle strabismus, or the type and magnitude of refractive error, nevertheless the focus of the present study was on evaluating the overall impact of residual amblyopia. In addition we did not study the relative changes in PedEyeQ scores from before to after treatment, or evaluate interventions to improve quality of life, or determine and these would be of interest in future studies.
Residual amblyopia affects reported functional vision and ER-QOL in children, as assessed using both child and proxy components of the recently-developed PedEyeQ. Parents of amblyopic children also report lower quality of life as assessed using the Parent PedEyeQ. The nature of concerns in children with residual amblyopia and their parents, reflected in lower scores across distinct PedEyeQ domains, helps broaden our understanding of the everyday impact of this common eye condition. The PedEyeQ may be useful for clinical management and in future amblyopia research.
Supplementary Material
ACKNOWLEDGMENTS:
a. Funding/Support: Financial assistance for this study came from National Institutes of Health Grants EY024333 (JMH, PI & EEB, Co-I), and EY022313 (EEB), and Mayo Foundation, Rochester, Minnesota.
b. Financial Disclosures: None of the authors have any financial disclosures
c. Other Acknowledgments: None
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.McKean-Cowdin R, Cotter SA, Tarczy-Hornoch K, et al. Prevalence of amblyopia or strabismus in Asian and non-Hispanic white preschool children: Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology 2013;120:2117–2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friedman DS, Repka MX, Katz J, et al. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months. The Baltimore Pediatric Eye Disease Study. Ophthalmology 2009;116:2128–2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Webber AL, Wood J. Amblyopia: prevalence, natural history, functional effects and treatment. Clin Exp Optom 2005;88:365–375. [DOI] [PubMed] [Google Scholar]
- 4.Abraham SV. Accommodation in the amblyopic eye. Am J Ophthalmol 1961;52:197–200. [DOI] [PubMed] [Google Scholar]
- 5.Agrawal R, Conner IP, Odom JV, Schwartz TL, Mendola JD. Relating binocular and monocular vision in strabismic and anisometropic amblyopia. Arch Ophthalmol 2006;124:844–850. [DOI] [PubMed] [Google Scholar]
- 6.Ciuffreda KJ, Hokoda SC, Hung GK, Semmlow JL, Selenow A. Static aspects of accommodation in human amblyopia. Am J Optom Physiol Opt 1983;60:436–449. [DOI] [PubMed] [Google Scholar]
- 7.Kelly KR, Jost RM, De La Cruz A, Birch EE. Amblyopic children read more slowly than controls under natural, binocular reading conditions. J AAPOS 2015;19:515–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKee SP, Levi DL, Movshon JA. The pattern of visual deficits in amblyopia. J Vis 2003;3:380–405. [DOI] [PubMed] [Google Scholar]
- 9.Rutstein RP, Corliss D. Relationship between anisometropia, amblyopia, and binocularity. Optom Vis Sci 1999;76:229–233. [DOI] [PubMed] [Google Scholar]
- 10.Weakley DR Jr. The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity. Ophthalmology 2001;108:163–171. [DOI] [PubMed] [Google Scholar]
- 11.Birch EE, Kelly KR. Pediatric ophthalmology and childhood reading difficulties: Amblyopia and slow reading. J AAPOS 2017;21:442–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kelly KR, Jost RM, De La Cruz A, et al. Slow reading in children with anisometropic amblyopia is associated with fixation instability and increased saccades. J AAPOS 2017;21:447–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Webber AL, Wood JM, Gole GA, Brown B. The effect of amblyopia on fine motor skills in children. Invest Ophthalmol Vis Sci 2008;49:594–603. [DOI] [PubMed] [Google Scholar]
- 14.O’Connor AR, Birch EE, Anderson S, Draper H. Relationship between binocular vision, visual acuity, and fine motor skills. Optom Vis Sci 2010;87:942–947. [DOI] [PubMed] [Google Scholar]
- 15.Kumaran SE, Khadka J, Baker R, Pesudovs K. Patient-reported outcome measures in amblyopia and strabismus: a systematic review. Clin Exp Optom 2018;101:460–484. [DOI] [PubMed] [Google Scholar]
- 16.Hatt SR, Leske DA, Castañeda YS, et al. Development of pediatric eye questionnaires for children with eye disease. Am J Ophthalmol 2019;200:201–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hatt SR, Leske DA, Castañeda YS, et al. Patient-derived questionnaire items for patient-reported outcome measures in pediatric eye conditions. J AAPOS 2018;22:445–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drover JR, Felius J, Cheng CS, Morale SE, Wyatt L, Birch EE. Normative pediatric visual acuity using single surrounded HOTV optotypes on the Electronic Visual Acuity Tester following the Amblyopia Treatment Study protocol. J AAPOS 2008;12:145–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leske DA, Hatt SR, Castañeda YS, et al. Validation of the Pediatric Eye Questionnaire (PedEyeQ) in children with visual impairment. Am J Ophthalmol 2019;208:124–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leske DA, Hatt SR, Castañeda YS, et al. Eye-related quality of life and functional vision in children wearing glasses. J AAPOS 2020. [DOI] [PMC free article] [PubMed]
- 21.Hatt SR, Leske DA, Castañeda YS, et al. Association of strabismus with reduced functional vision and eye-related quality of life in children. JAMA Ophthalmol 2020. in press. [DOI] [PMC free article] [PubMed]
- 22.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999;37:126–139. [DOI] [PubMed] [Google Scholar]
- 23.Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P. The PedsQL Family Impact Module: preliminary reliability and validity. Health Qual Life Outcomes 2004;2:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Webber AL, Wood JM, Gole GA, Brown B. Effect of amblyopia on self-esteem in children. Optom Vis Sci 2008;85:1074–1081. [DOI] [PubMed] [Google Scholar]
- 25.Birch EE, Castañeda YS, Cheng-Patel CS, et al. Self-perception of school-aged children with amblyopia and its association with reading speed and motor skills. JAMA Ophthalmol 2019;137:167–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sabri K, Knapp CM, Thompson JR, Gottlob I. The VF-14 and psychological impact of amblyopia and strabismus. Invest Ophthalmol Vis Sci 2006;47:4386–4392. [DOI] [PubMed] [Google Scholar]
- 27.Bogdanici ST, Costin D, Bogdanici CM. Quality of life for amblyopic children and their parents. Rev Med Chir Soc Med Nat Iasi 2015;119:214–220. [PubMed] [Google Scholar]
- 28.Birch EE, Castañeda YS, Cheng-Patel CS, et al. Self-perception in children aged 3 to 7 years with amblyopia and its association with deficits in vision and fine motor skills. JAMA Ophthalmol 2019;137:499–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koklanis K, Abel LA, Aroni R. Psychosocial impact of amblyopia and its treatment: a multidisciplinary study. Clinical and Experimental Ophthalmology 2006;34:743–750. [DOI] [PubMed] [Google Scholar]
- 30.Choong YF, Lukman H, Martin S, Laws DE. Childhood amblyopia treatment: psychosocial implications for patients and primary carers. Eye 2004;18:369–375. [DOI] [PubMed] [Google Scholar]
- 31.Guimaraes S, Carcao AA, Carvalho MR, Vieira MJ, Freitas C, Morgado P. Quality of life and mental health in amblyopic children treated with and without occlusion therapy. J AAPOS 2019;23:339.e1–339.e5. [DOI] [PubMed] [Google Scholar]
- 32.Wen G, McKean-Cowdin R, Varma R, et al. General health-related quality of life in preschool children with strabismus or amblyopia. Ophthalmology 2011;118:574–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.