Abstract
Objective:
This study aimed to assess the impact of non-pharmaceutical interventions on the COVID-19 epidemic in Oman.
Methods:
Data were retrieved from published national surveillance data between 24 February and 30 June 2020. To show the impact of the Government introduced public health intervention early in the epidemic, we used a simple disease-transmission model equation of the 2019-n CoV epidemic.
Results:
From all confirmed cases, the rates of intensive care unit admission were 4.56% (1824). We estimated an R0 of 3.11 with no intervention would result in nearly the entire population of Oman being infected within 65 days. A reduction of the R0 to 1.51 provided an estimated 89,056 confirmed cases, with 167 deaths or 0.4% mortality by June 30 with a requirement of 4052 intensive care unit beds. The current scenario (24 February to 30 June 2020) indicates an R0 of 1.41, resulting in 40,070 confirmed COVID-19 cases, 176 deaths and 69% of confirmed cases recovered.
Conclusion:
In early implementation of non-pharmaceutical interventions, an intensive lockdown has had a profound impact on the mitigation of a large-scale COVID-19 outbreak in Oman.
Keywords: COVID-19, Oman, non-pharmaceutical interventions, disease-transmission model
Advances in knowledge
We are presenting the results of epidemiological modelling, which will inform the policy-making that the COVID-19 pandemic containment strategies in Oman based on non-pharmaceutical interventions (NPIs) appear to be effective to scale back transmission of the virus.
Application to patient care
Our findings support early published modelling results, that within the absence of implementation of preventive and control measures in Oman, a COVID-19 outbreak could spread exponentially and overwhelm a healthcare system.
Early NPI implementation reduced the speed of transmission of COVID-19 in Oman.
Introduction
The 2019 novel coronavirus outbreak first reported in Wuhan city, Hubei Province, China, in December 20191 was proclaimed as a Public Health Emergency of International Concern by the World Health Organization (WHO) on 30 January 2020. By this time, there were 7736 cases and 179 deaths confirmed in the mainland China, and 107 cases confirmed in 21 other countries.2 By the end of June, the disease has spread to over 210 countries across all continents, with 10,688,547 confirmed cases of COVID-19 reported, including 516,383 deaths (8% case fatality rate (CFR)) and approximately 5.8 million recoveries.3
In the Eastern Mediterranean Region (EMR), COVID-19 had spread to all 22 countries by June 2020. The first five cases were reported in the United Arab Emirates (UAE) between 25 and 30 January 2020, and they notably had arrived from Wuhan City, China.4 The Islamic Republic of Iran confirmed an outbreak of COVID-19 on 19 February 2020 following two deaths from COVID-19 in Qom city. The virus spread rapidly across all 31 provinces within 2 weeks in Iran as the country did not adopt any quarantine or traffic restriction policies and other risk mitigation strategies.5 A total of 230, 211 confirmed cases were reported in Iran as of 30 June 2020, with only 27,766 cases being active. Saudi Arabia had the highest number of active cases 31% (59,767) of the confirmed cases.3
In Oman, the first two COVID-19 cases were notified on 24 February from the Muscat governorate (province), the capital of Oman, and were linked to travel to the Islamic of Iran.6,7 The disease then spread across all governorates in Oman, and by end of June, there were 40,045 confirmed cases, 16,847 (41%) active cases and a 0.62% CFR.5 Non-pharmaceutical interventions (NPIs) are the pillars of the public health response to the ongoing COVID-19 outbreaks. To describe the impact of NPIs8 in Oman from the notification of the COVID-19 outbreak until the 30 June 2020 to support evidence-based decision-making during various stages of the COVID-19 epidemic.
NPIs in Oman
Upon notification of the first case on 24 February and up to 30 June 2020, Oman has implemented unprecedented NPIs including screening of all arrivals, early case detection, isolation of sick and suspected, contact tracing and quarantine of exposed persons, wearing masks at the place of work, a physical distancing between everyone and those who have COVID-19 and those who do not. Additional interventions commenced on 12 March, including airport screening, stopping tourist visas and decreasing the non-essential national workforce by 30%. Social distancing measures were enforced. This was followed by the closure of parks, schools, malls and mosques, and restrictions in social gatherings such as postponement of large public events and mass gatherings like weddings.
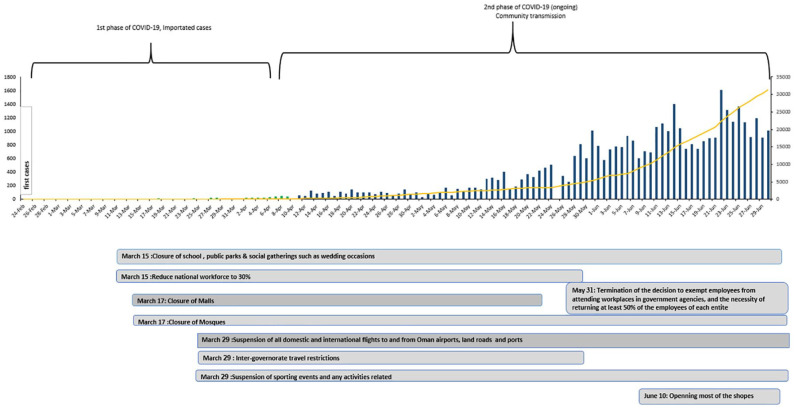
All shops were closed except for the essential ones. Air, land and sea borders in Oman were closed at the end of March. Inter-government travel restrictions were deployed across the country on 1 April, in all governorates, with a complete lockdown in the Mutrah Wilayat (district) in Muscat when a cluster of cases reported. This was followed by a total lockdown in the Muscat district. Lockdown measures were eased after 6 weeks on 31 May, with a return of 50% of government employees. On 10 June, most of the shops were allowed to open except in a few districts (Figure 1).
Figure 1.
Trend of COVID cases, and non-pharmaceutical intervention implemented.
Methodology
Data were retrieved from published national surveillance data9 between 24 February and 30 June 2020 and variables included the number of confirmed cases, the source of infection and patients’ outcomes (including recovery, hospitalization and mortality). To demonstrate the impact of public health intervention measures that were introduced early in the outbreak in Oman, we used simple disease-transmission model equation of the 2019-n CoV epidemic, and an excel mathematical model (spreadsheet model)10 to estimate the impact of the aforementioned control and mitigation strategies.
The projection model
The model is based on the following simple disease-transmission model equation of the 2019-n CoV epidemic.11
The first part of the equation represents exponential growth without control measures. R0 (pronounced ‘R-naught’) stands for the basic reproductive number. The variable t represents the number of serial intervals that have passed the upper limit of our sum. A serial interval is how long it takes on average for an infected person to spread the disease to R0 others. There are many different estimates of the serial duration from as little as 4 days to as long as 7.5 days. For our model, we used 5 days. i represents where to start. For the first part of the equation, this is 0 because we are starting at the beginning.
Controls implemented
The difference is the value of R, now Re, known as the effective reproduction rate. This number should be lower than R0 due to the introduction of control measures such as testing, quarantines and perhaps even the invention of a vaccine.
We modelled the different scenarios based on the following assumptions: (1) no intervention or controls, we used an estimate of R0 at 3.11 and a CFR of 2.63%.12 Two scenarios for early intervention 4 weeks after the first case were modelled using a mean R0 of 1.41; (2B) and a mean R0 of 1.57 the upper most point of the 95% confidence interval. The late two scenarios modelled were based on a late intervention of 6 weeks after first case with a mean R0 of 1.41 and R0 of 1.57 the upper most point of the 95% confidence interval.
The weekly and the overall average for the reproductive rate including the 95% confidence interval during the first 100 days were calculated for Oman. The mean and median were centrally distributed. Therefore, we used the average R0 and the upper end of the confidence interval to model the various scenarios. The fatality rate was calculated at 0.6% during the first 100 days.
Data analysis
To estimate the proportion of patients requiring intensive care unit (ICU) admission, we used the conservative estimate of 5% based on evidence from the Wuhan epidemic. The data indicate 2.3% of all confirmed cases or 46% of patients who were admitted to the ICU were on mechanical ventilation.13
Previous data from China show that 15% of all cases would be severe enough to warrant admission. However, later in the epidemic aggregated data from China and other countries point out that hospitalization rates varied by age group, with an admission rate of 4.25% (2.53–8.68), 8.16% (4.86–16.7), 11.8% (7.01–24.0) and 16.6% (9.87–33.8) for 40–49 years; 50–59 years, 60–69 years and 70–79 years, respectively. Overall, the projected proportion of patients admitted with severe COVID-19 disease was 25% of all cases.14 For this study, we presumed 25% of all confirmed cases would have a severe COVID-19 infection that warranted admission.
This study does not contravene the internal institutional review board and adheres to the Declaration of Helsinki. Therefore, ethical approval was not required as this study was based on secondary data extracted from an official source.
Results
The first case was confirmed on 24 February and 100 cases were documented in the following 30 days. Of the first 100 cases in Oman, 78 were imported – all were among Omani nationals. Forty cases (51%) from Iran and 18 cases (23%) were imported from the United Kingdom, the United States, Egypt and India. A minority6,7 of the cases originated from Italy and other Gulf countries. Of the first cases, 20 were due to secondary spread contacts. Importantly of the 100 cases, only one patient was admitted to the ICU and there were no recorded mortalities due to COVID-19 in the first 30 days while 67 patients recovered.
By 26 April 2020, the number of confirmed COVID-19 cases had increased 10-fold to over 1000. All cases after 25 March 2020 were locally acquired infections due to community transmission. Of the first 1000 cases, only 10% were non-Omani’s expatriates. The CFR was 0.5% of all confirmed cases. On day 85 of the outbreak 30 May, the number of confirmed COVID-19 cases surpassed 10,000. Non-Omani expatriates comprised 56% of the infected cases by day 85. The CFR declined to 0.47% of all confirmed cases. The case count increased rapidly with community with ongoing community transmission with cases increasing to 40,000 within reach the next 10,000 confirmed cases declined from 34 to 12 days to 20,000 cases, 10 days to 30,000 cases and 9 days to 40,000 cases (Figure 1). By 30 June, Oman recorded a total of 40,070 confirmed cases with 176 deaths and a CFR of 0.43%. Of the COVID-19 confirmed cases, 4.55% (1824) were admitted to the ICU with 69% (27,771) of confirmed cases have recovered by the end of June. Seventy-seven percent of all confirmed cases were in the Muscat governance, this due to more testing.
Projected COVID-19 cases and mortality
No NPIs
Applying the R0 of 3.11 and a CFR of 2.63%
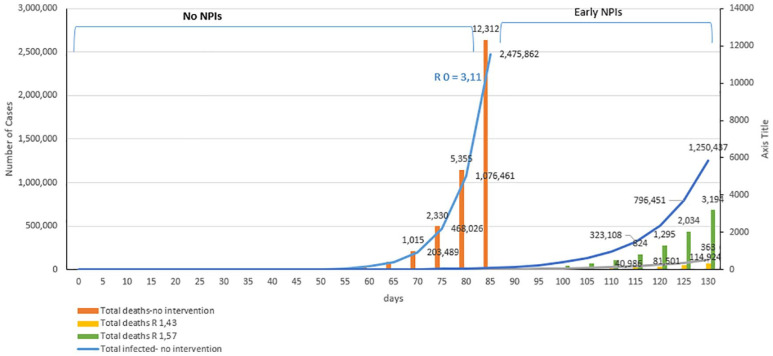
If no interventions were applied in Oman, approximately 70% (3,496,620) of the population would be infected with COVID-19 within 65 days of the first case.10 With a CFR of 2.63%, there would be 9511 deaths due to COVID-19 by day 65. However, if we apply the current CFR of 0.33%, then a total of 2263 deaths will be recorded by day 65. Based on our assumptions, 874,155 patients would require hospital admission and we estimate 174,831 ICU admissions. An estimated 80,418 patients would require mechanical ventilation (Figure 2).
Figure 2.
Impact of implementation of non-pharmaceutical interventions (NPIs).
Impact of the NPIs
Early institution of NPIs (notification of the first case and up to 25 March 2020)
By 25 March 2020, a significant number of NPIs were implemented in Oman, culminating with a complete lockdown. Based on the current trajectory (R0 = 1.41), the number of confirmed cases at day 115 (30 June), estimations from the model predict 40,986 confirmed cases and 129 (CFR = 0.63%) deaths (Figure 1). A total of 10,247 patients will require admissions for severe COVID-19 disease by day 115, 2050 patients to the ICU and 943 requiring mechanical ventilation.14
Projecting the estimates to the upper end of the 95% confidence interval using R0 1.57, there would be an estimated 323,108 cases with 824 deaths (CFR = 0.2%) by 30 June 2020 (Figure 2). An estimated 80,777 would be severe cases warranting hospitalization. ICU admissions are estimated at 16,155 with 7432 patients requiring mechanical ventilation.
Late institution of NPIs (8 weeks since reporting of the first case)
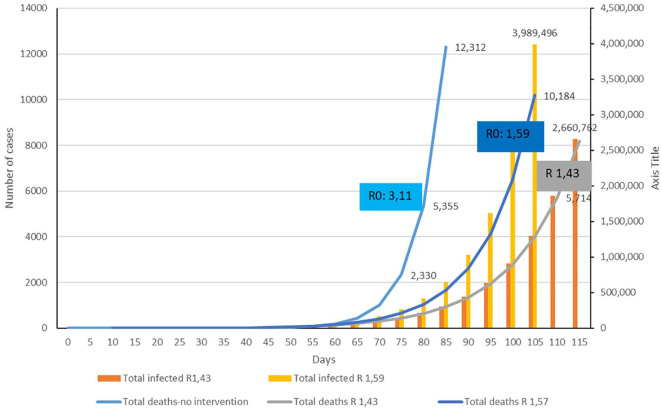
However, should NPIs have been delayed to 8 weeks after the first case on day 115 (30 June), the number of confirmed cases would have reached 2,660,762 with 52% of the population infected (Figure 3). There would have been an estimated 8183 deaths (CFR = 0.3%). An estimated 665,102 hospital admissions, with 133,038 cases requiring ICU admission and 61,198 patients needing mechanical ventilation.
Figure 3.
Late implementation of the non-pharmaceutical intervention (NPI).
A more pessimistic scenario would unfold with the R0 at 1.57 with approximately 80% (3,989,496) of the population being infected by day 105 (20 June 2020). An estimated 10,184 COVID-19-related deaths (CFR = 0.2%) would be recorded. An estimated 997,374 patients would require hospitalization, with 199,475 ICU admissions and 91,758 patients with COVID-19 requiring mechanical ventilation.
Discussion
The intensive lockdown, together with the supporting interventions of social distancing, suspension of all non-essential social gatherings, and the restriction of domestic and international travel have flattened the curve of COVID-19 in Oman.
The number of COVID-19 case numbers of 40,045 at day 115 with the use of earlier or current NPIs is significant less compared to the anticipated 3,496,620 million cases without any NPIs at an earlier point (day 85). This modelling exercise demonstrates that if the interventions had been delayed by a further 4 weeks, 2,660,762 or 52% of the population of Oman would have been infected by 30 June 2020 compared to the 40,045.
Likewise, we observed a large reduction in COVID-19 hospitalization from the 10,986 at day 115 with earlier NPI implementation compared with the estimated model of 874,155 cases without any NPIs. It should be noted that the model is based on the assumption that 25% of the confirmed cases would have severe COVID-19 infection that warranted admission according to Chinese experience. As has been demonstrated by our findings, the number of severe infections requiring hospital admission is far below the model projections.
The model projected the peak number of ICU beds required if no NPIs implemented are 80,418. This is approximately 434 times ICU capacity in Oman, which we presently tallied at 148 beds across the country. With earlier NPIs, there were only 1824 patients admitted to ICU by end of June. This figure is in lined with the projected model figure of 1864 ICU admissions in adopted model.
The reduction in the intensity of the burden added to the healthcare system as demonstrated by the projection and the implementation of NPIs in Oman are supported by a publication of the Imperial College of London that eluded a wide population, social distancing and lockdown implemented to the population would have the highest impact; and in conjunction with other NPIs, namely, home isolation of the COVID-19 cases and school and university closure have the greatest potential to suppress transmission to rapidly reduce the COVID-19 case incidence.15
In Oman, an intense and wide lockdown and strict social distancing measures implemented were maintained until the end of June 2020. Additional modelling studies implemented in the United Kingdom indicate that a combination of intense lockdown measures and physical distancing measures may be able to keep projected the COVID-19 case numbers at a level that would not overwhelm the healthcare system.16 A cross-sectional study conducted among transplant recipients in Saudi Arabia and Italy demonstrated that awareness and adherence to medical advice have a direct influence on the incidence of COVID-19.17
Of concern, the mortality rate for COVID-19 till the end of June 2020 is higher than the projected. As of day 115, 176 deaths were reported in contrast with the model projection of 129. This may be due to complications arising among patients with diabetes and other chronic health conditions or inaccurate allocation of non-COVID-19 mortality as COVID-19 mortality for expediency. Although in Oman 62% of the population are below 55 years of age, the early excessive mortality maybe due to an increased infection in older age group. Previous studies have shown higher than expected mortality in the over 65 years of age group.18
Our study is subject to several limitations as it is based on exponential growth and spread of the epidemic and does not account for the variety of ways in which individuals, and the government may implement NPIs and the varying effectiveness of those controls. It does not also account for possible mutation of the coronavirus (SARS-2), geographic spread and boundaries, and for variation in the population and the age structure of the population when it comes to natural immunity.19 Furthermore, we used data for the first 100 days in which the majority of new cases were in the Muscat governorate (provinces) of Oman and therefore have not accounted for the differences in the various governorates.
Conclusion
Applying a mere model of epidemic growth that caters for the implementation of NPIs efforts can offer helpful insights into the impact or transmission of COVID-19 that are not immediately observable in publicly reported data.
The model indicates a reduction in expected mortality, the number of anticipated hospitalizations, and the need for medical aid, intensive care admissions and mechanical ventilation. Our findings also indicate that early multiple implementations of NPIs of early COVID-19 case detection and patient isolation, the inter-country and governorate travel restrictions, and social distancing have possessed a significant impact on the mitigation of COVID-19 in Oman. The potential for a surge of cases exists with the easing of the lockdown strategy. Therefore, with the easing of lockdown measures, there is a desire to accentuate testing, contact tracing and localized quarantine of suspected cases, including a concerted health promotion strategy in order to sustain behaviour change at a population level and avoid complacency. In addition, it will be valuable to review this model within the next 2 months as the economy is re-opened, and strict intervention measures are eased.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: The ethical approval was not sought for this study because *REASON*. The manuscript reporting data did not include human subjects whatsoever in terms of the interview or using the patient’s direct data file and was based on secondary data extracted from the official national register of surveillance, which already published in an official domain. Therefore, ethical approval was not required as this study was based on secondary data extracted from an official source and adheres to the Declaration of Helsinki.
ORCID iD: Salah Al Awaidy  https://orcid.org/0000-0001-5112-3893
https://orcid.org/0000-0001-5112-3893
References
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382: 727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Durrheim DN, Gostin LO, Moodley K. When does a major outbreak become a public health emergency of international concern? Lancet Infect Dis 2020. Epub ahead of print 23 May 2020. DOI: 10.1016/S1473-3099(20)30401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Worldometer info. Worldometer COVID-19 data, https://www.worldometers.info/coronavirus/ (accessed 20 June 2020).
- 4. World Health Organization. World Health Organization Regional Office for Eastern Mediterranean weekly epidemiological monitor, 2020. Cairo, Egypt: World Health Organization Regional Office for Eastern Mediterranean. [Google Scholar]
- 5. Raoofi A, Takian A, Sari AA, et al. COVID-19 pandemic and comparative health policy learning in Iran. Arch Iran Med 2020; 23: 220–234. [DOI] [PubMed] [Google Scholar]
- 6. Khamis F, Al-Zakwani I, Al Naamani H, et al. Clinical characteristics and outcomes of the first 63 adult patients hospitalized with COVID-19: an experience from Oman. J Infect Publ Healt 2020; 13: 906–913, http://www.elsevier.com/locate/jiph [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Khamis F, Al Rashidi B, Al-Zakwani I, et al. Epidemiology of COVID-19 infection in Oman: analysis of the first 1304 cases. Oman Med J 2020; 35(3): e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization Regional Office for the Western Pacific. Calibrating long-term non-pharmaceutical interventions for COVID-19: principles and facilitation tools. Manila, Philippines: WHO Regional Office for the Western Pacific, 2020, https://apps.who.int/iris/handle/10665/332099 [Google Scholar]
- 9. Ministry of Health, Oman. Statements and updates, https://www.moh.gov.om/en/-5
- 10. Oliver B. A simple model for forecasting the impact of coronavirus and controls, https://www.jirav.com/blog/coronavirus-covid-19-model (2020, accessed 4 July 2020).
- 11. Tuite AR, Fisman DN. Reporting, epidemic growth, and reproduction numbers for the 2019 novel coronavirus (2019-nCoV) epidemic. Ann Inter Med 2020; 172: 567–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yadav S, Yadav PK. Basic reproduction rate and case fatality rate of COVID-19: application of meta-analysis. Medrxiv 2020, https://www.medrxiv.org/content/10.1101/2020.05.13.20100750v1
- 13. O’Driscoll M, Dos Santos GR, Wang L, et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. Epub ahead of print 2 November 2020. DOI: 10.1038/s41586-020-2918-0. [DOI] [PubMed] [Google Scholar]
- 14. Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis 2020; 20(6): 669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ferguson NM, Laydon D, Nedjati-Gilani G, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. London: Imperial College COVID-19 Response Team, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Davies NG, Kucharski AJ, Eggo RM, et al. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health 2020; 5(7): e375–e385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Colbourn T. COVID-19: extending or relaxing distancing control measures. Lancet Public Health 2020; 5: e236–e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Monaco A, Manzia TM, Angelico R, et al. Awareness and impact of non-pharmaceutical interventions during coronavirus disease 2019 pandemic in renal transplant recipients. Transp Proc 2020; 52: 2607–2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Driscoll M, Ribeiro Dos Santos G, Wang L, et al. Age-specific mortality and immunity patterns of SARS-CoV-2 infection in 45 countries. medRxiv. Epub ahead of print 26 August 2020. DOI: 10.1101/2020.08.24.20180851. [DOI] [PubMed] [Google Scholar]