Abstract
Objective
Despite the implementation of advanced health care safety systems including checklists, preventable perioperative sentinel events continue to occur and cause patient harm, disability, and death. We report on findings relating to otolaryngology practices with surgical safety checklists, the scope of intraoperative sentinel events, and institutional and personal response to these events.
Study Design
Survey study.
Setting
Anonymous online survey of otolaryngologists.
Methods
Members of the American Academy of Otolaryngology–Head and Neck Surgery were asked about intraoperative sentinel events, surgical safety checklist practices, fire safety, and the response to patient safety events.
Results
In total, 543 otolaryngologists responded to the survey (response rate 4.9% = 543/11,188). The use of surgical safety checklists was reported by 511 (98.6%) respondents. At least 1 patient safety event in the past 10 years was reported by 131 (25.2%) respondents; medication errors were the most commonly reported (66 [12.7%] respondents). Wrong site/patient/procedure events were reported by 38 (7.3%) respondents, retained surgical items by 33 (6.4%), and operating room fire by 18 (3.5%). Although 414 (79.9%) respondents felt that time-outs before the case have been the single most impactful checklist component to prevent serious patient safety events, several respondents also voiced frustrations with the administrative burden.
Conclusion
Surgical safety checklists are widely used in otolaryngology and are generally acknowledged as the most effective intervention to reduce patient safety events; nonetheless, intraoperative sentinel events do continue to occur. Understanding the scope, causes, and response to these events may help to prioritize resources to guide quality improvement initiatives in surgical safety practices.
Keywords: sentinel events, checklist, otolaryngology, adverse events, patient safety events, operating room safety, operating room fire, wrong-site surgery, wrong-patient surgery, retained foreign body, medical error, patient safety, quality improvement
The Joint Commission defines sentinel events as unexpected occurrences involving death or serious physical or psychological injury or the risk thereof.1 Such events are called “sentinel” because they signal the need for immediate investigation and response. Although The Joint Commission allows hospitals to define their own list of additional sentinel events, mandatory reportable surgical events include surgery on the wrong patient, surgery on the wrong site, performing the wrong procedure, operating room fire, and unintended retention of a foreign object. Sentinel events overlap with the National Quality Forum (NQF) list of serious reportable errors (termed colloquially as “never events”).2
The surgical checklist was adapted from the aviation industry to eliminate catastrophic accidents and is currently used in approximately 75% of operating rooms around the world.3 Checklists encompass many commonly labeled facets including preoperative huddles, in-room boarding process, preincisional time-outs, postoperative debriefs, and transfers to the next level of care. Checklists serve to increase communication, standardize review of pre- and postsurgical concerns, and prevent sentinel events. Although surgical checklists are now widely used, adherence to optimal use is variable. Furthermore, much of the evidence supporting checklists has centered around general surgery,4,5 while the evidence within otolaryngology has been more limited.
We set out to understand sentinel events that occur in the modern operating room since the World Health Organization (WHO) published the surgical safety checklist as part of their Safe Surgery Saves Lives campaign in 2009, sparking widespread adoption. We surveyed members of the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) on the use of surgical safety checklists, intraoperative sentinel events, and responses to such events. This survey investigated wrong-site, wrong-patient, and wrong-surgery incidents; all types of airway fires; inadvertent administration of wrong medication; and retained surgical items.
Methods
Survey Design
This study was developed and sponsored by the AAO-HNS Patient Safety and Quality Improvement Committee. The survey items, developed based on content from the WHO and NQF standards for checklists and sentinel event reporting, underwent iterative review by the committee members. It was then electronically distributed to all members of the AAO-HNS in February 2020. Respondents were asked about demographic information, checklist use, and 4 categories of patient safety events: wrong-site or wrong-patient surgery, surgical fires, wrong-medication events, and retained surgical items. Respondents who reported 1 or more events were queried about the event and response afterward. Survey questions are included in Supplemental Appendix 1. All responses were anonymous, and all responders were unique. No institutional review board approval was required for this anonymous quality improvement initiative devoid of individual patient data.
In the following article, terms are defined as follows. Patient safety events describe all reported events, although not all events resulted in patient harm. The term sentinel event is used according to The Joint Commission definitions, which consider any event of wrong surgery, fire, and retained foreign objects to be a sentinel event regardless of whether the event causes harm to the patient.6 Other events that also meet The Joint Commission definition of a sentinel event include “a patient safety event that reaches the patients and results in either death, permanent harm or severe temporary harm and intervention to sustain life.”6Wrong-site surgery is used broadly to encompass surgery involving the wrong patient, wrong procedure, wrong laterality, or wrong surgical site. The term wrong medication event is defined similarly broadly, encompassing administration of the wrong medication or wrong dose/concentration in the operating room. The level of harms from patient safety events was categorized by respondents using the National Coordinating Council for Medical Error Reporting and Prevention index.7
Analysis
We used a mixed-methods approach for analysis. Descriptive statistics were used to quantify member characteristics and survey responses. Multivariate logistic regression analyses were used to examine the relationship between demographic factors, use of checklists, and reporting of patient safety events. Forward stepwise regression was used to select variables to be included in the final model. We performed statistical analyses using SPSS, version 26 (IBM, Armonk, NY). We conducted qualitative content analysis on the free-text responses. Two authors (J.D.C. and K.B.) read through all of the free-text responses and categorized responses based on The Joint Commission’s top 10 root causes leading to sentinel events including communication, care planning, human factors, physical environment, health information technology related, medication use, continuum of care, assessment, information related, and leadership.8 Multiple root causes were allowed, and root causes were specified as communication when the sentinel event related to communication with patients, staff, or administration; human factors when relating to staff supervision, including resident or fellow oversight; and care planning involving interdisciplinary collaboration. We also derived 2 new categories for root causes that were not well specified in the established classification schemes, including (1) “Absence of Policies and Procedures,” which was identified on further detailed analysis of Joint Commission analysis of retained surgical items, and (2) “Unable to Retrieve the Retained Item” (derived de novo). A third author adjudicated disagreement in categorization of free-text responses (S.R.).
Results
Demographics
A total of 11,188 survey invitations were sent to members of the AAO-HNS, and 543 (4.9%) AAO-HNS members responded. Demographic characteristics of survey respondents are shown in Table 1 . At least 1 component of a surgical safety checklist was used by 511 (98.6%) respondents ( Table 2 ). In addition, 404 (78%) respondents used a separate time-out specific to the prevention of surgical fires. At least 1 intraoperative sentinel event was reported by 131 (25.2%) of respondents. Two events were reported by 13 respondents (2.5%), 3 events by 4 respondents (0.8%), and 4 events by 1 respondent (0.2%).
Table 1.
Demographic Characteristics of Survey Respondents.
| n | % | |
|---|---|---|
| Gender | ||
| Male | 122 | 22.5 |
| Female | 421 | 77.5 |
| Age, y | ||
| <40 | 105 | 19.3 |
| 40-50 | 295 | 54.3 |
| >50 | 143 | 26.3 |
| Years in practice | ||
| <10 | 144 | 26.5 |
| 10-20 | 273 | 50.3 |
| >20 | 126 | 23.2 |
| Practice type | ||
| Academic | 184 | 33.9 |
| Military | 14 | 2.6 |
| Multispecialty group | 82 | 15.1 |
| Otolaryngology group | 190 | 35.0 |
| Solo | 73 | 13.4 |
| Practice specialty area | ||
| Facial plastic and reconstructive surgery | 30 | 5.5 |
| General otolaryngology | 295 | 54.3 |
| Head and neck oncology | 62 | 11.4 |
| Laryngology | 19 | 3.5 |
| Otology/neurotology | 41 | 7.6 |
| Pediatric otolaryngology | 68 | 12.5 |
| Rhinology/skull base/allergy | 27 | 5.0 |
| Sleep medicine | 1 | 0.2 |
Table 2.
Surgical Safety Checklist Components.
| n | % | |
|---|---|---|
| Q6: Component of a time-out and/or surgical safety checklist used at institution (n = 518) | ||
| Preoperative marking of surgical site | 497 | 95.9 |
| An “All Stop” to direct all attention to the checklist | 379 | 73.2 |
| Time-out to confirm correct patient identification, correct procedure site, and correct procedure | 511 | 98.6 |
| Discussion of any special medications or equipment | 430 | 83.0 |
| Debrief including discussion of instrument, sponge, and needle counts after completion of procedures | 398 | 76.8 |
| No surgical safety checklist or time-out procedure routinely performed | 6 | 1.2 |
| I have no idea what components are included | 2 | 0.4 |
Wrong-Site Surgery
There were 38 (7.3%) of respondents who reported a wrong-site surgical event in the past 10 years ( Table 3 ). Among these events, 15.8% related to tonsillectomy and/or adenoidectomy (for example, tonsillectomy mistakenly completed although only adenoidectomy consented), 13.2% to wrong-side ear surgery, 10.5% to wrong-cutaneous-site surgery, 10.5% to frenulectomy (lip or tongue), 7.9% to wrong-site sinus surgery, 7.9% to wrong-side thyroid surgery, 2.6% to wrong-site oral lesion excision, 2.6% to wrong vocal cord surgery, 2.6% to wrong-site skull base surgery, and 26.3% were unspecified.
Table 3.
Incidence and Type of Sentinel Events.a
| n | % | ||
|---|---|---|---|
| Wrong site, wrong patient, wrong procedure | Q8: Involved in wrong-site, wrong-patient, wrong-procedure surgery in past 10 y (n = 518) | 38 | 7.3 |
| Q9: Type of event (n = 34) | |||
| Wrong-site surgery: laterality | 17 | 50.0 | |
| Wrong-site surgery: anatomic region | 11 | 32.4 | |
| Wrong-patient surgery | 1 | 2.9 | |
| Wrong-procedure surgery | 5 | 14.7 | |
| Wrong medication | Q26: Involved with any case involving inadvertent administration of the wrong medication during surgery in the past 10 y (n = 513) | 66 | 12.7 |
| Q27: Type of medication error (n = 61) | |||
| Injection of concentrated epinephrine (eg, instead of local anesthetic) | 17 | 27.9 | |
| Inadvertent injection of oxymetazoline (Afrin) | 4 | 6.6 | |
| Inadvertent administration of medication to which the patient had a known allergy | 12 | 19.7 | |
| Overadministration of opioids | 2 | 3.3 | |
| Wrong antibiotic | 4 | 6.1 | |
| Anesthetic/paralytic related | 10 | 15.2 | |
| Other topical/intralesional | 3 | 4.5 | |
| Other | 9 | 13.6 | |
| Retained surgical item | Q33: Involved with any case of a retained surgical item in the past 10 y (n =508) | 33 | 6.4 |
| Q34: Type of retained surgical item (n = 32) | |||
| Instrument | 3 | 9.4 | |
| Needle | 1 | 3.1 | |
| Sponge | 9 | 28.1 | |
| Temporary splint or packing (eg, Doyle nasal splint, nasal packing) | 9 | 28.1 | |
| Lost screw/hardware | 1 | 3.1 | |
| Other | 9 | 28.1 | |
| Q35: Factors that contributed to the occurrence of the retained surgical item (n = 48) | |||
| No surgical count | 1 | 2.1 | |
| Error in surgical count | 8 | 16.7 | |
| Item not included in surgical count | 8 | 16.7 | |
| Surgical count erroneously correct | 6 | 12.5 | |
| Item known to be lost, but could not be retrieved | 5 | 10.4 | |
| Time of day (late at night, weekend) | 2 | 4.2 | |
| Multiple teams in operating room | 6 | 12.5 | |
| Unexpected procedures performed | 1 | 2.1 | |
| Obese patient | 1 | 2.1 | |
| Other | 10 | 20.8 | |
Surgical Fire
Eighteen respondents (3.5%) reported a surgical fire ( Table 4 ) in the past 10 years. There were 4 (22.2%) airway fires during endoscopic procedures, 1 (5.6%) airway fire during an open procedure, and 3 (16.7%) other types of fire. These fires occurred during monitored anesthesia care in 5 (27.8%), during endoscopic airway surgery in 2 (11.1%), during endoscopic laser airway surgery in 2 (11.1%), during tonsillectomy in 2 (11.1%), during tracheostomy in 1 (5.6%), and unspecified in 5 (33.4%). Respondents reported no surgical fire time-out in 55.6% of fires (10 of 18 events).
Table 4.
Detailed Questions on Operating Room Fire.
| n | % | |
|---|---|---|
| Q7: Components of an OR fire time-out performed (n = 518) | ||
| Fire rating scale | 310 | 59.8 |
| Discussion of FiO2 | 250 | 48.3 |
| Discussion of potential fuel source | 164 | 31.7 |
| Discussion of potential ignition source | 192 | 37.1 |
| No operating room fire time-out procedure routinely performed | 114 | 22.0 |
| Q15: Involved in an operating room fire in the past 10 years (n = 514) | 18 | 3.5 |
| Q16: Type of OR fire (n = 18) | ||
| External flash fire or equipment/drapes only, no patient harm occurred | 6 | 33.3 |
| External fire resulting in patient harm, non-airway | 4 | 22.2 |
| Airway fire during endoscopic procedure | 4 | 22.2 |
| Airway fire during open procedure | 1 | 5.6 |
| Other type of OR fire | 3 | 16.7 |
| Q21: Components of OR fire time-out performed before the event (n = 18) | ||
| Fire rating scale | 2 | 11.1 |
| Discussion of FiO2 | 3 | 16.7 |
| Discussion of potential fuel source | 2 | 11.1 |
| Discussion of potential ignition source | 3 | 16.7 |
| No OR fire time-out performed | 10 | 55.6 |
| Do not recall | 3 | 16.7 |
| Other | 1 | 5.6 |
| Q17: Fuel source (n = 18) | ||
| Alcohol-based prep solution | ||
| Surgical drapes, towels, sponges, and gauze | 7 | 38.9 |
| Endotracheal tube or laryngeal mask | 5 | 27.8 |
| Organic matter | 1 | 5.6 |
| Other fuel | 5 | 27.8 |
| Q18: Ignition source (n = 18) | ||
| Electrosurgery unit (Bovie, Bipolar, etc) | 12 | 66.7 |
| Surgical laser | 2 | 11.1 |
| Fiber-optic light | 3 | 16.7 |
| Other ignition source | 1 | 5.6 |
Abbreviation: OR, operating room.
Wrong Medication
Cases of inadvertent administration of the wrong medication during surgery ( Table 3 ) were noted by 66 respondents (12.7%). These events included errors injecting concentrated epinephrine (27.9%), administration of a medication to which a patient had a known allergy (19.7%), anesthetic/paralytic related (15.2%), injection of oxymetazoline (6.6%), wrong antibiotic, other topical/intralesional medications, over administration of opioids (3.3%), and other events (13.6%).
Retained Surgical Item
Cases involving a retained surgical item ( Table 3 ) were reported by 33 (6.4%) respondents. The retained surgical items included sponges (28.1%), temporary splint or packing (28.1%), instrument (9.4%), needle (3.1%) lost screw/hardware (3.1%), and other items (28.1%). The factors most strongly associated with retained surgical items included error in surgical count (16.7%), item not included in surgical count (16.7%), multiple teams in the operating room (12.5%), and surgical count erroneously correct (12.5%).
Impact and Response to Sentinel Events
Patient safety events resulting in a least temporary harm (category d-h, Table 5 ) were most common in surgical fires (76.9%) followed by retained surgical items (24.1%), wrong-medication (15.9%), and wrong-site surgery (14.7%). Disclosure to patient and/or family/caregivers occurred in 97.1% of wrong-site surgical events, 86.2% of retained surgical items, 66.7% of wrong-medication events, and 53.8% of surgical fires. Institutional investigations were conducted in 63.2% to 88.4% of cases and most commonly included root cause analysis and actions.
Table 5.
Impact and Response to Sentinel Events.a
| n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| How patient affected by event | (a) Error occurred but did not reach patient | (b) Error occurred and reached patient but no harm | (c) Error occurred and reached patient who required additional monitoring or action to ensure no harm | (d) Error occurred causing temporary harm | (e) Error occurred causing temporary harm, requiring prolonged hospitalization and/or operative intervention | (f) Error occurred causing permanent harm | (g) Error Occurred causing permanent harm, requiring prolonged hospitalization and/or operative intervention | (h) Error occurred that required intervention to sustain life | (j) Other |
| Q10: Wrong site/patient/procedure (n = 34) | 0 (0) | 25 (73.5) | 3 (8.8) | 4 (11.8) | 1 (2.9) | 0 (0) | 0 (0) | 0 (0) | 1 (2.9) |
| Q20: OR fire (n = 13) | 5 (14.7) | 1 (7.7) | 2 (15.4) | 8 (61.5) | 0 (0) | 1 (7.7) | 0 (0) | 1 (7.7) | 0 (0) |
| Q28: Medication error (n = 57) | 4 (11.8) | 29 (50.8) | 18 (31.6) | 1 (1.8) | 5 (8.8) | 0 (0) | 1 (1.8) | 2 (3.5) | 1 (1.8) |
| Q36: Retained surgical item (n = 29) | 3 (8.8) | 15 (51.7) | 4 (13.8) | 2 (6.9) | 5 (17.2) | 0 (0) | 0 (0) | 0 (0) | 3 (10.3) |
| Event disclosed to patient or patient’s family/caregivers | (a) No disclosure (no reference to adverse event or error) | (b) All harmful errors disclosed | (c) Explanation provided for why the error occurred | (d) Discussion of how the error’s effects will be minimized | (e) Steps the physician (and institution) will take to prevent recurrence | (f) Apology for error | (g) Other | ||
| Q11: Wrong site/patient/procedure (n = 34) | 1 (2.9) | 26 (76.5) | 29 (85.3) | 16 (47.1) | 18 (52.9) | 26 (76.5) | 0 (0) | ||
| Q22: OR fire (n = 13) | 6 (46.2) | 8 (61.5) | 10 (76.9) | 2 (15.4) | 6 (46.2) | 5 (38.5) | 1 (7.7) | ||
| Q29: Medication error (n = 57) | 19 (33.3) | 33 (57.9) | 29 (50.9) | 22 (38.6) | 23 (40.4) | 25 (43.9) | 3 (5.3) | ||
| Q37: Retained surgical item (n = 29) | 4 (13.8) | 16 (55.2) | 18 (62.1) | 10 (34.5) | 11 (37.9) | 15 (51.7) | 2 (6.9) | ||
| Corrective action | (a) Financial/legal | (b) Disciplinary | (c) Education-based (including peer mentoring, etc) | (d) No corrective action was taken | (e) Other | ||||
| Q12: Wrong site/patient/procedure (n = 34) | 2 (5.9) | 2 (5.9) | 21 (61.8) | 6 (17.7) | 8 (23.5) | ||||
| Q23: OR fire (n = 13) | 5 (38.5) | 2 (15.4) | 11 (84.6) | 4 (30.8) | 2 (15.4) | ||||
| Q30: Medication error (n = 57) | 2 (3.5) | 3 (5.3) | 32 (56.1) | 19 (33.3) | 11 (19.3) | ||||
| Q38: Retained surgical item (n = 29) | 3 (10.3) | 1 (3.5) | 19 (65.5) | 8 (27.6) | 6 (20.7) | ||||
| Institutional investigation conducted to respond to event | (a) Event occurred but no institutional investigation conducted | (b) Yes, morbidity and mortality conference | (c) Yes, Root cause analysis and actions (RCA2) | (d) Yes, institutional investigation other than RCA2 | (e) Yes, peer review | (f) Unknown | (g) Other | ||
| Q13: Wrong site/patient/procedure (n = 34) | 6 (17.6) | 14 (41.2) | 19 (55.9) | 8 (23.5) | 8 (23.6) | 2 (5.9) | 1 (2.9) | ||
| Q24: OR fire (n = 13) | 3 (23.1) | 3 (23.1) | 8 (61.5) | 5 (38.5) | 3 (23.1) | 3 (23.1) | 0 (0) | ||
| Q31: Medication error (n = 57) | 21 (36.8) | 15 (26.3) | 23 (40.4) | 3 (5.26) | 10 (17.5) | 9 (15.8) | 1 (1.8) | ||
| Q39: Retained surgical item (n = 29) | 6 (20.7) | 13 (44.8) | 13 (44.8) | 4 (13.8) | 4 (13.8) | 3 (10.3) | 3 (10.3) | ||
Abbreviation: OR, operating room.
Level of harms assessed using the National Coordinating Council for Medication Error Reporting and Prevention.
Respondents felt that the interventions that have been most impactful to prevent serious patient safety events ( Table 6 ) were time-outs before case (79.9%), site marking (65.4%), and safety checklists to ensure preventive components (49.6%).
Table 6.
Systems to Track and Respond to Sentinel Events.
| n | % | |
|---|---|---|
| Q41: System at institution to track sentinel events (n = 518) | ||
| Voluntary reporting | 334 | 64.5 |
| Structured chart review (eg, NSQIP, ACS CSV, etc) | 274 | 52.9 |
| Automated capture through HER | 115 | 22.2 |
| Automated capture not build into HER | 27 | 5.2 |
| Unknown | 120 | 23.2 |
| Other | 15 | 2.9 |
| Q42: System at institution to respond to sentinel events (n = 518) | ||
| Morbidity and mortality conference | 299 | 57.7 |
| Root cause analysis and actions (RCA2) | 337 | 65.1 |
| Institutional investigation other than RCA2 | 162 | 31.3 |
| Peer review | 299 | 57.7 |
| None | 13 | 2.5 |
| Other | 24 | 4.6 |
| Q43: Most impactful interventions to prevent serious adverse events in otolaryngology (n = 518) | ||
| Time-outs before case | 414 | 79.9 |
| Debriefs after case | 152 | 29.3 |
| Safety checklists to ensure preventive components | 257 | 49.6 |
| Site marking | 339 | 65.4 |
| Team huddles | 161 | 31.1 |
| None | 30 | 5.8 |
| Other | 47 | 9.1 |
Abbreviations: ACS CSV, American College of Surgeons Children’s Surgery Verification; NSQIP, National Surgical Quality Improvement Program.
Associated Factors
We used logistic regression to evaluate the demographic factors gender, age, years in practice, practice type, specialty area, and use of checklists associated with reporting any patient safety event ( Table 7 ). In our final multivariable model, we found that reporting any patient safety event was associated with provider age <40 years (odds ratio [OR] 1.80, confidence interval [CI] 1.01-3.20) and practice specialty of head and neck oncology (OR 2.75, CI 1.50-5.05) or pediatric otolaryngology (OR 2.42, CI 1.33-4.39) as compared with general otolaryngology (reference). The use of a comprehensive checklist preoperatively was not associated with reporting a patient safety event.
Table 7.
Multivariable Logistic Regression of Factors Associated With Reporting Any Sentinel Event.a
| Univariate logistic regression | Multivariate logistic regression | |||
|---|---|---|---|---|
| OR | CI | OR | CI | |
| Gender | ||||
| Male | 1.00 | (Reference) | ||
| Female | 1.15 | 0.72-1.83 | ||
| Age, y | ||||
| <40 | 1.71 | 0.98-2.97 | 1.80 | 1.01-3.20 |
| 40-50 | 1.00 | (Reference) | Reference | |
| >50 | 0.65 | 0.40-1.05 | 0.73 | 0.45-1.20 |
| Years in practice | ||||
| <10 | 1.76 | 1.03-3.02 | ||
| 10-20 | 1.00 | (Reference) | ||
| >20 | 0.69 | 0.41-1.15 | ||
| Practice type | ||||
| Academic | 1.58 | 0.85-2.94 | ||
| Military | 1.44 | 0.39-5.38 | ||
| Multispecialty group | 0.77 | 0.36-1.64 | ||
| Otolaryngology group | 0.57 | 0.29-1.10 | ||
| Solo | 1.0 | (reference) | ||
| Practice specialty Area | ||||
| General otolaryngology (reference) | 1.0 | (reference) | 1.0 | (reference) |
| Facial plastic and reconstructive surgery | 1.97 | 0.85-4.58 | 1.82 | 0.77-4.27 |
| Head and neck oncology | 3.13 | 1.73-5.68 | 2.74 | 1.50-5.05 |
| Laryngology | 0.82 | 0.23-2.93 | 0.63 | 0.17-2.29 |
| Otology/neurotology | 1.36 | 0.61-3.05 | 1.38 | 0.61-3.13 |
| Pediatric otolaryngology | 2.57 | 1.43-4.62 | 2.42 | 1.33-4.39 |
| Rhinology/skull base/allergy | 2.32 | 0.98-5.50 | 2.19 | 0.87-5.04 |
| Use of checklists | ||||
| Noncomprehensive | 1.0 | (Reference) | ||
| Comprehensive | 0.83 | 0.56-1.23 | ||
Comprehensive checklists include preoperative marking, “All Stop,” confirm patient/procedure/site, discuss special medications, debrief. Bold font indicates significant factors on multivariate logistic regression.
Qualitative Content Analysis
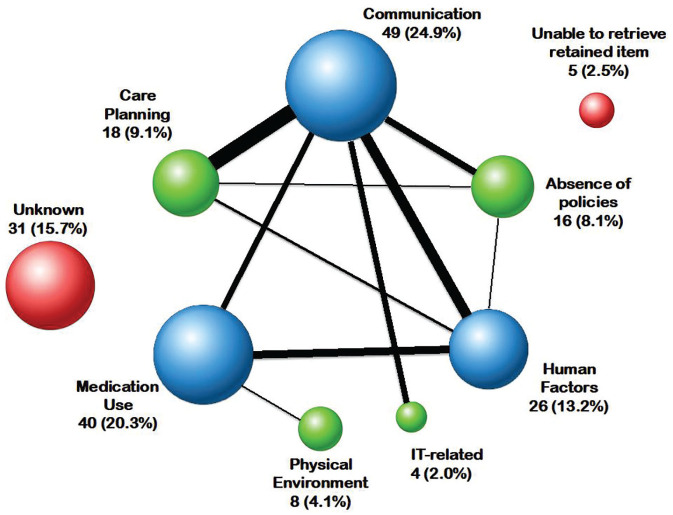
We categorized the root cause of the reported sentinel events into 10 categories based on The Joint Commission definitions. Qualitative analysis revealed 4 categories of root causes that accounted for more than 65% of reported sentinel events: communication (24.9%), medication use (20.3%), human factors (ex: staff supervision issues; 13.2%), and care planning (9.1%). Communication errors represented a hub in root cause analyses, sharing relationships with most other root causes identified ( Figure 1 ). Communication error was more common during wrong-site surgical events (48.1%), whereas absence of policies and procedures was more common in retained surgical items (39.0%; Table 8 ). Select quotes illustrating common root causes of sentinel events and perspectives on checklist use are shown in Tables 9 and 10 .
Figure 1.
Network analysis of root causes of patient safety events. Circle sizes correspond to the frequency of the root cause. Line thickness is proportional to the number of instances in which root causes of intraoperative events were shared. IT, information technology related.
Table 8.
Root Causes of Patient Safety Events.a
| n (%) | |||||
|---|---|---|---|---|---|
| Overall | Wrong-site surgery | OR fire | Medication use | Retained item | |
| Communication | 49 (24.9) | 25 (48.1) | 5 (25.0) | 13 (15.5) | 6 (14.6) |
| Medication use | 40 (20.3) | 40 (47.6) | |||
| Human factors | 26 (13.2) | 8 (15.4) | 14 (16.7) | 4 (9.8) | |
| Care planning | 18 (9.1) | 9 (17.3) | 5 (25.0) | 2 (2.4) | 2 (4.9) |
| Absence policies or procedures | 16 (8.1) | 16 (39.0) | |||
| Physical environment | 8 (4.1) | 6 (30.0) | 2 (2.4) | ||
| Unable to retrieve | 5 (2.5) | 5 (12.2) | |||
| Information technology related | 4 (2.0) | 3 (5.8) | 1 (1.2) | ||
| Unknown | 31 (15.7) | 7 (13.5) | 4 (20.0) | 12 (14.3) | 8 (19.5) |
Patient safety events could be categorized using more than one root cause.
Table 9.
Analysis of Qualitative Responses on Etiologies of Intraoperative Sentinel Events.
| Medication error |
| “1% lido with 1/100k epi being injected but several more mL’s needed. Scrub tech drew 1/1000 epi from plastic cup instead of lido with epi cup. Both cups were labeled correctly but not verified by tech prior to being drawn . . . patient had cardiac arrest.” |
| “The paralytic drug and the xylocaine with epi were in similar injection bottles with red caps and labeling.” |
| Retained foreign bodies |
| “Throat pack not included in count.” |
| “The patient was referred . . . because of his refractory rhinosinusitis. We found retained nasal packing in sinus cavity.” |
| Communication (eg, with patients or administration) |
| “The wrong thyroid lobe was initially removed because of mismarking and partly because of patient confusion.” |
| “Otologic surgical pack left in ear canal over 2 years causing severe foreign-body reaction.” |
| “Child went to the OR for T&A. schedulers mistakenly added BMT to schedule. . . . Time-out was done by nursing . . . without cross referencing the H&P.” |
| Equipment |
| “Light box ignited as fan had stopped working. As it was close to the anesthesia machine.” |
| Unable to retrieve item |
| “Drill bit broke off and floated into vestibule, unable to retrieve.” |
| Care planning (eg, interdisciplinary collaboration) |
| “Micro instrument was dropped into a body cavity and not retrieved . . . at the end of a 16-hour case with multiple teams, learners, and attendings.” |
| “Nurse anesthesia used 100% O2 without notifying surgeon.” |
| “Combined sinus dental procedure. Dental packing placed, was not removed by dental team. Was in sinus. Later extruded.” |
| “Inadvertent anesthetic admin of paralytic agent by a CRNA without alerting the attending.” |
| “A small throat pack was placed by the oral surgery team and placed entirely within the pharynx. The presence of the pack was not handed off to either the ablative or reconstructive team.” |
| “Anesthesia felt needed high O2 to proceed . . . the ETT slipped down a few mm and the laser hit the tip of the ETT.” |
| Health information technology |
| “Preoperative . . . CT mislabeled and misread in radiology, plan for surgery based on imaging, intraoperatively less disease noted after opening sinus.” |
| Human factors (eg, staff supervision issues) |
| “The patient was scheduled for tonsillectomy only; adenoidectomy inadvertently performed by the resident.” |
| “During a break the substitute anesthetist delivered the cephalosporin from the anesthesia drug cart without checking the orders.” |
| “Retained 2 × 2 sponge noted on count. Surgeon denied it was right and the patient was awakened and against protocol was sent to recovery the X-ray there showed the foreign body and patient returned to the OR.” |
| “Resident did not investigate where the Penrose drain was after the procedure. Patient was unsure about what they felt under dressing and pushed it in. . . . Did not have a stitch on drain to make it easier to remove.” |
Table 10.
Analysis of Qualitative Responses Regarding Attitudes Toward Checklists.
| Attitudes and perspectives on checklists | |
|---|---|
| Supportive of checklists/culture of safety | Lack of engagement/perceived burdensomeness |
| “There is simply no replacement of a well-educated, committed, stable operating room team.” | “Time-outs seem to be useless. . . . I think they’ve quickly devolved into nothing.” |
| “Involvement of the surgeon to ensure that any process used is important, valued and utilized regularly. Everyone in room needs to be empowered to help keep the case safe.” | “I find that the continued addition of extraneous environmental allergies have diluted the value of the time-out as one can see team members’ eyes glaze over as impertinent details continue to get added to the lists of required items.” |
| “Fostering a culture where any and all team members can raise concerns or questions without fear or intimidation.” | “Our checklists have become so lengthy and arduous and mostly not relevant to our cases that I feel they do more harm than good by directing attention and discussed away from pertinent things” |
Discussion
Our study highlights patterns of system failure that allow sentinel intraoperative events to persist in otolaryngology. Some of the data confirm what we already knew or suspected: that sentinel events take a variety of forms, that safety checklists are not uniformly embraced by surgeons, and that significant variations in practice exist. Other findings are new and alarming. For example, in more than half of the instances of operating room fires, no fire-related time-out had been conducted. Also, sentinel events were more likely to prompt full root cause analysis and actions than to be discussed at a departmental morbidity and mortality conference. Our study provides a framework for cataloguing the types of errors experienced by otolaryngologists in the modern operating room. Furthermore, root cause analysis and actions of events suggest opportunities for improvement in communication, medication use, care planning, and policies and procedures to prevent future events.
Investigating intraoperative sentinel events is challenging because of their rarity; the estimated incidence of wrong-site surgery is 1 per 100,000 procedures, and the incidence of retained surgical items is 1 per 8000 to 10,000 procedures.9,10 Understanding such events is critical for developing strategies that may prevent future harm to patients. Patient safety events tend to arise from remediable systems failures, and because sentinel events attract notice, they may represent the proverbial visible tip of a much larger iceberg of preventable patient safety events. Previous studies estimated that 9.6% to 10.8% of all errors in otolaryngology may have been prevented with closer adherence to an element on a checklist.11,12
Wrong-Site Surgery
In a previous survey in otolaryngology focusing on endoscopic sinus surgery, 9.3% of respondents described a case of wrong-site surgery13; however, the relevance of this finding to other areas of otolaryngology practice was unclear. In the present study, wrong-site sinus surgery represented only a small portion of reported events. Overall, 82% of wrong-site or wrong-side surgery involved wrong laterality or wrong anatomic region, most commonly related to wrong-ear surgery, wrong-cutaneous-lesion surgery, error in upper versus lower lip frenulectomy, wrong-sinus surgery, and wrong-site thyroid surgery. Wrong-procedure events were also reported, particularly in adenotonsillectomy.
Surgical Fires
Overall, 85% of surgical fires occur during head, neck, or upper chest procedures,14 and previous surveys have identified that 25% of otolaryngologists experience at least 1 surgical fire in their career.15 The pattern of surgical fires was classified by types of surgery, ignition source, and fuel source, and results mirrored findings of a previous survey of otolaryngologists a decade prior,15 suggesting the need for further progress in this area, despite broader adoption of polytetrafluoroethylene-coated Bovie tips that decrease maximal heat and eschar buildup as compared with stainless-steel tips. Of note, previous surveys did not explore the use of surgical fire time-outs. We observed that in 72.3% of surgical fires, a fire time-out was not performed (55.6%) or it was unknown whether or not fire time-out was performed (16.3%). Flash fires during removal of cutaneous lesions were frequently noted, and such episodes are possibly associated with flammable skin disinfection liquids as well as entrained oxygen from surgical draping. Such incidences could be avoided by discouraging the use of alcohol-containing disinfectants during surgeries at high risk for fire, allowing alcohol-based solutions to dry completely before draping, and avoiding administration of open oxygen beneath barrier draping.
Wrong Medication
Previous survey studies identified that 12.7% of otolaryngologists were aware of an error with concentrated epinephrine in the previous year.16 In our survey, wrong medication events were the most frequently reported patient safety event by respondents, and among these, errors involving the delivery of concentrated epinephrine were emphasized. Based on participants’ descriptions of events, preventive measures might include adding color or dye to specific medications; applying of particular medications on pledgets only; maintaining consistency of surgical team members; paying attention to timing of breaks during cases, particularly during shorter cases involving injectable medication; and having heightened awareness of the risk of handoff errors associated with staff discontinuity.
Retained Surgical Item
Limited prior research has focused on retained surgical items (commonly known as “unidentified retained foreign object” or URFO) in otolaryngology.12,17 Frequent causes of retained surgical items include so-called uncountable objects such as throat packs and nasal splints. These items are frequently not included in the surgical count, and these survey data illustrate a potential opportunity to improve tracking of currently uncounted items.
Root Causes of Sentinel Events
To identify the root cause of the sentinel events, we analyzed free-text descriptions for each event based on accepted Joint Commission categories. A few themes emerged relating to latent risks. Surgical cases that deviate from a common pattern, such as planning a pediatric tonsillectomy scheduled without adenoidectomy, are susceptible to error; uncounted items, such as throat packs, may be overlooked; paired structures, such as ears, sinuses, or tonsils, are inherently susceptible to confusion; and communication is an omnipresent challenge. Defects in procedures for communication, medication use, human factors, and care planning accounted for 65% of intraoperative sentinel events, highlighting the importance of intraoperative teamwork and challenges inherent in universal checklist implementation. Last, a significant number of fire-related events occurred in cases where a fire safety checklist had not been performed.
In contrast with our results that did not identify leadership as a frequent root cause, The Joint Commission’s identified leadership (eg, organizational planning) as one of the most common root causes of sentinel events.8 Qualitative free-text description of the events did not lend itself to understanding limitations in organizational structure and leadership making determining leadership failures. Furthermore, the structure of the survey may not have triggered respondents to describe issues related to institutional leadership.
Reporting and Investigation of Intraoperative Sentinel Events
Reporting and follow-up on sentinel events are necessary aspects of effecting changes that prevent harm. Although all institutions are required to have mechanisms for reporting sentinel events, it was notable that 26.1% of respondents did not know of institutional systems in place to track such events. This finding calls out the need for otolaryngologists to become more involved with and informed of their institutional systems to capture and respond to sentinel events. The relatively low rate of presentation at morbidity and mortality conferences of medication errors (26.3%) and OR fires (23.1%) versus for wrong site/patient procedure (41.2%) or retained surgical item (44.8%) may reflect the lack of access to morbidity and mortality conference across all care settings (private versus academic practice). There may be opportunities for increased presentation of such events to promote quality improvement in the context of morbidity and mortality conference.18
In addition, only 15% to 24% of wrong-site surgical, wrong medication, and retained surgical item events were reported to result in at least temporary harm. However, this may represent and underrepresentation of the true harms experienced by patients. A review found that in some cases, the harm never reached the patient (eg, an operating room fire that did not reach the patient). However, in other cases, respondents reported events such as wrong-site surgery that reached the patient as resulting in no harm because the patient did well. Physicians underestimate the severity that patients experience from patient safety events,19 and our results should be viewed with this in mind.
Perspectives About Checklists
Despite their purported benefits, checklists have provoked a backlash by those clinicians who cite concerns of inefficiency about administrative burden. Although most reported that checklists helped reduce serious patient safety events, several survey respondents commented on these frustrations. Lack of engagement with checklists not only undermines the effectiveness of the intervention but may also give the team a false sense of security.20 These issues emphasize the need to develop and maintain meaningful time-outs that facilitate effective communication and focus attention on specific procedural risks. Improperly implemented checklists may promote “box-ticking” without improving communication or creating a culture of safety. For example, the National Health Service in England mandated checklist use without support for implementation and reported high documentation with little clinically meaningful implementation.21 Checklists are simply a tool to foster team communication but require buy-in from all stakeholders.22
Successful Checklist Implementation
Successful surgical safety checklist implementation requires implementation leaders to persuasively justify the need and to show how to use the checklist.23 Furthermore, successful implementation requires adaptation to existing institutional frameworks and continuous feedback and improvement.24
Limitations
This study has several limitations and sources of bias, most of which are inherent in all self-reported surveys. The study methodology relied on respondent recollection of previous events, predisposing to recall bias and willingness to report details around patient safety events. A natural reporting bias occurs in self-selection, as those who have experienced a major patient safety event may be more likely to respond to the survey. The actual incidence of intraoperative sentinel events may be higher or lower than that which is reflected in survey responses, although the overall survey response rate of 4.9% compares favorably with previous response rates to AAO-HNS surveys12,13,16,25,26 Furthermore, the respondents included strong representation of different practice types and specialty areas; however, the demographics of respondents are not representative of overall AAO-HNS membership, most notably evident in a preponderance of women respondents (78%).
Because of these methodological limitations, we cannot determine whether checklists have changed the incidence of sentinel intraoperative events. Another limitation is the data capture. Although several categories of events were queried, the survey instrument allowed respondents to report only 1 event per category; furthermore, the thematic focus on checklists likely meant that some categories of harmful events highly relevant to otolaryngology, such as cranial nerve injury, were unlikely to be captured by this survey. Nonetheless, these data provide examples of areas in which checklists may be beneficial in reducing operative harm events and areas in which additional efforts are likely necessary to positively affect patient outcomes. Future studies should seek to prospectively investigate the incidence of sentinel intraoperative events in otolaryngology and to better understand the root causes and impactful solutions.
Conclusions
Surgical safety checklists were widely implemented across surgical fields more than a decade ago as a stop measure in preventing systems-related preventable errors. As otolaryngologists enter the next decade, it is necessary to consider where and why errors leading to patient safety events continue to occur. Our survey results indicate that intraoperative sentinel events in otolaryngology most commonly arise from errors in communication, medication use, human factors, care planning, and absence of policies or procedures. Checklists are a powerful tool but in isolation are not sufficient to build a team and culture of safety. Otolaryngologists should strive to develop specialty-specific, meaningful time-outs, and consistent checklist use, focusing attention on unique risks of each procedure and fostering environments in which all team members can effectively communicate in the interest of promoting patient safety.
Author Contributions
John D. Cramer, drafting, analysis, and interpretation of data for the work, critically revising the work for important intellectual content, approval of the final submission, agreement to be accountable for all aspects of the work; Karthik Balakrishnan, drafting, analysis and, interpretation of data for the work, critically revising the work for important intellectual content, approval of the final submission, agreement to be accountable for all aspects of the work; Soham Roy, analysis and interpretation of data for the work, critically revising the work for important intellectual content, approval of the final submission, agreement to be accountable for all aspects of the work; C. W. David Chang, analysis and interpretation of data for the work, critically revising the work for important intellectual content, approval of the final submission, agreement to be accountable for all aspects of the work; Emily F. Boss, drafting, analysis, and interpretation of data for the work, critically revising the work for important intellectual content, approval of the final submission, agreement to be accountable for all aspects of the work; Jean M. Brereton, analysis and interpretation of data for the work, acquisition of data, critically revising the work for important intellectual content, approval of the final submission, agreement to be accountable for all aspects of the work; Taskin M. Monjur, analysis and interpretation of data for the work, critically revising the work for important intellectual content, approval of the final submission, agreement to be accountable for all aspects of the work; Brian Nussenbaum, analysis and interpretation of data for the work, critically revising the work for important intellectual content, approval of the final submission, agreement to be accountable for all aspects of the work; Michael J. Brenner, drafting of the work, acquisition, analysis, and interpretation of data for the work, critically revising the work for important intellectual content, approval of the final submission, agreement to be accountable for all aspects of the work.
Disclosures
Competing interests: None.
Sponsorships: None.
Funding source: None.
Supplemental Material
Supplemental material, sj-docx-1-opn-10.1177_2473974X20975731 for Intraoperative Sentinel Events in the Era of Surgical Safety Checklists: Results of a National Survey by John D. Cramer, Karthik Balakrishnan, Soham Roy, C. W. David Chang, Emily F. Boss, Jean M. Brereton, Taskin M. Monjur, Brian Nussenbaum and Michael J. Brenner in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Footnotes
Supplemental Material: Additional supporting information is available at http://journals.sagepub.com/doi/suppl/10.1177/2473974X20975731
References
- 1. National Center for National Health Statistics. National Vital Statistics System: multiple cause of death data file. National Vital Statistics System: Multiple Cause of Death Data File, 1969-2017. [Google Scholar]
- 2. National Quality Forum. Serious Reportable Events. Accessed August 31, 2020 http://www.qualityforum.org/topics/sres/serious_reportable_events.aspx
- 3. Delisle M, Pradarelli JC, Panda N, et al. Methods for scaling simulation-based teamwork training. BMJ Qual Saf. 2020;29:98-102. [DOI] [PubMed] [Google Scholar]
- 4. Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491-499. [DOI] [PubMed] [Google Scholar]
- 5. Urbach DR, Govindarajan A, Saskin R, et al. Introduction of surgical safety checklists in Ontario, Canada. N Engl J Med. 2014;370:1029-1038. [DOI] [PubMed] [Google Scholar]
- 6. The Joint Commission. Sentinel Event Policy and Procedures. Accessed August 1, 2020 https://www.jointcommission.org/resources/patient-safety-topics/sentinel-event/sentinel-event-policy-and-procedures/ [PubMed] [Google Scholar]
- 7. National Coordinating Council for Medication Error Reporting and Prevention. Medication Error Index. Accessed August 1, 2020 https://www.nccmerp.org/ [Google Scholar]
- 8. The Joint Commission. Sentinel Events Statistics Released for 2014. https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/joint-commission-online/jconline_april_29_15pdf.pdf?db=web&hash=DEFFBC41623A360F1C1428A5E9602773 [Google Scholar]
- 9. Hempel S, Maggard-Gibbons M, Nguyen DK, et al. Wrong-site surgery, retained surgical items, and surgical fires: a systematic review of surgical never events. JAMA Surg. 2015;150:796-805. [DOI] [PubMed] [Google Scholar]
- 10. Gawande AA, Studdert DM, Orav EJ, et al. Risk factors for retained instruments and sponges after surgery. N Engl J Med. 2003;348:229-235. [DOI] [PubMed] [Google Scholar]
- 11. Helmio P, Blomgren K, Lehtivuori T, et al. Towards better patient safety in otolaryngology: characteristics of patient injuries and their relationship with items on the WHO Surgical Safety Checklist. Clin Otolaryngol. 2015;40:443-448. [DOI] [PubMed] [Google Scholar]
- 12. Shah RK, Kentala E, Healy GB, et al. Classification and consequences of errors in otolaryngology. Laryngoscope. 2004;114:1322-1335. [DOI] [PubMed] [Google Scholar]
- 13. Shah RK, Nussenbaum B, Kienstra M, et al. Wrong-site sinus surgery in otolaryngology. Otolaryngol Head Neck Surg. 2010;143:37-41. [DOI] [PubMed] [Google Scholar]
- 14. Mehta SP, Bhananker SM, Posner KL, et al. Operating room fires: a closed claims analysis. Anesthesiology. 2013;118:1133-1139. [DOI] [PubMed] [Google Scholar]
- 15. Smith LP, Roy S. Operating room fires in otolaryngology: risk factors and prevention. Am J Otolaryngol. 2011;32:109-114. [DOI] [PubMed] [Google Scholar]
- 16. Shah RK, Hoy E, Roberson DW, et al. Errors with concentrated epinephrine in otolaryngology. Laryngoscope. 2008;118:1928-1930. [DOI] [PubMed] [Google Scholar]
- 17. Kim BJ, Shoffel-Havakuk H, Johns MM., III Retained nasal trumpet for 20 months: an unusual foreign body. JAMA Otolaryngol Head Neck Surg. 2019;145:93-94. [DOI] [PubMed] [Google Scholar]
- 18. Nussenbaum B, Chole RA. Rethinking morbidity and mortality conference. Otolaryngol Clin North Am. 2019;52:47-53. [DOI] [PubMed] [Google Scholar]
- 19. Di Maio M, Gallo C, Leighl NB, et al. Symptomatic toxicities experienced during anticancer treatment: agreement between patient and physician reporting in three randomized trials. J Clin Oncol. 2015;33:910-915. [DOI] [PubMed] [Google Scholar]
- 20. Pugel AE, Simianu VV, Flum DR, et al. Use of the surgical safety checklist to improve communication and reduce complications. J Infect Public Health. 2015;8:219-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Russ S, Rout S, Caris J, et al. Measuring variation in use of the WHO surgical safety checklist in the operating room: a multicenter prospective cross-sectional study. J Am Coll Surg. 2015;220:1-11 e14. [DOI] [PubMed] [Google Scholar]
- 22. Leape LL. The checklist conundrum. N Engl J Med. 2014;370:1063-1064. [DOI] [PubMed] [Google Scholar]
- 23. Conley DM, Singer SJ, Edmondson L, et al. Effective surgical safety checklist implementation. J Am Coll Surg. 2011;212:873-879. [DOI] [PubMed] [Google Scholar]
- 24. Fourcade A, Blache J-L, Grenier C, et al. Barriers to staff adoption of a surgical safety checklist. BMJ Qual Safety. 2012;21:191-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lavin JM, Boss EF, Brereton J, et al. Responses to errors and adverse events: the need for a systems approach in otolaryngology. Laryngoscope. 2016;126:1999-2002. [DOI] [PubMed] [Google Scholar]
- 26. Shah RK, Boss EF, Brereton J, et al. Errors in otolaryngology revisited. Otolaryngol Head Neck Surg. 2014;150:779-784. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-opn-10.1177_2473974X20975731 for Intraoperative Sentinel Events in the Era of Surgical Safety Checklists: Results of a National Survey by John D. Cramer, Karthik Balakrishnan, Soham Roy, C. W. David Chang, Emily F. Boss, Jean M. Brereton, Taskin M. Monjur, Brian Nussenbaum and Michael J. Brenner in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation