Abstract
Introduction
The term neurodiversity is defined and discussed from the perspectives of neuroscience, psychology and campaigners with lived experience, illustrating the development of aetiological theories for included neurodevelopmental disorders. The emerging discourse is discussed with relevance to adults, social inclusion, occupational performance and the legislative obligations of organizations.
Sources of data
Literature is reviewed from medicine, psychiatry, psychology, sociology and popular press. No new data are presented in this article.
Areas of agreement
There is consensus regarding some neurodevelopmental conditions being classed as neurominorities, with a ‘spiky profile’ of executive functions difficulties juxtaposed against neurocognitive strengths as a defining characteristic.
Areas of controversy
The developing nomenclature is debated and the application of disability status versus naturally occurring difference. Diagnosis and legal protections vary geographically, resulting in heretofore unclear guidance for practitioners and employers.
Growing points
The evolutionary critique of the medical model, recognizing and updating clinical approaches considering the emerging consensus and paradigmatic shift.
Areas timely for developing research
It is recommended that research addresses more functional, occupational concerns and includes the experiences of stakeholders in research development, moving away from diagnosis and deficit towards multi-disciplinary collaboration within a biopsychosocial model.
Keywords: neurodiversity, neurodevelopmental disorders, disability, autism, ADHD, dyslexia, DCD, reasonable adjustments, accommodations
Neurodiversity at work
Neurodiversity has become a popular concept at work and is increasingly popular within the business press, following the promotion of targeted inclusion programs from famous companies such as SAP, Virgin and Microsoft1 as well as the worldwide docuseries ‘Employable Me’/The Employables’.2 However, from an academic point of view, neurodiversity is not yet well captured, suffers from poor and conflicting definitions, confusing, overlapping symptomatology and little guidance on practical support at work. This introductory article provides an overview of the history of neurodiversity in order to contextualize a description of occupational presentation, which has wide reaching impact on the social determinants of health. Bringing together threads from disparate research fields including medicine, psychology, sociology, education, management science and vocational rehabilitation, a multi-disciplinary, biopsychosocial summary of the current picture is presented. A key issue for clinicians is understanding how to respond to the emerging dynamics when delivering everyday consultation and treatment for individuals. Practice guidance is provided, as well as advice on referring individuals to available workplace support. Avenues for future, multi-disciplinary research are recommended.
Defining neurodiversity
The term ‘Neurodiversity’ was originally developed by stakeholders influenced by the social model of disability.3–5 It was based on ‘Biodiversity’, a term primarily devised for political ends: to advocate for conservation of all species, since a high level of biodiversity is considered desirable and necessary for a thriving ecosystem. Neurodiversity advocates adapted this principle to argue that society would benefit from recognizing and developing the strengths of autism or dyslexia (for example) instead of pathologizing their weaknesses.6,7 Within the discipline of psychology, though, weaknesses have historically been the focus of research and practice. Analysis of cognitive strengths is only used to differentiate between general learning disabilities and specific-learning disabilities. A definition has emerged for psychologists and educators which positions neurodiversity ‘within-individuals’ as opposed to ‘between-individuals’.8 To elucidate: the psychological definition refers to the diversity within an individual’s cognitive ability, wherein there are large, statistically-significant disparities between peaks and troughs of the profile (known as a ‘spiky profile’, see Fig. 1).8,9 A ‘neurotypical’ is thus someone whose cognitive scores fall within one or two standard deviations of each other, forming a relatively ‘flat’ profile,8 be those scores average, above or below. Neurotypical is numerically distinct from those whose abilities and skills cross two or more standard deviations within the normal distribution.
Fig. 1.
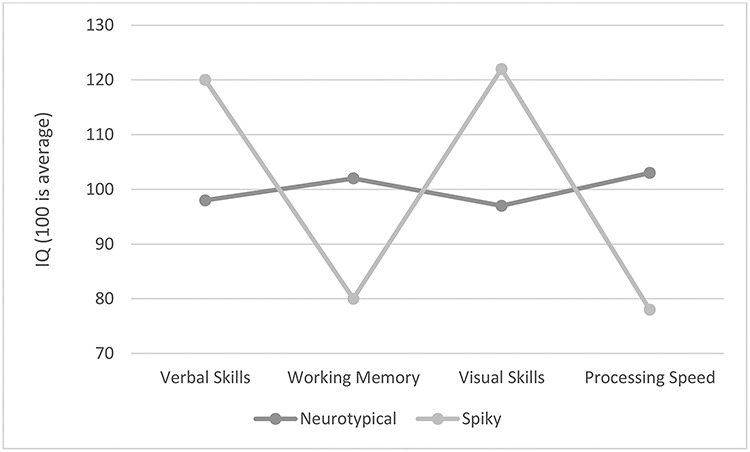
A ‘Spiky Profile’ showing example IQ scores.
Figure 1 is adapted from the British Psychological Society report on Psychology at Work,10 page 44, and depicts scores from the Wechsler Adult Intelligence Scale,11 which provides clear guidance on the level of difference between strengths and weaknesses that is typical or of clinical significance. Scores are used to support a diagnosis of dyslexia, Developmental Coordination Disorder (DCD, previously referred to as ‘dyspraxia’, see Table 2) and Attention Deficit Hyperactivity Disorder (ADHD)8,12,13 and to understand the cognitive ability of an employee following injury or illness.14
Table 2.
Timeline of neurominorities
| Condition | First records | Dominant 20th Century approaches | Since neuroscience paradigm |
|---|---|---|---|
| ADHD Prevalence around 5% worldwide54,113 but higher in USA.114 |
1798, some patients are described with an inability to maintain concentration; also referenced in 1844 as ‘Fidgety Phil’ syndrome,115 where no general disability can explain the difficulties related to an absence of ‘moral control’.116 | Known as hyper-kinetic reaction of childhood117 and Attention Deficit Disorder (with and without hyperactivity).118 Treatment with stimulants present from the 1940s, though not widely used initially as most behaviour attributed to poor parenting.116 |
Deficits in dopaminergic/noradrenalinergic pathways119 and combined executive functions120 implicated. Still mainly treated through stimulant medication augmented with psycho–social support for parents, teachers and individuals.113,121 |
| Autism Prevalence between <1 and 1.6% globally, affected by diagnostic criteria and access to services.122 |
Re-interpretation of historical medical and legal reports indicate case studies of autism in popular discourse since 1700s, both a specific difference issue related to eye contact and social communication as well as a general learning disability in which no ‘normal’ day-to-day social functions are observed.123 | ‘Refrigerator Mother’ hypothesis was proposed124 and Autism was considered a ‘Schizophrenia of Childhood’.125 Asperger’s syndrome used to differentiate high from low functioning.118,123 ‘Theory of Mind’—an observation-based theory inferring deficits in social imagination.126 The notion of an ‘Autistic Spectrum’ with behavioural symptoms along a continuum.127 |
Differences in connectivity of the brain, lower activity in pre-frontal cortex affecting executive functions108,128 and higher activity in sensory cortex resulting in sensory over-responsivity; ‘Intense World Theory’.106,107 Latest advice from American Psychiatric Association129 indicates one spectrum with different levels of IQ coexisting rather than determining separate sub-conditions. |
| DCD Prevalence estimated up to 6%.130 |
A physician named Collier is reported as providing the first report on ‘congenital maladroitness’ in the early 20th century131 defined as difficulty with motor coordination despite normal levels of intelligence. | Dyspraxia, developmental apraxia absorbed into the pejoratively named ‘Clumsy Child Syndrome’ in the later 20th century,132 however dyspraxia and developmental coordination disorder more widely used in diagnosis according to DSM criteria.118 | Consensus on terminology of Developmental Coordination Disorder (DCD) within DSM criteria.129 Neurobiological observed differences include internal modelling and executive functions deficits, but likely point again towards a complex whole brain approach in which several specific pathways may be all or partially compromised.130 |
| Dyslexia up to 10%45 | Dyslexia described as ‘word blindness’ in medical journals from the late 1800s, referring to both acquired and developmental inability to read despite otherwise normal levels of intelligence.133 | Initially thought to be related to visual perception134 but later in the 20th century this assumption was superseded by Phonological Deficit Theory and more specifically a deficit in the phonological component of working memory, part of the executive functions.135,136 Several other competing neurocognitive theories are proposed137 and there is a lack of a single, unifying theory.138 | Neuroimaging suggests that dyslexia is not caused by a single neurocognitive function but is instead a complex presentation with many potential causes, dependent on the interaction between individual neurocognitive capacity and the language that one speaks.139 |
To refer to individuals, the terms ‘neurodivergent’ ‘neurodifferent’ and ‘neurodiverse’ are in current use both academically and for self-identification; this is a matter of stakeholder debate.15–17 In recognition of the lack of consensus regarding which term is more appropriate, all may be referred to interchangeably, asking individuals how they prefer to identify. Spiky-profile conditions have historically been grouped under umbrella terms such as hidden impairments, specific-learning disabilities and neurodevelopmental disorders. Autistic autism researchers have critiqued the widespread use of deficit highlighting in nomenclature and advise a wide scale revision of language.18 A new umbrella term is proposed herein for included conditions that is neutral and statistically accurate: ‘neurominorities’.
Introduction: an emerging paradigm
Stakeholder activism
Judy Singer, the Australian sociologist, is widely credited with producing the first research-based publication of the term in 1999, following her thesis in which she synthesized her first-person experience in the middle of three generations of women ‘somewhere’ on the autistic spectrum, with critical disability studies.19 In the decades since publication, the term and its philosophy of difference, not deficiency, has been appropriated for a wider range of conditions, diagnoses and identities and formed a grass roots movement.17,20 This paper focuses on the main four neurominorities of ADHD, autism, DCD and dyslexia for ease of comparison, literature review and recommendation. It is acknowledged that this will overlook some conditions and complexities within the emerging paradigm, yet many of the principles can be applied in a wider context.
The Neurodiversity movement holds ambitions of equal rights for members, appreciation of the diversity of human cognition and political power to break down structures of exclusion.6 Nowhere has this argument been more compelling to date than the innovative technology, finance and defence industries, where programs to deliberately hire neurominority employees are becoming more frequent as talent strategies, rather than social responsibility projects.1,15,21–25 Neurominority employees may bring talents, yet, in line with the spiky profile, there may also be difficulties. Understanding the discourse is essential for understanding neurodiversity at work because it affects how we must fluidly move between medical and social models to support individuals and employers.
Ontological controversy
The disparity between the language and assumptions of psychological and medical ‘experts’ and the lived experience of ‘stakeholders’ has led to dissent and conflict both between and within these groups.6,17,26 For example, some argue that autism is inherently disabling irrespective of context27; some propose that differentiating between autistic people who are ‘high’ or ‘low’ functioning is fundamentally discriminatory,28 whereas others propose their identity to be a superpower.29 In practice, we will encounter individuals from all these polarized perspectives, some who feel strongly about their position, and will assert their right to be treated accordingly. However, we should not presume that those who do not self-advocate articulately to be without preference; agency in accessing professional services is compromised by layers of intersectional exclusion including race, gender, class and sexual orientation, as well as verbal skills themselves. In research, there are increasingly calls to include stakeholder voice (‘nothing about us without us’5) and to focus on matters of importance to those with lived experience, such as workplace adjustment interventions, outcomes and inclusion best practice, as opposed to diagnosis and deficits.30–32 Educopsychological and psychiatric debates include comorbidity and the difficulty distinguishing between the conditions,33–37 as well as controversy around the ‘correct’ approach for differential diagnosis, given that the main conditions are diagnoses of exclusion, in which there are no objective, clear measures of assessment.38–40 A clear way forward for medical research and clinical practice is thus lacking, and it is important to understand the confusing influence of a disconnected discourse upon occupational health guidance. Employers may look to experts for advice and find the advice incongruous with the popular business narrative. Employees may be hired as part of a talent program yet present with stress and anxiety. Practitioners are thus advised to enquire with patients directly for feedback and to approach any treatment sensitively, balancing the influence of intervention protocol controversy: for example, Applied Behavioural Analysis is considered abusive and traumatic by many autistic people.41
The biopsychosocial history of neurominorities
Psychological adoption
The umbrella term of neurodiversity began to replace ‘Specific Learning Difficulties’ for some educational psychologists in the late 2000s20,42,43 and became common within occupational psychology in the 2010s.13 In psychological literature, ADHD, autism, DCD and dyslexia are the conditions most frequently referred to under this banner, though others have also included mental health conditions such as depression and anxiety,6,9,20 general learning disability20 as well as Tourette Syndrome, dyscalculia, dysgraphia and acquired brain injury,9 depending upon whether the within or between definition is applied. Distinction has been made between conditions that are applied and developmental, clinical and developmental, acquired and transient or acquired and chronic9; Table 1 depicts a taxonomy of neurominorities adapted and updated from the British Psychological Society’s Psychology at Work report.10 (Please refer to the full chapter for more details).
Table 1.
A taxonomy of neurominorities
| Dyslexia, DCD, dyscalculia, dysgraphia | Tourette syndrome, autism and ADHD | Mental ill health | Neurological illness or brain injury |
|---|---|---|---|
| Applied, developmental neurominority | Clinical, developmental neurominority | Acquired neurominority (potentially transient) | Acquired neurominority |
| • Born with condition • Relates to applied, educational skills such as reading or motor control • Not considered a health condition | • Born with condition • Relates to behavioural skills such as communication and self-control • Considered a health condition (currently) | • Develops in response to a health condition such as anxiety or depression
• Could return to ‘neurotypical’ if health condition resolves |
• Develops in response to a health condition
• Potentially resolves as injury heals or worsens as health deteriorates |
The major themes within the medical history of the main developmental conditions are presented in the next section. Neurocognitive, psychosocial and legal commonalities are noted, within which occupational advice must be contextualized. A timeline of the various theories is depicted in Table 2. Note that all start with a pathologization of socially referenced behaviour or skill, followed by varying hypothetical causal nature/nurture theories. All include reference to ‘Executive Functions’ by the 21st century, defined as ‘goal-oriented self-regulation—including planning, organisation, response inhibition and behavioural sequencing’.44
An evolutionary critique of the psychomedical model
Given the extent of overlap between the conditions, the under-diagnosis of females who instead present with anxiety, depression or eating disorders,45,46 and the estimated prevalence of each condition, a reasonable estimate of all neurominorities within the population is around 15–20%, i.e. a significant minority. Research supports a genetic component to most conditions47 which, when considered with combined prevalence rates, suggests an evolutionary critique of the medical model: if neurodivergence is essentially disablement, why do we keep replicating the gene pool? The less extensive, yet persistent, body of work indicating specialist strengths within neurodiversity,9,20,48–52 supports the hypothesis that the evolutionary purpose of divergence is ‘specialist thinking skills’ to balance ‘generalist’ thinking skills (as per the ‘spiky profile’). The evolutionary perspective is congruent with the Neurodiversity movement and essential to understanding the occupational talent management perspective that is currently in vogue.
The psychomedical histories outlined in Table 2 speak to the evolutionary critique for two reasons. Firstly, they demonstrate the consistency of the ‘specific’ rather than ‘general’ nature of impairment (the spiky profile) across all four conditions over time, irrespective of the changing nature of causal theories. The conditions are named and identified according to their most prominent deficits, which are themselves contextualized within our normative educational social history. Dyslexia is discovered around the same time as literacy becomes mainstream through education; ADHD becomes more prevalent with the increasing sedentary lifestyles from the industrial revolution; autism increases in line with modern frequency of social communication and sensory stimulation and DCD as our day-to-day need for motor control of complex tools and machinery becomes embedded. The evolutionary critique of neurodevelopmental disorders is that their perceived pathology is related to what we consider normal in modern times, as opposed to what is normal development within the human species.3,7,53–55 Secondly of interest from the timeline in Table 2 is the final column, wherein we see that, despite consistent observation of similar neurobiological differences, we lack a single unifying theory for any condition.
Towards a biopsychosocial model
Most humans are average in all functional skills and intellectual assessment, some excel at all, some struggle in all and some have a spiky profile, excelling/average/struggling. The spiky profile may well emerge as the definitive expression of neurominority, within which there are symptom clusters that we currently call autism, ADHD, dyslexia and DCD; some primary research supports this notion.33,56 In the future, these may shift according to our educational and occupational norms such as social demands, sedentary lifestyles, literacy dependency and automation of gadgets. To elucidate, although there are clear biological markers for those with a spiky profile33,55 which lead to observable, measurable psychological differences, there is nothing innately disabling about those differences when we consider a traditional, tribe-based community of humans. Within the biopsychosocial model of neurodiversity, understanding work-related intervention and treatment becomes more about adjusting the fit between the person and their environment58 than about treating a disorder. Critical review of the extant biopsychosocial research supports the social model proposition that the individual is not disabled, but the environment is disabling.
The legal status of neurodiversity
Since the early 21st century, most nations have adopted disability legislation congruent with the United Nations Statute59 on the rights of Persons with Disabilities. Such legislation refers to the need for organizations to make ‘accommodations’, to use US terminology,60 referred to in the UK as ‘adjustments’,61 such that individuals with disabilities can learn, work and be included in society. The term accommodation is adopted for the remainder of this paper to denote the general process of compromise and flexibility; adjustment is used to refer to the implementation of equipment, services or changes to requirement, though in practice the two are used interchangeably dependent on geographical location. Note that there is no compulsion for individuals to change to fit in, no mention of treatment for individuals. Legally compliant intervention is at the organizational level, including the requirement for businesses, services and educators to work towards ‘Universal Design’, in which there is flexibility of environment, communication and tools to accommodate the widest possible range of human experience.62 Disability status is predicated not on diagnosis of condition, but on the assessment of functional impairment, the extent to which the individual is inhibited and excluded. One could have a diagnosis of diabetes, spinal injury, psychiatric disorder and be disabled or not, depending on the impact on ‘normal day-to-day functioning’ that persists over a minimum period, for example 12 months.61 The context may or may not disable the individual (‘disabled people’) as opposed to the disability automatically assigned to the person by nature of their diagnosis (person with a disability). From a legal perspective then, any form of neurominority may qualify for protections requiring accommodation depending on what is currently normal and how that interacts with an individual’s cluster of functional difficulties.
Neurodiversity should not be used as a synonym for disability, hence the adoption of the neurominority term herein. Many neurominority employees find themselves in need of disability accommodation at work.63,64 Irrespective of legal protection, social and occupational exclusion are endemic for neurominorities. Studies vary in the percentages quoted, yet there is persistent evidence of disproportional representation within prison populations,64–67 long-term unemployment32,68–70 and failure to achieve career potential.70,71 Exclusion rates point to an economic, social and moral imperative to improve outcome-based research, from which we can advise practitioners and individuals on which adjustments improve inclusion, within a biopsychosocial model.
Occupational considerations of neurodiversity
To summarize the context before moving to presentation and accommodation: an occupational narrative has developed around the ‘diamond in the rough’,72 in which neurominority employees resemble thwarted geniuses, who would be able to succeed given the right support, environment or tools. The extent to which this narrative is plausible for individuals is not well captured by academic research, which is biased towards reductive neuropsychology in search of ‘bits that are broken’3,73 as opposed to more functional, contextual performance. A reductive, medical paradigm of research is incongruent with the legal status of neurominorities as protected conditions in most developed countries, to which organizations must adjust. Given this, in the following section, a neutral pragmatic summary of knowledge regarding individual-level symptoms and occupational difficulties is attempted. The effectiveness of adjustments and issues related to systematic inclusion at the organizational level is discussed.
Occupational symptomatology
At the functional level, there are similarities between neurominorities in terms of presentation. As alluded to in Table 2, executive functions are a common psychological complaint, resulting in difficulties with short-term and working memory, attention regulation, planning, prioritizing, organization and time management. Self-regulation of work performance is required in many modern employment contexts and therefore these issues present as the most disabling for individuals.74 There is also commonality among strengths, many related to higher order cognitive functioning reliant on comprehension and creativity.75 Table 3, adapted again from the British Psychological Society’s 2017 report,10 describes reported strengths and weaknesses associated with the four main neurominorities. The comparatively fewer references regarding strengths may reflect a research bias as opposed to an accurate representation of lived experience; it certainly is incongruent with the ‘talent’ narrative that is becoming dominant in workplaces.
Table 3.
Work-related difficulties and strengths attributed to neurominorities
| Difficulty | Strength | |
|---|---|---|
| ADHD | Time management140 Concentration, attention and self-regulation difficulties141 Insomnia, depression, injury and absence142 Maintaining employment143 Difficulty with team work144 |
Creative thinking145 Visual-spatial reasoning ability8 Hyper-focus, passion and courage20 |
| Autism | Time management146 Concentration and coping with more than one task147 Social and communication difficulties148 Need for routine148 |
Memory ability, and other ‘specialist individual skills’ including reading, drawing, music and computation149 Innovative thinking and detail observation20 |
| DCD | Difficulties with driving, self-care, organization, communication and self-esteem32,51 Processing speed and working memory8 Persistence of motor difficulties in operating equipment150 |
High verbal comprehension ability8 |
| Dyslexia | Literacy, memory, organization, communication and self-esteem12,151 Memory, organizational skills, time management, stress management, literacy74 Workplace participation in terms of mental functions and social interactions63 Cognitive functioning and social self-esteem152,153 Higher incidence of worklessness and incarceration65,154 |
Entrepreneurialism50 Creativity and cognitive control153 Visual reasoning154 Practical skills, visual-spatial skills and story-telling ability155 |
Accommodations
The aim of occupational accommodations for neurominorities is to access the strengths of the spiky profile and palliate the struggles. The most frequently deployed adjustments31,76–78 fall into the categories listed in Table 4. Note that additional time to complete work is not mentioned; this adjustment is common in education but not at work, because it is not reasonable to pay someone the same money to produce less work. In exams, the validity of extra time is because we are measuring long-term memory or analytic skill via the medium of literacy alone, when verbal, visual and/or spatial skills may be more relevant in the workplace (for example multiple choice quizzes to assess medical knowledge). When assessment methods are more matched to the eventual job performance (for example observation of physical examination skills using role play patients) extra time becomes less important. This principle applies across education, recruitment and employment but is poorly understood by lay people or those without an understanding of cognitive functions and the antecedent components of job performance.
Table 4.
Typical adjustments for neurominorities
| Adjustment type | Example activity |
|---|---|
| Work Environment flexibility | Reducing sensory distractions by allowing flexible hours; use of private meeting rooms; noise-cancelling headphones; redesign of shared working space. |
| Schedule flexibility | Avoiding rush hour travel to prevent sensory overwhelm; remote working to avoid sensory overwhelm, improve concentration and reduce social communication demands. |
| Supervisor or co-worker support | Additional feedback time with supervisor; differences in instructions provided—more clarity or concreteness given. |
| Support from different stakeholders | Peer mentoring networks within the company; allowing support activities via employee assistance, mental health, or family support throughout the working day; allowing access to stakeholder groups and charities throughout the working day. |
| Executive functions coaching | Workplace coaching to focus on areas such as planning, prioritization, organizational skills using workplace coaching psychology. |
| Training | Adjustments to training provision including sending materials in advance or providing additional induction training. |
| Work-station adjustments | Use of dual screens to improve concentration, whiteboards and other aide memoires; standing desks with wobble boards to improve access to movement through the day. |
| Assistive technology and tools | Speech-to-text, text-to-speech software to reduce demands on literacy, handwriting skills and improve concentration; mind mapping software to support shift from overview to detailed thinking; specialist spell checkers designed for dyslexia; planning and memory software. |
| Literacy coaching | This will be targeted coaching based on the literacy requirements of the role rather than teaching basic skills, such as speed reading, making notes whilst reading, summarizing or structuring and planning written work. |
Adjustment effectiveness
There are very few studies evaluating the effectiveness of adjustments in the workplace and this is an urgent research need.79 Rice and Brooks30 stated the following in the conclusion of their adult dyslexia interventions review (p. 12): ‘good practice in this field rests almost entirely on professional judgment and common sense, rather than on evidence from evaluation studies’. Over-reliance on heuristical guidance must be addressed by the research communities, and requires collaboration within applied psychological sub-disciplines, occupational therapy, occupational medicine and human resources departments. The limited evidence that does exist broadly supports the implementation of adjustments64,74,77,80,81 but, without sophistication, we are unable to speak to quality control, return on investment or predict which type will work for different individuals/roles. Intensive personalized employment support (IPS) such as that provided to autistic people with multiple needs and people with moderate mental health conditions have found that the benefits only outweigh the costs when wider community measures such as housing and health costs are factored in.82–85 However, employment-based neurominority adjustments typically cost <£1200 per person,86 which is cheaper than the cost of re-recruiting87 and significantly cheaper than IPS. More broadly, cross-sectional research has indicated biases in cost perceptions of disability adjustment, with objective records of expenditure less than presumed.88 Although an appropriate evidence-base builds, practitioners must be guided by individual presentation, compromise and collaboration with employers, bearing in mind the biopsychosocial model and the strongly held opinions of individuals. Professionals can support the ambitions of the Neurodiversity movement in the workplace but must also maintain a cautious approach to prognosis of workplace performance improvements and job retention until we have more longitudinal data.
Accessing adjustments
In the UK, the Access to Work program funded by the Department of Work and Pensions provides a free assessment to over 30 000 disabled people per annum, including ~6000 neurominority employees or those with mental health needs.86 The program acts as triage and signposting, enabling individual employees to self-refer and acquire an assessment of workplace need, following which a report is produced recommending adjustment as per the types in Table 4. Access to Work is widely respected in the UK and valued by users89 but there is a clear short fall in resourcing, considering the number of eligible individuals likely to be working in the UK. There are few programs of its kind internationally. The same role is more typically provided informally or privately by Occupational Health, Human Resources or Employee Assistance Programs from an organizational point of view, acting on behalf of the company rather than the individual. Professionals providing these services are less likely to possess the specialist skills in working with executive functions deficit, and are liable to misdiagnose/mistreat executive dysregulation as stress, anxiety or wilful lack of motivation, particularly with women, black people and ethnic minorities.46,90,91–94 Clinicians are advised to check for specialist knowledge on referral rather than assume a mental health generalist will have required expertise. Adjustments tend to be provided as a compliance activity per individual, with few businesses looking systemically at Universal Design62,95 for neurominorities as would be recommended in the United Nations Convention on disability.59 Access to accommodations is thus predicated on individual disclosure, typically occurring following a conflict or episode of poor performance. Individuals are reluctant to voluntarily disclose in advance79,96,97 as they fear discrimination (with some justification98) and therefore the aims of the disability legislation programs worldwide are not yet having the intended effect on inclusion.99–101
Implications of the neurodiversity phenomenon for medical practitioners
In this final section, the potential ways in which medical practice can embrace the developments of the Neurodiversity movement and support individuals within a biopsychosocial model are explored.
Reactional stress and hidden neurominority
Physicians are likely to be interacting with neurominority individuals who are in work, unemployed, incarcerated or requiring health care. Neurominorities can be misdiagnosed as mental health issues due to symptoms overlapping with bipolar disorder, anxiety, depression and/or eating disorder.45,46,102 A presenting mental health need may be a direct consequence of unsupported neurominority; an individual who is frustrated, excluded and unable to reach potential will naturally feel anxious or depressed. We need to improve recognition of cognitive symptoms (as opposed to mood) in frontline medical and nursing services to ensure accurate signposting. There is a potential for a vicious cycle in which treatment for mood and stress will only mask an underlying cognitive deficit or difference leading to ‘revolving door’ patterns of health care access. Where possible, physicians should feel comfortable to ask about the possibility of a neurominority as an explanation for ongoing distress and underachievement and refer to a specialist psychiatrist or psychologist for confirmation. It must also be noted that those experiencing precarious employment and unemployment will be experiencing adverse impacts on health, stress and well-being more generally,103 that those with neurominorities are more likely to be under-employed and that access to diagnosis is compromised by intersectional influences of race, gender, sexual orientation and socioeconomic background.
Following diagnosis
Once a condition or conditions have been identified, an individual may feel vindicated, and experience catharsis. Psychology practitioners report their clients’ mental shift following correct diagnosis at the identity level and warn that, done badly, it can lead to disempowerment.12 However, done well, understanding one’s strengths and weaknesses can lead to breaking down barriers and removing self-reproach. A late diagnosis adult client reported ‘now that I understand my dyspraxia and that I literally have less processing power than most people, I don’t give myself such a hard time. I take things slowly, at my own pace, which reduces my anxiety and actually makes me do things more accurately’. Physicians can recommend approaching employers for accommodation advice, recommending Access to Work if in the UK and human resources departments globally. A benefit of increased, general Neurodiversity awareness has been capacity building within businesses to manage and respond to requests for adjustments. Although not every employer has an established process, and there are still incidences of discrimination, guidance from respected professional bodies in human resources is clear about legally-compliant activities and how to access them.104,105
Accommodations in providing medical treatment
Differences in sensory perception have been reported as a hallmark of neurominority internal experience,102–108 which may affect pain management, sleep patterns and increase routine-change difficulties during in-patient care. Pamphlets explaining treatment, obtaining consent, confirming after care may not be read or absorbed by those struggling with literacy or attention. Difficulties in independently maintaining organizational routines might affect self-management of medication protocols. Neurominority patients may therefore respond differently to treatment, with increased anxiety or confusion. A patient who appears unwilling to take responsibility for health care may be forgetful not defiant, even if they seem verbally competent, which could result in prejudicial treatment from clinicians. A significant risk is that a neurominority individual may experience a ‘meltdown’, defined as ‘an intense response to overwhelming situations’.109 For those with sensory sensitivity, overwhelm can be caused by pain, bright hospital lights, background noise, smells and continual changes in personnel. Someone experiencing a meltdown may scream, shout, swear and become physically aggressive to avoid being touched (as opposed to physically violent with intent to harm). Medical staff in all contexts need to be aware that any unnecessary physical contact or verbal persuasion in this circumstance may exacerbate distress rather than palliate and that an appropriate response is to provide calm, quiet decompression space wherever possible.
Treatment for mental ill health, insomnia and stress-related illness must be reviewed in terms of the reactive nature of distress in the context of continual sensory overload and/or exclusion. A common theme in discrimination for neurominorities is to be told to ‘try harder’ or ‘yes, but we all feel like that sometimes’, leading to self-doubt and increased exposure to harm. Validation of the biological nature of distress from clinicians can be liberating, but it does not follow that alleviating distress must always result from individual treatment. In this context, care must be taken to alleviate acute symptoms, but encourage long-term adaptation of the individual’s environment, developing self-awareness and agency over home situations and work. Psychosocial support referral should accompany pharmacological treatment; a multi-disciplinary approach is recommended. At work for example, occupational physicians specifically can advocate for neurominority inclusion with employers, by liaising with human resources and occupational psychologists to systemically improve environmental compatibility in building, schedule and work-station design accommodating assistive technology, sensory overwhelm, the need to move and reducing social anxiety.
Research avenues
The dearth of research about the occupational implications of neurodiversity is less of a gap, and more of a ‘blind spot’.110 Medical research could support the development of evidence-based practice in employment by incorporating long-term outcomes into treatment and diagnostic studies. Including dependent variables such as formal education, salary, hours of employment, job satisfaction and career attainment will provide occupational psychologists with much-needed data on inclusion and adjustment effectiveness. Collaborations with multi-disciplinary occupational health teams are required to improve our understanding of what works, for whom and when. A Realist methodology111 within a ‘Pragmatic Paradigm’112 can embrace the biopsychosocial model and enable us to provide better advice to individuals and employers. There is an opportunity to make a real difference to the lives of many and improve health outcomes through social inclusion using a neurodiversity focus.
Conclusions
From within an emerging paradigm, clinicians and researchers must appreciate the shift in discourse regarding neurodiversity from an active, vocal stakeholder group and embrace new avenues for study and practice that address practical concerns regarding education, training, work and inclusion. This article has provided an overview of the neurodiversity employment picture; namely high percentages of exclusion juxtaposed against a narrative of talent and hope. Understanding the importance of nomenclature, sensory sensitivity and the lasting psychological effects of intersectional social exclusion is key for physicians wanting to interact confidently and positively with neurominorities. The proposed biopsychosocial model allows us to provide therapeutic intervention (medical model) and recommend structural accommodation (legislative obligation) without pathologization (social model). In other words, we can deal pragmatically with the individuals who approach us and strive for the best outcomes, given their profile and environment. It is acknowledged that, by focusing on the main four developmental neurominorities to the exclusion of others, some nuance is unexplored, though the main principles herein can be applied more broadly. Summarized above are adjustments representing current best practice, though the need to assess and evaluate these beyond description and cross-sectional studies is highlighted. The neurodiversity phenomenon is coming of age and will begin to translate into public policy and education as well as employment. Medical and social scientists are uniquely placed to support an ambitious inclusion agenda through rigorous evaluative research partnerships.
Addendum
A new umbrella term is proposed herein for included conditions that is neutral, statistically accurate and has support from communities with lived experience: ‘neurominorities’.156,157
Data availability statement
No new data were generated or quantitatively analysed in support of this review.
Acknowledgements
The author thanks her academic supervisor, Prof. Almuth McDowall and Judy Singer for their dedication to collaboration, constructive critique and dialectic exchange.
References
- 1. Austin RD, Pisano GP. Neurodiversity as a competitive advantage. Harv Bus Rev 2017;95:96–105. https://hbr.org/2017/05/neurodiversity-as-a-competitive-advantage. [Google Scholar]
- 2. Wollaston S. Employable Me Review: Moving Telly that Destigmatises Disability – and Made Me Laugh. The Guardian; https://www.theguardian.com/tv-and-radio/2016/mar/24/employable-me-review-moving-telly-that-destigmatises-disability-and-made-me-laugh. Published 24th March 2016. [Google Scholar]
- 3. Krcek TE. Deconstructing disability and neurodiversity: controversial issues for autism and implications for social work. J Progress Hum Serv 2012;24:4–22. [Google Scholar]
- 4. Shakespeare, Watson N. Defending the social model. Disabil Soc 1997;12:293–300. doi: 10.1080/09687599727380. [DOI] [Google Scholar]
- 5. Charlton J. Nothing About Us Without Us: Disability Oppression and Empowerment. Berkley, CA: University of California Press; 1998. http://www.jstor.org/stable/10.1525/j.ctt1pnqn9. [Google Scholar]
- 6. Baker DL. The Politics of Neurodiversity: Why Public Policy Matters. Boulder, CO: Lynne Rienner Publishers; 2011. http://www.rds.hawaii.edu/ojs/index.php/journal/article/view/111/371. [Google Scholar]
- 7. Ortega F. The cerebral subject and the challenge of neurodiversity. Biosocieties. 2009;4:425–46. doi: 10.1017/S1745855209990287. [DOI] [Google Scholar]
- 8. Grant D. The psychological assessment of neurodiversity In: Pollak D. (ed.). Neurodiversity in Higher Education. Chichester, UK: Wiley-Blackwell, 2009,33–62 [Google Scholar]
- 9. Doyle N. Neurodiversity at work In: BPS, ed Psychology At Work:Improving Wellbeing and Productivity in the Workplace. Leicester: British Psychological Society; 2017:44–62. ISBN 978-1-85433-754-2 [Google Scholar]
- 10. BPS Psychology at Work. Leicester: British Psychological Society, 2017 [Google Scholar]
- 11. Weschler D. Weschler Adult Intelligence Scale Version IV. New York: Psychological Corporation, 2008 [Google Scholar]
- 12. McLoughlin D, Leather C. The Dyslexic Adult. Chichester: John Wiley and Sons, 2013 [Google Scholar]
- 13. McLoughlin D, Doyle N. The Psychological Assessment of Adults with Specific Performance Difficulties at Work. Leicester: British Psychological Society; 2013. https://www.bps.org.uk/sites/bps.org.uk/files/Policy/Policy - Files/DOP Psychological Assessment of Adults with Specific Difficulties.pdf. [Google Scholar]
- 14. Tyerman A, Meehan M. Vocational Assessment and Rehabilitation After Acquired Brain Injury: Inter - Agency Guidelines. London: Royal College of Physicians; 2004. http://books.google.co.uk/books?id=mevepd06yeQC. [Google Scholar]
- 15. Doyle N. Richard Branson Opens the Door to Bigger Thinking on Neurodiversity. Forbes; https://www.forbes.com/sites/drnancydoyle/2019/10/22/richard-branson-opens-the-door-to-bigger-thinking-on-neurodiversity-/. Published October 2019. [Google Scholar]
- 16. Singer J. Neurodivergent from what exactly? https://neurodiversity2.blogspot.com/. Internet Article. Published 2019. Accessed January 3, 2019.
- 17. Monzee J, Ouimet M, Schovanec J et al. Neurodiversity: 20th Anniversary of the Birth of a Concept. Parents Eclaires: Quebec, 2019 [Google Scholar]
- 18. Bottema-beutel K, Kapp SK, Lester JN et al. Avoiding Ableist Language: Suggestions for Autism Researchers. Autism in Adulthood 2020;00:1–12. doi: 10.1089/aut.2020.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Singer J. “Why can’t you be normal for once in your life?” From a problem with no name to the emergence of a new category of difference In: Corker M, French S (eds.). Disability Discourse. Buckingham, UK: Open University Press, 1999,59–67 [Google Scholar]
- 20. Armstrong T. The Power of Neurodiversity. Cambridge, MA: De Capo, 2010 [Google Scholar]
- 21. Comaford C. Is Neurodiversity the Rght Talent Path for Your Organization? Forbes; June 24th 2017. https://www.forbes.com/sites/christinecomaford/2017/06/24/competitive-advantage-why-your-organization-needs-to-embrace-neurodiversity/#62ed8ca63f65. [Google Scholar]
- 22. Higginbottom K. Why firms are embracing neurodiversity. HR Magazine, 1st March 2017. [Google Scholar]
- 23. Sniderman B. Neurodiversity: A New Talent Opportunity. Forbes; Published 30th October 2014. https://www.forbes.com/sites/brennasniderman/2014/10/30/neurodiversity-a-new-talent-opportunity/#58ab46271058. [Google Scholar]
- 24. Bernick M. Effective Autism (Neurodiversity) Employment. Forbes; https://www.forbes.com/sites/michaelbernick/2019/01/15/effective-autism-neurodiversity-employment-a-legal-perspective/#586692476c18. Published 15th January 2019. [Google Scholar]
- 25. Philipson A. GCHQ Employs More Than 100 Dyslexic and Dyspraxic Spies. The Telegraph; http://www.telegraph.co.uk/education/educationnews/11111584/GCHQ-employs-more-than-100-dyslexic-and-dyspraxic-spies.html. Published 2014. [Google Scholar]
- 26. Baron-Cohen S. The Concept of Neurodiversity is Dividing the Autism Community. The Scientific American; https://blogs.scientificamerican.com/observations/the-concept-of-neurodiversity-is-dividing-the-autism-community/. Published 30th April 2019. [Google Scholar]
- 27. Clements T. The Autistic Brothers: Two Unconventional Paths to Adulthood. England: Thomas Clements, 2018 [Google Scholar]
- 28. Alvares GA, Bebbington K, Cleary D et al. The misnomer of ‘high functioning autism’: intelligence is an imprecise predictor of functional abilities at diagnosis. Autism 2020;24:221–32. doi: 10.1177/1362361319852831. [DOI] [PubMed] [Google Scholar]
- 29. Thunberg G. No One Is Too Small To Make A Difference. UK: Penguin Random House, 2019 [Google Scholar]
- 30. Rice M, Brooks G. Developmental Dyslexia in Adults: A Research Review. London: National Research and Development Centre; 2004. http://www.nrdc.org.uk. [Google Scholar]
- 31. Patton E. Autism, attributions and accommodations neurodiverse workforce. Pers Rev 2019;48:915–34. doi: 10.1108/PR-04-2018-0116. [DOI] [Google Scholar]
- 32. Kirby A, Edwards L, Sugden D. Emerging adulthood and developmental co-ordination disorder. J Adult Dev 2011;18:107–13. doi: 10.1007/s10804-011-9123-1. [DOI] [PubMed] [Google Scholar]
- 33. Astle DE, Bathelt J, Holmes J. Remapping the cognitive and neural profiles of children who struggle at school. Dev Sci 2019;22:1–17. doi: 10.1111/desc.12747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hendren RL, Haft SL, Black JM et al. Recognizing psychiatric comorbidity with reading disorders. Front Psych 2018;9. doi: 10.3389/fpsyt.2018.00101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sumner E, Leonard HC, Hill EL. Overlapping phenotypes in autism Spectrum disorder and developmental coordination disorder: a cross-syndrome comparison of motor and social skills. J Autism Dev Disord 2016;46:2609–20. doi: 10.1007/s10803-016-2794-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Landgren M, Kjellman B, Gillberg C. Attention deficit disorder with developmental coordination disorders. Arch Dis childhoodisease Child 1998;79:207–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kilroy E, Cermak S, Aziz Z. A review of functional and structural neurobiology of the action observation network in autism Spectrum disorder and developmental coordination disorder. Brain Sci 2019;75:29. doi: 10.3390/brainsci9040075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. SASC Guidance on the Assessment of Students with SpLD. London: Student Assessment Standards Committee; http://www.sasc.org.uk/NewsItem.aspx?id=58. Published 2017 Accessed May 31, 2018. [Google Scholar]
- 39. Ihori D, Olvera P. Discrepancies, responses, and patterns: selecting a method of assessment for specific learning disabilities. Contemp Sch Psychol 2015;19:1–11. doi: 10.1007/s40688-014-0042-6. [DOI] [Google Scholar]
- 40. Snowling MJ. Specific learning difficulties. Psychiatry 2005;4:110–3. [Google Scholar]
- 41. Milton D. A critique of the use of Applied Behavioural Analysis (ABA): on behalf of the Neurodiversity manifesto steering group. Kent Acad Repos. Canterbury, UK: University of Kent, 2018. https://kar.kent.ac.uk/69268/1/Appliedbehaviouranalysis.pdf. [Google Scholar]
- 42. Jurecic A. Neurodiversity. Coll English 2007;69:421–42. [Google Scholar]
- 43. Pollack D. (ed.). Neurodiversity in Higher Education. Chichester, UK: Wiley-Blackwell, 2009 [Google Scholar]
- 44. Garner JK. Conceptualizing the relations between executive functions and self-regulated learning. J Psychol 2009;143:405–26. [DOI] [PubMed] [Google Scholar]
- 45. Quinn PO. Treating adolescent girls and women with ADHD: gender-specific issues. J Clin Psychol 2005;61:579–87. doi: 10.1002/jclp.20121. [DOI] [PubMed] [Google Scholar]
- 46. Mandy W, Tchanturia K. Do women with eating disorders who have social and flexibility difficulties really have autism? A case series. Mol Autism 2015;6:1–11. doi: 10.1186/2040-2392-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. D’Souza H, Karmiloff-Smith A. Neurodevelopmental disorders. Wiley Interdiscip Rev Cogn Sci 2017;8:1–10. doi: 10.1002/wcs.1398. [DOI] [PubMed] [Google Scholar]
- 48. White HA, Shah P. Uninhibited imaginations: creativity in adults with attention-deficit/hyperactivity disorder. Pers Individ Differ 2006;40:1121–31. doi: 10.1016/j.paid.2005.11.007. [DOI] [Google Scholar]
- 49. Meilleur AAS, Jelenic P, Mottron L. Prevalence of clinically and empirically defined talents and strengths in autism. J Autism Dev Disord 2015;45:1354–67. doi: 10.1007/s10803-014-2296-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Logan J. Dyslexic entrepreneurs: the incidence; their coping strategies and their business skills. Dyslexia 2009;15:328–46. [DOI] [PubMed] [Google Scholar]
- 51. Todd R. Working with Dyspraxia - a Hidden Asset Dyspraxia Foundation Guide for Employers. London: Dyspraxia Foundation, 2011 [Google Scholar]
- 52. Sedgwick JA, Merwood A, Asherson P. The positive aspects of attention deficit hyperactivity disorder: a qualitative investigation of successful adults with ADHD. Atten Defic Hyperact Disord 2019;241–53. [DOI] [PubMed] [Google Scholar]
- 53. Brownlow C. Re-presenting autism: the construction of NT syndrome. J Med Humanit 2010;31:243–55. doi: 10.1007/s10912-010-9114-4. [DOI] [PubMed] [Google Scholar]
- 54. Shelley-Tremblay JF, Rosen LA. Attention deficit hyperactivity disorder: an evolutionary perspective. J Genet Psychol 1996;157:443–53. doi: 10.1080/00221325.1996.9914877. [DOI] [PubMed] [Google Scholar]
- 55. Kapp SK, Gillespie-Lynch K, Sherman LE et al. Deficit, difference, or both? Autism and neurodiversity. Dev Psychol 2013;49:59–71. doi: 10.1037/a0028353. [DOI] [PubMed] [Google Scholar]
- 56. Karmiloff-Smith A. Nativism versus neuroconstructivism: rethinking the study of developmental disorders. Dev Psychol 2009;45:56–63. doi: 10.1037/a0014506. [DOI] [PubMed] [Google Scholar]
- 57. Williams NM, Zaharieva I, Martin A et al. Rare chromosomal deletions and duplications in attention-deficit hyperactivity disorder: a genome-wide. Lancet 2010;376:1401–8. doi: 10.1016/S0140-6736(10)61109-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lewin K. Principles of Topographical Psychology. New York: McGraw-Hill, 1936 [Google Scholar]
- 59. United Nations. United Nations Convention on the Rights of Persons with Disabilities. 2006:1–28. New York: United Nations. https://www.un.org/disabilities/documents/convention/convention_accessible_pdf.pdf.
- 60. U.S. Equal Employment Opportunities Commission Americans With Disabilities Act Washington, DC, United States Congress; 2008. https://www.eeoc.gov/laws/statutes/adaaa.cfm.
- 61. United Kingdom Parliament Equality Act. 2010. London: United Kingdom Parliament. http://www.legislation.gov.uk/ukpga/2010/15/introduction.
- 62. The Center for Universal Design The Principles of Universal Design, Version 2.0 . Raleigh, NC: Center for Universal Design; 1997. https://projects.ncsu.edu/ncsu/design/cud/about_ud/udprinciples.htm. Accessed May 15, 2020. [Google Scholar]
- 63. Beer J, Engels J, Heerkens Y et al. Factors influencing work participation of adults with developmental dyslexia: a systematic review. BMC Public Health 2014;14:1–77. doi: 10.1186/1471-2458-14-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Doyle N, McDowall A. Context matters: a systematic review of coaching as a disability accommodation. PLoS One 2019;14:1–30. doi: 10.1371/journal.pone.0199408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Snowling MJ, Adams JW, Bowyer-Crane C et al. Levels of literacy among juvenile offenders: the incidence of specific reading difficulties. Crim Behav Ment Health 2000;10:229–41. doi: 10.1002/cbm.362. [DOI] [Google Scholar]
- 66. Young S, González RA, Fridman M et al. The economic consequences of attention - deficit hyperactivity disorder in the Scottish prison system. BMC Psychiatry 2018;18:1–11. doi: 10.1186/s12888-018-1792-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Fazel S, Xenitidis K, Powell J. The prevalence of intellectual disabilities among 12 000 prisoners - a systematic review. Int J Law Psychiatry 2008;31:369–73. doi: 10.1016/j.ijlp.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 68. Jensen J, Lindgren M, Andersson K et al. Cognitive intervention in unemployed individuals with reading and writing disabilities. Appl Neuropsychol 2000;7:223–36. doi: 10.1207/S15324826AN0704_4. [DOI] [PubMed] [Google Scholar]
- 69. Edwin MF. Adult ADHD outcome audit based on NICE guidelines. Adv Ment Heal Intellect Disabil 2014;8:331–7. doi: 10.1108/AMHID-08-2013-0054. [DOI] [Google Scholar]
- 70. Carter EW, Austin D, Trainor AA. Predictors of postschool employment outcomes for young adults with severe disabilities. J Disabil Policy Stud 2012;23:50–63. doi: 10.1177/1044207311414680. [DOI] [Google Scholar]
- 71. G a H, Koller JR, Thomas CD. Post-high school outcomes of high IQ adults with learning disabilities. J Educ Gift 1999;22:266–81. [Google Scholar]
- 72. Doyle N, Patton E, Fung L et al. Diamond in the rough? Neurodiversity inclusion in practice In: Society of Industrial and Organizational Psychology Annual Conference. Bowling Green, OH: American Psychological Association, 2020 [Google Scholar]
- 73. Doyle N, Cleaver S. Collaborative research on dyslexia: incidence, adjustments, and health outcomes In: Division of Occupational Psychology Annual Conference. Nottingham: British Psychological Society, 2015 [Google Scholar]
- 74. Doyle N, McDowall A. Is coaching an effective adjustment for dyslexic adults? Coach An Int J Theory Pract 2015;8:154–68. [Google Scholar]
- 75. Hock MF. Effective literacy instruction for adults with specific learning disabilities: implications for adult educators. J Learn Disabil 2012;45:64–78. doi: 10.1177/0022219411426859. [DOI] [PubMed] [Google Scholar]
- 76. Corbière M, Villotti P, Lecomte T et al. Work accommodations and natural supports for maintaining employment. Psychiatr Rehabil J 2014;37:90–8. doi: 10.1037/prj0000033. [DOI] [PubMed] [Google Scholar]
- 77. Telwatte A, Anglim J, Wynton SKA et al. Workplace accommodations for employees with disabilities: a multi-level model of employer decision making. Rehabil Psychol 2017;61:7–19. [DOI] [PubMed] [Google Scholar]
- 78. Doyle N. Reasonable adjustments for dyslexia. Occup Heal Work 2019;16:28–31. [Google Scholar]
- 79. Santuzzi AM, Waltz PR, Finkelstein LM et al. Invisible disabilities: unique challenges for employees and organizations. Ind Organ Psychol 2014;7:204–19. doi: 10.1111/iops.12134. [DOI] [Google Scholar]
- 80. McGonagle AK, Beatty JE, Joffe R. Coaching for workers with chronic illness: evaluating an intervention. J Occup Health Psychol 2014;19:385–98. doi: 10.1037/a0036601. [DOI] [PubMed] [Google Scholar]
- 81. Dong S. Workplace accommodations, job performance and job satisfaction among individuals with sensory disabilities. Aust J Rehabil Couns 2013;19:1323–8922. [Google Scholar]
- 82. Heslin M, Howard L, Leese M et al. Randomized controlled trial of supported employment in England: 2 year follow-up of the supported work and needs (SWAN) study. World Psychiatry 2011;10:132–7. doi: 10.1002/j.2051-5545.2011.tb00035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Matza LS, Paramore C, Prasad M. A review of the economic burden of ADHD. Cost Eff Resour Alloc 2005;3:5. doi: 10.1186/1478-7547-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Jacob A, Scott M, Falkmer M et al. The costs and benefits of employing an adult with autism spectrum disorder: a systematic review. PLoS One 2015;10:1–16. doi: 10.1371/journal.pone.0139896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Knapp M, Patel A, Curran C et al. Supported employment: cost-effectiveness across six European sites. World Psychiatry 2013;12:60–8. doi: 10.1002/wps.20017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Melvill D, Stevens C, Vaid L. Access to Work Cost Benefit Analysis. London: Centre for Economic and Social Inclusion, 2015.
- 87. CIPD Annual Report. London: Chartered Institute of Personnel Development; 2007. https://www2.cipd.co.uk/NR/rdonlyres/746F1183-3941-4E6A-9EF6-135C29AE22C9/0/recruitmentsurv07.pdf.
- 88. Graffam J, Smith K, Shinkfield A et al. Employer benefits and costs of employing a person with a disability. J Vocat Rehabil 2002;17:251–63. [Google Scholar]
- 89. Adams L, Tindle A, Downing C et al. Access to Work: Qualitative Research with Applicants, Employers and Delivery Staff. London: Department of Work and Pensions; 2018
- 90. Quinn PO. Treating adolescent girls and women with ADHD: gender-specific issues. J Clin Psychol 2005;61:579–87. doi: 10.1002/jclp.20121. [DOI] [PubMed] [Google Scholar]
- 91. Kandola B. Racism at Work: The Danger of Indifference. Oxford: Pearn Kandola Publishing, 2018 [Google Scholar]
- 92. Kang S, Harvey EA. Racial Differences Between Black Parents’ and White Teachers' Perceptions of Attention-Deficit/Hyperactivity Disorder Behavior. Journal of Abnormal Child Psychology 2020;48:661–72. 10.1007/s10802-019-00600-y. [DOI] [PubMed] [Google Scholar]
- 93. Mandell DS, Wiggins LD, Carpenter LA et al. Racial/ethnic disparities in the identification of children with autism spectrum disorders. American Journal of Public Health 2009;99:493–8. 10.2105/AJPH.2007.131243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Young S, Adamo N, Ásgeirsdóttir BB et al. Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women. BMC Psychiatry 2020;20:404. 10.1186/s12888-020-02707-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Rios D, Magasi S, Novak C et al. Conducting accessible research: including people with disabilities in public health, epidemiological, and outcomes studies. Am J Public Health 2016;106:2137–44. doi: 10.2105/AJPH.2016.303448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Schrader S, Malzer V, Bruyère S. Perspectives on disability disclosure: the importance of employer practices and workplace climate. Empl Responsib Rights J 2014;26:237–55. doi: 10.1007/s10672-013-9227-9. [DOI] [Google Scholar]
- 97. Madaus JW, Foley TE, McGuire JM et al. Employment self-disclosure of postsecondary graduates with learning disabilities: rates and rationales. J Learn Disabil 2002;35:364–9. [DOI] [PubMed] [Google Scholar]
- 98. Colella A, DeNisi AS, Varma A. The impact of ratee’s disability on performance judgments and choice as partner: the role of disability-job fit stereotypes and interdependence of rewards. J Appl Psychol 1998;83:102–11. doi: 10.1037/0021-9010.83.1.102. [DOI] [PubMed] [Google Scholar]
- 99. Gerber PJ, Batalo CG, Achola EO. Dyslexia and learning disabilities in Canada and the UK: the impact of its disability employment laws. Dyslexia 2012;18:166–73. doi: 10.1002/dys.1441. [DOI] [PubMed] [Google Scholar]
- 100. Scope Disability employment gap has barely changed in a decade. 2018. https://www.scope.org.uk/About-Us/Media/Press-releases/May-2018-(1)/Disability-employment-gap-has-barely-changed-in-a. Published 2018. Accessed December 21 2019.
- 101. NAS The Autism Employment Gap: Too Much Information in the Workplace . London: The National Autistic Society; 2016. http://www.autism.org.uk/about/what-is/myths-facts-stats.aspx. [Google Scholar]
- 102. Livingston LA, Shah P, Happé F. Compensatory strategies below the behavioural surface in autism: a qualitative study. Lancet Psychol 2019;6:766–77. doi: 10.1016/S2215-0366(19)30224-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Paul KI, Moser K. Unemployment impairs mental health: meta-analyses. J Vocat Behav 2009;74:264–82. [Google Scholar]
- 104. ACAS Reasonable adjustments in the workplace. http://www.acas.org.uk/index.aspx?articleid=6074. Published 2016. Accessed May 4, 2018.
- 105. TUC Disabilty and Work. Revised Ed. London: Trade Union Congress; 2011. https://www.tuc.org.uk/sites/default/files/extras/disabilityandwork.pdf. [Google Scholar]
- 106. Markram K, Markram H. The intense world theory - a unifying theory of the neurobiology of autism. Front Hum Neurosci 2010;4:1–29. doi: 10.3389/fnhum.2010.00224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Shulamite AG, Hernandez L, Tottenham N et al. Daprettor M. neurobiology of sensory overresponsivity in youth with autism spectrum disorders. J Am Med Assoc Psychiatry 2015;72:778–86. doi: 10.1001/jamapsychiatry.2015.0737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Robertson CE, Baron-Cohen S. Sensory perception in autism. Nat Rev Neurosci 2017;18:671–84. doi: 10.1038/nrn.2017.112. [DOI] [PubMed] [Google Scholar]
- 109. Ryan S. Meltdowns, surveillance and managing emotions; going out with children with autism. Healthplace 2010;16:868–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Ozbilgin MF, Beauregard TA, Tatli A et al. Work-life, diversity and intersectionality: a critical review and research agenda. Int J Manag Rev 2011;13:177–98. doi: 10.1111/j.1468-2370.2010.00291.x. [DOI] [Google Scholar]
- 111. Triana R. Evidence-based policy: a realist perspective, by ray Pawson. J Policy Pract 2008;7:321–3. doi: 10.1080/15588740802262039. [DOI] [Google Scholar]
- 112. Simpson B. Pragmatism: a philosophy of practice In: Cassell C, Cunliffe AL, Grandy G (eds.). SAGE Handbook of Qualitative Business and Management Research Methods. London: Sage Publications Ltd, 2018,54–68. [Google Scholar]
- 113. Catalá-López F, Hutton B, Núñez-Beltrán A et al. The pharmacological and non-pharmacological treatment of attention deficit hyperactivity disorder in children and adolescents: a systematic review with network meta-analyses of randomised trials. PLoSONE 2017;12. doi: 10.1371/journal.pone.0180355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Danielson M, Bitsko R, Ghandour R et al. Prevalence of parent-reported ADHD diagnosis and associated treatment among US children and adolescents, 2016. J Clin Child Adolesc Psychol 2018;47:199–212. doi: 10.1080/15374416.2017.1417860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Lange KW, Reichl S, Lange KM et al. The history of attention deficit hyperactivity disorder. ADHD Atten Deficit Hyperact Disord 2010;2:241–55. doi: 10.1007/s12402-010-0045-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Sharkey L, Fitzgerald M. The History of Attention Deficit Disorder In: Handbook of Attention Deficit Disorder. Chichester, UK: John Wiley & Sons, 2007 [Google Scholar]
- 117. American Psychiatric Association Diagnostic and Statistical Manual of the Mental Disorders (DSM II), 2nd edn. Washington DC: American Psychiatric Publishing, 1968. [Google Scholar]
- 118. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-III), 3rd edn. Washington DC: American Psychiatric Publishing, 1980. [Google Scholar]
- 119. Engert V, Pruessner J. Dopaminergic and noradrenergic contributions to functionality in ADHD: the role of methylphenidate. Curr Neuropharmacol 2009;6:322–8. doi: 10.2174/157015908787386069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Willcutt EG, Doyle AE, Nigg JT, Faraone S V., Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry 2005;57(11):1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 121. Danielson M, Visser S, Chronis-Tuscano A et al. A national description of treatment among U.S. children and adolescents with ADHD. J Pediatr 2018;192:240–6. doi: 10.1016/j.jpeds.2017.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Elsabbagh M, Divan G, Koh Y et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res 2012;5:160–79. doi: 10.1002/aur.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Wolff S. The history of autism. Eur Child Adolesc Psychiatry 2004;13:201–8. doi: 10.1007/s00787-004-0363-5. [DOI] [PubMed] [Google Scholar]
- 124. Kanner L. Autistic disturbances of affective contact. Acta Paedopsychiatr 1968;35(4):100–136. [PubMed] [Google Scholar]
- 125. Evans B. How autism became autism: the radical transformation of a central concept of child development in Britain. Hist Human Sci 2013;26:3–31. doi: 10.1177/0952695113484320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Frith U, Happe F. Autism: beyond theory of mind. Cognition 1994;50:115–32. doi: 10.1016/0010-0277(94)90024-8. [DOI] [PubMed] [Google Scholar]
- 127. Wing L, Gould J. Severe impairments of social interaction and associated abnormalities in children: epidemiology and classification. J Autism Dev Disord 1979;9:11–29. [DOI] [PubMed] [Google Scholar]
- 128. Muhle RA, Reed HE, Stratigos KA et al. The emerging clinical neuroscience of autistic Spectrum disorder. J Am Med Assoc Psychiatry 2018;75:514–23. doi: 10.1001/jamapsychiatry.2017.4685. [DOI] [PubMed] [Google Scholar]
- 129. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM V), 5th edn. Washington DC: American Psychiatric Publishing, 2013. [Google Scholar]
- 130. Blank R, Barnett AL, Cairney J et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Dev Med Child Neurol 2019;61:242–85. doi: 10.1111/dmcn.14132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Collier J, Adie W. Diseases of the Nervous System In: Price, ed In: Textbook of Medicine, 1st edn. N/K: N/K, 1922,1332–711.
- 132. Gubbay S. The Clumsy Child: A Study of Developmental Apraxia and Agnostic Ataxia. London: WB Saunders, 1975. [Google Scholar]
- 133. Kirby P. A brief history of dyslexia. Psychologist 2018;31:56–9. https://thepsychologist.bps.org.uk/volume-31/march-2018/brief-history-dyslexia. [Google Scholar]
- 134. Orton ST. A neurological explanation of the reading disability. Educ Rec 1937;12:58–68. [Google Scholar]
- 135. Shaywitz SA. Dyslexia. N Engl J Med 1998;338:307–12. [DOI] [PubMed] [Google Scholar]
- 136. Swanson HL, Siegel LA. Learning disabilities as a working memory deficit. Issues Educ Contrib Educ Psychol 2001;7:1–48. [Google Scholar]
- 137. Elliot J, Grigorenko E. The Dyslexia Debate. Connecticut, US: Yale University, 2014. [Google Scholar]
- 138. Bishop DVM, Snowling MJ, Blakemore S-J (eds.). Neurocognitive Approaches to Developmental Disorders: Festschrift to Uta Frith. London: Psychology Press, 2007. [Google Scholar]
- 139. Siok WT, Spinks JA, Jin Z et al. Developmental dyslexia is characterized by the co-existence of visuospatial and phonological disorders in Chinese children. Curr Biol 2009;19:890–2. doi: 10.1016/j.cub.2009.08.014. [DOI] [PubMed] [Google Scholar]
- 140. Adamou M, Arif M, Asherson P et al. Occupational issues of adults with ADHD. BMC Psychiatry 2013;13:59. doi: 10.1186/1471-244X-13-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Prevatt F, Yelland S. An empirical evaluation of ADHD coaching in college students. J Atten Disord 2013;1–12. doi: 10.1177/1087054713480036. [DOI] [PubMed] [Google Scholar]
- 142. Kessler RC, Lane M, Stang PE, Brunt DL. The prevalence and workplace costs of adult attention deficit hyperactivity disorder in a large manufacturing firm. Psychol Med 2009;39:137–47. doi: 10.1017/S0033291708003309. [DOI] [PubMed] [Google Scholar]
- 143. Halmøy A, Fasmer OB, Gillberg C et al. Occupational outcome in adult ADHD: impact of symptom profile, comorbid psychiatric problems, and treatment: a cross-sectional study of 414 clinically diagnosed adult ADHD patients. J Atten Disord 2009;13:175–87. doi: 10.1177/1087054708329777. [DOI] [PubMed] [Google Scholar]
- 144. Coetze G, Gibbison G. Mediating influence of time management on the relationship between adult attention deficit disorder and the operational effectiveness of project managers. J Manag Dev 2013;35:970–84. doi: 10.1108/MRR-09-2015-0216. [DOI] [Google Scholar]
- 145. White HA, Shah P. Uninhibited imaginations: creativity in adults with attention-deficit/hyperactivity disorder. Pers Individ Dif 2006;40:1121–31. doi: 10.1016/j.paid.2005.11.007. [DOI] [Google Scholar]
- 146. Wehman P, Brooke V, Brooke AM et al. Employment for adults with autism spectrum disorders: a retrospective review of a customized employment approach. Res Dev Disabil 2016;53-54:61–72. doi: 10.1016/j.ridd.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 147. Howlin P, Alcock J, Burkin C. An 8 year follow-up of a specialist supported employment service for high-ability adults with autism or Asperger syndrome. Autism 2005;9:533–49. doi: 10.1177/1362361305057871. [DOI] [PubMed] [Google Scholar]
- 148. Katz N, Dejak I, Gal E. Work performance evaluation and QoL of adults with high functioning autism Spectrum disorders (HFASD). Work J Prev Assess Rehabil 2015;51:887–92. doi: 10.3233/WOR-152001. [DOI] [PubMed] [Google Scholar]
- 149. Meilleur AAS, Jelenic P, Mottron L. Prevalence of clinically and empirically defined talents and strengths in autism. J Autism Dev Disord 2015;45:1354–67. doi: 10.1007/s10803-014-2296-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Losse A, Henderson SE, Elliman D et al. Clumsiness in children--do they grow out of it? A 10-year follow-up study. Dev Med Child Neurol 1991;33:55–68. doi: 10.1111/j.1469-8749.1991.tb14785.x. [DOI] [PubMed] [Google Scholar]
- 151. Bartlett D, Moody S, Kindersley K. Dyslexia in the workplace. London: Wiley 2010. doi: 10.1002/9780470669341.ch1. [DOI] [Google Scholar]
- 152. Baker SF, Ireland JL. The link between dyslexic traits, executive functioning, impulsivity and social self-esteem among an offender and non-offender sample. Int J Law Psychiatry 2007;30:492–503. doi: 10.1016/j.ijlp.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 153. Leather C, Hogh H, Seiss E et al. Cognitive functioning and work success in adults with dyslexia. Dyslexia 2011;17:327–38. doi: 10.1002/dys.441. [DOI] [PubMed] [Google Scholar]
- 154. Karolyi C, Winner E, Gray W et al. Dyslexia linked to talent: global visual-spatial ability. Brain Lang 2003;85:427–31. [DOI] [PubMed] [Google Scholar]
- 155. Eide B, Eide F. The Dyslexic Advantage. Plume: New York, NY, 2011. [Google Scholar]
- 156. Singer J. Odd People In: The Birth of Community Amongst People on the “Autistic Spectrum”: a Personal Exploration of a New Social Movement based on Neurological Diversity. Sydney: University of Technology, 1998. [Google Scholar]
- 157. Walker N. Throw away the master’s tools: liberating ourselves from the pathology paradigm In: Bascombe J. (Ed.), Loud Hands: Autistic People, Speaking. Washington DC: Autistic Self Advocacy Network, 2012,225–237 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or quantitatively analysed in support of this review.


