Supplemental Digital Content is available in the text.
Keywords: angiography, dilatation, odds ratio, percutaneous coronary intervention, stent
Abstract
Background:
Clinical implications of online 3-dimensional optical frequency domain imaging (3D-OFDI)-guided stenting for bifurcation lesions have not been investigated in the randomized controlled trials. The purpose of this study was to determine whether online 3D-OFDI-guided stenting is superior to angiography-guided percutaneous coronary intervention (PCI) in terms of incomplete stent apposition at the bifurcation segment.
Methods:
The OPTIMUM trial (Online 3-Dimensional Optical Frequency Domain Imaging to Optimize Bifurcation Stenting Using UltiMaster Stent) was a randomized, multicenter clinical trial. Eligible patients had an angiographically significant stenosis in the bifurcation lesion treated with a provisional single stent strategy using the Ultimaster sirolimus eluting stent. Patients were randomly allocated to either online 3D-OFDI-guided or angiography-guided PCI. Patients randomized to 3D-OFDI guidance underwent online 3D-OFDI assessment after rewiring into the jailed side branch after stenting and proximal optimization technique, while in the angiography guidance arm, rewiring was performed using conventional fluoroscopic/angiographic guidance. The primary end point of this trial was the postprocedural average percentage of malapposed struts per lesion assessed by OFDI in the confluence zone of the main and side branches.
Results:
Between June 8, 2017 and September 26, 2018, 110 patients with 111 bifurcation lesions were randomized at 4 Japanese centers. Of these, 56 patients with 57 lesions were treated with 3D-OFDI-guided PCI, whereas 54 patients with 54 lesions were treated with angiography-guided PCI. In the 3D-OFDI guidance arm, the feasibility of online 3D-OFDI was 98.2%. The average percentage of incomplete stent apposition per lesion at bifurcation was lower in the 3D-OFDI guidance arm than that in the angiography guidance arm (19.5±15.8% versus 27.5±14.2%, P=0.008). The superiority of the 3D-OFDI guidance arm was also confirmed in the strut level analysis (odds ratio: 0.54 [95% CI, 0.36–0.81]; P=0.003).
Conclusions:
Online 3D-OFDI-guided bifurcation PCI was superior to angiography-guided bifurcation PCI in terms of acute incomplete stent apposition at bifurcation.
Registration:
URL: https://www.clinicaltrials.gov. Unique identifier: NCT02972489.
What Is Known
Intravascular optical frequency domain imaging has a clear advantage over conventional angiography in depicting a bifurcation lesion without limitations of angiography such as overlap and foreshortening.
The feasibility and efficacy of online 3-dimensional-optical frequency domain imaging guidance for bifurcation percutaneous coronary intervention have been reported based on retrospective observational data but have not yet been investigated in the context of a randomized controlled trial.
What the Study Adds
The randomized OPTIMUM trial (Online 3-Dimensional Optical Frequency Domain Imaging to Optimize Bifurcation Stenting Using UltiMaster Stent) first showed online 3-dimensional-optical frequency domain imaging–guided stenting for bifurcation to be superior to angiography-guided stenting in terms of acute incomplete stent apposition at bifurcation with excellent feasibility.
Further trials are warranted to confirm the long-term clinical benefit of online 3-dimensional-optical frequency domain imaging–guided stenting for bifurcation lesions.
Percutaneous coronary intervention (PCI) with drug-eluting stent (DES) implantation is a common revascularization method for coronary artery disease with appropriate complexity of disease. By nature, coronary arteries taper at bifurcations with a flow conservation from main vessel (MV) and side branch (SB). Currently, coronary bifurcation lesions account for 15% to 20% of all patients undergoing PCI.1 Because of the uneven distribution of shear stress at the bifurcation lesions, early plaque progression occurs in the lateral aspect of the bifurcation with low shear stress, often resulting in continuous atherosclerotic plaque extending from the proximal MV toward the daughter branches.2 Stenting of the coronary bifurcation is complex and requires modification of the coronary stents shape from their cylindrical geometry to fit the natural tapering anatomy of the bifurcation. This modification of stent shape is achieved through balloon dilatation following stent deployment through proximal optimization technique (POT), standard post dilatation, and kissing balloon dilatation (KBD) technique.
The current guidelines for myocardial revascularization of coronary bifurcations recommend a provisional one stent strategy as a default stenting technique.3 After placing a DES in the MV across SB ostium, POT with larger balloon is performed. This is followed by recrossing the wire to the SB and the KBD is recommended.4 Ideally, to reconstruct natural shape and restore rheology at the bifurcation, any presence of metallic strut in front of the SB should be avoided. Technically, this could be achieved by recrossing through the optimal distal cell of the MV stent before the KBD (Figure I in the Data Supplement).5
Angiography is inherently limited in the visualization of both bifurcation carina and the stent structure. Recently, optical frequency domain imaging (OFDI: LUNAWAVE, Terumo Corporation, Tokyo, Japan) with its high-speed pullback has enabled 3-dimensional (3D) reconstruction of complex bifurcation anatomies and its relationship with the metallic structure. This novel imaging functionality is available in consoles and ready to use in the catheterization laboratory as an online software tool. Previous retrospective data and published case reports have suggested that it is feasible to perform online visualization of the bifurcation rewiring position and that this approach can improve acute outcomes such as incomplete stent apposition (ISA). However, additional OFDI pullback step in the catheterization laboratories will increase the amount of total contrast volume as well as procedural time for the patients.6,7 The efficacy of online 3D-OFDI-guided PCI in reduction of ISA has not yet been investigated prospectively in the context of a randomized controlled trial.
The main objective of this trial was to determine the superiority of the online 3D-OFDI-guided PCI to angiography-guided PCI in terms of ISA at the coronary bifurcation segment.
Methods
The authors declare that all supporting data are available within the article and its Data Supplement.
Study Design and Patients
The design of the OPTIMUM trial (Online 3-Dimensional Optical Frequency Domain Imaging to Optimize Bifurcation Stenting Using UltiMaster Stent; NCT 02972489) has been described elsewhere.8 The OPTIMUM trial was a randomized (1:1; 3D-OFDI guidance arm versus angiography guidance arm), active control, multicenter clinical trial across 4 Japanese canters (Table I in the Data Supplement). Major eligibility criteria were the presence of de novo, native, previously unstented bifurcation lesion(s) with a SB diameter of ≥2.0 mm (by visual estimation) to be treated by PCI with a single stent strategy. Detailed inclusion and exclusion criteria are shown in Table II in the Data Supplement. All patients signed the informed consent. The study was approved by the central and local ethics committees.
Randomization
Patients who met the eligibility criteria were randomly assigned (1:1) to either 3D-OFDI-guided PCI or angiography-guided PCI. Randomization was performed by local investigators using a Web-based software with random blocks stratified by center.8
Procedures
Detailed information on the study procedure has been provided elsewhere.8 For all bifurcation lesions, the intention was to treat them with a provisional single stent strategy with the Ultimaster sirolimus eluting stent(s) (Terumo Corporation, Tokyo, Japan). The Ultimaster DES is available in diameters from 2.25 to 4.0 mm, and in lengths from 12 to 38 mm. Stent size was determined by the distal reference MV diameter. After stenting the MV, POT was mandatory with 0.25 to 0.5 mm larger balloon than the device size following the recommendations by the European Bifurcation Club.9 In both arms, the proximal reference measured by OFDI before stent implantation could be used for the selection of the balloon size for POT. Patients randomized to 3D-OFDI guidance arm underwent online 3D-OFDI assessment of the MV after rewiring into the jailed SB following stent implantation. The OFDI image was acquired from approximately >10 mm distal to the distal edge of the MV stent with blood removal by contrast media at a pullback-speed of 20 mm/s. The recrossing point was assessed with online 3D-OFDI image reconstruction on the console. The TERUMO OFDI console incorporates online software of 3D imaging with a possibility of stent enhancement, which enables the online reconstruction within one minute. If the wire was not positioned in the optimal cell (as defined in Figure II in the Data Supplement8), further attempts to redirect the wire through the right cell were performed, with subsequent OFDI imaging to confirm the position in 2-dimensional and online 3D reconstructions. The final recrossing position was recorded based on the online 3D OFDI image.
In the angiography guidance arm, wire recrossing into the SB was performed using conventional fluoroscopic/angiographic guidance. Both groups received final kissing balloon dilatation (FKBD) using balloons matching the size of the SB and of the distal MV. After performing FKBD, final OFDI imaging was performed to document the primary end point for both treatment arms.
OFDI recordings were assessed by an independent core laboratory (Cardialysis B.V., Rotterdam, The Netherlands). The OFDI analysts were blinded to the patient’s allocations. Quantitative analysis was performed using a dedicated semi-automated contour- detection system (QCU-CMS; Medis medical imaging systems bv, Leiden, The Netherlands) according to standard methods.6,10 Detailed methodology of the quantitative analysis of OFDI is shown in the Data Supplement. All angiography recordings were also analyzed by the core lab with a bifurcation dedicated quantitative coronary angiography software (Coronary Angiography Analysis System [CAAS], version 5.9, Pie Medical Imaging, Maastricht, the Netherlands).
If a case a second stent at the SB was needed due to eg, dissection, slow-flow, or high residual stenosis, the additional stenting was performed at operator’s discretion.
Dual antiplatelet therapy was continued at least 6 months in accordance with the European Society of Cardiology guidelines.3
End Points
The primary end point was superiority of 3D-OFDI guidance on the average postprocedural (FKBD) percentage of malapposed struts (or ISA) per lesion assessed by OFDI in the main branch of the bifurcation, which was calculated for each treated lesion as the ratio of the malapposed struts to the total number of struts in the bifurcation region (Figure III in the Data Supplement).11 The primary end point was also analyzed on a strut-by-strut basis considering each strut as a binary outcome (malapposed or apposed). Malapposed struts included nonapposed struts at the SB orifice. Struts located at the ostium of side branches, with no vessel wall behind, were defined as nonapposed struts at the SB orifice.11 Secondary OFDI end points are listed in the Data Supplement.12 The amount of contrast media, radiation time, and the procedure time at the index procedure were evaluated as a secondary safety end point. Of note, this trial was designed as a proof-of-concept, feasibility study of 3D-OFDI-guided, coronary bifurcation PCI with an imaging primary end point (malapposition); the study is underpowered for clinical end points. The clinical follow-up at 6- and 12-months post-procedure was performed to ensure the safety of the patients by either hospital visit or telephone contact. All-cause death, myocardial infarction, revascularization, and stent thrombosis according to ARC definition were reported.13
Statistical Analysis
Based on the data from past registries, angioguidance would result in a 26% average malapposition rate per lesion (20% SD) in bifurcation segment (confluence zone of main branch and side branch) and a 5% attrition rate due to insufficient quality of the OFDI image could be expected.7,14 Assuming that 3D-OFDI guidance reduces average malapposition rate per lesions by 50% (a 13% for the 3D-OFDI-guidance with a 20% SD), a sample size of 106 patients would be needed to demonstrate superiority of 3D-OFDI guidance with a 5% 2-sided level of significance (alpha) and a statistical power of 90%. The primary analyses were based on the intention to treat population. The averaging percentage method for the primary end point has to face the 2 following statistical issues: (1) the imposed limits on the distribution; (2) unequal weight for each strut. To address these issues, as a post hoc sensitivity analysis, the primary end point of the incidence of malapposed struts at bifurcation was also analyzed considering each strut as a binary outcome (malapposed or apposed) with a mixed-effects logistic regression model, accounting for the correlation of multiple struts within the same patient/lesion by including patient/lesion as a random effect. There were no formal interim analyses and stopping guidelines.
Categorical variables are summarized as frequencies and percentages and were compared between groups using Pearson χ2 or Fisher exact test, as appropriate. Continuous variables are presented as mean±SD or median (interquartile) and compared between groups using 2-tailed, unpaired t tests or Mann-Whitney test, as appropriate. Stratified analysis of lesions with 3 different patterns of configurations of overhanging struts at the carina was performed on the average percentage of ISA per lesion at bifurcation using 1-way ANOVA. A Tukey test was performed to identify the group with the greatest effect on the responsible variable.
A 2-sided P value of <0.05 was considered to indicate statistical significance. All statistical analyses were performed with SPSS (version 27.0.0, IBM, New York).
Role of the Funding Source
The OPTIMUM study was an investigator-initiated trial, the grant was given to the Meditrix (research organization) who acted as a sponsor per request of investigators. The grant-giver (TERUMO) did not have any role in design, data collection, interpretation, and writing of the manuscript. Intravascular imaging itself is fully reimbursed by national insurance in Japan and OFDI was therefore conducted as a part of daily practice.
Results
Between June 8, 2017 and Sep 26, 2018, 110 patients with 111 bifurcation lesions were randomized to 3D-OFDI-guided PCI (56 patients with 57 lesions) and angiography-guided PCI (54 patients with 54 lesions; Figure 1). Representative cases in each arm are shown in Figure 2.
Figure 1.

Study flow chart. 3D indicates 3-dimensional; ISA, incomplete stent apposition; KBD, kissing balloon dilatation; L, lesion; OFDI, optical frequency domain imaging; PCI, percutaneous coronary intervention; and POT, proximal optimization technique.
Figure 2.

Representative cases of angiography-guided and online 3-dimensional (3D)-optical frequency domain imaging (OFDI)-guided percutaneous coronary intervention. Sixty-nine-y-old female with Medina 0, 1, 0 left main (LM) bifurcation lesion (diameter stenosis by quantitative coronary angiography: 58% in left anterior descending artery [LAD]) was randomized to the angiography arm (A). A 3.0×15 mm Ultimaster stent (B: yellow dotted line) was implanted in the LM toward proximal LAD, followed by proximal optimization technique (POT) with a 4.0 mm balloon and subsequent wire recrossing to the left circumflex artery. After final kissing balloon dilatation (KBD), 3D-OFDI was performed for documentation purpose, which revealed presence of metallic struts in front of the side branch ostium (C). The frequency of malapposed struts (D: yellow arrow) was 33.9% by cross-sectional OFDI image. Fifty-eight-y-old male with Medina 1, 1, 1, LAD bifurcation lesion was randomized to the 3D-OFDI arm (E). A 3.0×28 mm Ultimaster stent (F: yellow dotted line) was implanted in the LAD followed by POT. After the first attempt of rewiring to the diagonal branch, 3D-OFDI revealed suboptimal position of the wire (A2-S) according to the specific classification (G). According to the protocol, crossing of the wire to the diagonal branch was repeated to achieve optimal wiring through the distal cell. A subsequent OFDI pullback confirmed the optimal position of the recrossing wire (H: A1-L). After KBD, the final OFDI image demonstrated wide opening of the sidebranch ostium without overhanging metallic structure (I and J: yellow arrow indicates malapposed strut).
Baseline characteristics did not differ between the 2 arms (Table 1). A majority of patients presented with stable angina or silent ischemia (91% in the 3D-OFDI guidance arm, 94% in the angiography guidance arm). Lesion and procedural characteristics are shown in Table 2. In the 3D-OFDI-guided treatment group, there were fewer left main (LM) bifurcation lesions (1.8% versus 14.8% in the angiography guidance arm, P=0.013) but more left anterior descending artery-diagonal branch bifurcation lesions (73.7% in the 3D-OFDI arm versus 51.9% in the angiography arm, P=0.017). The parameters derived from quantitative coronary angiography did not differ between the treatment arms (Table 3). The mean angle between distal MV and SB was relatively small in both arms (53.3±18.4° in the 3D-OFDI guidance arm versus 54.0±23.3° in the angiography guidance arm, P=0.853).
Table 1.
Baseline Characteristics
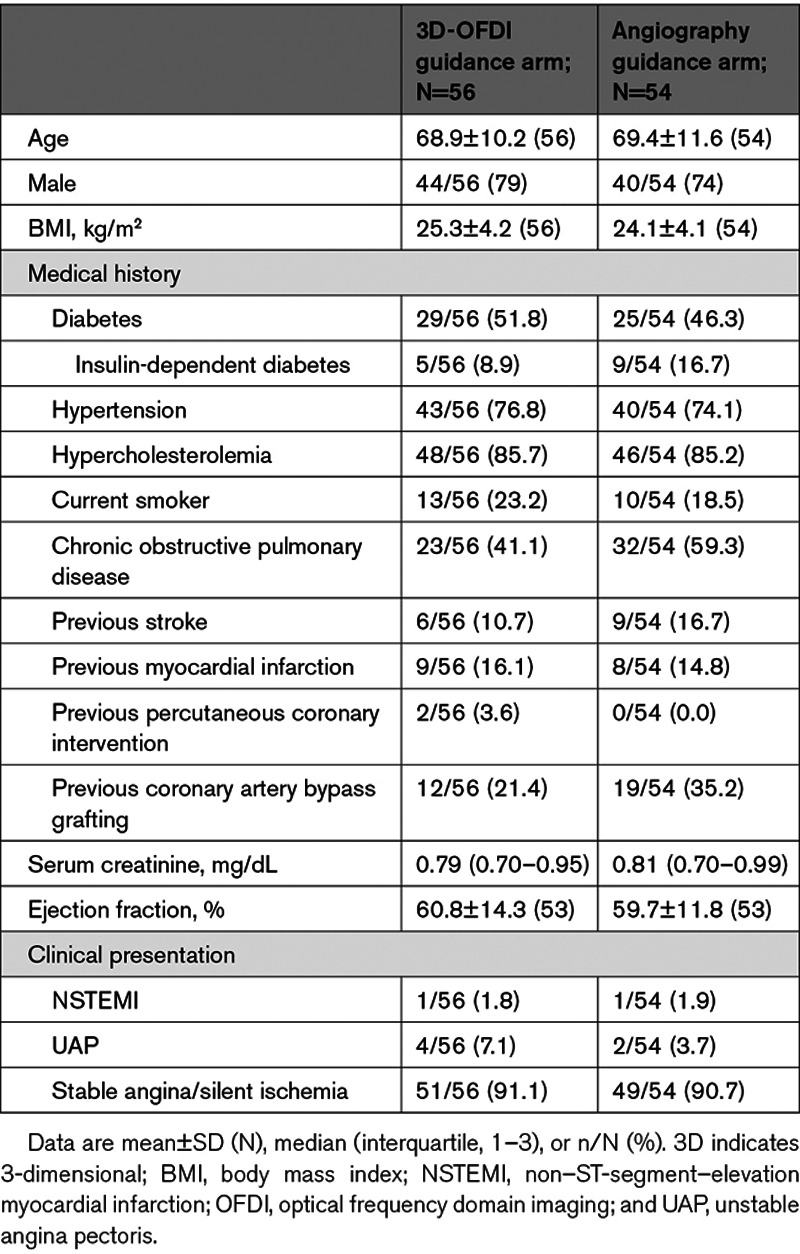
Table 2.
Lesion and Procedural Characteristics at Lesion Level

Table 3.
Dedicated Bifurcation QCA Results

Procedures
All lesions were treated with the Ultimaster DES, and POT was performed in 98.2% of the lesions (98.2% in the 3D-OFDI guidance arm versus 98.1% in the angiography guidance arm).
The final OFDI assessment after FKBD was successfully performed in 56 lesions (98.2%) and 52 lesions (96.3%) in the 3D-OFDI guidance arm and the angiography guidance arm, respectively (Figure 1). In a patient randomized to the angiography arm, a second Ultimaster stent was implanted after the final OFDI assessment, using the T-stent technique because of the dissection in the side branch. After the final OFDI assessment, additional POT was performed in 7 lesions (12.7%) in the 3D-OFDI arm and 8 lesions (16.0%) in the angiography arm (P=0.842) and additional KBD was performed in 6 lesions (10.9%) in the 3D-OFDI arm and 4 lesions (8.0%) in the angiography arm (P=0.862).
3D-OFDI Assessment of Wire Recrossing Position
Identification of the wire recrossing point with 3D-OFDI imaging during the procedure was feasible in 98.2% of lesions (56/57 lesions). The frequency of optimal cell rewiring identified by the first 3D-OFDI was 55.4% (31/56); the success rate increased to 68% at the second attempt and eventually increased to 100% after >3 attempts. The median number of 3D-OFDI runs to achieve optimal cell rewiring was 1 (interquartile range: 1–3). Regarding configurations of overhanging struts at carina, pattern A (no ring at carina) was observed in 19% of vessels, pattern B (ring at carina) was in 39%, and pattern C (ring at carina with multiple second distal compartments) was in 40% (Figure IV in the Data Supplement).
Acute ISA at Bifurcation
OFDI assessment after the FKBD was successfully performed in 56 lesions (98.2%) in the 3D-OFDI guidance arm and 52 lesions (96.3%) of the angiography guidance arm (Figure 1). Because of insufficient imaging quality, the final assessment of ISA was not feasible in 3 cases (one in the 3D-OFDI guidance arm and 2 in the angiography guidance arm). Final OFDI images after the FKBD were analyzable and available in 55 lesions and 50 lesions in the 3D-OFDI guidance arm and the angiography guidance arm, respectively.
The primary end point of superiority of online 3D-OFDI-guided PCI to the angiography-guided PCI was reached: the average percentage of malapposed struts at bifurcation in the 3D-OFDI guidance arm was significantly lower than in the angiography guidance arm (19.5±15.8% versus 27.5±14.2%, P=0.008; Figure 3). In the strut level post hoc sensitivity analysis with a mixed-effects logistic regression model, the incidence of malapposition in the 3D-OFDI guidance arm was also significantly lower than in the angiography guidance arm (21.4% [981/4583 struts] versus 29.6% [1337/4512 struts], odds ratio: 0.54 [95% CI, 0.36–0.81], P=0.003, Figure 3). In the 3D-OFDI guidance arm, the risk of malapposed struts was influenced by the complexity of configurations of overhanging struts at carina (12.0±10.1% in pattern A, 26.3±18.8% in pattern B, and 16.4 ±12.4 in pattern C, P value for overall P=0.024, Figure IV in the Data Supplement).
Figure 3.
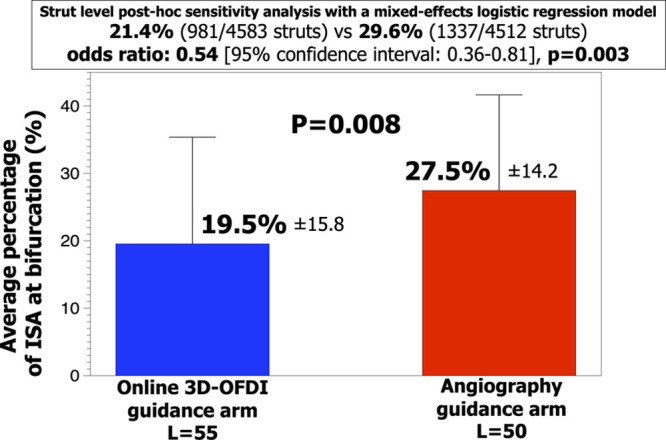
Average percentage of acute incomplete stent apposition per lesion at bifurcation. 3D indicates 3-dimensional; ISA, incomplete stent apposition; L, lesion; and OFDI, optical frequency domain imaging.
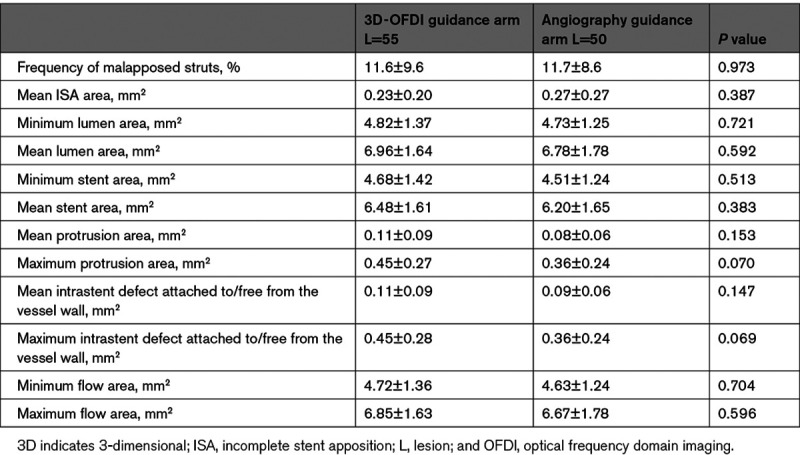
The quantitative OFDI results in the entire stented segment of the main branch did not differ between the 2 arms: the percentage of malapposed struts was 11.6±9.6% versus 11.7%±8.6% (P=0.973), minimum lumen area was 4.82±1.37 versus 4.73±1.25 mm2 (P=0.721), and mean lumen area was 6.96±1.64 versus 6.78±1.78 mm2 (P=0.592) in the 3D-OFDI guidance arm and the angiography guidance arm, respectively (Table 4). The frequencies of ISA in proximal and distal main branch also did not differ between the 2 arms. Quantitative OFDI results of the stented segment at bifurcation, proximal and distal to bifurcation are tabulated in Table III in the Data Supplement.
Table 4.
Secondary OFDI End Points After Final Kissing Balloon Dilatation in the Entire Main Branch Including Proximal, Bifurcation, and Distal Segment
The amount of contrast media, radiation time, and procedure time did not differ between arms (Table 2).
Clinical Outcomes up to 1-Year Follow-Up
Target lesion related event was not observed in the participants over 1-year follow-up. Nontarget lesion revascularization occurred in 7 and 3 patients in the 3D-OFDI and angiography arm, respectively. One patient in the 3D-OFDI arm died because of infectious myocarditis after transcatheter aortic valve implantation.
Discussion
To the best of our knowledge, the present study is the first randomized controlled trial to evaluate feasibility and efficacy of online 3D-OFDI-guided PCI for bifurcation. The main findings are the followings.
Online 3D-OFDI for identification of the wire recrossing point was feasible in all but one case (56/57 lesions, 98.2%). Optimal wire recrossing was achieved in all lesions guided by the online 3D-OFDI (56/56 lesions, 100%).
Online 3D-OFDI-guided PCI was superior to the angiography-guided PCI in terms of percentage of acute ISA at the bifurcation.
Optimal rewiring remained unachievable after POT in 45% of lesions.
The configurations of overhanging struts at carina might influence the risk of acute ISA at bifurcation in patients treated with the online 3D-OFDI-guided PCI.
In the present study, a superiority of the 3D-OFDI-guided PCI over the angiography-guided PCI was demonstrated in relation to acute ISA in the confluence zone of bifurcation. The feasibility of online 3D-OFDI in the present trial was as high as 98.2%, which was higher than previous registries using off-line optical coherence tomography (OCT) assessment. In a study of Okamura et al,11 the feasibility of the offline 3D-OCT assessment of the guidewire recrossing point after MV stenting was 89.9%. With the improvement of the console software, online assessment likely contributed to excellent feasibility through timely feedback to operators about the imaging acquisition.
In the OFDI-guidance arm, the rate of optimal cell rewiring at the first attempt was 55.4%, indicating that even after POT, in about half of the cases the wiring position was not optimal. This underlines the importance of 3D-OFDI guidance to reduce the overhanging struts in front of the side-branch ostium. Overhanging metallic struts in the bifurcation could alter microcirculation around the stent struts, reduce the coverage of struts with an area of high shear rate (metallic carina), increase the neointimal growth within the area of low shear stress causing neointimal bridge between the rim of the ostium and metallic structure,15 and finally may hinder the access to the side-branch in case of repeat revascularization in the distal side-branch at later stage. Foin et al16 reported that ISA not only affects blood flow patterns assessed by shear rate calculated in computational fluid dynamic simulation but also delays the process of strut coverage in the clinical OCT study. The pathological study also demonstrated that a higher prevalence of late stent thrombosis in DES in bare metal stent was associated with higher rate of uncovered struts at flow divider sites such as the carina region, which is likely because of flow disturbances.17 In a case report from a serial 3D-OCT follow-up of a natural course of jailed SB after MV stenting without the FKBD, Diletti et al18 reported that neointimal tissue attached on jailed struts in front of the SB ostium, which resulted in reduced blood flow areas of the SB ostium at 6 months.
By implementing the OFDI guidance, optimal wiring was achieved in 13% of lesions at the second attempt and in 32% of lesions at >3 attempts. Eventually, the frequency increased to 100% with median numbers of attempts of 1 (interquartile range, 1–3). These findings show that utilization of this technology can result in optimal rewiring and subsequently superior stent apposition. To achieve the optimal wiring, pulling back of the MB wire (or a third wire in the same direction) is recommended using angiographic projection with best visualization of the ostia of 2 daughter branches.4 When this technique fails, the use of angiographic projection perpendicular to side-branch ostial plane may be useful; although the distal main branch and side branch are overlapped in this projection, this specific angiographic view corresponds to the 3D-OFDI image of the side branch ostium, viewed from the main branch toward the distal side branch. The second wire could be manipulated and advanced into the optimal crossing point using the first recrossing wire (through the proximal cell) as landmark.
Despite a greater number of attempts to cross the optimal cell with OFDI imaging, there were no significant differences between the 3D-OFDI guidance arm and the angiography guidance arm in terms of amount of contrast media, radiation time, and procedure time. This may be attributed to shorter length of the OFDI pullback with a small amount of contrast media at the second or later attempts, since ≈10 mm visualization around polygon of confluence suffices for recognition of the wire recrossing point.
In the current study, the optimal recrossing point was identified differently according to configurations of overhanging rings and links, to avoid extreme deformation of the stent. Previous registry data have demonstrated that a link-free configuration is favorable for SB dilatation11; however, the location of the link at the bifurcation is not controllable during implantation by operators. In the current study, therefore, whenever the distal ring and/or link were in contact with the carina, the second distal cell was defined as optimal recrossing point instead of the most distal cell. This classification was incorporated into the electronic case report form and helped the operator to achieve the optimal recrossing point when the 3D-OFDI guidance was used. In addition, ring-free configuration (type A) was associated with a lower incidence of ISA at bifurcation in the 3D-OFDI arm. However, it should be acknowledged that ring-free configuration (type A) was observed only in 19.0% of lesions in the 3D-OFDI arm and the high prevalence of nonring-free configuration (type B: 39.0%) with the worst incidence of ISA at bifurcation (26.3±18.8%) might result in moderate incidence of ISA at bifurcation in the overall 3D-OFDI arm (19.5±15.8%). Although, 61% of lesions had type A and C configurations which potentially have derived benefit from the 3D-OFDI-guided bifurcation PCI and might be worth the effort of achieving favorable mechanical finding such as less ISA at bifurcation. However, this stratified analysis by the configurations was post hoc and underpowered for comparison of 3 configurations. Furthermore, the distribution of the configurations in the angiography arm could not be evaluated, as OFDI had not been performed before wire recrossing in the angiography arm according to the protocol. Further study is needed to evaluate this specific question.
Finally, ISA in bifurcation is strictly dependent on (1) the type of stent used, (2) size of SB, (3) severity of the SB lesion, and (4) angle between MV and SB: (1) DES with closed cell and more-link design can be associated with more malapposition. However, most of the currently available DESs have open cell and 2- or 3-link design. Therefore, the generalizability of the present study is acceptable with regard to type of DESs; (2) in our cohort, the reference SB diameter was relatively small (1.96 mm in the 3D-OFDI arm and 2.13 mm in the angiography arm) and large SB has theoretically advantage from distal crossing. In particular, in the 3D-OFDI arm, only one LM bifurcation was included despite randomization (8 in the angiography arm); (3) in the present study, the severity of the SB lesions was mild to moderate (30.5% in the 3D-OFDI arm and 27.3% in the angiography arm) and resulted in a few inclusions of the true bifurcation (19.3% in the 3D-OFDI arm and 7.4% in the angiography arm). The bifurcation lesions with severe SB stenosis can further benefit from distal crossing and the achievement of distal crossing in these lesions seems difficult even under the 3D-OFDI guidance due to limited workspace for the wire; (4) theoretically, the narrow angle between MB and SB may advantageously allow distal crossing and the bifurcation angle in the present trial was indeed relatively narrow (53.3° in the 3D-OFDI arm and 54.0° in the angiography arm). Overall, it is impossible to discriminate the effect of these 4 factors on acute ISA in the present trial because of limited sample size and unbalanced bifurcation lesion characteristics. Further trial with more complex and higher risk bifurcation lesion is needed to address this issue.
Limitations
The present study has several limitations. First, the clinical relevance of the overhanging struts in the bifurcation cannot be proven because of the limited sample size and the lack of clinical follow-up. The study was not designed to evaluate clinical outcomes and the impact of difference in ISA at bifurcation on clinical outcomes remains to be elucidated. Furthermore, in the primary end point of the present trial, the malapposition was strictly limited to few struts across the origin of the SB appropriately quantified in this mechanistic evaluation of the 2 strategies of implantation. However, this limited difference in malapposition may be insufficient to influence the clinical outcome. Second, the allocation of guidance strategy was not blinded for the operator; therefore, there may be an inborn risk of bias toward the technology. Third, the generalizability of the LM bifurcation results is limited because of a low prevalence and uneven distribution of LM bifurcation (1.8% in the 3D-OFDI arm versus 14.8% in the angiography arm). Along the same line, a low prevalence of true bifurcation and relatively small mean SB diameter may limit the generalizability of the 3D-OFDI-guided bifurcation PCI, although these lesions theoretically might benefit from OCT guidance. Fourth, KBD was mandatory in the present trial, although a clinical advantage of KBD after crossover stenting is controversial.19,20 A main concern with KBD is the stent deformation in the proximal MV; therefore, POT after KBD is recommended by the European Bifurcation Club9 to avoid the elliptical shape of stent dilation in proximal MV. However, in the present trial, POT after KBD was not mandatory according to the protocol and performed in minority of lesions (12.7% in the 3D-OFDI arm and 16.0% in the angiography arm). Fifth, preprocedural OFDI assessment was performed in 96.3% of lesions in the angiography guidance arm, which may result in similar minimum and mean stent area between both arms (Table 4). Furthermore, the ISA in proximal and distal main branch did not differ between the 2 arms probably because of mandated POT and high adoption rate of preprocedural OFDI assessment in the angiography arm (Table III in the Data Supplement). Finally, in the angiography guidance arm, final OFDI was mandatory for documentation which may affect the amount of contrast media, radiation time, and procedure time among patients in this arm. Furthermore, in the 3D-OFDI arm, the operator may have intended to save angiographic contrast medium and shorten the radiation and procedure time in the context of an open-label design.
Conclusions
In a series of predominantly non-LM bifurcation lesions, online 3D-OFDI-guided PCI demonstrated excellent feasibility and was superior to angiography guidance in reducing acute ISA at bifurcation. Three-dimensional-OFDI imaging guidance may therefore be preferable in bifurcation PCI. Further trials are warranted to confirm the long-term clinical benefit of these favorable mechanical findings.
Sources of Funding
This study was sponsored by Meditrix with grant from Terumo Corporation.
Disclosures
Dr Sotomi reports personal fees from Terumo Corporation, during the conduct of the study; personal fees from Bayer, personal fees from Daiichi-Sankyo, personal fees from Amgen Astellas BioPharma, personal fees from Boehringer Ingelheim, personal fees from Bristole-Myers Squibb, personal fees from Abbott Vascular Japan, personal fees from Boston Scientific Japan, personal fees from Cardinal Health, personal fees from Medtronic, personal fees from Biosensors, outside the submitted work. Dr Muramatsu reports research grants to Fujita Health University from Terumo Corporation, Tokyo, Japan. Dr Ozaki reports research grants to Fujita Health University from Terumo Corporation, Tokyo, Japan. Dr Serruys reports personal fees from Abbott Laboratories, AstraZeneca, Biotronik, GLG Research, Medtronic, Sino Medical Sciences Technology, Société Europa Digital Publishing, Stentys France, Svelte Medical Systems, Philips/Volcano, St Jude Medical, Qualimed, and Xeltis, outside the submitted work. Dr Okamura reports personal fees from Terumo Corporation, during the conduct of the study; personal fees from Abbot Vascular Japan, personal fees from Medtronic, personal fees from Edwards Life Science, personal fees from Boston Scientific Japan, personal fees from Daiichi Sankyo, personal fees from Astellas, personal fees from Boehringer Ingelheim, personal fees from MSD, personal fees from Sanofi, personal fees from Tanabe Mitsubishi, outside the submitted work. The other authors report no conflicts.
Supplementary Material
Footnotes
Nonstandard Abbreviations and Acronyms
- 3D
- 3-dimensional
- DES
- drug-eluting stent
- FKBD
- final kissing balloon dilatation
- ISA
- incomplete stent apposition
- MV
- main vessel
- OCT
- optical coherence tomography
- OFDI
- optical frequency domain imaging
- OPTIMUM
- Online 3-Dimensional Optical Frequency Domain Imaging to Optimize Bifurcation Stenting Using UltiMaster Stent
- PCI
- percutaneous coronary intervention
- SB
- side branch
Drs Onuma and Kogame contributed equally to this work.
The Data Supplement is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCINTERVENTIONS.120.009183.
For Sources of Funding and Disclosures, see page 365.
Contributor Information
Norihiro Kogame, Email: kamexon@gmail.com.
Yohei Sotomi, Email: sotomiyohei@gmail.com.
Yosuke Miyazaki, Email: yskmiyazaki@gmail.com.
Taku Asano, Email: ta.brilliantsea@gmail.com.
Kuniaki Takahashi, Email: kuniaki.t.0125@gmail.com.
Hideyuki Kawashima, Email: h.kawashima429@gmail.com.
Masafumi Ono, Email: ono.msfm@gmail.com.
Yuki Katagiri, Email: ykatagiri.ggl@gmail.com.
Hiroyuki Kyono, Email: h.kyono@gmail.com.
Shimpei Nakatani, Email: shimpei1979@gmail.com.
Takashi Muramatsu, Email: takam0401@gmail.com.
Faisal Sharif, Email: faisal.sharif@nuigalway.ie.
Yukio Ozaki, Email: yukio.ozaki7@gmail.com.
Patrick W. Serruys, Email: patrick.w.j.c.serruys@gmail.com.
References
- 1.Lassen JF, Holm NR, Stankovic G, Lefèvre T, Chieffo A, Hildick-Smith D, Pan M, Darremont O, Albiero R, Ferenc M, et al. Percutaneous coronary intervention for coronary bifurcation disease: consensus from the first 10 years of the European bifurcation club meetings. EuroIntervention. 2014;10:545–560. doi: 10.4244/EIJV10I5A97 [DOI] [PubMed] [Google Scholar]
- 2.Asakura T, Karino T. Flow patterns and spatial distribution of atherosclerotic lesions in human coronary arteries. Circ Res. 1990;66:1045–1066. doi: 10.1161/01.res.66.4.1045 [DOI] [PubMed] [Google Scholar]
- 3.Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165. doi: 10.1093/eurheartj/ehy394 [DOI] [PubMed] [Google Scholar]
- 4.Banning AP, Lassen JF, Burzotta F, Lefèvre T, Darremont O, Hildick-Smith D, Louvard Y, Stankovic G. Percutaneous coronary intervention for obstructive bifurcation lesions: the 14th consensus document from the European bifurcation club. EuroIntervention. 2019;15:90–98. doi: 10.4244/EIJ-D-19-00144 [DOI] [PubMed] [Google Scholar]
- 5.Onuma Y, Katagiri Y, Burzotta F, Holm NR, Amabile N, Okamura T, Mintz GS, Darremont O, Lassen JF, Lefèvre T, et al. Joint consensus on the use of OCT in coronary bifurcation lesions by the European and Japanese bifurcation clubs. EuroIntervention. 2019;14:e1568–e1577. doi: 10.4244/EIJ-D-18-00391 [DOI] [PubMed] [Google Scholar]
- 6.Okamura T, Onuma Y, Garcia-Garcia HM, Bruining N, Serruys PW. High-speed intracoronary optical frequency domain imaging: implications for three-dimensional reconstruction and quantitative analysis. EuroIntervention. 2012;7:1216–1226. doi: 10.4244/EIJV7I10A194 [DOI] [PubMed] [Google Scholar]
- 7.Okamura T, Onuma Y, Yamada J, Iqbal J, Tateishi H, Nao T, Oda T, Maeda T, Nakamura T, Miura T, et al. 3D optical coherence tomography: new insights into the process of optimal rewiring of side branches during bifurcational stenting. EuroIntervention. 2014;10:907–915. doi: 10.4244/EIJV10I8A157 [DOI] [PubMed] [Google Scholar]
- 8.Miyazaki Y, Muramatsu T, Asano T, Katagiri Y, Sotomi Y, Nakatani S, Takahashi K, Kogame N, Higuchi Y, Ishikawa M, et al. On-line three-dimensional OFDI guided PCI vs. angiography guided in bifurcation lesions: design and rationale of the randomized OPTIMUM trial. EuroIntervention. 2019;40:EIJ-D-18-00902 doi: 10.4244/EIJ-D-18-00902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lassen JF, Burzotta F, Banning AP, Lefèvre T, Darremont O, Hildick-Smith D, Chieffo A, Pan M, Holm NR, Louvard Y, et al. Percutaneous coronary intervention for the left main stem and other bifurcation lesions: 12th consensus document from the European bifurcation club. EuroIntervention. 2018;13:1540–1553. doi: 10.4244/EIJ-D-17-00622 [DOI] [PubMed] [Google Scholar]
- 10.Nakatani S, Sotomi Y, Ishibashi Y, Grundeken MJ, Tateishi H, Tenekecioglu E, Zeng Y, Suwannasom P, Regar E, Radu MD, et al. Comparative analysis method of permanent metallic stents (XIENCE) and bioresorbable poly-L-lactic (PLLA) scaffolds (Absorb) on optical coherence tomography at baseline and follow-up. EuroIntervention. 2016;12:1498–1509. doi: 10.4244/EIJY15M10_03 [DOI] [PubMed] [Google Scholar]
- 11.Okamura T, Nagoshi R, Fujimura T, Murasato Y, Yamawaki M, Ono S, Serikawa T, Hikichi Y, Norita H, Nakao F, et al. Impact of guidewire recrossing point into stent jailed side branch for optimal kissing balloon dilatation: core lab 3D optical coherence tomography analysis. EuroIntervention. 2018;13:e1785–e1793. doi: 10.4244/EIJ-D-17-00591 [DOI] [PubMed] [Google Scholar]
- 12.Onuma Y, Thuesen L, van Geuns RJ, van der Ent M, Desch S, Fajadet J, Christiansen E, Smits P, Holm NR, Regar E, et al. ; TROFI Investigators. Randomized study to assess the effect of thrombus aspiration on flow area in patients with ST-elevation myocardial infarction: an optical frequency domain imaging study–TROFI trial. Eur Heart J. 2013;34:1050–1060. doi: 10.1093/eurheartj/ehs456 [DOI] [PubMed] [Google Scholar]
- 13.Garcia-Garcia HM, McFadden EP, Farb A, Mehran R, Stone GW, Spertus J, Onuma Y, Morel MA, van Es GA, Zuckerman B, et al. ; Academic Research Consortium. Standardized end point definitions for coronary intervention trials: the academic research consortium-2 consensus document. Circulation. 2018;137:2635–2650. doi: 10.1161/CIRCULATIONAHA.117.029289 [DOI] [PubMed] [Google Scholar]
- 14.Alegría-Barrero E, Foin N, Chan PH, Syrseloudis D, Lindsay AC, Dimopolous K, Alonso-González R, Viceconte N, De Silva R, Di Mario C. Optical coherence tomography for guidance of distal cell recrossing in bifurcation stenting: choosing the right cell matters. EuroIntervention. 2012;8:205–213. doi: 10.4244/EIJV8I2A34 [DOI] [PubMed] [Google Scholar]
- 15.Onuma Y, Grundeken MJ, Nakatani S, Asano T, Sotomi Y, Foin N, Ng J, Okamura T, Wykrzykowska JJ, de Winter RJ, et al. Serial 5-year evaluation of side branches jailed by bioresorbable vascular scaffolds using 3-dimensional optical coherence tomography: insights from the ABSORB cohort B trial (A clinical evaluation of the bioabsorbable everolimus eluting coronary stent system in the treatment of patients with de novo native coronary artery lesions). Circ Cardiovasc Interv. 2017;10:e004393 doi: 10.1161/CIRCINTERVENTIONS.116.004393 [DOI] [PubMed] [Google Scholar]
- 16.Foin N, Gutiérrez-Chico JL, Nakatani S, Torii R, Bourantas CV, Sen S, Nijjer S, Petraco R, Kousera C, Ghione M, et al. Incomplete stent apposition causes high shear flow disturbances and delay in neointimal coverage as a function of strut to wall detachment distance: implications for the management of incomplete stent apposition. Circ Cardiovasc Interv. 2014;7:180–189. doi: 10.1161/CIRCINTERVENTIONS.113.000931 [DOI] [PubMed] [Google Scholar]
- 17.Nakazawa G, Yazdani SK, Finn AV, Vorpahl M, Kolodgie FD, Virmani R. Pathological findings at bifurcation lesions: the impact of flow distribution on atherosclerosis and arterial healing after stent implantation. J Am Coll Cardiol. 2010;55:1679–1687. doi: 10.1016/j.jacc.2010.01.021 [DOI] [PubMed] [Google Scholar]
- 18.Diletti R, Farooq V, Muramatsu T, Gogas BD, Garcia-Garcia HM, van Geuns RJ, Serruys PW. Serial 2- and 3-dimensional visualization of side branch jailing after metallic stent implantation: to kiss or not to kiss.? JACC Cardiovasc Interv. 2012;5:1089–1090. doi: 10.1016/j.jcin.2012.04.013 [DOI] [PubMed] [Google Scholar]
- 19.Niemelä M, Kervinen K, Erglis A, Holm NR, Maeng M, Christiansen EH, Kumsars I, Jegere S, Dombrovskis A, Gunnes P, et al. ; Nordic-Baltic PCI Study Group. Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic bifurcation study III. Circulation. 2011;123:79–86. doi: 10.1161/CIRCULATIONAHA.110.966879 [DOI] [PubMed] [Google Scholar]
- 20.Kim YH, Lee JH, Roh JH, Ahn JM, Yoon SH, Park DW, Lee JY, Yun SC, Kang SJ, Lee SW, et al. Randomized comparisons between different stenting approaches for bifurcation coronary lesions with or without side branch stenosis. JACC Cardiovasc Interv. 2015;8:550–560. doi: 10.1016/j.jcin.2015.01.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


