Abstract
We write this manuscript amid a global pandemic and a heightened awareness of the underlying structural racism in the United States (US), unmasked by the recent killing of George Floyd and multiple other unarmed Black Americans (Spring 2020). Our purpose is to highlight the role of social determinants of health (SDOH) on stroke disparities, to inspire dialogue, to encourage research to deepen our understanding of the mechanism by which SDOH impact stroke outcomes, and to develop strategies to address SDOH and reduce stroke racial/ethnic disparities. We begin by defining SDOH and health disparities in today’s context; we then move to discussing SDOH and stroke, particularly secondary stroke prevention, and conclude with possible approaches to addressing SDOH and reducing stroke disparities. These approaches include: 1) building on prior work; 2) enhancing our understanding of populations and sub-populations, including intersectionality, of people who experience stroke disparities; 3) prioritizing populations and points along the stroke care continuum when racial/ethnic disparities are most prominent; 4) understanding how SDOH impact stroke disparities in order to test SDOH interventions that contribute to the disparity; 5) partnering with communities; and 6) exploring technologic innovations. By building on the prior work and expanding efforts to address SDOH, we believe that stroke disparities can be reduced.
We write this manuscript amid a global pandemic and a heightened awareness of the underlying structural racism in the United States (US), unmasked by the recent killing of George Floyd and multiple other unarmed Black Americans (Spring 2020). Despite much uncertainty, we do know that the normal we knew cannot be the normal of our future. We are hopeful that we, as stroke clinicians and researchers, and we, as a country, can take a hard look at the disparate health outcomes in the US, recognize the injustice, and create revolutionary change to ensure health equity. The purpose of this manuscript is to highlight the role of the fundamental causes of disease and intermediate social determinants on stroke disparities, and to encourage dialogue and strategies to address SDOH and reduce stroke racial/ethnic disparities. We begin by defining social determinants of health (SDOH) and health disparities in today’s context, we then move to discussing SDOH and stroke outcomes, and conclude with possible strategies to address SDOH.
The Coronavirus disease 2019 (COVID-19) pandemic has revealed the precarious state of our racial and ethnic historically disadvantaged populations. COVID-19 is disproportionally impacting Black and Latinx populations who are more likely to be infected and more likely to die from COVID-19 than Non-Hispanic White Americans.1–3 For example, Black people comprise about 14% of Michigan’s population, yet Black people comprise 35% of Michigan cases and 40% of the COVID-19 deaths.4 Similarly, in New York City, Black and Latinx Americans are about two times more likely to die from complications of COVID-19 as compared to Non-Hispanic White Americans.5 Limited data also indicate disparities among American Indian, Alaska Native populations, and Pacific Islander populations.6 The US experience of COVID-19 has highlighted health disparities and the important role of SDOH.1 With regards to stroke, COVID-19 may impact stroke directly and indirectly and may exacerbate disparities.7–9 For example, hospital presentations for acute stroke declined at the start of the COVID-19 pandemic,10 and this decline may have been even greater among Black stroke patients.8 Public health experts have long recognized the strong association between SDOH and health inequities but have encountered significant structural, political, individual and other barriers in trying to address these critical health issues.
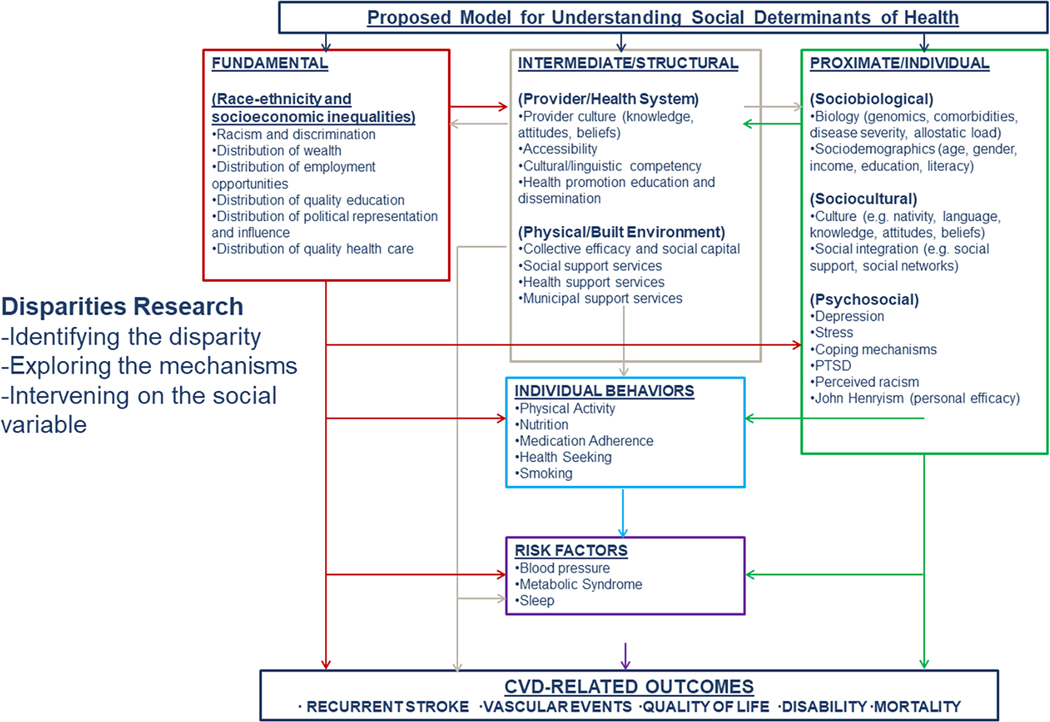
The World Health Organization defines the SDOH as the conditions in which people are born, grow, work, live and age, and the wider set of forces and systems shaping the conditions of daily life.11 SDOH are non-clinical and non-biological social factors that impact health. SDOH include fundamental causes of disease such as racism and discrimination, unequal distribution of power, income, wealth, and education, societal values of equity and fairness that impact health directly and indirectly via intermediate structural factors including health care access, health care quality, support services, housing and transportation and intermediate individual factors (Figure).11–13 These upstream factors then contribute to disparities related to individual behaviors, risk factors, and ultimately health outcomes, including morbidity and mortality. Social determinants can alter the experience of chronic diseases, infectious diseases, and significantly impact quality of life across the lifespan. In many instances, the social inequalities related to these health determinants disproportionately impact racial/ethnic historically disadvantaged populations.
Figure legend:
Reproduced from Environmental Health Perspectives with permission from the authors. Modified from Schulz, et al 12005:113:1817-182513
Healthy People 2020 defines health disparity as a “particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; gender; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to racism, discrimination, or exclusion.”14 To address racial/ethnic health disparities, interventions cannot solely improve health in racial and ethnic historically disadvantaged populations, but must also decrease or eliminate gaps in disease risk and outcomes between racial and ethnic historically disadvantaged populations and non-Hispanic White populations.
Conceptualizing Social Determinants of Health and Stroke
Stroke is a disease of disparities. Indeed every aspect of the stroke continuum from prevention through treatment to recovery is associated with differential gradients by race-ethnicity.15 Fundamental causes of disease, including structural racism, and intermediate structural factors such as long-standing inequities in education, access to care, access to healthy foods, and others may underlie many of these disparities. Some stroke disparities are access focused. For example, racial and ethnic historically disadvantaged populations are less likely to access emergency medical services and are more likely to have delayed arrival at the Emergency Department.16, 17 Some of the disparities may be the result of educational and socioeconomic differences, awareness of stroke signs and symptoms, language barriers, and reluctance to seek attention because of immigration status.15, 18 Finally, stigma and discrimination through implicit bias and structural racism may contribute to psychological stress and increase the risk of poor outcomes.19, 20 Thus, addressing SDOH is important to reducing stroke disparities.
Social Determinants in Secondary Stroke Prevention
Within the first year of stroke, over 10% of stroke survivors have a recurrent stroke with up to 30% over 5 years.21 Studies indicate that Black people have a higher risk of recurrent stroke than Non-Hispanic White people,22–24 although findings are mixed.25 Data are more limited among Latinx populations, and particularly lacking among those who are not Mexican American. Notably, among Mexican Americans the disparity in recurrent stroke has declined over time such that there was no longer evidence of a stroke recurrence disparity in a population based stroke surveillance study.26 Hypertension is a prominent risk factor for recurrent stroke. Yet, stroke survivors are more likely to have unrecognized hypertension, and among those with known hypertension, less likely to have controlled blood pressure than those without a stroke.27 Additionally, studies demonstrate that Black stroke survivors are more likely to have hypertension and are more likely to have uncontrolled BP following stroke as compared to non-Hispanic White stroke survivors.27–30
Treatment of hypertension may reduce the risk of recurrent stroke, and as such guidelines recommend strategies to achieve this goal.31, 32,33 Yet, although hypertension is readily treatable through behavior modifications, such as healthy eating and physical activity, and maintenance of medication therapy, reducing hypertension remains a challenge among stroke survivors.34 Recent interventions have been mixed in demonstrating efficacious risk reduction.35–37
One reason for the mixed efficacy may be that many secondary stroke prevention interventions focus on the individual without taking into consideration SDOH, often having limited focus on the context within which the person lives and the systems within which they seek care. Evidence is accumulating that incremental increases in the burden of the SDOH are associated with hypertension and stroke incidence.38, 39 Regarding context, Black and Latinx people often faced numerous barriers to their health prior to their stroke and as stroke survivors these challenges may be enhanced by the disproportionate disability experienced by Black and Mexican American stroke survivors compared to non-Hispanic White stroke survivors.40–42 For example, a stroke survivor’s opportunity to exercise and maintain a healthy diet may be limited if their neighborhood has poor walkability and lacks healthy food options.43 Furthermore, their ability to access medical care and maintain their medication therapy may be reduced due to expense, insurance or unreliable public transportation or ride sharing.44 A recent Cochrane review of secondary stroke prevention found that organizational interventions may improve blood pressure control, while interventions that solely focus on patient-level barriers to BP control had no impact on BP reduction or control.34 We believe that SDOH are a significant contributor to disparities in health and that addressing the fundamental causes of disease as well as the more intermediate SDOH may improve the health of stroke survivors.
Consideration of strategies to address fundamental causes of disease and intermediate social determinants in secondary stroke prevention
Addressing both the fundamental causes of disease and the intermediate SDOH may decrease stroke disparities. One approach to addressing the fundamental causes of disease, structural racism, discrimination, power and income and wealth inequality, is to enact local, state and national policy measures to promote equity.45 While this may be beyond the scope of the stroke community, we believe our role is to inform that policy through health services and epidemiologic research, creation and rigorous testing of interventions, and by being faithful allies and advocates with our patients and communities as they advocate on behalf of their needs. For example, we found that insurance status and insurance coverage were associated with utilization of post-acute care among working age stroke survivors, which could inform policy on Medicaid expansion and coverage.46, 47
Addressing the intermediate SDOH such as access to medical care and the built environment may be more readily within the scope of influence of the stroke community. We believe that we can design interventions that have a social determinant focus that move beyond improving, for example access to stroke care for everyone, to interventions that reduce the racial and ethnic gap in access to medical care. One example of an intervention that reduced the ethnic gap in secondary stroke prevention is the DESERVE trial.36 DESERVE was a multi-ethnic randomized clinical trial that focused on improving self-efficacy through a community worker and patient narrative skills based intervention. While not powered for analysis by race/ethnicity, DESERVE demonstrated significant hypertension reduction among Latinx participants while no differences were found among White and Black participants.
To stimulate discussion on approaches to addressing SDOH and reducing stroke disparities, we present some options in the context of stroke survivors:
Learn from Prior Interventions
Over the past decade, there has been progress towards reducing stroke disparities. We believe that our work could evolve further by continuing to work together and learning from each other. While interventions focusing on stroke survivors cannot be directly compared, we advocate for qualitative comparison across interventions, with an emphasis on strategies taken to address specific drivers of disparities and SDOH. We urge those interested in and those who have studied stroke SDOH and racial/ethnic disparities and those who have performed interventions to start a dialogue. While every study population, setting and intervention are different, we believe there is much to be learned across populations and interventions. We believe that only by reflecting on and evaluation of what went right and what went wrong can we make progress toward reducing disparities.
Enhance our Understanding of Populations and Sub-Populations who Experience Stroke Disparities
To date most of the stroke disparities research has focused on Black and Latinx populations. Expanding our work to include understanding and addressing inequities faced by American Indians, Alaska Natives, Asians, Native Hawaiians, Pacific islanders and others is needed. In addition, within Black and Latinx populations, there are sub-populations who have different experiences and different risks. For example, while people of Mexican origin comprise the largest proportion of the Latinx population, other Latinx origin groups have populations in the US of over 1 million, including Puerto Rico, El Salvador, Cuba, Dominican Republic, Guatemala and Colombia and these Latinx sub-populations may face unique challenges and have varying vascular risk factor profiles. Similarly, recent Latinx immigrants likely face different challenges than 3rd generation Latinx individuals or likewise recent Black immigrants may face different challenges than Black people whose ancestors have lived in the US for several generations. In addition, further consideration of the role of intersectionality such as sex, socioeconomic status, gender identity, sexual orientation and race/ethnicity on disparities is warranted. Understanding unique, high risk populations begins by collecting data to identify the sub-populations and intersectionality which then allows interventions to be tailored to the population specific needs.
Prioritizing Populations and Points along the Stroke Care Continuum when Racial/Ethnic Disparities are most Prominent
Stroke care can be thought of in stages across the care continuum from stroke incidence to acute stroke hospitalization to post-acute care to stroke survivorship. Stroke disparities may vary in magnitude and the degree to which interventions may reduce the disparity. For example, racial differences in stroke incidence and prevalence comparing Black Americans and Non-Hispanic White Americans are persistent,48, 49 while ethnic differences in incidence among Mexican Americans is declining.50 These examples are not meant to be a comprehensive review or meta-analysis but are meant to encourage critical evaluation and prioritization of populations and points along the stroke care continuum most in need of intervention.
Understanding how SDOH Impact Stroke Disparities in order to Test SDOH Interventions that are Contributing to the Disparity
In clinical practice, social risk-informed care and social risk-targeted care are two approaches to addressing unmet social needs.51 In social risk-informed care, traditional healthcare delivery is adapted according to information about patients’ social needs. Utilization of medical translation services, extending clinic hours, querying food insecurity before prescribing medications, and increasing point of care testing are examples of social risk-informed care adaptations. This type of care likely requires trust between the patient and provider to develop tailored strategies for addressing stroke needs in the context of social needs and healthy system modification to identify and mitigate risk at a structural level. In social-risk targeted care, clinical encounters are leveraged to reduce patients’ unmet social needs. While the processes for screening for unmet social needs have evolved, there may be multiple barriers to implementing these screening tools into practice.52 Because SDOH concerns have traditionally fallen outside of medical care, these program typically rely on community resources to address the SDOH needs.53 Yet, community resources may not exist. For example, lack of adequate community resources may have contributed to lack of effectiveness of stroke survivor interventions.54, 55 Overall, there is lack of evidence of the effectiveness of both social risk- informed care and social risk-targeted care; yet the field is rapidly evolving and evidence will accumulate to guide clinical best practices.51, 56–58
With regards to stroke, SDOH likely impact health differently along various stages of the stroke care continuum. Both a better understanding of the mechanistic pathways whereby SDOH contribute to stroke disparities and development of effective interventions to address the modifiable drivers of disparities on this mechanistic pathway are needed. More specifically, identifying SDOH through primary and secondary data and understanding their causal mechanisms in stroke disparities across the stroke care continuum, from primary stroke prevention to stroke survivorship, will inform intervention development and testing and ultimately lead to guidelines and widespread implementation of effective interventions.
Partner with Communities
Much of health is outside the healthcare system and in the community.59 The community social and political structure, community needs, and community strengths and challenges are often opaque to stroke providers and researchers necessitating academic-community partnerships. Community engagement could range from equitable partnership such as in Community Based Participatory Research60 to other forms of community engagement such as formation of community advisory boards or community ethics review boards which may be better suited for certain topics or situations. We are agnostic to the form of community engagement but strongly advocate for some form of community engagement.
Community engagement is important for several reasons including: 1) ensuring the clinical care and research topics are community placed, identified as a community need and the interventions are culturally congruent with the community; 2) building in sustainability from the start—there has been increasing recognition in the field of implementation science that intervention sustainability is best established from the start; 3) academic and community bi-directional learning.61 For academic partners and providers this often includes a deeper understanding of how the SDOH impact the health of the community and their patients.
Technological Innovation
One criticism of technology is that it solves ‘problems of convenience but does not cure the sick’.62 However, this is beginning to change. Since the start of the COVID pandemic we have seen an unprecedented uptake of tele-health. In addition, the evolution of wearables and remote patient monitoring promotes greater opportunity for self-management and care outside of the clinic. Technology is exciting because it is scalable and may offer more cost-efficient solutions. As health technology evolves it will be important to remain mindful of SDOH so that the promise of health technology promotes equity.
Conclusion
We leave you with three points: 1) it is important to not only improve the health of racial and ethnic historically disadvantaged populations but also to reduce the gaps in health experienced by these populations; 2) understanding the social determinants among populations and specific sub-populations is critical to inclusivity; and 3) strategies to reduce racial/ethnic disparities include informing policies to address the fundamental causes of disease and designing social determinant focused interventions to address the intermediate social determinants. In conclusion, we are hopeful in response to the dual crisis, the COVID-19 pandemic and the killing of George Floyd and countless others unarmed Black Americans, that now is the start of real change in the recognition of the role of SDOH and needed actions to reduce stroke disparities. To this point, National Institute of Neurologic Disorders and Stroke (NINDS), currently has a request for information related to research on health disparities and inequities in neurological disorders which we would like to encourage broad participation. Finally, we strongly support the recent call for an embrace of the moral determinants of health, a collective endeavor for securing the health of communities.59 By working together to address SDOH, we believe that stroke disparities can be reduced.
Acknowledgments
Funding: NIH/NIMHD U01MD010579 (Skolarus)
Abbreviations:
- (SDOH)
social determinants of health
- (NINDS)
National Institute of Neurologic Disorders and Stroke
Footnotes
Disclosures: The authors have no relevant disclosures
References
- 1.Yancy CW. Covid-19 and african americans. JAMA. 2020 [DOI] [PubMed] [Google Scholar]
- 2.The coronavirus is infecting and killing black americans at an alarmingly high rate. https://www.washingtonpost.com/nation/2020/04/07/coronavirus-is-infecting-killing-black-americans-an-alarmingly-high-rate-post-analysis-shows/. Accessed April 19, 2020.
- 3.Chow DS, Soun J, Gavis-Bloom J, Weinberg B, Chang P, Mutasa S, Monuki E, Park JI, Xie X, Bota D. The disproportionate rise in covid-19 cases among hispanic/latinx in disadvantaged communities of orange county, california: A socioeconomic case-series. medRxiv. 2020 [Google Scholar]
- 4.African Americans lead in coronavirus cases, deaths in Michigan; https://www.freep.com/story/news/local/michigan/2020/04/02/michigan-coronavirus-by-race-deaths-african-americans-tests-covid-19/5116025002/. Accessed April 7, 2020.
- 5.Nyc health. Covid-19: Data. https://www1.nyc.gov/site/doh/covid/covid-19-data.page. Accessed August 6, 2020.
- 6.Webb Hooper M, Napoles AM, Perez-Stable EJ. Covid-19 and racial/ethnic disparities. JAMA. 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katz JM, Libman RB, Wang JJ, Sanelli P, Filippi CG, Gribko M, Pacia SV, Kuzniecky RI, Najjar S, Azhar S. Cerebrovascular complications of covid-19. Stroke. 2020;0:STROKEAHA120031265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cummings C, Almallouhi E, Kasab SA, Spiotta AM, Holmstedt CA. Blacks are less likely to present with strokes during the covid-19 pandemic. Stroke.0:STROKEAHA.120.031121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lowenstein CJ, Solomon SD. Severe covid-19 is a microvascular disease. Circulation. 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsiao J, Sayles E, Antzoulatos E, Stanton RJ, Sucharew H, Broderick JP, Demel SL, Flaherty ML, Grossman AW, Kircher C, et al. Effect of covid-19 on emergent stroke care. Stroke.0:STROKEAHA.120.030499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Healthy people 2020: Social determinants. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed April 19, 2019.
- 12.Marmot M. Social determinants of health inequalities. The Lancet. 2005;365:1099–1104 [DOI] [PubMed] [Google Scholar]
- 13.Schulz AJ, Kannan S, Dvonch JT, Israel BA, Allen A 3rd, James SA, House JS, Lepkowski J. Social and physical environments and disparities in risk for cardiovascular disease: The healthy environments partnership conceptual model. Environmental health perspectives. 2005;113:1817–1825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Healthy people 2020: Disparities. https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities#6. Accessed April 19, 2020.
- 15.Cruz-Flores S, Rabinstein A, Biller J, Elkind MSV, Griffith P, Gorelick PB, Howard G, Leira EC, Morgenstern LB, Ovbiagele B, et al. Racial-ethnic disparities in stroke care: The american experience. Stroke. 2011;42:2091–2116 [DOI] [PubMed] [Google Scholar]
- 16.Ekundayo OJ, Saver JL, Fonarow GC, Schwamm LH, Xian Y, Zhao X, Hernandez AF, Peterson ED, Cheng EM. Patterns of emergency medical services use and its association with timely stroke treatment: Findings from get with the guidelines-stroke. Circulation: Cardiovascular Quality and Outcomes. 2013 [DOI] [PubMed] [Google Scholar]
- 17.Tong D, Reeves MJ, Hernandez AF, Zhao X, Olson DM, Fonarow GC, Schwamm LH, Smith EE. Times from symptom onset to hospital arrival in the get with the guidelines–stroke program 2002 to 2009. Stroke. 2012 [DOI] [PubMed] [Google Scholar]
- 18.Hsia AW, Edwards DF, Morgenstern LB, Wing JJ, Brown NC, Coles R, Loftin S, Wein A, Koslosky SS, Fatima S, et al. Racial disparities in tissue plasminogen activator treatment rate for stroke. Stroke. 2011;42:2217–2221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams O, Ovbiagele B. Stroking out while black-the complex role of racism. JAMA Neurol. 2020 [DOI] [PubMed] [Google Scholar]
- 20.Spruill TM, Butler MJ, Thomas SJ, Tajeu GS, Kalinowski J, Castañeda SF, Langford AT, Abdalla M, Blackshear C, Allison M, et al. Association between high perceived stress over time and incident hypertension in black adults: Findings from the jackson heart study. Journal of the American Heart Association. 2019;8:e012139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohan KM, Wolfe CD, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP. Risk and cumulative risk of stroke recurrence: A systematic review and meta-analysis. Stroke. 2011;42:1489–1494 [DOI] [PubMed] [Google Scholar]
- 22.Albright KC, Huang L, Blackburn J, Howard G, Mullen M, Bittner V, Muntner P, Howard V. Racial differences in recurrent ischemic stroke risk and recurrent stroke case fatality. Neurology. 2018;91:e1741-e1750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kamel H, Zhang C, Kleindorfer DO, Levitan EB, Howard VJ, Howard G, Soliman EZ, Johnston SC. Association of black race with early recurrence after minor ischemic stroke or transient ischemic attack: Secondary analysis of the point randomized clinical trial. JAMA Neurology. 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park JH, Ovbiagele B. Association of black race with recurrent stroke risk. J Neurol Sci. 2016;365:203–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Howard G, Kissela BM, Kleindorfer DO, McClure LA, Soliman EZ, Judd SE, Rhodes JD, Cushman M, Moy CS, Sands KA. Differences in the role of black race and stroke risk factors for first vs recurrent stroke. Neurology. 2016;86:637–642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sozener CB, Lisabeth LD, Shafie-Khorassani F, Kim S, Zahuranec DB, Brown DL, Skolarus LE, Burke JF, Kerber KA, Meurer WJ. Trends in stroke recurrence in mexican americans and non-hispanic whites. Stroke. 2020:STROKEAHA. 120.029376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brenner DA, Zweifler RM, Gomez CR, Kissela BM, Levine D, Howard G, Coull B, Howard VJ. Awareness, treatment, and control of vascular risk factors among stroke survivors. J Stroke Cerebrovasc Dis. 2010;19:311–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pergola PE, White CL, Szychowski JM, Talbert R, Brutto Od, Castellanos M, Graves JW, Matamala G, Pretell EJ, Yee J, et al. Achieved blood pressures in the secondary prevention of small subcortical strokes (sps3) study: Challenges and lessons learned. American Journal of Hypertension. 2014;27:1052–1060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zahuranec DB, Wing JJ, Edwards DF, Menon RS, Fernandez SJ, Burgess RE, Sobotka IA, German L, Trouth AJ, Shara NM, et al. Poor long-term blood pressure control after intracerebral hemorrhage. Stroke. 2012;43:2580–2585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White CL, Pergola PE, Szychowski JM, Talbert R, Cervantes-Arriaga A, Clark HD, Del Brutto OH, Godoy IE, Hill MD, Pelegrí A, et al. Blood pressure after recent stroke: Baseline findings from the secondary prevention of small subcortical strokes trial. American Journal of Hypertension. 2013;26:1114–1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Katsanos AH, Filippatou A, Manios E, Deftereos S, Parissis J, Frogoudaki A, Vrettou A-R, Ikonomidis I, Pikilidou M, Kargiotis O. Blood pressure reduction and secondary stroke prevention: A systematic review and metaregression analysis of randomized clinical trials. Hypertension. 2017;69:171–179 [DOI] [PubMed] [Google Scholar]
- 32.Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, Woodward M, MacMahon S, Turnbull F, Hillis GS. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: Updated systematic review and meta-analysis. The Lancet. 2016;387:435–443 [DOI] [PubMed] [Google Scholar]
- 33.Group SS. Blood-pressure targets in patients with recent lacunar stroke: The sps3 randomised trial. The Lancet. 2013;382:507–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bridgwood B, Lager KE, Mistri AK, Khunti K, Wilson AD, Modi P. Interventions for improving modifiable risk factor control in the secondary prevention of stroke. Cochrane Database of Systematic Reviews. 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feldman PH, McDonald MV, Trachtenberg M, Trifilio M, Onorato N, Sridharan S, Silver S, Eimicke J, Teresi J. Reducing hypertension in a poststroke black and hispanic home care population: Results of a pragmatic randomized controlled trial. American Journal of Hypertension. 2020;33:362–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boden-Albala B, Goldmann E, Parikh NS, Carman H, Roberts ET, Lord AS, Torrico V, Appleton N, Birkemeier J, Parides M, et al. Efficacy of a discharge educational strategy vs standard discharge care on reduction of vascular risk in patients with stroke and transient ischemic attack: The deserve randomized clinical trial. JAMA Neurology. 2019;76:20–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheng EM, Cunningham WE, Towfighi A, Sanossian N, Bryg RJ, Anderson TL, Barry F, Douglas SM, Hudson L, Ayala-Rivera M. Efficacy of a chronic care–based intervention on secondary stroke prevention among vulnerable stroke survivors: A randomized controlled trial. Circulation: Cardiovascular Quality and Outcomes. 2018;11:e003228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reshetnyak E, Ntamatungiro M, Pinheiro LC, Howard VJ, Carson AP, Martin KD, Safford MM. Impact of multiple social determinants of health on incident stroke. Stroke. 2020;51:2445–2453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.King JB, Pinheiro L, Ringel JB, Bress AP, Shimbo D, Muntner P, Reynolds K, Cushman M, Howard G, Manly J, et al. Abstract 13: Racial differences in the impact of multiple social vulnerabilities to health disparities and hypertension and death in the reasons for geographic and racial differences in stroke (regards) study. Circulation. 2020;141:A13–A13 [Google Scholar]
- 40.Cooper LA, Hill MN, Powe NR. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. Journal of General Internal Medicine. 2002;17:477–486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burke JF, Feng C, Skolarus LE. Divergent poststroke outcomes for black patients: Lower mortality, but greater disability. Neurology. 2019;93:e1664-e1674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lisabeth LD, Sánchez BN, Baek J, Skolarus LE, Smith MA, Garcia N, Brown DL, Morgenstern LB. Neurological, functional, and cognitive stroke outcomes in mexican americans. Stroke. 2014;45:1096–1101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morgenstern LB, Escobar JD, Sánchez BN, Hughes R, Zuniga BG, Garcia N, Lisabeth LD. Fast food and neighborhood stroke risk. Annals of neurology. 2009;66:165–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Levine DA, Kiefe CI, Houston TK, Allison JJ, McCarthy EP, Ayanian JZ. Younger stroke survivors have reduced access to physician care and medications: National health interview survey from years 1998 to 2002. Arch Neurol. 2007;64:37–42 [DOI] [PubMed] [Google Scholar]
- 45.Adler NE, Cutler DM, Jonathan J, Galea S, Glymour M, Koh HK, Satcher D. Addressing social determinants of health and health disparities. National Academy of Medicine. 2016:1–16 [Google Scholar]
- 46.Skolarus L, Meurer W, Burke J, Bettger JP, Lisabeth L. Effect of insurance status on postacute care among working age stroke survivors. Neurology. 2012;78:1590–1595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Skolarus LE, Burke JF, Morgenstern LB, Meurer WJ, Adelman EE, Kerber KA, Callaghan BC, Lisabeth LD. Impact of state medicaid coverage on utilization of inpatient rehabilitation facilities among patients with stroke. Stroke. 2014;45:2472–2474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Howard G, Moy CS, Howard VJ, McClure LA, Kleindorfer DO, Kissela BM, Judd SE, Unverzagt FW, Soliman EZ, Safford MM, et al. Where to focus efforts to reduce the black-white disparity in stroke mortality: Incidence versus case fatality? Stroke. 2016;47:1893–1898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, Khatri P, Adeoye O, Ferioli S, Broderick JP, et al. Stroke incidence is decreasing in whites but not in blacks: A population-based estimate of temporal trends in stroke incidence from the greater cincinnati/northern kentucky stroke study Stroke. 2010;41:1326–1331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lisabeth LD, Brown D, Zhang X, Kim S, Case E, Zahuranec D, Smith M, Morgenstern L. Abstract 87: Eighteen-year trends in ischemic stroke rates in a bi-ethnic population. Stroke. 2020;51:A87–A87 [Google Scholar]
- 51.Gottlieb L, Fichtenberg C, Alderwick H, Adler N. Social determinants of health: What’s a healthcare system to do? Journal of Healthcare Management. 2019;64:243–257 [DOI] [PubMed] [Google Scholar]
- 52.Implementing community resource referral technology: Facilitators and barriers described by early adopters. Health Affairs. 2020;39:662–669 [DOI] [PubMed] [Google Scholar]
- 53.Chaiyachati KH, Grande DT, Aysola J. Health systems tackling social determinants of health: Promises, pitfalls, and opportunities of current policies. Am J Manag Care. 2016;22:e393-e394 [PubMed] [Google Scholar]
- 54.Forster A, Young J. Specialist nurse support for patients with stroke in the community: A randomised controlled trial. BMJ (Clinical research ed.). 1996;312:1642–1646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Forster A, Young J, Chapman K, Nixon J, Patel A, Holloway I, Mellish K, Anwar S, Breen R, Knapp M. Cluster randomized controlled trial: Clinical and cost-effectiveness of a system of longer-term stroke care. Stroke. 2015;46:2212–2219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alderwick HAJ, Gottlieb LM, Fichtenberg CM, Adler NE. Social prescribing in the u.S. And england: Emerging interventions to address patients’ social needs. American Journal of Preventive Medicine. 2018;54:715–718 [DOI] [PubMed] [Google Scholar]
- 57.Gottlieb L, Cottrell EK, Park B, Clark KD, Gold R, Fichtenberg C. Advancing social prescribing with implementation science. The Journal of the American Board of Family Medicine. 2018;31:315. [DOI] [PubMed] [Google Scholar]
- 58.Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. American Journal of Preventive Medicine. 2017;53:719–729 [DOI] [PubMed] [Google Scholar]
- 59.Berwick DM. The moral determinants of health. JAMA. 2020 [DOI] [PubMed] [Google Scholar]
- 60.Springer MV, Skolarus LE. Community-based participatory research. Stroke. 2019;50:e48–e50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annual review of public health. 1998;19:173–202 [DOI] [PubMed] [Google Scholar]
- 62.The age of decadence. https://www.nytimes.com/2020/02/07/opinion/sunday/western-society-decadence.html. Accessed April 22, 2020.